- 1University of North Carolina at Greensboro, Greensboro, NC, United States
- 2High Point University, High Point, NC, United States
- 3Dansville Dental Professionals, Dansville, NY, United States
Background: Retrograde peri-implantitis is an infection at the apex of an implant, leading to progressive bone loss. We present a surgical technique that is an alternative to implant removal or “implantoplasty.”
Case: A 47-year-old patient developed retrograde peri-implantitis 18 months after implant placement. As the infection was localized to the apex of the implant, an apicoectomy was performed on the implant. Post-operative serial periapical radiographs showed reparative tissue within 4 months, and a follow-up radiograph showed complete bone restoration 2 years later.
Practical Implications: The findings of this case suggest a viable alternative to condemnation and removal of an implant with a periapical infection. It may be viable to resect the contaminated portion of the implant, graft the defect, and gain long-term retention and service of the implant.
Introduction
The replacement of missing teeth with dental implants is a cost-effective and common procedure. As with any surgical procedure, implants are subject to complications, such as peri-implant disease. Peri-implant disease can be broken down into two categories: peri-implant mucositis, and peri-implantitis. Peri-implantitis is soft tissue inflammation around the implant, with progressive loss of supporting bone (1). Peri-implantitis can be further divided into marginal and retrograde peri-implantitis, which are distinguished by marginal and periapical bone loss, respectively (2).
Retrograde peri-implantitis has been reported to be less common than marginal peri-implantitis (2). The two most common treatment options for retrograde peri-implantitis are removal of the implant or surgical regenerative treatment, which consists of implant surface debridement and placement of bone graft material (3). However, implant surface debridement, or “implantoplasty,” has been documented in the literature to have several drawbacks, including the difficulty of complete access and the concern over titanium particles being left in the lesion (4). However, cases of alternative surgical treatment beyond removal or implantoplasty are rare (5). The priority of surgical treatment is to fully remove the source of the infection and create an environment conducive to tissue regeneration (3, 4). Here we describe the surgical treatment of symptomatic retrograde peri-implantitis through a direct apicoectomy of the implant.
Treatment
A 47-year-old patient with a history of smoking and periodontal disease sought implant treatment. The maxillary central incisors had been removed 1 year prior due to resorption of the roots. Treatment with partial dentures had not been satisfactory to the patient and implants were proposed as an option. The patient-specific risks and benefits of implants were discussed, and the patient signed an informed consent.
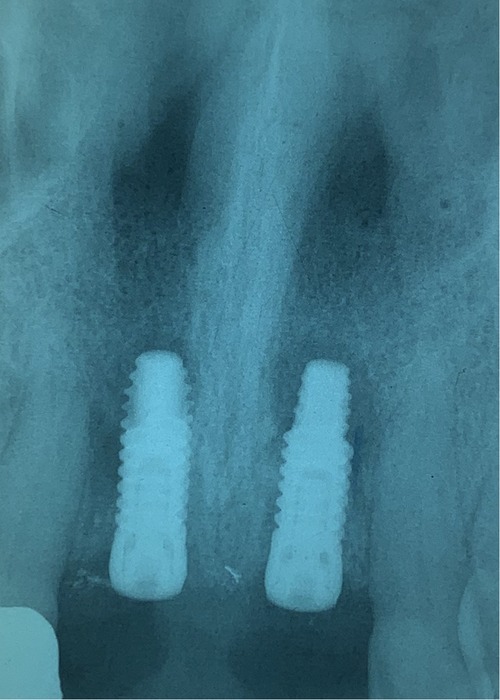
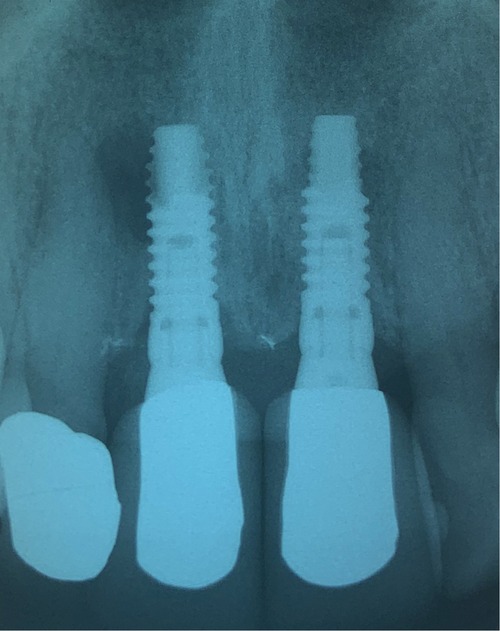
