- 1Ningbo College of Health Sciences, Ningbo, China
- 2Department of Cardiovascular Disease, Ningbo Medical Center Lihuili Hospital, Ningbo, China
Introduction
Atrial fibrillation (AF), which is the most common cardiac arrhythmia, accounts for approximately one-third of hospitalizations for cardiac rhythm disturbances. Each year, more than 5 million people develop AF on this planet, with a significant impact on health care (1). AF is independently associated with significant morbidity and mortality, including a four- to five-fold increased risk for stroke, a three-fold risk for heart failure, a two-fold increased risk for dementia, and a significant risk for premature death (1, 2).
For all patients with AF, the current guidelines report that we think about not only stroke prevention, rate/rhythm control, but also risk factor modification (3, 4). Evidence accumulated in recent years indicates that risk factor management is associated with significant clinical and cost-effectiveness benefits on AF. Many potential modifiable risk factors that contributed to the underlying atrial substrate and, therefore, to AF development have been described, such as hypertension, obstructive sleep apnea, obesity, and diabetes (1, 3, 4). Due to its high prevalence in the general population, hypertension is the most common modifiable risk factor associated with AF (5), and poorly controlled blood pressure (BP) has been associated with elevated AF risk (6, 7). A study showed that hypertension (defined as systolic blood pressure (SBP) >140 mmHg or diastolic blood pressure >90 mmHg or receiving antihypertensive treatment) increased the risk of AF by 56% (8). In a recent large, observational study in close to 1 million Koreans, Kim et al. showed that the incidence of incident AF gradually increased in response to increased BP (9). Even “pre-hypertension” (SBP 130–139 mmHg) was associated with incident AF (9). Besides, hypertension increases the risk of cardiovascular events in patients with AF. In the ROCKET AF trial, a prospective, multicenter, double-blind, randomized controlled trial in patients with non-valvular AF and moderate to high risk of stroke, 90.5% of 14,256 anticoagulated patients had hypertension (10). Vemulapalli et al. found that the risk of stroke or systemic embolism in these patients increased significantly for every 10-mmHg increase in screening SBP (10). In the ARISTOTLE trial of more than 18,000 patients (mean age 70 years) with non-valvular AF, patients with uncontrolled BP at any point during the 2-year trial were associated with a 53% increased risk of ischemic stroke, a 38% increased risk of myocardial infarction, and an 85% increased risk of hemorrhagic stroke (11). These data underscore the importance of intensive antihypertensive therapy to achieve intensive BP control to reduce the risk of new-onset AF and improve the outcome of AF. However, the ideal BP treatment goals for improving the substrate and outcome of AF remain to be defined.
Mechanisms of Hypertension-Related AF
When someone has high BP, the heart needs to pump against that stress hour after hour, day after day. The stress results in left ventricular (LV) hypertrophy, decreased diastolic function with impaired LV filling, with subsequent rising left atrial pressures with left atrial hypertrophy and enlargement, increased atrial fibrosis, and slowing of intra-atrial and interatrial elec-velocities (12, 13). Such a distortion of atrial anatomy and physiology ultimately predisposes to AF. In a study of patients with essential hypertension free of other cardiovascular conditions (n = 2,482), the incidence of AF was 0.46% per year, and age or increased LV mass was the only independent predictors of incident AF during a 5-year follow-up (14). Left atrial pressure also increases with ischemic or valvular heart disease and myopathies that are often associated with systemic hypertension, potentially leading to AF (15). Atrial remodeling induced by hypertension is known as atrial cardiomyopathy, which is described in detail in a recent expert consensus (16).
The abnormal atrial substrate is reversible. A study demonstrated that the renin–angiotensin–aldosterone system blockers could improve atrial electrical and structural remodeling (17). BP reduction following renal sympathetic denervation (RSD) in patients with resistant hypertension was associated with the global atrial conduction improvement (18).
