- 1Department of Critical Care Medicine, Kaohsiung Veterans General Hospital, Kaohsiung, Taiwan
- 2Section of Cardiology, Department of Internal Medicine, Kaohsiung Veterans General Hospital, Kaohsiung, Taiwan
- 3School of Medicine, National Yang-Ming University, Taipei, Taiwan
- 4Department of Physical Therapy, Fooyin University, Kaohsiung, Taiwan
- 5Department of Emergency Medicine, Taipei Veterans General Hospital, Taipei, Taiwan
- 6Institute of Emergency and Critical Care Medicine, College of Medicine, National Yang-Ming University, Taipei, Taiwan
- 7Joint Commission of Taiwan, New Taipei City, Taiwan
Background and Purpose: In-hospital cardiac arrest (IHCA) has high mortality rate, which needs more research. This multi-center study aims to evaluate potential risk factors for mortality in patients after IHCA.
Methods: Data for this study retrospectively enrolled IHCA patients from 14 regional hospitals, two district hospitals, and five medical centers between 2013 June and 2018 December. The study enrolled 5,306 patients and there were 2,871 patients in subgroup of intensive care unit (ICU) and emergency room (ER), and 1,894 patients in subgroup of general wards.
Results: As for overall IHCA patients, odds ratio (OR) for mortality was higher in older patients (OR = 1.69; 95% CI:1.33–2.14), those treated with ventilator (OR = 1.79; 95% CI:1.36–2.38) and vasoactive agents (OR = 1.88; 95% CI:1.45–2.46). Whereas, better survival was reported in IHCA patients with initial rhythm as ventricular tachycardia (OR = 0.32; 95% CI: 0.21–0.50) and ventricular fibrillation (OR = 0.26; 95% CI: 0.16–0.42). With regard to ICU and ER subgroup, there was no mortality difference among different nursing shifts, whereas for patients in general wards, overnight shift (OR = 1.83; 95% CI: 1.07–3.11) leads to poor outcome.
Conclusion: For IHCA patients, old age, receiving ventilator support and vasoactive agents reported poor survival. Overnight shift had poor survival for IHCA patients in general wards, despite no significance in overall and ICU/ER subgroups.
Introduction
In-hospital cardiac arrest (IHCA) has high mortality rate (1). The majority of data are derived from the American Heart Association's Get With The Guidelines-Resuscitation (GWTG-R) registry, which reported 9 to 10 IHCA cases per 1,000 admissions from 2008 to 2017 (2, 3).
Despite successful resuscitation, only few resuscitated patients have good neurologic conditions at discharge (4). Targeted temperature management (TTM) after cardiac arrest remains the primary neuroprotective approach following cardiac arrest (5, 6).
Compared to other critical cardiovascular conditions, including stroke, myocardial infarction, and OHCA, IHCA has received little attention (1). Thus, this study was conducted to evaluate the potential risk factors for mortality in patients after IHCA.
Methods
This cross-sectional study analyzed the IHCA data set of The Taiwan Clinical Performance Indicator (TCPI) system, which was founded by the Joint Commission of Taiwan (JCT) in 2011. The Human Research Committee of Kaohsiung Veterans General Hospital approved this study.
Data Source and Study Population
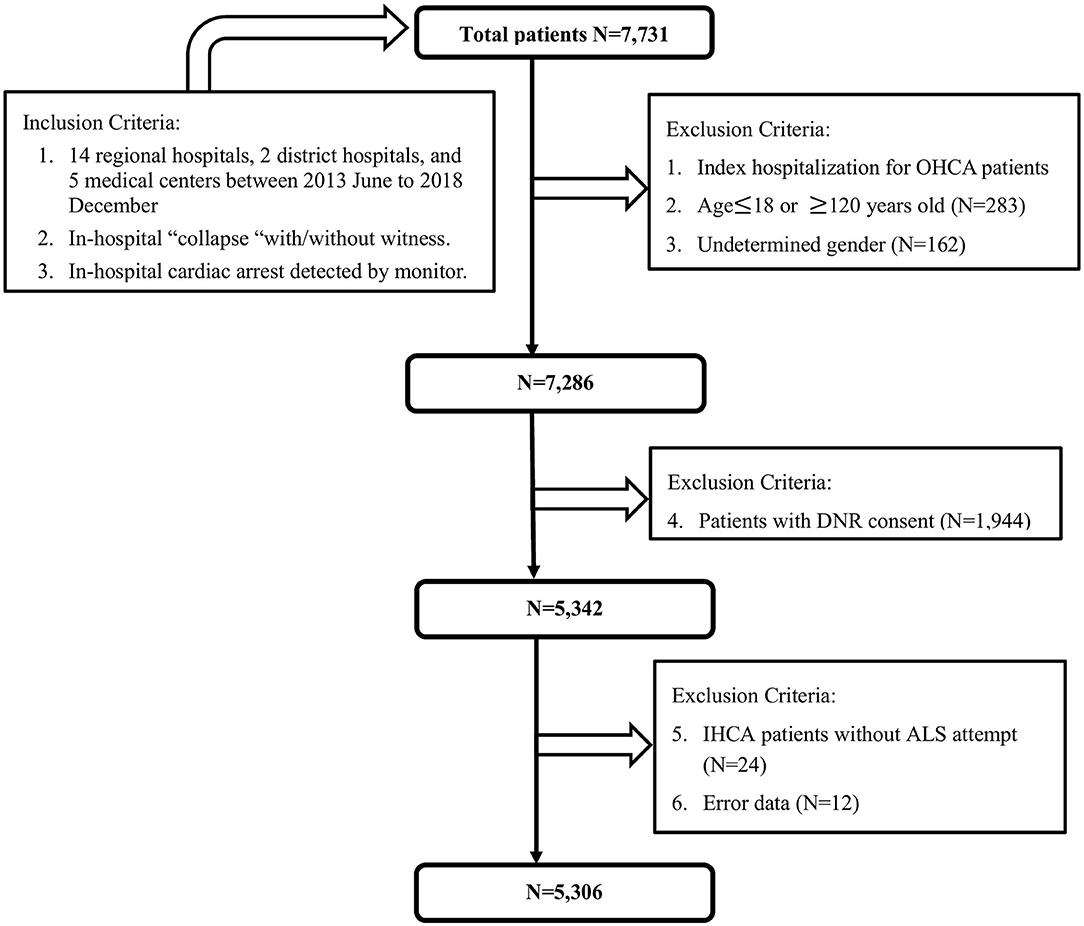
This registered multicenter study retrospectively enrolled IHCA patients from 14 regional hospitals, two district hospitals, and five medical centers between June 2013 and December 2018. A total of 7,731 cases were included. We excluded patients with undetermined sex, age younger than 18 years, with a do-not-resuscitate (DNR) order, and those not receiving resuscitation. JCT staff supervised this registry and checked the numbers of IHCA patients to confirm that all IHCA patients in enrolled hospitals were included in this study. Finally, 5,306 patients were included in the analysis (Figure 1). The IHCA event locations were collected including intensive care unit (including coronary care units), emergent department, ordinary ward, examination room, postoperative recovery room, outpatient department, operating theater or coronary angiography laboratory and others. Total 54.1% of IHCA occurred in ICU/ER and 35.7% of IHCA occurred in general ward. Only 10.2% of IHCA occurred in examination room, postoperative recovery room, outpatient department, operating theater or coronary angiography laboratory, etc. Finally, there were 2,871 and 1,894 patients in the ICU/ER subgroup and general ward subgroup, respectively. Fetal arrhythmia was defined brady-arrhythmias or tachy-arrhythmias leading to sudden cardiac death (7). Ventricular tachycardia (VT) and ventricular fibrillation (VF) are kinds of fetal arrhythmia.
