- Department of Cardiology, Dushu Lake Hospital Affiliated to Soochow University, Medical Center of Soochow University, Suzhou Dushu Lake Hospital, Suzhou, China
Background: The treatment of atrial fibrillation (AF) has made significant progress, but the prevention of AF has not received the attention it deserves. A few recent large-sized studies have conducted dose response analysis and reported different conclusions from previous studies on alcohol consumption and AF risk.
Objectives: The aim of this study is to examine the potential non-linear association between alcohol consumption and risk of AF and explore the potential differences of gender.
Methods: In this updated dose-response meta-analysis, PubMed, Embase and Cochrane databases were searched until June 2022. Risk estimates were reported as relative risk (RR) with 95% confidence intervals (CIs). The random-effects restricted cubic spline models are used to evaluate the potential non-linear association between alcohol consumption and AF risk.
Results: A total of 10,151,366 participants with 214,365 cases of AF enrolled in 13 prospective studies. The overall meta-analysis showed that a 1 drink/day increase in alcohol consumption increased the risk of AF by 6% (RR: 1.06; 95% CI: 1.03–1.08). In gender subgroup analysis, pooled results were different between men (RR: 1.08; 95% CI: 1.05–1.11) and women (RR: 1.05; 95% CI: 0.96–1.14). A linear relationship between alcohol consumption and risk of AF was found in men (p = 0.87) while a J-shaped curve was observed in women (p = 0.00). Regional subgroup analysis yielded broadly comparable results in Americas (RR: 1.07; 95% CI: 1.03–1.12), Europe (RR: 1.04; 95% CI: 0.99–1.1) and Asia (RR: 1.07; 95% CI: 0.99–1.14).
Conclusion: The relationship between AF risk and alcohol consumption is linear in men, while a potential non-linear J-shaped relationship is shown in women.
Condensed abstract: We conducted a dose-response meta-analysis on the relationship between alcohol consumption and risk of atrial fibrillation. We merged the data of over 10 million participants and found gender differences in the pattern of association with AF and alcohol consumption. The relationship between AF risk and alcohol consumption is linear in men, while a potential non-linear J-shaped relationship is shown in women. In summary, this research is vital in furthering our understanding of the role of alcohol consumption in new-onset AF, especially among different genders.
Introduction
As the most common clinical arrhythmia, Atrial fibrillation (AF) is influencing over 34 million people worldwide with the increase of risk of stroke, heart failure (HF) and dementia (1, 2), resulting in a tremendous public health burden (3). Although catheter ablation has made substantial progress in the treatment of AF, its prevention has not been given adequate attention. To date, only a few significant risk factors for AF have been identified, like age, male sex, cardiac disease, hypertension, diabetes, obesity and smoking (4). Therefore, the modifiable risk factors that may help reduce the risk of AF must be identified.
There have been several publications (5–8) by far identifying that alcohol has an unambiguous association with AF development, however, some uncertainty may exist over the threshold at which risk is increased. Three previous meta-analyses observed a linear dose-response with an increasing level of alcohol consumption, demonstrating a greater risk of incident AF, and no difference was found between men and women (9–11). Specifically, a study that concluded prospective studies described that the risk of new-onset AF increased by 8% for every 12 g of alcohol intake per day (11). However, several recent studies and the latest meta-analysis failed to demonstrate the link between AF and low to moderate alcohol consumption, and no gender differences was found as well (12–15). A cohort study even suggested using a curvilinear association rather than a linear one to describe this relationship (13). Furthermore, one recent study of more than 9 million participants found the preventive effect of mild drinking on AF (16). Therefore, further research with more focus on alcohol consumption is suggested.
This paper performed an updated dose-response meta-analysis of prospective studies to examine the potential non-linear association of alcohol consumption with the risk of AF and explore the potential gender differences.
Methods
This meta-analysis was conducted based on the guidelines for the Meta-Analysis Of Observational Studies in Epidemiology (MOOSE) (17).
Search strategy
The literature of electronic databases (PubMed, Embase, Cochrane) was methodically and comprehensively searched for eligible studies up to June 2022. The following search strategies were used to retrieve articles in English: ‘atrial fibrillation’ and ‘alcohol’. Further manual collection of references attached to retrieved articles was performed to identify other pertinent studies.
Eligible criteria
The selection was based on the following inclusion criteria: (1) prospective design; (2) at least three types of alcohol consumption were reported; (3) numbers of participants and cases in each type of alcohol consumption were reported; (4) the adjusted relative risk (RR) and the corresponding 95% confidence interval (CI) of incident AF in each type of alcohol consumption were reported.
Study selection and data extraction
After an electronic search of studies, the retrieved articles were selected with analysis of the title, abstract and full texts progressively according to inclusion criteria. The characteristics and data collected from eligible studies included: author, country, year, sex, age, number of cases and participants, follow-up duration, and types of alcohol consumption.
Quality assessment
Quality assessment criteria were used to evaluate the quality of eligible studies based on the Newcastle-Ottawa scale (NOS) (18). The scale gives a maximum of nine points for each study: two for comparability, three for result assessment of outcomes, and four for selection. Studies that scored ≥7 were defined as high quality.
Statistical analysis
STATA version 15.0 was used to perform all statistical analyses. The adjusted RR with corresponding 95% CI for the occurrence of AF in each category of alcohol consumption was considered as the effect size. The I2 statistic was adopted to evaluate the heterogeneity among eligible studies with 25, 50, and 75% representing low, moderate, and high heterogeneity, respectively (19). In addition, subgroup analysis was also performed by sex to explore gender differences. The influence of each study on the overall pooled results was observed using sensitivity analysis. Publication bias was assessed with funnel plots and Egger’s regression tests (20). Subsequently, a two-stage random-effect dose-response meta-analysis was conducted to assess the dose-response relationship between AF and alcohol consumption (11, 21, 22). With a generalized least-squares regression method, an alcohol consumption model was established to restrict cubic splines with three knots (23). The null hypothesis that the coefficient of the second spline is equal to zero was tested for calculating a p-value of non-linearity. The exposure value refers to the midpoint of the corresponding range of alcohol consumption. The lower boundary was set to zero when the lowest type was open. The midpoint was assumed as 1.5 times the upper boundary if the upper boundary for the highest category was not reported. If one drink corresponded to 12 grams of alcohol, alcohol consumption was converted into drinks/day (11).
