- 1Faculty of Health, School of Health and Human Performance, Dalhousie University, Halifax, NS, Canada
- 2Division of Medical Oncology, Department of Medicine, Faculty of Medicine, Dalhousie University, Halifax, NS, Canada
- 3Faculty of Medicine, Beatrice Hunter Cancer Research Institute, Dalhousie University, Halifax, NS, Canada
- 4School of Kinesiology, Acadia University, Wolfville, NS, Canada
Background: Few studies have examined differences in cancer survivors' physical activity and exercise behaviors by race/ethnicity and none have explored this relationship in a Canadian context.
Purpose: To explore the underlying factors that influence physical activity and exercise participation in African, Caribbean, and Black (ACB) cancer survivors.
Methods: Semi-structured interviews were conducted with eight ACB cancer survivors residing in Nova Scotia, Canada. Interviews broadly explored three main topics: (1) Exploring physical activity and exercise knowledge; (2) Barriers and facilitators to physical activity and exercise; and (3) Perceptions of cancer specific exercise trials and programs. Participant interviews were audio-recorded and transcribed verbatim and analyzed using an inductive thematic analysis.
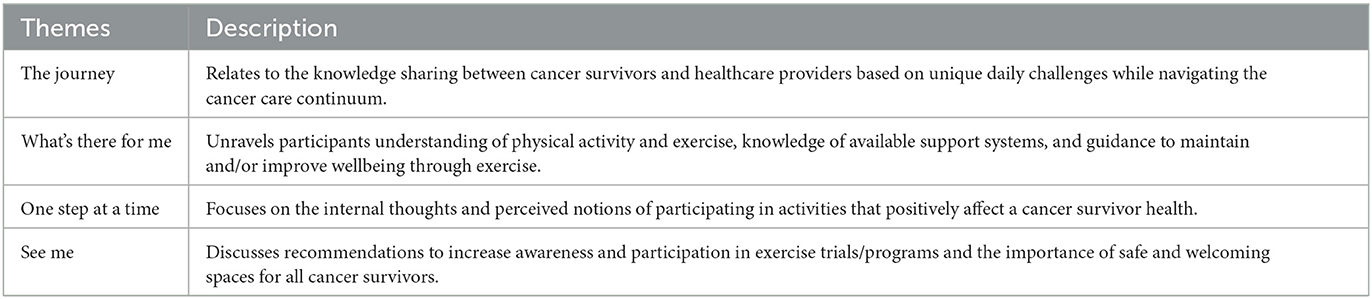
Results: An overall storyline of “No One Told Me” along with four primary themes emerged from the participant interviews. Theme 1, “the journey” describes the lack of knowledge sharing between healthcare providers and cancer survivors. Theme 2, “what's there for me” unravels participants understanding of physical activity and exercise, knowledge of available support, and guidance to maintain and/or improve wellbeing through exercise. Theme 3, “one step at a time” spotlights participants thoughts and perceptions of participating in physical activity and exercise. Theme 4, “See ME,” considers recommendations to increase awareness and participating in physical activity and exercise trials/programs and the importance of providing safe and welcoming spaces for all.
Discussion: This study offers insight into the barriers confronted by ACB cancer survivors when considering participation in physical activity and exercise. Participants were largely aware of the benefits of being physically active but described a lack of perceived knowledge sharing and welcoming spaces. Further investigation is needed to identify strategies to improve representation of ACB cancer survivors in clinical exercise studies and community, cancer-specific exercise programming.
1 Introduction
Given the lack of routinely collected race-based data, the impact of race/ethnicity on cancer incidence in Canada is not well understood. However, data from the United States shows that important racial and ethnic disparities exist. For example, compared to non-Hispanic white men and women, Black men have a 73% higher incidence rate of prostate cancer (1) and Black women have a 22% higher incidence rate of cervical cancer (2).
While cancer mortality rates have declined for all racial groups, African Americans continue to bear the highest mortality rates for most cancers (3, 4). For example, despite lower incidence, Black women are 40% more likely to die of breast cancer and 65% more likely to die of uterine cancer than white women (4). Moreover, despite steady improvements in overall cancer survival in both Canada and the United States, Black cancer patients/survivors (CS) continue to have a significantly lower 5-year survival rate compared to white CS (64% vs. 69%) (5, 6).
Despite improved survivorship across all populations, racially/ethnically diverse populations continue to experience a disproportionate cancer burden (1, 7, 8). Although comparable Canadian data are lacking, compared to white CS, Black CS living in the United States are at a higher risk of comorbid disease, cancer recurrence, second cancers, and as noted above, mortality (2, 9–11). This higher risk is driven by a complex interaction of genetics, tumor biology, socioeconomic inequalities, environment, cultural barriers, and sensitivity as well as systemic, institutional, and structural racism resulting in distrust of the health care system and a hesitancy to seek care in a timely manner (7).
With a large and growing population of CS, survivorship care has become a vital component of overall cancer care. Although advancements in treatments have resulted in improved survival, many CS will be confronted with long-term and late effects of cancer treatments negatively impacting their overall quality of life. Some of the most frequently reported concerns include loss of physical function, fatigue, joint pain, anxiety, sleep disturbances, neuropathy, and memory and concentration problems (12). CS are also known to have a higher burden of comorbid disease and premature mortality (13–16). Many of these concerns have been shown to be more prevalent in Black CS than white CS (13).