Indications for TTM, Ventilator and Vasoactive Therapy
TTM has been recommended for post-resuscitation care of comatose patients after CA event (6, 8). Intubation and ventilator therapy are indicated for cardiac arrest patients not responsive, ineffective or not possible to bag-mask ventilation, and were needed for protected airway (9). The use of the vasopressors were recommended for the resuscitation of cardiac arrest patients in current guideline (10).
Statistical Analysis
For data analysis, SAS software version 9.4 (SAS Institute, Inc., Cary, NC) was used. Percentile values were used to express categorical data, analyzed using the chi-square test. Multivariable logistic regression model was used to calculate odds ratio (OR) and associated 95% confidence intervals (95% CIs) for significant variables, including sex, age, hospital level, direct cause, and initial rhythm. A P-value <0.05 was considered statistically significant.
Results
The patients' basic characteristics are listed in Table 1. The majority of the initially detected rhythms were pulseless electrical activity (PEA) (41.6%) and asystole (27.5%), and the leading cause of IHCA was fatal arrythmia (35.7%).
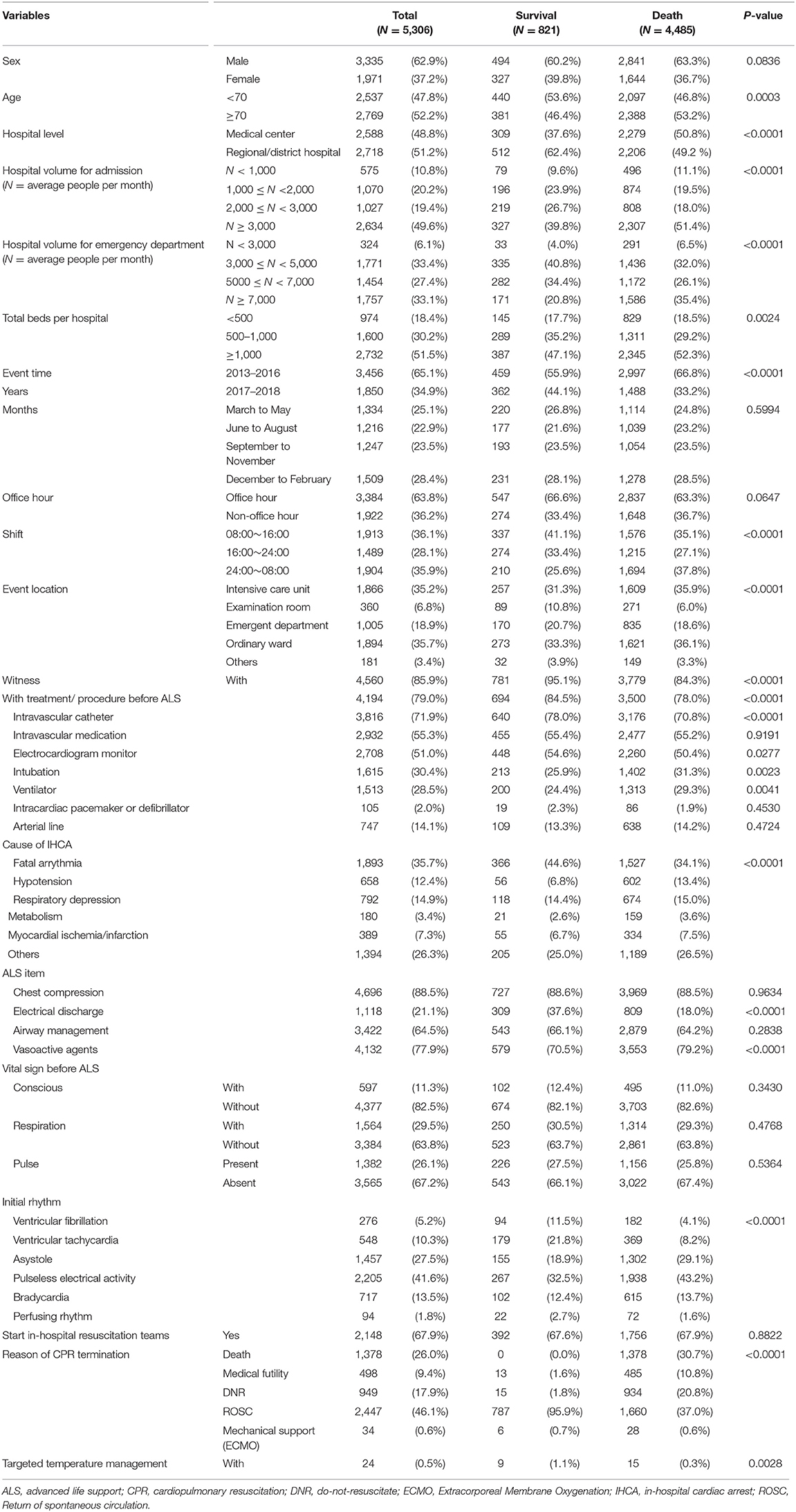
Table 1. Basic characteristics of in-hospital cardiac arrest patients in a multicenter cohort study.
