- 1Department of Oral and Maxillofacial Surgery, Stomatological Hospital of Xiamen Medical College, Xiamen, China
- 2Xia-men Key Laboratory of Stomatological Disease Diagnosis and Treatment, Xiamen, Fujian, China
- 3State Key Laboratory of Oral & Maxillofacial Reconstruction and Regeneration, Key Laboratory of Oral Biomedicine Ministry of Education, Hubei Key Laboratory of Stomatology, School & Hospital of Stomatology, Wuhan University, Wuhan, China
- 4Department of Oral and Maxillofacial Head Neck Surgery, School & Hospital of Stomatology, Wuhan University, Wuhan, China
This study retrospectively analyzed 112 patients who underwent mandibular reconstruction with vascularized iliac crest flaps using different fixation strategies in routine clinical practice. Under comparable defect lengths and heights, reconstruction using mini plates was associated with the shortest operative time (p < 0.001), while postoperative drainage duration showed no significant difference among groups (p = 0.958). The number of iliac bone segments varied significantly among fixation methods: reconstruction plates (alone or combined with mini plates) were predominantly applied in multi-segmental reconstructions, whereas mini plates were mainly used for single-segmental repairs. Postoperative quality of life was evaluated using the University of Washington Quality of Life Questionnaire (UW-QoL). Although the fixation methods were selected according to defect complexity and surgical requirements, all approaches achieved satisfactory outcomes, and no significant difference in overall quality-of-life scores was observed among the three groups (p = 0.354). However, a significant difference was observed in the “Swallowing” domain, with patients in the mini plate group reporting better swallowing function (p = 0.009).
1 Introduction
The mandible is a critical bony structure of the maxillofacial region, responsible for functions such as mastication, speech, and facial aesthetics. Segmental defects resulting from tumors, trauma, infections, or congenital malformations not only impair patients’ functional and aesthetic outcomes but may also lead to psychological distress (Pickrell and Hollier, 2017). Vascularized iliac crest flap transplantation, owing to its abundant bone volume, reliable blood supply, and excellent shaping capability, has emerged as one of the most preferred methods for mandibular defect reconstruction (Yang et al., 2023). This technique, utilizing iliac crest flaps pedicled on the deep circumflex iliac vessels, effectively restores mandibular continuity and function while enabling the simultaneous repair of soft tissue defects with skin islands or internal oblique muscles (Yu et al., 2020).
Clinically, internal fixation of transplanted bone predominantly involves the use of reconstruction plates and titanium miniplates (Stanford-Moore and Murr, 2022). Reconstruction plates, characterized by robust fixation strength and broad adaptability, are commonly employed in complex defects, such as those crossing the midline or involving the condyle (Kreutzer et al., 2023). However, their large volume and stress-shielding effects may impact facial aesthetics and lead to bone resorption (Zhang et al., 2019). In contrast, titanium miniplates, with their small size, thin profile, and ease of application, have minimal impact on appearance, exhibit low stress-shielding effects, and are particularly suitable for simple defects and pediatric or adolescent patients to minimize interference with mandibular development (Graillon et al., 2023). Nevertheless, their fixation strength may be insufficient for multi-segmental repairs or stress-concentration areas (Graillon et al., 2022). However, existing studies have not yet systematically evaluated the influence of different fixation methods on vascularized iliac crest flaps and their clinical outcomes.
To address the question “Can titanium miniplates provide superior fixation for iliac crest flaps?” The study systematically compared the fixation stability, applicability, and complication profiles of titanium miniplates and reconstruction plates. This study aims to: (1) Identify defect types and segment numbers where titanium miniplates may outperform reconstruction plates, (2) Assess differences in complication rates between the two fixation methods, and (3) Optimize fixation method selection based on defect characteristics, thereby providing evidence-based guidance for clinicians to improve mandibular reconstruction outcomes.
2 Materials and methods
This study included 112 cases of mandibular defect reconstruction using vascularized iliac crest flaps performed at the Department of Oral and Maxillofacial-Head and Neck Oncology Surgery, School of Stomatology, Wuhan University, between January 2019 and December 2022 (Figure 1). Before surgery, all patients underwent high-resolution spiral CT scans of both the maxillofacial and iliac regions to obtain accurate anatomical data. The imaging data were processed using Mimics 19.0 software (Materialise, Belgium) to generate three-dimensional models of the donor and recipient sites. Surgeons collaborated with biomedical engineers to perform virtual osteotomies and simulate bone resection based on the lesion extent and reconstructive requirements. Customized surgical guides for mandibular resection, iliac bone harvesting, contouring, and graft positioning were then digitally designed. These guides were fabricated using 3D printing to assist in accurate intraoperative execution. In addition, titanium reconstruction plates were pre-bent manually according to the 3D-printed postoperative model, enabling precise transfer of the preoperative virtual plan to the actual surgery and ensuring accurate alignment of the bone segments.
