Explore article hub
- 1Faculty of Health Sciences and Medicine, University of Lucerne, Lucerne, Switzerland
- 2Swiss Paraplegic Research (SPF), Nottwil, Switzerland
Abstract
The World Health Organization (WHO) concept of human functioning represents a new way of thinking about health that has wide-ranging consequences. This article explicates this paradigm shift, illustrates its potential impact, and argues that societies can profit by implementing functioning as the third indicator of health, complementing morbidity and mortality. Human functioning integrates biological health (the bodily functions and structures that constitute a person’s intrinsic health capacity) and lived health (a person’s actual performance of activities in interaction with their environment). It is key to valuing health both in relation to individual well-being and societal welfare—operationalizing the United Nations Sustainable Development Goal (SDG) 3 principle that health is a public good. Implementing functioning as defined and conceptualized in the International Classification of Functioning, Disability and Health (ICF) could profoundly benefit practices, research, education, and policy across health systems and health strategies and help integrate health and social systems. It also offers a foundation for reconceptualizing multidisciplinary health sciences and for augmenting epidemiology with information derived from peoples’ lived experiences of health. A new interdisciplinary science field—human functioning sciences—itself holds the promise to integrate research inputs and methods from diverse biomedical and social disciplines to provide a more comprehensive understanding of human health. To realize these opportunities, we must address formidable methodological, implementation, and communication challenges throughout health systems and broader society. This endeavor is vital to orientate health systems toward what matters most to people about health, to unlock the societal economic investment in health that is essential for individual and population-level well-being, and to drive progress toward achieving the SDGs.
Key points
- The concept of human functioning integrates biological health (the bodily functions and structures that constitute a person’s intrinsic health capacity) with lived health (a person’s actual performance of activities in interaction with their environment).
- Functioning is the bridge that links health to individual well-being and societal welfare—thereby accounting for the value of health and potentially unlocking investment and progress toward achieving United Nations Sustainable Development Goal (SDG) 3.
- A paradigm shift implementing human functioning as the third indicator of health (complementing mortality and morbidity) could profoundly benefit practices, research, and policy across health systems and health strategies.
- Functioning also provides a basis for reconceptualizing multidisciplinary health sciences; a new interdisciplinary science field—human functioning sciences—itself holds promise to integrate diverse research inputs and methods to provide a fuller understanding of human health.
- To realize the opportunities offered by this rethinking of health we must address formidable methodological, implementation, and communication challenges within health systems and society.
Introduction
At the core of the United Nations’ 2030 Agenda for Sustainable Development adopted in 2015 are the 17 Sustainable Development Goals (SDGs) that provide a “blueprint for peace and prosperity for people and the planet, now and into the future”. Among these goals is SDG3 Good Health and Well-being: “To ensure healthy lives and promote well-being for all at all ages” (1). Progress in the implementation of SDG3 is measured in terms of targets to reduce mortality and morbidity through public health measures and health system strengthening. These targets are interdependent and consistent with the other Goals that seek global agreement and concerted action on fundamental 21st-century development concerns, such as global poverty, hunger and inequality, environmental degradation, and weakening institutions. In recent years, the global situation has been made more dire by the COVID-19 pandemic, growing pressure on health services, and increased disparities in health outcomes between and within countries (2).
Academic discussions regarding SDG3 have criticized the adequacy of the indicators of mortality and morbidity (3–5), but little has been said about the purported link between health and well-being. Scholars standardly distinguish subjective from objective well-being: the former is analyzed into a composite of positive affect and cognitive evaluation or life satisfaction (6) and the latter either as a capability, the material conditions to achieve an individual life goal (7), or more generally as an opportunity to flourish (8). Yet there is general agreement that health is either a component or a determinant of individual well-being. There is also agreement that the provision of healthcare and public health are public goods that contribute to overall societal welfare. By contributing to individual well-being in the aggregate they enable everyone to realize their potential, thereby enhancing productivity, increasing social opportunity, and reducing inequalities, thus improving societal welfare (9, 10).
The wording of SDG3 nonetheless poses a challenge: why should we think that a robust public health and healthcare system that extends life and decreases the incidence of diseases, injuries, and other health conditions will alone significantly improve individual well-being and societal welfare? After all, living a long time is not necessarily living well: data suggest that living longer can mean living in worse health (11), and while the absence of disease and injury may be necessary, it is not sufficient for human flourishing or societal welfare. There is something else that health contributes. Intuitively, while living longer without diseases and injuries is obviously relevant to well-being, a key driver of both individual well-being and societal welfare is being able to do and become what we wish—achieving our aspirations, goals, and values and in general acting in ways that make our lives worth living. If we are to take seriously the claim that there is a bridge between health and individual well-being and societal being, we need to fundamentally rethink why health is important to us or, more precisely, what actually matters to us about our health.
The World Health Organization (WHO) has initiated just such a rethinking. WHO collects international comparable health information, understood biomedically and standardized in terms of the International Statistical Classification of Diseases and Related Health Problems (ICD) (12). This information is used to monitor the health indicators of mortality and morbidity. In recent decades, WHO has argued that another body of health information that is equally important both for clinical and public health must be systematically collected and used across all components of the health system. Conceptually, this is information about how a person’s health state affects their daily life, i.e., information that describes the actual lived experience of health. In 2001, WHO released its International Classification of Functioning, Disability and Health (ICF) to operationalize this concept by capturing these essential data in an internationally comparable way (13).
The concept of human functioning—WHO’s technical term—is at the core of the ICF. Functioning includes the functions and structures of the body that constitute the intrinsic health capacity of a person as well as the actual performance of simple and complex activities in interaction with the person’s physical, human-built environment and social environment. In other words, functioning comprises the domains of both biological health and lived health, where lived health is fully contextualized as an outcome of interactions between a person’s intrinsic health capacity and features of their environment (Figure 1). Across the lifespan, all of us experience pain, anxiety, fatigue and weakness, tight joints, skin sores, and other sensory, mobility, and cognitive impairments. These experiences are what matters to us and why we seek out healthcare in the first place. When we find that we cannot climb stairs painlessly, walk as far as we used to, clean or dress ourselves, read a book, make and keep friends, do all the homework we need to do, or perform our jobs, these concrete, real-life difficulties are the lived experience of health. Complementing the traditional biomedical understanding of health, this essential component of lived health creates a more meaningful operationalization of what health means to us.
