- 1Department of Scientific Research and Education, The Second People's Hospital of Foshan, Foshan, China
- 2Department of Cardiology, The Second People's Hospital of Foshan, Foshan, China
- 3Department of Orthopedics, The Second People's Hospital of Foshan, Foshan, China
Background: HF and osteoporosis shared many common etiological risk factors. However, studies exploring whether patients with HF were associated with a higher risk of osteoporotic fracture resulted in inconsistent findings. This meta-analysis aimed to summarize the association between HF and the risk of incident fracture.
Methods: Following the Meta-analysis of Observational Studies in Epidemiology group recommendations, we searched multiple electronic databases (PubMed, Cochran Library, and EMBASE) for related studies from inception to April 30, 2021. Studies evaluating the risk of incident fracture in patients with HF compared with those without HF were included for analysis. The random-effects models were used to combine the estimated hazard ratios (HRs) of incident fracture associated with HF.
Results: We included 8 observational studies for meta-analysis. The sample size ranged from 5,613 to 87,748 participants, with a total of 260,410 participants included. The median follow-up duration was 5.0 years. Random-effects model analyses showed that compared with control groups, patients with HF were associated with a higher risk of all incident fractures (HR = 1.67, 95% CI = 1.30–2.16, P < 0.001) and hip fracture (HR = 2.20, 95% CI = 1.28–3.77, P < 0.001). The risk of all incident fractures was increased in all subgroup analyses according to age, sample size, sex, and follow-up duration.
Conclusions: Patients with HF were associated with a higher risk of incident fracture, as well as hip fracture.
Introduction
With a growing aging population world, heart failure (HF) has become a growing global public health burden. It was estimated that there were more than 37.7 million HF patients globally (1, 2). HF is a disabling clinical syndrome with high rates of morbidity and mortality (3, 4). In the past decades, significant progress had been achieved in the treatment of HF, and the life expectancy of HF patients had been improved. However, they are more prone to develop many age-related complications, such as dementia, venous thromboembolism and fracture (5–7). Therefore, better determination of the association between HF and the risk of these chronic morbidities would be helpful for the medical care of patients with HF.
Fractures, especially osteoporotic fractures, may share some common risk factors for HF, such as aging, diabetes mellitus, cigarette smoking, and menopause (5, 8). Recently, epidemiological data have shown that in patients with HF, the prevalence of fractures is higher than that in those without HF (9, 10). However, some cohort studies showed that there was a positive association between HF and risk of incident fractures (11–13), however, others did not show a significant association (14, 15). Furthermore, the most devastating complication of osteoporosis is hip fracture; which was associated with high complications and mortality (16, 17), while the risk of hip fracture in patients with HF was still controversial.
To address these inconsistent data, we conducted this study, pooling data from available observational studies to summarize the association between HF and the risk of incident fracture.
Methods
Search strategies and study selection criteria
We performed this meta-analysis following the Meta-analysis of Observational Studies in Epidemiology (MOOSE) group recommendations (18) and searched the electronic databases (PubMed, Cochran Library, and EMBASE) for potentially related studies from inception to April 30, 2021. The combined text and MeSH heading search strategies were used, with terms related to “fracture” and “heart failure”. No language and publication form restrictions were used. The strategy for searching PubMed is presented in Supplementary Table 1.
Two researchers from our team independently reviewed the extracted articles and included studies for meta-analysis if they met the underlying inclusion criteria: 1. Observational studies with adult participants (aged ≥18 years); 2. Studies evaluated the risk of incident fracture in patients with HF compared with those without HF; 3. The risk of fracture associated with HF should be adjusted for confounding factors.
The exclusion criteria were: 1. The association between HF and fracture was only reported in cross-sectional design; 2. Studies with a follow-up duration <1 year. If there were duplicated reports using data from the same observational study, we only included the latest published data for meta-analysis.
Extraction of the data and study quality assessment
Extraction of the data was conducted by two researchers independently. We extracted key information from the studies, including country, publication year, author, study design, study sample, mean/median age, sex proportion, HF and control cases, follow-up duration, and outcomes.
