Introduction
The blood pressure (BP) is the force generated by the heart that drives circulation of the blood. After Scipione Riva-Rocci first introduced the sphygmomanometer at the beginning of last century, for decades arterial hypertension (hypertension) was considered to be “essential” for securing the perfusion of vital organs, as the brain, heart, and kidney. The term “essentielle hypertonie,” coined by the German clinicians, was indeed meant to underline the fact that BP, alongside the heart beat, is the essence of life, as there can be no life without BP. This led to contend that the higher the BP values, the better for vital organs perfusion, a view testified by Paul Dudley White’s, one of the top cardiologists of the last century, statement: “Hypertension may be an important compensatory mechanism, which should not be tampered with, even were it certain we could control it.”
It took the randomized clinical trials in the eighties of the last century to dismantle this misconception, and finally prove that lowering BP was beneficial, e.g., better than placebo for lowering cardiovascular events (1–3). Hypertensiologists should indeed be proud of the fact that antihypertensive treatment has been the first cardiovascular therapy whose efficacy has been proven beyond doubts with randomized clinical trials and use of hard end points. Several decades of epidemiological and experimental research, along with a number of further large-scale clinical trials [reviewed in Ref. (4–6)], have now led the widely accepted concept that hypertension is the “number one” cardiovascular risk factor, not only because of its very high prevalence but also for its tight relationship with cerebro- and cardiovascular events.
In westernized countries around 40% of the adult men and women have hypertension, which puts them at an excess risk of stroke, both hemorrhagic and ischemic, acute coronary syndromes, heart failure, and chronic kidney disease with the ensuing need for renal replacement therapy. Considering that worldwide about 13.5% of premature deaths were attributed to hypertension in 2001, the World Health Organization defined hypertension “a humanitarian tragedy on a planetary scale” (7, 8).
Achievements in the Management of Hypertension
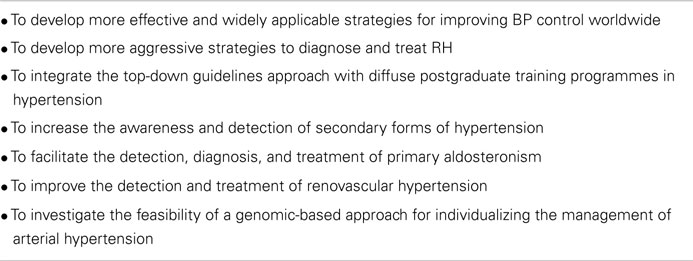
The increasing awareness of the detrimental effects of hypertension has been paralleled by the development of an overwhelming amount of knowledge on cardiovascular pathophysiology. This has had enormous fallout in the diagnostic approach and treatment of many other cardiovascular diseases. It has also led to the development of effective non-pharmacologic measures and pharmacologic agents. Accordingly, current guidelines recommend a number of life-style changes to improve the control of BP values, both in primary prevention and as a valuable addition to pharmacologic treatment. The latter has made terrific steps since the Kempner fruits and rice diet, and the first introduction of the ganglio-plegic drugs in the sixties of the previous century. Accordingly, more than 100 drugs, alone or in predefined combinations, are now available for the treatment of hypertension. Notwithstanding these progresses, far too many hypertensive patients continue to have BP far above the target values that would be desirable based on their overall cardiovascular risk profile. Current, estimates of uncontrolled hypertension indicate that up to 30–40% of the patients have BP values above target. Hence, there are several challenges that need to be addressed in the near future (Table 1).