Physical activity and exercise for CS mitigates many treatment related adverse effects, reduces comorbid disease risk, cancer recurrence, second cancers, and improves quality of life and overall survival (17–20). With a growing body of evidence touting the benefits of exercise, several national and international agencies have disseminated exercise guidelines indicating that, at a minimum, CS should avoid inactivity (19–22). A recent systematic review found that most CS view exercise as beneficial but are confronted by several barriers to participation. Cancer and treatment related side-effects, presence of comorbidities, fear of injury/safety concerns, low self-efficacy and motivation, and a lack of time, money, program accessibility, and social support are frequently reported barriers. Conversely symptom relief, health benefits, social support by health care professionals, other CS, and family, and the accessibility and availability of cancer-specific programming were found to be strong facilitators (23). Burse et al. (24) reported similar barriers and facilitators to exercise among Black women with breast and endometrial cancer, but also highlighted faith as a commonly reported facilitator. These factors likely contribute to the fact that relatively few CS are sufficiently active to reap the many health benefits (25). Notably, compared to white CS, Black CS have been shown to be less likely to meet the recommended exercise guidelines (13). However, few studies have examined differences in CS physical activity and exercise behaviors by race/ethnicity (26) and none have explored this relationship in a Canadian context. Nova Scotia, a small province in Canada of ~1 million people, is home to a unique population (2.3%) of peoples of African, Caribbean, and Black (ACB) descent, and is said to be the birthplace of Black culture in Canada (27–29). Thus, this study sought to explore the factors (i.e., attitudes, barriers, facilitators) that influence physical activity and exercise engagement in ACB CS (30).
2 Methods
2.1 Design and procedures
This study employed a qualitative descriptive approach with individual, semi-structured interviews. A qualitative descriptive design was selected to elicit ACB CS perceptions of and experiences with exercise, which could then be used to inform the design and implementation of patient-centered exercise interventions (31, 32). Potential participants expressing an interest in learning more about the study were contacted by the first author. Those meeting the study inclusion criteria were invited to complete a one-time interview by phone or video conference. This study was approved by the Nova Scotia Health Research Ethics Board (ROMEO REB File #: 1027043). Participants provided written informed consent before completing any study related procedures.
2.2 Participant recruitment
Participants were recruited through several Black-led community organizations including the Health Association of African Canadians, African Nova Scotian Decade for People of African Descent Coalition, Black Physicians of Canada, and other trusted groups in the Nova Scotian ACB community. Recruitment posters were also shared through social media platforms, cancer support groups, and on notice boards in oncology outpatient clinics. Participants were eligible if they: (1) self-identified as ACB; (2) living with/beyond a cancer diagnosis; (3) were 19 years of age or older; (4) resided in Nova Scotia at the time of the interview; and (5) were able to understand and speak English.
2.3 Data collection
Semi-structured interviews were conducted between March 2022 and May 2022. All interviews were conducted by the lead author (CJC), a clinical exercise physiologist with expertise in cancer and exercise programming and a founding member of the Black Wellness Cooperative. The interview began with a brief introduction to the interviewer, overview of the study purpose, and general participant demographic and cancer history questions. The semi-structured interview broadly explored three main topics: (1) Exploring physical activity and exercise knowledge; (2) Barriers and facilitators to physical activity and exercise; and (3) Perceptions of cancer specific exercise trials. Prompts and follow-up questions were employed to elicit more detailed responses (Supplementary File). Interviews lasted between 12 min and 32 min and were audio-recorded and transcribed verbatim. Participants were recruited until data saturation was achieved.
2.4 Data analyses
Transcribed interviews were analyzed using an inductive thematic analysis as described by Braun and Clark (33). Phase 1 included familiarization with the data by reading interview transcripts three times and making notes along the way. In phase 2, a coding system was generated to identify relevant information. Phase 3 included identifying emerging themes by reviewing the coded data, followed by reviewing potential themes for quality and relevance to the data in phase 4. In phase 5, themes were clearly defined and then reported in phase 6. To ensure rigor, all transcripts were reviewed and coded by CJC and BH-H who has extensive qualitative expertise. Patterns and topics were discussed, and four main themes were identified. The resulting themes were reviewed by all members of the research team to ensure appropriate coding. Participants were offered the chance to read their transcripts and emerging themes to ensure their thoughts and feelings were conveyed appropriately, however none chose to do so. To protect participant identity, pseudonyms have been used in supporting quotations.
3 Results
3.1 Participant characteristics
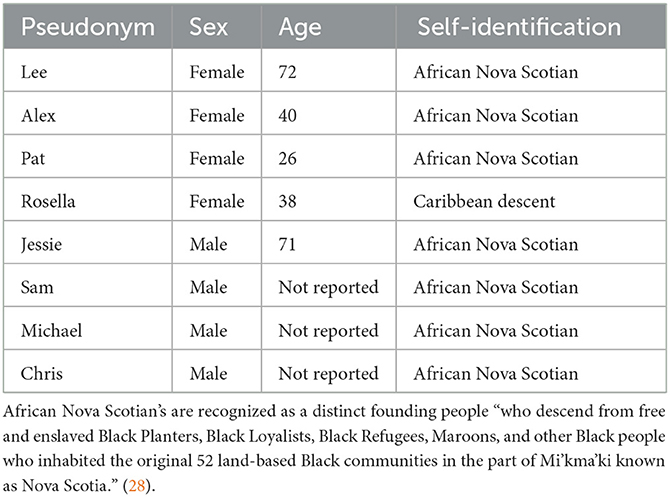
Eight ACB CS (4 females and 4 males) agreed to be interviewed (Table 1). Cancer diagnoses varied and included prostate, pancreas, bone marrow, endocrine, lymphoma, breast, liver, bowel, lung, and thyroid cancer. Some participants had more than one cancer. All participants underwent surgery, seven received chemotherapy, five received additional radiation therapy, and three received hormone therapy. The average time from diagnosis to the interview was 4.22 years. All participants resided in the Halifax Regional Municipality, an amalgamation of over 200 communities and neighborhoods in Nova Scotia, Canada at the time of the interview. To ensure participant anonymity cancer diagnoses and treatments have been described in aggregate form.
