- 1Public Health Faculty, Sriwijaya University, Kota Palembang, Indonesia
- 2Research Center for Public Health and Nutrition, National Research and Innovation Agency, Cibinong, Indonesia
- 3Health Development Policy Agency, Ministry of Health, Jakarta, Indonesia
- 4Department of Public Health, Universitas Indonesia Maju, Jakarta, Indonesia
Background: Health workers who should be role models for the community not to smoke and live a healthy life are still consuming cigarettes. Java and Bali (especially Java) are the biggest contributors to health worker deaths due to COVID-19 in Indonesia. This study aims to determine the association of smoking behavior and hypertension among health workers in Java and Bali. The researchers conducted this study in 2021 and designed it with a cross-sectional design. Data was collected online using the Lime Survey as a data collection tool. The data analysis used was logistic regression to determine the association of smoking and hypertension.
Result: A number of 7.6% of health workers were still smoking and 10.4% were suffering from hypertension during the COVID-19 pandemic. This study shows that the proportion of health workers with hypertension is two times that of smokers (18.0%) compared to non-smokers (9.8%). Logistic regression showed that smoking has a 20% higher risk of developing hypertension (OR = 1.97; 95%CI = 1.01–1.41; p = 0.034).
Conclusion: Among health workers on the islands of Java and Bali, there are still many who smoke, and this puts them at a higher risk of experiencing hypertension.
1. Introduction
Tobacco use has caused the death of more than 200 million people over the last 30 years (1). Cigarette smoking and other tobacco use impose a growing public health burden globally (2). More than 8 million people die yearly from smoking tobacco. Approximately 5 million people are killed annually by tobacco use (3). The harmful effects of smoking are responsible for illness, death, and impoverishment, extending well beyond individual and population health as billions of dollars in lost productivity and healthcare expenditure (4).
Indonesia has the third-highest smoking prevalence globally, only after China and India (5). According to the World Bank report, nearly 40% of the total population with age equal to or above 15 years smoke, while 76% of Indonesian males are the highest smoker group globally (6). This nation contributed to 60 million active smokers in the world. The smoking prevalence has remained high from 34.7% in 2007, 36.5% in 2013, and 33.8% in 2018 (6, 7). Based on the WHO Framework Convention on Tobacco Control, health workers have an important role to play in reducing the prevalence of smokers through smoking cessation efforts (8), including in Indonesia.
Indonesia has health workers spread across Indonesia to help smokers stop smoking. Smokers are also more likely to quit smoking when they receive counseling from health workers (9). Unfortunately, there are still health workers who are active smokers, so this condition contributes to the prevalence rate of smokers and hinders smoking cessation programs in Indonesia (10, 11). Health workers who should be role models for the community not to smoke and live a healthy life are still consuming cigarettes (12, 13). Health workers should not smoke cigarettes because they should become role models for the community to control tobacco.
East Java and Central Java are the largest tobacco industrial areas in Indonesia (14). Most governments on the islands of Java and Bali have implemented Smoke-Free Areas. Regional rules regarding smoke-free areas have been introduced at the provincial and district/city levels. These regulations encompass health care facilities as one of the designated smoke-free areas (15–17). However, there are still many smoking health workers in the area. Some health workers on the island of Java smoke because they are tired after work (11). Study in Grobogan, Central Java found that 35% of health service employee were smoked (18), likewise it was found that 36% of health workers aged 31–40 in Bali (10). The negative impact of smoking behavior also threatens the health condition of health workers. Study said that physician smokers tend to be associated with hypertension and obesity (19). The condition of hypertension in health workers in Indonesia can be seen in research conducted in Palembang (20).
Smoking health workers exacerbates the pandemic because smoking is a risk factor for the severity and death of Covid-19 (21). Furthermore, another study also explained that the prediction of the incidence of hypertension in workers by 9% could occur due to the influence of daily cigarette consumption, and the number of cigarettes used reached 10–20 cigarettes/day (22). However, the impact of smoking behavior on health workers still requires further evidence, especially in Java and Bali, because they have the most significant number of health workers in Indonesia. Even so, there is little evidence of smoking behavior among health workers and its implications for smoking-related diseases in Java and Bali, Indonesia. This study aims to determine the association of smoking behavior and hypertension among health workers in Java and Bali. This study is necessary to provide evidence of smoking prevalence from the health personnel sector to strengthen the tobacco control effort in Indonesia.