We used the Newcastle–Ottawa Quality Assessment Scale (NOS) for observational cohort studies to evaluate the quality of the included studies (19). In brief, the NOS assessed the study quality based on the following features: selection (3 items, up to 3 scores in total), comparability (1 item, up to 2 scores) and exposure/outcome (3 items, up to 3 scores in total). Therefore, the total score ranged from 0 to 9 based on the NOS evaluation. In this study, we defined included studies as good (≥7 scores), fair (4–6 scores) or poor quality (<4 scores), respectively (20–22).
Statistical analysis
All the statistical analyses were performed using RevMan 5.3 (The Cochrane Collaboration, Copenhagen, Denmark). The primary outcome in our study was defined as the risk of any fractures associated with HF compared with the participants. The secondary outcome was the risk of hip fracture. Multivariable adjusted hazard ratios (HRs) were extracted for pooled analysis. If the adjusted HRs were reported based on multiple different statistical models, we used the data which adjusted the most comprehensive confounders for analysis. We combined the HRs and their standard errors using the inverse variance approach. If the risk of fractures was reported as risk ratios (RRs), these data are considered approximate HRs (23). In cases where the odds ratios (ORs) were reported, they were converted to RRs by the following formula: RR = OR/([1 – pRef] + [pRef × OR]), where pRef is defined as the prevalence of the outcome (fractures) in the reference group (control group) (23, 24). The random-effects models were used to combine the log HRs and their corresponding standard errors. The I2 statistics were used to test the heterogeneity among the included studies, and a value of I2 > 50% was an indication of significant heterogeneity.