3.2 Themes
An overarching storyline entitled “no one told me” emerged from the participant interviews. This storyline reflects the limitations and barriers that contributed to the four primary themes; “The Journey,” “What's there for me,” “One step at a time,” and “See me” (Table 2).
3.2.1 No one told me
Despite the length of active surveillance after being diagnosed, participants commonly identified themes during the entirety of the cancer journey that hindered their ability to be fully aware and confident of what was happening and what supportive resources were available to them. Some participants identified that information shared was limited to their diagnosis and treatment plan, with little information provided on the ways their daily lives may be affected. While participants were aware of activities that might improve their wellbeing and support them through their cancer journeys, they reported that they did not receive specific recommendations or referrals to support engagement in these activities. As a result, participants noted that they felt hesitant in participating.
3.2.2 The journey
Participants noted the need to continually adapt each day to their new life as a CS and the lack of information and guidance by their oncologist and other members of the health care team surrounding exercise and nutrition. Alex stated, “My hematologist never told me about like going out and like staying active, like after my chemo like go for walks or eat healthy and stuff like that, they never really told me anything about that.” Alex was reflecting on her desire to do more and live better but did not feel the information and the importance of exercising was shared.
Participants also expressed a lack of knowledge and supportive information about elements that could positively and negatively impact their journey and daily changes to their “old” life. Charlie, recalled that “after my surgery I was kind of left to my own devices and I went back to what I was doing previously and what that did was it stretched my scarring.” Thus, it appears that Charlie did not seem to receive any information about what she should or should not do, which resulted in Charlie having a longer recovery period because of issues with scar tissue. This discouraged her from being as active as she was prior to her cancer diagnosis.
3.2.3 What's there for me?
It was evident that participants believed physical activity and exercise was good for their overall wellbeing prior to and after being diagnosed with cancer. Sam shared how he understood physical activity stating, “you know it just means continually being involved in different type of participation whether it be exercise, walking, golfing, any activity that keeps the juices flowing, right.” Jessie expressed his understanding of exercise as:
“Well, you're able to, to breathe better you know. You expand your lung capacity, you're able to do more such as you know walking, jogging, that sort of thing, you're able to extend how long you can do it. And just overall good and wellbeing.” (Jessie)
Both Sam and Jessie understood the importance of exercise, however when they were diagnosed with cancer, the importance of physical activity and exercise was not discussed by members of their health care team.
Several participants were able to differentiate between the commonly interchangeable used terms physical activity and exercise. Kelly provided examples of exercise in relation to housework:
“Physical activity can take any form, it can be cleaning your house, it could be out doing your gardening, it can be mowing your lawn. Exercise to me is more of there's a specific purpose to the exercise that you're doing. So, if I'm going to the gym, I'm going to the gym because I want to work on certain things, but overall physical activity can work on all of those things all at once.” (Kelly)
Moreover, Chris saw physical activity as “something that you do daily, like it's a daily activity that you do to keep your mind occupied.” Incorporating physical activity into your daily routines was one way in which Chris was able to stay active and focused on something other than their health.
Participants also acknowledged the important psychological benefits associated with physical activity and exercise, noting its significance in helping to remain positive throughout their cancer journey. The focus on mental health and reference to the importance of keeping mentally strong was shared by several participants. Charlie and Jessie talked about the benefits of physical activity and exercise with respect to their mental health.
“When I am physically active, I feel more mobile, and I have just like more confidence in what my body can take on. My mental health, so even just moving my body a little bit, provides, I think it's like a serotonin bomb, I immediately have an improvement in my mood” (Charlie)
“Well, I mean I know my physical activity, I'm sure keeps me mentally strong, you know as much as it works to keep your body in condition, it also keeps your mind active and keeps you I don't know, it can help keep you somewhat sane sometimes, especially going through treatment” (Jessie)
Despite being knowledgeable of the benefits of physical activity and exercise, many participants felt unsure of what was safe to perform during treatment and survivorship. Nearly all participants mentioned that nowhere along their cancer journey did their health care providers discuss the benefits of maintaining an active lifestyle unless brought up by the survivors themselves. Alex talked about how “while I was doing my chemo and stuff, they never really told me to be active or anything.”
There was no discussion with Alex and her healthcare providers about the benefits of physical activity and exercise for individuals diagnosed with cancer. Unlike Alex, Chris who was active after asking a question to their physician was encouraged to continue to do what he liked.
“Once I was able to go back to the gym, like my last surgery and stuff when I went to have my checkup I asked the guy I talked to if I could go to the gym and he said you can do anything you want.” (Chris)
Chris, although approved to return to the gym, was not informed by their caregivers about the benefits of physical activity and exercise as a CS. Overall, there were expressions of a lack of guidance and knowledge sharing resulting in confusion on what activities are safe or should be avoided.
“I have kind of like saggy areas now and I went to my surgeon and she was like well you shouldn't have been lifting weights, and I'm like nobody said that to me. We all knew that's what I did beforehand, but no one said to stop doing it afterwards” (Charlie)
The journey for many of the CS was not an easy one. For some it was two steps forward, one step back and several felt alone as they look their first steps into being a CS.
3.2.4 One step at a time
Barriers and facilitators to participating in physical activity and exercise increased as participants navigated through their cancer journeys. As a result, participants noted they could not complete physical activities as they once did and believed that there was an overall decrease in their wellbeing.