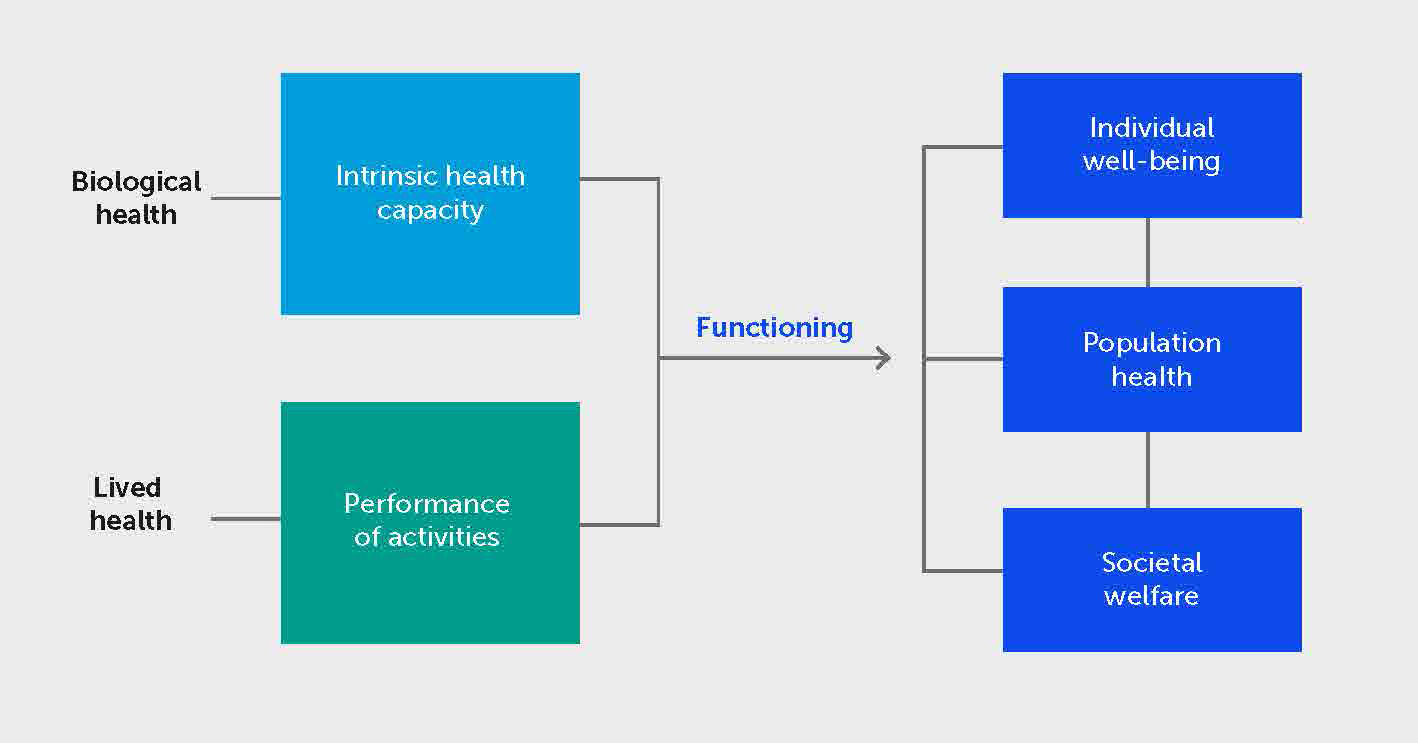
Figure 1 Human functioning is the bridge that links health to individual well-being and societal welfare. Functioning incorporates biological health (the physiological and psychological functions and anatomical structures of the body that constitute the intrinsic health capacity of a person to perform human activities) and lived health (the individual’s actual performance of activities in interaction with their actual physical, built, and social environments). Functioning—both capacity and performance—is the bridge between health and individual well-being: objective human flourishing or subjective happiness and cognitive satisfaction. Functioning also drives overall population health and societal welfare. This link to individual well-being and societal welfare constitutes the value of health for individuals and society at large, operationalizing the underlying principle of SDG3 that health is a fundamental public good.
WHO’s concept of human functioning, we argue, constitutes a rethinking of health: a new understanding and conceptualization of health with wide-ranging consequences. Although domains of functioning have been used in health outcome measures for decades, this application does not fully capture the power of the concept of functioning. Functioning is not simply an outcome of health; by capturing the lived experience of health it is conceptually intrinsic to health and accounts for the value of health both for individuals and society at large.
From a public health perspective, functioning augments the biomedical view of health measured in terms of the indicators of mortality and morbidity. Functioning constitutes WHO’s third health indicator of health (14). Avoiding premature mortality and controlling morbidity are obviously important to us, as individuals and as society at large, but only to the extent to which they are conducive to enhanced functioning and so better health. Population aging (15), adding more years to our lives, underscores the equal importance of adding more life to our years (16). The increased prevalence of non-communicable diseases and chronic health conditions—which lead to a decline in functioning—is concerning, and from the perspective of society they warrant increased investment in prevention and cure. But the impact of these trends also points to the need to prepare our healthcare systems to focus on optimizing functioning (17). Moreover, operationalizing health as human functioning completes the picture of health envisaged by SDG3 by explaining why health is a driver of individual well-being and, in turn, why population health contributes to societal welfare.
This article explicates more fully WHO’s notion of human functioning, illustrates its potential impact on health and society at large, and argues that societies can profit by implementing functioning systematically as the third indicator of health. Specifically, we first explain functioning as a rethinking of health, one that more clearly exposes the conceptual and empirical link between health and both individual well-being and societal welfare. Secondly, we illustrate the implications of this paradigm shift across all components of health systems and other social systems. Finally, we outline the broader scientific and social opportunities as well as the formidable methodological, implementation, and communication challenges that this new thinking about health entails.
Human functioning as the new thinking about health
James Fries’ seminal 1980 article highlighting “compression of morbidity” might in retrospect be seen as an important starting point for raising awareness of the need to assess the successes of preventive, promotive, and curative health interventions in terms of people’s actual lived experience of health (18). Fries was in effect pointing to the need for a new outcome measure that captures what people actually care about when it comes to their health. Fries was one of the first to signal the importance of assessing health interventions and health states in terms of people’s daily lived experiences. Since then, outcomes research has flourished, relying on a myriad of measures, from the Health Assessment Questionnaire (HAQ) that Fries himself was involved in to a variety of “functional status” measures: the Sickness Impact Profile (SIP), Nottingham Health Profile (NHP), Medical Outcomes Study Questionnaire Short Form 36 (SF-36), WHO’s own Disability Assessment Schedule (WHODAS 2.0), and many others. The application of the functioning perspective has also informed health and social policy, most significantly in the development of econometric tools such as the Global Burden of Disease (19).
Recognizing the salience of the lived experience of health in people’s lives was the starting point of a rethinking of health incorporated into WHO’s development of the ICF. The foundational premise was that human functioning was not simply a consequence of health conditions such as diseases and injuries, but was actually constitutive of the lived experience of health states. More significantly, it was recognized that, as experienced, functioning is the result of complex interactions between intrinsic bodily states and the external world—the environment in all its dimensions. More recent work has emphasized that functioning incorporates two fundamental health phenomena, which can be called biological health and lived health (20). Biological health comprises all physiological and psychological functions, anatomical structures, and, by virtue of these functions in various combinations, the resulting “capacity” of the person to perform all human activities, from the very simple to the very complex. Lived health, while grounded in biological health, goes beyond it to include the actual performance of activities in the physical, human-built, attitudinal, and social environments that constitute the person’s complete lived context. These environmental factors may make it harder to perform activities (e.g., poor air quality, inaccessible physical environments, or stigma and social exclusion) or easier (e.g., assistive technology, accessible buildings, supportive attitudes, and social arrangements) (21). The notion of functioning in effect brings health down to earth to the practical, everyday experience in which all of us live with health-related reductions in our capacity to carry out activities and, given the demands and assistance provided by environments in which we live, how we actually perform these activities.
This, then, is the revolution in our understanding of health represented by the notion of human functioning: from the perspective of lived health, the actual performance of activities in one’s actual environment, functioning constitutes the bridge between biological health and our well-being, understood either as an objective good—human flourishing—or subjectively as happiness, both affective and cognitive. There is qualitative evidence in support of this proposition (22), but it is also highly intuitive: people care about their health when it impacts their lives, their ambitions, their plans, and their happiness. Well-being is achieved through functioning, and so health is a driver of well-being. In short, the ICF notion of functioning is the key to understanding the value of health in terms of individual well-being and societal welfare (21), operationalizing the underlying message of SDG3 that health is a fundamental public good.
Implications for health systems and society at large
The novel conceptualization of health in terms of human functioning, operationalized by the ICF classifications, could profoundly change practice, education, research, and policy across health systems and wider social systems. It is difficult to precisely map all these implications since health systems are complex adaptive systems (23). And each of these areas face implementation challenges that are unique to them, and often formidable: there is not enough research, the science is simply not there, relevant technologies are unavailable, and there can be economic and political obstacles that get in the way. That said, ongoing work provides insight into what we can expect.
Integrating human functioning across health system building blocks
The implications of functioning across WHO’s six building blocks of health systems are shown in Figure 2 (24), and an overview of use cases of functioning information across these six functions of the health system is displayed in Table 1. Rather than discuss the role of functioning in each function, we take a step back and focus on WHO’s own interest in formalizing the classification of functioning.