Publication bias of the primary and secondary outcomes was assessed by inspecting funnel plots. We performed the sensitivity analyses by changing the random-effects model to the fixed-effects model in the meta-analysis. Furthermore, the pooled HRs were recalculated by excluding one study at a time to determine the effects of each study on the results. We also performed subgroup analyses of the primary outcome according to sex, age, sample size, and follow-up duration. All P-values are two-tailed, and a P-value < 0.05 was considered with statistical significance.
Results
Key characteristics of the included studies
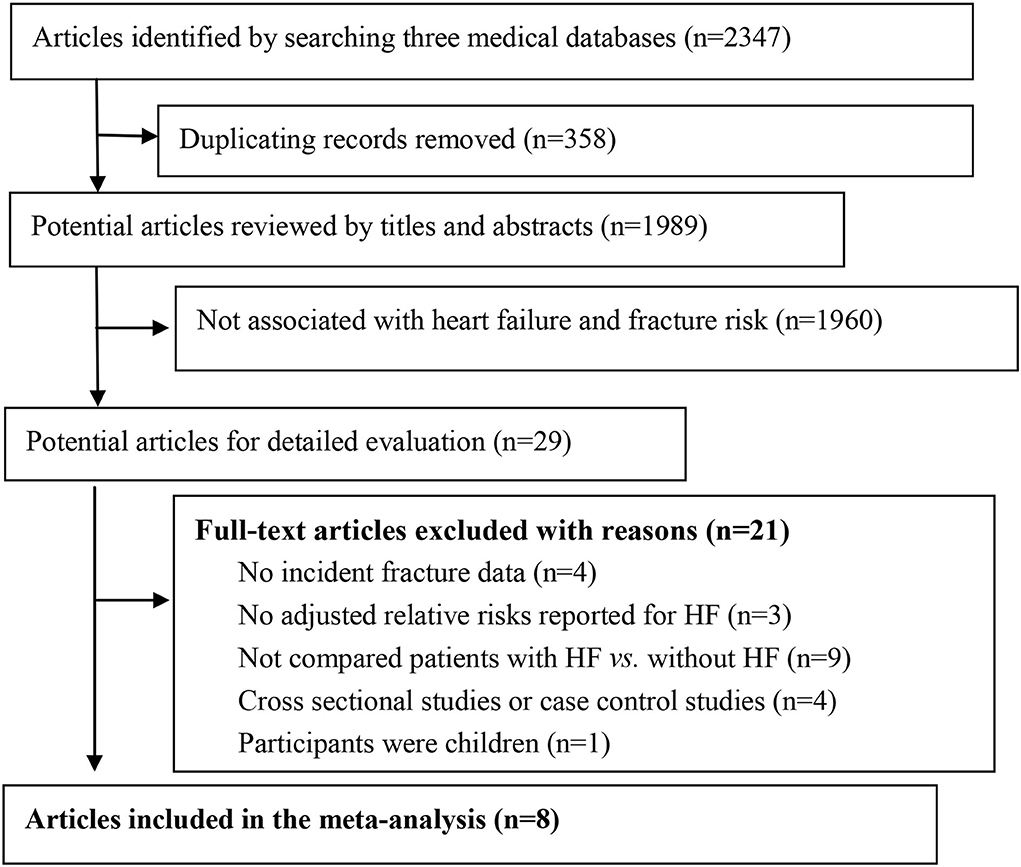
The flow of study selection for meta-analysis was presented in Figure 1. After searching the electronic databases, we identified 2,347 potential articles. After excluding duplication items, we screened the titles and abstracts, and reviewed 29 full texts to identify related studies. Finally, we excluded 21 studies according to predefined exclusion criteria (Supplementary Table 2), and included 8 studies for meta-analysis. In the included studies, 2 of them were nest case–control studies, and 6 were cohort studies (11–15, 25–27). The main characteristics of these studies are shown in Table 1. One study was from China, and all the other 7 studies were from Europe or USA. The sample size ranged from 5,613 to 87,748 participants, with a total of 260,410 participants included. The median follow-up duration was 5.0 years (ranging from 1.0 to 35.0 years). According to our predefined quality assessment criteria using NOS, 6 of the included studies were defined as good quality (>7 scores), and 2 of them were defined as fair quality (both with 6 scores), respectively. The adjusted confounders in the included studies are presented in Supplementary Table 3.
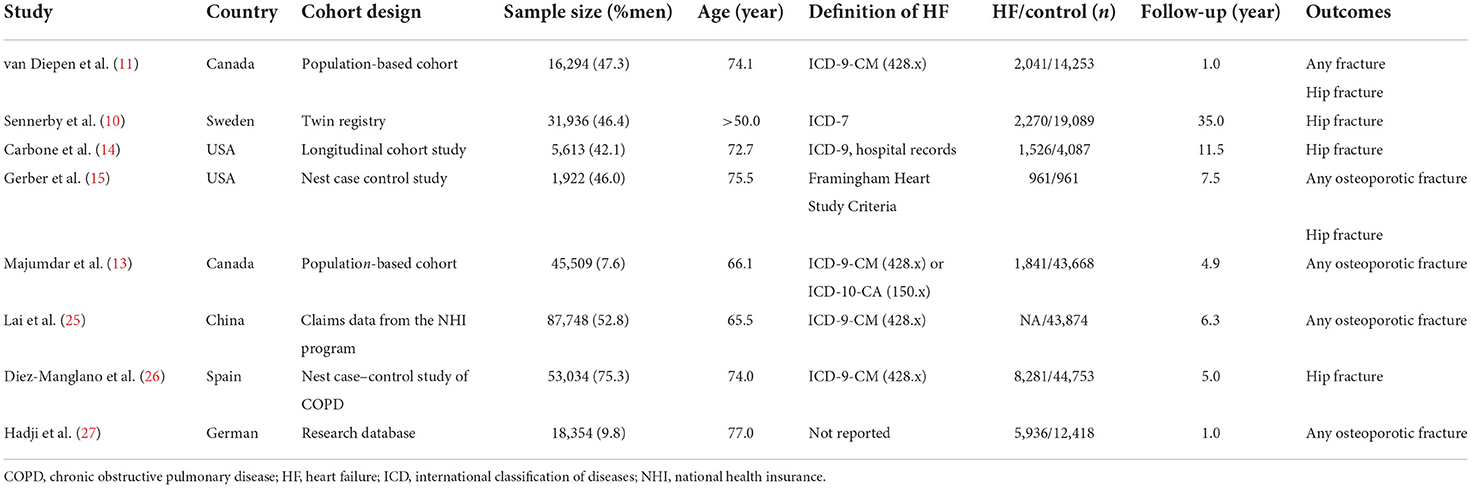
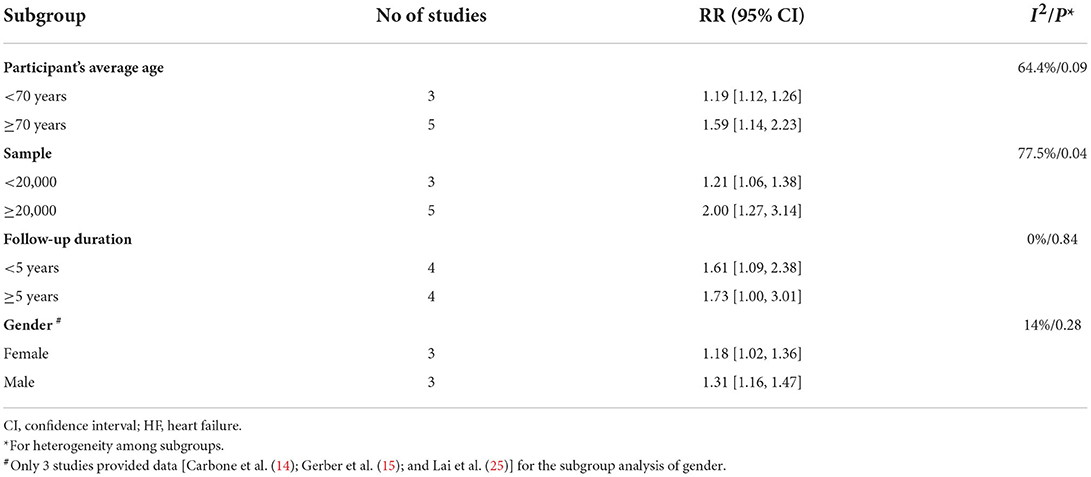
