- 1Center for Community-Based Healthcare Research and Education (CoHRE), Head Office for Research and Academic Information, Shimane University, Shimane, Japan
- 2Department of Sports Sociology and Health Sciences, Faculty of Sociology, Kyoto Sangyo University, Kyoto, Japan
- 3Department of Pharmacology, Faculty of Medicine, Shimane University, Shimane, Japan
- 4Center for Primary Health Care Research, Lund University, Malmö, Sweden
- 5Tominaga Dental Office, Shimane, Japan
- 6Department of Laboratory Medicine, Faculty of Medicine, Shimane University, Shimane, Japan
- 7Faculty of Human Sciences, Shimane University, Shimane, Japan
Objective: An elevated sodium-to-potassium (Na/K) ratio in urine increases the risk of hypertension. Tooth loss in older adults can lead to a diminished nutritional state, including alterations in the Na/K ratio. However, the relationship between denture use and changes in the Na/K ratio among individuals with tooth loss has not been sufficiently explored. This study examined whether denture use modifies the association between tooth loss and changes in the Na/K ratio.
Methods: Surveys in 2016 and 2018 included 473 older adults. The Na/K ratio was measured using spot urine tests. A dental hygienist evaluated the number of teeth and the use of dentures. We used generalized linear models to analyze the combined effect of the number of teeth and denture use on changes in the Na/K ratio.
Results: Participants without dentures in the 0–19 teeth group showed a significant association with changes in the Na/K ratio (B = 0.635; 95% confidence interval = 0.038, 1.232) compared to those with ≥28 teeth, but denture users with 0–19 teeth did not show significant association. No significant association with changes in the Na/K ratio was observed in denture users and non-users with 20–27 teeth.
Conclusion: In non-denture users with fewer than 20 teeth, the Na/K ratio was markedly elevated, but in denture users with fewer than 20 teeth it was not significant. These findings highlight the importance of promoting denture use in older adults with few remaining teeth to maintain their Na/K balance.
1 Introduction
According to Health Japan 21 (the second term) (1), the salt intake of the Japanese population is decreasing, but has not yet reached the target level. Additionally, vegetable intake has fallen short of the set goal, and improving the nutritional status of residents remains a public health priority in Japan. The 2017 American College of Cardiology/American Heart Association hypertension guidelines recommend increasing potassium and reducing sodium intake (2). The Japanese Society of Hypertension recently issued a consensus statement on the practical use and target value of the urine sodium-to-potassium (Na/K) ratio in assessing hypertension risk for Japanese individuals (3). Despite challenges in measurement accuracy (3–5), the measurement of the urine Na/K ratio, based on a combination of sodium and potassium levels in spot urine, is considered less invasive, resulting in minimal burden on participants. Additionally, spot urine test is a simpler test compared to the 24-h urine collection method (6). Consequently, the urine Na/K ratio is anticipated to be utilized as a novel indicator related to health (3, 7). In previous research, the Na/K ratio was found to be associated with blood pressure levels (8, 9), cardiovascular disease mortality, and all-cause mortality (10, 11). Therefore, reducing the dietary Na/K ratio is important to promote population health.
Oral conditions can impair dietary nutrient intake (12, 13). However, there is limited research examining the correlation between oral conditions and sodium and potassium levels. Marito et al. reported a negative association between the number of remaining teeth and masticatory performance and Na/K ratio (14). Nomura et al. reported no association between denture use and sodium or potassium (15). Both were cross-sectional studies; to the best of our knowledge, no longitudinal associations have been examined. Meanwhile, previous studies have shown that non-replaced missing teeth are associated with hypertension (16, 17). The association between poor oral conditions, such as the non-replaced missing teeth, and hypertension may potentially involve the Na/K ratio (14). In other words, the restoration of tooth loss with dentures could contribute to the enhancement of masticatory function and subsequent improvement in nutritional intake, potentially promoting an overall improvement in health status, including cognitive function (12, 18). Thus, we posited a hypothesis that the utilization of dentures would ameliorate the equilibrium between sodium and potassium concentrations in older adults who have experienced remarkable tooth loss. In this study, we examined whether denture use modified the association between tooth loss and changes in Na/K ratios in older Japanese adults.