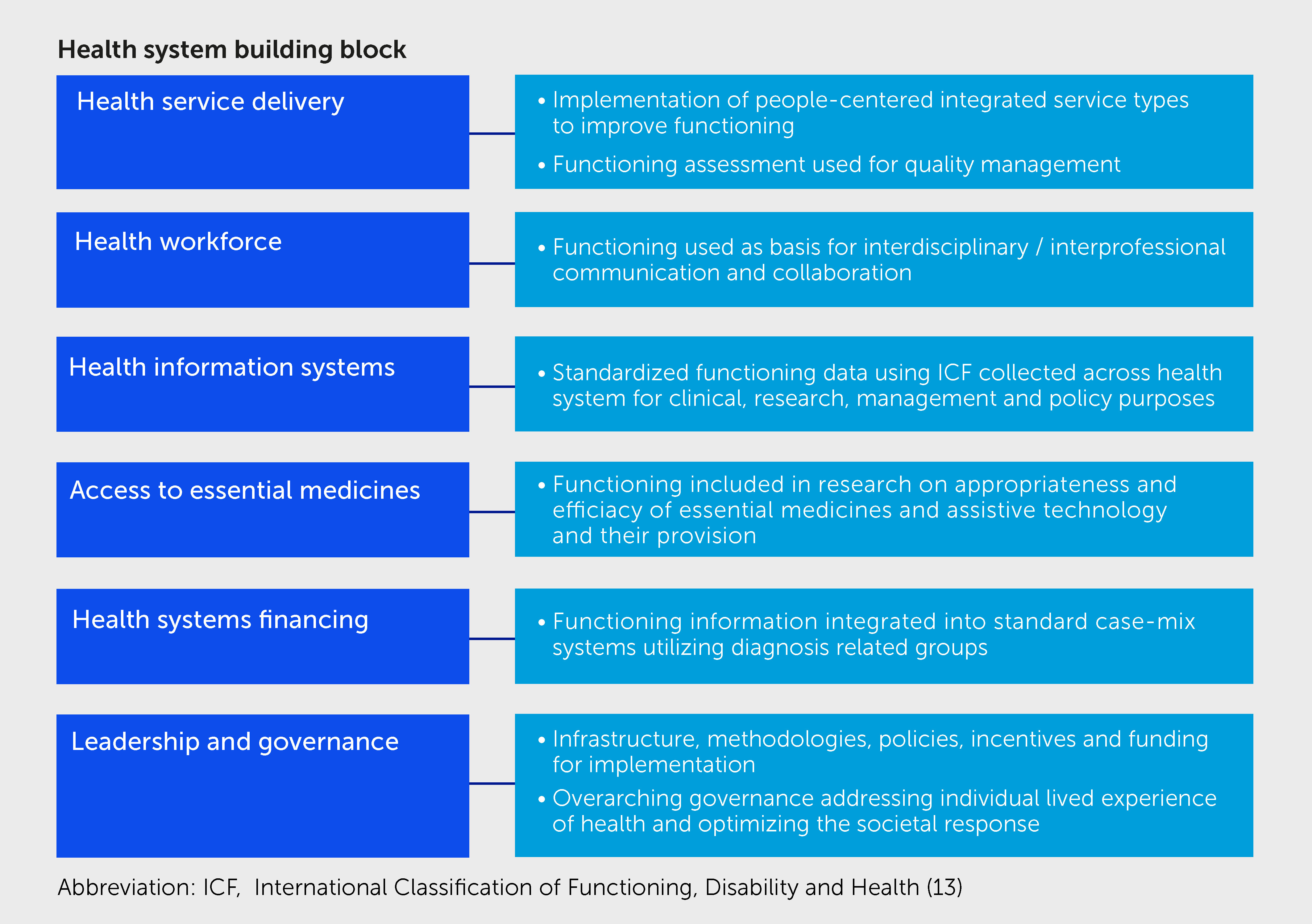
Figure 2 Highlights for implementing human functioning within health systems. The implementation of functioning has implications across all six of the World Health Organization building blocks of health systems.
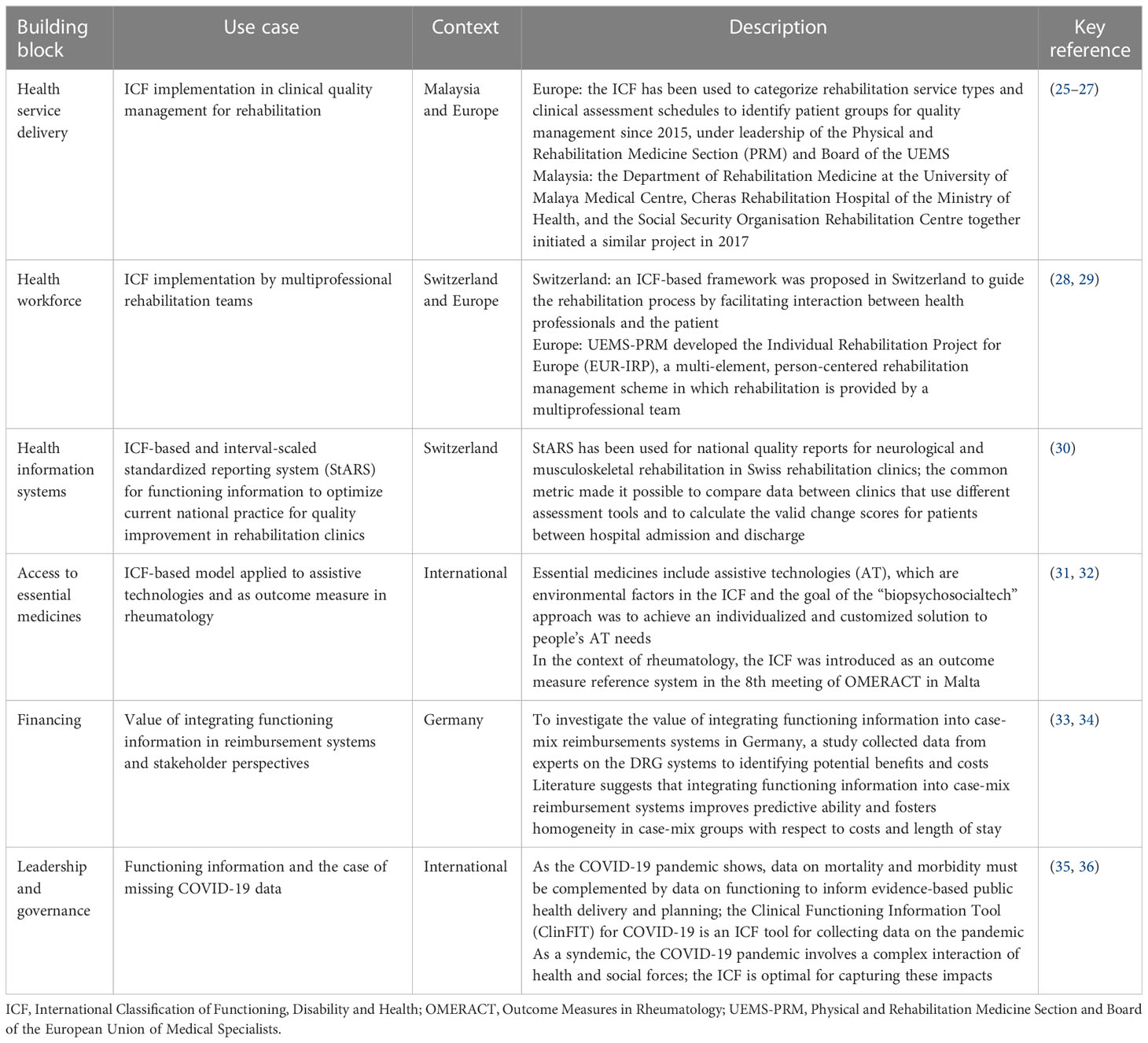
Table 1 Human functioning information in the World Health Organization’s six building blocks of the health system.
From WHO’s perspective, ICF is most relevant to the health information component of health systems, complementing its two other data classifications, ICD and the International Classification of Health Interventions (ICHI) (37), which together allow for the routine collection of data concerning all three indicators of health status—mortality, morbidity, and functioning. To be useful at all levels of the health system—i.e., to health professionals, managers, policymakers, and global health agencies—health information must not only be reliable but comparable and thus standardized and interoperable.
Considerable advances have already been made to standardize human functioning data for optimal use across the health system, using ICF as a reference system for routine reporting of functioning information for clinical, research, management, and policy purposes. Considerable effort has gone into developing and validating ICF-derived ICF Core Sets for perspicuous reporting of functioning for many health conditions and application areas (38) as well as minimal generic sets for basic health data reporting requirements (39–41). The ICF is widely used in the development and validation of both specific and general measurement instruments that can be tailored for clinical use (42, 43), as well as population-level data collection questionnaires and clinical intervention monitoring and quality management. Linking rules have been developed that map data on functioning collected with any standard patient data collection tool—HAQ, SF-36, and Functional Independence Measure (FIM)—onto ICF categories (44–46). These and other developments give us confidence that applications of functioning information in the context of health will not be confronted with unsurmountable methodological obstacles in the future (30, 47).
