- 1Department of Pharmacology and Toxicology, Michigan State University, East Lansing, MI, United States
- 2Department of Medicine, Renaissance School of Medicine at Stony Brook University, Stony Brook, NY, United States
- 3Department of Surgery, Henry Ford Pancreatic Cancer Center, Detroit, MI, United States
- 4Biostatistics Shared Resource at Stony Brook Cancer Center, Stony Brook, NY, United States
- 5Department of Family, Population and Preventive Medicine, Renaissance School of Medicine at Stony Brook University, Stony Brook, NY, United States
- 6Department of Medicine, NYC Health + Hospitals/Kings County Hospital Center, Brooklyn, NY, United States
- 7Department of Medicine, State University at New York (SUNY) Downstate Health Sciences University, Brooklyn, NY, United States
- 8Department of Biochemistry and Molecular Biology, Michigan State University, East Lansing, MI, United States
- 9Department of Pathology, Henry Ford Health, Detroit, MI, United States
Background: Previous analyses of bulk colon and rectal adenocarcinoma (COAD/READ) RNA-sequence data comparing African ancestry (AA) and European ancestry (EA) groups have reported differentially expressed genes related to the immune response. However, these previous analyses of AA versus EA tissues did not control for mismatch-repair enzyme (MMR)/microsatellite instability (MSI) status, which is also associated with altered expression of immune related genes, and is used to determine eligibility for immune checkpoint inhibitor therapy.
Methods: TCGA-COAD-READ bulk RNA-sequence data were analyzed to identify immune related genes that were significantly associated with AA and MMR-deficient (MMR-d)/MSI-High (MSI-H) groups. Reverse transcriptase-quantitative polymerase chain reaction (RT-qPCR) assays for selected immune genes relative to two reference genes, (C1ORF43 and RAB7A) were conducted on an independent set of AA (n = 59) vs. EA (n = 59) formalin-fixed paraffin embedded (FFPE) samples enriched for MMR-d/MSI-H samples. Multiple linear regression models were employed to investigate ancestry and MMR/MSI status while controlling other variables.
Results: Multivariable regression analysis of the TCGA-COAD-READ data revealed that CXCL10 expression was lower in AA vs. EA groups and higher in MMR-d/MSI-H vs. MMR-proficient (MMR-p)/MSI-Low (MSI-L)+microsatellite stable (MSS) groups while controlling for COAD/READ location and stage. Neither COAD/READ stage or location were significant while controlling for ancestry and MMR/MSI status. CXCL10 is an important chemokine that regulates the tumor immune microenvironment. The number of AA MMR-d/MSI-H samples in the TCGA-COAD-READ dataset was too low (n = 9) to detect a significant effect of AA on CXCL10 expression across MMR/MSI status. CXCL10 mRNA levels measured by RT-qPCR in an independent set of COAD FFPE samples enriched for AA MMR-d/MSI-H samples, confirmed that CXCL10 expression was higher in MMR-d/MSI-H samples compared to MMR-p/MSI-L+MSS, however, differences in CXCL10 expression between AA vs. EA did not reach significance.
Discussion: These results did not detect significant effects of AA on CXCL10 expression across MMR/MSI status.
1 Introduction
Colorectal adenocarcinoma (COAD/READ) is the second leading cause of all cancer related deaths in the US (1). In the US, the African continental ancestry population group has both a higher incidence and poorer survival for COAD/READ compared with the European ancestry (EA) group (1). Multiple factors including socioeconomic factors that affect access to prevention and early diagnosis of COAD/READ (2) contribute, but do not fully explain these disparities. Previous studies of COAD/READ bulk RNA sequencing data generated from fresh/frozen COAD/READ samples have reported African vs. European ancestry (AA vs. EA) tissues exhibit numerous differentially expressed genes (DEGs), including genes related to the tumor immune microenvironment (3–10). A major limitation of these studies is the small numbers of African ancestry (AA) samples included in these studies. Most of the previous analyses used The Cancer Genome Atlas (TCGA) RNA-sequencing dataset (11), which has the largest but still limited number (n=64) of AA COAD/READ samples, in addition to data generated from smaller sets of 6–15 AA COAD samples.
These previous analyses were conducted without considering mismatch repair enzyme-deficiency/microsatellite-high (MMR-d/MSI-H) status as a potential confounding variable. Universal screening of COAD/READ biopsies and surgical resection pathology specimens for MMR-d/MSI-H status is now routinely conducted at US medical centers. This is because MMR-d/MSI-H patients are more responsive to immune checkpoint inhibitors (12). This may relate to higher expression of immune related genes, such as C-X-C motif chemokine 10 (CXCL10) gene (13, 14). MMR-d/MSI-H status is associated with increased cytoplasmic damaged DNA, which triggers the cyclic GMP-AMP synthase - stimulator of interferon genes (c-GAS/STING) pathway. This leads to activation of interferon gamma signaling pathways and activation of the CXCL10-CXCR3 axis, which has been shown to regulate immune cell homing and activation (14, 15).