“My old perception of exercise and physical activity was like pretty intense, hard core, pushing myself to my limits consistently. And I just could not do that after my cancer diagnosis from so many perspectives. Physically I couldn't do what I could do before. Mentally, I wasn't sure I wanted to be pushing that way anymore.” (Charlie)
Although participants were aware of the benefits of physical activity, it was mentioned that their treatment related side effects, physical limitations, and other priorities were common reasons why they were not as active as they thought they should be. Several participants shared their ongoing struggle with physical activity, noting that:
“Well now that I'm finally feeling a little bit better after my chemo, I just want to relax. Like I don't want to do anything, I don't want to leave the house or anything. So I found it put a big barrier on me being physical and stuff like that because I just don't, didn't want to do anything, like it literally drains your body like so when you do get the energy, by the time I got the energy back it was time to get my kids and then 3 days later after I had my kids then it's time to go back to my chemo” (Pat)
“I've got bad knees, I've got sore joints, you know and that's what I find is really stopped me from wanting to go out and exercise any more cause my knees, my joints, all that arthritis in them now and all that they say these drugs could be a factor” (Jessie)
“The frustrating thing is side effects and how it can affect whether I'm going to go out and do something. So, with one of the side effects, if I go out and it's cold my brain plays tricks on me, so it tells me that my hands are burning, or my throat is burning, or my toes are burning. So, when I go out it's not fun and if I'm feeling nausea or if I have heartburn, which I've had the last week, I wasn't up to doing any kind of physical activity” (Charlie)
In addition to treatment related side effects, three participants indicated that their environment was a barrier to being physically active. Alex reflected on the lack of sidewalks in her community.
“Well, I find it's very hard in my neighborhood because of the fact that there's no sidewalks within the community so it's, I mean it's safe in some type of instance but then at the same time it's not. Like when I take my kids out and stuff you have to walk in the middle of the road and then if we see a car coming, we have to stop and go over to the side of the road just for safety reasons” (Alex)
Many participants were aware however, of the potential their environments had to facilitate outdoor activities and did not see their current neighborhood as a barrier to be active outside.
“I'm really fortunate, it is easy cause I'm like, well there's no sidewalks which is unfortunate, but I'm really close to a path so there's a path in my neighborhood that's close to my house that I have access to that goes along a lake. And I also have a backyard which I can do activity in.” (Charlie)
“I don't think there's anything, well what could probably make it harder for some who don't have money to do it, but then you don't really need money because you can go outside and go for a walk. You can do pretty much anything, you can do anything in your house or outside if you want to” (Chris)
“Well, I guess walking wise I live in North End Halifax, so from the point of view of just getting out and walking that's my own right? You know there's nothing in the area to prevent you, in the immediate area” (Jessie)
These three participants were able to express the convenience of walking and make the connection between walking as a feasible mode to be active for health, while understanding other modes may be limited through situational barriers.
Six participants were aware of facilities and programs that were being offered to the general public pertaining to physical activity support and exercise programs within their local communities, yet none had enrolled. A sub theme of One Step at a Time was “to tell or not to tell” which was identified as a key reason for individuals choosing not to participate in these programs. This subtheme emerged given the lack of non-cancer specific programming and/or trained exercise professionals in the field. As reflected by Lee, Pat, and Jesse, the need to constantly re-tell their cancer story contributed to mental and emotional hardships.
“And I just, I'm always constantly having to reiterate what I'm going through. And it's all so emotionally and mentally straining. What I'm looking for is somewhere that I feel safe, comfortable, and if someone who is trained to train cancer patients so that if something happens, they'll know what to do and they'll understand what I'm feeling” (Lee)
“I want people there that would like be able to tell us okay you're not pushing, don't push yourself too hard, like you could go harder, whatever, like stuff like that, like just to help, like because they would know like and especially if we were able to say o.k. this is the type of cancer we had, this is what affected us during the cancer” (Pat)
“There's all kinds of programs at the community center that promote it you know, but not cancer. I did the exercises and guidance when I was going through the treatments. I did like the encouragement from the PREP program, and you know just once I start something, I like to finish it, so once I got into the program I kept doing it until I got to the end of. But there isn't anything like that now. I don't know” (Jessie)
While participants expressed a desire to engage in exercise programs, they additionally noted they were not aware of programs where they would feel fully understood as ACB CS. This lack of recognition is reflected in the next theme, “See ME.”
3.2.5 See ME
All participants expressed that while they had no prior knowledge of programs that encouraged CS to be active within or outside of their local communities, they would have taken advantage of these programs if someone had told them. Charlie expressed, “if someone had said go to this group with other survivors and people who had just had surgery, I definitely would have done that because I really needed the guidance.” Similarly, Jessie mentioned, “if there was a program there that was set up for people with that cancer, I mean I would try to take advantage of that, of course.”
The importance of feeling welcomed was relevant for all eight participants. Participants expressed a need to feel seen and represented in some capacity as being important. Charlie commented that “for someone from the Black community it may be the importance of wanting to feel welcome in the recreational activity because most activities that I participate in there are very few people that look like me there.” Instructor support and encouragement were also highlighted as important program qualities. Pat commented that she was “not uncomfortable with color, like I wouldn't care if you were purple, blue or green, but it would be more like motivation.” When considering joining an exercise program for CS, participants expressed a need for an instructor who is there for the right reasons, is knowledgeable in the field and sees the individual along with their cancer diagnosis.