2 Materials and methods
2.1 Study design and participants
This study was part of the Shimane Community-Based Healthcare Research and Education study. The Shimane Community-Based Healthcare Research and Education study is conducted to elucidate various factors contributing to lifestyle diseases in older adults (17, 19–21). This study employed data amassed during health checkups conducted in June 2016 and June 2018 in Okinoshima Town, Shimane, Japan. An aggregate of 842 older adults partook in the health examination in 2016 (baseline), and 502 participants were reevaluated in 2018 (follow-up). Upon the exclusion of nine participants due to incomplete information for study variables (Na/K ratio evaluated utilizing spot urine tests, n = 7; oral health status, n = 2), data from 473 participants were incorporated into the analysis. The study protocol received approval from the Medical Research Ethics Committee of Shimane University, Faculty of Medicine (approval number: 20051214-3), and adhered to the Code of Ethics of the World Medical Association (1964 Declaration of Helsinki and its subsequent amendments). Prior to enrollment in the study, written informed consent was procured from all participants.
2.2 Measurements
Sodium and potassium levels were assessed using spot urine tests. Spot urine was collected at the site of the health checkups (7, 19, 20). This test may have a lower precision compared to the 24 h urine collection method (3, 6); spot urine tests are practical in a large older population. Quantification of sodium and potassium concentrations was executed utilizing a BioMajesty 6070 G analyzer (JEOL Ltd., Tokyo, Japan). The Na/K ratio was computed by dividing the quantity of excreted sodium by the quantity of excreted potassium. Alterations in the Na/K ratio were determined by deducting the baseline data from the follow-up data (19).
This study used the number of teeth and denture use as indicators of oral health status. Intraoral examinations were performed by a trained dental hygienist, with the examiner and participants seated. The number of remaining teeth (functional teeth) was counted via oral visual examination. According to previous studies [9, 10], we divided the participants into three groups: individuals with ≥28, 20–27, and 0–19 teeth. Denture use (no or yes) was recorded by a dental hygienist.
In addition, a questionnaire was used to collect data on sex (male or female), age (years), smoking habits (no or yes), and alcohol consumption (no, sometimes, or daily; assessed from the question “How often do you drink?”) Body mass index was calculated from the recorded height and weight (kg/m2) and divided into three categories using Asian cut-off points (underweight: <18.5 kg/m2; normal: 18.5–22.9 kg/m2; overweight: ≥23.0 kg/m2) (22).
2.3 Statistical analysis
Regarding participant characteristics, frequency data are reported as numbers and percentages, and continuous data are presented as means and standard deviations. Generalized linear models (GLM) were used to estimate unstandardized regression coefficients (B) and 95% confidence intervals (CI) for changes in the Na/K ratio in relation to the combined variable of the number of teeth and denture use. To test the use of dentures as a potential effect modifier of the number of teeth and Na/K ratio, the number of teeth was entered together with denture use as a combined variable. The study participants were systematically classified into the following five groups, as reported by a previous study (17): (1) those possessing 28 or more teeth (serving as the reference group), (2) individuals with a tooth count ranging from 20–27 who utilize dentures, (3) participants with 20–27 teeth who do not use dentures, (4) participants with a tooth count between 0 and 19 who make use of dentures, and (5) those with 0–19 teeth who do not use dentures. We observed a moderate correlation between the number of teeth and denture use (r = 0.67; P < .001); therefore, considering multicollinearity, the number of teeth and denture use were included separately in the GLM. All analyses were adjusted for sex, age, body mass index, smoking habits, and alcohol consumption. All statistical analyses were performed using SPSS Statistics for Windows (version 29.0; IBM Corp., Armonk, NY). Statistical significance was set at P < .05.