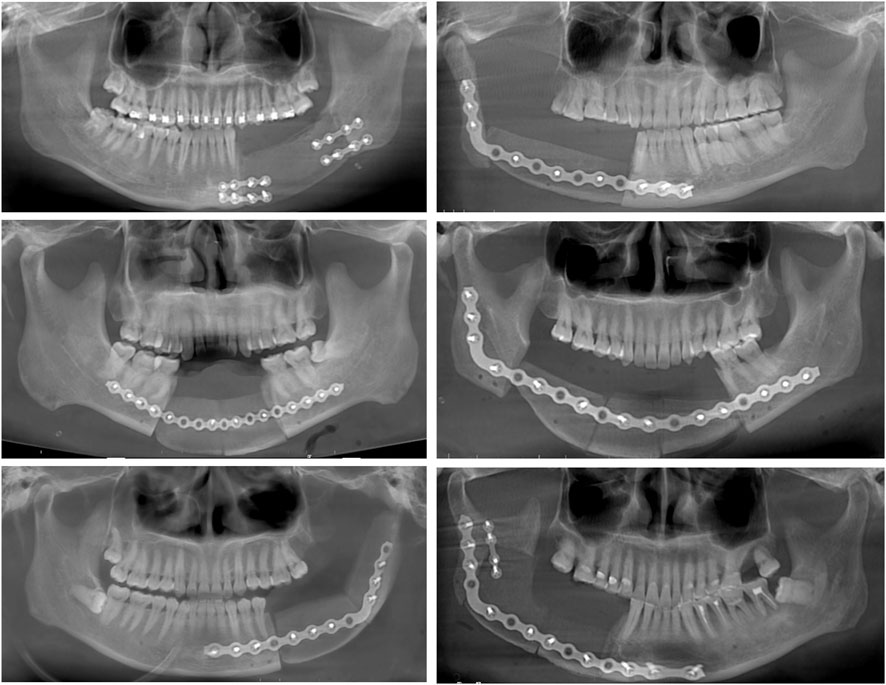
Figure 1. Demonstration of cases with different types of mandibular defects and number of grafted bone segments using two types of internal fixation: reconstruction plate and small titanium plate.
The inclusion criteria of the study were: (1) complete electronic medical records, preoperative and postoperative imaging data, and pathological diagnoses; (2) postoperative follow-up of at least 1 year. Exclusion criteria were: (1) severe preoperative systemic diseases; (2) incomplete follow-up data. The study was approved by the hospital ethics committee (2023 B23) and registered at the Clinical Trial Registry Center on 18 July 2023 (ChiCTR2300073660), with written informed consent obtained from all participants for the use of their data in this research.
The mandibular defect types were classified according to Brown’s classification system, specifically as mandibular lateral defect (Type I), hemimandibulectomy (Type II), anterior mandibulectomy (Type III), and extensive anterior mandibulectomy (Type IV) (Brown et al., 2016). Postoperative quality of life was evaluated using the University of Washington Quality of Life Questionnaire (UW-QoL) (Hassan and Weymuller, 1993; Lin et al., 2025a; Lin et al., 2025b). Complications, including plate or screw exposure, loosening, or fracture, were identified through postoperative computed tomography (CT) follow-up and physical examinations. All statistical analyses were performed using SPSS Statistics software (version 26.0; IBM Corp., Armonk, NY, United States). Based on the results of normality testing, variables with a normal distribution were analyzed using one-way analysis of variance (ANOVA), whereas non-normally distributed variables were evaluated using the Kruskal–Wallis H test. Categorical variables were compared using the chi-square test or Fisher’s exact test. Data are presented as mean ± standard deviation or median (interquartile range), as applicable. A p value <0.05 was considered statistically significant.
