- 1Department of Critical Care Medicine, Samsung Medical Center, Sungkyunkwan University School of Medicine, Seoul, Republic of Korea
- 2Division of Cardiology, Department of Medicine, Heart Vascular Stroke Institute, Samsung Medical Center, Sungkyunkwan University School of Medicine, Seoul, Republic of Korea
Background: Limited data are available on the association of malnutrition with the occurrence of delirium in the cardiac intensive care unit (CICU). Thus, we aimed to analyze whether nutritional indices and their components can predict the development of delirium in CICU.
Methods: We enrolled 2,783 patients admitted to the CICU of Samsung Medical Center for more than 24 h between September 2012 and December 2018. We assessed the nutritional status at admission using three indices, the Prognostic Nutrition Index (PNI), the Geriatric Nutritional Risk Index (GNRI), and the Controlling Nutritional Status (CONUT). Then, we compared predictive performances for the occurrence of delirium among nutritional indices using Delong’s test.
Results: Delirium developed in 678 patients (24.3%) assessed three times daily for 7 days of CICU stay. Nutritional indices had fair predictive performance for development of delirium in critically ill cardiac patients using the area under the receiver-operating characteristic curve (AUROC: 0.729 for the GNRI, 0.728 for PNI, and 0.762 for CONUT). Furthermore, the AUROC of albumin alone (0.77, 95% CI, 0.75–0.79) was significantly greater than that of either GNRI (p < 0.001) or PNI (p < 0.001). In a multivariable analysis including each component of nutritional indices, albumin was a significant predictor for delirium but not absolute lymphocyte count, bodyweight/ideal bodyweight, or total cholesterol level as a component of nutritional indices.
Conclusion: Predictive performances of nutritional indices for the occurrence of delirium were acceptable in patients admitted to CICU. Albumin alone might be a helpful and straightforward indicator for the occurrence of delirium.
Introduction
Delirium is a frequent complication in patients admitted to the intensive care unit (ICU). It has been associated with increased risk of mortality, development of post-ICU cognitive impairment, and longer ICU and hospital stays (1, 2). In recent decades, the application of advanced medical devices for the treatment of cardiovascular disease has been significantly expanded, and the number of critically ill patients with underlying cardiac disease has increased (3). Accordingly, the incidence of delirium in the cardiac intensive care unit (CICU) has substantially increased and is comparable to that in other medical ICUs (4). Furthermore, recent studies have reported associations between delirium and clinical outcomes in critically ill cardiac patients (5, 6).
Malnutrition is an essential risk factor for delirium in elderly patients (7). Several nutritional indices have been developed to assess the risk of malnutrition in critically ill patients. First, the Prognostic Nutritional Index (PNI) was created in 1980 to evaluate preoperative nutritional conditions and surgical risk for gastrointestinal surgery (8). The Geriatric Nutritional Risk Index (GNRI) was developed to estimate the risk of morbidity and mortality in elderly medical patients (9). The Controlling Nutritional Status (CONUT) is widely used for daily assessment of the nutritional status of inpatients (10).
Although several studies have reported an association of delirium with mortality in ICU patients, limited studies are available on the relationship between nutritional status and delirium in CICU patients. Therefore, the goal of the present study was (i) to assess the predictive performance of nutritional indices (PNI, GNRI, and CONUT) and their components in CICU patients and (ii) to investigate clinical factors associated with delirium in this population.
Methods
Study population
All consecutive patients who were admitted to the CICU between September 1, 2012, and December 31, 2018, were eligible for the study. A total of 4,261 patients who were 18 years old or older was admitted to the CICU at Samsung Medical Center in Seoul, Republic of Korea. We excluded 1,473 patients who stayed in the CICU for less than 24 h and three patients for whom we were not able to calculate nutritional indices due to limited data. The Institutional Review Board of Samsung Medical Center approved this study (IRB. No. 2020–10-102) and waived the requirement for informed consent because of the observational nature of the study. Patient information was anonymized and de-identified before analysis.
Cardiac intensive care unit management
Our unit is a 12-bed ICU with a 1:2 nurse-to-patient ratio offering level 1 care for critically ill cardiac patients. To provide comprehensive critical care to patients with various cardiovascular diseases and complex comorbidities, the CICU is equipped with invasive and noninvasive devices to monitor patients’ hemodynamic status and provide advanced therapeutic technologies. With the high-intensity staffing model, patients are managed by a dedicated cardiac intensivist who is board certified in interventional cardiology and critical care medicine (11). Cardiac surgery support is promptly assessable. In addition, multidisciplinary care is provided via consultation with a dietitian, pharmacist, and respiratory care practitioner.
The clinical practice guidelines published by The Society of Critical Care Medicine were adopted for general intensive care (12). The Confusion Assessment Method for ICU (CAM-ICU) assessment was performed by nurses three times a day on patients with a Richmond Agitation-Sedation Scale of −3 (indicating movement or eye-opening to voice but no eye contact) or higher. The recorded CAM-ICU results were re-checked every day by a senior nurse. Nutrition support team consultation was available for nutrition therapy.