Problem of Resistant Hypertension
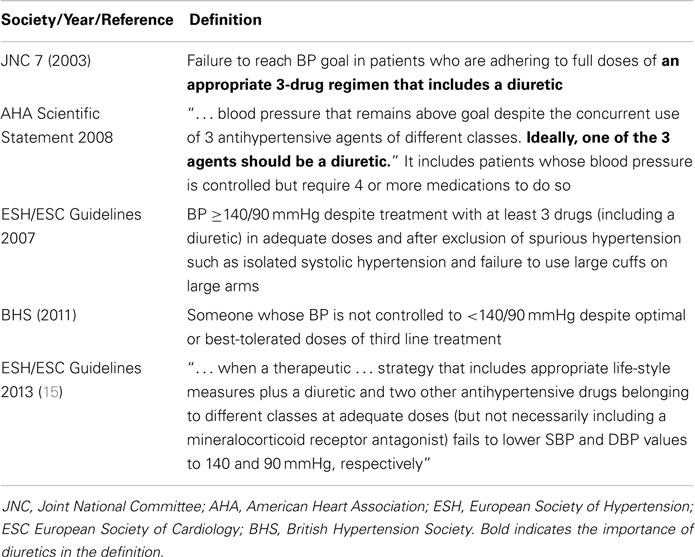
Considering that uncontrolled hypertension leads to excess target organ damage and complications (9), the patients with resistant hypertension (RH) are still exposed to an excess risk of CV events (10). Recognizing the importance of this re-emerging problem the major scientific societies, both in Europe and in North America, have introduced the concept of drug “resistant” or refractory hypertension and developed definitions for this condition (Table 2). Albeit varying slightly across societies, these definitions are useful in drawing attention to this problem. They also underline the fact that hypertension is a heterogeneous condition whose pathophysiological mechanisms still remain elusive in many patients.
Hence, a major challenge for the coming years entails developing more aggressive research and novel therapeutic strategies for RH, if we are not going to passively accept a situation that takes still too many lives every year worldwide.
Current Strategies to Fight Hypertension
The general approach adopted thus far by most international scientific societies and national societies to address the issue of improving the control of hypertension, has been through the release of guidelines for the management of hypertension. For example, the European Society of Cardiology (ESC) and the European Society of Hypertension (ESH) have jointly released guidelines repeatedly in the last two decades (11–15) and more recently in 2013.
These guidelines are commendable in that they provided useful practical information on evaluation of biomarkers for risk stratification, life-style measures, and strategy of management, including use of the most recent sympathetic renal denervation and baroreceptor stimulation therapy. However, in spite of their publication in multiple journals, and notwithstanding these progresses in treatment, the prevalence of uncontrolled hypertension did not fall, but rather continued to rise. This is clear-cut evidence that guidelines – based approaches are by themselves not sufficient to solve the problem of the poor BP control at the population level. Looking at the latest edition of the ESH/ESC guidelines some reasons for this failure are readily evident. The paper is made of 76 pages, 14 tables, 5 figures, and 735 references (15). This is an overwhelming amount of information that exceeds by far the amount evidence that any busy general practitioner or practicing clinicians dealing with a multitude of patients crowding the waiting rooms of their outpatient clinics can ever possibly read. Recognizing this problem the ESH has prepared a digest version of the European guidelines, but the impact of this “simplified” approach is still to be seen.
As common to other guidelines, the method exploited in writing these guidelines was a “top-down” approach, e.g., from level of evidence and class of recommendation, mainly produced by randomized clinical trials, to practical advices, rather than a problem-oriented “bottom-up” approach. While understandable and obviously scientifically sound, this top-down approach contributed to building up the complexity of the guidelines, and to produce their resulting scant impact in clinical practice.
Hence, a major challenge facing the hypertension community is to conceive and develop novel strategies for continuous medical education in the field of hypertension, having always in mind the final users, e.g., the doctors and the patients.
Additionally, given the complexity of the hypertension field, which requires a multidisciplinary medical formation, with notions spanning from cardiology, to endocrinology, to internal medicine, to nephrology to clinical pharmacology, at least in Europe, there is an urgent need for developing postgraduate training programs in hypertension. To the best of my knowledge the only such programs is the International PhD Program in Arterial Hypertension and Vascular Biology, which was developed at our University in 2001 in conjunction with the Medical Academy of Gdansk and with Charitè University in Berlin and is to be extended to the University of Maastricht next year.