3 Results
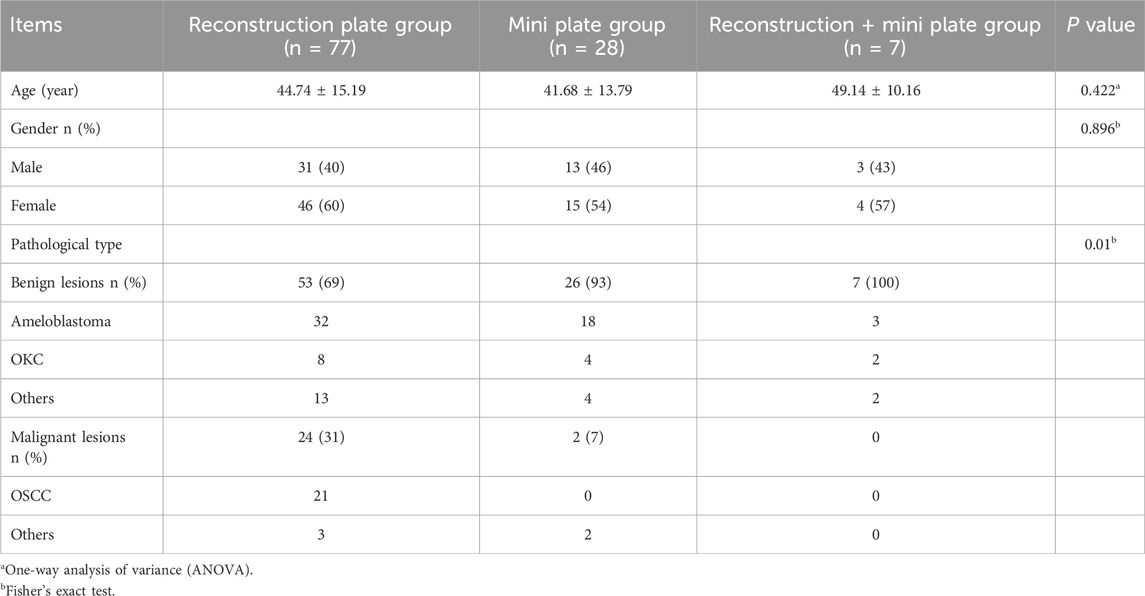
3.1 Patient characteristics
This study enrolled 112 patients who underwent single-stage reconstruction of segmental mandibular defects with vascularized iliac crest flaps, with iliac bone harvest lengths ranging from 4.49 to 13.2 cm. Four cases included skin islands or internal oblique muscles for soft tissue defect repair. The cohort comprised 47 males and 65 females, with ages ranging from 11 to 74 years. Pathological diagnoses primarily included ameloblastoma, odontogenic keratocyst, gingival carcinoma, and floor-of-mouth carcinoma (Table 1). The follow-up rates in the three groups were 85.7%, 78.6%, and 71.4%, respectively, and the follow-up duration showed no statistically significant difference (p = 0.620).
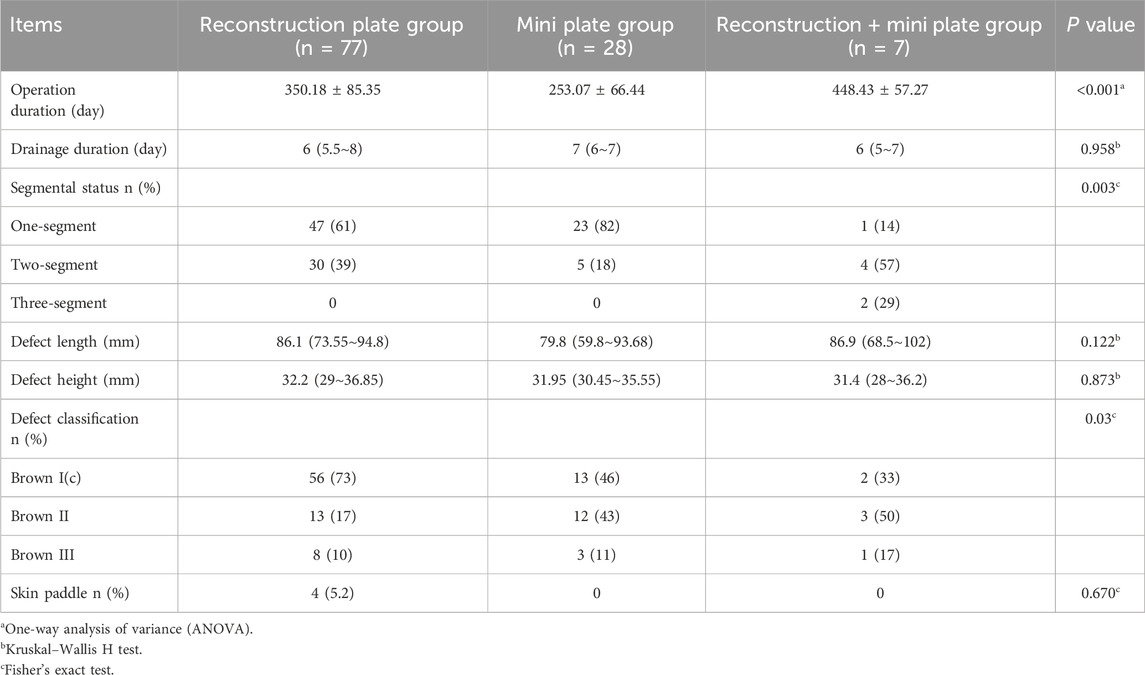
3.2 Perioperative characteristics
As shown in Table 2, the operative time was the shortest in the group treated with mini plates alone, whereas the postoperative drainage duration did not differ significantly among the three groups (p = 0.958). Reconstruction plates (either alone or combined with mini plates) were more frequently applied in multi-segmental iliac crest flap reconstructions, while mini plates were