- 1Department of Pediatric Emergency Medicine, China Medical University Children's Hospital, China Medical University, Taichung, Taiwan
- 2Department of Medicine, College of Medicine, China Medical University, Taichung, Taiwan
- 3Department of Medical Research, China Medical University Children's Hospital, China Medical University, Taichung, Taiwan
- 4Department of Pediatrics, Children's Medical Center, Taichung Veterans General Hospital, Taichung, Taiwan
- 5School of Medicine, National Yang-Ming Chiao-Tung University, Taipei, Taiwan
- 6School of Medicine, Kaohsiung Medical University, Kaohsiung, Taiwan
- 7Department of Cardiology, Taipei Veterans General Hospital, Taipei, Taiwan
- 8Department of Public Health, Chung Shan Medical University, Taichung, Taiwan
- 9Department of Medicine, Taichung Tzu Chi Hospital, The Buddhist Tzu Chi Medical Foundation, Taichung, Taiwan
- 10Department of Medicine, College of Medicine, Tzu Chi University, Hualien, Taiwan
Background: The effect of smoking on short-term outcomes among patients with acute coronary syndrome (ACS) undergoing percutaneous coronary intervention (PCI) is controversial. However, little is known about the impact of smoking on long-term outcomes in patients with stable coronary artery disease (CAD) who receive PCI.
Methods: A total of 2,044 patients with stable CAD undergoing PCI were evaluated. They were divided into two groups according to smoking status (current smokers vs. non-smokers). Baseline characteristics, exposed risk factors, angiographic findings, and interventional strategies were assessed to compare the long-term clinical outcomes between groups. Predictors for myocardial infarction (MI), all-cause death, cardiovascular (CV) death, and repeated PCI procedures were also analyzed.
Results: Compared with non-smokers, current smokers were younger and mostly male (both P < 0.01). They also had a lower prevalence of chronic kidney disease (CKD) and diabetes (both P < 0.01). Drugs including a P2Y12 receptor inhibitor of platelets (P2Y12 inhibitor), beta-blockers (BB), and statins were used more frequently in current smokers (P < 0.01, P < 0.01, P = 0.04, respectively). Freedom from all-cause death and CV death was lower in the non-smoker group (P < 0.001, P = 0.003, respectively). After adjustment, logistic regression revealed smoking was a major predictor for all-cause death and repeated PCI procedure [hazard ratio(HR): 1.71 and 1.46, respectively].
Conclusions: Smoker's paradox extends to long-term outcome in patients with stable CAD undergoing PCI, which is partially explained by differences in baseline characteristics. However, smoking strongly predicted all-cause mortality and repeated PCI procedures in patients with stable CAD undergoing PCI.
Introduction
Coronary artery disease (CAD) is a very common cardiovascular disease; except for standard coronary angiography, precise detection of CAD via deep learning technique and artificial intelligence are in development (1–7). Percutaneous coronary intervention (PCI) refers to coronary revascularization via various devices including balloon angioplasty or stent deployment. PCI is a common clinical practice in patients with stable CAD. Nevertheless, major adverse clinical events (MACE), including myocardial infarction (MI), revascularization and death can occur in patients after receiving PCI (8). Major risk factors, including diabetes mellitus (DM), hypertension dyslipidemia, and smoking could affect outcomes in patients with stable CAD who receive PCI. “Smoker's paradox” is not a new concept, it was firstly mentioned in 1995 to describe the unpredictable favorable outcome of reduced short-term mortality in smokers after acute coronary syndrome (9, 10). However, most studies describe smoker's paradox include both current and former smokers under the general classification of “smoking,” which might confound the true beneficial effect of nicotine withdraw; while excluding former smokers might clarify whether this phenomenon exist or not.
Literature Review
The impact of smoking on outcomes in patients with acute coronary syndrome (ACS) or acute myocardial infarction (AMI) who receive PCI remains conflicting (11, 12). As for patients with ST elevation myocardial infarction (STEMI) receiving primary PCI, smokers had a similar one-year mortality rate compared with non-smokers (13, 14). On the contrary, some studies have revealed current smokers had better long-term outcomes compared with non-smokers with STEMI who were undergoing primary PCI. They also had more favorable post-infarction LV remodeling (15, 16). Given non-ST elevation acute coronary syndrome (NSTE-ACS), smokers seemed to have higher one-year mortality compared with non-smokers (17), while other study reported the existence of the smoker's paradox (18). The above differences were summarized in Table 1.
Hypothesis
In patients with stable CAD, current smokers have a greatly increased risk of future cardiovascular events, including mortality, compared with never-smokers (19). Other reported that after adjusting for differences in age, there did not appear to be any protective effect of smoking on 6-months cardiovascular outcomes in patients with stable CAD following PCI (20). Nevertheless, the effect of smoking on long-term outcomes in patients with stable CAD receiving PCI remains obscure. We hypothesize smoker's paradox extends to stable CAD patients undergoing PCI after long-term follow-up. Therefore, a longitudinal, prospective observational study was conducted to compare the influence of smoking on long-term outcomes between current smokers and non-smokers in patients with stable CAD after undergoing PCI. In addition, predictors for adverse clinical outcomes in both groups were further analyzed.