3 Results
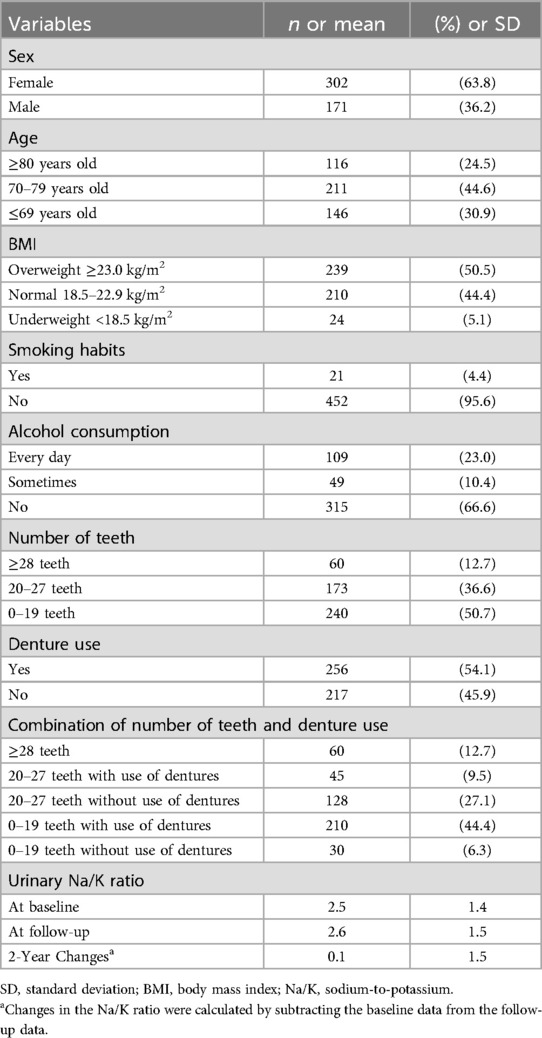
Table 1 presents participant characteristics. The number of participants with 0–19 teeth, 20–27 teeth, and 28 or more teeth (%) was 240 (50.7), 173 (36.6), and 60 (12.7), respectively. The mean (standard deviation) Na/K ratios at baseline, follow-up, and 2-year changes were 2.5 (1.4), 2.6 (1.5), and 0.1 (1.5), respectively.
Table 2 and Figure 1 show the association between the combined variable of number of teeth and denture use and changes in the Na/K ratio. When using ≥28 teeth as the reference group, a significant increase in the Na/K ratio was observed in participants without dentures with 0–19 teeth (B = 0.635; 95% CI = 0.038, 1.232; P = .037), but denture users with 0–19 teeth did not show significant association with changes in the Na/K ratio (B = 0.431; 95% CI = −0.034, 0.896; P = .069). No significant association with changes in the Na/K ratio was observed in denture users (B = 0.192; 95% CI = −0.344, 0.728; P = .483) or non-users (B = 0.145; 95% CI = −0.300, 0.589; P = .523) with 20–27 teeth.
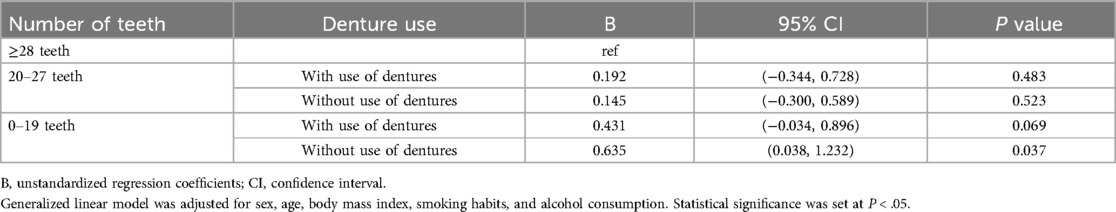
Table 2. Association between combined variable of number of teeth and use of dentures and changes in sodium-to-potassium ratio among older adults.