predominantly used in single-segmental cases. The distribution of defect classifications showed slight variations among the groups. In the reconstruction plate group, four patients received skin paddles, but the use of skin islands did not reach statistical significance between groups.
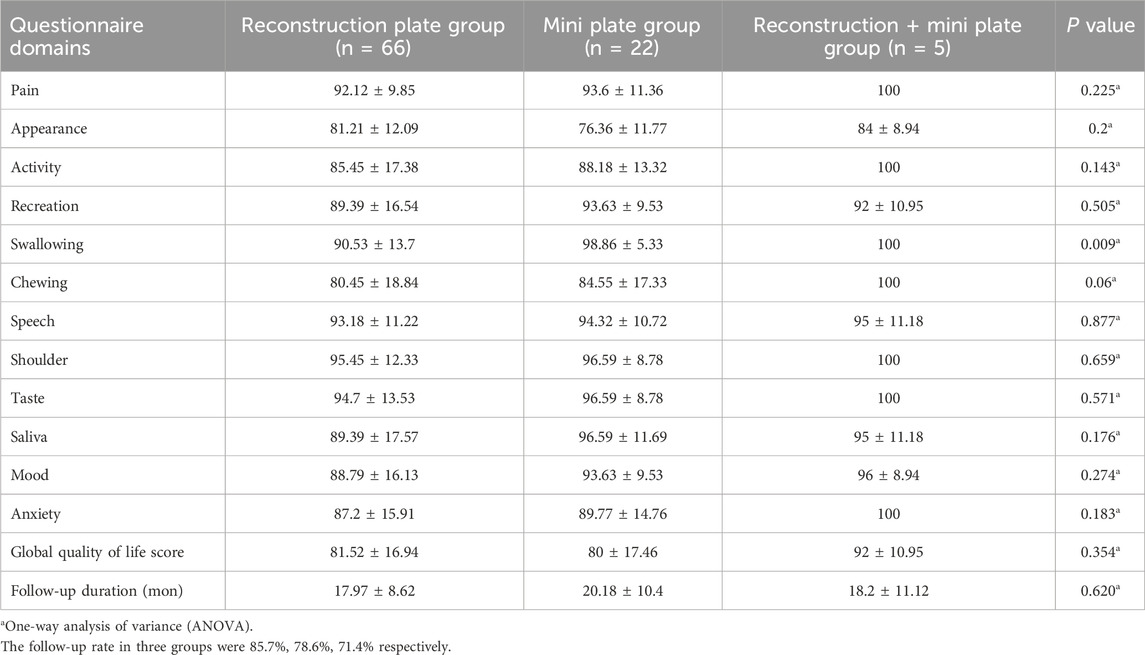
3.3 Quality of life assessment
The University of Washington Quality of Life Questionnaire (UW-QoL) was used to evaluate patients’ postoperative recovery (Table 3). Among the 12 assessed domains, only swallowing showed a statistically significant difference among the three groups, with the reconstruction plate group scoring significantly lower than the mini plate group (p = 0.009). For chewing, slight variations were observed among groups, but the difference did not reach statistical significance (p = 0.06). In other key domains such as pain, appearance, and speech, no significant differences were found between the groups. To exclude the potential impact of malignant tumors on QoL scores in patients reconstructed with reconstruction plates, we separately analyzed benign cases from both groups. The results were consistent with the overall QoL findings, as shown in Supplementary Table S1.