Materials and Methods
Study Design and Population
A prospective longitudinal study was conducted via catheterization data review from July 2011 through December 2018. Stable patients with CAD aged 20 to 90 years were recruited who underwent PCI at the inpatient clinic at the Taichung Tzu Chi Hospital, Taiwan. The patients were divided into two groups: current smokers or non-smokers. Patients with end-stage heart failure (HF), a previous history of malignancy, and scheduled PCI were excluded. Most patients were obtained during regular visits in the outpatient department (OPD). For patients who were lost to follow-up, a phone call was used to contact the patients themselves or their families. A survey of four-year clinical outcomes regarding all-cause death and major adverse cardiovascular events (MACE), including myocardial infarction, (MI), cardiovascular death (CV death), and repeated PCI procedures were completed at the end of the study. The Institution Review Board and ethics committee of Taichung Tzu Chi Hospital approved the study protocol, and no informed consent was required. This cohort study also fulfilled the guidance of Strengthening the Reporting of Observational Studies in Epidemiology (STROBE) statement (21).
Data Processing, Measurements, and Analysis
Baseline characteristics, including body habitus, biochemical profiles, angiographic findings from cardiac catheterization, major risk factors, and variant therapeutic strategies such as drug medications and interventional procedures (balloon angioplasty, bare metal stent deployment, or drug-eluting stent deployment) were obtained. The criteria for major risk factors are described as follows: Diabetes Mellitus was defined as a fasting plasma glucose level > 126 mg/dL, a casual plasma glucose level > 200 mg/dL, or a hemoglobin A1c (HbA1c) level > 6.5% (22). Hypertension was defined as a BP of 140/90 mm Hg or higher, BP levels for which the benefits of pharmacologic treatment have been definitely established (23). Chronic kidney disease (CKD) was defined as an estimated glomerular filtration rate (eGFR) < 60 ml/min/1.73 m2, which is equal to or more than stage III chronic kidney disease (CKD) (24). Hypercholesterolemia was defined as a serum cholesterol level of more than 200 mg/dL or an LDL-C level > 100 mg/dL (25). Previous MI history was defined as a history of MI prior to index PCI, accompanied by a three-fold elevation of cardiac enzymes from the baseline value.
As for the hemodynamic data, central aortic pressures were measured continuously, and mean values were calculated during catheterization. Angiographic findings, including the number of diseased vessels and lesions were calculated, the lesion severity and complexity were evaluated via the synergy between PCI with Taxus Express paclitaxel-eluting stent (Boston Scientific, Marlborough, MA, USA) and cardiac surgery score (SYNTAX score) (26). Related clinical parameters including general characteristics, hemodynamic data, exposed risk factors, and interventional strategies were compared between current smokers and non-smokers. In addition, significant predictors for all-cause death and MACE were identified.
Statistical Analysis
The analysis was primarily used to compare the differences between the two groups. Pearson's chi-squared test and Fisher's exact test was used to examine categorical variables. Analysis of variance (ANOVA) was used to test continuous variables. The log-rank test and Kaplan-Meier survival curves were used for comparing the survival difference. The Cox proportional hazards model was used to test the effect of independent variables on hazards. P-values < 0.05 were considered significant. All analyses were performed using SPSS for Windows, Version 24.0 (IBM Corp., Armonk, NY, USA).
Results
Baseline Characteristics of Study Population
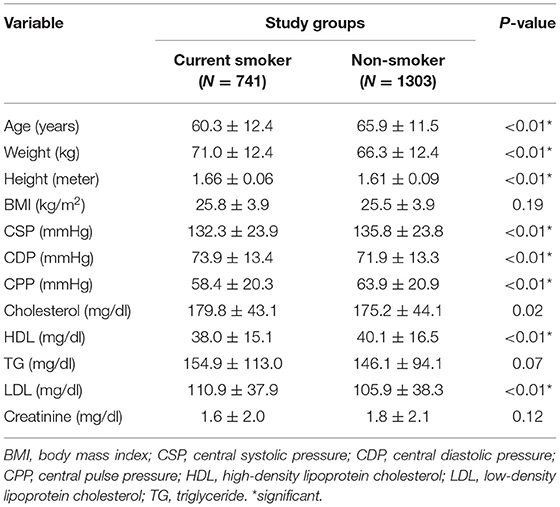
During the study period, a total of 2,044 patients with stable CAD who had undergone PCI were assessed. Among them, 741 patients were current smokers and 1,303 patients were non-smokers, respectively. The mean follow-up time for current smokers and non-smokers was 49.3 ± 33.5 months and 48.0 ± 37.4 months, respectively (P = 0.43). Baseline clinical characteristics are listed in Table 2. Current smokers were younger than non-smokers (60.3 ± 12.4 vs. 65.9 ± 11.5 years old, P < 0.01). Current smokers had higher serum total cholesterol (179.8 ± 43.1 vs. 175.2 ± 44.1 mg/dL, P < 0.01) and low density lipoprotein cholesterol (LDL-C) levels (110.9 ± 37.9 vs. 105.9 ± 38.3 mg/dL). There was no difference in body mass index (BMI) between groups (P = 0.19). Given the hemodynamic data, current smokers had a lower central pulse pressure (CPP) than non-smokers (58.4 ± 20.3 vs. 63.9 ± 20.9 mmHg, P < 0.01).