Nutritional indices
Nutritional status was assessed using the PNI, GNRI, and CONUT based on blood test results measured on the day of admission to CICU to identify risk scores of malnutrition in critically ill patients. The PNI is calculated as follows: 10 x serum albumin concentration (g/dL) + 0.005 x absolute lymphocyte count (ALC, number/mm2) in peripheral blood (13). Patients with a PNI score > 38 were considered normal, patients with a score of 35–38 were at risk of moderate malnutrition, and patients with a score < 35 were classified as at risk of severe malnutrition. The GNRI is calculated as follows: 14.89 x serum albumin (g/dL) + 41.7 x [bodyweight/ideal bodyweight (IBW)] (9). Patients were categorized into four groups according to GNRI score: major risk (GNRI score < 82), moderate risk (82 ≤ GNRI score < 92), low risk (92 ≤ GNRI score < 98), and no risk (98 ≤ GNRI score). The CONUT was obtained based on serum albumin concentration, cholesterol level, and ALC (14). According to the CONUT score, patients were divided into four groups: normal (0–1 point), mild risk (2–4 points), moderate risk (5–8 points), and severe risk (9–12 points).
Data collection
After reviewing the medical records, a trained study coordinator retrospectively collected clinical, laboratory, and outcome data. To accurately evaluate the total number of days at risk of delirium, we did not include days when the patient was in a coma as defined by a Richmond Agitation-Sedation Scale assessment of −4 (unresponsive to voice but responded to physical stimulation) or − 5 (unresponsive to voice and physical stimulation) (15). Delirium was defined as CAM-ICU positivity at any time during the assessment three times daily for up to 7 days of CICU stay. Polypharmacy was defined as the routine use of five or more medications (16).
Statistical analysis
Descriptive statistics were performed to compare the clinical characteristics and outcomes between the delirium and non-delirium groups. Continuous variables were presented as median and interquartile range or mean ± standard deviation and were compared with a Mann–Whitney U test. Categorical variables were expressed as number and percentage and were analyzed using Chi-square tests or Fisher’s exact tests, where applicable. The model’s predictive ability to discriminate between patients who had and did not have delirium was estimated using the receiver operating