“Having a program that the instructor can like focus, I mean not just focus on me, like focus on other individuals, but focus on me, make sure I'm doing what I'm doing properly and then they know what exercises to do. Like say don't do that, do this instead. Just someone who's invested, who's not just going to like, someone who's not just there for a pay check, you know what I mean?” (Lee)
“It's a lot. Because I don't get remission like some cancer patients do and I don't have a cure, they don't have a cure for me, so I'm like dealing with this for the rest of my life, you know what I mean? So, to find something for me, I'll say for me, kind of selfish but, find something for me would be so amazing” (Alex)
4 Discussion
This study illuminates some of the internal and external barriers, as well as facilitators for ACB CS to be physically active. While participants expressed an understanding of the benefits of exercise, they noted a lack of guidance and a desire to be invited to welcoming spaces supporting exercise and physical activity for all CS.
4.1 The journey
The literature defines the cancer journey to span across the time of diagnosis to the completion of treatment and long into survivorship (34). Addressing information needs for CS at different stages of their cancer journey can help them cope with and digest the challenges of their diagnosis and any obstacles they may face (35, 36). Tran et al. (35) surveyed over 72 000 CS, ages 16 and older, to examine their experience and overall satisfaction with their care during their cancer journey. They found that CS valued an abundance of information early on in their journey. Information about their care and possible adverse effects were associated with better CS satisfaction and perceived control of their wellbeing. Similarly, Li et al. (36) reported improvements in CS health outcomes, improved symptoms, physical functioning, physiological status, and pain with proper CS-provider communication. In contrast, poor CS-provider communication can result low satisfaction. Song et al. (37) explored the experiences of American ACB survivors and reported low satisfaction in communication around cancer information, shared decision making, empathy and understanding and respect, ultimately resulting in a negative survivorship experience.
Everyone's cancer journey is unique. There will be daily challenges, changes, and obstacles, but positive guidance and knowledge sharing can help CS overcome or adapt to these situations. Increasing awareness, availability and support of physical activity and exercise programs within the ACB community can be a positive mechanism to improve quality of life while navigating the cancer continuum. Encouraging safe, welcoming, and uplifting spaces is important to increase participation in exercise programs.
4.2 What's there for me?
Consistent with the findings of this study, a significant proportion of healthcare professionals do not discuss the importance of physical activity and exercise with their cancer patients (38). Despite this, many CS are still aware of the benefits of physical activity and exercise on their wellbeing (17, 39). Caperchione et al. (40) reported that most CS agree that exercise was safe and beneficial during and after their cancer treatment. Notably, although they saw it as a positive, half of the surveyed CS would not consider participating. They believed the provided exercise recommendations from the oncologist may not be aligned with the CS perceptions of exercise. Further, their results suggested that half of the CS would prefer receiving on-going exercise recommendations and counseling from an exercise specialist who is part of the oncology team. These findings could lead to a system where oncologists and nurses can provide insight on the safety of exercising in tandem with a referral to an exercise specialist to facilitate further adherence.
4.3 One step at a time
Similar to Hirschey et al. (26) participants in this study reported treatment related side effects (e.g., fatigue, pain), emotional wellbeing (“…mentally, I was wasn't sure that I wanted to push anymore.” – Charlie), environmental barriers (i.e., walkable neighborhood), and competing demands. Commonly perceived barriers personal barriers such as lack of time and knowledge did not seem to be significant barriers to engaging in physical activity. Piacentine et al. (41) found through a focus group with American ACB breast CS, that despite knowing the benefits, physical activity and exercise were never made a priority and took a back seat to other daily responsibilities (family, work, etc.). They also reported that exercise was not part of their treatment plan and noted that their healthcare team emphasized proper nutrition, but not the importance of exercise. The significance of the role of the healthcare team in promoting physical activity in CS has been widely documented (42–44) and was emphasized by participants in the current study who highlighted the importance of feeling valued and a need for greater knowledge sharing and support from healthcare providers to be physically active.
A unique barrier among the participants in this study that was not noted in the literature, was the burden of retelling their cancer journey. As healthcare providers across Nova Scotia continue to use various databases to store health records, individuals continue to carry the burden of reiterating their medical journey when faced with a new provider (45). Although not all exercise programs are in a clinical setting or physician-referred, a form of harmonized medical records may be beneficial in clinical research settings for recruitment and consenting potential participants to minimize the distress of reliving difficult moments.
4.4 See ME
Despite the racial disparities and prevalence of comorbidities, there is limited data on ACB CS participation in exercise trials and programs. Participants in the current study reported an increase in awareness of specific cancer programs essential to increase participation. Black et al. (46) found integrating ACB CS preferences and needs into programming is essential to improve participation. They concluded that the program should support efforts to maintain physical activity and exercise throughout the cancer journey, instructors should understand the physical and emotional impact of cancer, face-to-face communication and share strategies to cope with potential adverse effects from treatment and other potential lifestyle barriers. In Nova Scotia, Evans et al. (47) explored the perceptions and experiences of ACB breast and prostate CS. In their study, focus group participants expressed feelings of being disenfranchised from health care due to distance to treatment services, difficulty in transportation and racist attitudes of healthcare professionals. These disparities may be factors influencing low enrollment rates in current exercise trials for CS in Nova Scotia and need to be explored further.