Demographic and Clinical Data
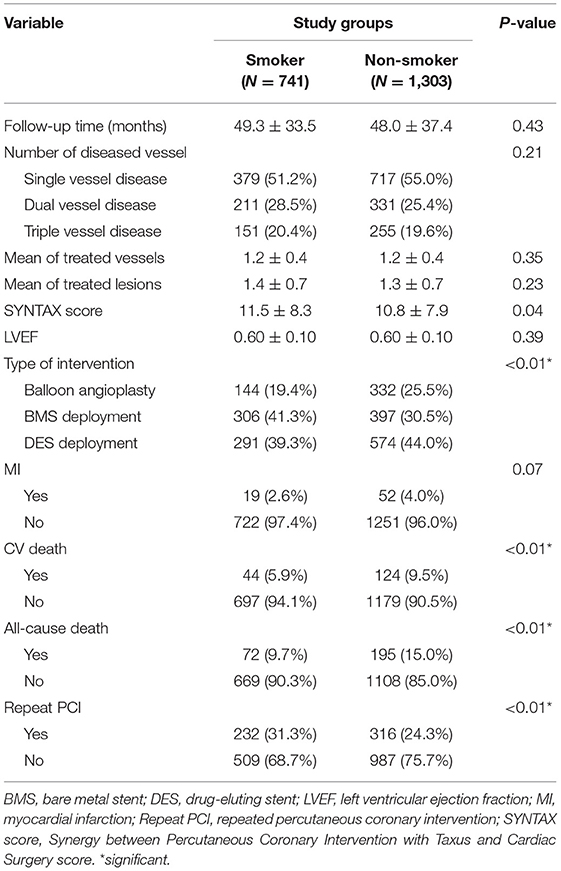
Patient demographic and clinical data is shown in Table 3. Current smokers were mostly men (P < 0.01) and had a lower prevalence of DM and CKD, but a higher prevalence of previous MI compared with non-smokers (all P < 0.01). After the index PCI, current smokers were prescribed P2Y12 inhibitors, beta blockers, and statins more frequently than non-smokers (P < 0.01, P < 0.01, P = 0.04, respectively).
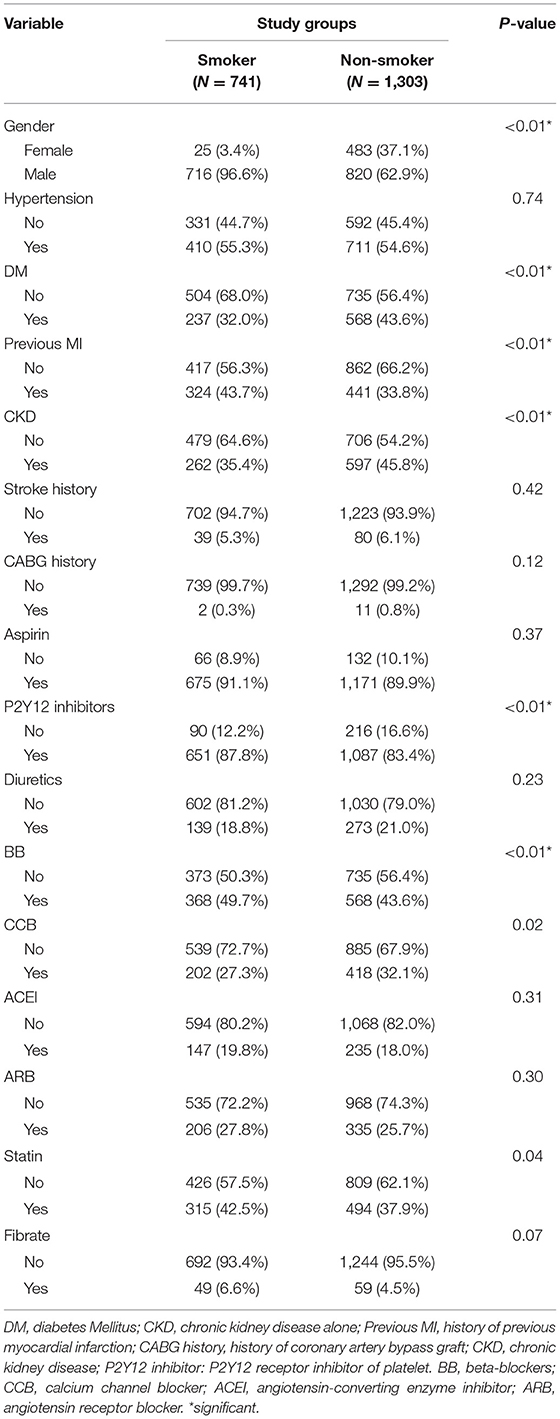
Table 3. Demographics and clinical data of study population, and medications prescribed after index PCI among groups.