characteristic curve. The receiver operating characteristic curve is presented to demonstrate the performance of delirium for the area under the curve (AUROC) and 95% confidence interval (CI). Discriminant functions were compared by a 2-tailed paired comparison of the ROC curve by DeLong’s method (17). Variables with a p value less than 0.05 on univariate analyzes and clinically relevant a priori variables were entered into the multiple logistic regression model. Results were reported as each variable’s odds ratio (OR) with 95% CI. A two-tailed p value less than 0.05 was considered statistically significant for all analyzes. Data were analyzed using R Statistical Software (Version 3.2.5; R Foundation for Statistical Computing, Vienna, Austria).
Results
Clinical characteristics
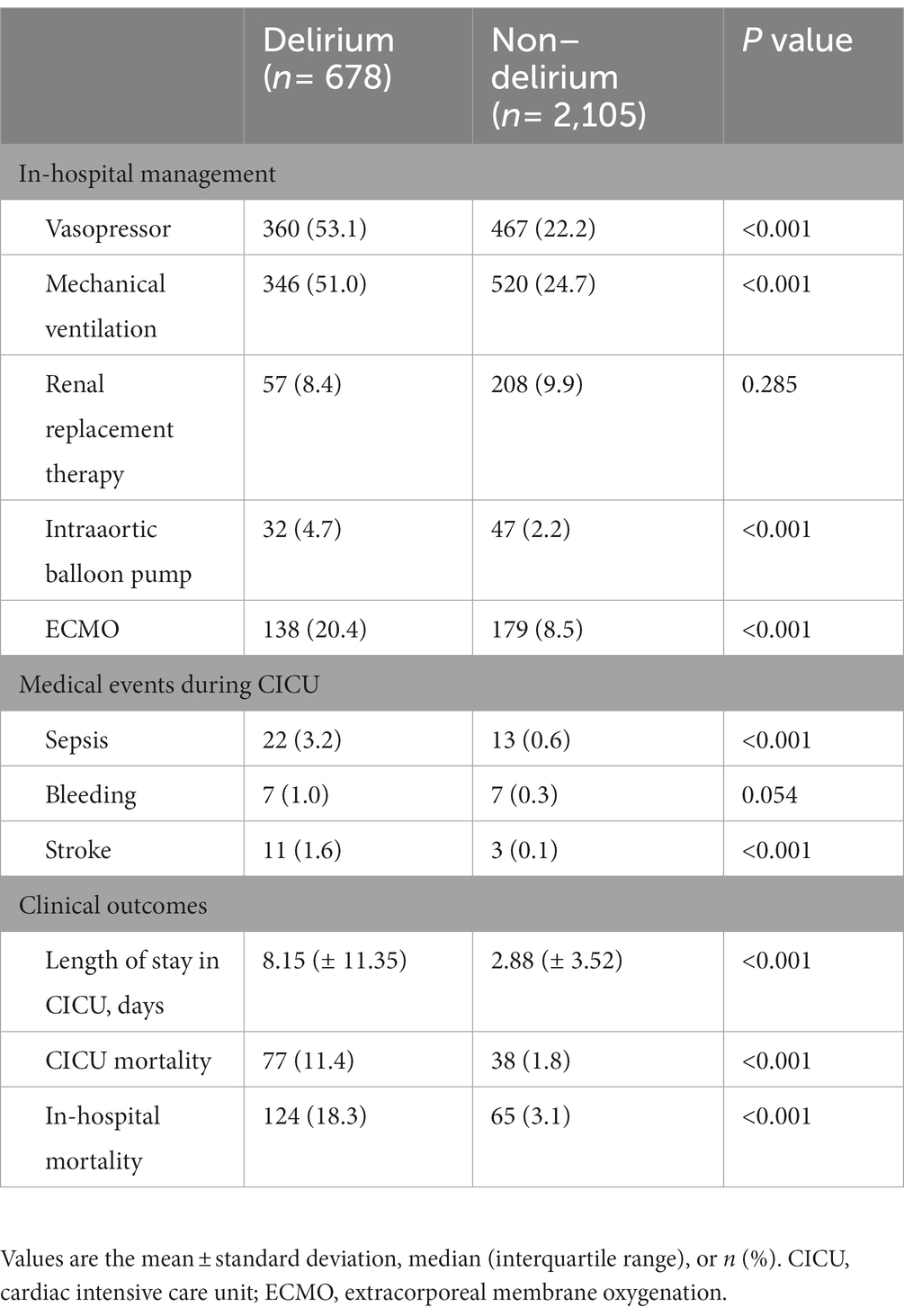
During the study period, 2,783 patients were finally enrolled in this analysis; 678 patients (24.3%) have occurred delirium during CICU admission. The characteristics of the patients are shown in Table 1. Patients in the delirium group were older and higher-risk subjects with lower body mass index and more comorbidities than those in the non-delirium group. There was no difference between the two groups in the CICU admission diagnosis and polypharmacy. Cardiac arrest before CICU admission (20.9% vs. 6.3%; p < 0.001) and Sequential Organ Failure Assessment score (6.97 ± 3.47 vs. 3.39 ± 2.71; p < 0.001) were higher in the delirium group than in the non-delirium group. In the laboratory findings at CICU admission, ALC [1.13 (0.7–1.8) x103/μL vs. 1.62 (1.1–2.3) x103/μL; p < 0.001], albumin [3.2 (2.8–3.6) g/dL vs. 3.9 (3.4–4.2) g/dL; p < 0.001], and total cholesterol [119.5 (94.0–152.0) mg/dL vs. 150.0 (121.5–183.0) mg/dL; p < 0.001] were significantly lower in the delirium group.
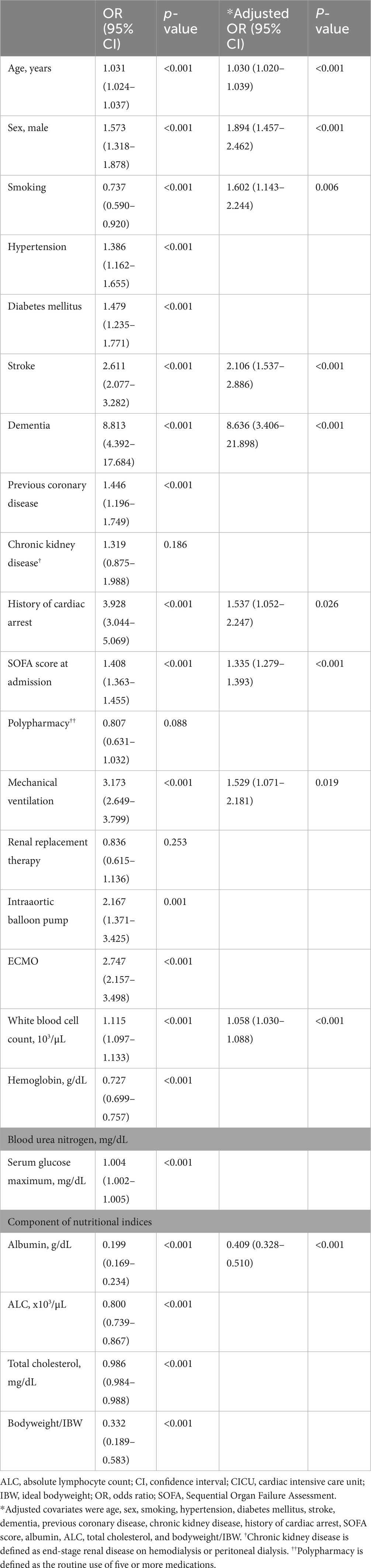
Cardiac intensive care unit management and clinical outcomes
Patients in the delirium group were more likely to receive vasopressor, mechanical ventilator, intraaortic balloon pump, and extracorporeal membrane oxygenator interventions than were those in the non-delirium group during the CICU stay (Table 2). Compared with the non-delirium group, CICU length of stay (8.15 ± 11.35 days vs. 2.88 ± 3.52 days; p < 0.001), CICU mortality (11.4% vs. 1.8%; p < 0.001), and in-hospital mortality (18.3% vs. 3.1%; p < 0.001) were higher in the delirium group.