Long-Term Benefit of Goal-Directed BP Reduction in AF
BP control can reduce the occurrence and progression of AF. In patients referring to AF ablation, a previous study demonstrated that poorly treated hypertension almost wholly eliminated the effect of AF ablation (19). Conversely, the ARREST-AF trial showed that aggressive risk factor management, including achieving a target BP of <130/80 mmHg at least 80% of the time, could improve the long-term success of AF ablation (20). Similarly, in a recent randomized trial of 302 patients with hypertension and symptomatic AF randomized to AF ablation with or without RSD, RSD was associated with a significant reduction in BP and AF recurrence at 12 months (21). Besides, in a post hoc analysis of the LIFE study of more than 8,831 patients (mean age 67 years) with LV hypertrophy, compared with placebo (SBP ≥142 mmHg) during a mean of 4.6 years follow-up, antihypertensive treatment targeting SBP <140 mmHg and SBP <130 mmHg was associated with a 24 and 40% lower risk of new-onset AF, respectively (22). The benefit for the achievement of an SBP of ≤ 130 mmHg in the prevention of AF was also evidenced in the prespecified secondary outcome of the Cardio-Sis trial, which demonstrated that new-onset AF occurred in 3.8% of patients in the usual control group (SBP <140 mmHg) and 1.8% of patients in the tight control group (SBP <130 mmHg) (23).
BP control can also improve outcomes in AF patients. Patients with both AF and hypertension had an increased risk of stroke when compared with patients with either condition alone (24). Active treatment lowering mean BP by 7.3/3.4 mmHg was associated with a 34% reduction in stroke (25). In a retrospective study from China, conducted in anticoagulated hypertensive patients with AF, those who achieved a target BP <130/80 mmHg showed a lower incidence of ischemic stroke and a similar risk of major bleeding and intracranial bleeding than patients with higher BP values (26).
What Is the Ideal BP in the Prevention of AF?
The role of hypertension as a modifiable risk factor for AF is established but still incompletely known. In particular, what is the ideal BP treatment target from the perspective of improving the substrate of AF? For this objective, Parcha et al. conducted a post hoc analysis aiming to study the influence of a more intensive reduction in SBP to <120 mmHg on incident AF. A total of 8,549 participants in the SPRINT Trial were eligible for primary analysis (27). The results showed that there was a similar rate of new-onset AF in intensive (target SBP <120 mmHg) and standard (target SBP <140 mmHg) treatment arms (27). That is, a more intensive reduction in SBP to <120 mmHg would not reduce new-onset AF compared with the goal SBP <140 mmHg. This result was consistent with the results of Thomas et al., who conducted a case-controlled study of patients undergoing treatment for hypertension (28). Compared with a reference SBP level of 120–129 mmHg, both SBP ≥150 mmHg and SBP <120 mmHg were at higher risk of incident AF in multivariable logistic regression models (28). The J-curve relationship between BP and new-onset AF was also observed in the control of hypertension in patients undergoing catheter ablation. In a randomized study, Parkash et al. randomly assigned 184 patients with AF and a BP >130/80 mmHg to aggressive BP (target <120/80 mmHg) or standard BP treatment (target <140/90 mmHg) prior to their scheduled AF catheter ablation (29). This study found that targeting SBP to <120 mmHg did not reduce atrial arrhythmia recurrence after catheter ablation of AF during a median follow-up period of 14 months (29).
These findings suggest that a target SBP of 120–129 mmHg may be the ideal SBP in the prevention of AF. However, this aspect was not confirmed in a post hoc analysis of the Women's Health Study, which showed a negative linear association between BP and the risk of incident AF during a median follow-up period of 14 years (6). Their time-updated analyses suggested that the substantial risk of incident AF reductions might be obtained even if SBP was ≤120 mmHg (6). Optimal BP targets to improve the substrate of AF need to be verified in future randomized trials.
What Is the Ideal BP for Improving the Outcome of AF?
