- 1CAU Thrombosis and Biomarker Center, Chung-Ang University Gwangmyeong Hospital, Gwangmyeong, Republic of Korea
- 2Department of Internal Medicine, Chung-Ang University College of Medicine, Seoul, Republic of Korea
- 3Department of Cardiology and Angiology, University Hospital Tübingen, Eberhard Karls Universtität Tübingen, Tübingen, Germany
- 4Cardiocenter, Third Faculty of Medicine, Charles University and University Hospital Kralovske Vinohrady, Prague, Czech Republic
Editorial on the Research Topic
The individualization of antiplatelet therapy in coronary artery disease: escalation or de-escalations
Among patients with acute coronary syndrome (ACS) undergoing percutaneous coronary intervention (PCI), the use of potent P2Y12 inhibitor (e.g., prasugrel or ticagrelor) is associated with a reduction in ischemic events as well as an increase in bleeding events compared with clopidogrel treatment. Therefore, finding an optimal balance between the efficacy and safety of antiplatelet strategies after PCI (i.e., optimal disease entity, regimen, potency, and duration) has been one of the challenging projects. Recently, the main issue in this field has shifted toward reducing serious bleeding without increasing ischemic risk. Thereafter, numerous clinical trials have evaluated clinical benefits of the de-escalation antiplatelet strategies compared with the conventional strategy (1, 2).
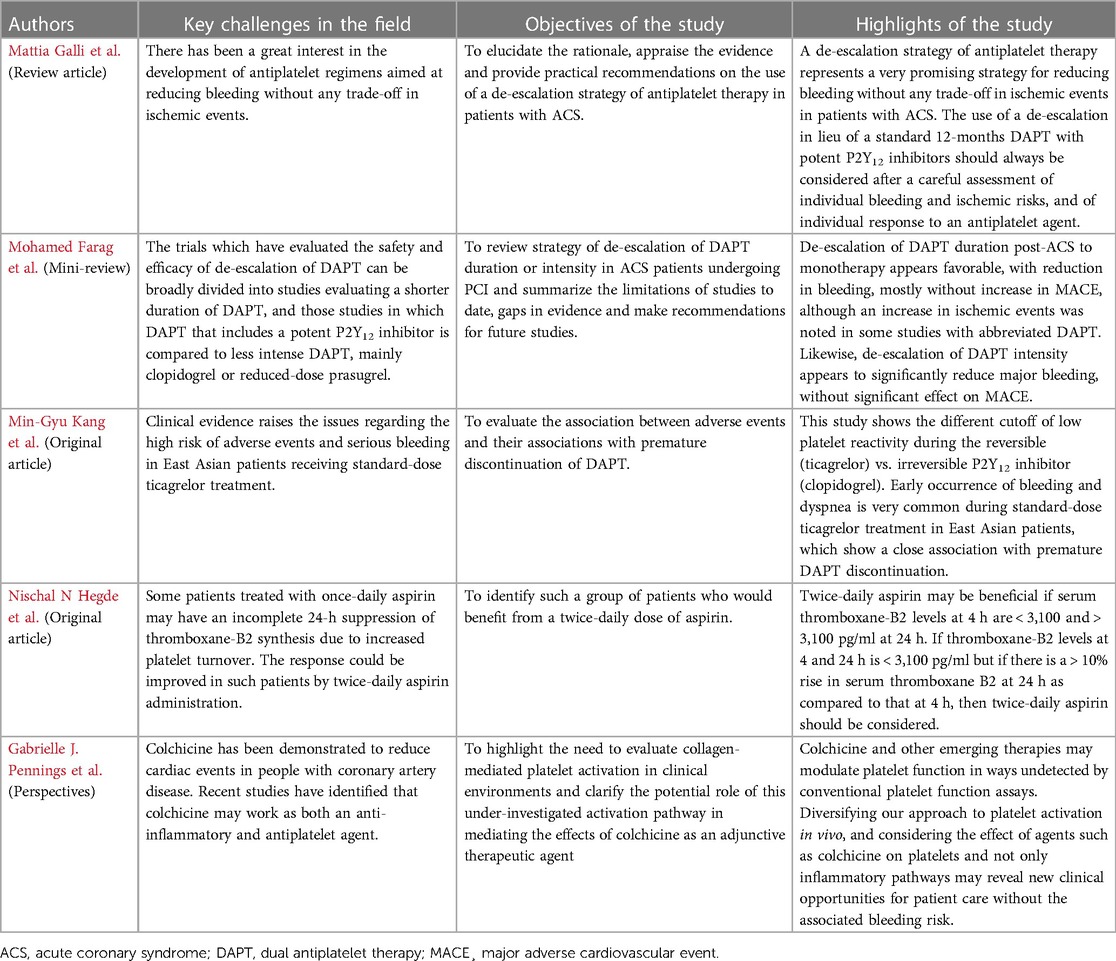
This Research Topic section contains five papers and aims at widening the current knowledge on the personalized antithrombotic therapy, mostly targeting on “de-escalation strategy” of dual antiplatelet therapy (DAPT) in PCI-treated patients with coronary artery disease (CAD).