Under Diagnosis and Under Treatment of Secondary Hypertension
Undiagnosed forms of secondary hypertension likely contribute substantively to the on-going epidemics of uncontrolled hypertension. Currently, at referral centers for hypertension, up to 25% of the patients are found to be affected by secondary forms of hypertension, a figure 5- to 10-fold higher than those reported in the major textbooks. The latter reported data mainly based on dated epidemiologic studies that mostly made use of obsolete diagnostic strategies. This apparent increase in prevalence of secondary hypertension means that if a proper diagnostic workup were systematically exploited, an underlying cause of hypertension could be identified in about one patient every four. Hence, a substantial proportion of the patients now mislabeled as “essential hypertension” can thus be either long-term cured or, at least, their BP values can be brought under control, as recently shown to be the case for primary aldosteronism (16).
In spite of the high rate of secondary hypertension, in the most recent ESC/ESH guidelines only a quarter page was devoted to the screening and diagnostic workup of these forms (15), which left practicing physicians with the perception that this is a “niche” problem, while it is altogether evident that it is not. Of little help in this regard was the release of specific guidelines for some endocrine forms of secondary hypertension, including primary aldosteronism (17) and pheochromocytoma (18). These guidelines were prepared by “specialists for specialists.” Therefore, they are perceived to be too complex to be effectively implemented into clinical practice. Accordingly, far too many potentially curable patients are left with a questionable diagnosis of primary (essential) hypertension simply because they were not properly investigated beforehand.
The Problem of Primary Aldosteronism
There is no doubt that primary aldosteronism is the most common endocrine, and probably also the most under diagnosed and under treated, cause of hypertension. As a result of this, many patients, who could be long-term cured (16), are exposed to antihypertensive treatment for their entire lifetime. At the same time, they remain exposed to an excess risk of CV events. A number of reasons can account for this ominous situation. The still diffuse, albeit wrong, perception that primary aldosteronism is exceptionally rare is the first of them. The second entails the fact that, as already mentioned, the diagnostic workup is too complex (17). The development of simplified diagnostic algorithms based on novel, omics-derived biomarkers is therefore, a major challenge for the hypertension community for the years to come. These algorithms could then be used to screen these patients leading to a more targeted treatment with ensuing improved BP control.
The Problem of Atherosclerotic Renovascular Hypertension
Atherosclerotic renal artery stenoses (ARAS) are increasingly found due to aging of the population. They account for about 90% of all renal artery lesions (19) and, through cholesterol emboli, they can lead to cortical infarcts, ischemic nephropathy, and eventually chronic renal failure. Moreover, through activation of the renin–angiotensin–aldosterone system (RAAS) they have other nefarious effects, including inflammation, oxidative stress, endothelial dysfunction, hypertension, thus accelerating widespread cardiovascular disease (20).
Although stenosis is generally held to attain hemodynamic significance only when the luminal narrowing is at least 70%, as compared to the nearby unaffected vessel or, if between 50 and 70%, when the trans-stenotic peak or mean pressure gradient is >20 or >10 mmHg, respectively (21), these threshold values are to be regarded cautiously as discussed elsewhere (22).
Until 1978, when Grüntzig introduced percutaneous transluminal renal angioplasty (PTRA) (23), patients with ARAS were treated medically or surgically. Observational, retrospective, and controlled trials thereafter suggested that PTRA could be beneficial over medical treatment for preserving renal function and improving BP control if followed by stenting [reviewed in Ref. (22)]. However, PTRA plus stenting (PTRAS) could not unequivocally be shown to overcome medical therapy in the few available randomized clinical trials. These trials, however, had limitations in study design, inclusion and exclusion criteria, and treatment options that led to seriously challenge their results and conclusions (24–26).