Predictive performance for delirium
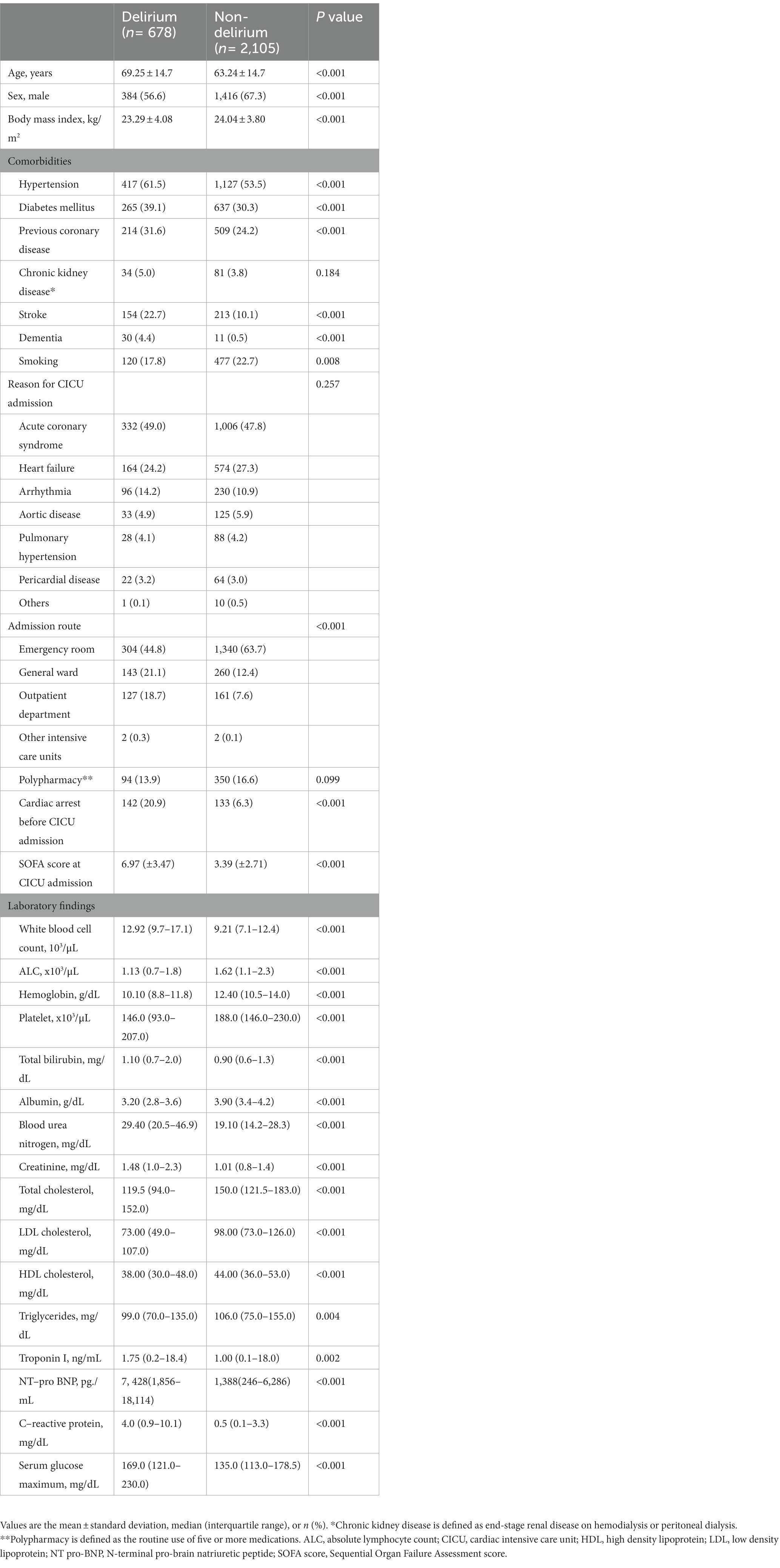
The distribution of delirium according to the value of each component in the three nutritional indices is shown in cubic spline curves (Figure 1). According to the increasing level of albumin, the occurrence of delirium tended to decrease linearly (Figure 1A). However, U-shaped correlation was observed for increased level of ALC, bodyweight/IBW, and total cholesterol with delirium (Figures 1B–D).
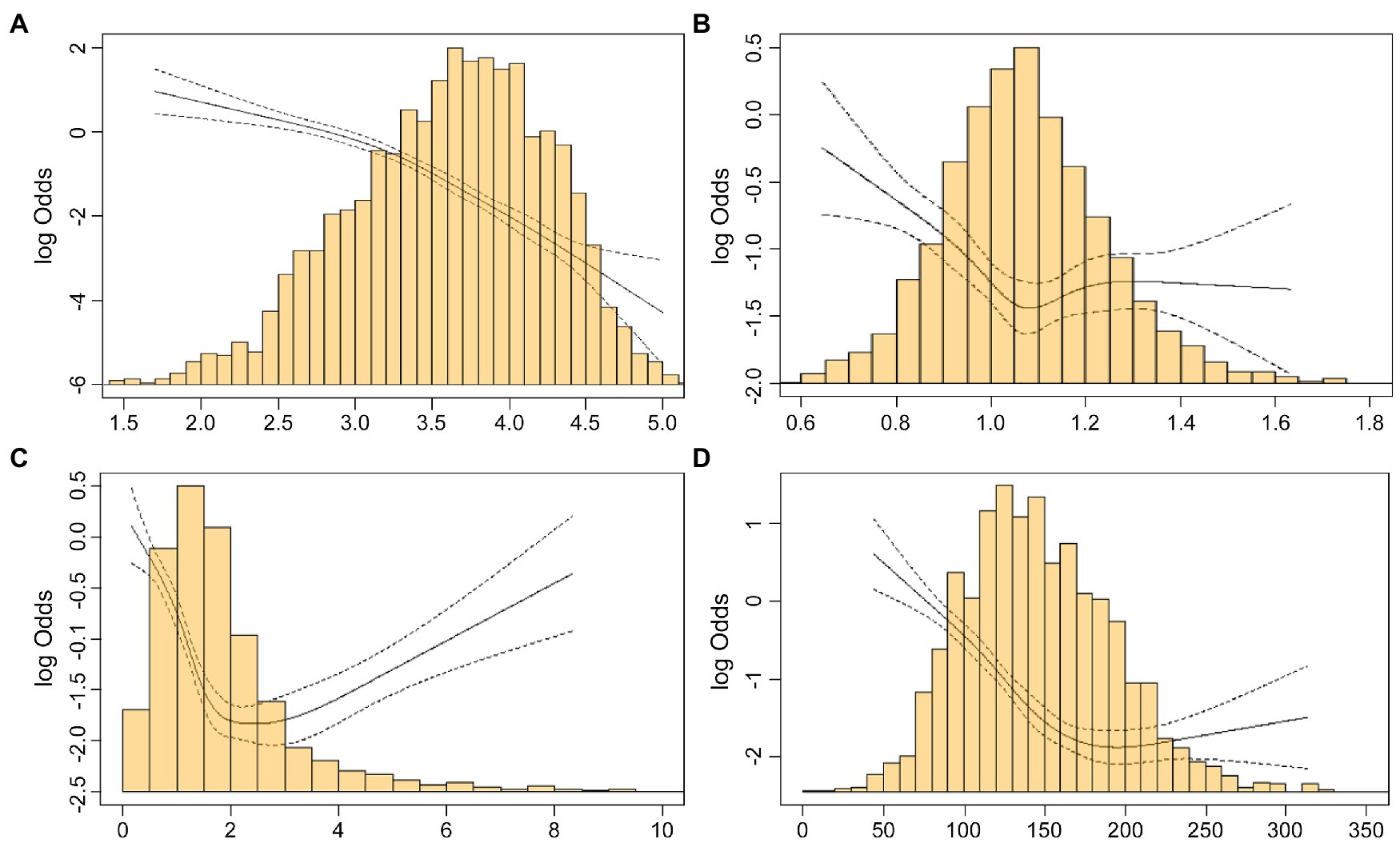
Figure 1. Restricted cubic spline plot of the relationships between components of nutrition indices and delirium. The solid line is the log odds, and the dashed lines are the upper and lower 95% confidence limits. (A) Restricted cubic spline plot for the association between albumin (g/dL) and delirium. (B) Restricted cubic spline for the association between bodyweight/ideal bodyweight and delirium. (C) Restricted cubic spline for the association between absolute lymphocyte count (x103/μL) and delirium. (D) Restricted cubic spline for the association between total cholesterol (ml/dL) and delirium.