Whether stricter BP control provides additional protection in patients with both AF and hypertension is unclear. Kim et al. analyzed data in 298,374 Korean adults with hypertension and non-valvular AF to determine the optimal BP threshold in patients with AF (30). They reported that in comparison with a reference BP level of 120–129/80 mmHg, patients with BP >130/80 mmHg or <120/80 mmHg presented significantly higher risks of major cardiovascular events, including intracranial hemorrhage, ischemic stroke, myocardial infarction, and heart failure requiring hospitalization (30). In the SPRINT trial, ~35% (n = 281) of participants with preexisting AF achieved the BP level of <120/80 mmHg at 3 months (27). Similarly, SBP <120 mmHg was not associated with a lower risk of adverse cardiovascular events compared with those with preexisting AF and BP of ≥120/80 mmHg (27). That implies that a BP of 120–129/80 mmHg might be the optimum BP for patients with AF undergoing hypertension treatment.
BP Treatment Targets in Patients With AF Across Major Hypertension Guidelines
Table 1 compares eight sets of hypertension guidelines last updated between 2016 and 2019 (15, 31–38). With gaps in the evidence base, expert panels disagree on whether guidelines of hypertension should list patients with AF as a specific population and provide a recommendation for BP goal to be achieved in this specific circumstance. The 2019 Japanese Society of Hypertension guidelines recommend that an SBP target of 130 mmHg is effective in preventing the new onset of AF, cardiovascular events (e.g., stroke), and anticoagulation-related bleeding in patients with both AF and hypertension (32). The 2018 European Society of Cardiology and European Society of Hypertension guidelines and 2018 Chinese Guidelines of Hypertension suggest that BP treatment targets in individuals with AF should be at least <140 mmHg, and that <130 should be considered if tolerable (34, 38). The 2018 Korean Society of Hypertension guidelines state that in patients with AF and hypertension, lowering BP can decrease the incidence of fatal bleeding during antithrombotic treatment. However, BP should be maintained above 120/70 mmHg (37). The 2017 American Heart Association/American College of Cardiology (AHA/ACC) guidelines of hypertension recommend BP targets <130/80 mmHg in all hypertensive patients with different recommendation levels according to the risk of cardiovascular disease (15). The Canadian, United Kingdom, and Australia guidelines of hypertension neither list patients with AF as a specific population nor suggest a BP target goal in this situation (31, 33, 35).
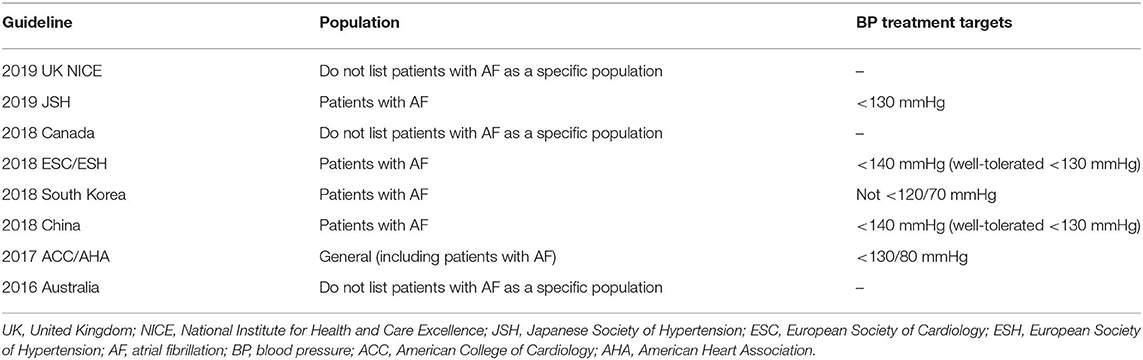
Table 1. Blood pressure treatment targets in patients with atrial fibrillation across major hypertension guidelines.