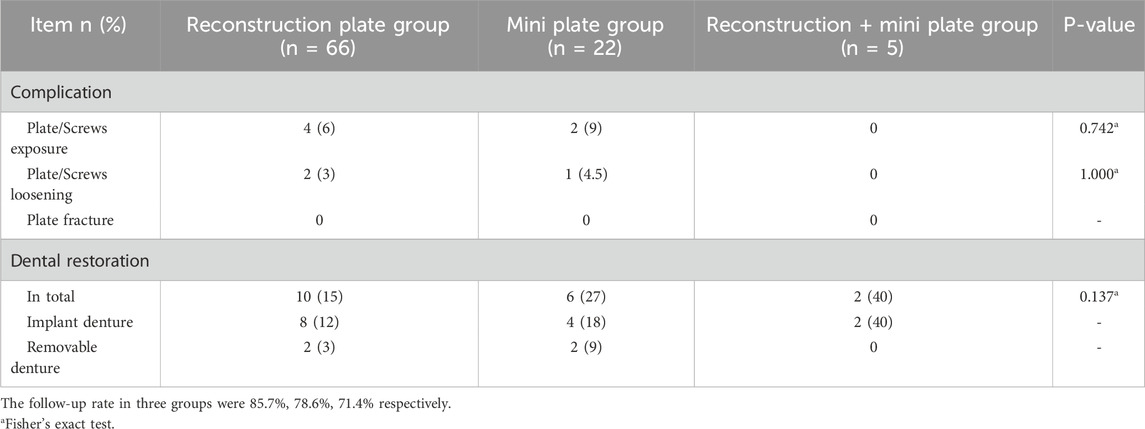
3.4 Complications and dental restoration
Fixation-related complications mainly included plate or screw exposure, loosening, and plate fracture, which were typically manifested by the development of fistulas with purulent discharge and confirmed through postoperative imaging examinations. The detailed incidence of these complications is summarized in Table 4. In addition, we investigated the prosthodontic rehabilitation status of patients in each group, and the overall rate of successful dental restoration was generally low across all groups.
4 Discussion
The use of iliac crest flaps pedicled on the deep circumflex iliac vessels, combined with titanium plate fixation, has become a mainstream approach for mandibular defect reconstruction (Garajei et al., 2021). In clinical practice, long-span reconstruction plates, mini plates, or a combination of both are commonly employed (Wang et al., 2024). This study provides a large-scale retrospective analysis of patients treated with these three fixation strategies, aiming to offer practical insights into their clinical application and outcomes.
The choice of fixation method in mandibular reconstruction extends beyond a purely technical decision and reflects a balance between biomechanical stability, surgical accessibility, and anatomical restoration (Wang et al., 2024). In general, reconstruction plates remain indispensable for large or load-bearing defects, as their rigidity ensures structural integrity under functional stress. However, their bulkiness and potential stress-shielding effects necessitate cautious use in regions where aesthetic contour and bone vitality are critical (Urken et al., 1998; Robey et al., 2008; Knitschke et al., 2022). Mini plates, on the other hand, offer a less invasive and more flexible option in anatomically confined spaces, allowing precise adaptation with minimal interference to surrounding tissues (Robey et al., 2008). The selective or combined use of both fixation systems underscores the importance of individualized planning—tailoring fixation to the defect’s geometry, functional requirements, and the surgeon’s intraoperative assessment. Rather than suggesting superiority of one method over another, our findings highlight that appropriate fixation selection, guided by defect characteristics and reconstructive principles, may be more decisive for long-term outcomes than the fixation choice.
From clinical perspective, although operative time varied among fixation methods, this difference mainly reflects surgical complexity rather than technical superiority, as mini plates were generally applied to less extensive, single-segmental reconstructions. The comparable drainage duration and similar rates of major complications—such as plate exposure, loosening, or fracture—suggest that both fixation systems offer acceptable safety profiles when appropriately selected. Postoperative UW-QoL assessment showed that although there was no significant difference in overall quality of life among the three groups, variations were observed in specific domains such as swallowing. The difference in swallowing scores between fixation methods may be attributed to variations in defect morphology, surgical exposure, and perioperative soft-tissue management. Mini plates are typically used in more localized reconstructions, causing less disruption to the oropharyngeal musculature and facilitating earlier restoration of swallowing coordination. In contrast, reconstruction plates are generally applied in anatomically more complex reconstructions, where wider surgical dissection and postoperative stiffness may transiently affect swallowing function. These factors collectively may account for the observed differences rather than the fixation hardware itself.