The results of angiographic findings and clinical outcomes are shown in Table 4. There was no difference in the number of diseased vessels, treated vessels, and treated lesions between both groups (all P = NS); however, current smokers had a higher SYNTAX score compared with non-smokers (P = 0.04). They also received more balloon angioplasty and bare-metal stent (BMS), but less drug-eluting stent (DES) deployment than non-smokers (P < 0.01). Current smokers had a lower rate of all-cause death and CV death than non-smokers (P < 0.01, P < 0.01, respectively); however, they had a higher rate of repeat PCI procedures than non-smokers (P < 0.01). The cumulative curve of freedom from MI, CV death, all-cause death, and repeated PCI procedures between the 2 groups is shown in Figure 1. Freedom from all-cause death and CV death was higher in the current smokers group (P < 0.001, P < 0.003, respectively), but they had a lower freedom from repeated PCI procedures (P < 0.001).
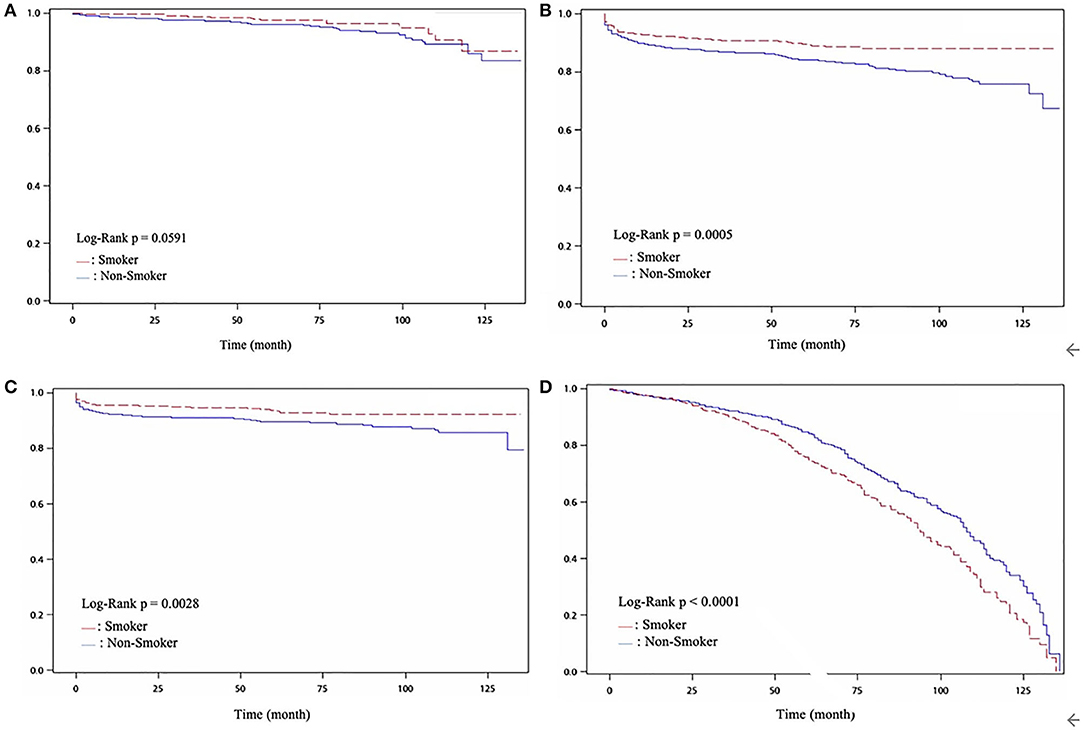
Figure 1. (A) Cumulative ratio of freedom from MI between two groups (P = 0.0591); (B) Cumulative ratio of freedom from all-cause death between two groups (P < 0.001); (C) Cumulative ratio of freedom from CV death between two groups (P < 0.003); (D) Cumulative ratio of freedom from Re-PCI between two groups (P < 0.001.
Predictors for Clinical Outcome
The predictors for all-cause death and MACE are shown in Table 5 (multivariate regression was used for this analysis). Before adjusting, age was related to all-cause death while smoking status was related to repeated PCI procedure. After adjusting, age no longer remained significant to any clinical outcome but smoking was found to be an independent risk factor for all-cause death and repeated PCI procedures after adjustment for age, DM, and CKD. As for predictors of clinical outcome, DM and previous MI history increased the risk of all-cause death, while usage of aspirin and angiotensin-converting enzyme inhibitor (ACEI) would reduce the risk of all-cause death. Use of aspirin and statins reduced the risk of CV death. Finally, CKD, high SYNTAX score, and use of P2Y12 inhibitors increased the risk of repeated PCI procedures; whereas usage of ACEI and statins would reduce the risk of repeated PCI procedures.