2. Material and methods
This cross-sectional study used data from a study mapping the risk behavior of non-communicable diseases among employees at the relevant Provincial/District/City/ Regional Technical Implementation Units (UPTD) Health Offices in Java and Bali. The study population was health workers in all areas of Java and Bali and all relevant provincial/city/district/UPTD health office employees. The majority of health workers who died due to COVID-19 came from the medical profession, namely 730 people, 670 nurses, and 388 midwives. East Java occupies the top position as the province with the highest number of deaths from health workers in Indonesia, namely 643 people. West Java and Central Java are followed with a total of 225 health personnel deaths and 193 people, respectively. Health workers in Indonesia who died due to COVID-19 and health workers who died due to comorbid or congenital diseases. Java and Bali (especially Java) are the biggest contributors to the deaths of health workers in Indonesia (23).
This research uses online data collection because the ongoing threat of the COVID-19 outbreak still needs to be monitored. There is an appeal from the Indonesian government to continue limiting people's movements due to COVID-19. Researchers conducted pre-test trials to determine the validity and reliability of the questionnaire and estimate the time required for respondents to complete it. This trial was conducted online in August 2021 in West Nusa Tenggara Province. At the trial stage, the validity of the smoking question was good, but the reliability was low. To increase reliability, the research team improved the narrative of the smoking question so that it was easier for respondents to understand and be consistent in answering, then the questionnaire being used for collecting data. The trial showed a self-report duration of 10–15 min. This study was conducted from September to October 2021. Questionnaire have been changed to digital form in the LimeSurvey application. LimeSurvey is an online survey platform that has easy facilities for preparing templates, sending surveys, and analyzing results at affordable prices. The questionnaire link are distributed to all respondents through the provincial health office structure to the puskesmas or other UPTD Health Office. The UPTD of the health office includes regional hospitals, health laboratories, and health centers. The sampling technique for online data collection can be non-probability sampling. This method involves selecting a sample of participants based on non-random criteria. Non-probability sampling may be less representative than probability sampling, but it can still provide useful information (24).The research received significant respondents (21,095) at the end of data collection. Using the formula of the Lemeshow health study sample for two-sample hypothesis testing of proportions (25), an estimated prevalence of hypertension in the smoker group was 21,22%, and the prevalence of hypertension in the non-smoker group was 19,06% based on the previous study (26) and a 95% confidence interval 0.10 wide (0.05 on either side), the minimum sample required was 16,978. Thus, the number of samples we analysed was larger than the minimum needed.
The outcome variable in this study was hypertension from self-reporting blood pressure in the last month. Hypertension was categorized inti two groups: normal if systolic <140 mmHg and diastolic <90 mmHg; hypertension if systolic ≥140 mmHg or the diastolic ≥90 (27).
The independent variable was smoking behavior and socio-demographic factors, including education, age, and gender. The researchers divided respondents who smoke into two groups: respondents who do not smoke (never smoke or former) and respondents who smoke (occasional and every day).
Data were analyzed using SPSS software. The data analysis used is a descriptive statistical analysis to see the characteristics of the data and logistic regression analysis to determine the association between smoking behavior and the incidence of hypertension. The researchers measured the significant relationship at the 0.05 significance level.
2. Results
2.1. Characteristics of respondents
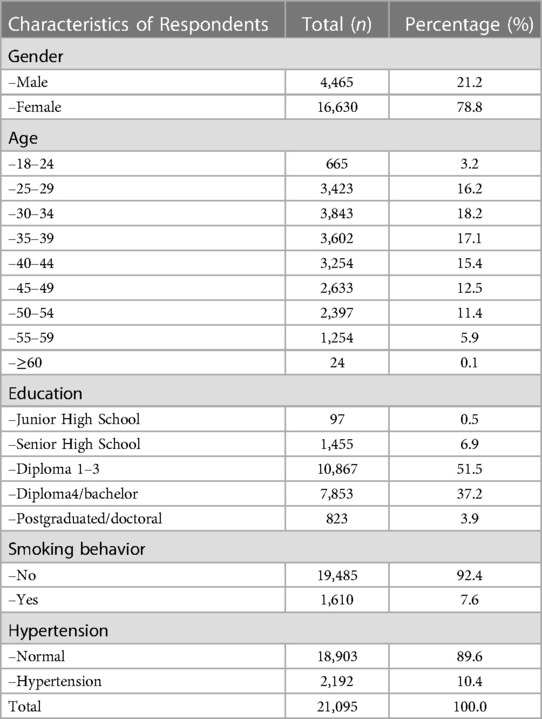
Table 1 is a descriptive demographic of the character of the Provincial/City/Regency/UPTD Health Office employees who participated in this survey. The results show the majority who took part in this survey were female, amounting to 78.8% (16,630), while only 21.2% (4,465) were male. Respondents with education level Diploma 1–3 are the most respondents with a percentage of 51.5% (10,867). The second-largest number of respondents, when viewed from the level of education, are respondents with Diploma to bachelor education, which is 37.2% (7,853). Also, in Table 1, respondents aged 30–34 years are respondents with the highest proportion, namely 18.2% (3,843). The second-largest age group is respondents aged 35–39, as much as 17.1% (3,602). Several 7.6% of health workers were still smoking and 10.4% were suffering from hypertension during the COVID-19 pandemic.