The performances of albumin, PNI, GNRI, and CONUT for delirium prediction were compared and are shown in Figure 2. Among three nutritional indices, the AUROC of the CONUT was higher than those of the PNI and GNRI. Algorithm discrimination performance of albumin alone (AUC = 0.770; 95% CI, 0.750–0.790) and CONUT (AUC = 0.762; 95% CI, 0.750–0.790; p = 0.275) for delirium were not significantly different; however, discrimination was superior to that of the GNRI (AUC = 0.729; 95% CI, 0.706–0.753; p < 0.001) and PNI (AUC = 0.728; 95% CI, 0.706–0.751; p < 0.001).
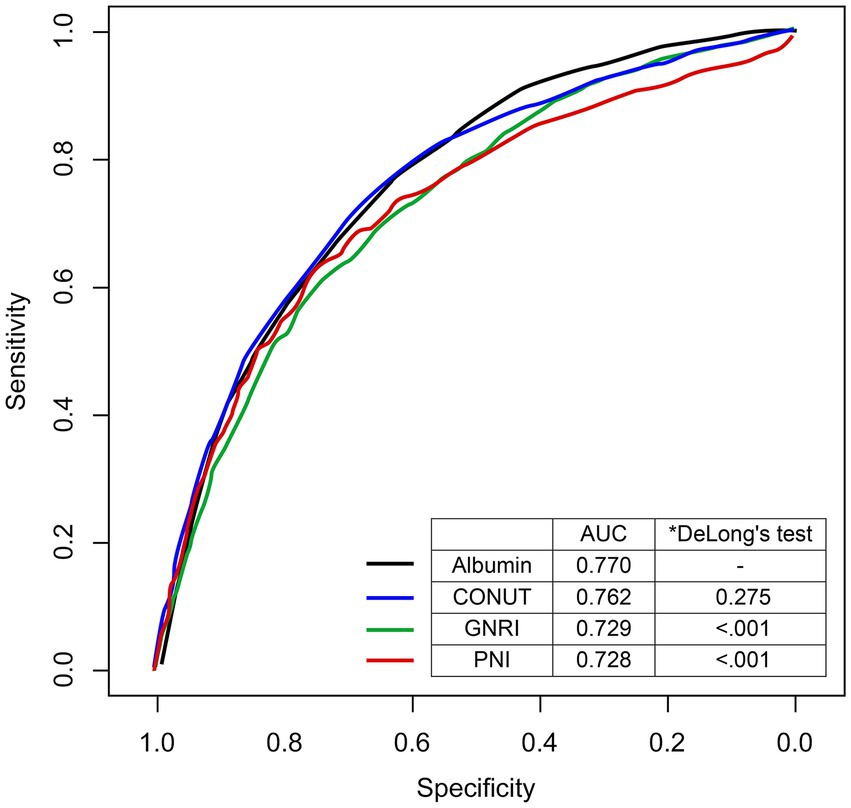
Figure 2. The receiver-operating characteristic curve comparing the predictive performances for delirium. The predictive performances of nutritional indices were calculated using Delong’s test and compared to those of albumin. AUC, area under the curve; CONUT, Controlling Nutritional Status; GNRI, Geriatric Nutritional Risk Index; PNI, Prognostic Nutritional Index.