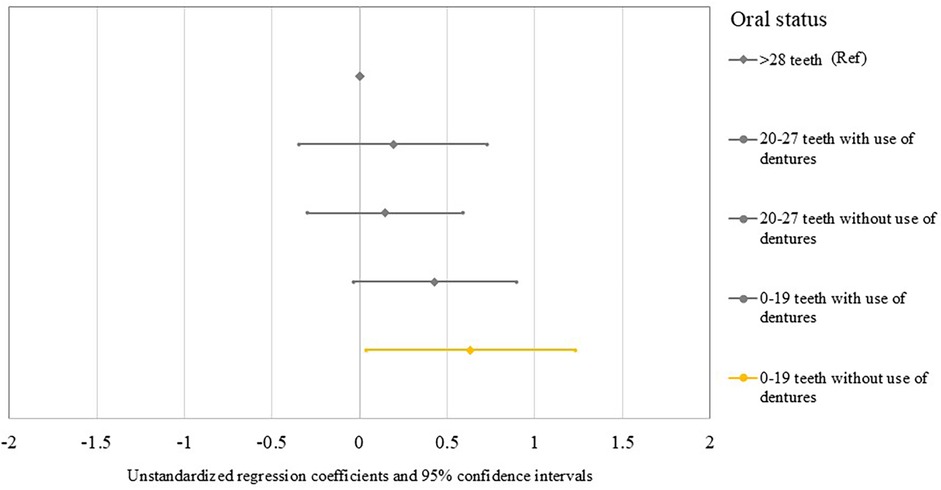
Figure 1. Forest plots show the unstandardized regression coefficients and 95% confidence intervals for changes in the Na/K ratio in relation to the combined variable of the number of teeth and use of dentures.
4 Discussion
This study examined whether the possible modification of the association between tooth loss and changes in the Na/K ratio in older adults was due to the use of dentures. When there are few remaining teeth (0–19 teeth), the Na/K ratio may increase when dentures are not used. However, in denture users with fewer than 20 teeth, this increase was not significant. These results suggest that conducting educational training for oral health may impact the nutritional status through regular denture maintenance (23). In addition, dentures can help restore esthetics, enhancing social interactions in older adults (24). However, there may be instances where the use of dentures is avoided owing to poor quality and discomfort, such as pain (25). In particular, occluding pairs may contribute to masticatory function more than the number of remaining teeth (26). Therefore, from the perspectives of sociability and functionality, it is necessary to regularly review the condition of the dentures.
A previous study by Marito et al. reported negative associations between oral health and the Na/K ratio in 894 older Japanese adults (14). In their study, calibrated dental examiners assessed the number of remaining teeth in each participant, and Na/K ratios were estimated using a brief self-administered diet history questionnaire. Their bivariate correlation analysis resulted in a correlation coefficient of −0.07 (P = .03). Although our study employed different measurement and analysis methods, it supports the concept that tooth scarcity increases the Na/K ratio. Nomura et al. conducted a study involving 701 older Japanese individuals examining denture usage through questionnaires and sodium or potassium intake using the brief self-administered diet history questionnaire (15). The results showed no difference in sodium or potassium intake based on denture use. Therefore, although previous studies have not created combined variables for tooth loss and denture use—making comparisons difficult—our findings provide a new perspective on the relationship between nutritional status, the number of teeth, and the use of dentures.
Potential mechanisms that could elucidate the association between tooth loss and alterations in the Na/K ratio have been put forth. The masticatory function in older adults possessing fewer than 20 residual teeth is reportedly inferior compared to their counterparts with a greater number of teeth. However, the utilization of denture prostheses could potentially aid in the restoration of masticatory function (27). The utilization of dentures may be linked to variations in the nutritional status of older adults experiencing extensive tooth loss (28). Those with significant tooth loss in later life commonly encounter challenges in consuming raw fruits and vegetables, given the increased masticatory effort required compared to other food types (29, 30). This may limit their overall food choices, eventually leading to health problems such as hypertension through nutritional imbalances (28, 29). Lee et al. reported that poor nutritional condition, attributed to challenges in food selection and consumption, has been identified as a mediating factor in the relationship between unsatisfactory masticatory function and an elevated risk of mortality (31). Furthermore, mastication with dentures may help maintain hippocampal activity, potentially playing a role in preserving cognitive abilities and memory (32). Additionally, the presence and functioning of periodontal mechanoreceptors in the teeth during mastication are crucial (33). The removal of these receptors during tooth extraction leads to a decline in masticatory ability. Maintaining periodontal mechanoreceptor activity, which depends on the type of implants or dentures used in treatment, is also an important aspect for ensuring proper nutritional intake. Therefore, considering both oral conditions and dietary Na/K ratios is important to promote population health, especially among older adults.