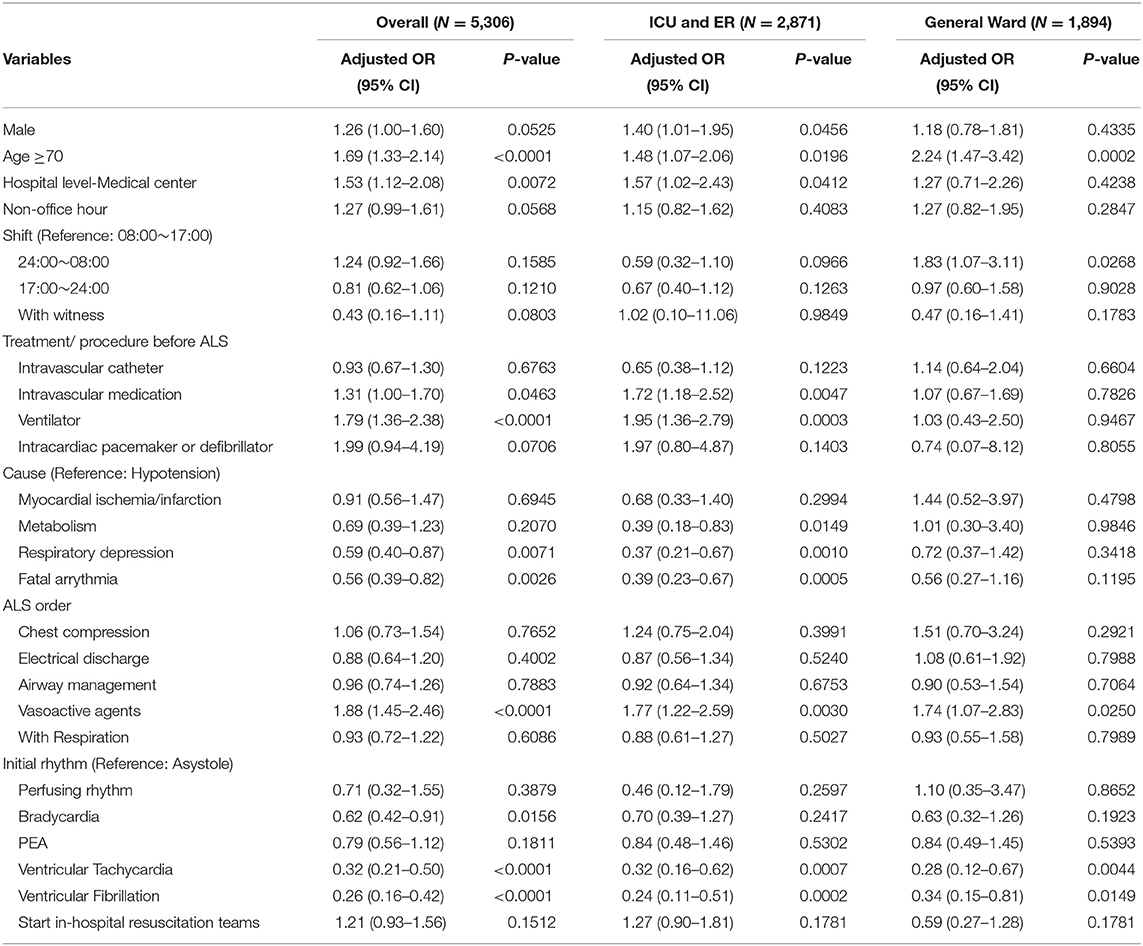
Survival ratios of IHCA patients according to basic characteristics are shown in Figure 2. There was no sex difference in survival ratios (Figure 2A). Factors for poor survival included old age (Figure 2B), medical center (Figure 2C), large hospital volume for admission with >3,000 patients per month on average (Figure 2D), and total beds >1,000 (Figure 2F). Events occurring between 24:00 and 08:00 had poor outcomes (Figure 2J). Events occurring at the ICU showed poor outcomes, whereas events at the examination room showed better outcomes (Figure 2K). Moreover, better survival was reported in patients with a witness during the attack (Figure 2L).
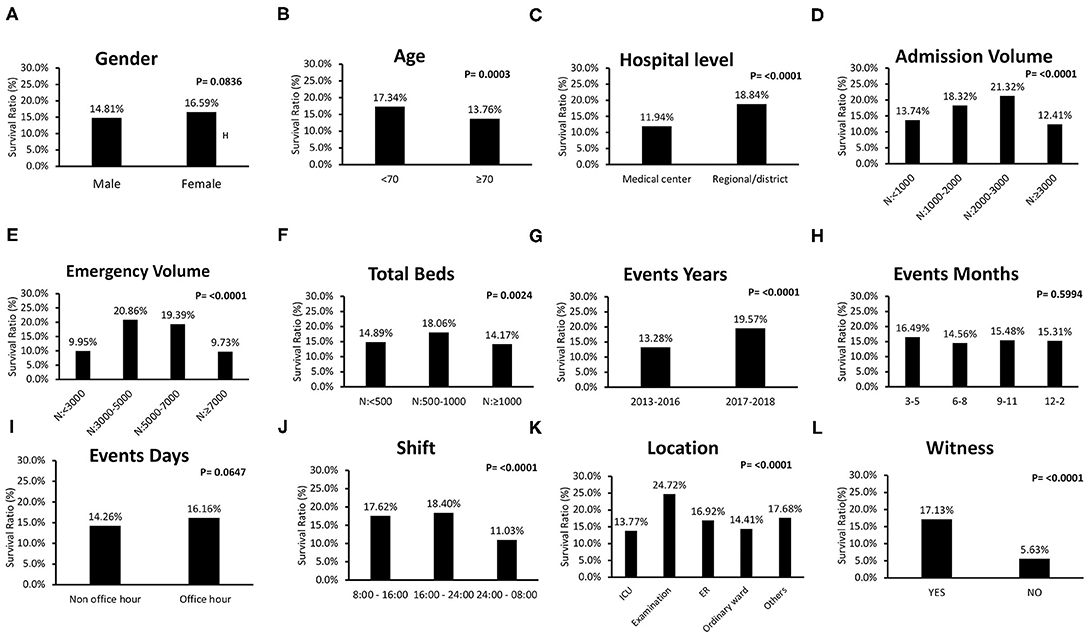
Figure 2. Comparisons of survival rate of individual clinical characteristic of in-hospital-cardiac-arrest (IHCA) patients. (A) There was no sex difference in survival (male: 14.8%; female: 16.6%, P = 0.0836). (B–F) Factors for poor survival included old age (<70 years: 17.3%; ≥70 years: 13.8%, P = 0.0003), medical center (medical center: 11.9%; regional/district hospital: 18.8%, P < 0.0001), large hospital volume for admission with >3,000 patients per month on average, large hospital volume for emergency room with >7,000 patients per month on average, and total beds >1,000. (G) Events occurring in the recent year had better outcomes. (H) There was no difference in IHCA outcome among different months. (I) There was no difference in IHCA outcome between events occurring during office and non-office hours. (J) Events occurring between 24:00 and 08:00 showed poor outcomes. (K) Event location at intensive care unit (ICU) showed poor outcomes, whereas, event location at examination room presented better outcomes (ICU: 13.8%; examination room: 24.7%; emergent department: 16.9%; ordinary ward: 14.4%; others: 17.7%, P < 0.000 1). (L) Better survival was reported in patients with a witness (with: 17.1% without: 5.6%, P < 0.0001).