4.5 Strengths and limitations
A strength of this research is that, to the best of our knowledge, it is the first to explore the knowledge, preferences, and barriers of physical activity and exercise in ACB survivors residing in Canada. Notwithstanding the significance of this research, the study is not without limitations. While qualitative methods are not intended to be extrapolated to the general population, the study sample was limited to ACB cancer survivors living in Nova Scotia. As healthcare systems and access to cancer-specific programming varies from province to province, participants from other parts of Canada may have other important perspectives. Given the potential for self-selection bias, it is also possible that participants in the current study viewed physical activity and exercise more favorably and their desire for greater knowledge sharing and access exercise programs may not reflect those who do not value these activities. Finally, no health care providers were interviewed. Future research should explore their perspectives regarding knowledge sharing and facilitating access to cancer-specific exercise programs.
5 Conclusions
This study offers insight into the underlying factors that influence physical activity and exercise participation in ACB CS in Canada. Participants discussed a general lack of awareness of cancer and exercise specific programming, a lack of perceived clinician communication, and a need to be seen and better supported both as a CS and as a person of ACB descent with cancer. The major themes of: What's There for Me and One Step at a Time, illustrate the unique experience and narrative of ACB survivors navigating their cancer journeys. Key findings from this study include:
1. ACB survivors are largely aware of the benefits of being active throughout the cancer journey; however a greater emphasis on the psychosocial benefits is needed. Reinforcement and reiteration by their cancer care providers would validate and help direct action;
2. Tailored outreach strategies (e.g., creating trusted relationships with recognized community leaders, continued education for healthcare providers on the benefits of exercise, inclusive marketing materials) and welcoming spaces may be essential in improving diversity in exercise programs and trials; and
3. Collaborative medical record storage should be considered to minimize participant burden of re-telling their cancer journey.
Future researchers can build on this study as a starting point and guide for digging deeper into asking the right questions to uncover how to improve representation of ACB CS in clinical exercise studies and community exercise programming designed for CS. This study illustrated a gap in knowledge sharing between healthcare providers and ACB CS. It has also identified a need to further investigate healthcare providers knowledge of exercise and physical activity for ACB CS and their willingness to prescribe and/or refer their ACB patients to existing programs.
Data availability statement
The datasets presented in this article are not readily available because consent to share with outside investigators was not obtained. Requests to access the datasets should be directed to MK, bWVsYW5pZS5rZWF0c0BkYWwuY2E=.
Ethics statement
The studies involving humans were approved by Nova Scotia Health Research Ethics Board. The studies were conducted in accordance with the local legislation and institutional requirements. The participants provided their written informed consent to participate in this study.
Author contributions
CC, BH-H, and MK: conceptualization and writing and editing. CC, BH-H, SG, JF, and MK: methodology. CC: data collection and transcription. CC and BH-H: analyses. All authors contributed to manuscript revision, read, and approved the submitted version.
Funding
CC was supported by a Maritime SPOR Trainee Support Award. The authors declare that no additional funds, grants, or other support were received during the preparation of this manuscript.
Acknowledgments
Portions of this work originally appeared in CC master's thesis, Preferences, Barriers and Facilitators to Exercise and Physical Activity in Cancer Survivors of African, Caribbean, and Black descent in Nova Scotia. The authors would like to thank the participants who made this work possible.
Conflict of interest
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
The author(s) MK declared that they were an editorial board member of Frontiers, at the time of submission. This had no impact on the peer review process and the final decision.
Publisher's note
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
Supplementary material
The Supplementary Material for this article can be found online at: https://www.frontiersin.org/articles/10.3389/fcacs.2023.1229028/full#supplementary-material
References
1. Zavala VA, Bracci PM, Carethers JM, Carvajal-Carmona L, Coggins NB, Cruz-Correa MR, et al. Cancer health disparities in racial/ethnic minorities in the United States. Br J Cancer. (2021) 124:315–32. doi: 10.1038/s41416-020-01038-6
2. Giaquinto AN, Miller KD, Tossas KY, Winn RA, Jemal A, Siegel RL. Cancer statistics for African American/black people 2022. CA Cancer J Clin. (2022) 72:202–29. doi: 10.3322/caac.21718
3. DeSantis CE, Miller KD, Goding Sauer A, Jemal A, Siegel RL. Cancer statistics for African Americans, 2019. CA Cancer J Clin. (2019) 69:211–33. doi: 10.3322/caac.21555
4. Cancer Facts Figures 2023. (2023) Available online at: https://www.cancer.org/research/cancer-facts-statistics/all-cancer-facts-figures/2023-cancer-facts-figures.html (accessed November 21, 2023).
5. Ellison LF. The cancer survival index: Measuring progress in cancer survival to help evaluate cancer control efforts in Canada. Health Rep. (2021) 32:14–26. doi: 10.25318/82-003-x202100900002-eng
6. SEER*Explorer. (2023) Available online at: https://seer.cancer.gov/statistics-network/explorer/application.html?site=1&data_type=4&graph_type=5&compareBy=race&chk_race_9=9&chk_race_8=8&series=9&sex=1&age_range=1&hdn_stage=101&advopt_precision=1&advopt_show_ci=on&hdn_view=0&advopt_show_apc=on&advopt_display=2#resultsRegion0 (accessed May 5, 2023).
7. Williams PA, Zaidi SK, Sengupta R. AACR cancer disparities progress report 2022. Cancer Epidemiol Biomarkers Prev. (2022) 31:1249–50. doi: 10.1158/1055-9965.EPI-22-0542
8. Government of Canada SC. Do Cancer Incidence and Mortality Rates Differ Among Ethnicities in Canada? (2021) Available online at: https://www150.statcan.gc.ca/n1/pub/82-003-x/2021008/article/00001-eng.htm (accessed May 5, 2023).