Factors associated with delirium
Univariable logistic regression analysis indicated that 15 characteristics of CICU patients were associated with delirium (Table 3). In multivariable analysis, age, sex, smoking, stroke, dementia, Sequential Organ Failure Assessment score, mechanical ventilation, and white blood cell were associated with increased risk of delirium, while albumin level at CICU admission (adjusted OR 0.555; 95% CI 0.402–0.767; p < 0.001) was associated with decreased risk of delirium.
Discussion
We investigated the associations of nutritional indices and their components with delirium in CICU patients from a single-center registry. The major findings were as follows: (i) nutritional indices (PNI, GNRI, and CONUT) had fair predictive performances for delirium in CICU patients; (ii) predictive performance of albumin alone for delirium was superior to those of PNI and GNRI and similar to that of CONUT; and (iii) among the components of nutritional indices, albumin was an independent predictor of delirium, whereas ALC, bodyweight/IBW, and total cholesterol were not.
Delirium is an emerging complication of CICU stay, with a reported incidence range from 5.7 to 40% (18–20). There are several possible causes for the increased incidence of delirium in CICU. First of all, acute respiratory failure caused by cardiac origin has been a leading indication for CICU admission, and recent studies have described temporal increases in mechanical ventilation support in CICU populations (21). Although the clinical practice guidelines for adult patients in the ICU recommend light sedation, some mechanically ventilated patients require deep sedation to control pain and agitation during the early phase of respiratory failure (12). For deep sedation, intravenous administration of opioids and benzodiazepines is often used, and their use is associated with delirium (22). Furthermore, the CICU has become considerably more complex with advanced medical devices, increasing CICU patient complications (3). Therefore, delirium has recently been recognized as a common comorbidity for CICU patients.
Several prospective cohort studies have evaluated the incidence of postoperative delirium in malnourished patients undergoing coronary artery bypass grafting and have found that malnutrition is associated with postoperative delirium (7, 23). Meta-analysis to determine the risk factors of delirium after orthopedic surgery in elderly patients has also shown malnutrition as an important factor for delirium after surgery (24). In CICU patients, Sugita et al. conducted a prospective cohort study to evaluate the association between malnutrition and delirium in critically ill cardiac patients (25). Of 653 CICU patients, 58 (8.9%) developed delirium, for which PNI and CONUT were both reported to be independent predictors of delirium, but GNRI was not. They suggested that ALC, included in PNI and CONUT but not in GNRI, might be an important prognostic factor associated with inflammation in delirium patients. However, in the present study, U-shaped correlation was observed between increased level of ALC and delirium. Furthermore, the discrimination performance of PNI for delirium was similar to those of CONUT and GNRI.
Albumin is the most abundant protein in the plasma and is a major transporter of many compounds in blood (26). A recent study of surgical ICU patients by Yeh DD, et al. found that serum albumin levels and pre-albumin levels may reflect baseline nutrition status. However, changes in serum albumin and pre-albumin levels during ICU stays may not indicate nutritional adequacy in the ICU (27). This is because albumin synthesis can be affected by numerous acute and chronic disease processes, and serum albumin level can provide predictive insights into the effects of disease on protein metabolism. Hypoalbuminemia can be observed in acute illness due to increased capillary leakage or decreased synthesis due to inflammation, underlying malnutrition, or hepatic synthetic dysfunction (28). Therefore, albumin is a well-known predictor of mortality in critically ill patients (29). Recent studies have reported the association between albumin level and delirium, and meta-analysis of risk factors of delirium occurrence among elderly patients in medical ICUs has found that low albumin level is associated with delirium (30). Zhang et al. analyzed 700 elderly patients admitted to the ICU after non-cardiac surgery and found that preoperative hypoalbuminemia was associated with an increased risk of postoperative delirium (31). Similarly, we found the decrease in albumin level is a risk factor of developing delirium in CICU patients. Furthermore, albumin alone revealed an inverse linear correlation with delirium, and its predictive performance was superior to those of PNI and GNRI and similar to that of CONUT. Compared with other variables included in nutritional indices, only albumin showed a linear correlation with delirium. Therefore, albumin might be a helpful and simple indicator for predicting delirium in CICU patients. This finding should be validated in future studies, and the mechanism of the relationship between albumin and delirium should be investigated further.
Although this study provides additional information on the associations of albumin and nutritional indices with delirium in CICU patients, several limitations should be noted. First, our study used nonrandomized registry data. Therefore, selection bias and confounding factors might have affected our results. Second, we evaluated delirium only using CAM-ICU. However, the CAM-ICU is generally used for delirium assessment in general ICUs, and we used this tool for routine practice in ICU management including CICU. Finally, we did not include individual information on nutritional support during CICU management collect pre albumin level for comparing albumin for nutritional status. Further studies including detailed knowledge of nutritional support would be informative.
Conclusion
Predictive performances of nutritional indices for the occurrence of delirium were acceptable, and albumin alone as a component of nutritional indices might be a simple and helpful indicator of delirium in patients admitted to a CICU.
Data availability statement
The raw data supporting the conclusions of this article will be made available by the authors, without undue reservation.
Ethics statement
The studies involving human participants were reviewed and approved by the Institutional Review Board of Samsung Medical Center approved this study (IRB. No. 2020-10-102) and waived the requirement for informed consent because of the observational nature of the study.