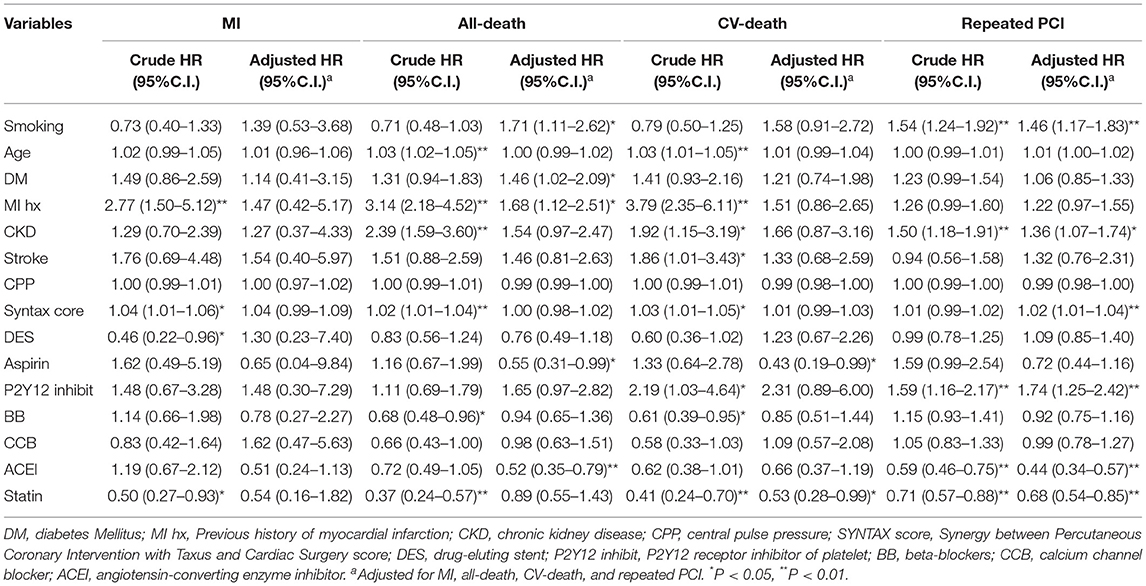
Table 5. Significant crude and adjusted predictors of outcome in Cox proportion hazard model for MI, All-death, CV-death, Repeated PCI.
Discussion
The role of smoking on short-term outcomes in patients with ACS remains controversial. On the other hand, the influence of smoking on long-term outcomes in patients with stable CAD undergoing PCI is not clear. In contrast with adverse short-term cardiovascular outcomes observed in smokers, it seemed that current smokers have a better long-term prognosis in terms of all-cause mortality, cardiovascular mortality and repeated PCI procedures compared with non-smokers, and thus confirm our hypothesis. In addition, DM and CKD were predictors for all-cause death, while usage of aspirin and ACEI was associated with reduced risk. Finally, CKD, SYNTAX score, and use of P2Y12 inhibitors predicted repeat PCI procedures, but usage of ACE inhibitors and statins reduced the risk of repeat PCI.
In the present study, current smokers were 5 years younger than non-smokers, and there was no difference in the prevalence of hypertension between the two groups. However, central systolic pressure (CSP) was lower and central diastolic pressure (CDP) was higher in current-smokers compared with non-smokers, therefore current-smokers presented with a lower average central pulse pressure (CPP). This result might imply current smokers had less arterial stiffness and vascular resistance than non-smokers due to younger age, which is consistent with a previous study (27). On the other hand, although current smokers had a higher percentage of elevated serum total cholesterol and LDL-C, they also used statins more frequently than non-smokers after receiving PCI. This may negate the adverse effect of dyslipidemia on coronary atherosclerosis and clinical events.
Current smokers had a lower prevalence of DM and CKD, but a higher prevalence of MI history than non-smokers. This is compatible with a previous study that reported current-smokers had fewer adverse clinical profiles than non-smokers (28). Nevertheless, DM and MI history remained significantly correlated with all-cause death, while CKD was significantly related to repeated PCI procedures. This result is similar with previous studies that focused on adverse predictors for patients undergoing PCI. DM and previous MI have been reported to be predictors for all-cause death while CKD was a predictor for repeated PCI procedures (29).
Platelet P2Y12 inhibitors and statins were used more frequently in smokers compared with non-smokers after receiving PCI in the current study. Clopidogrel was used more often than ticagrelor and prasugrel was not available. The role of smoking on clopidogrel activity remains controversial. Some studies have concluded current smokers may have a higher clopidogrel metabolite exposure and pharmacodynamic effects than non-smokers (30), while cessation of smoking in clopidogrel-treated patients after PCI increased both VerifyNow P2Y12 platelet reaction units (PRUs) and platelet activity (31, 32). Another study postulated the lower PRUs were due to higher hemoglobin levels in current smokers than non-smokers, and there was no difference of PRUs after adjustment for hemoglobin (33). In our study, usage of P2Y12 inhibitors failed to reduce mortality but was associated with higher repeated PCI procedures. This was probably due to the high prevalence of previous MIs and multi-vessel disease in the study population. On the other hand, The use of ACEIs reduced all-cause death and repeat PCI procedures in patients with stable CAD irrespective of smoking status, which is consistent with previous reports (34, 35). Usage of statins also reduced CV death and the risk of repeated PCI procedures even though current-smokers and non-smokers had mildly elevated LDL-C levels. This suggests the use of statins could improve clinical outcomes in patients with stable CAD after receiving PCI even though there is a paucity of large scale clinical studies available.