The rapid advancement of computer-assisted surgical technology has greatly enhanced the precision and predictability of vascularized bone flap transplantation (van Baar et al., 2021; Li et al., 2020; Shen et al., 2012). By acquiring high-resolution spiral CT scans of both the donor and recipient sites, patient-specific three-dimensional models can be generated, allowing for personalized virtual surgical planning through close collaboration between surgeons and biomedical engineers. The use of customized surgical guides—including cutting guides for mandibular resection, harvesting guides for iliac bone, and positioning guides for flap placement—has significantly improved intraoperative accuracy and reduced technical variability. Such digital integration facilitates precise bone alignment and tension-free fixation, thereby promoting reliable bone union. Mini plates are considered more favorable for promoting bone healing (Robey et al., 2008; Steffen et al., 2023). A study has shown that, in the short-term postoperative period, mini plates can achieve better bone healing compared with reconstruction plates; however, in the long term, the differences between the two fixation methods are not significant (Wang et al., 2024). In our series, no cases of apparent osseous non-union were observed during follow-up, reflecting the practical benefit of meticulous preoperative design rather than fixation technologies. These findings highlight how digital technology serves as a powerful adjunct in optimizing flap design and fixation accuracy, contributing to safer and more reproducible reconstructive outcomes.
This study has several limitations. As a retrospective analysis, it was not possible to completely eliminate the influence of surgeon preference in the selection of fixation methods. Nevertheless, as discussed above, fixation choice in our center is largely determined by the defect’s extent, anatomical location, and functional demands rather than by individual bias. In addition, due to the limited number of malignant cases within the mini plate group, subgroup comparisons based solely on pathology were of limited statistical value. To minimize this effect, we performed a separate analysis including only benign lesions, and the results remained consistent with the overall QoL findings (see Supplementary Table S1). Furthermore, the “Reconstruction + Mini Plate” subgroup had a small sample size for QoL and complication analysis, which may lead to insufficient statistical power. Despite our best efforts to conduct comprehensive postoperative follow-up, the total sample size remains limited, and long-term outcomes require validation in larger, prospective, multi-center studies. Future research integrating objective functional assessments and longitudinal quality-of-life data will be essential to further substantiate and refine these findings.
5 Conclusion
In summary, this study provides a descriptive overview of clinical outcomes associated with different fixation strategies used in mandibular reconstruction with vascularized iliac crest flaps. In our cohort, mini plates were typically selected for single-segment defects, whereas reconstruction plates were used for multi-segmental defects requiring enhanced mechanical stability. These choices reflected standard surgical practice rather than experimental allocation. Both fixation approaches yielded satisfactory postoperative outcomes, and no significant differences were observed in long-term overall quality of life. However, a statistically significant difference was noted in the “Swallowing” domain, where patients treated with mini plates reported better postoperative swallowing function, which may be related to differences in defect morphology and surgical exposure rather than the fixation device itself. Therefore, the present findings should be interpreted as reflecting real-world applications of fixation methods tailored to defect characteristics, rather than as evidence of the superiority of one technique over the other.
Data availability statement
The original contributions presented in the study are included in the article/Supplementary Material, further inquiries can be directed to the corresponding authors.
Ethics statement
The studies involving humans were approved by Medical Ethics Committee of Wuhan University Stomatological Hospital. The studies were conducted in accordance with the local legislation and institutional requirements. The participants provided their written informed consent to participate in this study. Written informed consent was obtained from the individual(s) for the publication of any potentially identifiable images or data included in this article.
Author contributions
W-qL: Investigation, Project administration, Writing – original draft. DL: Data curation, Formal Analysis, Writing – original draft. RZ: Data curation, Methodology, Writing – original draft. HL: Investigation, Methodology, Writing – review and editing. BZ: Software, Writing – original draft. JJ: Supervision, Writing – review and editing. YZ: Resources, Supervision, Writing – review and editing. BL: Investigation, Supervision, Writing – review and editing. TW: Supervision, Writing – review and editing.