Figure 3 includes survival ratios of treatment or procedure before ALS and ALS-associated items. The survival ratio with different causes of IHCA and other managements are reported in Figure 4. Fatal arrhythmia as the cause of IHCA had better survival (Figure 4A). Patients who underwent TTM had better outcomes (Figure 4B). Initially-detected ventricular fibrillation (VF) was associated with better survival ratios (Figure 4D). Moreover, there was no difference in survival between patients with and without in-hospital resuscitation teams (Figure 4C).
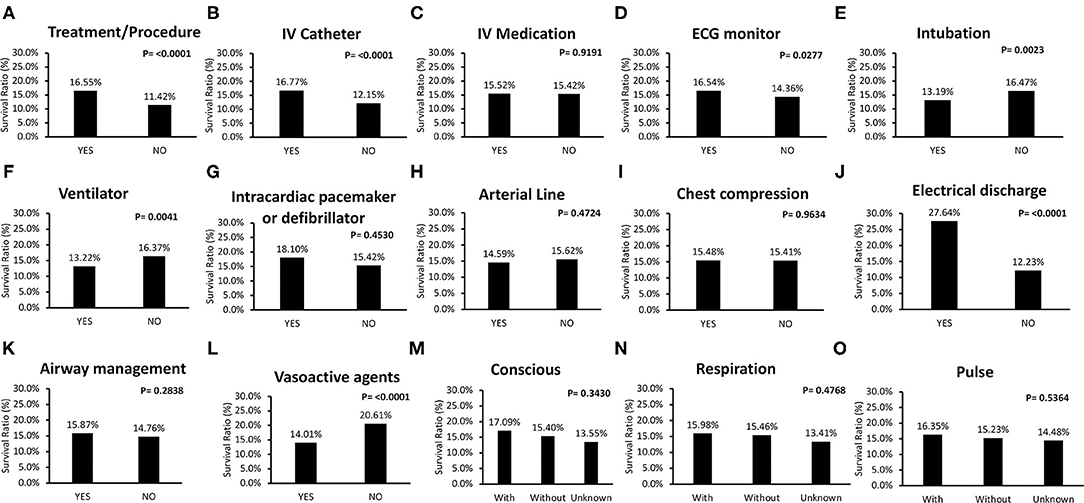
Figure 3. Comparisons of survival rate of treatment or procedure before advanced life support (ALS) and ALS associated items for in-hospital-cardiac-arrest (IHCA) patients. (A,B,D–F) Treatment or procedure contributed to better outcome, including intravascular (IV) catheter, electrocardiogram (ECG) monitor, intubation, and ventilator. (C) IV medication had no contribution to survival. (G,H). There were no survival differences for IHCA patients to have intracardiac pacemaker or defibrillator, and arterial line before ALS. (I,K) Regarding ALS order, chest compression and airway management did not affect overall IHCA survival rate. (J,L) Patients received electrical discharge (with electrical discharge: 27.6%; without electrical discharge: 12.2%, P < 0.0001) and not be prescribed with vasoactive agents also presented better outcome (with vasoactive agents: 14.0%; without vasoactive agents: 20.6%, P < 0.0001) had better survival. (M–O) Vital sign before ALS, such as conscious, reparation, and pulse did not affect overall survival.