2.2. Smoking behavior of health workers in Java and Bali
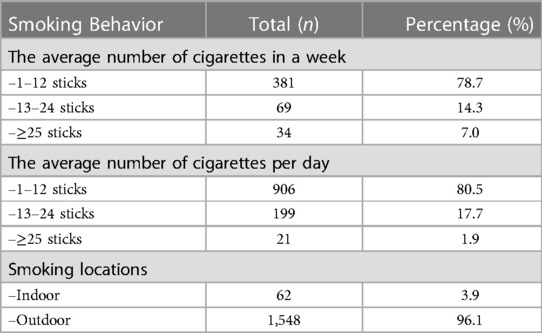
Table 2 describes the two groups of smokers: researchers divided respondents who smoke into two groups: respondents who do not smoke every day (sometimes) and respondents who smoke every day. Among them, 34 respondents (7.0%) who did not smoke daily reported spending more than 25 cigarettes weekly. The highest number of smokers consume 1–12 cigarettes weekly (381 respondents or 78.7%). In addition, the average number of cigarettes consumed daily is 1–12 cigarettes a day (80.5%), but some employees smoke more than 25 daily (1.9%). Most smokers smoked outdoors (1,548 respondents or 96.1%). However, some smokers smoke indoors (62 respondents or 3.9%).
2.3. Association between smoking behavior and hypertension category
Table 3 shows that the proportion of health workers with hypertension is two times that of smokers (18.0%) compared to non-smokers (9.8%). A significant association between smoking behavior and the hypertension category of health workers in Java and Bali in 2021. That can be seen from logistic regression showed that smoking has a 20% higher risk of developing hypertension (OR = 1.97; 95%CI = 1.01–1.41; p = 0.034).

Table 3. Logistic regression between smoking behavior and hypertension of health workers in Java and Bali in 2021.
3. Discussion
This study's main finding proves that health personnel still become active smokers, 8.38% of the total respondents. Nevertheless, health personnel should give an example to stop smoking. It becomes essential to do a depth analysis. The findings of this study are still higher than the study in the U.S., which found that the prevalence of smoking among health professionals was minor than 6% (28). This study's finding is also higher than Malaysia's, which found that the overall smoking prevalence of health workers was 1.6% (29).
Currently, the prevalence of tobacco use in healthcare workers worldwide is unknown (30). Research showed that compared to men in the general population in low- and lower-middle-income countries, including Indonesia, male health workers have a 20% higher prevalence of smoking among health workers. However, it is still lower than in Armenia, Syria (30%), Pakistan, and Tunisia (50%). Meanwhile, the prevalence of smoking among female health workers in Indonesia, Nepal, and Syria tends to have a lower prevalence (<5%) and is highest in Armenia and Pakistan (<15%) (30). These results align with research in Asia which found that the smoking behavior of male health workers is higher than that of female health workers (31).
Previous research on Sumatra, Indonesia, found that 75.6% of Tebing Tinggi City health service employees smoked (32). Several factors, including knowledge about smoking and the smoking behavior of colleagues, can influence smoking behavior among health workers. The behavior of co-workers is very influential; in fact, up to 32% of smoker respondents share cigarettes with co-workers, and 54% do not recommend that co-workers who smoke move to the designated smoking room available (18). As many as 17.8% of health service employees and smokers who do not agree with the implementation of smoke-free areas, but they agree that smoking also impacts non-smokers around them (32).
On the contrary, a study in Italy found that smoking prevalence among hospital employees was 47% (42% among doctors and 43% among nurses); 30% admit to smoking in hospitals, and three-quarters of smokers want to quit (33). This figure is greater than the findings of this study. The study implies that smoking among healthcare professionals may still be very high and maybe twice the level observed in the general population included in this study. It could happen because health workers from high-income countries tend to have lower prevalence rates than those from middle- and low-income countries (30, 34).
Cases of health workers who smoke mostly come from those with low incomes, fewer years of formal education, and specific nursing specialties (25). Another study showed that work stress was most associated with nurses who graduated from high school, lack of nurses, nurses who had many overtime hours, nurses with the most shifts, and the lowest level of education (35). The findings are similar to this study. Another factor is the cultural norms of smoking behavior which are still readily accepted by the Indonesian population so that health personnel can still reach these norms, so they decide to become active smokers (36).