But the recognition of the importance of the concept of human functioning has implications beyond health information encompassing every other component of the health system (Figure 2). Leadership and governance provide oversight, regulation, and design of health systems, including setting priorities, scaling up interventions, and implementing sustainable and accountable policies. For example, WHO has argued, health systems governance has the responsibility to create the infrastructure, methodologies, and financial support to ensure the systematic collection and use of functioning information in order to move beyond a purely biomedical understanding of health to one that more fully reflects societal requirements (33, 48). Among other things, the COVID-19 pandemic showed the importance of governance to fully address the individual lived experience of this pandemic (35). Functioning also directly impacts service delivery, both in terms of analysis of service types (25, 49, 50) and as a basis for quality management (26, 51, 52). In the case of the health workforce, one of the first applications of the ICF was to provide a “language” in which interdisciplinary teams of health professionals could communicate (28, 53). It is a common theme that interprofessional collaboration, demanded by increasingly complex treatment plans that cross health disciplines, is often stymied by communication obstacles that a functioning-based common language can remove (54). This is particularly relevant to WHO’s consistent call for “people-centered healthcare” (55), which encourages health professionals and healthcare systems to ensure that services are designed and delivered in ways that are directly relevant to people’s lived experiences. The appropriateness and efficacy of many essential medical products and certainly all assistive technologies depends on the degree to which they contribute not merely to survival or patient satisfaction, but also to improvement in functioning, as is increasingly being recognized (56). Finally, for health financing, adding functioning information into standard case-mix systems utilizing diagnosis-related groups improves the capacity of these financing structures to capture the differences in patient needs for services in the acute care setting and influence financial priorities (34).
Human functioning and the health strategy of rehabilitation
Functioning is relevant across all five of the health strategies (14). Health promotion and disease prevention need information on biological health to create and provide public health interventions. The curative strategy depends on information about biological health for treatment planning and information about lived health for outcomes to assess treatment efficacy. Palliation relies on appraisals of levels of functioning to make sense of quality of life near and at the end of life. But it is the health strategy of rehabilitation that depends most strongly on functioning information; indeed, functioning is at the core of the raison d’être of rehabilitation.
The ICF has fundamentally transformed our understanding of the aim and rationale of rehabilitation. The ICF insight that at the core of health is an experience shaped both by states of the body and mind and by features of the person’s environment and personal attributes is directly aligned with the core aim of rehabilitation. Accordingly, rehabilitation professionals were quick to recognize the significance of the notion of functioning as a core element of rehabilitation science and practice. Although rehabilitation traditionally relied on cognate terms such as “functional loss,” “functional limitation,” and “functional incapacity,” it was only after ICF was introduced that it was possible to succinctly define rehabilitation as the health strategy that aims to optimize patients’ functioning in the context of their personal capabilities and in interaction with the physical, human-built, attitudinal, and social environment (17, 20, 50, 57–61).
For rehabilitation practice and science, the concrete implementation of the ICF has primarily meant integrating functioning information into existing health information systems as an important way to advance WHO’s Rehabilitation 2030 Initiative aimed at strengthening rehabilitation in national health systems (62). Technical developments and guidelines (20, 63) help to identify, for particular rehabilitation interventions or services, what ICF domains to use, how to link existing data collected from standard questionnaires, measures, and instruments to ICF domains, and how to quantitatively align scoring systems from different instruments into a single common metric (30, 47) to provide standardized and internationally comparable functioning information. Although much additional technical and implementation research is required, and many practical challenges have yet to be overcome, or even identified, enough has been accomplished in the last decade to begin the development of guidelines for applying the ICF as a standard reference language for reporting rehabilitation interventions in the clinic and in research studies.
Societal gains from human functioning
Rethinking health in terms of human functioning can underpin economic arguments supporting and defining adequate levels of social investment in health and healthcare. All countries are concerned about health systems performance and the economic efficiency of healthcare service delivery, and WHO’s flagship initiative of Universal Health Coverage (64) addresses the necessity for equitable distribution and availability of healthcare resources. It is well recognized that there are indirect socioeconomic benefits of healthcare, such as avoiding productivity losses associated with ill health and the associated loss of functioning. These benefits, the added societal value of healthcare, have been argued to be a component of well-being that can lead to higher gross domestic product (GDP) per capita in the long run as a result of increased labor force participation and productivity (65). Measuring the contribution of health to well-being has been challenging since the relationship between the two has been under-conceptualized (66). Yet the notion of human functioning can support the economic case for the social investment in health because it bridges health and well-being and accounts for the intrinsic and instrumental value of healthcare (8). Recently, functioning has provided the value-base for economic investment in specific service areas, such as rehabilitation (67).
The repeated calls for “value-based” healthcare, championed by Harvard Business School professor Michael Porter, urge a transformation of the healthcare system away from competition over ways to shift or limit costs and restrict services to maximize profit to a competition of increasing value for patients (68). The goal of healthcare, Porter argues, is what matters for patients and what should unite the interests of all actors in the system, namely good health outcomes (69, 70). A strategy of healthcare reform, in short, needs to identify and rigorously measure not only survival and recovery but sustainability and optimization of functioning.
The notion of functioning may also help to bridge another gap in our understanding of the impact of health on societal welfare overall. We have known for decades that individual and population health outcomes are shaped by a complex interaction between our genes, age and sex, features of our physical, social, and economic environment, and our own behaviors. Healthcare itself accounts for only 10–20% of the modifiable (i.e., non-genetic) contribution to positive health outcomes (71), while the remaining 80–90% consists of health behaviors, socio-economic conditions, and physical environmental factors (72). This suggests that while health system improvements will undoubtedly improve population health, a far greater benefit might be achieved by systematic societal actions in other areas of social policy (education, employment, transportation, social welfare, and the environment).
The political, administrative, and policy bifurcation between “health” and “social” hampers policy action to improve population health. Recently, the United Kingdom’s Health Foundation has suggested that local National Health Services (NHS) should be empowered as “anchor institutions” to broker non-healthcare inputs into local communities from social sectors—transportation, environment, and social services (73). Nevertheless, this approach does not dismantle the entrenched health vs social structural dichotomy; rather, it trades on the fact that the NHS can oversee employment-related health determinants as an employer, as a source of procurement strategies, and as a land and capital asset holder and environmental advocate. A true resolution would find a path to integrate health and health-related social sectors so that the collaboration between them is fluid and facilitates policy reforms that can only be achieved by means of cross-sectorial cooperation. Rethinking health in terms of human functioning has the potential to, finally, bridge the traditionally separate “health” and “social” cultures in order to improve our understanding of the determinants of health to society’s considerable benefit.
Opportunities for health sciences, education and training
We can envisage many opportunities from rethinking health in terms of human functioning and focus here on two broad areas: health sciences and education and training.
Health sciences
Fundamentally, the concept of human functioning could be the basis to reconceptualize multidisciplinary health sciences as an integrated and coherent scientific field of study. This reconceptualization opens the door to a broader understanding of epidemiology by moving beyond its traditional focus on mortality and morbidity and incorporating functioning. An emerging “functioning epidemiology” could pave the way towards the recognition of the need for human functioning sciences as a distinct component of health sciences. At this point, although we can only glimpse these potential developments, they clearly signal both the opportunity and the need to expand academic capacity accordingly.
It is not an understatement to say that health research has expanded astoundingly over the last century, thanks to the contributions of numerous scientific disciplines, from the biological and natural sciences to social sciences, humanities, and engineering (74). The field of health sciences faces a challenge in encompassing and integrating diverse scientific disciplines to comprehensively understand and respond to individual and population-level health needs within a single field of study. The concept of human functioning—particularly the distinction between biological and lived health—can help here by identifying the relevant sciences that comprise health research and how they contribute to the societal response to health needs. A scientific description of biological health depends on biological and other natural science tools to account for a person’s intrinsic ability to perform activities. The description of lived health, on the other hand, involves sciences that explain the interaction between the biological and the environmental. Finally, explaining society’s response to the individual’s health needs depends on scientific understanding of institutions and social processes involved in society’s health and health-related systems that respond both to underlying biological needs and environmental determinants of health and lived health.