De-escalation strategy of antiplatelet therapy in acute coronary syndrome: reviews
Two articles reviewed the recent interest in the development of antiplatelet regimens aimed at reducing bleeding without any trade-off in ischemic events. Mattia Galli et al. and Mohamed Farag et al. reviewed the rationale, regimens, timing and combined limitations of “de-escalation antiplatelet strategy” in patients with ACS. De-escalation of DAPT duration appears favorable, with reduction in bleeding, mostly without increase in ischemic events, despite an increase in ischemic events in some studies using abbreviated DAPT. Likewise, de-escalation of DAPT intensity appears to significantly reduce major bleeding, without significant effect on ischemic events. Timing of de-escalation strategy may not be fixed because this strategy has been tested at different time points: (1) 2–3 days post-PCI (e.g., guided de-escalation); (2) after 1–3 months of DAPT, followed by P2Y12 inhibitor monotherapy (e.g., clopidogrel or ticagrelor); and (3) after 3–6 months of DAPT, followed by aspirin monotherapy. Since the clinical benefit of de-escalation strategy may be influenced by a number of factors (e.g., ethnicity, gender, and disease entity and phase), this concept in the current era can be applicable mostly for selected clinical scenarios, such as high-bleeding risk (HBR) (3).
Recent meta-analyses have compared the net benefits of various de-escalation strategies in ACS patients (4, 5). Compared with the conventional DAPT strategy, most of the current de-escalation strategies have shown the reduction of clinical events, except of increased risk in ischemic event during short-term DAPT, followed by aspirin monotherapy. Intensity de-escalation of P2Y12 inhibitor showed the best benefit in reducing the net clinical event, while short-term DAPT followed by antiplatelet monotherapy was most beneficial in decreasing major bleeding. Meanwhile, a recent individual patient meta-analysis demonstrated that the de-escalation strategy significantly reduced the risks of ischemic (hazard ratio [HR], 0.761; 95% confidence interval [CI], 0.597–0.972; log rank P = 0.029) and bleeding (HR, 0.701; 95% CI, 0.606–0.811; log rank P < 0.001) endpoints together (5). Compared to the guided de-escalation, the unguided de-escalation had a significantly larger impact on reducing bleeding endpoint (P for interaction = 0.007).
De-escalation strategy of antiplatelet therapy in East Asian patients
East Asian patients have been shown to be more vulnerable to bleeding and less thrombogenic to ischemic event compared with Caucasian patients, a condition known as the “East Asian paradox” (6, 7). In addition, responsiveness to potent P2Y12 inhibitor appears greater in East Asians than Westerners. Therefore, clinical benefit of de-escalation strategy in ACS patients may be pronounced in these patients. A recent meta-analysis indicated the unique risk–benefit trade-off of de-escalation strategy in East Asian vs. Caucasian patients (8). In East Asian patients, reduction of DAPT intensity or duration could minimize bleeding without safety concerns. In Caucasian patients, reduction of DAPT intensity may incur an ischemic penalty, while DAPT abbreviation has no overall benefit.