Results
Literature search
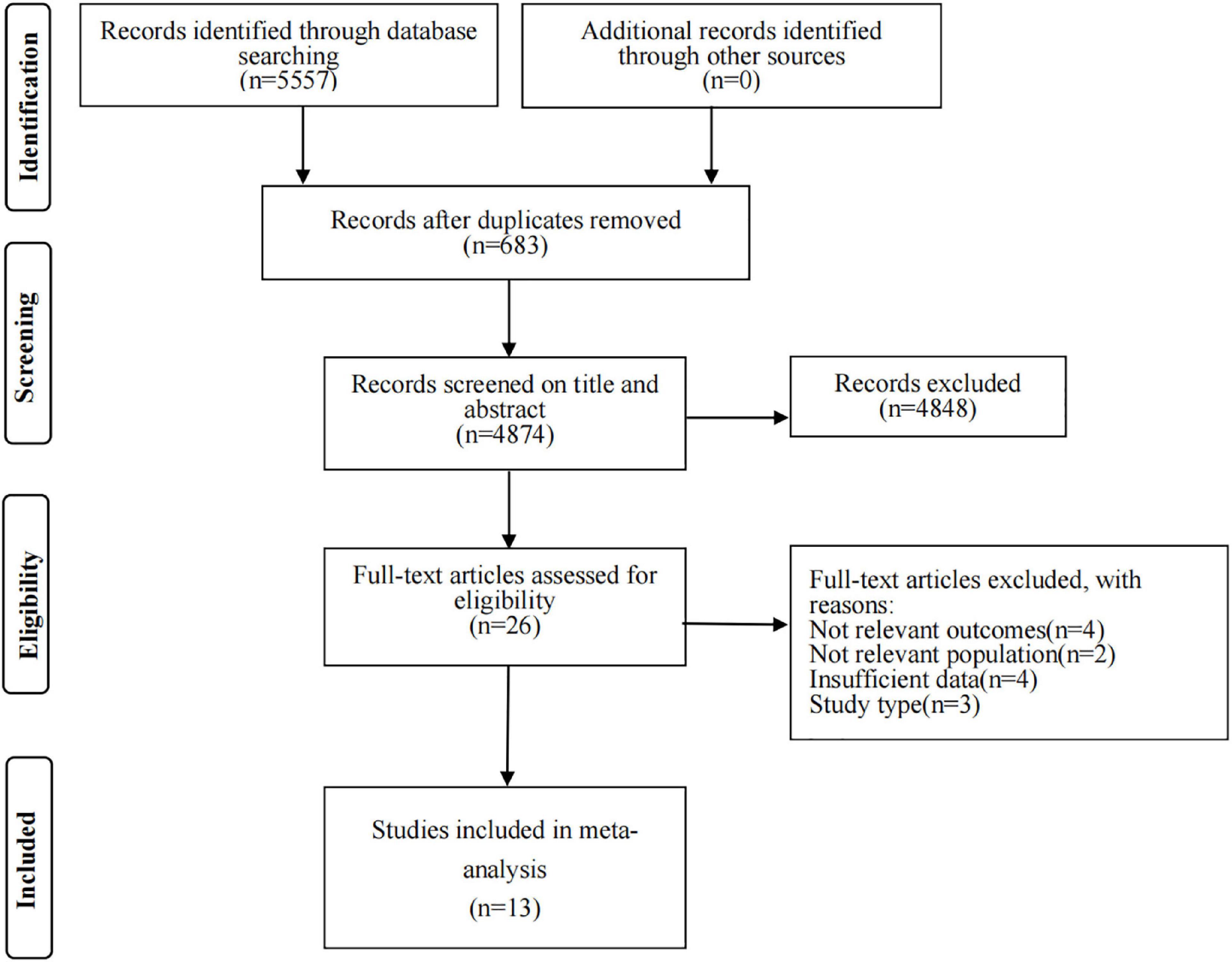
Figure 1 displays a flow chart of the literature search. In short, the initial search strategy retrieved a total of 5,557 citations. After the removal of 683 duplicates, the title and abstract were screened to exclude 4,874 studies. The full-text articles of the remaining 26 citations were screened. Eventually, 13 articles meeting all inclusion criteria were included in the meta-analysis (11–13, 15, 16, 24–31).
Study characteristics
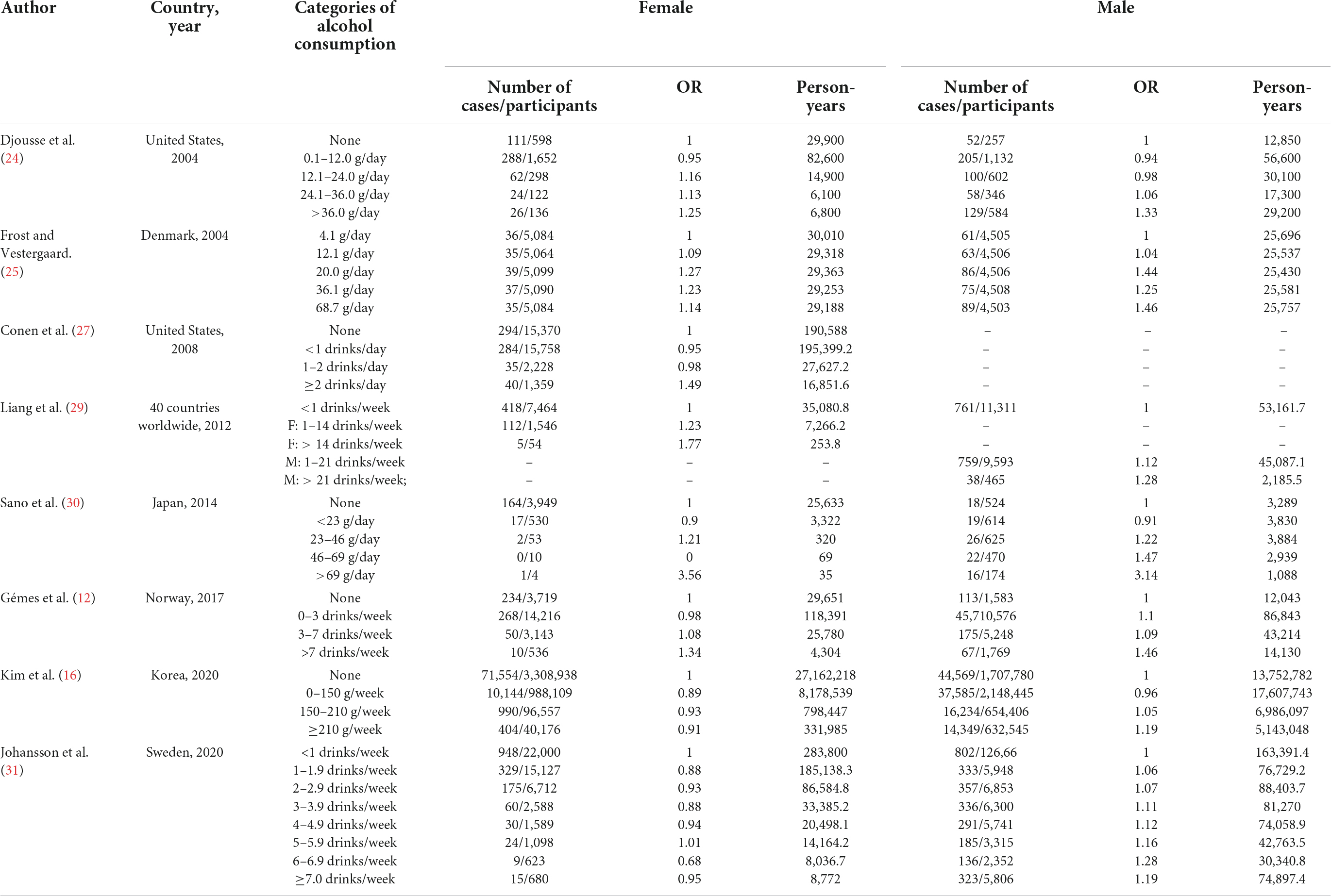
Table 1 shows the characteristics of eligible studies. Overall, 13 prospective articles were included in the final meta-analysis, representing a total of 10,151,366 participants with 214,365 cases of AF. Both men and women were recruited in the majority of studies except one that recruited women only (27). Table 2 displays the key data of eight studies (11, 12, 24, 25, 27–30) included in the sex-subgroup analysis.