This study also proves that health personnel who smoke have a history of grade 1 hypertension (14.7%), grade 2 hypertension (2.9%), and critical hypertension (0.4%). Various studies in Indonesia are also in line with the result of this study. They revealed the negative impacts of smoking from decreased productivity experienced by young people, which can cause catastrophic diseases, including diabetes, heart disease, and various types of cancer (1, 37, 38). In addition to causing an addictive effect, this nicotine product can cause hypertension by binding to the blood. An unhealthy lifestyle, such as consuming junk food and lacking physical activity, also supports this, but it was unobserved in this study.
Hypertension is a global health problem, especially in low- and middle-income countries (39). Based on a study by Prakash Ghimire et al., the prevalence of hypertension among health workers in Nepal was 35.31%. The factors influencing this are age, education level, marital status, low vegetable and fruit consumption, low physical activity, alcohol consumption, and stress levels (40). Research from Po-Ya Chang on hypertension in nurses in Taiwan informs us that factors that influence nurses who suffer from hypertension are stress levels, age, BMI, working hours a week, and taking care of family members (41).
The results of the research conducted by Tantya Issumantri stated that smoking employees at the Kulon Progo puskesmas continued to smoke as usual in the puskesmas area, even though there had been regulations prohibiting smoking in the puskesmas environment. Even the officers did not reprimand or remind them if visitors to the puskesmas smoked in that environment (42). That shows that health workers are also less concerned about smoking behavior, which can impact health. Alya Binda Ulinuha et al. corroborated this research, concluding that health workers who smoke are already aware of the adverse effects of smoking. However, they believe smoking will bring them peace, health, and the absence of disease symptoms. Health workers who smoke intend to quit, but determination and execution are still lacking (11).
Another study finding is that the percentage of health workers exposed to cigarette smoke daily is still relatively high at 26.36%. It has the same finding with the exposure to second-hand smoke of health workers in Malaysia; it was 21% and 39% at home and in public places (29). It happens because certain spots, such as parking lots, behind the building, or outside areas close to the building's surroundings, do not cover the smoke-free area. Another extreme possibility is exposure to second-hand smoke in inpatient, office management, and administration rooms (33, 34). In addition, 85% of the population is still exposed to cigarette smoke in public places, supported by the weak regulation of smoke-free areas in public transportation, universities, and education places in Indonesia compared to other Asian countries (43). Air quality is also affected by cigarette smoke. Air measurements conducted at several primary healthcare facilities in Spain that are part of the Smoke-free Primary Health Care Programme have shown that there is still exposure to cigarette smoke in specific areas such as staff rooms and reception areas. These areas had the highest levels of airborne nicotine with maximum values of 1.40 and 0.60 mg/m3, respectively (19). This second-hand smoke issue causes a somewhat dangerous impact on clinical and hospital health services.
Health personnel should not smoke cigarettes because they should become a role model for the community to control tobacco. The 2024 National Medium-Term Development Plan targets 350 districts/cities with 40% of primary health care providing Stop Smoking Services by 2024 in Indonesia (44). Fulfilling this target may experience obstacles whether health personnel is still against tobacco control efforts. In addition, Indonesia's National Health Insurance (NHI) had to cover IDR 10.5–15.5 trillion or around 56%–59% of the total healthcare costs for smoking-related diseases in 2019 (45). Those diseases are suffered by NHI participants which are include health and non-health personnel. Data regarding the burden of claims for smoking-related illnesses suffered by health personnel nationally still requires further research. This burden requires the role of health workers and awareness of health workers not to become smokers.
The COVID-19 pandemic has put health systems around the world under stress. During the handling of Covid-19, health workers were the party most at risk of exposure to hazards, including exposure, long working hours, psychological stress, fatigue, work fatigue, stigma, and physical (46). The health workforce is one of the six building blocks of the health system recognized by WHO (47), which is the key to the health system, having the ability to deal with external shocks such as outbreaks (48).
The ongoing role of health workers in long-term recovery after a pandemic provides evidence for the role of health workers in pandemic preparedness and strengthening the public health system (49). The vital role of health workers in dealing with a pandemic includes (1) facilitating vaccinations and appointments in all areas with low vaccination rates. Health workers deal with various challenges in the pandemic, including virus problems, mental health issues, and obstacles in vaccine access. They tackle these challenges by (1) building trust with the community through involvement in community activities, increasing community recognition, and promoting accessibility to support services; and (2) sustaining progress in public health despite funding instability (50). The role of health workers is not only as assistants but also as agents of social change and community activation (51). This critical role leaves Health workers well-positioned to respond in times of crisis but also to work for long-term recovery and rebuilding, promoting community resilience (52).