We implanted two 3.5 × 12 mm titanium implants into the maxillary central incisor sites 8 and 9 using a two-stage technique, with final restorations placed after 5 months (Figure 1). The placement of the implants was successful, and serial periapical radiographs showed healthy osseointegration through 10 months post implantation. After 18 months, the patient reported that the gingiva around the #8 implant had developed pain. Initial antibiotic treatment of penicillin VK 500 mg three times daily was prescribed, which provided some relief, and when the patient was available for an appointment, we performed a physical exam as well as a periapical radiograph. The radiograph (Figure 2) showed a radiolucency located around the apex of the implant. A physical examination of the patient found that the implant was stable but the area above the implant was tender to palpation. The discernible bone loss and pain led to the diagnosis of retrograde peri-implantitis.
After obtaining patient consent for the treatment plan, we proceeded with a full-thickness flap at the muco-gingival junction. We found that the periapical lesion had perforated the facial and lingual plates of the maxilla. The defect was unroofed, and the socket was flushed with saline and chlorhexidine, exposing the contaminated portion of the implant. The infected apex was removed using high-speed carbide burs and continuous lavage with chilled saline. The removed portion was determined to be 5 mm in length, leaving 7 mm remaining implanted, which was determined to be a sufficient length for the implant to remain functional. Upon removal of the apex of the implant, the entire socket could be clearly visualized. The field was curetted and debrided and then was flushed again with chlorhexidine and saline to ensure the removal of any titanium particles.
Once the field was observed to be clear, the lingual wall of the defect was covered with a resorbable membrane, and the osseous defect was grafted using crushed cancellous and cortical bone mixed with 0.1cc of Cleocin. The facial wall was covered with a resorbable membrane, and the primary closure was performed using 5-0 PGA sutures. The prescribed post-operative care consisted of oral antibiotics and rinsing with saline.
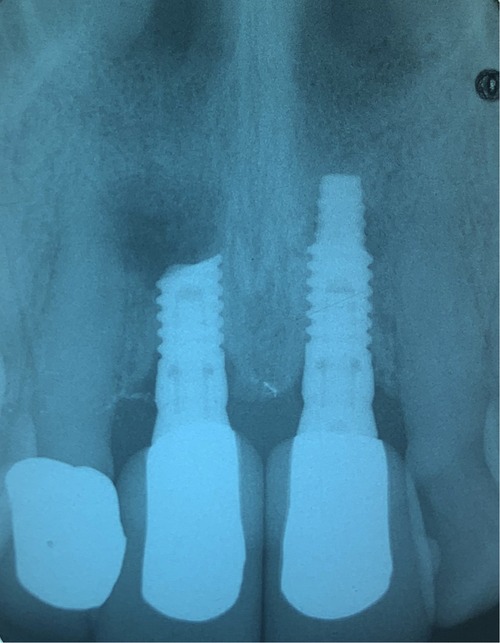
At the post-operative appointment, the patient reported that their pain had greatly improved with the removal of the infected apex of the implant, and the implant remained functional and firm. Serial periapical radiographs at 1, 2, and 4 months (Figure 3) showed initial reparative tissue above the implant, during which time the patient remained asymptomatic. A radiograph after 2 years shows complete bone remodeling (Figure 4). The patient was followed for 6 years with successful function and retention of the implant.
Discussion
We have described a case of retrograde peri-implantitis around the apex of a titanium implant. An apicoectomy was performed on the implant. The patient's condition was monitored, and bone remodeling was observed in periapical radiographs in less than 4 months, with successful implant maintenance for more than 6 years.