The comprehensive, multi-dimensional model of human functioning therefore offers a foundational understanding of health sciences that takes account of biological, social, and other environmental determinants of health and the societal response to health needs.
Integrating lived experience into epidemiology
Currently, the scope of epidemiology mirrors the conventional understanding of health as primarily explicable in terms of normal biological processes disrupted by disease, injury, and other sources of impairment or infirmity, manifested at the individual and population levels. As such, it is the study and analysis of distributional patterns, causes, and effects of disruptive health conditions on clinical or general populations. Mortality and morbidity are the conventional health indicators capturing (albeit to a limited degree) the effects of health conditions through premature death and impairments or morbidities. Even the relatively new sub-disciplines of social epidemiology and life-course epidemiology, which more fully appreciate the significance of the wider social context and human health trajectories, restrict their investigations to the impact of context and time on health conditions as primary outcomes. This traditional epidemiology is a robust science grounded in powerful statistical and other highly credible methodologies. However, it is of limited value in comprehending people’s lived experience of health, which demands consideration of health states in light of personal resources and in interaction with a contextual environment, broadly construed. There is, therefore, an opportunity to augment traditional epidemiology with a “functioning epidemiology” to fully account for the lived experience of health (75). The first step to doing this is the recognition that functioning is the third health indicator after mortality and morbidity (14, 36).
Human functioning sciences: an emerging distinct scientific field
Human functioning, as we have argued, can provide a multidimensional foundation for the field of health sciences. Functioning also paves the way for a new interdisciplinary science field, human functioning sciences, that holds the promise of integrating research inputs and methods from diverse biomedical and social disciplines to provide a fuller understanding of human health (Figure 3). Although there are undoubtedly challenges to address, the aim of the human functioning sciences is clear: to understand the lived experience of health at the personal level. It would explore the links between health and individual well-being, identifying and implementing the societal response to functioning needs so as to secure the bridge between healthcare and public health and societal welfare. It is not inconceivable that human functioning sciences might emerge in much the same way that neuroscience did in the 1950s and 1960s (76) with the recognition of an integrative conception of brain and behavior that relied on the results of anatomy, biochemistry, neurology, physiology, and pharmacology but which went beyond this and was more than the sum of those sciences. Human functioning sciences, in short, not only respond to the call to reject reductivism in health research (and “putting the patient back together” (77)) but also to use functioning as the integrative conception of health as the basis for a truly interdisciplinary health science.
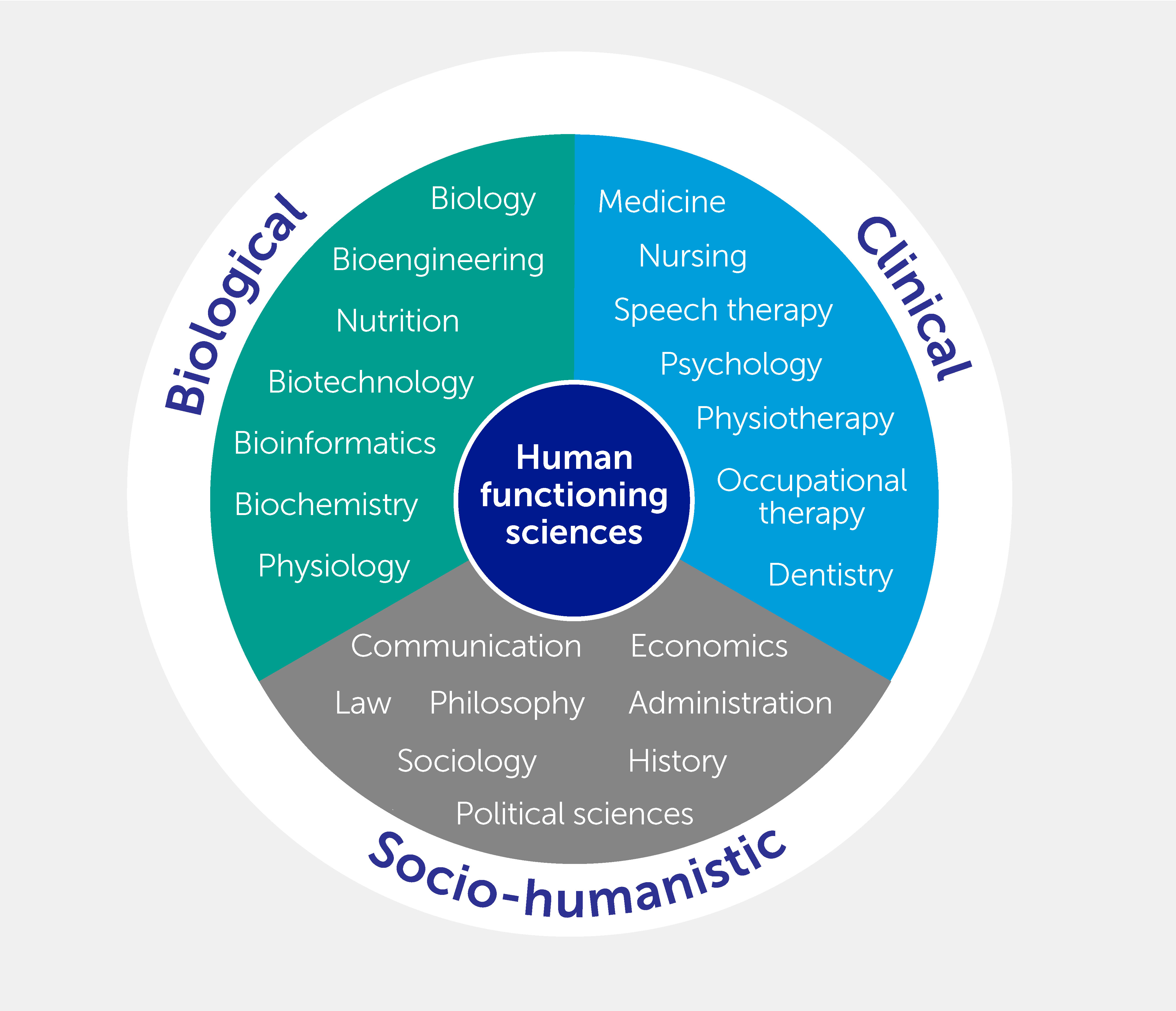
Figure 3 Examples of scientific disciplines rooted in the biological, clinical, and socio-humanistic traditions engaging in the new field of study termed human functioning sciences.
Teaching and training capacity
Concomitant with the emergence of human functioning sciences is the need to develop a new generation of researchers and policy entrepreneurs who will constitute the research and academic workforce for the implementation of the new thinking in healthcare, health science and society at large. This opportunity entails potential transformative academic changes requiring innovative curriculum and program development as well as institutional and organizational changes to degree programs that include collaborative or cross-faculty arrangements (78). Training in human functioning sciences, from bachelor’s degrees through to doctoral degree programs and beyond, should emphasize interdisciplinary research with an implementation orientation. The conceptual model of functioning can clarify how we describe the adaptive processes constitutive of changes—not only changes in individual health capacity but also changes in performance arising from alterations to the person’s environment to better accommodate individual needs. Realistically, these academic arrangements would likely be structured around focal applications of particular societal interaction, such as rehabilitation (79) and healthy aging (80).
Communication challenges in rethinking health
The recognition and implementation of human functioning as a new way of thinking about health entail communication challenges that need to be addressed. This challenge is at the heart of moving from theory to practice, from a shift in conception to new institutions, new actions, and a new cultural understanding of health.
First, for a new paradigm to become effective practice, it is fundamental to agree on the appropriateness, value, and benefits of the terms, concepts, and operational guidance that it proposes. Knowledge translation from evidence to practice must spread at the macro-, meso-, and micro-levels of health systems and along the continuum of care. This requires an awareness of the role of functioning from truly interdisciplinary work and, at the same time, a focus on functioning as a promising language to enhance interdisciplinarity in healthcare, in light of what really matters to patients. All this can be achieved by promoting communication around the notion of functioning and increasing awareness among health professionals using successful implementation cases and scientific evidence gathered during the last two decades. System communication has the important but difficult task of preparing for the global implementation of functioning as a bridge between health and well-being, which is an essential conceptual issue with practical implications.