Indonesia already has the principal tobacco control regulations that apply to all circles, namely Government Regulation no. 109 of 2012 concerning the Safety of Materials Containing Addictive Substances in the Form of Tobacco Products for Health (53). However, the regulation, which is already ten years old, urgently needs revision to keep up with current developments. One of these developments is the need to include health workers in tobacco control efforts. Minister of Home Affairs Regulation Number 17 of 2021 concerns guidelines for preparing local government work plans for 2022. This regulation will at least increase the number of Public Health Centers (Puskesmas) that support tobacco control and establish smoking cessation services. On the other hand, Indonesia still needs to sign or ratify the FCTC; MPOWER guides the country's national health policy and tobacco control strategy. However, in collaboration with non-governmental organizations (NGOs), the government has demonstrated some commitment to addressing tobacco-related health issues (14).
This study is one of the research projects that reveal a controversial issue, and they are the findings of smoking behavior among civil servants and health personnel. To the author's knowledge, there have been rare instances of this conducted in Indonesia. However, conducting an online study raises the potential for bias and uneven distribution of the sample, including more women in the sex group, which is a limitation of this study. Future studies can improve the result of this study by conducting face-to-face in-depth interviews with health workers to explore the causes of their continuing smoking behavior and the most appropriate cessation method for them.
4. Conclusions
This study shows that there are still smokers among health workers during the COVID-19 pandemic (7.6%), as well as those who suffer from hypertension (10.4%). The proportion of hypertension is higher in smokers (18.0%). and smokers have a higher risk of developing hypertension. The Government of Indonesia and medical and health associations need to formulate strict policies and sanctions for the health personnel proven to have smoking behavior. Health facilities need to apply strict sanctions to health personnel proven to smoke. All health personnel must be role models for not smoking and support Indonesia's goal of developing a smoking cessation clinic in primary health care. Researchers must conduct further studies to investigate the causes of smoking behavior among health workers and identify the most suitable cessation methods to encourage them to quit smoking.
Data availability statement
The data that support the findings of this study are available from the Data Management Laboratory of the National Institute of Health Research and Development (NIHRD), Ministry of Health of Indonesia. Data can be made available after approval of a written request to the Data Management Laboratory—NIHRD. Requests to access the datasets should be directed to dGV0eXIyNzIwMDJAZ21haWwuY29t.
Ethics statement
Ethical approval for the research was obtained from the ethics committee of the Health Research and Development Agency, Ministry of Health of Indonesia Number LB. 02.01./1/KE.091/2021 and informed consent from the respondents. The patients/participants provided their written informed consent to participate in this study.
Author contributions
All authors contributed equally to the study. M, WN, and TR were involved in the conception and design of the study, while ZN and FR were responsible for organizing the database and conducting the statistical analysis. M, WN, TR, and RH wrote the first draft of the manuscript. TR, RH, ZN, RM, and AK wrote sections of the manuscript. All authors contributed to the article and approved the submitted version.
Funding
The Center for Humanities and Health Management, The Agency for Health Research and Development, Ministry of Health—of the Republic of Indonesia funded this research through their DIPA budget for 2021.
Acknowledgment
The authors would like to express their gratitude and appreciation to all health workers on duty at the health services in Java and Bali who have been willing to become respondents to this research. We would also like to thank the Directorate of Health Promotion and the Center for Humanities and Health Management, the Indonesian Ministry of Health, who have supported and facilitated the data collection of this research.
Conflict of interest
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
Publisher's note
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
References
1. Reitsma MB, Kendrick PJ, Ababneh E, Abbafati C, Abbasi-Kangevari M, Abdoli A, et al. Spatial, temporal, and demographic patterns in prevalence of smoking tobacco use and attributable disease burden in 204 countries and territories, 1990–2019: a systematic analysis from the global burden of disease study 2019. Lancet. (2021) 397(10292):2337–60. doi: 10.1016/S0140-6736(21)01169-7
2. Blackadar CB. Historical review of the causes of cancer. World J Clin Oncol. (2016) 7:54–86. doi: 10.5306/wjco.v7.i1.54
3. Reitsma MB, Fullman N, Ng M, Salama JS, Abajobir A, Abate KH, et al. Smoking prevalence and attributable disease burden in 195 countries and territories, 1990–2015: a systematic analysis from the global burden of disease study 2015. Lancet. (2017) 389(10082):1885–906. doi: 10.1016/S0140-6736(17)30819-X
4. West R. Tobacco smoking: health impact, prevalence, correlates and interventions. Psychol Heal. (2017) 32(8):1018–36. doi: 10.1080/08870446.2017.1325890
5. Zheng R, Marquez PV, Ahsan A, Wang Y, Hu X. Cigarette affordability in Indonesia: 2002–2017. Washington, DC: World Bank (2018).