While disease in implants has been reported to be as high as 25% overall, retrograde peri-implantitis has a reported prevalence of 0.26% and can arise as late as 4 years after implant placement (6, 7). However, this percentage can be increased by as much as 15x in smokers with a history of periodontal disease (8). Once a diagnosis of retrograde peri-implantitis has been made due to the observation of periapical bone loss, treatment through either surgical intervention or implant removal is almost always required (2). A common surgical intervention of direct debridement and implant decontamination has been found to be successful in roughly half of cases in a clinically controlled study, yet it has been suggested that the removal of implant surface texture may prevent reosseointegration (3, 9).
In our case, the patient was a smoker with periodontal disease, which greatly increased the overall chance of implant failure. Retrograde peri-implantitis has been found to be caused by bacteria left behind during the initial implant surgery, or spontaneously in patients with a history of periodontal disease (7, 10). In our case, the second cause of retrograde peri-implantitis is more likely. Our patient had previously had resorption of the root of the tooth which the implant replaced, which implies a compromised local environment that was more likely to develop inflammation (1, 6).
By performing an apicoectomy, we were able to more fully ensure bacterial pocket elimination directly than could be obtained without the removal of the apex. The apicoectomy allows for complete access to the field, which permits careful removal of all infectious material. The use of curettage and chlorhexidine during the surgery helped to ensure the removal of all bacterial biofilm, although there is a lack of literature on a preferred method of chemical implant decontamination (8). The clear field also helps to ensure no titanium particles are left behind, which is a significant concern in treatment via surface debridement (4, 11). Additionally, the use of human allograft material was successful, but no conclusive study has shown the superiority of one bone substitute over others for retrograde peri-implantitis (3, 4).
An apicoectomy was chosen over implant removal or surface debridement due to the location and size of the abscess, as well as the length of the implant. Implant removal and surface debridement are two of the most common treatments for RPI, as well as the use of xenograft to enable bone growth (10). The location of our patient's implant made it difficult to fully access the entire infected site without the removal of the apex. In our case, the patient was left with approximately 7 mm of implant after the apicoectomy, which has been shown to be an adequate length for successful implant maintenance (12). Additionally, implant removal was disfavored as an option by the patient for aesthetic reasons. Subsequent removal of the implant was not ruled out as a potential future treatment, if post-operative periapical radiographs showed continued progression of bone loss, or if bone remodeling was not observed. However, with our approach, the patient retained the aesthetic and functional success of the implant while the lesion healed.
While an apicoectomy of the implant was successful in this case, other treatments for retrograde peri-implantitis should be considered by the professional during planning, as our approach does have some limitations. Primarily, the cutting of the apex of the implant must be accompanied by sufficient irrigation to prevent overheating of the adjacent bone. If the healthy bone reaches a sustained temperature of 47C for more than 1 min, it can become necrotic (13). Our approach is also limited by the length of the healthy implant. As much length should be maintained as possible, in order to increase the success of the implant. Our approach also requires a substantial amount of healthy bone in order to facilitate remodeling and continued implant stability.
Conclusions
We have described the successful treatment of retrograde peri-implantitis through an apicoectomy of an implant. The findings from this case suggest that immediate removal of implants with periapical lesions is not always necessary and offers an alternative approach to implant surface debridement or implantoplasty. With careful consideration, an apicoectomy can provide an alternative, conservative treatment for retrograde peri-implantitis by dentists.
Data availability statement
The original contributions presented in the study are included in the article/Supplementary Material, further inquiries can be directed to the corresponding author/s.
Author contributions
MJH, DDH, and KLH contributed equally to this manuscript and accept responsibility for the content within. KLH was responsible for patient treatment and management and development of the original case.