Alcohol consumption and atrial fibrillation risk
The overall meta-analysis showed that a 1 drink/day increase in alcohol consumption increased the risk of AF by 6% (RR: 1.06; 95% CI: 1.03–1.08) (Figure 2). There was moderate heterogeneity between studies (I2: 64.0%). Sensitivity analysis (Figure 3) indicated that our results were stable and reliable. Funnel plots (Figure 4) and Egger’s test (p = 0.07) suggested no evidence of publication bias. In subgroup analysis (Figures 5A,B), pooled results were different between men (RR: 1.08; 95% CI: 1.05–1.11) and women (RR: 1.05; 95% CI: 0.96–1.14). Moreover, there was also a linear dose-response association between alcohol consumption and risk of incident AF according to a dose-response meta-analysis (p = 0.7) (Figure 6A). A similar linear relationship was also observed in men (p = 0.87) (Figure 6B). However, a non-linear J-shaped curve was found in women (p = 0.00) with a higher risk of AF at alcohol consumption more than 1.4 drinks/day (Figure 6C). Regional subgroup analysis yielded broadly comparable results, Americas (RR: 1.07; 95% CI: 1.03–1.12), Europe (RR: 1.04; 95% CI: 0.99–1.1) and Asia (RR: 1.07; 95% CI: 0.99–1.14) (Figure 7).
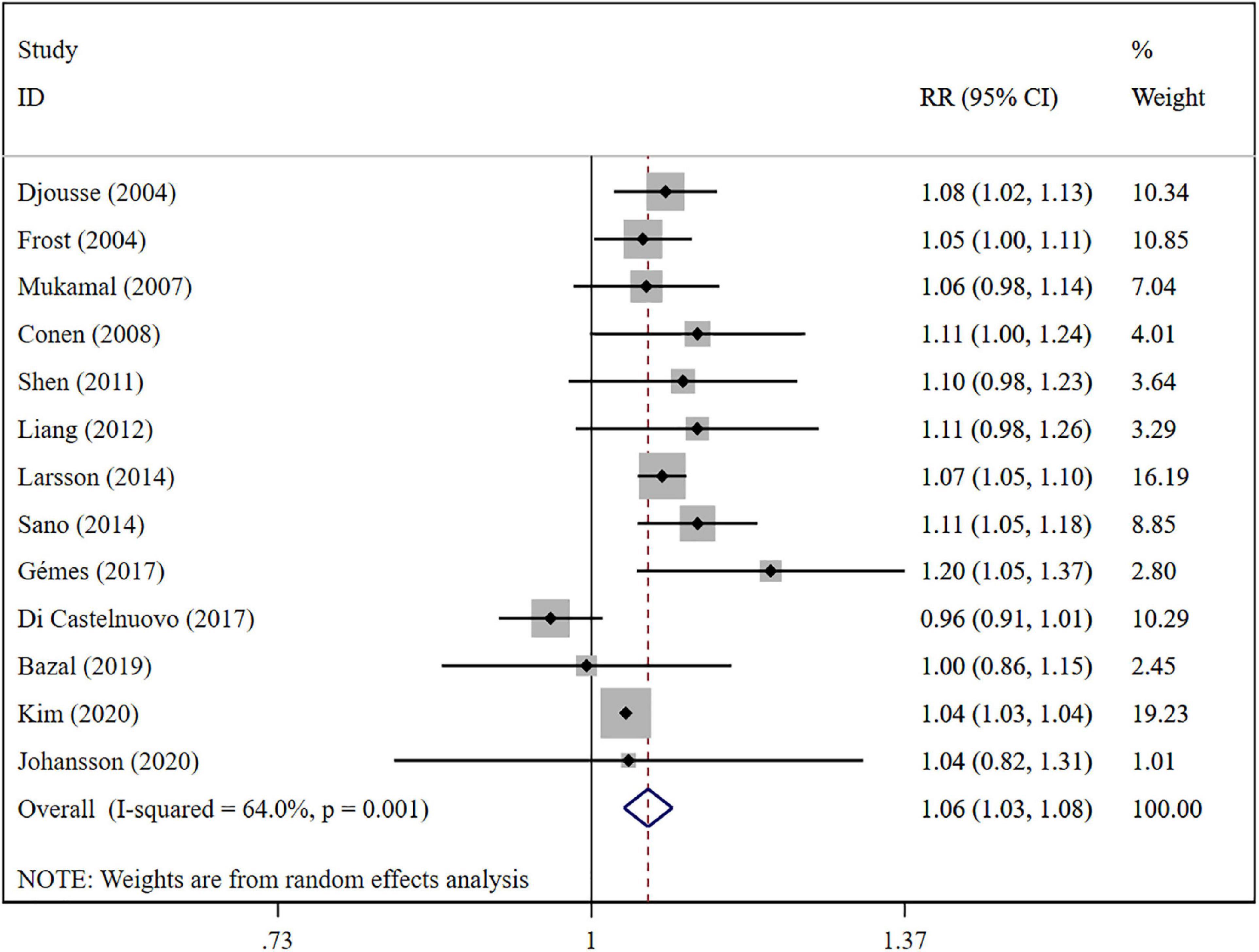
Figure 2. Forest plot of relative risks of atrial fibrillation per 1 drink/day increment in alcohol consumption.