6. Health Development Policy Agency. Adult smokers in Indonesia have increased in the last ten years. Jakarta: Health Development Policy Agency (2022).
7. NIHRD IM. Laporan nasional riset kesehatan dasar 2018. Jakarta: Lembaga Penerbit Badan Litbangkes (2018).
8. World Health Organization. WHO Framework convention on tobacco control. Geneva: World Health Organization (2003).
9. Erawati M, Andriany M. The prevalence and demographic risk factors for latent tuberculosis infection (LTBI) among healthcare workers in semarang, Indonesia. J Multidiscip Healthc. (2020) 13:197–206. doi: 10.2147/JMDH.S241972
10. Aryda LNT, Sundari LPR. Profil perokok pada tenaga kesehatan di rumah sakit jiwa provinsi bali. E-J Med Udayana. (2015) 4(3):1–15. Available at: https://ojs.unud.ac.id/index.php/eum/article/view/12928/8695.
11. Ulinuha AB, Widjanarko B, Indraswari R. Gambaran perilaku merokok tenaga kesehatan di puskesmas kaliwiro kabupaten wonosobo tahun 2021. MEDIA Kesehat Masy Indones. (2022) 21(6):363–73. doi: 10.14710/mkmi.21.6.363-373
12. Lobelo F, de Quevedo IG. The evidence in support of physicians and health care providers as physical activity role models. Am J Lifestyle Med. (2016) 10:36–52. doi: 10.1177/1559827613520120
13. Perry L, Xu X, Gallagher R, Nicholls R, Sibbritt D, Duffield C. Lifestyle health behaviors of nurses and midwives: the ‘fit for the future’ study. Int J Environ Res Public Health. (2018) 15(5):1–16. doi: 10.3390/ijerph15050945
14. Kusumawardani N, Tarigan I, Suparmi Schlotheuber A. Socio-economic, demographic and geographic correlates of cigarette smoking among Indonesian adolescents: results from the 2013 Indonesian basic health research (RISKESDAS) survey. Glob Health Action. (2018) 11(1):1–9. doi: 10.1080/16549716.2018.1467605
15. Province R secretary of Bali. Bali provincial regulation No. 10 of 2011 on smoke-free areas. Denpasar: Province R Secretary of Bali (2011).
16. Ministry of Law and Human Rights Republic of Indonesia. Law of the republic of Indonesia number 36 of 2009 concerning health. Jakarta: Ministry of Law and Human Rights Republic of Indonesia (2009).
17. Regional Secretary of West Java Province. Regional regulation of west Java province number 11 of 2019 concerning non-smoking areas. Bandung: Regional Secretary of West Java Province (2019). Available at: http://jdih.dprd.jabarprov.go.id/dokumen/peraturan-daerah/2019/11
18. Herawardhani A, Widjanarko B, Prabamurti PN. Faktor-Faktor yang berhubungan dengan perilaku merokok pegawai dinas kesehatan kabupaten grobogan. Media Kesehat Masy Indones. (2021) 20(4):268–74. doi: 10.14710/mkmi.20.4.268-274
19. Fernández E, Fu M, Martínez C, Martínez-Sánchez JM, López MJ, Martín-Pujol A, et al. Secondhand smoke in hospitals of catalonia (Spain) before and after a comprehensive ban on smoking at the national level. Prev Med. (2008) 47(6):624–8. doi: 10.1016/j.ypmed.2008.09.003
20. Setiawan TD. Faktor risiko hipertensi esensial pada petugas kesehatan di rumah sakit muhammadiyah palembang skripsi. Palembang: Palembang Muhammadiyah University (2021).
21. Hasni I, Nursal DGA, Markolinda Y, Masrizal M, Yusmayanti Y. Faktor risiko merokok, komorbid dengan keparahan COVID-19 (systematic review & meta-analisis). J Kesmas (Kesehatan Masyarakat) Khatulistiwa. (2022) 9(2):81. doi: 10.29406/jkmk.v9i2.3423
22. Hardati AT, Ahmad RA. Pengaruh aktivitas fisik terhadap kejadian hipertensi pada pekerja (analisis data riskesdas 2013). Ber Kedokt Masy. (2017) 33(10):467. doi: 10.22146/bkm.25783
23. Yayasan Warga Berdaya untuk Kemanusiaan. Health Worker Mortality Statistics. (2023). Available at: https://nakes.laporcovid19.org/statistik (cited 2023 Mar 26).