The Direction of Future Research
Note, though, that new-onset AF was detected by hospital admissions, medical records, and the scheduled study ECGs in the trials mentioned in this paper. The results of intermittent ECG may not always reflect the “true” incidence of new-onset AF. AF can come and go, particularly early in the course of the disease. It is not uncommon for paroxysmal AF to go undetected in intermittent monitoring, which results in a low detection rate of new incident AF cases. Even an ECG taken over a longer period (>24 h) using a Holter monitor does not always lead to a reliable diagnosis of existing AF. In a study of 82 outpatients ≥65 years old with hypertension, diabetes mellitus, and no history of AF or any other cardiovascular, Philippsen et al. found that only 11.8% of patients with asymptomatic AF, which was detected by implantable loop record (ILR), had AF episodes on a 72-h Holter monitoring (39). Another difficult issue is regarding BP measurement in AF. In the presence of AF, variations in ventricular filling time, stroke volume, and contractility may lead to increased beat-to-beat BP variability, which may affect BP estimation using both the auscultatory and oscillometric methods (40). All these would critically impact the result of correlation analyses. An optimal approach to assess the impact of hypertension on AF in large population-based cohort studies remains unclear. Given insufficient sensitivity in detecting sporadic arrhythmias (such as paroxysmal AF) by intermittent monitoring, a continuous rhythm monitoring strategy (such as ILR), although invasive, overcomes many of the limitations of intermittent monitoring in assessing the rate of incident AF and helps evaluate the real effect of hypertension on AF. New mHealth technologies may also provide a promising infrastructure for a more objective and longitudinal assessment of new-onset AF. For this reason, the AF detection function of wearable devices, which receive extensive attention from device manufacturers and cardiologists, has become a focus of research (41). Although current guidelines do not recommend automated BP monitor in the presence of AF (31, 34, 35, 42), the research results about its ability of AF detection during routine BP measurement are promising and worth further studies (43, 44).
Conclusion
Hypertension is a powerful trigger for AF and increases the risk of cardiovascular events in patients with AF. To date, the available evidence supports targeting BP at guideline-recommended levels for primary prevention and management of AF, with J- or U-curve relationship existing between BP and substrate/outcome of AF.
Author Contributions
XM and XX wrote the manuscript, conceptualized the idea, and reviewed and approved the final manuscript for publication. Both authors contributed to the article and approved the submitted version.
Funding
This work was supported in part by the Natural Science Foundation of Ningbo 2017A610200 (XX).
Conflict of Interest
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
References
1. Chung MK, Eckhardt LL, Chen LY, Ahmed HM, Gopinathannair R, Joglar JA, et al. Lifestyle and risk factor modification for reduction of atrial fibrillation: a scientific statement from the american heart association. Circulation. (2020) 141:e750–e72. doi: 10.1161/CIR.0000000000000748
2. Issa ZF, Zipes DP. Clinical Arrhythmology and Electrophysiology: A Companion to Braunwald's Heart Disease. Philadelphia: Elsevier. (2018). p. 434.
3. January CT, Wann LS, Calkins H, Chen LY, Cigarroa JE, Cleveland JC Jr, et al. 2019 AHA/ACC/HRS Focused Update of the 2014 AHA/ACC/HRS guideline for the management of patients with atrial fibrillation: a report of the American college of cardiology/American heart association task force on clinical practice guidelines and the heart rhythm society in collaboration with the society of thoracic surgeons. Circulation. (2019) 140:e125–51. doi: 10.1161/CIR.0000000000000719