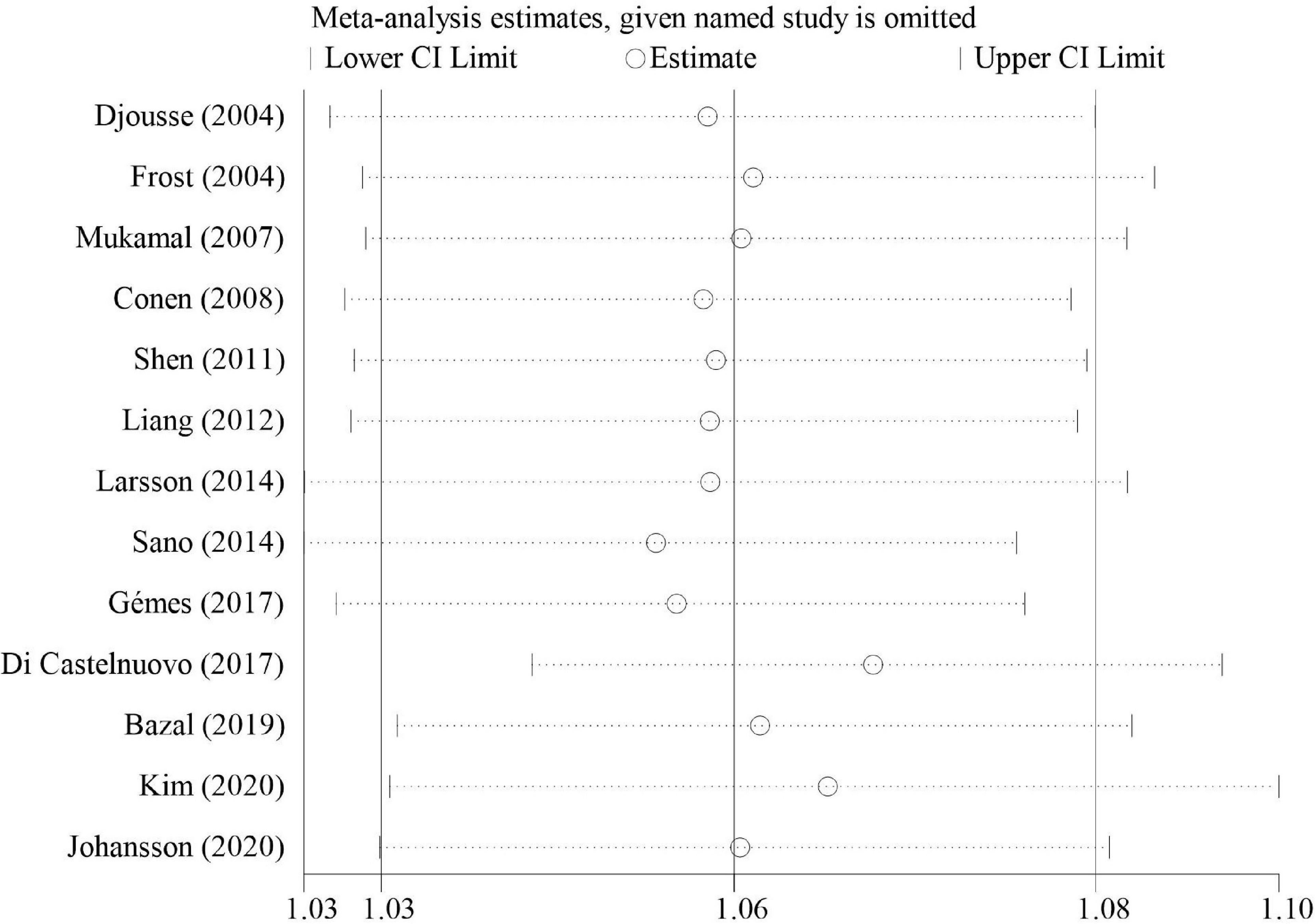
Figure 3. Sensitivity analysis of relative risks of atrial fibrillation per 1 drink/day increment in alcohol consumption.
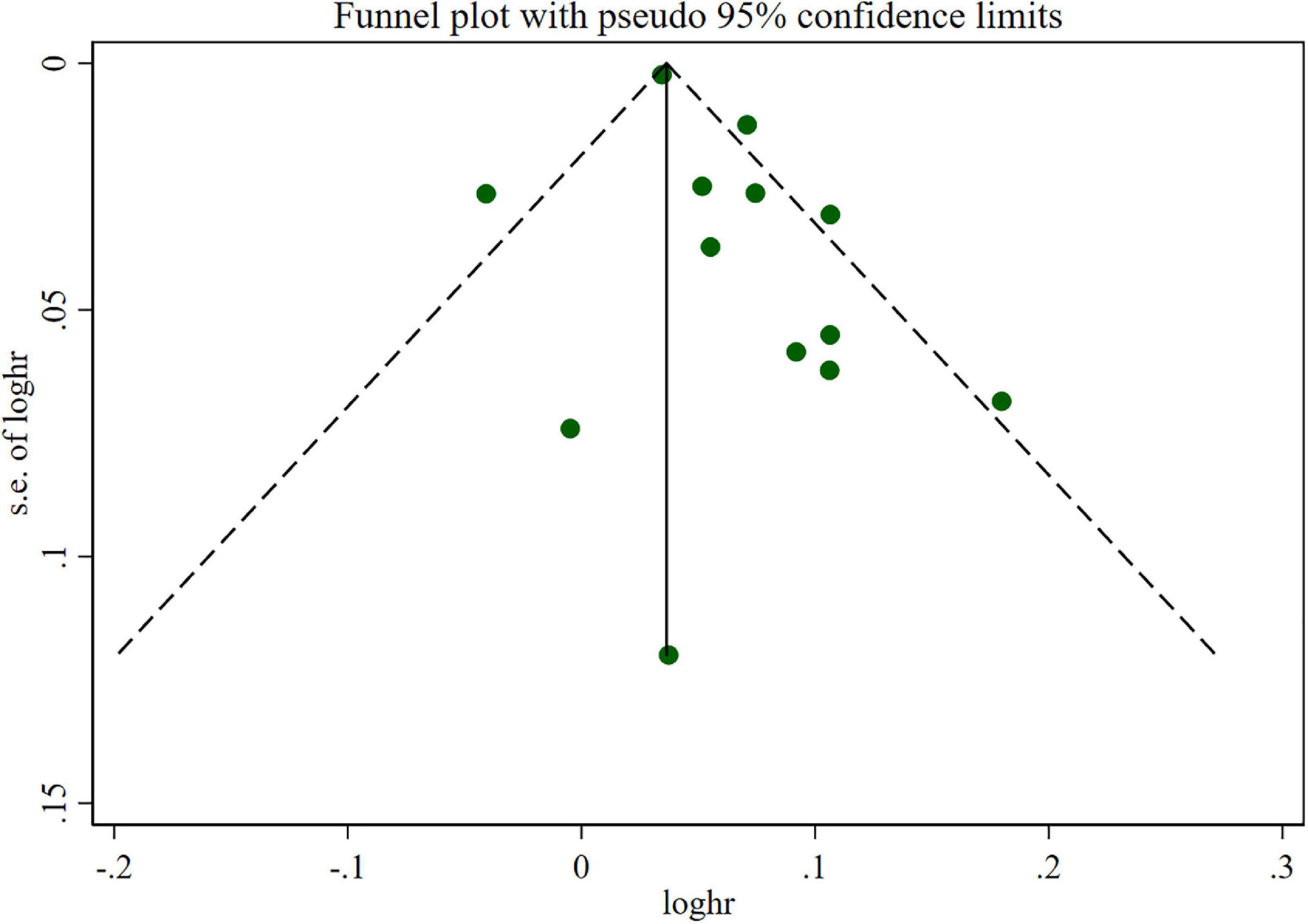
Figure 4. Funnel plots of relative risks of atrial fibrillation per 1 drink/day increment in alcohol consumption.