Table 1. Baseline characteristics of the included studies exploring the risk of fracture associated with HF.
Primary outcome
There was significant heterogeneity observed among the included studies for the association between baseline HF and—risk of any fractures (I2 = 95%, P < 0.001). Random-effects model analyses showed that compared with control groups, patients with HF were associated with a higher risk of incident fractures in follow-up duration (HR = 1.67, 95% CI = 1.30–2.16, P < 0.001; Figure 2). By inspection of the funnel plot, we did not observe significant publication bias (Supplementary Figure 1). The sensitivity analyses confirmed that the results were not significantly changed by changing the random-effects models with the fixed-effects models for analysis, or excluding one study at a time to recalculate the results.
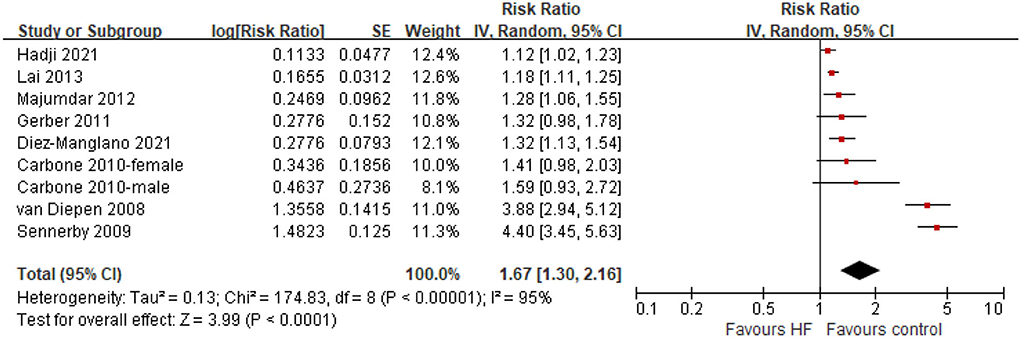
Figure 2. Forest plot of comparison: HF vs. control, outcome: all fractures. CI, confidence interval; HF, heart failure.
The results of the subgroup analyses were shown in Table 2. The risk of fractures was increased in all subgroup analyses according to age, sample size, sex, and follow-up duration (HR range from 1.18 to 2.0).
Secondary outcome
Five studies provided data for the meta-analysis of the hip fracture in HF patients. Significant heterogeneity was observed among these studies (I2 = 94%, P < 0.001). Random-effects model analyses showed that compared with control groups, patients with HF were associated with a higher risk of hip fracture (HR = 2.20, 95% CI = 1.28–3.77, P < 0.001; Figure 3). No significant publication bias was observed (Supplementary Figure 2). Similarly, sensitivity analyses confirmed that the results were not significantly changed by changing the statistical models, or excluding one study at a time. We did not perform subgroup analyses due to the limited number of the available studies.