4. Kirchhof P, Benussi S, Kotecha D, Ahlsson A, Atar D, Casadei B, et al. 2016 ESC Guidelines for the management of atrial fibrillation developed in collaboration with EACTS. Eur Heart J. (2016) 37:2893–962. doi: 10.5603/KP.2016.0172
5. Huxley RR, Lopez FL, Folsom AR, Agarwal SK, Loehr LR, Soliman EZ, et al. Absolute and attributable risks of atrial fibrillation in relation to optimal and borderline risk factors: the Atherosclerosis Risk in Communities (ARIC) study. Circulation. (2011) 123:1501–8. doi: 10.1161/CIRCULATIONAHA.110.009035
6. Conen D, Tedrow UB, Koplan BA, Glynn RJ, Buring JE, Albert CM. Influence of systolic and diastolic blood pressure on the risk of incident atrial fibrillation in women. Circulation. (2009) 119:2146–52. doi: 10.1161/CIRCULATIONAHA.108.830042
7. Lau DH, Nattel S, Kalman JM, Sanders P. Modifiable risk factors and atrial fibrillation. Circulation. (2017) 136:583–96. doi: 10.1161/CIRCULATIONAHA.116.023163
8. Toren K, Schioler L, Soderberg M, Giang KW, Rosengren A. The association between job strain and atrial fibrillation in Swedish men. Occup Environ Med. (2015) 72:177–80. doi: 10.1136/oemed-2014-102256
9. Kim YG, Han KD, Choi JI, Yung Boo K, Kim DY, Oh SK, et al. Impact of the duration and degree of hypertension and body weight on new-onset atrial fibrillation: a nationwide population-based study. Hypertension. (2019) 74:e45–e51. doi: 10.1161/HYPERTENSIONAHA.119.13672
10. Vemulapalli S, Hellkamp AS, Jones WS, Piccini JP, Mahaffey KW, Becker RC, et al. Blood pressure control and stroke or bleeding risk in anticoagulated patients with atrial fibrillation: results from the rocket AF trial. Am Heart J. (2016) 178:74–84. doi: 10.1016/j.ahj.2016.05.001
11. Rao MP, Halvorsen S, Wojdyla D, Thomas L, Alexander JH, Hylek EM, et al. Blood pressure control and risk of stroke or systemic embolism in patients with atrial fibrillation: results from the apixaban for reduction in stroke and other thromboembolic events in atrial fibrillation (aristotle) trial. J Am Heart Assoc. (2015) 4:e002015. doi: 10.1161/JAHA.115.002015
12. Verdecchia P, Angeli F, Reboldi G. Hypertension and atrial fibrillation: doubts and certainties from basic and clinical studies. Circ Res. (2018) 122:352–68. doi: 10.1161/CIRCRESAHA.117.311402
13. Medi C, Kalman JM, Spence SJ, Teh AW, Lee G, Bader I, et al. Atrial electrical and structural changes associated with longstanding hypertension in humans: implications for the substrate for atrial fibrillation. J Cardiovasc Electrophysiol. (2011) 22:1317–24. doi: 10.1111/j.1540-8167.2011.02125.x
14. Verdecchia P, Reboldi G, Gattobigio R, Bentivoglio M, Borgioni C, Angeli F, et al. Atrial fibrillation in hypertension: predictors and outcome. Hypertension. (2003) 41:218–23. doi: 10.1161/01.HYP.0000052830.02773.E4
15. Whelton PK, Carey RM, Aronow WS, Casey DE Jr, Collins KJ, Dennison Himmelfarb C, et al. 2017 ACC/AHA/AAPA/ABC/ACPM/AGS/APhA/ASH/ASPC/NMA/PCNA guideline for the prevention, detection, evaluation, and management of high blood pressure in adults: a report of the american college of cardiology/american heart association task force on clinical practice guidelines. Hypertension. (2018) 71:e13–e115. doi: 10.1161/HYP.0000000000000076
16. Goette A, Kalman JM, Aguinaga L, Akar J, Cabrera JA, Chen SA, et al. EHRA/HRS/APHRS/SOLAECE expert consensus on atrial cardiomyopathies: definition, characterization, clinical implication. Heart Rhythm. (2017) 14:e3–e40. doi: 10.1016/j.hrthm.2016.05.028
17. Matsuyama N, Tsutsumi T, Kubota N, Nakajima T, Suzuki H, Takeyama Y. Direct action of an angiotensin II receptor blocker on angiotensin II-induced left atrial conduction delay in spontaneously hypertensive rats. Hypertens Res. (2009) 32:721–6. doi: 10.1038/hr.2009.89