A recent meta-analysis of seven studies comprising a total of 2155 patients, including the recently reported CORAL Study, showed that compared to baseline, diastolic BP fell more at follow-up in patients in the endovascular than in the medical treatment arm (P = 0.002) (22). Moreover, patients with ARAS receiving endovascular treatment required less anti-antihypertensive drugs at follow-up than those medically treated. Hence, the lower diastolic BP was achieved despite a greater reduction in the mean number of antihypertensive drugs (necessary to control BP (P < 0.001) (22). Identical conclusions were reached by at least three meta-analyses: the first on 527 patients recruited in five prospective multicentre FDA-approved trials (27), the second, a Cochrane meta-analysis, for both diastolic BP and lowered antihypertensive therapy (28), and the third for lowered antihypertensive therapy (29).
Conclusive evidence that PTRAS lowers incident cardiovascular and renal events more than medical therapy in patients with ARAS remains, however, to be provided, likely because all these studies were too small in size and too short in duration to achieve this result. Accordingly, the optimal treatment of ARAS patients remains a highly controversial issue. Currently, this translates in ample variation in clinical practice, even though available guidelines on treatment of ARAS identified some compelling indications to revascularization. These recommendations are based on class I, level of evidence B (Table 3) (30).
Therefore, another major challenge is to plan well-designed clinical research to improve clinical care of the increasing number of elderly patients with atherosclerotic renal artery stenosis and hypertension. The Medical and Endovascular Treatment of Atherosclerotic Renal Artery Stenosis (METRAS) now on-going (METRAS study) 1 (31) can be an example of these.
Gender-Related Differences in BP
There are clear-cut gender-specific differences that contribute to the well-known dimorphism in CV risk between genders: fertile women have lower BP values than age-matched men; the opposite is true after menopause. Notwithstanding this, the mechanisms underlying this BP gender dimorphism are just starting to be unraveled. For example, investigating the gender-related regulation of aldosterone production Caroccia et al recently found a major role for estradiol. The estrogen tonically inhibits aldosterone production by acting through beta-receptor, as when this effect is removed by pharmacological blockade or molecular knocking down of this nuclear receptor, the hormone exerts a potent stimulatory role on aldosterone production acting via the GEPR-1 receptor (32). Establishing whether such mechanisms is important for determining the changes in BP values in women with aging, during the menstrual cycle, or during long-term treatment with estrogen-receptor modulators, which are being prescribed to a multitude of women with estrogen-receptor positive breast cancer, is a key question to be addressed with specific research in the future decade.
Lights and Shadows of Genomics of Hypertension
In the last two decades, impressive efforts and resources have been devoted to the search for the genes causing hypertension. Advancements have been accomplished for some monogenic forms, like Familial Hyperaldosteronism (FH)-1 (GRA), Liddle syndrome, Gordon syndrome, and more recently FH-3 (33–35). Almost invariably the rewarding strategy has been to start from phenotypically well-characterized pedigrees, mostly involving cases of endocrine hypertension, use linkage analysis to pinpoint the underlying genes and mutations. Results of large-scale association studies have not, however, been equally impressive and rewarding even with use of the more sophisticate and expensive genome-wide scanning studies. Even when association of BP with genetic variants were identified, the relative risk of hypertension in the individual carrying the variants was tiny. Consequently, the impact of these studies on clinical practice has been negligible.
A major challenge for the future is therefore to improve the stratification of the hypertensive patients not only for gender, age, and/or BP values but also for traits that can better lend themselves for the genetic analysis.
Pharmacogenomics and Future Perspectives
Pharmacogenomics is attracting increasing attention in scientific circles and in the popular press, mainly because of the promise of personalized Medicine. Short of being able to cure or to prevent hypertension in the majority of the cases, genomics research might eventually fulfill every hypertensiologist’s dream, which is to move from the current “trial-and-error” drug treatment strategy to offering patients a precisely targeted drug at a precisely calibrated dose – and to do so without wreaking adverse effects.