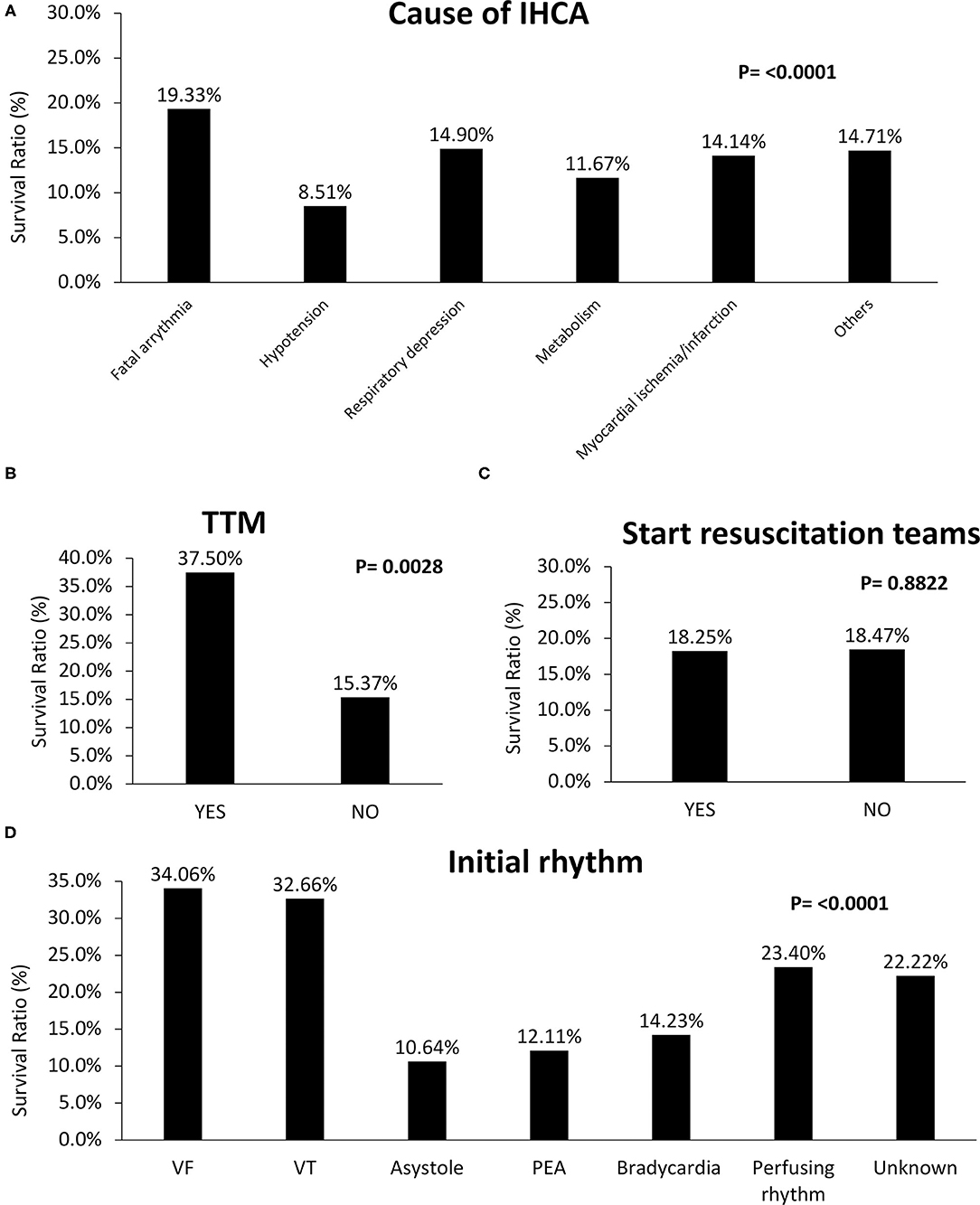
Figure 4. Comparisons of survival rate of different causes and initial rhythm of in-hospital-cardiac-arrest (IHCA) and other specific managements. (A) Fatal arrhythmia as the cause of IHCA had better survival. (B) Patients who underwent TTM (with: 37.5%; without TTM: 15.4%, P = 0.0028) had better outcomes. (C) Starting in-hospital resuscitation teams had no benefit on survival (with: 18.3%; without: 18.5%, P = 0.8822). (D) Initially detected ventricular fibrillation (VF) revealed better survival rates (VF: 34.1%; ventricular tachycardia (VT): 32.7%; asystole: 10.6%; PEA: 12.1%; bradycardia: 14.2%; perfusing rhythm: 23.4%; unknown: 22.2%, P < 0.0001).
The basic characteristics of the general ward and ICU/ER subgroups are reported in Table 2. The general ward subgroup had more patients aged >70 years and more IHCA events occurring during overnight shifts. The ICU/ER subgroup had more IHCA events occurring during office hours, more witnessed IHCA patients, and more patients receiving treatment or procedure before ALS. Moreover, the proportion of starting in-hospital resuscitation teams was higher in the general subgroup.
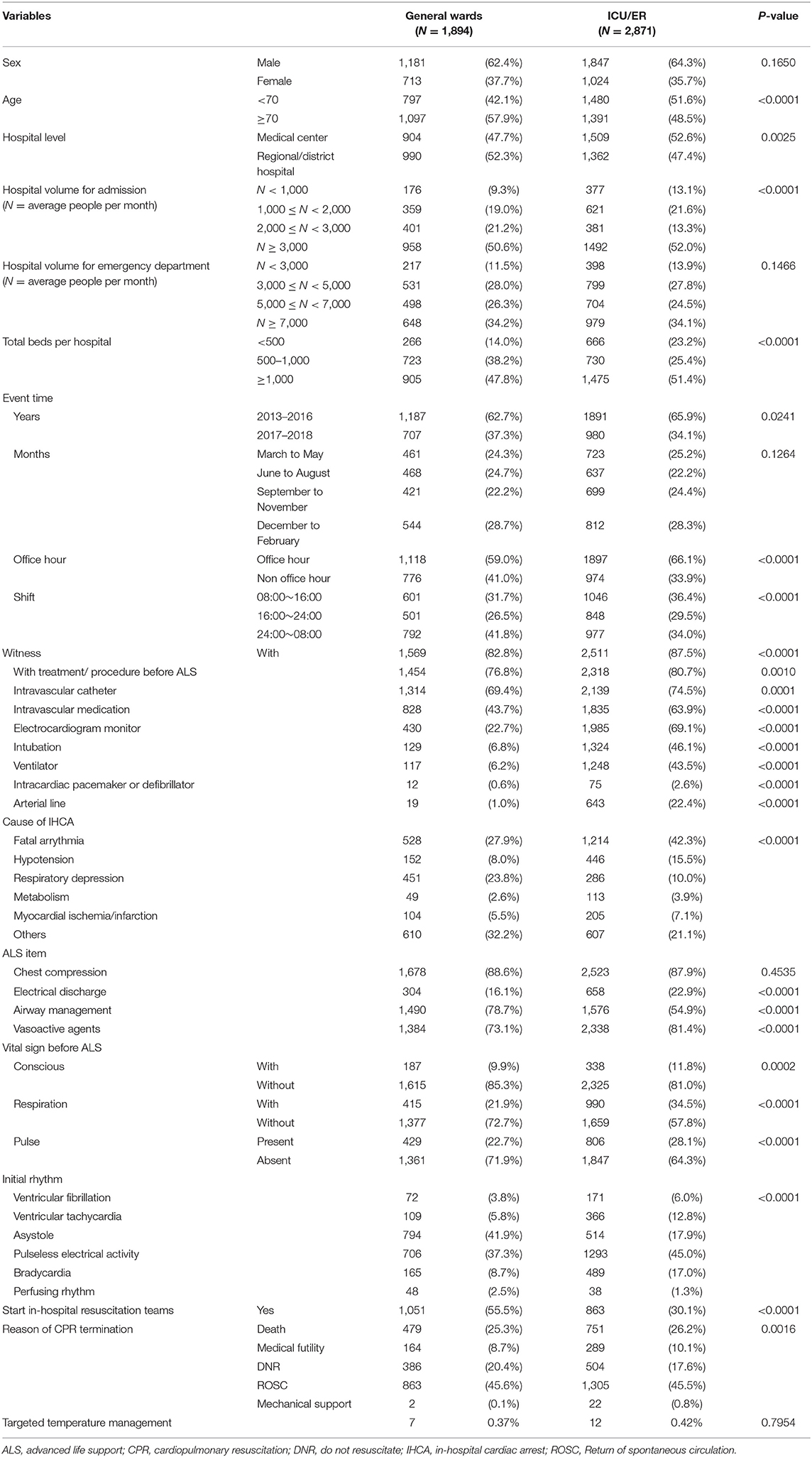
Table 2. Basic characteristics of in-hospital cardiac arrest patients in subgroups of general wards and intensive care unit/emergency room.