Funding
The authors declare that financial support was received for the research and/or publication of this article. This work was supported by Fujian Provincial Department of Education’s Research Projects for Young and Middle-aged Teachers in Education (JAT200712).
Conflict of interest
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
Generative AI statement
The authors declare that Generative AI was used in the creation of this manuscript. During the preparation of this work, the authors utilized ChatGPT and DeepSeek to assist with translation and language polishing. After using these tools, the authors meticulously reviewed and edited the content as needed and take full responsibility for the content of the publication.
Any alternative text (alt text) provided alongside figures in this article has been generated by Frontiers with the support of artificial intelligence and reasonable efforts have been made to ensure accuracy, including review by the authors wherever possible. If you identify any issues, please contact us.
Publisher’s note
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
Supplementary material
The Supplementary Material for this article can be found online at: https://www.frontiersin.org/articles/10.3389/fbioe.2025.1688458/full#supplementary-material
References
Brown, J. S., Barry, C., Ho, M., and Shaw, R. (2016). A new classification for mandibular defects after oncological resection. Lancet Oncol. 17 (1), e23–e30. doi:10.1016/s1470-2045(15)00310-1
Garajei, A., Kheradmand, A. A., Miri, S. R., and Emami, A. (2021). A retrospective study on mandibular reconstruction using iliac crest free flap. Ann. Med. Surg. (Lond). 66, 102354. doi:10.1016/j.amsu.2021.102354
Graillon, N., Guyot, L., Thollon, L., Godio-Raboutet, Y., Roux, M. L., and Foletti, J. M. (2022). Do mandibular titanium miniplates affect the biomechanical behaviour of the mandible? A preliminary experimental study. J. Stomatol. Oral Maxillofac. Surg. 123 (6), e675–e681. doi:10.1016/j.jormas.2022.02.007
Graillon, N., Foletti, J. M., Godio-Raboutet, Y., Guyot, L., Varazzani, A., and Thollon, L. (2023). Mandibular titanium miniplates change the biomechanical behaviour of the mandible in the case of facial trauma: a three-dimensional finite element analysis. Bioeng. (Basel) 10 (9), 994. doi:10.3390/bioengineering10090994
Hassan, S. J., and Weymuller, E. A. (1993). Assessment of quality of life in head and neck cancer patients. Head. Neck 15 (6), 485–496. doi:10.1002/hed.2880150603
Knitschke, M., Yonan, M., Roller, F. C., Pons-Kuhnemann, J., Attia, S., Howaldt, H. P., et al. (2022). Osseous union after jaw reconstruction with fibula-free flap: conventional vs. CAD/CAM patient-specific implants. Cancers (Basel) 14 (23), 5774. doi:10.3390/cancers14235774
Kreutzer, K., Lampert, P., Doll, C., Voss, J. O., Koerdt, S., Heiland, M., et al. (2023). Patient-specific 3D-printed mini-versus reconstruction plates for free flap fixation at the mandible: retrospective study of clinical outcomes and complication rates. J. Craniomaxillofac Surg. 51 (10), 621–628. doi:10.1016/j.jcms.2023.09.019
Li, Y., Shao, Z., Zhu, Y., Liu, B., and Wu, T. (2020). Virtual surgical planning for successful second-stage mandibular defect reconstruction using vascularized iliac crest bone flap: a valid and reliable method. Ann. Plast. Surg. 84 (2), 183–187. doi:10.1097/sap.0000000000002102
Lin, H., Deng, W., Zhang, L., Ge, Z., Ma, C., Wu, T., et al. (2025a). Unleashing the potency of multi-segmental DCIA flap in mandibular reconstruction with the aid of virtual surgery- A retrospective cohort study. J. Craniomaxillofac Surg. 53 (5), 484–490. doi:10.1016/j.jcms.2024.12.018