While the vision of uncovering new targets for pharmacologic intervention and of creating novel agents for individualized treatment glimmers tantalizingly distantly on the horizon, much closer to application might be the use of information about how genetic variations affect the efficacy of drugs to guide prescribing decisions for agents currently on the market.
There are sound reasons to predict that pharmacogenomics will eventually succeed in fulfilling this is promise. Technological advances that enable to identify millions of DNA sequence variations swiftly and inexpensively, and to correlate them with phenotypic characteristics, are occurring with a restless rhythm (36). Indeed, it is conceivable that someday soon DNA sequencing will be a routine part of the workup for hypertensive patients, at the very least to identify a patient’s sensitivity to drugs that are likely to produce adverse effects.
The National Institutes of Health consortium on pharmacogenetics research network (PGRN) is collecting information on how genetic variation contributes to differences in drug response among patients and data about specific proteins, genes, and pathways is being integrated into the Pharmacogenetics and Pharmacogenomics Knowledge Base (37). Hence, we might not be a long way from the day when a patient presents a DNA “chip,” a key-chain tag bearing his electronic health record, to a physician and gets a dose of personalized treatment of hypertension.
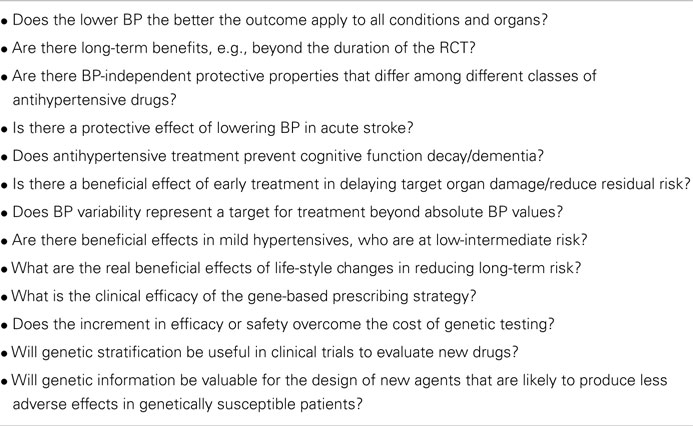
However, a good deal of research still needs to be performed in clinical trails to address multiple questions (Table 3). Among such questions a major place regards the clinical trials to evaluate the clinical efficacy of the gene-based prescribing strategy, and to determine whether the increment in efficacy or safety warrants the cost of genetic testing. Moreover, genetic stratification in clinical trials will be needed to evaluate new drugs – and indeed, genetic information will be invaluable for the design of new agents to serve as alternatives to existing drugs that are likely to produce adverse effects in genetically susceptible patients.
Conflict of Interest Statement
The author declares that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
Acknowledgments
This study was supported by research grants from F.O.R.I.C.A. (www.forica.it).
Footnote
References
1. Effects of treatment on morbidity in hypertension. II. Results in patients with diastolic blood pressure averaging 90 through 114 mm Hg. JAMA (1970) 213(7):1143–52. doi: 10.1001/jama.213.7.1143
2. Five-year findings of the hypertension detection and follow-up program. II. Mortality by race-sex and age. hypertension detection and follow-up program cooperative group. JAMA (1979) 242(23):2572–7. doi:10.1001/jama.242.23.2572
Pubmed Abstract | Pubmed Full Text | CrossRef Full Text | Google Scholar
3. Doyle AE. Cardiovascular morbidity and mortality in mild hypertension: the Australian trial. J Cardiovasc Pharmacol (1985) 7(Suppl 2):S10–3. doi:10.1097/00005344-198507002-00003
Pubmed Abstract | Pubmed Full Text | CrossRef Full Text | Google Scholar
4. MacMahon S, Rodgers A. Blood pressure, antihypertensive treatment and stroke risk. J Hypertens Suppl (1994) 12(10):S5–14.