In the multivariable logistic regression model, OR for mortality was higher in older patients, those receiving ventilator support before ALS, and those receiving vasoactive agents during ALS in the overall IHCA patient group (Table 3). On the contrary, patients with respiratory depression as the cause of IHCA, rather than hypotension showed better outcomes. In the ICU/ER subgroup (Table 3), better survival was reported in patients with respiratory depression rather than hypotension as the cause of IHCA, and patients with initially detected VT and VF had better outcome. For the general ward subgroup, patients with older age and attacks occurring between 24:00 and 08:00 (compared to 08:00–17:00) had poor outcomes. Moreover, initial rhythms of VT and VF were shown to reduce the mortality risk in IHCA patients in overall, ICU/ER and general ward subgroups.
Discussion
This multicenter cohort study analyzed the association between IHCA patients and healthcare-related risk factors. Compared to the previous GWTG-R cohort data from the United States (U.S.) involving IHCA patients with a mean age of 66 years, our patients' mean age was 68 years and 62.9% of our patients were male (Table 1), whereas in the GWTG-R, 58% were male. The presenting rhythm in the GWTG-R was most often non-shockable (81%), which was comparable to our study finding showing that 82.6% of the patients had a non-shockable rhythm (1, 2). Survival to hospital discharge was ~25% in GWTG-R, whereas in our study, this was 15.5% (2). Previous study had a 7-year follow-up between 2000 and 2007, with 507 medical/surgical participating hospitals, and total 86,748 IHCA patients. It indicated lower survival during night hours in comparison with event occurred during day/evening hours (11). In comparison with this large sample size, our study followed 6 years, and had relatively small sample size with only 7,731 cases, however, our study analyzed the differences between survival and death subgroups to get information about the potential risk factors for IHCA mortality, in addition to the focus on the association between survival and event time. Preceding evidence indicated a 3% increase in in-hospital survival rates among IHCA patients between 2000 and 2004 (12). Moreover, advanced cardiac life support (ACLS) training and adherence contributed to better outcome of IHCA patients (13). Whereas, in comparison to previous study (11), rate of survival to discharge in overnight shift was not improved (14.7 vs. 11.03%), which might be attributed to hospital level and disease severity.
Old Age Is a Predictor of Worse Overall Outcome
Age is one of the predictors of the Cardiac Arrest Survival Post Resuscitation In-hospital Score (CASPRI) score. A previous study indicated that increased age is associated with poor survival, especially for patients aged >70 years (1, 14). One single-center analysis of IHCA outcomes indicated that younger patients were more likely to survive the initial IHCA (15), which supported our study finding that age ≥70 years (OR= 1.69; 95% CI:1.33–2.14) (Table 3) was a predictor of worse overall outcome.
Overnight Shift in General Wards Increased Mortality Risk of IHCA Patients
The patient-to-nurse ratio should be <9:1 in medical centers, 12:1 in regional hospitals, and 15:1 in district hospitals, according to Taiwan's local medical law standards. However, in Taiwan, the actual patient-to-nurse ratio is approximately 10–11:1 in general wards for day shifts and 20–30:1 for night shifts. This workload is five times higher than that of institutions in Europe or the U.S (16, 17).
Previous research reported 31% mortality for a 8:1 ratio for patients within 30 days of hospitalization (18, 19). Our study reported that overnight shift was associated with increased mortality of IHCA patients in general wards, which could be attributed to the highly disproportionate patient-to-nurse ratios and overload for overnight nursing staff in general wards (20). Previous study with a large sample size with 86,748 IHCA patients (58, 593 cases during day/evening hours; 28,155 cases during night hours) indicated lower survival during night hours in comparison with event occurred during day/evening hours (11), which supported our result.
Initially-Detected VT/VF and Respiratory Depression as the Direct Cause of IHCA had Better Survival
Compared to all rhythms and non-shockable rhythms, VF and pulseless VT showed better survival and were two to three times more likely to survive to hospital discharge (1, 21). Higher prevalence of respiratory insufficiency was shown if the duration of preceding hospitalization was longer (22). Pre-existing data indicated that attempts at intubation may delay timely defibrillation and interruption in chest compressions, contributing to poor outcomes (23). However, in patients with respiratory depression as the cause of IHCA, intubation was not associated with worse survival (24).
Our study reported that patients with respiratory depression as the cause of IHCA had better survival in overall cohort and ICU/ER subgroup, but not in general ward subgroup. This result might be due to the fact that predictable or avoidable cardiac arrest may occur if patients had respiratory depression as the direct cause of IHCA events, and whether timely intubation affect survival.
IHCA Patients With a Witness Showed Better Survival, and No Survival Difference Was Noted Between Patients With and Without In-Hospital Resuscitation Teams
Many IHCA cases are considered preventable or avoidable, and witnessed IHCA events are associated with improved outcomes (25, 26). Our study reported that witnessed IHCA patients in the ICU/ER subgroup did not have better outcomes, whereas the overall cohort and general ward subgroup showed better outcomes. This difference could be attributed to the existence of well-monitored settings and alarm systems in ICU/ER to offer timely response, despite the absence of a witness.
Early detected cardiac arrest events in monitored settings and early warning systems are associated with improved outcomes (27, 28). Event location at an examination room showed better outcomes in our study (Figure 2K). In our study, there was no survival difference between patients with and without in-hospital resuscitation teams (Figure 4C) (Table 3). This result is the contribution of well-trained staff, with sufficient skills to respond to possible preventable IHCA events in usual care.