4.1 Limitations
First, we could not establish a strong causal relationship because this study employed a retrospective design. Second, this study was exclusively composed of inhabitants from specific areas who engaged in health checkups. Furthermore, Okinoshima, the town under study, is an island with a higher likelihood of food choices being limited. This may be particularly significant in cases where oral function is diminished. Although the findings of this study may be challenging to generalize because of a potential sampling bias, these results may represent a significant step toward understanding potential issues related to regional disparities and limited food environments. Third, the results drawn in our study are reported on a limited sample size; therefore, the statistical power was low. Fourth, the spot urine test used to measure sodium and potassium levels in the present study may have a lower precision compared to the 24 h urine collection method (6). However, when applying the 24 h urine collection method to older adults, there is a potential for collection errors. Spot urine testing offers the advantage of reducing the burden on older adults. Moreover, in order to investigate the dietary content of the participants, it is necessary to utilize Dietary Records (34), 24 h Dietary Recalls (35), and the Food Frequency Questionnaire (36) as dietary surveys other than urine tests. By doing so, there is a possibility that future research can clarify the association between tooth loss and changes in nutrition based on specific dietary content. Fifth, we did not investigate whether the dentures were partial or complete. Therefore, it cannot be ruled out that this difference may have influenced the results (33). Finally, the unmeasured variables were not included as confounders. For example, a study in the United States has reported a correlation between potassium levels and diet costs (37). This suggests that the economic status of older adults may influence food choices. Therefore, future studies should examine the influence of additional variables [e.g., educational level (38) and social isolation (39)]. Based on the above considerations, future research should include large-scale observational studies as well as randomized controlled trials to investigate whether the use of dentures (treatment) can improve dietary habits (40), such as increasing vegetable intake, and thereby maintaining a favorable Na/K ratio.
4.2 Conclusion
This study showed that the non-use of dentures appeared to worsen the adverse effects of tooth loss on the Na/K ratio, whereas the Na/K ratio did not increase in denture users with tooth loss. These findings highlight the importance of promoting denture use in older adults with few remaining teeth to maintain their Na/K balance. Future research is needed to investigate whether the use of dentures, that is, oral care, can improve dietary habits and maintain a favorable Na/K ratio.
Data availability statement
The datasets presented in this article are not readily available because The consent of the participants did not include a provision for the data to be shared publicly. Requests to access the datasets should be directed to Medical Research Ethics Committee, Shimane University Faculty of Medicine (kenkyu@med.shimane-u.ac.jp).
Ethics statement
The studies involving humans were approved by Medical Research Ethics Committee, Shimane University Faculty of Medicine. The studies were conducted in accordance with the local legislation and institutional requirements. The participants provided their written informed consent to participate in this study.
Author contributions
TA: Formal analysis, Investigation, Writing – original draft, Writing – review & editing. TH: Formal analysis, Investigation, Writing – original draft, Writing – review & editing. HU: Conceptualization, Investigation, Writing – review & editing. KW: Conceptualization, Writing – review & editing. KO: Data curation, Investigation, Writing – review & editing. KT: Validation, Writing – review & editing. SY: Validation, Writing – review & editing. MI: Conceptualization, Investigation, Writing – review & editing.
Funding
The author(s) declare that no financial support was received for the research and/or publication of this article.
Acknowledgments
The authors greatly appreciate the cooperation of the study participants and Shimane CoHRE study members for their assistance.
Conflict of interest
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
Publisher's note
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
Abbreviations
GLM, generalized linear models; Na/K, sodium-to-potassium.
References
1. Ministry of Health, Labor and Welfare. The Second Term of National Health Promotion Movement in the Twenty First Century: A Basic Direction for Comprehensive Implementation of National Health Promotion (2022). Available online at: https://www.mhlw.go.jp/stf/seisakunitsuite/bunya/kenkou_iryou/kenkou/kenkounippon21.html (accessed August 12, 2024).