Although current smokers had a lower rate of all-cause death and CV death than non-smokers, smoking was no more significant to both outcomes after adjusting for age, which implicates a lead-time bias might explain the smoking paradox in the survival analysis of all-cause death and CV death. There was no difference in the number or distribution of diseased vessels, treated vessels, and lesions between the two groups, but the SYNTAX score was higher in current smokers than non-smokers. Nevertheless, bare metal stents (BMS) deployment was performed more frequently in current-smokers; whereas, more drug-eluting stents (DES) were deployed in non-smokers. Collectively these factors might cause increased repeated PCI procedures in current smokers during long-term follow up (36).
Finally, we summarized the outcome differences between current smokers and non-smokers. In the long-term follow up, current smokers had a lower rate of all-cause death and CV death, but a higher rate of repeated PCI procedures than non-smokers. Based on the results of the adjusted regression model, we found smoking, DM and previous MI history predicted the hazard of all-cause death. Smoking, presence of CKD, SYNTAX score, and use of P2Y12 inhibitors predicted the hazard for repeated PCI. Aspirin could reduce both all-cause mortality and cardiovascular mortality. Although smoker's paradox still exists in patients with stable CAD undergoing PCI, it was explained by young age and few clinical adverse characteristics in current smokers. Smoking remained an adverse predictor for long-term clinical outcomes in patients with stable CAD undergoing PCI, this is firstly described. According to this study, cessation of smoking is recommended from viewpoint of preventive medicine, while aspirin usage could reduce long-term mortality in patients undergoing PCI whether smoke or not.
Study Limitations
First, the amount of daily cigarette consumption and duration of smoking was not fully surveyed in this study, which might affect the extent of coronary atherosclerosis and thus influence the long-term outcome. Second, the age difference in study groups may cause lead-time bias, which could confound the survival analysis. Third, the number of MIs in both groups were too few to yield statistical significance, the possibility of inadequate follow-up time might exist. Fourth, despite of exclusion of end stage HF patients, a lower LVEF has an direct impact on mortality. This can be a potential confounding factor if the subgroup of patient with lower LVEF data were not captured in both groups. Finally, although clinical trials comparing the effect of smoking on stable CAD patients undergoing PCI is difficult for ethical reasons, whether aggressive cessation of smoking could improve long-term outcomes in smokers with stable CAD after receiving PCI remains to be clarified.
Conclusions
The smoker's paradox extends to long-term outcome in stable CAD patients after undergoing PCI, which might be due to few clinical adverse characters in current smokers. However, smoking status independently predicted all-cause death and repeated PCI procedures in stable CAD patients after undergoing PCI. Further investigation of smoker's paradox between current smokers and ex-smokers via deep learning technique and artificial intelligence might be helpful.
Data Availability Statement
The original contributions presented in the study are included in the article/supplementary materials, further inquiries can be directed to the corresponding author/s.
Ethics Statement
The studies involving human participants were reviewed and approved by the Institution Review Board and Ethics Committee of Taichung Tzu Chi Hospital. Written informed consent was not required for this study, in accordance with the local legislation and institutional requirements.
Author Contributions
M-JL and H-PW conceived and designed the study. S-LJ and S-LC collected the study data. C-CH performed the statistical analysis. H-PW and S-LJ drafted the manuscript. M-JL revised the manuscript. All authors had read and approved the final manuscript.
Funding
This study was supported by a grant from the Department of Research, Taichung Tzu Chi Hospital, Taiwan and the China Medical University Hospital (Grant Number: C1090903010).
Conflict of Interest
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
Publisher's Note
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
References
1. Shoeibi A, Khodatars M, Alizadehsani R, NGhassemi N, Jafari M, Moridian P, et al. Automated detection and forecasting of COVID-19 using deep learning techniques: a review. arXiv:2007.10785. (2020).
2. Shoeibi A, Khodatars M, Jafari M, Moridian P, Rezaei M, Alizadehsani R, et al. Applications of deep learning techniques for automated multiple sclerosis detection using magnetic resonance imaging: a review. arXiv. (2021) 136:104697. doi: 10.1016/j.compbiomed.2021.104697
3. Sadeghi D, Shoeibi A, Ghassemi N, Moridian P, Khadem A, Alizadehsani R, et al. An overview on artificial intelligence techniques for diagnosis of schizophrenia based on magnetic resonance imaging modalities: methods, challenges, and future works. arXiv preprint arXiv:2103.03081. (2021).
4. Shoeibi A, Ghassemi N, Khodatars M, Jafari M, Moridian P, Alizadehsani R, et al. Applications of epileptic seizures detection in neuroimaging modalities using deep learning techniques: methods, challenges, and future works. arXiv preprint arXiv:2105.14278. (2021).