5. Rodgers A, MacMahon S, Gamble G, Slattery J, Sandercock P, Warlow C. Blood pressure and risk of stroke in patients with cerebrovascular disease. The United Kingdom Transient Ischaemic Attack Collaborative Group. BMJ (1996) 313(7050):147. doi:10.1136/bmj.313.7050.147
6. Law MR, Morris JK, Wald NJ. Use of blood pressure lowering drugs in the prevention of cardiovascular disease: meta-analysis of 147 randomised trials in the context of expectations from prospective epidemiological studies. BMJ (2009) 338:b1665. doi:10.1136/bmj.b1665
Pubmed Abstract | Pubmed Full Text | CrossRef Full Text | Google Scholar
7. Kearney PM, Whelton M, Reynolds K, Whelton PK, He J. Worldwide prevalence of hypertension: a systematic review. J Hypertens (2004) 22(1):11–9. doi:10.1097/00004872-200401000-00003
Pubmed Abstract | Pubmed Full Text | CrossRef Full Text | Google Scholar
8. Lawes CM, Vander Hoorn S, Rodgers A; International Society of Hypertension. Global burden of blood-pressure-related disease, 2001. Lancet (2008) 371(9623):1513–8. doi:10.1016/S0140-6736(08)60655-8
Pubmed Abstract | Pubmed Full Text | CrossRef Full Text | Google Scholar
9. Cuspidi C, Meani S, Fusi V, Valerio C, Catini E, Sala C, et al. Prevalence and correlates of left atrial enlargement in essential hypertension: role of ventricular geometry and the metabolic syndrome: the evaluation of target organ damage in hypertension study. J Hypertens (2005) 23(4):875–82. doi:10.1097/01.hjh.0000163158.14493.23
Pubmed Abstract | Pubmed Full Text | CrossRef Full Text | Google Scholar
10. Daugherty SL, Powers JD, Magid DJ, Tavel HM, Masoudi FA, Margolis KL, et al. Incidence and prognosis of resistant hypertension in hypertensive patients. Circulation (2012) 125(13):1635–42. doi:10.1161/CIRCULATIONAHA.111.068064
Pubmed Abstract | Pubmed Full Text | CrossRef Full Text | Google Scholar
11. European Society of Hypertension-European Society of Cardiology Guidelines Committee. 2003 European society of hypertension-European society of cardiology guidelines for the management of arterial hypertension. J Hypertens (2003) 21(6):1011–53. doi:10.1097/00004872-200306000-00001
12. Mancia G, De Backer G, Dominiczak A, Cifkova R, Fagard R, Germano G, et al. 2007 guidelines for the management of arterial hypertension: the task force for the management of arterial hypertension of the European society of hypertension (ESH) and of the European society of cardiology (ESC). J Hypertens (2007) 25(6):1105–87. doi:10.1097/HJH.0b013e3281fc975a
13. Lurbe E, Cifkova R, Cruickshank JK, Dillon MJ, Ferreira I, Invitti C, et al. Management of high blood pressure in children and adolescents: recommendations of the European society of hypertension. J Hypertens (2009) 27(9):1719–42. doi:10.1097/HJH.0b013e32832f4f6b
14. Mancia G, Laurent S, Agabiti-Rosei E, Ambrosioni E, Burnier M, Caulfield MJ, et al. Reappraisal of European guidelines on hypertension management: a European society of hypertension task force document. Blood Press (2009) 18(6):308–47. doi:10.3109/08037050903450468