2. Whelton PK, Carey RM, Aronow WS, Casey DE Jr., Collins KJ, Dennison Himmelfarb C, et al. 2017 Acc/Aha/Aapa/Abc/Acpm/Ags/Apha/Ash/Aspc/Nma/Pcna guideline for the prevention, detection, evaluation, and management of high blood pressure in adults: executive summary: a report of the American college of cardiology/American heart association task force on clinical practice guidelines. Hypertension. (2018) 71:1269–324. doi: 10.1161/hyp.0000000000000066
3. Hisamatsu T, Kogure M, Tabara Y, Hozawa A, Sakima A, Tsuchihashi T, et al. Practical use and target value of urine sodium-to-potassium ratio in assessment of hypertension risk for Japanese: consensus statement by the Japanese society of hypertension working group on urine sodium-to-potassium ratio. Hypertens Res. (2024) 47:3288–302. doi: 10.1038/s41440-024-01861-x
4. Iwahori T, Ueshima H, Torii S, Saito Y, Kondo K, Tanaka-Mizuno S, et al. Diurnal variation of urinary sodium-to-potassium ratio in free-living Japanese individuals. Hypertens Res. (2017) 40:658–64. doi: 10.1038/hr.2016.187
5. Kogure M, Nakamura T, Tsuchiya N, Hirata T, Nochioka K, Narita A, et al. Consideration of the reference value and number of measurements of the urinary sodium-to-potassium ratio based on the prevalence of untreated home hypertension: TMM cohort study. Hypertens Res. (2022) 45:866–75. doi: 10.1038/s41440-021-00843-7
6. Ilich JZ, Blanusa M, Orlić ZC, Orct T, Kostial K. Comparison of calcium, magnesium, sodium, potassium, zinc, and creatinine concentration in 24-H and spot urine samples in women. Clin Chem Lab Med. (2009) 47:216–21. doi: 10.1515/cclm.2009.039
7. Mirmiran P, Gaeini Z, Bahadoran Z, Ghasemi A, Norouzirad R, Tohidi M, et al. Urinary sodium-to-potassium ratio: a simple and useful indicator of diet quality in population-based studies. Eur J Med Res. (2021) 26:1–8. doi: 10.1186/s40001-020-00476-5
8. Mente A, O'Donnell MJ, Rangarajan S, McQueen MJ, Poirier P, Wielgosz A, et al. Association of urinary sodium and potassium excretion with blood pressure. N Engl J Med. (2014) 371:601–11. doi: 10.1056/NEJMoa1311989
9. Jackson SL, Cogswell ME, Zhao L, Terry AL, Wang CY, Wright J, et al. Association between urinary sodium and potassium excretion and blood pressure among adults in the United States: national health and nutrition examination survey, 2014. Circulation. (2018) 137:237–46. doi: 10.1161/circulationaha.117.029193
10. Yang Q, Liu T, Kuklina EV, Flanders WD, Hong Y, Gillespie C, et al. Sodium and potassium intake and mortality among us adults: prospective data from the third national health and nutrition examination survey. Arch Intern Med. (2011) 171:1183–91. doi: 10.1001/archinternmed.2011.257
11. Okayama A, Okuda N, Miura K, Okamura T, Hayakawa T, Akasaka H, et al. Dietary sodium-to-potassium ratio as a risk factor for stroke, cardiovascular disease and all-cause mortality in Japan: the Nippon Data80 cohort study. BMJ open. (2016) 6:e011632. doi: 10.1136/bmjopen-2016-011632
12. Walls AWG, Steele JG, Sheiham A, Marcenes W, Moynihan PJ. Oral health and nutrition in older people. J Public Health Dent. (2000) 60:304–7. doi: 10.1111/j.1752-7325.2000.tb03339.x
13. Chan AKY, Tsang YC, Jiang CM, Leung KCM, Lo ECM, Chu CH. Diet, nutrition, and oral health in older adults: a review of the literature. Dent J. (2023) 11(9):222. doi: 10.3390/dj11090222