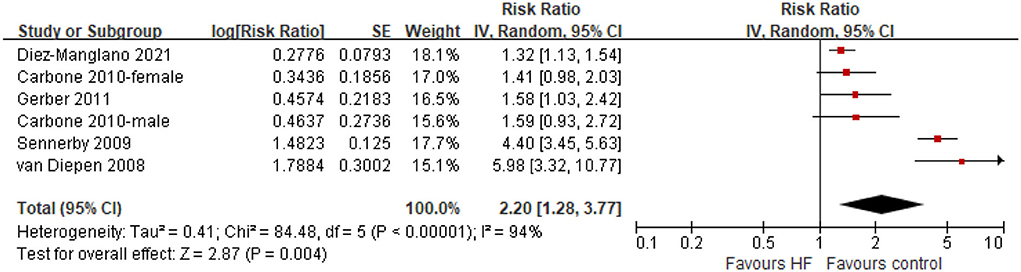
Figure 3. Forest plot of comparison: HF vs. control, outcome: hip fractures. CI, confidence interval; HF, heart failure.
Discussion
In this comprehensive meta-analysis, we included 8 observational studies, comprising a total of 260,410 participants for analysis. We found that after a median follow-up duration of 5.0 years, patients with HF were associated with a higher risk of any incident fracture, as well as hip fracture. The results were consistent among multiple subgroup comparisons.
Several underlying pathophysiological mechanisms had been advocated to explain the link between HF and osteoporotic fractures. It was well known that HF and osteoporosis shared many etiological risk factors, including older age, diabetes, renal insufficiency, cigarette smoking and physical inactivity (5). The pathophysiological change, such as activation of the renin angiotensin aldosterone system, increased levels of oxidative stress and inflammatory cytokines, vitamin D deficiency, hyperparathyroidism, and reduced tissue perfusion in HF may further increase the risk of osteoporosis, and fractures (8, 28, 29). Furthermore, some medications used to treat HF may affect bone health and fracture risk, especially loop diuretics, which had been reported to be associated with loss of bone mineral density and increased fracture risk (30). Interestingly, a large cohort study with 31,936 Swedish twins showed that the risk of hip fracture risk was increased in the co-twin analyses, especially in identical twins, indicated that genes predispose to the development of CVD and fractures (11).
Our study was in line with a previously published meta-analysis by Ge et.al, which showed that the risk of any fractures (RR 1.66, 95% CI 1.14–2.43) and hip fracture (RR 3.45, 95% CI 1.86–6.40) were higher in patients diagnosed with HF compared with that in controls (31). However, to better explore the relationship between HF and fractures, we only included cohort studies with multi-variable adjustment for analysis, and excluded the cross-sectional studies. Furthermore, we included the most recently published data which allow us to generate multiple subgroups analyses, further supporting the findings.
There are some indications for clinical practice from our study. Both HF and osteoporotic fractures are highly prevalent in the aging society. They are common causes of disability, hospitalizations, and mortality, causing a heavy public burden to the health system and society. However, current academic guidelines for the management of treatment of HF do not propose clearly suggestions for screening, prevention and management of osteoporosis or osteoporotic fracture in patients with HF (32, 33). Based on the significant association between HF and incident fractures documented in our study, we propose that future HF guidelines should consider covering this important issue. For clinical physicians taking care of HF patients, better attention should be paid to bone health and amelioration of osteoporotic fracture risk. It was known that increased physical activity and smoking cessation can improve bone health and had been proposed in osteoporosis guidelines (34). In patients with HF, such lifestyle changes were also important to improve the life quality and outcomes. Future studies are needed to test the efficacy and safety of anti-osteoporosis drugs in patients with HF.