Study Limitations
First, our data were acquired from a unified medical record sheet filled out by professional practitioners, and information on comorbidities, past medical history, and underlying diseases were unavailable. Thus, post-resuscitation survival predictor such as CASPRI score could not be calculated. Second, detailed information such as definite collapse time, vital sign before resuscitation, and initial rhythm at collapse were not shown if IHCA events occurred in situations without monitor or witness. Moreover, resuscitation time, other interventions or devices and additional medical therapy were not documented. Finally, this was a multicenter, registered study, thus, future prospective randomized studies are required to confirm our findings. Finally, patients who underwent TTM had better outcomes, and this result was associated with the impact of TTM on post-resuscitation development rather than selection bias. However, this study enrolled IHCA patients between 2013 June and 2018 December, whereas national health insurance in Taiwan did not covered TTM until 2018 June. Selection bias might exist once life expectancy and economic issue were considered, however, there was no difference in terms of proportion of hypotension as cause of IHCA regardless receiving TTM or not (with: 16.67%; without: 12.38%, P = 0.5293). Furthermore, compared with previous study more than one decade ago, despite the improvement in ACLS training, rate of survival to discharge in overnight shift was not improved, which might be attributed to hospital level and disease severity. However, the evaluation of disease severity was our limitation.
Study Strengths
This large registered multicenter study for adult IHCA patients enrolled different hospital levels and evaluated potential risk factors for mortality in patients after IHCA. Previous large sample size study focused on the association between survival and event time, thus it divided IHCA patients into events occurred during night hours and during day/evening hours (1). Our study analyzed the differences between survival and death subgroups to get information about the potential risk factors for IHCA mortality. Moreover, comparison between general wards and ICU/ER subgroups also strengthened the impact of patient-to-nurse ratios on survival for IHCA patients. The finding that overnight shift increased the mortality risk of IHCA patients in general wards or in both ICU and ER prompts the effort to achieve better work environments and decrease patient-to-nurse ratios in the future.
Conclusions
IHCA patients, including those in ICUs, ERs, and general wards, who are receiving ventilator support and vasoactive agents had poor survival. Better survival was observed in patients with VT and VF as initial rhythms. However, old age had a negative effect on overall survival. Overnight shifts were associated with poor survival in the general ward subgroup, although no significance was found in the overall cohort and ICU/ER subgroup. Thus, efforts to decrease patient-to-nurse ratios during overnights shift might improve survival in patients after IHCA.
Data Availability Statement
The original contributions generated for this study are included in the article/supplementary material, further inquiries can be directed to the corresponding author/s.
Ethics Statement
The studies involving human participants were reviewed and approved by The Institutional Review Board (IRB) of the Kaohsiung Veterans General Hospital approved this study (No. VGHKS19- EM 12-01). Written informed consent was not required for this study as the JCT dataset consists of de-identified secondary data for research purposes.Written informed consent for participation was not required for this study in accordance with the national legislation and the institutional requirements.
Author Contributions
W-CH: concept and design. S-YW and E-HY: acquisition, analysis, or interpretation of data. M-TW: drafting of the manuscript. W-CH and DY: critical revision of the manuscript for important intellectual content. S-YW and E-HY: statistical analysis. W-CH: administrative, technical, or material support. W-CH and H-HL: supervision. All authors contributed to the article and approved the submitted version.
Funding
This study was supported by grants from the Kaohsiung Veterans General Hospital, Kaohsiung, Taiwan, VGHKS19-EM12-01.
Conflict of Interest
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
Acknowledgments
We would like to thank Mister Chiu Yong Chih for his expert statistical assistance.
References
1. Andersen LW, Holmberg MJ, Berg KM, Donnino MW, Granfeldt A. In-hospital cardiac arrest: a review. JAMA. (2019) 321:1200–10. doi: 10.1001/jama.2019.1696
2. Merchant RM, Yang L, Becker LB, Berg RA, Nadkarni V, Nichol G, et al. Incidence of treated cardiac arrest in hospitalized patients in the United States. Crit Care Med. (2011) 39:2401–6. doi: 10.1097/CCM.0b013e3182257459
3. Holmberg M, Ross C, Fitzmaurice GM, Chan P, Duval-Arnould J, Grossestreuer AV, et al. Incidence of adult in-hospital cardiac arrest in the United States. Abstract presented at: American Heart Association Resuscitation Science Symposium.Chicago, IL (2018).
4. Belletti A, Benedetto U, Putzu A, Martino EA, Biondi-Zoccai G, Angelini GD, et al. Vasopressors during cardiopulmonary resuscitation. A network meta-analysis of randomized trials. Crit Care Med. (2018) 46:e443–51. doi: 10.1097/CCM.0000000000003049
5. Soar J, Callaway CW, Aibiki M, Bottiger BW, Brooks SC, Deakin CD, et al. Part 4: Advanced life support: 2015 international consensus on cardiopulmonary resuscitation and emergency cardiovascular care science with treatment recommendations. Resuscitation. (2015) 95:e71–120. doi: 10.1161/CIR.0000000000000273
6. Callaway CW, Donnino MW, Fink EL, Geocadin RG, Golan E, Kern KB, et al. Part 8: post-cardiac arrest care: 2015 American heart association guidelines update for cardiopulmonary resuscitation and emergency cardiovascular care. Circulation. (2015) 132:S465–82. doi: 10.1161/CIR.0000000000000262
7. Ueyama T, Moritani K, Shimizu A, Kakugawa H, Matsuzaki M. Lethal arrhythmias–etiological view and therapeutic approach. Nihon Rinsho. (2002) 60:1269–77.