14. Marito P, Hasegawa Y, Tamaki K, Sta Maria MT, Yoshimoto T, Kusunoki H, et al. The association of dietary intake, oral health, and blood pressure in older adults: a cross-sectional observational study. Nutrients. (2022) 14: 1279. doi: 10.3390/nu14061279
15. Nomura Y, Ishii Y, Suzuki S, Morita K, Suzuki A, Suzuki S, et al. Nutritional status and oral frailty: a community based study. Nutrients. (2020) 12: 2886. doi: 10.3390/nu12092886
16. Carra MC, Fessi S, Detzen L, Darnaud C, Julia C, Hercberg S, et al. Self-reported periodontal health and incident hypertension: longitudinal evidence from the Nutrinet-Santé E-Cohort. J Hypertens. (2021) 39:2422–30. doi: 10.1097/hjh.0000000000002941
17. Abe T, Tominaga K, Ando Y, Hamano T, Yano S, Isomura M, et al. Reduced masticatory performance and not using dentures are associated with hypertension in older adults with tooth loss: the Shimane Cohre study. Hypertens Res. (2022) 45: 1553–62. doi: 10.1038/s41440-022-00976-3
18. Chen H, Iinuma M, Onozuka M, Kubo K-Y. Chewing maintains hippocampus-dependent cognitive function. Int J Med Sci. (2015) 12:502–9. doi: 10.7150/ijms.11911
19. Abe T, Endo T, Hamano T, Okuyama K, Yano S. Changes in the urinary sodium-to-potassium ratio are associated with blood pressure change in older Japanese adults: a 7-year longitudinal study. J Clin Med. (2022) 11: 5093. doi: 10.3390/jcm11175093
20. Ferdaus SI, Kohno K, Hamano T, Takeda M, Yamasaki M, Isomura M, et al. Altitudes of residential areas affect salt intake in a rural area in Japan: a Shimane Cohre study. Hypertens Res. (2015) 38:895–8. doi: 10.1038/hr.2015.91
21. Abe T, Okuyama K, Kamada M, Kitayuguchi J, Hamano T, Waki H, et al. Association between flexibility activity and blood-pressure change among older adults in Japan: a 5-year longitudinal study. Scand J Med Sci Sports. (2023) 33:1552–9. doi: 10.1111/sms.14386
22. WHO Expert Consultation. Appropriate body-mass index for Asian populations and its implications for policy and intervention strategies. Lancet. (2004) 363:157–63. doi: 10.1016/s0140-6736(03)15268-3
23. Roessler DM. Complete denture success for patients and dentists. Int Dent J. (2003) 53:340–5. doi: 10.1111/j.1875-595X.2003.tb00908.x
24. Roumanas ED. The social solution—denture esthetics, phonetics, and function. J Prosthodont. (2009) 18:112–5. doi: 10.1111/j.1532-849X.2009.00440.x
25. Smith PA, Entwistle VA, Nuttall N. Patients’ experiences with partial dentures: a qualitative study. Gerodontology. (2005) 22:187–92. doi: 10.1111/j.1741-2358.2005.00084.x
26. Huang Y-F, Liu S-P, Muo C-H, Chang C-T. The impact of occluding pairs on the chewing patterns among the elderly. J Dent. (2021) 104:103511. doi: 10.1016/j.jdent.2020.103511
27. Tatematsu M, Mori T, Kawaguchi T, Takeuchi K, Hattori M, Morita I, et al. Masticatory performance in 80-year-old individuals. Gerodontology. (2004) 21:112–9. doi: 10.1111/j.1741-2358.2004.00018.x
28. Inomata C, Ikebe K, Okubo H, Takeshita H, Mihara Y, Hatta K, et al. Dietary intake is associated with occlusal force rather than number of teeth in 80-Y-old Japanese. JDR Clin Trans Res. (2017) 2:187–97. doi: 10.1177/2380084416673963
29. Sheiham A, Steele JG, Marcenes W, Finch S, Walls AW. The impact of oral health on stated ability to eat certain foods; findings from the national diet and nutrition survey of older people in Great Britain. Gerodontology. (1999) 16:11–20. doi: 10.1111/j.1741-2358.1999.00011.x