Several major strengths should be noted in our study. First, we only included studies which had adjusted for multiple confounding factors for analysis. Therefore, the association between HF and the increased risk of fractures could not be attributed to the effect of potential confounders or shared common risk factors. Second, although there was significant heterogeneity observed among the included studies for the association between baseline HF and risk of any fractures, the risk of fractures was increased in all subgroup analyses according to age, sample size, sex, and follow-up duration, which further supported the conclusion in our study. However, several limitations in the current study should be acknowledged. First, due to the observational design of the included studies, we cannot establish a causation relationship between HF and fractures. Furthermore, 7 of the included studies were from Europe or USA, and only one study was from China. Therefore, the association between HF and risk of fracture could not be generalized to other populations. Second, different medicines for the treatment of HF may have different effects on osteoporosis, and further affect the risk of fractures. However, the treatment strategies in these HF cohorts were not adjusted. Third, some important risk factors for fractures were not evaluated and adjusted, such as levels of 25 hydroxy vitamin D and bone mineral density. Only one study reported the adjustment of anti-osteoporosis medication (27). Therefore, unadjusted confounders might have affected the results.
Conclusion
Patients with HF were associated with a higher risk of incident fracture, as well as hip fracture during follow-up. Better attention should be paid to ameliorating the risk of osteoporotic fracture in the management of HF.
Data availability statement
The original contributions presented in the study are included in the article/Supplementary material, further inquiries can be directed to the corresponding authors.
Author contributions
X-pL, X-yJ, J-dW, and Y-QL: research idea and study design. X-pL, X-yJ, J-dW, and D-lL: data acquisition. J-dW and J-xW: data analysis/interpretation. X-PL, X-yJ, and J-dW: statistical analysis. J-dW and Y-QL: supervision and mentorship. All authors contributed important intellectual content during manuscript drafting or revision and accept accountability for the overall work by ensuring that questions pertaining to the accuracy or integrity of any portion of the work are appropriately investigated and resolved.
Conflict of interest
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
Publisher's note
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
Supplementary material
The Supplementary Material for this article can be found online at: https://www.frontiersin.org/articles/10.3389/fcvm.2022.977082/full#supplementary-material
References
1. Bui AL, Horwich TB, Fonarow GC. Epidemiology and risk profile of heart failure. Nat Rev Cardiol. (2011) 8:30–41. doi: 10.1038/nrcardio.2010.165
2. Vos T, Flaxman AD, Naghavi M, Lozano R, Michaud C, Ezzati M, et al. Years lived with disability (YLDs) for 1,160 sequelae of 289 diseases and injuries 1990–2010: a systematic analysis for the global burden of disease study 2010. Lancet. (2012) 380:2163–96. doi: 10.1016/S0140-6736(12)61729-2
3. Wu J, Zheng H, Liu X, Chen P, Zhang Y, Luo J, et al. Prognostic value of secreted frizzled-related protein 5 in heart failure patients with and without type 2 diabetes mellitus. Circ Heart Fail. (2020) 13:e7054. doi: 10.1161/CIRCHEARTFAILURE.120.007054