8. Peberdy MA, Callaway CW, Neumar RW, Geocadin RG, Zimmerman JL, Donnino M, et al. Part 9: post-cardiac arrest care: 2010 American heart association guidelines for cardiopulmonary resuscitation and emergency cardiovascular care. Circulation. (2010) 122:S768–86. doi: 10.1161/CIRCULATIONAHA.110.971002
9. Part 8: advanced challenges in resuscitation. Section 2: toxicology in ECC. European Resuscitation Council. Resuscitation. (2000) 46:261–6. doi: 10.1016/S0300-9572(00)00287-2
10. Link Mark S, Berkow Lauren C, Kudenchuk Peter J, Halperin Henry R, Hess Erik P, Moitra Vivek K, et al. Part 7: adult advanced cardiovascular life support. Circulation. (2015) 132:S444–64. doi: 10.1161/CIR.0000000000000261
11. Peberdy MA, Ornato JP, Larkin GL, Braithwaite RS, Kashner TM, Carey SM, et al. Survival from in-hospital cardiac arrest during nights and weekends. JAMA. (2008) 299:785–92. doi: 10.1001/jama.299.7.785
12. Morrison LJ, Neumar RW, Zimmerman JL, Link MS, Newby LK, McMullan PW Jr., et al. Strategies for improving survival after in-hospital cardiac arrest in the United States: 2013 consensus recommendations: a consensus statement from the American Heart Association. Circulation. (2013) 127:1538–63. doi: 10.1161/CIR.0b013e31828b2770
13. Moretti MA, Cesar LA, Nusbacher A, Kern KB, Timerman S, Ramires JA. Advanced cardiac life support training improves long-term survival from in-hospital cardiac arrest. Resuscitation. (2007) 72:458–65. doi: 10.1016/j.resuscitation.2006.06.039
14. Chan PS, Spertus JA, Krumholz HM, Berg RA, Li Y, Sasson C, et al. A validated prediction tool for initial survivors of in-hospital cardiac arrest. Arch Intern Med. (2012) 172:947–53. doi: 10.1001/archinternmed.2012.2050
15. Riley LE, Mehta HJ, Lascano J. Single-center in-hospital cardiac arrest outcomes. Indian J Crit Care Med. (2020) 24:44–8. doi: 10.5005/jp-journals-10071-23327
16. Liang YW, Chen WY, Lee JL, Huang LC. Nurse staffing, direct nursing care hours and patient mortality in Taiwan: the longitudinal analysis of hospital nurse staffing and patient outcome study. BMC Health Serv Res. (2012) 12:44. doi: 10.1186/1472-6963-12-44
17. Central News Agency. Taiwan: Majority of Taiwan Hospitals Facing Shortage of Nurses: Poll. Available online at: http://www.taiwannews.com.tw/etn/news_content.php?id=1576842. (accessed April 21, 2011)
18. Aiken LH, Clarke SP, Sloane DM, Sochalski J, Silber JH. Hospital nurse staffing and patient mortality, nurse burnout, and job dissatisfaction. JAMA. (2002) 288:1987–93. doi: 10.1001/jama.288.16.1987
19. Liang YW, Tsay SF, Chen WY. Effects of nurse staffing ratios on patient mortality in Taiwan acute care hospitals: a longitudinal study. J Nurs Res. (2012) 20:1–7. doi: 10.1097/JNR.0b013e3182466ddc
20. Chang H-L, Lin C-F. Taiwanese registered nurses' reasons for failure to practice. Int J Nurs Clin Pract. (2016) 3:5. doi: 10.15344/2394-4978/2016/176
21. Benjamin EJ, Virani SS, Callaway CW, Chamberlain AM, Chang AR, Cheng S, et al. Heart disease and stroke statistics-2018 update: a report from the American heart association. Circulation. (2018) 137:e67–492. doi: 10.1161/CIR.0000000000000558
22. Tran S, Deacon N, Minokadeh A, Malhotra A, Davis DP, Villanueva S, et al. Frequency and survival pattern of in-hospital cardiac arrests: the impacts of etiology and timing. Resuscitation. (2016) 107:13–8. doi: 10.1016/j.resuscitation.2016.07.006
23. Bradley SM, Zhou Y, Ramachandran SK, Engoren M, Donnino M, Girotra S. Retrospective cohort study of hospital variation in airway management during in-hospital cardiac arrest and the association with patient survival: insights from Get With The Guidelines-Resuscitation. Crit Care. (2019) 23:158. doi: 10.1186/s13054-019-2426-5
24. Andersen LW, Granfeldt A, Callaway CW, Bradley SM, Soar J, Nolan JP, et al. Association between tracheal intubation during adult in-hospital cardiac arrest and survival. JAMA. (2017) 317:494–506. doi: 10.1001/jama.2016.20165
25. Brady WJ, Gurka KK, Mehring B, Peberdy MA, O'Connor RE. In-hospital cardiac arrest: impact of monitoring and witnessed event on patient survival and neurologic status at hospital discharge. Resuscitation. (2011) 82:845–52. doi: 10.1016/j.resuscitation.2011.02.028
26. Larkin GL, Copes WS, Nathanson BH, Kaye W. Pre-resuscitation factors associated with mortality in 49,130 cases of in-hospital cardiac arrest: a report from the National Registry for Cardiopulmonary Resuscitation. Resuscitation. (2010) 81:302–11. doi: 10.1016/j.resuscitation.2009.11.021
27. Perman SM, Stanton E, Soar J, Berg RA, Donnino MW, Mikkelsen ME, et al. Location of in-hospital cardiac arrest in the United States-variability in event rate and outcomes. J Am Heart Assoc. (2016) 5:e003638. doi: 10.1161/JAHA.116.003638
Keywords: intensive care unit, in-hospital cardiac arrest, overnight shift, patient-to-nurse ratio, survival, targeted temperature management
Citation: Wang M-T, Huang W-C, Yen DH-T, Yeh E-H, Wu S-Y and Liao H-H (2021) The Potential Risk Factors for Mortality in Patients After In-Hospital Cardiac Arrest: A Multicenter Study. Front. Cardiovasc. Med. 8:630102. doi: 10.3389/fcvm.2021.630102
Received: 16 November 2020; Accepted: 22 February 2021;
Published: 16 March 2021.
Edited by:
Gen-Min Lin, Hualien Armed Forces General Hospital, TaiwanReviewed by:
Christoph Sinning, University Heart and Vascular Center Hamburg (UHZ), GermanyJuha Sinisalo, University of Helsinki and Helsinki University Hospital, Finland
Copyright © 2021 Wang, Huang, Yen, Yeh, Wu and Liao. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Hsun-Hsiang Liao, c2hpbmdAamN0Lm9yZy50dw==; Wei-Chun Huang, d2NodWFuZ2x1bHVAZ21haWwuY29t
†These authors have contributed equally to this work
 Mei-Tzu Wang
Mei-Tzu Wang Wei-Chun Huang
Wei-Chun Huang David Hung-Tsang Yen5,6
David Hung-Tsang Yen5,6