Conflict of interest
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
Publisher's note
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
References
1. Sarmast ND, Wang HH, Sajadi AS, Angelov N, Dorn SO. Classification and clinical management of retrograde peri-implantitis associated with apical periodontitis: a proposed classification system and case report. J Endod. (2017) 43(11):1921–24. doi: 10.1016/j.joen.2017.06.034
2. Ramanauskaite A, Juodzbalys G, Tozum TF. Apical/retrograde periimplantitis/implant periapical lesion: etiology, risk factors, and treatment options: a systematic review. Implant Dent. (2016) 25(5):684–97. doi: 10.1097/ID.0000000000000424
3. Aljohani M, Yong SL, Bin Rahmah A. The effect of surgical regenerative treatment for peri-implantitis: a systematic review. Saudi Dent J. (2020) 32(3):109–19. doi: 10.1016/j.sdentj.2019.10.006
4. Khoury F, Keeve PL, Ramanauskaite A, Schwarz F, Koo KT, Sculean A, et al. Surgical treatment of peri-implantitis - consensus report of working group 4. Int Dent J. (2019) 69(Suppl 2):18–22. doi: 10.1111/idj.12505
5. Bianchini MA, Galarraga-Vinueza ME, Apaza-Bedoya K, De Souza JM, Magini R, Schwarz F. Two to six-year disease resolution and marginal bone stability rates of a modified resective-implantoplasty therapy in 32 peri-implantitis cases. Clin Implant Dent Relat Res. (2019) 21(4):758–65. https://doi.org/10.1111/cid.1277330985073
6. Sarmast ND, Wang HH, Soldatos NK, Angelov N, Dorn S, Yukna R, et al. A novel treatment decision tree and literature review of retrograde peri-implantitis. J Periodontol. (2016) 87(12):1458–67. doi: 10.1902/jop.2016.160219
7. Brisman DL, Brisman AS, Moses MS. Implant failures associated with asymptomatic endodontically treated teeth. J Am Dent Assoc. (2001) 132(2):191–5. doi: 10.14219/jada.archive.2001.0154
8. Al-Sabbagh M, Shaddox LM. Is peri-implantitis curable? Dent Clin North Am. (2019) 63(3):547–66. doi: 10.1016/j.cden.2019.02.003
9. Mercado F, Hamlet S, Ivanovski S. Regenerative surgical therapy for peri-implantitis using deproteinized bovine bone mineral with 10% collagen, enamel matrix derivative and Doxycycline-A prospective 3-year cohort study. Clin Oral Implants Res. (2018) 29(6):583–91. doi: 10.1111/clr.13256
10. Bianchini MA, Galarraga-Vinueza ME, Bedoya KA, Correa B, de Souza Magini R, Schwarz F, et al. Implantoplasty enhancing peri-implant bone stability over a 3-year follow-up: a case series. Int J Periodontics Restorative Dent. (2020) 40(1):e1–8. doi: 10.11607/prd.3849
11. Valente NA, Andreana S. Treatment of peri-implantitis using a combined decontaminative and regenerative protocol: case report. Compend Contin Educ Dent. (2018) 39(2):96–101. PMID: 29388783
12. Manfro R, Garcia GF, Bortoluzzi MC, Fabris V, Bacchi A, Elias CN. Apicoectomy and scanning electron microscopy analysis of an implant infected by apical (retrograde) peri-implantitis: a case letter. J Oral Implantol. (2018) 44(4):287–91. doi: 10.1563/aaid-joi-D-16-00162
Keywords: retrograde peri-implantitis, peri-Implantitis, implantoplasty, apicoectomy, surgical treatment
Citation: Hoffman MJ, Hale DD and Hale KL (2022) Case Report: One alternative surgical treatment for retrograde peri-implantitis. Front. Dent. Med 3:923041. doi: 10.3389/fdmed.2022.923041
Received: 18 April 2022; Accepted: 23 August 2022;
Published: 13 September 2022.
Edited by:
Monica Prasad Gibson, University of Alberta, CanadaReviewed by:
Saverio Capodiferro, University of Bari Aldo Moro, ItalyGerardo Pellegrino, University of Bologna, Italy
© 2022 Hoffman, Hale and Hale. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Matthew J Hoffman, bV9ob2ZmbTJAdW5jZy5lZHU=
Specialty Section: This article was submitted to Reconstructive Dentistry, a section of the journal Frontiers in Dental Medicine
 Matthew J Hoffman
Matthew J Hoffman Demetria D Hale2
Demetria D Hale2 Kenneth L Hale
Kenneth L Hale