5. Alizadehsani R, Khosravi A, Roshanzamir M, Abdar M, Sarrafzadegan N, Shafie D, et al. Coronary artery disease detection using artificial intelligence techniques: a survey of trends, geographical differences and diagnostic features 1991–2020. Comput Bio Med. (2021) 128:104095. doi: 10.1016/j.compbiomed.2020.104095
6. Sharifrazi D, Alizadehsani R, Joloudari JH, Shamshirband S, Hussain S, Sanidoix ZA, et al. CNN-KCL: Automatic Myocarditis Diagnosis Using Convolutional Neural Network Combined With K-Means Clustering. doi: 10.20944/preprints202007.0650.v1
7. Sharifrazi D, Alizadehsani R, Izadi NH, Roshanzamir M, Shoeibi A, Khozeimeh F, et al. Hypertrophic cardiomyopathy diagnosis based on cardiovascular magnetic resonance using deep learning techniques. SSRN Electronic J. (2021). Available online at: https://ssrn.com/abstract=3855445
8. Williams DO, Abbott JD, Kip KE, DEScover Investigators. Outcomes of 6906 patients undergoing percutaneous coronary intervention in the era of drug-eluting stents: report of the DEScover Registry. Circulation. (2006) 114:2154–62. doi: 10.1161/CIRCULATIONAHA.106.667915
9. Aune E, Røislien J, Mathisen M, Thelle DS, Otterstad JE. The “smoker's paradox” in patients with acute coronary syndrome: a systematic review. BMC med. (2011) 9:97. doi: 10.1186/1741-7015-9-97
10. Grines CL, Topol EJ, O'Neill WW, George BS, Kereiakes D, Phillips HR, et al. Effect of cigarette smoking on outcome after thrombolytic therapy for myocardial infarction. Circulation. (1995) 91:298–303 doi: 10.1161/01.CIR.91.2.298
11. Coutinho Cruz M, Ilhão Moreira R, Abreu A, Timóteo AT, Sá Carvalho R, Ferreira L, et al. The smoker's paradox in acute coronary syndrome: is it real? Rev Port Cardiol. (2018) 37:847–55. doi: 10.1016/j.repc.2017.12.005
12. Weisz G, Cox DA, Garcia E, Tcheng JE, Griffin JJ, Guagliumi G, et al. Impact of smoking status on outcomes of primary coronary intervention for acute myocardial infarction–the smoker's paradox revisited. Am Heart J. (2005) 150:358–64. doi: 10.1016/j.ahj.2004.01.032
13. Redfors B, Furer A, Selker HP, Thiele H, Patel MR, Chen S, et al. Effect of smoking on outcomes of primary PCI in patients with STEMI. J Am Coll Cardiol. (2020) 75:1743–54. doi: 10.1016/j.jacc.2020.02.045
14. Steele L, Lloyd A, Fotheringham J, Sultan A, Iqbal J, Grech ED. A retrospective cohort study of the association between smoking and mortality after acute ST-segment elevation myocardial infarction. Postgrad Med J. (2017) 93:489–93. doi: 10.1136/postgradmedj-2016-134605
15. Ciccarelli G, Barbato E, Golino M, Cimmino G, Bartunek J, Di Serafino L, et al. Prognostic factors in patients with STEMI undergoing primary PCI in the clopidogrel era: role of dual antiplatelet therapy at admission and the smoking paradox on long-term outcome. J Interv Cardiol. (2017) 30:5–15. doi: 10.1111/joic.12360
16. Symons R, Masci PG, Francone M, Claus P, Barison A, Carbone I, et al. Impact of active smoking on myocardial infarction severity in reperfused ST-segment elevation myocardial infarction patients: the smoker's paradox revisited. Eur Heart J. (2016) 37:2756–64. doi: 10.1093/eurheartj/ehv738
17. Robertson JO, Ebrahimi R, Lansky AJ, Mehran R, Stone GW, Lincoff AM. Impact of cigarette smoking on extent of coronary artery disease and prognosis of patients with non-ST-segment elevation acute coronary syndromes: an analysis from the ACUITY Trial (acute catheterization and urgent intervention triage strategy) JACC Cardiovasc Interv. (2014) 7:372–9. doi: 10.1016/j.jcin.2013.11.017
18. Amor-Salamanca A, Devesa-Cordero C, Cuesta-Díaz A, Carballo-López MC, Fernández-Ortiz A, García-Rubira JC. Smoking paradox in acute coronary syndrome without ST-segment elevation. Med Clin. (2011) 136:144–8. doi: 10.1016/j.medcli.2010.01.039
19. Bouabdallaoui N, Messas N, Greenlaw N, Ferrari R, Ford I, Kim M, et al. Impact of smoking on cardiovascular outcomes in patients with stable coronary artery disease. Eur J Prev Cardiol. (2020) 2047487320918728. doi: 10.1177/2047487320918728
20. Mohamedali B, Shroff A. Impact of smoking status on cardiovascular outcomes following percutaneous coronary intervention. Clin Cardiol. (2013) 36:372–7. doi: 10.1002/clc.22134
21. Vandenbroucke JP, von Elm E, Altman DG, Gøtzsche PC, Mulrow CD, Pocock SJ, et al. Strengthening the reporting of observational studies in epidemiology (STROBE):explanation and elaboration. Ann Intern Med. (2007) 147:W163–94. doi: 10.7326/0003-4819-147-8-200710160-00010-w1
22. American Diabetes Association. Diagnosis and classification of diabetes mellitus. Diabetes Care. (2013) 36:S67–74. doi: 10.2337/dc13-S067