4. Li W, Huang A, Zhu H, Liu X, Huang X, Huang Y, et al. Gut microbiota-derived trimethylamine N-oxide is associated with poor prognosis in patients with heart failure. Med J Aust. (2020) 213:374–9. doi: 10.5694/mja2.50781
5. Loncar G, Cvetinovic N, Lainscak M, Isakovic A, von Haehling S. Bone in heart failure. J Cachexia Sarcop Muscle. (2020) 11:381–93. doi: 10.1002/jcsm.12516
6. Xu T, Huang Y, Liu Z, Bai Y, Ma Z, Cai X, et al. Heart failure is associated with increased risk of long-term venous thromboembolism. Korean Circ J. (2021) 51:766–80. doi: 10.4070/kcj.2021.0213
7. Blach A, Pangle A, Azhar G, Wei J. Disparity and multimorbidity in heart failure patients over the age of 80. Gerontol Geriatr Med. (2022) 8:1682825323. doi: 10.1177/23337214221098901
8. Aluoch AO, Jessee R, Habal H, Garcia-Rosell M, Shah R, Reed G, et al. Heart failure as a risk factor for osteoporosis and fractures. Curr Osteoporos Rep. (2012) 10:258–69. doi: 10.1007/s11914-012-0115-2
9. Mazziotti G, Baracca M, Doga M, Porcelli T, Vescovi PP, Giustina A. Prevalence of thoracic vertebral fractures in hospitalized elderly patients with heart failure. Eur J Endocrinol. (2012) 167:865–72. doi: 10.1530/EJE-12-0566
10. Sennerby U, Farahmand B, Ahlbom A, Ljunghall S, Michaelsson K. Cardiovascular diseases and future risk of hip fracture in women. Osteoporos Int. (2007) 18:1355–62. doi: 10.1007/s00198-007-0386-0
11. van Diepen S, Majumdar SR, Bakal JA, McAlister FA, Ezekowitz JA. Heart failure is a risk factor for orthopedic fracture: a population-based analysis of 16,294 patients. Circulation. (2008) 118:1946–52. doi: 10.1161/CIRCULATIONAHA.108.784009
12. Sennerby U, Melhus H, Gedeborg R, Byberg L, Garmo H, Ahlbom A, et al. Cardiovascular diseases and risk of hip fracture. JAMA. (2009) 302:1666–73. doi: 10.1001/jama.2009.1463
13. Majumdar SR, Ezekowitz JA, Lix LM, Leslie WD. Heart failure is a clinically and densitometrically independent risk factor for osteoporotic fractures: population-based cohort study of 45,509 subjects. J Clin Endocrinol Metab. (2012) 97:1179–86. doi: 10.1210/jc.2011-3055
14. Carbone L, Buzkova P, Fink HA, Lee JS, Chen Z, Ahmed A, et al. Hip fractures and heart failure: findings from the cardiovascular health study. Eur Heart J. (2010) 31:77–84. doi: 10.1093/eurheartj/ehp483
15. Gerber Y, Melton LR, Weston SA, Roger VL. Osteoporotic fractures and heart failure in the community. Am J Med. (2011) 124:418–25. doi: 10.1016/j.amjmed.2010.11.029
16. Wurdemann FS, Krijnen P, van Zwet EW, Arends AJ, Heetveld MJ, Trappenburg MC, et al. Trends in data quality and quality indicators 5 years after implementation of the Dutch hip fracture audit. Eur J Trauma Emerg Surg. (2022) 2022:1–14. doi: 10.1007/s00068-022-02012-y
17. Tai TW, Hwang JS Li CC, Hsu JC, Chang CW, Wu CH. The impact of various anti-osteoporosis drugs on all-cause mortality after hip fractures: a nationwide population study. J Bone Miner Res. (2022) 37:1520–6. doi: 10.1002/jbmr.4627
18. Stroup DF, Berlin JA, Morton SC, Olkin I, Williamson GD, Rennie D, et al. Meta-analysis of observational studies in epidemiology: a proposal for reporting. Meta-analysis of observational studies in epidemiology (MOOSE) group. JAMA. (2000) 283:2008–12. doi: 10.1001/jama.283.15.2008
19. Wells GA, Shea B, O'Connell D, Peterson J, Welch V, Losos M. The Newcastle-Ottawa Scale (NOS) for Assessing the Quality of Nonrandomised Studies in Meta-Analyses. Ottawa, ON: Ottawa Hospital Research Institute (2010). Available online at: http://www.ohri.ca/programs/clinical_epidemiology/oxford.asp (accessed June 1, 2010).