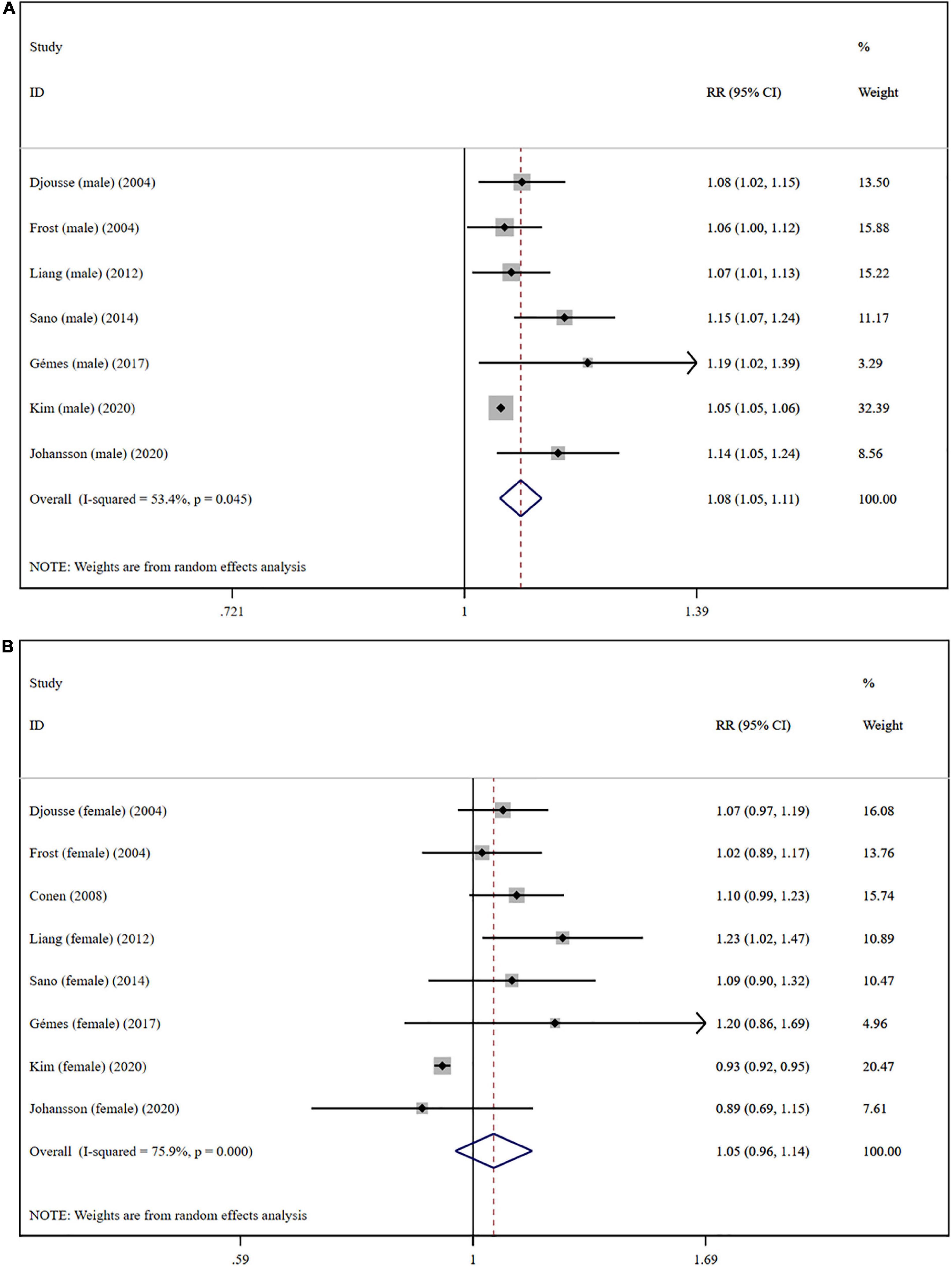
Figure 5. Subgroup analysis of relative risks of atrial fibrillation per 1 drink/day increment in alcohol consumption in different gender. (A) Men; (B) women.
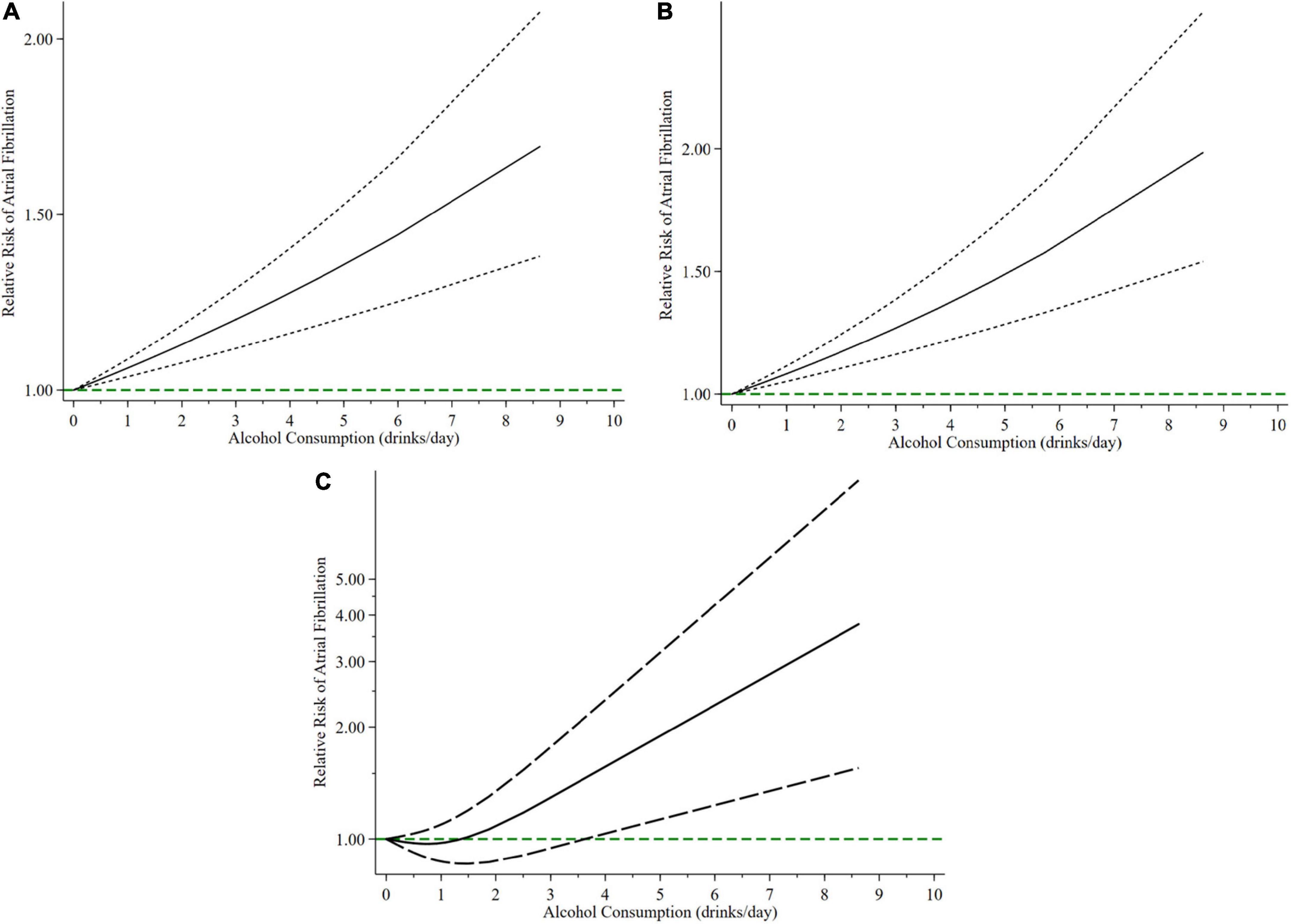
Figure 6. The relationship between relative risks of atrial fibrillation with different alcohol consumption. Continuous line shows non-linear association and long-dashed lines depict 95% confidence intervals. (A) In total; (B) men; (C) women.