9. Kabat GC, Ginsberg M, Sparano JA, Rohan TE. Risk of recurrence and mortality in a multi-ethnic breast cancer population. J Racial Ethn Health Disparities. (2017) 4:1181–8. doi: 10.1007/s40615-016-0324-y
10. Asare M, McIntosh S, Culakova E, Alio A, Umstattd Meyer MR, Kleckner AS, et al. Assessing physical activity behavior of cancer survivors by race and social determinants of health. Int Q Community Health Educ. (2019) 40:7–16. doi: 10.1177/0272684X19857427
11. Doose M, Steinberg MB, Xing CY, Lin Y, Cantor JC, Hong CC, et al. Comorbidity management in black women diagnosed with breast cancer: the role of primary care in shared care. J Gen Intern Med. (2021) 36:138–46. doi: 10.1007/s11606-020-06234-x
12. Schmidt ME, Goldschmidt S, Hermann S, Steindorf K. Late effects, long-term problems and unmet needs of cancer survivors. Int J Cancer. (2022) 151:1280–90. doi: 10.1002/ijc.34152
13. Beebe-Dimmer JL, Albrecht TL, Baird TE, Ruterbusch JJ, Hastert T, Harper FWK, et al. The detroit research on cancer survivors (ROCS) pilot study: a focus on outcomes after cancer in a racially diverse patient population. Cancer Epidemiol Biomark Prev Publ Am Assoc Cancer Res Cosponsored Am Soc Prev Oncol. (2019) 28:666–74. doi: 10.1158/1055-9965.EPI-18-0123
14. Leach CR, Weaver KE, Aziz NM, Alfano CM, Bellizzi KM, Kent EE, et al. The complex health profile of long-term cancer survivors: prevalence and predictors of comorbid conditions. J Cancer Surviv Res Pract. (2015) 9:239–51. doi: 10.1007/s11764-014-0403-1
15. Gotze H, Taubenheim S, Dietz A, Lordick F, Mehnert A. Comorbid conditions and health-related quality of life in long-term cancer survivors-associations with demographic and medical characteristics. J Cancer Surviv Res Pract. (2018) 12:712–20. doi: 10.1007/s11764-018-0708-6
16. Cavers D, Habets L, Cunningham-Burley S, Watson E, Banks E, Campbell C. Living with and beyond cancer with comorbid illness: a qualitative systematic review and evidence synthesis. J Cancer Surviv Res Pract. (2019) 13:148–59. doi: 10.1007/s11764-019-0734-z
17. Stout NL, Baima J, Swisher AK, Winters-Stone KM, Welsh J. A systematic review of exercise systematic reviews in the cancer literature (2005-2017). PM R. (2017) 9:S347–84. doi: 10.1016/j.pmrj.2017.07.074
18. Schwartz AL, de Heer HD, Bea JW. Initiating exercise interventions to promote wellness in cancer patients and survivors. Oncol Williston Park N. (2017) 31:711–7.
19. Campbell KL, Winters-Stone KM, Wiskemann J, May AM, Schwartz AL, Courneya KS, et al. Exercise guidelines for cancer survivors: consensus statement from international multidisciplinary roundtable. Med Sci Sports Exerc. (2019) 51:2375–90. doi: 10.1249/MSS.0000000000002116
20. Hayes SC, Newton RU, Spence RR, Galvão DA. The exercise and sports science Australia position statement: exercise medicine in cancer management. J Sci Med Sport. (2019) 22:1175–99. doi: 10.1016/j.jsams.2019.05.003
21. Schmitz KH, Courneya KS, Matthews C, Demark-Wahnefried W, Galvao DA, Pinto BM, et al. American college of sports medicine roundtable on exercise guidelines for cancer survivors. Med Sci Sports Exerc. (2010) 42:1409–26. doi: 10.1249/MSS.0b013e3181e0c112
22. Segal R, Zwaal C, Green E, Tomasone JR, Loblaw A, Petrella T, et al. Exercise for people with cancer: a clinical practice guideline. Curr Oncol Tor Ont. (2017) 24:40–6. doi: 10.3747/co.24.3376
23. Elshahat S, Treanor C, Donnelly M. Factors influencing physical activity participation among people living with or beyond cancer: a systematic scoping review. Int J Behav Nutr Phys Act. (2021) 18:50. doi: 10.1186/s12966-021-01116-9
24. Burse NR, Bhuiyan N, Mama SK, Schmitz KH. Physical activity barriers and resources among black women with a history of breast and endometrial cancer: a systematic review. J Cancer Surviv Res Pract. (2020) 14:556–77. doi: 10.1007/s11764-020-00873-z
25. Hyland KA, Jacobs JM, Lennes IT, Pirl WF, Park ER. Are cancer survivors following the national comprehensive cancer network health behavior guidelines? An assessment of patients attending a cancer survivorship clinic. J Psychosoc Oncol. (2018) 36:64–81. doi: 10.1080/07347332.2017.1399193
26. Hirschey R, Xu J, Lea DF, Milner JL, Duggins P, Coleman K, et al. Barriers and facilitators to the engagement of physical activity among Black and African American cancer survivors during and after treatments. Supp Care Cancer Off J Multinatl Assoc Support Care Cancer. (2023) 31:136. doi: 10.1007/s00520-023-07601-0
27. Our History – Black Cultural Centre for Nova Scotia (2023) Available online at: https://bccns.com/our-history/ (accessed May 5, 2023).
28. Dalhousie University. African Nova Scotian Strategy. (2023) Available online at: https://www.dal.ca/about-dal/african-nova-scotian-connection/african-nova-scotian-strategy.html (accessed May 5, 2023).
29. Government of Canada SC. Diversity of the Black Population in Canada: An Overview. (2019) Available online at: https://www150.statcan.gc.ca/n1/pub/89-657-x/89-657-x2019002-eng.htm (accessed November 23, 2023).