20. Cai X, Zheng S, Liu Y, Zhang Y, Lu J, Huang Y. Nonalcoholic fatty liver disease is associated with increased risk of atrial fibrillation. Liver Int. (2020) 40:1594–600. doi: 10.1111/liv.14461
21. Zheng S, Qiu M, Wu J, Pan XF, Liu X, Sun L, et al. Long-chain omega-3 polyunsaturated fatty acids and the risk of heart failure. Ther Adv Chronic Dis. (2022) 13:374130192. doi: 10.1177/20406223221081616
22. Cai X, Liu X, Sun L, He Y, Zheng S, Zhang Y, et al. Prediabetes and the risk of heart failure: a meta-analysis. Diabetes Obes Metab. (2021) 23:1746–53. doi: 10.1111/dom.14388
23. Yang Y, Li W, Zhu H, Pan XF, Hu Y, Arnott C, et al. Prognosis of unrecognised myocardial infarction determined by electrocardiography or cardiac magnetic resonance imaging: systematic review and meta-analysis. BMJ. (2020) 369:m1184. doi: 10.1136/bmj.m1184
24. Mai L, Wen W, Qiu M, Liu X, Sun L, Zheng H, et al. Association between prediabetes and adverse outcomes in heart failure. Diabetes Obes Metab. (2021) 23:2476–83. doi: 10.1111/dom.14490
25. Lai SW, Liao KF, Lai HC, Tsai PY, Lin CL, Chen PC, et al. Risk of major osteoporotic fracture after cardiovascular disease: a population-based cohort study in Taiwan. J Epidemiol. (2013) 23:109–14. doi: 10.2188/jea.JE20120071
26. Diez-Manglano J, Berges VM, Martinez BL, Poblador-Plou B, Gimeno-Miguel A, Martinez HP, et al. Chronic obstructive pulmonary disease and incidence of hip fracture: a nested case-control study in the EpiChron cohort. Int J Chron Obstruct Pulmon Dis. (2020) 15:2799–806. doi: 10.2147/COPD.S270713
27. Hadji P, Schweikert B, Kloppmann E, Gille P, Joeres L, Toth E, et al. Osteoporotic fractures and subsequent fractures: imminent fracture risk from an analysis of German real-world claims data. Arch Gynecol Obstet. (2021) 304:703–12. doi: 10.1007/s00404-021-06123-6
28. Carbone LD, Cross JD, Raza SH, Bush AJ, Sepanski RJ, Dhawan S, et al. Fracture risk in men with congestive heart failure risk reduction with spironolactone. J Am Coll Cardiol. (2008) 52:135–8. doi: 10.1016/j.jacc.2008.03.039
29. Carbone LD, Vasan S, Prentice RL, Harshfield G, Haring B, Cauley JA, et al. The renin-angiotensin aldosterone system and osteoporosis: findings from the Women's Health Initiative. Osteoporos Int. (2019) 30:2039–56. doi: 10.1007/s00198-019-05041-3
30. Heo JH, Rascati KL, Lopez KN, Moffett BS. Increased fracture risk with furosemide use in children with congenital heart disease. J Pediatr. (2018) 199:92–8. doi: 10.1016/j.jpeds.2018.03.077
31. Ge G, Li J, Wang Q. Heart failure and fracture risk: a meta-analysis. Osteoporos Int. (2019) 30:1903–9. doi: 10.1007/s00198-019-05042-2
32. McDonagh TA, Metra M, Adamo M, Gardner RS, Baumbach A, Bohm M, et al. 2021 ESC Guidelines for the diagnosis and treatment of acute and chronic heart failure: developed by the task force for the diagnosis and treatment of acute and chronic heart failure of the European Society of Cardiology (ESC). With the special contribution of the Heart Failure Association (HFA) of the ESC. Eur J Heart Fail. (2022) 24:4–131. doi: 10.1093/eurheartj/ehab368
33. Heidenreich PA, Bozkurt B, Aguilar D, Allen LA, Byun JJ, Colvin MM, et al. 2022 AHA/ACC/HFSA guideline for the management of heart failure: a report of the American College of Cardiology/American Heart Association joint committee on clinical practice guidelines. J Am Coll Cardiol. (2022) 79:e263–421. doi: 10.1161/CIR.0000000000001063
Keywords: heart failure, risk, osteoporosis, osteoporotic fracture, hip fracture
Citation: Liu X-p, Jian X-y, Liang D-l, Wen J-x, Wei Y-h, Wu J-d and Li Y-Q (2022) The association between heart failure and risk of fractures: Pool analysis comprising 260,410 participants. Front. Cardiovasc. Med. 9:977082. doi: 10.3389/fcvm.2022.977082
Received: 27 June 2022; Accepted: 27 September 2022;
Published: 14 October 2022.
Edited by:
Alberto Palazzuoli, University of Siena, ItalyReviewed by:
Luigi Gennari, University of Siena, ItalyAnne Pizard, INSERM U955 Institut Mondor de Recherche Biomédicale (IMRB), France
Copyright © 2022 Liu, Jian, Liang, Wen, Wei, Wu and Li. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Jian-di Wu, ZnNkcnd1QDEyNi5jb20=; Yi-Qun Li, bHlxMjcwM0AxMjYuY29t
†These authors have contributed equally to this work and share first authorship
 Xiao-peng Liu1†
Xiao-peng Liu1† Jian-di Wu
Jian-di Wu