23. Chobanian AV, Bakris GL, Black HR, Cushman WC, Green LA, Izzo JL Jr, et al. The seventh report of the joint national committee on prevention, detection, evaluation, and treatment of high blood pressure: the JNC 7 report. JAMA. (2003) 289:2560–72. doi: 10.1001/jama.289.19.2560
24. National Kidney Foundation. K/DOQI clinical practice guidelines for bone metabolism and disease in chronic kidney disease. Am J Kid Disney Dis. (2003) 42:S1–201. doi: 10.1016/S0272-6386(03)00905-3
25. Expert Expert Panel on Detection Evaluation and and Treatment of High Blood Cholesterol In Adults. Executive summary of the third report of the national cholesterol education program (NCEP). expert panel on detection, evaluation, and treatment of high blood cholesterol in adults (adult treatment panel III). JAMA. (2001) 285:2486–97. doi: 10.1001/jama.285.19.2486
26. Serruys PW, Morice MC, Kappetein AP, Colombo A, Holmes DR, Mack MJ, et al. Percutaneous coronary intervention versus coronary-artery bypass grafting for severe coronary artery disease. N Engl J Med. (2009) 360:961–72. doi: 10.1056/NEJMoa0804626
27. Wu HP, Lin MJ. Central aortic pressure and long-term outcome in hypertensive patients undergoing percutaneous coronary intervention. Sci Rep. (2020)10:17420. doi: 10.1038/s41598-020-74619-3
28. Angeja BG, Kermgard S, Chen MS, McKay M, Murphy SA, Antman EM, et al. The smoker's paradox: insights from the angiographic substudies of the TIMI trials. J ThrombThombolysis. (2002) 13:133–39. doi: 10.1023/A:1020470721977
29. Lin MJ, Lee J, Chen CY, Huang CC, Wu HP. Chronic kidney disease and diabetes associated with long-term outcomes in patients receiving percutaneous coronary intervention. BMC Cardiovasc Disord. (2017) 17:242. doi: 10.1186/s12872-017-0673-4
30. Gurbel PA, Bliden KP, Logan DK, Kereiakes DJ, Lasseter KC, White A, et al. The influence of smoking status on the pharmacokinetics and pharmacodynamics of clopidogrel and prasugrel: the PARADOX study. J Am Coll Cardiol. (2013) 62:505–12. doi: 10.1016/j.jacc.2013.03.037
31. Ramotowski B, Gurbel PA, Tantry U, Bracha JS, Karazniewicz-Łada M, Lewandowski Z, et al. Effect of smoking cessation on the pharmacokinetics and pharmacodynamics of clopidogrel after PCI: the smoking cessation paradox study. Thromb Haemost. (2020) 120:449–56. doi: 10.1055/s-0039-3402758
32. Park KW, Kang SH, Kang J, Jeon KH, Park JJ, Han JK, et al. Enhanced clopidogrel response in smokers is reversed after discontinuation as assessed by VerifyNow assay: additional evidence for the concept of 'smokers' paradox'. Heart. (2012) 98:1000–6. doi: 10.1136/heartjnl-2011-301565
33. Kim YG, Suh JW, Kang SH, Park JJ, Yoon CH, Cho YS, et al. Cigarette smoking dose not enhance clopidogrel responsiveness after adjusting VerifyNow P2Y12 reaction units for the influence of hemoglobin level. JACC Cardiovasc Interv. (2016) 9:1680–90. doi: 10.1016/j.jcin.2016.05.036
34. Fox KM EURopean EURopean trial On reduction of cardiac events with Perindopril in stable coronary Artery disease Investigators. Efficacy of perindopril in reduction of cardiovascular events among patients with stable coronary artery disease: Randomized, double-blind, placebo-controlled, multicenter trial (the EUROPA study). Lancet. (2003) 362:782–8. doi: 10.1016/S0140-6736(03)14286-9
35. Heart Outcomes Prevention Evaluation Study Investigators, Yusuf S, Sleight P, Pogue J, Bosch J, Davies R, et al. Effects of an angiotensin-converting-enzyme inhibitor, ramipril on cardiovascular events in high-risk patients. N Engl J Med. (2000) 342:145–53. doi: 10.1056/NEJM200001203420301
Keywords: percutaneous coronary intervention, smoker's paradox, stable coronary artery disease, risk factors, long-term outcome
Citation: Wu H-P, Jan S-L, Chang S-L, Huang C-C and Lin M-J (2022) Correlation Between Smoking Paradox and Heart Rhythm Outcomes in Patients With Coronary Artery Disease Receiving Percutaneous Coronary Intervention. Front. Cardiovasc. Med. 9:803650. doi: 10.3389/fcvm.2022.803650
Received: 28 October 2021; Accepted: 03 January 2022;
Published: 11 February 2022.
Edited by:
Tommaso Gori, Johannes Gutenberg University Mainz, GermanyReviewed by:
Afshin Shoeibi, K. N. Toosi University of Technology, IranEric Chong, Farrer Park Hospital, Singapore
Copyright © 2022 Wu, Jan, Chang, Huang and Lin. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Mao-Jen Lin, ZXNpb245N0B5YWhvby5jb20udHc=
†These authors have contributed equally to this work
 Han-Ping Wu
Han-Ping Wu Sheng-Ling Jan
Sheng-Ling Jan Shih-Lin Chang5,7
Shih-Lin Chang5,7