Lin, H., Zeng, B., Zhang, L., Xiong, X., Shao, Z., Bu, L., et al. (2025b). Vascularized iliac crest free flap in maxillofacial reconstruction: pearls and pitfalls from 437 clinical application. J. Stomatol. Oral Maxillofac. Surg. 126 (3S), 102318. doi:10.1016/j.jormas.2025.102318
Pickrell, B. B., and Hollier, L. H. (2017). Evidence-based medicine: mandible fractures. Plast. Reconstr. Surg. 140 (1), 192e–200e. doi:10.1097/prs.0000000000003469
Robey, A. B., Spann, M. L., McAuliff, T. M., Meza, J. L., Hollins, R. R., and Johnson, P. J. (2008). Comparison of miniplates and reconstruction plates in fibular flap reconstruction of the mandible. Plast. Reconstr. Surg. 122 (6), 1733–1738. doi:10.1097/prs.0b013e31818a9ac5
Shen, Y., Sun, J., Li, J., Ji, T., and Li, M. M. (2012). A revised approach for mandibular reconstruction with the vascularized iliac crest flap by virtual surgical planning. Plast. Reconstr. Surg. 129 (3), 565e–566e. doi:10.1097/prs.0b013e3182419b42
Stanford-Moore, G., and Murr, A. H. (2022). Mandibular angle fractures. Facial Plast. Surg. Clin. North Am. 30 (1), 109–116. doi:10.1016/j.fsc.2021.08.009
Steffen, C., Sellenschloh, K., Willsch, M., Soares, A. P., Morlock, M. M., Heiland, M., et al. (2023). Patient-specific miniplates versus patient-specific reconstruction plate: a biomechanical comparison with 3D-printed plates in mandibular reconstruction. J. Mech. Behav. Biomed. Mater 140, 105742. doi:10.1016/j.jmbbm.2023.105742
Urken, M. L., Buchbinder, D., Costantino, P. D., Sinha, U., Okay, D., Lawson, W., et al. (1998). Oromandibular reconstruction using microvascular composite flaps: report of 210 cases. Arch. Otolaryngol. Head. Neck Surg. 124 (1), 46–55. doi:10.1001/archotol.124.1.46
van Baar, G. J. C., Schipper, K., Forouzanfar, T., Leeuwrik, L., Winters, H. A. H., Ridwan-Pramana, A., et al. (2021). Accuracy of computer-assisted surgery in maxillary reconstruction: a systematic review. J. Clin. Med. 10 (6), 1226. doi:10.3390/jcm10061226
Wang, Y., Wang, X., Bai, J., Guo, S., Shang, Z., and Shao, Z. (2024). Comparison of reconstruction plates and miniplates in mandibular defect reconstruction with free iliac flap. Clin. Oral Investig. 28 (11), 585. doi:10.1007/s00784-024-05985-9
Yang, Z. Y., Kang, Y. F., Lv, X. M., LiuFu, J. F., Zhang, L., Shan, X. F., et al. (2023). Iliac crest towards alveolar processes or mandibular inferior margin in mandibular reconstruction with a vascularized iliac bone flap: which is better? Clin. Oral Investig. 27 (2), 751–758. doi:10.1007/s00784-022-04823-0
Yu, Y., Zhang, W. B., Liu, X. J., Guo, C. B., Yu, G. Y., and Peng, X. (2020). Double-barrel fibula flap versus vascularized iliac crest flap for mandibular reconstruction. J. Oral Maxillofac. Surg. 78 (5), 844–850. doi:10.1016/j.joms.2020.01.003
Keywords: titanium miniplate, reconstruction plate, mandibular reconstruction, vascularized iliac crest flap, complication, fixation method, mini plate, quality of life
Citation: Lin W-q, Liu D, Zhou R, Lin H, Zeng B, Jia J, Zhao Y, Liu B and Wu T (2025) Can titanium miniplates provide superior fixation compared to reconstruction plates in mandibular repair with iliac crest flaps? A retrospective study. Front. Bioeng. Biotechnol. 13:1688458. doi: 10.3389/fbioe.2025.1688458
Received: 19 August 2025; Accepted: 17 November 2025;
Published: 02 December 2025.
Edited by:
Dedong Vincent Yu, Shanghai Jiaotong University School of Medicine Affiliated Sixth People’s hospital, ChinaReviewed by:
Philipp Lampert, Charité University Medicine Berlin, GermanyNadin Abouseif, Ajman University, United Arab Emirates
Copyright © 2025 Lin, Liu, Zhou, Lin, Zeng, Jia, Zhao, Liu and Wu. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Bing Liu, bGl1YmluZzk5MDlAd2h1LmVkdS5jbg==; Tianfu Wu, d3V0aWFuZnVAd2h1LmVkdS5jbg==
†These authors have contributed equally to this work
 Wen-qing Lin1,2†
Wen-qing Lin1,2† Jun Jia
Jun Jia Bing Liu
Bing Liu Tianfu Wu
Tianfu Wu