24. Fricker RD. Sampling methods for online surveys. SAGE Handb Online Res Methods. (2016):162–83. doi: 10.4135/9781473957992
25. Lwanga SK, Lemeshow S, The World Health Organization. Sample size determination in health studies : A practical manual/S. K. Lwanga and S. Lemeshow. Geneva PP—Geneva: World Health Organization (1991). 80. Available at: https://apps.who.int/iris/handle/10665/40062
26. Nar B, Batubara NS, Anastsya R, Juni AR. Factors related to the event of hypertension in early adults in the work area of hulu sihapas puskesmas 2022. Atlantis Press International BV (2023). p. 179–86. Available at: http://dx.doi.org/10.2991/978-94-6463-032-9_26.
27. Armstrong C. JNC 8 Guidelines for the management of hypertension in adult. Am Fam Physician. (2013) 90(7):503–4. Available at: http://www.aafp.org/afp/2014/1001/p503.html
28. Islami F, Torre LA, Jemal A. Global trends of lung cancer mortality and smoking prevalence. Transl Lung Cancer Res. (2015) 4(4):327–38. doi: doi: 10.3978/j.issn.2218-6751.2015.08.04
29. Rahman A, Mambaly M, Keshavarzi F, Baig MAI, Hariadha E, Farrukh MJ. Evaluation of smoking prevalence, second-hand smoke exposure, attitudes of tobacco control, and smoking cessation knowledge among pharmacy and medical students in a private university, Malaysia. J Pharm Bioallied Sci. (2022) 14:38–45. doi: 10.4103/jpbs.jpbs_334_21
30. Nilan K, McKeever TM, McNeill A, Raw M, Murray RL. Prevalence of tobacco use in healthcare workers: a systematic review and meta-analysis. PLoS One. (2019) 14(7):1–26. doi: 10.1371/journal.pone.0220168
31. Rahman A, Huriah T. The smoking behavior of health workers in Asia: a literature review. J Keperawatan Indones. (2021) 24(2):118–30. doi: 10.7454/jki.v24i2.864
32. Khairatunnisa IF. Hubungan persepsi tentang kawasan tanpa rokok (KTR) dengan perilaku merokok pegawai di dinas kesehatan kota tebing tinggi. J JUMANTIK. (2019) 4(1):69–81. doi: 10.30829/jumantik.v4i1.4062
33. Giorgi E, Marani A, Salvati O, Mangiaracina G, Prestigiacomo C, Osborn JF, et al. Towards a smoke-free hospital: how the smoking status of health professionals influence their knowledge, attitude and clinical activity. Results from a hospital in central Italy. Ann Ig. (2015) 27(2):447–59. doi: 10.7416/ai.2015.2031
34. Tong EK, Strouse R, Hall J, Kovac M, Schroeder SA. National survey of U.S. Health professionals’ smoking prevalence, cessation practices, and beliefs. Nicotine Tob Res. (2010) 12(7):724–33. doi: 10.1093/ntr/ntq071
35. Juranić B, Rakošec Ž, Jakab J, Mikšić Š, Vuletić S, Ivandić M, et al. Prevalence, habits and personal attitudes towards smoking among health care professionals. J Occup Med Toxicol. (2017) 12(1):1–8. doi: 10.1186/s12995-017-0166-5
36. Besson A, Tarpin A, Flaudias V, Brousse G, Laporte C, Benson A, et al. Smoking prevalence among physicians: a systematic review and meta-analysis. Int J Environ Res Public Health. (2021) 18(24):1–58. doi: 10.3390/ijerph182413328
37. Moeis F, Hartono RK, Nurhasana R, Satrya A, Dartanto T. Relieving or doubling burden: non-communicable diseases (NCDs) of electronic and conventional cigarette users (dual users) in Indonesia. 2021 AUA ICSGS acad conf (2021). p. 1.
38. Hartono RK, Hamid SA, Hafizurrachman M. Do the number of cigarettes smokes per day contribute to the incident of malignant cancer? Asian Pacific J Cancer Prev. (2019) 20(5):1403–8. doi: 10.31557/APJCP.2019.20.5.1403
40. Ghimire P, Khadka A, Anuwatnonthakate A, Trongsakul S. Prevalence and factors associated with hypertension among health workers of central hospitals in Nepal. The Indones J Health. (2020) 15(3):325-38. doi: 10.20473/ijph.vl15il.2020.325-338
41. Chang PY, Chiou ST, Lo WY, Huang N, Chien LY. Stressors and level of stress among different nursing positions and the associations with hyperlipidemia, hyperglycemia, and hypertension: a national questionnaire survey. BMC Nurs. (2021) 20(1):1–10. doi: 10.1186/s12912-021-00777-y
42. Issumantri T. Perception of smoking employees at puskesmas kulon progo district towards smoking prohibition in health facilities. Yogyakarta: Gadjah Mada University (2015).