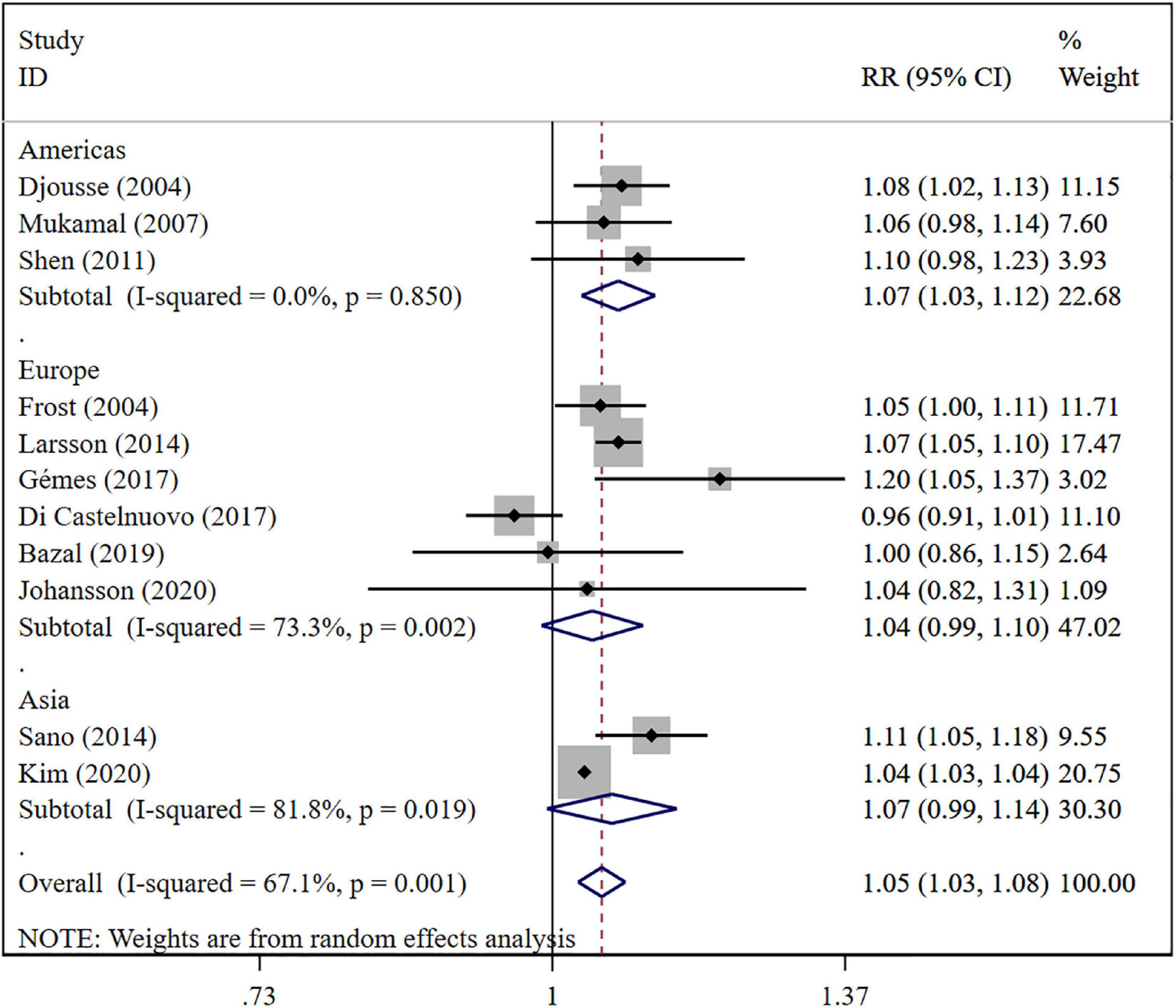
Figure 7. Subgroup analysis of relative risks of atrial fibrillation per 1 drink/day increment in alcohol consumption in different region.
Discussion
This study is an updated dose-response meta-analysis for evaluating the association between AF risk and alcohol consumption. Considering the shortcomings of previous meta-analyses (9–11, 14), the latest comprehensive meta-analysis of high-quality prospective studies and almost 10 million participants was conducted, along with subgroup and sensitivity analysis, to obtain more reliable results. Specifically, five more studies (12, 13, 15, 16, 31) involving a total of 9,943,654 participants with 202,301 cases were included in our study on the basis of the last meta-analysis published in 2014 (11). The newly included studies had lager sample sizes than those before, and two studies conducted dose-response analysis (12, 13).
In total, our results showed a 6% increase in AF risk for per drink one day, which is inconsistent with three previous meta-analyses (9–11), but the risk increased linearly with alcohol consumption remained found. Moreover, subgroup analysis suggested that the pattern of responses to alcohol consumption may vary differently between men and women. One drink/day increase in alcohol consumption is not significantly associated with the development of AF in women. In addition, a linear association was found in men, while a J-shaped curve was observed in women. It can be considered that drinking at any dose may increase the risk of AF in men. For women, however, more than 1.4 drinks/day may increase the risk of AF in women, and less than 1.4 drinks/day even may have a protective effect. Our findings confirmed gender difference in pattern of response to alcohol consumption, which are partially consistent with a recent meta-analysis (14). This meta-analysis found that an average of 1–2 standard drinks per day (moderate alcohol intake) had an increased AF risk compared with lower alcohol intake for men, but not for women. A study only for women also discovered this potential non-linear relationship and confirmed that less than 2 alcoholic drinks/day cannot induce an increased risk of AF (27).
Alcohol may contribute as a trigger of AF and long-term regular consumption promotes progressive atrial remodeling (32). Acute alcohol consumption, as a trigger, may act on electrophysiological milieu for AF through cellular and autonomic effects, such as shortening atrial and pulmonary vein action potential (33, 34), shortening atrial effective refractory period (35), and slowing atrial conduction (35). In addition, habitual drinking induces AF by directly affecting the left atrial substrate and interacting with other risk factors (left ventricular dysfunction, obstructive sleep apnea, hypertension, etc.) (32).
The protective effect of drinking (less than 1.4 drinks/day) in women needs further validation. There may be a variety of reasons for the observed gender difference in this study. Firstly, different dose-response associations may be related to different types of alcoholic beverage consumption. Ethanol and polyphenols in wine may be synergistic, thereby reducing the risk of chronic cardiovascular disease (CVD) (36). It was also found that the proportion of women drinking wine was significantly higher than that of men (31). Secondly, a recent study found that drinking frequency could be an important risk factor for new-onset AF, with an even greater influence than the amount of alcohol consumption in each drinking session (16). Indeed, men tend to have more frequent drinking habits. Thirdly, most of the included studies collected information about alcohol consumption through questionnaires or interviews, which may different social implications for men and women. In response to questionnaires, participants tend to underestimate their actual alcohol consumption (37). Fourth, AF is less prevalent in middle-aged women than in men (38), which may affect the results to a certain extent.
As for the regional subgroup, there was not enough data for a dose-response analysis. Some researches (28, 39, 40) found that dietary exposures other than alcohol, for example caffeine, fish, omega-3 polyunsaturated fatty acids, do associate with risk of AF recent years. As known, there are obvious differences in dietary structure among the United States, Asia and Europe, so some other dietary factors like caffeine which were not be adjusted might influence the subgroup analysis result.
The sample size of more than 10 million is the advantage of meta-analysis in this study, providing high statistical capacity to detect the relationship between AF risk and alcohol consumption. Moreover, all eligible studies are designed prospectively to minimize the likelihood of selection bias and recall bias. Nevertheless, there are also some limitations in this meta-analysis that may affect conclusions. First, although no statistical evidence of publication bias was detected, the likelihood of publication bias cannot be excluded due to the small number of studies. Second, there was moderate heterogeneity in preliminary meta-analysis, which needs to be considered when interpreting the results. The lack of corresponding exposure data prevented us from addressing the moderate heterogeneity. Third, due to the complex mechanism of AF, it is difficult to guarantee that our results are not affected by other confounding factors.