18. McLellan AJ, Schlaich MP, Taylor AJ, Prabhu S, Hering D, Hammond L, et al. Reverse cardiac remodeling after renal denervation: atrial electrophysiologic and structural changes associated with blood pressure lowering. Heart Rhythm. (2015) 12:982–90. doi: 10.1016/j.hrthm.2015.01.039
19. Mohanty S, Mohanty P, DI Biase L, Bai R, Trivedi C, Santangeli P, et al. Long-term outcome of catheter ablation in atrial fibrillation patients with coexistent metabolic syndrome and obstructive sleep apnea: impact of repeat procedures versus lifestyle changes. J Cardiovasc Electrophysiol. (2014) 25:930–8. doi: 10.1111/jce.12468
20. Pathak RK, Middeldorp ME, Lau DH, Mehta AB, Mahajan R, Twomey D, et al. Aggressive risk factor reduction study for atrial fibrillation and implications for the outcome of ablation: the ARREST-AF cohort study. J Am Coll Cardiol. (2014) 64:2222–31. doi: 10.1016/j.jacc.2014.09.028
21. Steinberg JS, Shabanov V, Ponomarev D, Losik D, Ivanickiy E, E. Kropotkin, et al. Effect of renal denervation and catheter ablation vs catheter ablation alone on atrial fibrillation recurrence among patients with paroxysmal atrial fibrillation and hypertension: the eradicate-af randomized clinical trial. JAMA. (2020) 323:248–55. doi: 10.1001/jama.2019.21187
22. Okin PM, Hille DA, Larstorp AC, Wachtell K, Kjeldsen SE, Dahlöf B, et al. Effect of lower on-treatment systolic blood pressure on the risk of atrial fibrillation in hypertensive patients. Hypertension. (2015) 66:368–73. doi: 10.1161/HYPERTENSIONAHA.115.05728
23. Verdecchia P, Staessen JA, Angeli F, de Simone G, Achilli A, Ganau A, et al. Usual versus tight control of systolic blood pressure in non-diabetic patients with hypertension (Cardio-Sis): an open-label randomised trial. Lancet. (2009) 374:525–33. doi: 10.1016/S0140-6736(09)61340-4
24. Lip GY, Nieuwlaat R, Pisters R, Lane DA, Crijns HJ. Refining clinical risk stratification for predicting stroke and thromboembolism in atrial fibrillation using a novel risk factor-based approach: the euro heart survey on atrial fibrillation. Chest. (2010) 137:263–72. doi: 10.1378/chest.09-1584
25. Arima H, Hart RG, Colman S, Chalmers J, Anderson C, Rodgers A, et al. Perindopril-based blood pressure-lowering reduces major vascular events in patients with atrial fibrillation and prior stroke or transient ischemic attack. Stroke. (2005) 36:2164–9. doi: 10.1161/01.STR.0000181115.59173.42
26. Ho LY, Siu CW, Yue WS, Lau CP, Lip GY, Tse HF. Safety and efficacy of oral anticoagulation therapy in Chinese patients with concomitant atrial fibrillation and hypertension. J Hum Hyperten. (2011) 25:304–10. doi: 10.1038/jhh.2010.57
27. Parcha V, Patel N, Kalra R, Kim J, Gutierrez OM, Arora G, et al. Incidence and implications of atrial fibrillation/flutter in hypertension: insights from the sprint trial. Hypertension. (2020) 75:1483–90. doi: 10.1161/HYPERTENSIONAHA.120.14690
28. Thomas MC, Dublin S, Kaplan RC, Glazer NL, Lumley T, Longstreth WT, et al. Blood pressure control and risk of incident atrial fibrillation. Am J Hyperten. (2008) 21:1111–6. doi: 10.1038/ajh.2008.248
29. Parkash R, Wells GA, Sapp JL, Healey JS, Tardif JC, Greiss I, et al. Effect of aggressive blood pressure control on the recurrence of atrial fibrillation after catheter ablation: a randomized, open-label clinical trial (SMAC-AF [substrate modification with aggressive blood pressure control]). Circulation. (2017) 135:1788–98. doi: 10.1161/CIRCULATIONAHA.116.026230
30. Kim D, Yang PS, Kim TH, Jang E, Shin H, Kim HY, et al. Ideal blood pressure in patients with atrial fibrillation. J Am Coll Cardiol. (2018) 72:1233–45. doi: 10.1016/j.jacc.2018.05.076
31. National Guideline Centre (UK). Hypertension in Adults: Diagnosis and Management. London: National Institute for Health and Care Excellence (2019). p. 41.