Second, the question of how to inform the public about human functioning (public dissemination) is another challenge. There are benefits to achieving public understanding: knowledge about functioning, health, and well-being can help the public better understand and accept health investments and resource allocation, especially when other social goods are in competition for limited resources. Participatory democracies flourish when, putting the important distinction between “lay” people and “experts” aside, people understand what can influence optimal health policies. Targeting the public is a task embedded in institutional communication and requires strategies for public campaigns centered on functioning.
Third, at the level of healthcare provider-patient interaction, there is strong evidence that the use of the functioning framework and the ICF during the interaction facilitates goal-setting and intervention management (81, 82). ICF provides a common language between health professionals and patients for shared decision-making. In light of this, knowledge of functioning constitutes an important topic to enrich patients’ health literacy. Patient education on functioning holds the promise of a “language” to bridge the gap between the point of view of the health professionals and the lived experience of the patients.
Conclusion
The conceptual and evidence base exists to support the implementation of human functioning as the third indicator of health, complementing morbidity and mortality. This requires coordinated action across health systems, including the scaling and extension of use cases. Significant challenges in implementing this new paradigm exist: while the methodological challenges are well on the way to being resolved, true implementation is in its infancy and the communication challenge has yet to be fully comprehended. Addressing these challenges and associated inertia is vital to orientate health systems toward what matters most to people about health based on their lived experience of health. Moreover, by bridging health and well-being, human functioning offers a basis for the societal economic investment in health that is essential both for individual and population-level well-being and for progress toward achieving all of the SDGs to which all countries are committed.
Data availability statement
The original contributions presented in the study are included in the article/supplementary material. Further inquiries can be directed to the corresponding author.
Author contributions
JB and GS conceived the underlying concept and designed the manuscript together with SR and CB. JB, with assistance from CB, wrote the section on the application of functioning information in the six building blocks of WHO’s health system. SR wrote the section on communication. JB wrote the overall manuscript with support from CB, GS, and SR. All authors provided critical feedback. CB coordinated the project. All authors contributed to the article and approved the submitted version.
Acknowledgments
The authors would like to thank Lee Baker and Susanne Stucki for their support during the preparation of the manuscript.
Conflict of interest
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
The reviewer WF declared a past collaboration with the authors JB, GS to the handling editor.
Publisher’s note
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
References
1. United Nations. Transforming our world: the 2030 agenda for sustainable development. Available at: https://sdgs.un.org/2030agenda (Accessed September 5, 2022).
2. World Health Organization. Rapid assessment of service delivery for NCDs during the COVID-19 pandemic. Geneva: World Health Organization (2020). Available at: https://www.who.int/publications/m/item/rapid-assessment-of-service-delivery-for-ncds-during-the-covid-19-pandemic (Accessed September 5, 2022).
3. GBD 2017 SDG Collaborators. Measuring progress from 1990 to 2017 and projecting attainment to 2030 of the health-related sustainable development goals for 195 countries and territories: a systematic analysis for the global burden of disease study 2017. Lancet (2018) 392:2091–138. doi: 10.1016/s0140-6736(18)32281-5
4. Doctor H, Rashidian A, Hajjeh R, Al-Mandhari A. Improving health and mortality data in Eastern Mediterranean region countries: implementation of the international classification of diseases, 11th revision (ICD-11). East Mediterr Health J (2021) 27(2):111–12. doi: 10.26719/2021.27.2.111
5. Grépin KA, Irwin BR, Sas Trakinsky B. On the measurement of financial protection: an assessment of the usefulness of the catastrophic health expenditure indicator to monitor progress towards universal health coverage. Health Syst Reform (2020) 6:e1744988. doi: 10.1080/23288604.2020.1744988
6. Diener E. Subjective well-being: The science of happiness and a proposal for a national index. Am Psychol (2000) 55:34–43. doi: 10.1037/0003-066X.55.1.34
7. Nussbaum MC. Creating capabilities: the human development approach. Cambridge, MA: Harvard University Press (2013). doi: 10.2307/j.ctt2jbt31
8. Daniels N. Just health: meeting health needs fairly. Cambridge: Cambridge University Press (2008).
9. Tov W, Diener E. The well-being of nations: linking together trust, cooperation, and democracy. In: Sullivan BA, Snyder M, Sullivan J, editors. Cooperation: the political psychology of effective human interaction. Malden, MA: Blackwell Publishing (2008) 323–42.
10. Office of Disease Prevention and Health Promotion. Health-related quality of life and well-being. (2020). Available at: https://wayback.archive-it.org/5774/20220413203043/https://www.healthypeople.gov/2020/about/foundation-health-measures/Health-Related-Quality-of-Life-and-Well-Being (Accessed September 5, 2022).
11. Chatterji S, Byles J, Cutler D, Seeman T, Verdes E. Health, functioning, and disability in older adults – present status and future implications. Lancet (2015) 385:563–75. doi: 10.1016/s0140-6736(14)61462-8
12. World Health Organization. International classification of diseases. Geneva: World Health Organization (2019). Available at: https://www.who.int/standards/classifications/classification-of-diseases (Accessed September 5, 2022).
13. World Health Organization. International classification of functioning, disability and health. Geneva: World Health Organization (2001).
14. Stucki G, Bickenbach J. Functioning: the third health indicator in the health system and the key indicator for rehabilitation. Eur J Phys Rehabil Med (2017) 53:134–8. doi: 10.23736/s1973-9087.17.04565-8
15. United Nations, Department of Economic and Social Affairs, Population Division. World population ageing 2015 – highlights (St/Esa/Ser.A/368) (2015). New York: United Nations. Available at: https://www.un.org/en/development/desa/population/publications/pdf/ageing/WPA2015_Highlights.pdf (Accessed September 5, 2022).
16. World Health Organization. World report on ageing and health. Geneva: World Health Organization (2015). Available at: https://apps.who.int/iris/handle/10665/186463 (Accessed March 21 2023).
17. Stucki G, Bickenbach J, Gutenbrunner C, Melvin J. Rehabilitation:the health strategy of the 21st century. J Rehabil Med (2018) 50:309–16. doi: 10.2340/16501977-2200
18. Fries JF. Aging, natural death, and the compression of morbidity. N Engl J Med (1980) 303:130–5. doi: 10.1056/nejm198007173030304
19. Eyal N, Hurst SA, Murray CJ eds. Measuring the global burden of disease: philosophical dimensions. New York: Oxford University Press (2020).
20. Stucki G, Bickenbach J, Melvin J. Strengthening rehabilitation in health systems worldwide by integrating information on functioning in national health information systems. Am J Phys Med Rehabil (2017) 96:677–81. doi: 10.1097/phm.0000000000000688
21. Stucki G, Bickenbach J. Health, functioning, and well-being: individual and societal. Arch Phys Med Rehabil (2019) 100:1788–92. doi: 10.1016/j.apmr.2019.03.004
22. Hartley S, McArthur M, Coenen M, Cabello V, Covelli V, Roszczynska-Michta J, et al. Narratives reflecting the lived experiences of people with brain disorders: common psychosocial difficulties and determinants. PloS One (2014) 9(5):e96890. doi: 10.1371/journal.pone.0096890
23. Plsek PE, Greenhalgh T. Complexity science: the challenge of complexity in healthcare. BMJ (2001) 323:625–8. doi: 10.1136/bmj.323.7313.625
24. World Health Organization. Everybody’s business – strengthening health systems to improve health outcomes: WHO’s framework for action (2007). Geneva: World Health Organization. Available at: https://apps.who.int/iris/handle/10665/43918 (Accessed 21 March 2023).