In summary, this study provides further information about the role of alcohol consumption in new-onset AF, particularly between different genders. Regrettably, it is difficult to give a recommended amount of alcohol intake to prevent AF based on the current data.
Conclusion
The relationship between AF risk and alcohol consumption is linear in men, while a potential non-linear J-shaped relationship is shown in women. An individual participant data meta-analysis of harmonized data across individual studies could help address some of the uncertainties in the shape of the relationship between different types of alcohol consumption and AF risk.
Data availability statement
The original contributions presented in this study are included in the article/supplementary material, further inquiries can be directed to the corresponding authors.
Author contributions
HJ, XM, and YJ contributed equally to the study. XM conceived of the presented idea. HJ interpreted the data being published and made figures. HJ and YJ wrote the manuscript with support from XM, JY, and JS. TC and YZ revised the manuscript. All authors contributed to the article and approved the submitted version.
Funding
This work was supported by grants from National Natural Science Foundation of China (81873486), the Science and Technology Development Program of Jiangsu Province-Clinical Frontier Technology (BE2022754), Clinical Medicine Expert Team (Class A) of Jinji Lake Health Talents Program of Suzhou Industrial Park (SZYQTD202102), Suzhou Key Discipline for Medicine (SZXK202129), Demonstration of Scientific and Technological Innovation Project (SKY2021002), Suzhou Dedicated Project on Diagnosis and Treatment Technology of Major Diseases (LCZX202132), and Research on Collaborative Innovation of Medical Engineering Combination (SZM2021014). The funders had no roles in study design, data collection and analysis, decision to publish, or preparation of the manuscript.
Conflict of interest
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
Publisher’s note
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
Abbreviations
AF, atrial fibrillation; HF, heart failure; MOOSE, Meta-Analysis Of Observational Studies in Epidemiology; RR, relative risk; CI, confidence interval; NOS, Newcastle-Ottawa scale; CVD, cardiovascular disease.
References
1. Chugh SS, Havmoeller R, Narayanan K, Singh D, Rienstra M, Benjamin EJ, et al. Worldwide epidemiology of atrial fibrillation: a Global Burden of Disease 2010 Study. Circulation. (2014) 129:837–47. doi: 10.1161/CIRCULATIONAHA.113.005119
2. Kivimaki M, Nyberg ST, Batty GD, Kawachi I, Jokela M, Alfredsson L, et al. Long working hours as a risk factor for atrial fibrillation: a multi-cohort study. Eur Heart J. (2017) 38:2621–8. doi: 10.1093/eurheartj/ehx324
3. Andersson T, Magnuson A, Bryngelsson IL, Frøbert O, Henriksson KM, Edvardsson N, et al. All-cause mortality in 272,186 patients hospitalized with incident atrial fibrillation 1995-2008: a Swedish nationwide long-term case-control study. Eur Heart J. (2013) 34:1061–7. doi: 10.1093/eurheartj/ehs469
4. Benjamin EJ, Chen PS, Bild DE, Mascette AM, Albert CM, Alonso A, et al. Prevention of atrial fibrillation: report from a national heart, lung, and blood institute workshop. Circulation. (2009) 119:606–18. doi: 10.1161/CIRCULATIONAHA.108.825380
5. Wong JA, Conen D. Alcohol consumption, atrial fibrillation, and cardiovascular disease: finding the right balance. Eur Heart J. (2021) 42:1178–9. doi: 10.1093/eurheartj/ehaa955
6. Russo AM. Alcohol intake and risk of stroke in atrial fibrillation: the lesser the better, but this is not enough. Eur Heart J. (2021) 42:4769–71. doi: 10.1093/eurheartj/ehab657
7. Reddiess P, Aeschbacher S, Meyre P, Coslovsky M, Kühne M, Rodondi N, et al. Alcohol consumption and risk of cardiovascular outcomes and bleeding in patients with established atrial fibrillation. Cmaj. (2021) 193:E117–23. doi: 10.1503/cmaj.200778
8. Voskoboinik A, Kalman JM, De Silva A, Nicholls T, Costello B, Nanayakkara S, et al. Alcohol abstinence in drinkers with atrial fibrillation. N Engl J Med. (2020) 382:20–8. doi: 10.1056/NEJMoa1817591
9. Samokhvalov AV, Irving HM, Rehm J. Alcohol consumption as a risk factor for atrial fibrillation: a systematic review and meta-analysis. Eur J Cardiovasc Prev Rehabil. (2010) 17:706–12. doi: 10.1097/HJR.0b013e32833a1947
10. Kodama S, Saito K, Tanaka S, Horikawa C, Saito A, Heianza Y, et al. Alcohol consumption and risk of atrial fibrillation: a meta-analysis. J Am Coll Cardiol. (2011) 57:427–36. doi: 10.1016/j.jacc.2010.08.641
11. Larsson SC, Drca N, Wolk A. Alcohol consumption and risk of atrial fibrillation: a prospective study and dose-response meta-analysis. J Am Coll Cardiol. (2014) 64:281–9. doi: 10.1016/j.jacc.2014.03.048
12. Gemes K, Malmo V, Laugsand LE, Loennechen JP, Ellekjaer H, László KD, et al. Does moderate drinking increase the risk of atrial fibrillation? The Norwegian HUNT (Nord-Trondelag Health) study. J Am Heart Assoc. (2017) 6:e007094. doi: 10.1161/JAHA.117.007094
13. Di Castelnuovo A, Costanzo S, Bonaccio M, Rago L, De Curtis A, Persichillo M, et al. Moderate alcohol consumption is associated with lower risk for heart failure but not atrial fibrillation. JACC Heart Fail. (2017) 5:837–44.