15. ESH/ESC Task Force for the Management of Arterial Hypertension. 2013 Practice guidelines for the management of arterial hypertension of the European society of hypertension (ESH) and the European society of cardiology (ESC): ESH/ESC task force for the management of arterial hypertension. J Hypertens (2013) 31(10):1925–38. doi:10.1097/HJH.0b013e328364ca4c
16. Rossi GP, Cesari M, Cuspidi C, Maiolino G, Cicala MV, Bisogni V, et al. Long-term control of arterial hypertension and regression of left ventricular hypertrophy with treatment of primary aldosteronism. Hypertension (2013) 62:62–9. doi:10.1161/HYPERTENSIONAHA.113.01316
Pubmed Abstract | Pubmed Full Text | CrossRef Full Text | Google Scholar
17. Funder JW, Carey RM, Fardella C, Gomez-Sanchez CE, Mantero F, Stowasser M, et al. Case detection, diagnosis, and treatment of patients with primary aldosteronism: an endocrine society clinical practice guideline. J Clin Endocrinol Metab (2008) 93(9):3266–81. doi:10.1210/jc.2008-0104
Pubmed Abstract | Pubmed Full Text | CrossRef Full Text | Google Scholar
18. Lenders JW, Duh QY, Eisenhofer G, Gimenez-Roqueplo AP, Grebe SK, Murad MH, et al. Pheochromocytoma and paraganglioma: an endocrine society clinical practice guideline. J Clin Endocrinol Metab (2014) 99(6):1915–42. doi:10.1210/jc.2014-1498
Pubmed Abstract | Pubmed Full Text | CrossRef Full Text | Google Scholar
19. Krijnen P, van Jaarsveld BC, Steyerberg EW, Man in‘t Veld AJ, Schalekamp MA, Habbema JD. A clinical prediction rule for renal artery stenosis. Ann Intern Med (1998) 129(9):705–11. doi:10.7326/0003-4819-129-9-199811010-00005
Pubmed Abstract | Pubmed Full Text | CrossRef Full Text | Google Scholar
20. Montecucco F, Mach F. Atherosclerosis is an inflammatory disease. Semin Immunopathol (2009) 31(1):1–3. doi:10.1007/s00281-009-0146-7
21. Olin JW. Role of duplex ultrasonography in screening for significant renal artery disease. Urol Clin North Am (1994) 21(2):215–26.
22. Caielli P, Frigo AC, Pengo MF, Rossitto G, Maiolino G, Seccia TM, et al. Treatment of atherosclerotic renovascular hypertension: review of observational studies and a meta-analysis of randomized clinical trials. Nephrol Dial Transplant (2014). doi:10.1093/ndt/gfu072
Pubmed Abstract | Pubmed Full Text | CrossRef Full Text | Google Scholar
23. Gruntzig A. Transluminal dilatation of coronary-artery stenosis. Lancet (1978) 1(8058):263. doi:10.1016/S0140-6736(78)90500-7
24. White CJ. Kiss my astral: one seriously flawed study of renal stenting after another. Catheter Cardiovasc Interv (2010) 75(2):305–7. doi:10.1002/ccd.22416
25. Henry M, Benjelloun A, Henry I, Polydorou A, Hugel M. Renal angioplasty and stenting: is it still indicated after ASTRAL and STAR studies? J Cardiovasc Surg (Torino) (2010) 51(5):701–20.