43. Nurhasana R, Ratih SP, Djaja K, Hartono RK, Dartanto T. Passive smokers’ support for stronger tobacco control in Indonesia. Int J Environ Res Public Health. (2020) 17(6):1–9. doi: 10.3390/ijerph17061942
44. Indonesia PR. Peraturan Presiden (PERPRES) No. 18 Tahun 2020 tentang Rencana Pembangunan Jangka Menengah Nasional Tahun 2020–2024.
45. Center for Indonesia's Strategic Development Initiatives (CISDI). Beban biaya untuk penyakit terkait merokok 2019. Center for Indonesia's Strategic Development Initiatives. (2021).
46. WHO. Rights, roles and responsibilities of health workers, including critical considerations for occupational safety and health: interim guidance-2. Geneva: World Health Organization (2020). p. 1–2.
47. World Health Organization. Everybody's business : strengthening health systems to improve health outcomes : wHO's Frmaework for action. Geneva: World Health Organization (2007). 44.
48. Hanefeld J, Mayhew S, Legido-Quigley H, Martineau F, Karanikolos M, Blanchet K, et al. Towards an understanding of resilience: responding to health systems shocks. Health Policy Plan. (2018) 33(3):355–67. doi: 10.1093/heapol/czx183
49. Perry HB, Chowdhury M, Were M, LeBan K, Crigler L, Lewin S, et al. Community health workers at the Dawn of a new era: 11. CHWs leading the way to “health for all.”. Health Res Policy Sys. (2021) 19(Suppl 3):1–21. doi: 10.1186/s12961-021-00761-7
50. Nawaz S, Moon KJ, Vazquez R, Navarrete JR, Trinh A, Escobedo L, et al. Evaluation of the community health worker model for COVID-19 response and recovery. J Community Health. (2023) 48(3):430–45. doi: 10.1007/s10900-022-01183-4
51. Rich ML, Miller AC, Niyigena P, Franke MF, Bosco Niyonzima J, Socci A, et al. Excellent clinical outcomes and high retention in care among adults in a community-based HIV treatment program in rural Rwanda. J Acquir Immune Defic Syndr. (2012) 59(3):e35–42. doi: 10.1097/QAI.0b013e31824476c4
52. Chemali S, Mari-Sáez A, El Bcheraoui C, Weishaar H. Health care workers’ experiences during the COVID-19 pandemic: a scoping review. Hum Resour Health. (2022) 20(1):1–17. doi: 10.1186/s12960-022-00724-1
53. Ministry of Law and Human Rights Republic of Indonesia. Government regulation of the Republic of Indonesia number 109 of 2012 concerning the safety of materials containing addictive substances in the form of tobacco products for health. Jakarta: Ministry of Law and Human Rights Republic of Indonesia (2012).
Keywords: COVID-19, smoking, hypertension, health worker smoking, health workers, Java and Bali
Citation: Misnaniarti, Nugraheni WP, Nantabah ZK, Restuningtyas FR, Hartono RK, Rachmawati T, Mubasyiroh R and Kusnali A (2023) Smoking behavior and hypertension among health workers during the COVID-19 pandemic: a case study in Java and Bali-Indonesia. Front. Cardiovasc. Med. 10:1146859. doi: 10.3389/fcvm.2023.1146859
Received: 18 January 2023; Accepted: 18 July 2023;
Published: 14 August 2023.
Edited by:
Al Asyary, University of Indonesia, IndonesiaReviewed by:
Shazia Rehman, Central South University, ChinaRony Darmawansyah Alnur, Universitas Muhammadiyah Prof Dr Hamka, Indonesia
Emma Rachmawati, Universitas Muhammadiyah Prof Dr Hamka, Indonesia
© 2023 Misnaniarti, Nugraheni, Nantabah, Restuningtyas, Hartono, Rachmawati, Mubasyiroh and Kusnali. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Misnaniarti bWlzbmFuaWFydGlAZmttLnVuc3JpLmFjLmlk
 Misnaniarti
Misnaniarti Wahyu Pudji Nugraheni
Wahyu Pudji Nugraheni Zainul Khaqiqi Nantabah
Zainul Khaqiqi Nantabah Fraschiska Rizky Restuningtyas
Fraschiska Rizky Restuningtyas Risky Kusuma Hartono
Risky Kusuma Hartono Tety Rachmawati
Tety Rachmawati Rofingatul Mubasyiroh
Rofingatul Mubasyiroh Asep Kusnali
Asep Kusnali