Min-Gyu Kang et al. demonstrated potent antiplatelet effect of standard-dose ticagrelor (i.e., 90-mg twice daily), and its associations with short-term adverse events and DAPT discontinuation. First, reversibly-binding ticagrelor showed the different cutoff for 1-month bleeding episodes compared with irreversibly-binding clopidogrel [≤20 vs. ≤110 P2Y12 reaction unit (PRU) measured by VerifyNow assay]. Second, patients on ticagrelor showed the higher risks of 1-month bleeding compared with those on clopidogrel [any bleeding: 45.6% vs. 23.6%; odds ratio (OR), 2.71]. Third, early occurrence of bleeding episode was significantly associated with low level of PRU (OR, 2.68). Fourth, type of P2Y12 inhibitor (ticagrelor vs. clopidogrel: OR, 2.19) and bleeding episode (OR, 2.94) were independent predictors for dyspnea occurrence. During standard-dose ticagrelor in East Asian patients, prevalence of low platelet reactivity was very popular (PRU ≤ 20: 68.1%) compared with that (PRU ≤ 110: 16.5%) during 75-mg clopidogrel, which may suggest the unmet need to develop up-front de-escalation strategy with reduced-dose ticagrelor in these patients.
Personalized allocation of aspirin for secondary prevention of coronary artery disease
Recent clinical trials have focused early discontinuation of aspirin following PCI. However, aspirin resistance determined by platelet function test may be associated with an increased risk of thrombotic event, prominent during the early phase post-PCI. In a large-scale PCI cohort (n = 7,090), aspirin resistance (the highest quintile measured by Multiplate assay) showed a significantly higher risk of death or stent thrombosis at 1 year (OR, 1.78; 95% CI, 1.39–2.27; P < 0.0001) (9). Therefore, adequate suppression of thromboxane synthesis is required to prevent occurrence of thrombotic events in high-risk patients with ACS. The responsiveness to aspirin in such patients could be improved by twice-daily aspirin administration. Nischal N Hegde et al. suggested the laboratory criteria to identify subjects who would benefit from a twice-daily aspirin dose. Twice-daily aspirin was effective if serum thromboxane-B2 levels at 4 h are <3,100 and >3,100 pg/ml at 24 h. If thromboxane-B2 at 4 h and 24-hours is >3,100 pg/ml, a twice-daily aspirin did not suggest enough antiplatelet effect and switching with potent P2Y12 inhibitors may be another option overcoming this huddle. Because low-dose aspirin could not achieve adequate inhibition of thromboxane-B2 following PCI in high-risk patients, alternative strategy against this issue would be required in these subjects.
Collagen-induced platelet activation as a potential target of colchicine
Colchicine with anti-inflammatory effect demonstrates the clinical benefit against ischemic events in patients with stable angina or ACS (10, 11). Gabrielle J. Pennings et al. focused on antiplatelet effect of colchicine, primarily targeting on collagen-induced platelet activation via glycoprotein (GP)VI. Concentration of therapeutic-dose colchicine led to a significant decrease in collagen-induced platelet aggregation and altered GPVI level. Switching from aspirin to colchicine could be another plausible de-escalation strategy in ACS patients with enhanced inflammation, which effect should be tested in the future trials.
Summary
The present Research Topic indicates an overview of the need and possibilities of individualizing antiplatelet therapy based on the current knowledge and available evidence (Table 1). Although de-escalation antiplatelet strategy represents a very promising concept, its globalization still has a number of limitations in ACS patients with high-ischemic profiles. Application of de-escalation DAPT strategy (e.g., reduced-dose prasugrel or ticagrelor) may be a default strategy option in East Asian patients with HBR phenotype. Furthermore, early discontinuation of aspirin may not be applicable for all-comers following PCI and its switching with colchicine is a potential treatment that could be available in the future.
Author contributions
SYL has drafted the manuscript. All the authors have read and approved the final version of the manuscript. All authors contributed to the article and approved the submitted version.