26. Sarac TP. Influence and critique of the ASTRAL and CORAL Trials. Semin Vasc Surg (2011) 24(3):162–6. doi:10.1053/j.semvascsurg.2011.11.001
Pubmed Abstract | Pubmed Full Text | CrossRef Full Text | Google Scholar
27. Weinberg I, Keyes MJ, Giri J, Rogers KR, Olin JW, White CJ, et al. Blood pressure response to renal artery stenting in 901 patients from five prospective multicenter FDA-approved trials. Catheter Cardiovasc Interv (2014) 83(4):603–9. doi:10.1002/ccd.25263
Pubmed Abstract | Pubmed Full Text | CrossRef Full Text | Google Scholar
28. Jenks S, Yeoh SE, Conway BR. Balloon angioplasty, with and without stenting, versus medical therapy for hypertensive patients with renal artery stenosis. Cochrane Database Syst Rev (2014) 12:CD002944. doi:10.1002/14651858.CD002944.pub2
29. Bavry AA, Kapadia SR, Bhatt DL, Kumbhani DJ. Renal artery revascularization: updated meta-analysis with the CORAL trial. JAMA Intern Med (2014) 174(11):1849–51. doi:10.1001/jamainternmed.2014.4332
30. Hirsch AT, Haskal ZJ, Hertzer NR, Bakal CW, Creager MA, Halperin JL, et al. ACC/AHA 2005 Practice guidelines for the management of patients with peripheral arterial disease (lower extremity, renal, mesenteric, and abdominal aortic): a collaborative report from the American Association for Vascular Surgery/Society for Vascular Surgery, Society for Cardiovascular Angiography and Interventions, Society for Vascular Medicine and Biology, Society of Interventional Radiology, and the ACC/AHA task force on practice guidelines (Writing committee to develop guidelines for the management of patients with peripheral arterial disease): endorsed by the American Association of Cardiovascular and Pulmonary Rehabilitation; National Heart, Lung, and Blood Institute; Society for Vascular Nursing; TransAtlantic Inter-Society Consensus; and Vascular Disease Foundation. Circulation (2006) 113(11):e463–654. doi:10.1161/CIRCULATIONAHA.106.174526
31. Rossi GP, Seccia TM, Gallina V, Muiesan ML, Leoni L, Pengo M, et al. Prospective appraisal of the prevalence of primary aldosteronism in hypertensive patients presenting with atrial flutter or fibrillation (PAPPHY Study): rationale and study design. J Hum Hypertens (2013) 27(3):158–63. doi:10.1038/jhh.2012.21
Pubmed Abstract | Pubmed Full Text | CrossRef Full Text | Google Scholar
32. Caroccia B, Seccia TM, Campos AG, Gioco F, Kuppusamy M, Ceolotto G, et al. GPER-1 and estrogen receptor-beta ligands modulate aldosterone synthesis. Endocrinology (2014) 155(11):4296–304. doi:10.1210/en.2014-1416
Pubmed Abstract | Pubmed Full Text | CrossRef Full Text | Google Scholar
33. Choi M, Scholl UI, Yue P, Bjorklund P, Zhao B, Nelson-Williams C, et al. K+ channel mutations in adrenal aldosterone-producing adenomas and hereditary hypertension. Science (2011) 331(6018):768–72. doi:10.1126/science.1198785
Pubmed Abstract | Pubmed Full Text | CrossRef Full Text | Google Scholar
34. Scholl UI, Nelson-Williams C, Yue P, Grekin R, Wyatt RJ, Dillon MJ, et al. Hypertension with or without adrenal hyperplasia due to different inherited mutations in the potassium channel KCNJ5. Proc Natl Acad Sci U S A (2012) 109(7):2533–8. doi:10.1073/pnas.1121407109
Pubmed Abstract | Pubmed Full Text | CrossRef Full Text | Google Scholar
35. Monticone S, Hattangady NG, Penton D, Isales CM, Edwards MA, Williams TA, et al. A novel Y152C KCNJ5 mutation responsible for familial hyperaldosteronism type III. J Clin Endocrinol Metab (2013) 98(11):E1861–5. doi:10.1210/jc.2013-2428
Pubmed Abstract | Pubmed Full Text | CrossRef Full Text | Google Scholar
Keywords: aldosterone, hyperaldosteronism, heart damage, cardiac dysfunction
Citation: Rossi GP (2015) The challenges of arterial hypertension. Front. Cardiovasc. Med. 2:2. doi: 10.3389/fcvm.2015.00002
Received: 25 November 2014; Accepted: 08 January 2015;
Published online: 03 February 2015.
Edited and reviewed by: Tarek Francis Antonios, St. George’s University of London, UK
Copyright: © 2015 Rossi. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) or licensor are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence:Z2lhbnBhb2xvLnJvc3NpQHVuaXBkLml0
 Gian Paolo Rossi
Gian Paolo Rossi