32. Umemura S, Arima H, Arima S, Asayama K, Dohi Y, Hirooka Y, et al. The japanese society of hypertension guidelines for the management of hypertension (JSH 2019). Hyperten Res. (2019) 42:1235–481. doi: 10.1038/s41440-019-0284-9
33. Nerenberg KA, Zarnke KB, Leung AA, Dasgupta K, Butalia S, McBrien K, et al. Hypertension Canada's 2018 guidelines for diagnosis, risk assessment, prevention, and treatment of hypertension in adults and children. Can J Cardiol. (2018) 34:506–25. doi: 10.1016/j.cjca.2018.02.022
34. Williams B, Mancia G, Spiering W, Agabiti Rosei E, Azizi M, Burnier M, et al. 2018 ESC/ESH Guidelines for the management of arterial hypertension. Eur Heart J. (2018) 39:3021–104. doi: 10.1093/eurheartj/ehy339
35. Gabb GM, Mangoni AA, Anderson CS, Cowley D, Dowden JS, Golledge J, et al. Guideline for the diagnosis and management of hypertension in adults - 2016. Med J Aust. (2016) 205:85–9. doi: 10.5694/mja16.00526
36. Lee HY, Shin J, Kim GH, Park S, Ihm SH, Kim HC, et al. 2018 Korean Society of Hypertension Guidelines for the management of hypertension: part II-diagnosis and treatment of hypertension. Clin Hyperten. (2019) 25:20. doi: 10.1186/s40885-019-0124-x
37. Kim KI, Ihm SH, Kim GH, Kim HC, Kim JH, Lee HY, et al. 2018 Korean society of hypertension guidelines for the management of hypertension: part III-hypertension in special situations. Clin Hyperten. (2019) 25:19. doi: 10.1186/s40885-019-0123-y
38. Joint Committee for Guideline Revision. 2018 Chinese guidelines for prevention and treatment of hypertension-a report of the revision committee of chinese guidelines for prevention and treatment of hypertension. J Geriatr Cardiol. (2019) 16:182–241. doi: 10.11909/j.issn.1671-5411.2019.03.014
39. Philippsen TJ, Christensen LS, Hansen MG, Dahl JS, Brandes A. Detection of subclinical atrial fibrillation in high-risk patients using an insertable cardiac monitor. JACC. Clin Electrophysiol. (2017) 3:1557–564. doi: 10.1016/j.jacep.2017.06.020
40. Cohen DL, Townsend RR. Blood pressure in patients with atrial fibrillation: part 1–measurement. J Clin Hyperten. (2017) 19:98–9. doi: 10.1111/jch.12905
41. Perez MV, Mahaffey KW, Hedlin H, Rumsfeld JS, Garcia A, Ferris T, et al. Large-scale assessment of a smartwatch to identify atrial fibrillation. N Engl J Med. (2019) 381:1909–17. doi: 10.1056/NEJMoa1901183
42. Clark CE, McDonagh STJ, McManus RJ. Accuracy of automated blood pressure measurements in the presence of atrial fibrillation: systematic review and meta-analysis. J Hum Hyperten. (2019) 33:352–64. doi: 10.1038/s41371-018-0153-z
43. Omboni S, Verberk WJ. Opportunistic screening of atrial fibrillation by automatic blood pressure measurement in the community. BMJ Open. (2016) 6:e010745. doi: 10.1136/bmjopen-2015-010745
Keywords: hypertension, atrial fibrillation, risk factor, guideline, cardiovascular outcome
Citation: Meng X and Xu X (2020) What Is the Ideal Blood Pressure Treatment Target for Primary Prevention and Management of Atrial Fibrillation? Front. Cardiovasc. Med. 7:586183. doi: 10.3389/fcvm.2020.586183
Received: 22 July 2020; Accepted: 26 October 2020;
Published: 27 November 2020.
Edited by:
Indranill Basu-Ray, Memphis VA Medical Center (VHA), United StatesReviewed by:
Stefano Omboni, Istituto Italiano di Telemedicina, ItalyCopyright © 2020 Meng and Xu. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Xiaoyong Xu, Z2xtZmUxQGdtYWlsLmNvbQ==
 Xianghong Meng
Xianghong Meng Xiaoyong Xu
Xiaoyong Xu