30. Nowjack-Raymer RE, Sheiham A. Numbers of natural teeth, diet, and nutritional status in US adults. J Dent Res. (2007) 86:1171–5. doi: 10.1177/154405910708601206
31. Lee M-S, Huang Y-C, Wahlqvist ML. Chewing ability in conjunction with food intake and energy status in later life affects survival in Taiwanese with the metabolic syndrome. J Am Geriatr Soc. (2010) 58:1072–80. doi: 10.1111/j.1532-5415.2010.02870.x
32. Piancino MG, Tortarolo A, Polimeni A, Bramanti E, Bramanti P. Altered mastication adversely impacts morpho-functional features of the hippocampus: a systematic review on animal studies in three different experimental conditions involving the masticatory function. PLoS One. (2020) 15:e0237872. doi: 10.1371/journal.pone.0237872
33. Trulsson M. Sensory-motor function of human periodontal mechanoreceptors. J Oral Rehabil. (2006) 33:262–73. doi: 10.1111/j.1365-2842.2006.01629.x
34. Livingstone MB, Prentice AM, Strain JJ, Coward WA, Black AE, Barker ME, et al. Accuracy of weighed dietary records in studies of diet and health. Br Med J. (1990) 300:708–12. doi: 10.1136/bmj.300.6726.708
35. Wen X, Zhou L, Stamler J, Chan Q, Van Horn L, Daviglus ML, et al. Agreement between 24 h dietary recalls and 24 h urine collections for estimating sodium intake in China, Japan, UK, USA: the international study of macro- and micro-nutrients and blood pressure. J Hypertens. (2019) 37:814–9. doi: 10.1097/hjh.0000000000001941
36. Wakai K. A review of food frequency questionnaires developed and validated in Japan. J Epidemiol. (2009) 19:1–11. doi: 10.2188/jea.JE20081007
37. Drewnowski A, Rehm CD, Maillot M, Monsivais P. The relation of potassium and sodium intakes to diet cost among U.S. Adults. J Hum Hypertens. (2015) 29:14–21. doi: 10.1038/jhh.2014.38
38. Margozzini P, Berrios R, García-Huidobro R, Véliz C, Valle C, Vargas JP, et al. Number of remaining teeth and its association with educational level in Chilean adults: data from the national health survey 2016−2017. Int J Dent. (2020) 2020:8848190. doi: 10.1155/2020/8848190
39. Qi X, Pei Y, Wang K, Han S, Wu B. Social isolation, loneliness and accelerated tooth loss among Chinese older adults: a longitudinal study. Community Dent Oral Epidemiol. (2023) 51:201–10. doi: 10.1111/cdoe.12727
Keywords: health checkups, tooth loss, Na/K ratio, older adults, salt intake
Citation: Abe T, Hamano T, Usuda H, Wada K, Okuyama K, Tominaga K, Yano S and Isomura M (2025) Non-use of dentures after tooth loss is associated with elevated sodium/potassium ratios in older adults: a retrospective cohort study. Front. Dent. Med. 6:1479896. doi: 10.3389/fdmed.2025.1479896
Received: 13 August 2024; Accepted: 8 April 2025;
Published: 24 April 2025.
Edited by:
Saurabh Jain, Jazan University, Saudi ArabiaReviewed by:
Maria Grazia Piancino, University of Turin, ItalyValentino Natoli, European University of Madrid, Spain
Copyright: © 2025 Abe, Hamano, Usuda, Wada, Okuyama, Tominaga, Yano and Isomura. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Takafumi Abe, dC1hYmVAbWVkLnNoaW1hbmUtdS5hYy5qcA==
 Takafumi Abe
Takafumi Abe Tsuyoshi Hamano
Tsuyoshi Hamano Haruki Usuda
Haruki Usuda Koichiro Wada1,3
Koichiro Wada1,3 Kenta Okuyama
Kenta Okuyama Shozo Yano
Shozo Yano Minoru Isomura
Minoru Isomura