14. Gallagher C, Hendriks JML, Elliott AD, Wong CX, Rangnekar G, Middeldorp ME, et al. Alcohol and incident atrial fibrillation - a systematic review and meta-analysis. Int J Cardiol. (2017) 246:46–52. doi: 10.1016/j.ijcard.2017.05.133
15. Bazal P, Gea A, Martínez-González MA, Salas-Salvadó J, Asensio EM, Muñoz-Bravo C, et al. Mediterranean alcohol-drinking pattern, low to moderate alcohol intake and risk of atrial fibrillation in the PREDIMED study. Nutr Metab Cardiovasc Dis. (2019) 29:676–83. doi: 10.1016/j.numecd.2019.03.007
16. Kim YG, Han KD, Choi JI, Boo KY, Kim DY, Lee KN, et al. Frequent drinking is a more important risk factor for new-onset atrial fibrillation than binge drinking: a nationwide population-based study. Europace. (2020) 22:216–24. doi: 10.1093/europace/euz256
17. Stroup DF, Berlin JA, Morton SC, Olkin I, Williamson GD, Rennie D, et al. Meta-analysis of observational studies in epidemiology: a proposal for reporting. Meta-analysis Of Observational Studies in Epidemiology (MOOSE) group. JAMA. (2000) 283:2008–12. doi: 10.1001/jama.283.15.2008
18. Stang A. Critical evaluation of the Newcastle-Ottawa scale for the assessment of the quality of nonrandomized studies in meta-analyses. Eur J Epidemiol. (2010) 25:603–5. doi: 10.1007/s10654-010-9491-z
19. Higgins JP, Thompson SG, Deeks JJ, Altman DG. Measuring inconsistency in meta-analyses. BMJ. (2003) 327:557–60. doi: 10.1136/bmj.327.7414.557
20. Egger M, Davey Smith G, Schneider M, Minder C. Bias in meta-analysis detected by a simple, graphical test. BMJ. (1997) 315:629–34. doi: 10.1136/bmj.315.7109.629
21. Greenland S, Longnecker MP. Methods for trend estimation from summarized dose-response data, with applications to meta-analysis. Am J Epidemiol. (1992) 135:1301–9. doi: 10.1093/oxfordjournals.aje.a116237
22. Orsini N, Li R, Wolk A, Khudyakov P, Spiegelman D. Meta-analysis for linear and nonlinear dose-response relations: examples, an evaluation of approximations, and software. Am J Epidemiol. (2012) 175:66–73. doi: 10.1093/aje/kwr265
23. Harrell FE Jr., Lee KL, Pollock BG. Regression models in clinical studies: determining relationships between predictors and response. J Natl Cancer Inst. (1988) 80:1198–202. doi: 10.1093/jnci/80.15.1198
24. Djoussé L, Levy D, Benjamin EJ, Blease SJ, Russ A, Larson MG, et al. Long-term alcohol consumption and the risk of atrial fibrillation in the Framingham Study. Am J Cardiol. (2004) 93:710–3. doi: 10.1016/j.amjcard.2003.12.004
25. Frost L, Vestergaard P. Alcohol and risk of atrial fibrillation or flutter: a cohort study. Arch Intern Med. (2004) 164:1993–8. doi: 10.1001/archinte.164.18.1993
26. Mukamal KJ, Psaty BM, Rautaharju PM, Furberg CD, Kuller LH, Mittleman MA, et al. Alcohol consumption and risk and prognosis of atrial fibrillation among older adults: the Cardiovascular Health Study. Am Heart J. (2007) 153:260–6. doi: 10.1016/j.ahj.2006.10.039
27. Conen D, Tedrow UB, Cook NR, Moorthy MV, Buring JE, Albert CM. Alcohol consumption and risk of incident atrial fibrillation in women. Jama. (2008) 300:2489–96. doi: 10.1001/jama.2008.755
28. Shen J, Johnson VM, Sullivan LM, Jacques PF, Magnani JW, Lubitz SA, et al. Dietary factors and incident atrial fibrillation: the Framingham Heart Study. Am J Clin Nutr. (2011) 93:261–6. doi: 10.3945/ajcn.110.001305
29. Liang Y, Mente A, Yusuf S, Gao P, Sleight P, Zhu J, et al. Alcohol consumption and the risk of incident atrial fibrillation among people with cardiovascular disease. CMAJ. (2012) 184:E857–66. doi: 10.1503/cmaj.120412
30. Sano F, Ohira T, Kitamura A, Imano H, Cui R, Kiyama M, et al. Heavy alcohol consumption and risk of atrial fibrillation. The Circulatory Risk in Communities Study (CIRCS). Circ J. (2014) 78:955–61. doi: 10.1253/circj.CJ-13-1387
31. Johansson C, Lind MM, Eriksson M, Wennberg M, Andersson J, Johansson L. Alcohol consumption and risk of incident atrial fibrillation: a population-based cohort study. Eur J Intern Med. (2020) 76:50–7. doi: 10.1016/j.ejim.2020.02.022
32. Voskoboinik A, Prabhu S, Ling LH, Kalman JM, Kistler PM. Alcohol and atrial fibrillation: a sobering review. J Am Coll Cardiol. (2016) 68:2567–76. doi: 10.1016/j.jacc.2016.08.074
33. Zhao Y, Sun J, Hu J, Bo N, Yu B. [Effect of ethanol and its metabolites on acetylcholine-sensitive K(+) channel Kir3.1 protein expression of neonatal rat primary atrial cardiomyocytes]. Zhonghua Xin Xue Guan Bing Za Zhi. (2015) 43:609–13.
34. Chen YC, Chen SA, Chen YJ, Tai CT, Chan P, Lin CI. Effect of ethanol on the electrophysiological characteristics of pulmonary vein cardiomyocytes. Eur J Pharmacol. (2004) 483:215–22. doi: 10.1016/j.ejphar.2003.10.042
35. Gould L, Reddy CV, Becker W, Oh KC, Kim SG. Electrophysiologic properties of alcohol in man. J Electrocardiol. (1978) 11:219–26. doi: 10.1016/S0022-0736(78)80120-4
36. Haseeb S, Alexander B, Baranchuk A. Wine and cardiovascular health: a comprehensive review. Circulation. (2017) 136:1434–48. doi: 10.1161/CIRCULATIONAHA.117.030387
37. Stockwell T, Zhao J, Sherk A, Rehm J, Shield K, Naimi T. Underestimation of alcohol consumption in cohort studies and implications for alcohol’s contribution to the global burden of disease. Addiction. (2018) 113:2245–9. doi: 10.1111/add.14392
38. Magnussen C, Niiranen TJ, Ojeda FM, Gianfagna F, Blankenberg S, Njølstad I, et al. Sex differences and similarities in atrial fibrillation epidemiology, risk factors, and mortality in community cohorts: results from the BiomarCaRE consortium (biomarker for cardiovascular risk assessment in Europe). Circulation. (2017) 136:1588–97.
39. Surma S, Romańczyk M, Filipiak KJ, Lip GYH. Coffee and cardiac arrhythmias: up-date review of the literature and clinical studies. Cardiol J. (2022) [Online ahead of print]. doi: 10.5603/CJ.a2022.0068
40. Borges MC, Haycock PC, Zheng J, Hemani G, Holmes MV, Davey G, et al. Role of circulating polyunsaturated fatty acids on cardiovascular diseases risk: analysis using Mendelian randomization and fatty acid genetic association data from over 114,000 UK Biobank participants. BMC Med. (2022) 20:210. doi: 10.1186/s12916-022-02399-w
Keywords: alcohol, atrial fibrillation, meta-analysis, gender difference, risk
Citation: Jiang H, Mei X, Jiang Y, Yao J, Shen J, Chen T and Zhou Y (2022) Alcohol consumption and atrial fibrillation risk: An updated dose-response meta-analysis of over 10 million participants. Front. Cardiovasc. Med. 9:979982. doi: 10.3389/fcvm.2022.979982
Received: 28 June 2022; Accepted: 14 September 2022;
Published: 30 September 2022.
Edited by:
Sebhat Erqou, Brown University, United StatesReviewed by:
Domenico Giovanni Della Rocca, Texas Cardiac Arrhythmia Institute, United StatesKazuo Miyazawa, RIKEN Yokohama, Japan
Copyright © 2022 Jiang, Mei, Jiang, Yao, Shen, Chen and Zhou. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Yafeng Zhou, emhvdXlhZmVuZzczQDEyNi5jb20=; Tan Chen, Y2hlbnRhbjEyMzQ1QDEyNi5jb20=
 Hezi Jiang
Hezi Jiang Xiaofei Mei
Xiaofei Mei Yufeng Jiang
Yufeng Jiang Jialu Yao
Jialu Yao Yafeng Zhou
Yafeng Zhou