25. Selb M, Zampolini M, Delargy M, Kiekens C, Stucki G. Specifying clinical assessment schedules for the European framework of rehabilitation service types: the perspective of the physical and rehabilitation medicine section and board of the European union of medical specialists. Eur J Phys Rehabil Med (2019) 55:834–44. doi: 10.23736/s1973-9087.19.05961-6
26. Engkasan JP, Stucki G, Ali S, Yusof YM, Hussain H, Latif LA. Implementation of clinical quality management for rehabilitation in Malaysia. J Rehabil Med (2018) 50:346–57. doi: 10.2340/16501977-2283
27. Stucki G, Zampolini M, Selb M, Ceravolo MG, Delargy M, Varela Donoso E, et al. European Framework of rehabilitation services types: the perspective of the physical and rehabilitation medicine section and board of the European union of medical specialists. Eur J Phys Rehabil Med (2019) 55:411–17. doi: 10.23736/s1973-9087.19.05728-9
28. Rentsch HP, Bucher P, Dommen Nyffeler I, Wolf C, Hefti H, Fluri E, et al. The implementation of the ‘International classification of functioning, disability and health’ (ICF) in daily practice of neurorehabilitation: an interdisciplinary project at the kantonsspital of Lucerne, Switzerland. Disabil Rehabil (2003) 25:411–21. doi: 10.1080/0963828031000069717
29. Zampolini M, Selb M, Boldrini P, Branco CA, Golyk V, Hu X, et al. The individual rehabilitation project as the core of person-centred rehabilitation – the physical and rehabilitation medicine section and board of the European union of medical specialists framework for rehabilitation in Europe. Eur J Phys Rehabil Med (2022) 58(4):503–10. doi: 10.23736/s1973-9087.22.07402-0
30. Maritz R, Tennant A, Fellinghauer C, Stucki G, Prodinger B. Creating a common metric based on existing activities of daily living tools to enable standardized reporting of functioning outcomes achieved during rehabilitation. J Rehabil Med (2020) 52:jrm00085. doi: 10.2340/16501977-2711
31. Scherer MJ. It is time for the biopsychosocialtech model. Disabil Rehabil Assist Technol (2020) 15:363–4. doi: 10.1080/17483107.2020.1752319
32. Boonen A, Stucki G, Maksymowych W, Rat AC, Escorpizo R, Boers M. The omeract-ICF reference group: integrating the ICF into the omeract process: opportunities and challenges. J Rheumatol (2009) 36:2057–60. doi: 10.3899/jrheum.090357
33. Hopfe M, Prodinger B, Bickenbach JE, Stucki G. Optimizing health system response to patient’s needs: an argument for the importance of functioning information. Disabil Rehabil (2018) 40:2325–30. doi: 10.1080/09638288.2017.1334234
34. Hopfe M, Stucki G, Marshall R, Twomey CD, Üstün TB, Prodinger B. Capturing patients’ needs in casemix: a systematic literature review on the value of adding functioning information in reimbursement systems. BMC Health Serv Res (2016) 16:40. doi: 10.1186/s12913-016-1277-x
35. Boes S, Sabariego C, Bickenbach J, Stucki G. How to capture the individual and societal impacts of syndemics: the lived experience of COVID-19. BMJ Glob Health (2021) 6(10):e006735. doi: 10.1136/bmjgh-2021-006735
36. Boggs D, Polack S, Kuper H, Foster A. Shifting the focus to functioning: essential for achieving sustainable development goal 3, inclusive universal health coverage and supporting COVID-19 survivors. Glob Health Action (2021) 14:1903214. doi: 10.1080/16549716.2021.1903214
37. World Health Organization. International classification of health interventions. Geneva: World Health Organization (2018). Available at: https://www.who.int/standards/classifications/international-classification-of-health-interventions (Accessed 21 March 2023).
38. Bickenbach J, Stucki G, Cieza A, Selb M. ICF core sets: manual for clinical practice. Göttingen: Hogrefe Publishing GmbH (2021).
39. Cieza A, Oberhauser C, Bickenbach J, Chatterji S, Stucki G. Towards a minimal generic set of domains of functioning and health. BMC Public Health (2014) 14:218. doi: 10.1186/1471-2458-14-218
40. Prodinger B, Cieza A, Oberhauser C, Bickenbach J, Üstün B, Chatterji S, et al. Toward the international classification of functioning, disability and health (ICF) rehabilitation set: a minimal generic set of domains for rehabilitation as a health strategy. Arch Phys Med Rehabil (2016) 97:875–84. doi: 10.1016/j.apmr.2015.12.030
41. Ehrmann C, Prodinger B, Stucki G, Cai W, Zhang X, Liu S, et al. ICF generic set as new standard for the system wide assessment of functioning in China: a multicentre prospective study on metric properties and responsiveness applying item response theory. BMJ Open (2018) 8:e021696. doi: 10.1136/bmjopen-2018-021696
42. Frontera W, Gimigliano F, Melvin J, Li J, Li L, Lains J, et al. ClinFIT: ISPRM’s universal functioning information tool based on the WHO’s ICF. J Int Soc Phys Rehabil Med (2019) 2:19–21. doi: 10.4103/jisprm.jisprm_36_19
43. Selb M, Stucki G, Li J, Mukaino M, Li L, Gimigliano F, et al. Developing ClinFIT COVID-19: an initiative to scale up rehabilitation for COVID-19 patients and survivors across the care continuum. J Int Soc Phys Rehabil Med (2021) 4:174–83. doi: 10.4103/jisprm-000128
44. Prodinger B, O’Connor RJ, Stucki G, Tennant A. Establishing score equivalence of the functional independence measure motor scale and the barthel index, utilising the international classification of functioning, disability and health and rasch measurement theory. J Rehabil Med (2017) 49:416–22. doi: 10.2340/16501977-2225
45. Prodinger B, Küçükdeveci AA, Kutlay S, Elhan AH, Kreiner S, Tennant A. Cross-diagnostic scale-banking using rasch analysis: developing a common reference metric for generic and health condition-specific scales in people with rheumatoid arthritis and stroke. J Rehabil Med (2020) 52:jrm00107. doi: 10.2340/16501977-2736
46. Maritz R, Tennant A, Fellinghauer C, Stucki G, Prodinger B. The functional independence measure 18-item version can be reported as a unidimensional interval-scaled metric: internal construct validity revisited. J Rehabil Med (2019) 51:193–200. doi: 10.2340/16501977-2525
47. Maritz R, Ehrmann C, Prodinger B, Tennant A, Stucki G. The influence and added value of a standardized assessment and reporting system for functioning outcomes upon national rehabilitation quality reports. Int J Qual Health Care (2020) 32:379–87. doi: 10.1093/intqhc/mzaa058
48. World Health Organization. WHO global disability action plan 2014-2021. better health for all people with disability. Geneva: World Health Organization (2015). Available at: https://www.who.int/publications/i/item/who-global-disability-action-plan-2014-2021 (Accessed 21 March 2023).
49. Meyer T, Gutenbrunner C, Kiekens C, Skempes D, Melvin JL, Schedler K, et al. ISPRM discussion paper: proposing a conceptual description of health-related rehabilitation services. J Rehabil Med (2014) 46:1–6. doi: 10.2340/16501977-1251
50. Gutenbrunner C, Bickenbach J, Kiekens C, Meyer T, Skempes D, Nugraha B, et al. ISPRM discussion paper: proposing dimensions for an international classification system for service organization in health-related rehabilitation. J Rehabil Med (2015) 47:809–15. doi: 10.2340/16501977-2002
51. Scheel-Sailer A, Selb M, Gmünder HP, Baumberger M, Curt A, Hund-Georgiadis M, et al. Towards the implementation of clinical quality management at the national level: description of current types of rehabilitation services for spinal cord injury/disorder in Switzerland using an interdisciplinary consensus process. Eur J Phys Rehabil Med (2022) 58:190–8. doi: 10.23736/s1973-9087.21.06923-9
52. Prodinger B, Tennant A, Stucki G, Cieza A, Üstün TB. Harmonizing routinely collected health information for strengthening quality management in health systems: requirements and practice. J Health Serv Res Policy (2016) 21:223–8. doi: 10.1177/1355819616636411
53. Selb M, Glassel A, Escorpizo R. ICF-based tools in rehabilitation toward return to work: facilitating inter-professional communication and comprehensive documentation. In: Escorpizo R, Brage S, Homa D, Stucki G, editors. Handbook of vocational rehabilitation and disability evaluation: application and implementation of the ICF. New York: Springer (2015) 471–94.