Author contributions
TK, RK, SN, CC, KC, C-MP, and JY contributed to conception and design of the study. TK, SN, CC, and KC organized the database. TK, RK, and JY performed the data analysis and interpretation. TK wrote the first draft of the manuscript. TK, RK, C-MP, and JY revised the manuscript. All authors contributed to manuscript revision, read, and approved the submitted version.
Conflict of interest
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
Publisher’s note
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
Abbreviations
ALC, absolute lymphocyte count; AUROC, area under the receiver operating characteristic curve; CAM-ICU, confusion assessment method for the intensive care unit; CI, confidence interval; CICU, cardiac intensive care unit; CONUT, Controlling Nutritional Status; GNRI, Geriatric Nutritional Risk Index; IBW, ideal bodyweight; ICU, intensive care unit; OR, odds ratio; PNI, Prognostic Nutrition Index.
References
1.Ely, EW, Shintani, A, Truman, B, Speroff, T, Gordon, SM, Harrell, FE Jr, et al. Delirium as a predictor of mortality in mechanically ventilated patients in the intensive care unit. JAMA. (2004) 291:1753–62. doi: 10.1001/jama.291.14.1753
2.Girard, TD, Thompson, JL, Pandharipande, PP, Brummel, NE, Jackson, JC, Patel, MB, et al. Clinical phenotypes of delirium during critical illness and severity of subsequent long-term cognitive impairment: a prospective cohort study. Lancet Respir Med. (2018) 6:213–22. doi: 10.1016/S2213-2600(18)30062-6
3.Holland, EM, and Moss, TJ. Acute noncardiovascular illness in the cardiac intensive care unit. J Am Coll Cardiol. (2017) 69:1999–2007. doi: 10.1016/j.jacc.2017.02.033
4.Grotti, S, and Falsini, G. Delirium in cardiac patients. Eur Heart J. (2017) 38:2244. doi: 10.1093/eurheartj/ehx380
5.Falsini, G, Grotti, S, Porto, I, Toccafondi, G, Fraticelli, A, Angioli, P, et al. Long-term prognostic value of delirium in elderly patients with acute cardiac diseases admitted to two cardiac intensive care units: a prospective study (DELIRIUM CORDIS). Eur Heart J Acute Cardiovasc Care. (2018) 7:661–70. doi: 10.1177/2048872617695235
6.Ritchie, C, Walters, RW, Ramaswamy, S, and Alla, VM. Impact of delirium on mortality in patients hospitalized for heart failure. Int J Psychiatry Med. (2021) 57:212–25. doi: 10.1177/00912174211028019
7.Ringaitienė, D, Gineitytė, D, Vicka, V, Žvirblis, T, Šipylaitė, J, Irnius, A, et al. Impact of malnutrition on postoperative delirium development after on pump coronary artery bypass grafting. J Cardiothorac Surg. (2015) 10:74. doi: 10.1186/s13019-015-0278-x
8.Buzby, GP, Mullen, JL, Matthews, DC, Hobbs, CL, and Rosato, EF. Prognostic nutritional index in gastrointestinal surgery. Am J Surg. (1980) 139:160–7. doi: 10.1016/0002-9610(80)90246-9
9.Bouillanne, O, Morineau, G, Dupont, C, Coulombel, I, Vincent, JP, Nicolis, I, et al. Geriatric nutritional risk index: a new index for evaluating at-risk elderly medical patients. Am J Clin Nutr. (2005) 82:777–83. doi: 10.1093/ajcn/82.4.777
10.Ignacio de Ulibarri, J, Gonzalez-Madrono, A, de Villar, NG, Gonzalez, P, Gonzalez, B, Mancha, A, et al. CONUT: a tool for controlling nutritional status. First validation in a hospital population. Nutr Hosp. (2005) 20:38–45.