30. Chiekwe J,. Preferences, Barriers Facilitators to Exercise Physical Activity in Cancer Survivors of African, Caribbean, Black descent in Nova Scotia. (2022) Available online at: https://DalSpace.library.dal.ca//handle/10222/81895 (accessed September 22, 2022).
31. Kim H, Sefcik JS, Bradway C. Characteristics of qualitative descriptive studies: a systematic review. Res Nurs Health. (2017) 40:23–42. doi: 10.1002/nur.21768
32. Sandelowski M. Whatever happened to qualitative description? Res Nurs Health. (2000) 23:334–40. doi: 10.1002/1098-240x(200008)23:4<334::aid-nur9>3.0.co;2-g
33. Braun V, Clarke V. Using thematic analysis in psychology. Qual Res Psychol. (2006) 3:77–101. doi: 10.1191/1478088706qp063oa
34. Garcia DO, Thomson CA. Physical activity and cancer survivorship. Nutr Clin Pract Off Publ Am Soc Parenter Enter Nutr. (2014) 29:768–79. doi: 10.1177/0884533614551969
35. Tran Y, Lamprell K, Nic Giolla Easpaig B, Arnolda G, Braithwaite J. What information do patients want across their cancer journeys? A network analysis of cancer patients' information needs. Cancer Med. (2019) 8:155–64. doi: 10.1002/cam4.1915
36. Li CC, Matthews AK, Dossaji M, Fullam F. The relationship of patient-provider communication on quality of life among African-American and white cancer survivors. J Health Commun. (2017) 22:584–92. doi: 10.1080/10810730.2017.1324540
37. Song L, Hamilton JB, Moore AD. Patient-healthcare provider communication: perspectives of African American cancer patients. Health Psychol Off J Div Health Psychol Am Psychol Assoc. (2012) 31:539–47. doi: 10.1037/a0025334
38. Alderman G, Semple S, Cesnik R, Toohey K. Health care professionals' knowledge and attitudes toward physical activity in cancer patients: a systematic review. Semin Oncol Nurs. (2020) 36:151070. doi: 10.1016/j.soncn.2020.151070
39. Morishita S, Suzuki K, Okayama T, Inoue J, Tanaka T, Nakano J, et al. Recent findings in physical exercise for cancer survivors. Phys Ther Res. (2023) 26:10–6. doi: 10.1298/ptr.R0023
40. Caperchione CM, Sharp P, Phillips JL, Agar M, Liauw W, Harris CA, et al. Bridging the gap between attitudes and action: a qualitative exploration of clinician and exercise professional's perceptions to increase opportunities for exercise counselling and referral in cancer care. Patient Educ Couns. (2022) 105:2489–96. doi: 10.1016/j.pec.2021.11.002
41. Piacentine LB, Robinson KM, Waltke LJ, Tjoe JA, Ng AV. Promoting team-based exercise among African American breast cancer survivors. West J Nurs Res. (2018) 40:1885–902. doi: 10.1177/0193945918795313
42. Schmitz KH, Campbell AM, Stuiver MM, Pinto BM, Schwartz AL, Morris GS, et al. Exercise is medicine in oncology: engaging clinicians to help patients move through cancer. CA Cancer J Clin. (2019) 69:468–84. doi: 10.3322/caac.21579
43. Parker NH, Arlinghaus KR, Johnston CA. Integrating physical activity into clinical cancer care. Am J Lifestyle Med. (2018) 12:220–3. doi: 10.1177/1559827618759478
44. Ramsey I, Chan A, Charalambous A, Cheung YT, Darling HS, Eng L, et al. Exercise counselling and referral in cancer care: an international scoping survey of health care practitioners' knowledge, practices, barriers, and facilitators. Support Care Cancer. (2022) 30:9379–91. doi: 10.1007/s00520-022-07342-6
45. Persaud N. A national electronic health record for primary care. CMAJ Can Med Assoc J J Assoc Medicale Can. (2019) 191:E28–9. doi: 10.1503/cmaj.181647
46. Black KZ, Johnson LS, Samuel-Hodge CD, Gupta L, Sundaresan A, Nicholson WK. Perceived barriers and preferred components for physical activity interventions in African-American survivors of breast or endometrial cancer with type 2 diabetes: the SUCCESS framework. Support Care Cancer Off J Multinatl Assoc Support Care Cancer. (2018) 26:231–40. doi: 10.1007/s00520-017-3839-9
Keywords: African, Black, Caribbean, cancer survivor, exercise, barriers, facilitators, qualitative
Citation: Chiekwe CJ, Hamilton-Hinch B, Grandy SA, Fowles J and Keats MR (2024) “No one told me”: exploring factors influencing physical activity participation in Black Nova Scotian cancer survivors. Front. Cancer Control Soc. 1:1229028. doi: 10.3389/fcacs.2023.1229028
Received: 04 July 2023; Accepted: 21 December 2023;
Published: 12 January 2024.
Edited by:
Elena Amaricai, Victor Babes University of Medicine and Pharmacy, RomaniaReviewed by:
Elizabeth Blackman, Fox Chase Cancer Center, United StatesRussell McIntire, Lehigh University, United States
Copyright © 2024 Chiekwe, Hamilton-Hinch, Grandy, Fowles and Keats. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Melanie R. Keats, bWVsYW5pZS5rZWF0c0BkYWwuY2E=
 C. Joy Chiekwe
C. Joy Chiekwe Barbara Hamilton-Hinch1
Barbara Hamilton-Hinch1 Melanie R. Keats
Melanie R. Keats