54. Müller C, Plewnia A, Becker S, Rundel M, Zimmermann L, Körner M. Expectations and requests regarding team training interventions to promote interdisciplinary collaboration in medical rehabilitation–a qualitative study. BMC Med Educ (2015) 15:135. doi: 10.1186/s12909-015-0413-3
55. World Health Organization. Regional office for the Western pacific, in: People-centred healthcare: a policy framework. Geneva: World Health Organization (2007). Available at: https://www.who.int/publications/i/item/9789290613176 (Accessed 21 March 2023).
56. European Network for Health Technology Assessment. Endpoints used for relative effectiveness assessment: clinical endpoints. European network for health technology assessment. (2015). Available at: https://www.eunethta.eu/endpoints-used-for-relative-effectiveness-assessment-clinical-endpoints-amended-ja1-guideline-final-nov-2015/ (Accessed September 5, 2022).
57. Stucki G, Melvin J. The international classification of functioning, disability and health: a unifying model for the conceptual description of physical and rehabilitation medicine. J Rehabil Med (2007) 39:286–92. doi: 10.2340/16501977-0044
58. Stucki G, Cieza A, Melvin J. The international classification of functioning, disability and health (ICF): a unifying model for the conceptual description of the rehabilitation strategy. J Rehabil Med (2007) 39:279–85. doi: 10.2340/16501977-0041
59. Gutenbrunner C, Meyer T, Melvin J, Stucki G. Towards a conceptual description of physical and rehabilitation medicine. J Rehabil Med (2011) 43:760–4. doi: 10.2340/16501977-0866
60. Meyer T, Gutenbrunner C, Bickenbach J, Cieza A, Melvin J, Stucki G. Towards a conceptual description of rehabilitation as a health strategy. J Rehabil Med (2011) 43:765–9. doi: 10.2340/16501977-0865
61. Stucki G, Bickenbach J, Selb M, Melvin J. The international classification of functioning, disability and health. In: Frontera WR, DeLisa JA, Basford JR, Bockenek W, Chae J, Robinson LR, et al, editors. DeLisa’s physical medicine and rehabilitation: principles and practice. Philadelphia: Wolters Kluwer (2020) 208–26.
62. World Health Organization. Rehabilitation 2030 initiative. Geneva: World Health Organization (2022). Available at: https://www.who.int/initiatives/rehabilitation-2030 (Accessed September 5, 2022).
63. Stucki G, Pollock A, Engkasan JP, Selb M. How to use the international classification of functioning, disability and health as a reference system for comparative evaluation and standardized reporting of rehabilitation interventions. Eur J Phys Rehabil Med (2019) 55:384–94. doi: 10.23736/s1973-9087.19.05808-8
64. World Health Organization. Universal health coverage. Geneva: World Health Organization (2022). Available at: https://www.who.int/health-topics/universal-health-coverage#tab=tab_1 (Accessed September 5, 2022).
65. Organisation for Economic Co-operation and Development. The economy of well-being: creating opportunities for people’s well-being and economic growth (SDD/DOC(2019)2). Paris: Organisation for Economic Co-operation and Development (2019). Available at: https://www.oecd.org/officialdocuments/publicdisplaydocumentpdf/?cote=SDD/DOC(2019)2&docLanguage=En#:~:text=The%20%E2%80%9CEconomy%20of%20Well%2Dbeing,2 (Accessed September 5, 2022).
66. Daniel MH. Valuing health: well-being, freedom, and suffering. New York: Oxford University Press (2015).
67. Jordan N, Deutsch A. Why and how to demonstrate the value of rehabilitation services. Arch Phys Med Rehabil (2022) 103(7S):S172–7. doi: 10.1016/j.apmr.2021.06.028
68. Porter ME. A strategy for healthcare reform–toward a value-based system. N Engl J Med (2009) 361:109–12. doi: 10.1056/NEJMp0904131
69. Porter ME. What is value in healthcare? N Engl J Med (2010) 363:2477–81. doi: 10.1056/NEJMp1011024
70. Porter ME, Lee TH. From volume to value in healthcare: the work begins. JAMA (2016) 316:1047–8. doi: 10.1001/jama.2016.11698
71. Alderwick H, Vuik S, Ham C, Patel H, Siegel S. Healthy populations: designing strategies to improve population health. Doha, Qatar: World Innovation Summit for Health (2016). Available at: https://www.kingsfund.org.uk/sites/default/files/field/field_publication_file/WISH%20Healthy%20populations.pdf (Accessed 21 March 2023).
72. Magnan S. Social determinants of health 101 for healthcare: five plus five, in: NAM perspectives. Washington, DC: National Academy of Medicine (2017). Available at: https://nam.edu/wp-content/uploads/2017/10/Social-Determinants-of-Health-101.pdf (Accessed September 5, 2022).
73. Reed S, Göpfert A, Wood S, Allwood D, Warburton W. Building healthier communities: the role of the NHS as an anchor institution. London: The Health Foundation (2019). Available at: https://www.health.org.uk/publications/reports/building-healthier-communities-role-of-nhs-as-anchor-institution (Accessed 21 March 2023).
74. Stucki G, Rubinelli S, Reinhardt JD, Bickenbach JE. Towards a common understanding of the health sciences. Gesundheitswesen (2016) 78:e80–4. doi: 10.1055/s-0042-108442
75. Fellinghauer B, Reinhardt J, Stucki G. Towards an epidemiology of functioning. In: Franchignoni F, editor. Advances in rehabilitation research issues in physical and rehabilitation medicine. Pavia: Maugeri Foundation Books (2010) 53–68.
76. Society for Neuroscience. The creation of neuroscience. the society for neuroscience and the quest for disciplinary unity 1969–1995. Washington, DC: Society for Neuroscience (2022). Available at: https://www.sfn.org/about/history-of-sfn/the-creation-of-neuroscience/~/media/SfN/Images/HistoryofSfN/pdf/HistoryofSfN.ashx (Accessed September 5, 2022).
77. Greene JA, Loscalzo J. Putting the patient back together – social medicine, network medicine, and the limits of reductionism. N Engl J Med (2017) 377:2493–9. doi: 10.1056/NEJMms1706744
78. Stucki G. Developing human functioning and rehabilitation research. part I: academic training programs. J Rehabil Med (2007) 39:323–33. doi: 10.2340/16501977-0037
79. Frontera WR, Stucki G, Engkasan JP, Francisco GE, Gutenbrunner C, Hasnan N, et al. Advancing academic capacity in physical and rehabilitation medicine to strengthen rehabilitation in health systems worldwide: a joint effort by the European academy of rehabilitation medicine, the association of academic physiatrists, and the international society of physical and rehabilitation medicine. Am J Phys Med Rehabil (2022) 101:897–904. doi: 10.1097/PHM.0000000000002067
80. Stucki G, Bickenbach J, Frontera W. Why rehabilitation should be included in international healthy ageing agendas. Am J Phys Med Rehabil (2019) 98:251–2. doi: 10.1097/phm.0000000000001111
81. Constand MK, MacDermid JC. Applications of the international classification of functioning, disability and health in goal-setting practices in healthcare. Disabil Rehabil (2014) 36:1305–14. doi: 10.3109/09638288.2013.845256
Keywords: functioning, health, well-being, health system, sustainable development goals
Citation: Bickenbach J, Rubinelli S, Baffone C and Stucki G. The human functioning revolution: implications for health systems and sciences. Front Sci (2023) 1:1118512. doi: 10.3389/fsci.2023.1118512
Received: 07 December 2022; Accepted: 26 April 2023;
Published: 31 May 2023.
Edited by:
Maria Gabriella Ceravolo, Marche Polytechnic University, ItalyReviewed by:
Walter Frontera, University of Puerto Rico, Puerto RicoHannah Kuper, London School of Hygiene & Tropical Medicine, United Kingdom
Copyright © 2023 Bickenbach, Rubinelli, Baffone and Stucki. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Sara Rubinelli, c2FyYS5ydWJpbmVsbGlAcGFyYXBsZWdpZS5jaA==
†These authors share first authorship
 Jerome Bickenbach
Jerome Bickenbach Sara Rubinelli
Sara Rubinelli Cristiana Baffone
Cristiana Baffone Gerold Stucki
Gerold Stucki