Conflict of interest
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
Publisher's note
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
References
1. Collet JP, Thiele H, Barbato E, Barthélémy O, Bauersachs J, Bhatt DL, et al. 2020 ESC guidelines for the management of acute coronary syndromes in patients presenting without persistent ST-segment elevation. Eur Heart J. (2021) 42(14):1289–367. doi: 10.1093/eurheartj/ehaa575
2. Lawton JS, Tamis-Holland JE, Bangalore S, Bates ER, Beckie TM, Bischoff JM, et al. 2021 ACC/AHA/SCAI guideline for coronary artery revascularization: executive summary: a report of the American college of cardiology/American heart association joint committee on clinical practice guidelines. Circulation. (2022) 145(3):e4–e17. doi: 10.1161/CIR.0000000000001039
3. Urban P, Mehran R, Colleran R, Angiolillo DJ, Byrne RA, Capodanno D, et al. Defining high bleeding risk in patients undergoing percutaneous coronary intervention: a consensus document from the academic research consortium for high bleeding risk. Eur Heart J. (2019) 40:2632–53. doi: 10.1093/eurheartj/ehz372
4. Laudani C, Greco A, Occhipinti G, Ingala S, Calderone D, Scalia L, et al. Short duration of DAPT versus De-escalation after percutaneous coronary intervention for acute coronary syndromes. JACC Cardiovasc Interv. (2022) 15(3):268–77. doi: 10.1016/j.jcin.2021.11.028
5. Kang J, Rizas KD, Park KW, Chung J, van den Broek W, Claassens DMF, et al. Dual antiplatelet therapy de-escalation in acute coronary syndrome: an individual patient meta-analysis. Eur Heart J. (2023) 44(15):1360–70. doi: 10.1093/eurheartj/ehac829
6. Jeong YH. “East Asian paradox”: challenge for the current antiplatelet strategy of “one-guideline-fits-all races” in acute coronary syndrome. Curr Cardiol Rep. (2014) 16(5):485. doi: 10.1007/s11886-014-0485-4
7. Kim HK, Tantry US, Smith SC, Jeong MH, Park SJ, Kim MH, et al. The East Asian paradox: an updated position statement on the challenges to the current antithrombotic strategy in patients with cardiovascular disease. Thromb Haemost. (2021) 121:422–32. doi: doi: 10.1055/s-0040-1718729
8. Gorog DA, Jeyalan V, Markides RIL, Navarese EP, Jeong YH, Farag M. Comparison of De-escalation of DAPT intensity or duration in East Asian and Western patients with ACS undergoing PCI: a systematic review and meta-analysis. Thromb Haemost. (2023). doi: 10.1055/s-0043-57030. [Epub ahead of print]37072035
9. Mayer K, Bernlochner I, Braun S, Schulz S, Orban M, Morath T, et al. Aspirin treatment and outcomes after percutaneous coronary intervention: results of the ISAR-ASPI registry. J Am Coll Cardiol. (2014) 64(9):863–71. doi: 10.1016/j.jacc.2014.05.049
10. Tardif JC, Kouz S, Waters DD, Bertrand OF, Diaz R, Maggioni AP, et al. Efficacy and safety of low-dose colchicine after myocardial infarction. N Engl J Med. (2019) 381(26):2497–505. doi: 10.1056/NEJMoa1912388
Keywords: individualization, antiplatelet therapy, coronary artery disease, colchicine, de-escalation, ethnicity
Citation: Lee SY, Geisler T, Motovska Z and Jeong Y-H (2023) Editorial: The individualization of antiplatelet therapy in coronary artery disease: escalation or de-escalations. Front. Cardiovasc. Med. 10:1219689. doi: 10.3389/fcvm.2023.1219689
Received: 9 May 2023; Accepted: 19 May 2023;
Published: 6 June 2023.
Edited and Reviewed by: Hugo Ten Cate, Maastricht University Medical Centre, Netherlands
© 2023 Lee, Geisler, Motovska and Jeong. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Young-Hoon Jeong Z29vZG9jdG9yQG5hdmVyLmNvbQ== eW91bmdnb29kb2N0b3JAZ21haWwuY29t
 Sang Yeub Lee
Sang Yeub Lee Tobias Geisler
Tobias Geisler Zuzana Motovska
Zuzana Motovska Young-Hoon Jeong
Young-Hoon Jeong