11.Na, SJ, Chung, CR, Jeon, K, Park, CM, Suh, GY, Ahn, JH, et al. Association between presence of a cardiac intensivist and mortality in an adult cardiac care unit. J Am Coll Cardiol. (2016) 68:2637–48. doi: 10.1016/j.jacc.2016.09.947
12.Devlin, JW, Skrobik, Y, Gelinas, C, Needham, DM, Slooter, AJC, Pandharipande, PP, et al. Clinical practice guidelines for the prevention and Management of Pain, agitation/sedation, delirium, immobility, and sleep disruption in adult patients in the ICU. Crit Care Med. (2018) 46:e825–73. doi: 10.1097/CCM.0000000000003299
13.Alvares-da-Silva, MR, and Reverbel da Silveira, T. Comparison between handgrip strength, subjective global assessment, and prognostic nutritional index in assessing malnutrition and predicting clinical outcome in cirrhotic outpatients. Nutrition. (2005) 21:113–7. doi: 10.1016/j.nut.2004.02.002
14.Li, W, Li, M, Wang, T, Ma, G, Deng, Y, Pu, D, et al. Controlling nutritional status (CONUT) score is a prognostic factor in patients with resected breast cancer. Sci Rep. (2020) 10:6633. doi: 10.1038/s41598-020-63610-7
15.Colantuoni, E, Dinglas, VD, Ely, EW, Hopkins, RO, and Needham, DM. Statistical methods for evaluating delirium in the ICU. Lancet Respir Med. (2016) 4:534–6. doi: 10.1016/S2213-2600(16)30138-2
16.Pazan, F, and Wehling, M. Polypharmacy in older adults: a narrative review of definitions, epidemiology and consequences. Eur Geriatr Med. (2021) 12:443–52. doi: 10.1007/s41999-021-00479-3
17.DeLong, ER, DeLong, DM, and Clarke-Pearson, DL. Comparing the areas under two or more correlated receiver operating characteristic curves: a nonparametric approach. Biometrics. (1988) 44:837–45. doi: 10.2307/2531595
18.Pauley, E, Lishmanov, A, Schumann, S, Gala, GJ, van Diepen, S, and Katz, JN. Delirium is a robust predictor of morbidity and mortality among critically ill patients treated in the cardiac intensive care unit. Am Heart J. (2015) 170:79–86.e1. doi: 10.1016/j.ahj.2015.04.013
19.Ibrahim, K, McCarthy, CP, McCarthy, KJ, Brown, CH, Needham, DM, Januzzi, JL Jr, et al. Delirium in the cardiac intensive care unit. J Am Heart Assoc. (2018) 7:e008568. doi: 10.1161/JAHA.118.008568
20.Chang, YL, Tsai, YF, Lin, PJ, Chen, MC, and Liu, CY. Prevalence and risk factors for postoperative delirium in a cardiovascular intensive care unit. Am J Crit Care. (2008) 17:567–75. doi: 10.4037/ajcc2008.17.6.567
21.Jentzer, JC, van Diepen, S, Barsness, GW, Katz, JN, Wiley, BM, Bennett, CE, et al. Changes in comorbidities, diagnoses, therapies and outcomes in a contemporary cardiac intensive care unit population. Am Heart J. (2019) 215:12–9. doi: 10.1016/j.ahj.2019.05.012
22.Pisani, MA, Murphy, TE, Araujo, KL, Slattum, P, Van Ness, PH, and Inouye, SK. Benzodiazepine and opioid use and the duration of intensive care unit delirium in an older population. Crit Care Med. (2009) 37:177–83. doi: 10.1097/CCM.0b013e318192fcf9
23.Velayati, A, Vahdat Shariatpanahi, M, Shahbazi, E, and Vahdat, SZ. Association between preoperative nutritional status and postoperative delirium in individuals with coronary artery bypass graft surgery: a prospective cohort study. Nutrition. (2019) 66:227–32. doi: 10.1016/j.nut.2019.06.006
24.Yang, Y, Zhao, X, Gao, L, Wang, Y, and Wang, J. Incidence and associated factors of delirium after orthopedic surgery in elderly patients: a systematic review and meta-analysis. Aging Clin Exp Res. (2021) 33:1493–506. doi: 10.1007/s40520-020-01674-1
25.Sugita, Y, Miyazaki, T, Shimada, K, Shimizu, M, Kunimoto, M, Ouchi, S, et al. Correlation of nutritional indices on admission to the coronary intensive care unit with the development of delirium. Nutrients. (2018) 10:1712. doi: 10.3390/nu10111712
26.Fanali, G, di Masi, A, Trezza, V, Marino, M, Fasano, M, and Ascenzi, P. Human serum albumin: from bench to bedside. Mol Asp Med. (2012) 33:209–90. doi: 10.1016/j.mam.2011.12.002
27.Yeh, DD, Johnson, E, Harrison, T, Kaafarani, HMA, Lee, J, Fagenholz, P, et al. Serum levels of albumin and Prealbumin do not correlate with nutrient delivery in surgical intensive care unit patients. Nutr Clin Pract. (2018) 33:419–25. doi: 10.1002/ncp.10087
28.Soeters, PB, Wolfe, RR, and Shenkin, A. Hypoalbuminemia: pathogenesis and clinical significance. JPEN J Parenter Enteral Nutr. (2019) 43:181–93. doi: 10.1002/jpen.1451
29.Knaus, WA, Wagner, DP, Draper, EA, Zimmerman, JE, Bergner, M, Bastos, PG, et al. The APACHE III prognostic system. Risk prediction of hospital mortality for critically ill hospitalized adults. Chest. (1991) 100:1619–36. doi: 10.1378/chest.100.6.1619
30.Ahmed, S, Leurent, B, and Sampson, EL. Risk factors for incident delirium among older people in acute hospital medical units: a systematic review and meta-analysis. Age Ageing. (2014) 43:326–33. doi: 10.1093/ageing/afu022
Keywords: delirium, albumin, malnutrition, cardiac intensive care unit, nutrition indexes
Citation: Kim TW, Ko RE, Na SJ, Chung CR, Choi KH, Park C-M and Yang JH (2023) Associations of albumin and nutritional index factors with delirium in patients admitted to the cardiac intensive care unit. Front. Cardiovasc. Med. 10:1100160. doi: 10.3389/fcvm.2023.1100160
Edited by:
Thomas A. Zelniker, Medical University of Vienna, AustriaReviewed by:
Jiuann Huey Lin, University of Pittsburgh, United StatesDae-Hwan Bae, Chungbuk National University Hospital, Republic of Korea
Copyright © 2023 Kim, Ko, Na, Chung, Choi, Park and Yang. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Jeong Hoon Yang, amh5c21jQGdtYWlsLmNvbQ==
†These authors have contributed equally to this work
 Tae Wan Kim
Tae Wan Kim Ryoung Eun Ko
Ryoung Eun Ko Soo Jin Na1
Soo Jin Na1 Jeong Hoon Yang
Jeong Hoon Yang