A univariate analysis of two publicly accessible AA vs. EA bulk RNA sequence datasets revealed that CXCL10 expression was lower in AA vs. EA groups (16). To test the hypothesis that ancestry could affect CXCL10 expression levels across MMR/MSI status, the AA vs. EA TCGA-COAD-READ RNA-seq was reanalyzed with a focus on both ancestry and MMR/MSI status. Because COAD samples annotated for both ancestry and MMR/MSI status were not available in commercial tissue banks, we assembled an independent set of 134 AA and EA COAD formalin fixed paraffin embedded (FFPE) samples from three medical centers. This independent cohort included roughly equal numbers of AA MMR-d/MSI-H, AA MMR-p/MSI-L+MSS, EA MMR-d/MSI-H, and EA MMR-p/MSI-L+MSS, because of our focus on African ancestry and MMR-d/MSI-H COAD/READ. This cohort is therefore enriched for self-identified African ancestry and MMR-d/MSI-H because only ~12% of US COAD/READ cases has evidence of African ancestry (17) and only ~15% have MMR-d/MSI-H status (18).
2 Methods
2.1 Data acquisition and identification of DEGs
The Cancer Genome Atlas Colonic adenocarcinoma (TCGA-COAD) RNA sequence data from AA (n = 64) and EA (n =284) groups was downloaded as unstranded STAR (raw) counts and processed TPM by using TCGAbiolinks R/Bioconductor package (19). The following clinical metadata variables were also downloaded from TCGA: 1.) age at time of collection (years); 2. sex (male/female); self-identified ancestry (African/European); COAD/READ tumor location (right, left; COAD/READ stage (I,II,III,IV); and MSI status. MSI status was available for 327 out of 348 samples (20). For 17 of 21 samples without MSI-status values, the Microsatellite Analysis for Normal Tumor InStability (MANTIS) scores in the TCGA-COAD-READ database were used to categorize MSI status (21). Samples with MANTIS scores < 0.4 were categorized as MMR-p/MSI-L+MSS and scores ≥ 0.4 were categorized as MMR-d/MSI-H. The raw counts of 15 AA and 18 EA COAD samples from the SUNY Stonybrook/Downstate medical centers were downloaded from Gene Expression Omnibus (GEO) with the accession number GSE146009 (7). The COAD data in GSE146009 was downloaded from 15 AA and 18 EA samples, which were annotated with respect to ancestry but not for MMR/MSI status. The raw counts were used as input for identifying differentially expressed genes (DEGs) using edgeR (22). After using edgeR to normalize the raw counts, the resulting “cpm” counts were used as input into the wilcox.test function in R (v4.0.2) as previously described (23). The threshold for identifying DEGs was the absolute value│log2 fold change│≥ 1 and adjusted p-value <0.05 The consensus molecular subtypes (CMS) labels reported for the TCGA-COAD-READ dataset based on CMS network and CMS Random Forest (RF) were downloaded from cms_labels_public_all.txt - syn4978511 - Files (24). The abundance of tumor associated T-cells was estimated using CIBERSORT analysis of the TCGA-COAD-READ RNA-sequence data (25).
2.2 Assembly of COAD FFPE samples from three US medical centers.
Assembly of 134 de-identified adult (age > 18) human COAD/READ FFPE tissue samples archived between 2012 and 2024 from three US medical institutions, Stony Brook University Hospital (Stony Brook, NY), New York City Health + Hospitals (NYCH+H)/Kings County Hospital (KCH, Brooklyn, NY), and Henry Ford Health Center (Detroit, MI) was approved by the Stony Brook Institutional Review Board (sIRB2024-0020) with reliance forms reviewed by the Institutional Review Boards for Henry Ford Health Center and Michigan State University. No reliance form was required for NYCH+H/KCH since the research protocol included an honest broker that oversaw HIPAA compliance, was conducted with waiver of consent and was determined to be not human research by its Institutional Review Board (IRB1949860). Only initial surgical resections of treatment-naïve sporadic COAD-READ (excluding inflammatory bowel disease-associated and hereditary COAD-READ syndromes) were selected for analysis. The samples were linked to deidentified clinical metadata curated from electronic medical records by physicians at each of the three medical centers using a common data dictionary as previously described (26). The variables collected for the metadata included: 1.) age at the time of the sample collection (years), 2.) sex (male/female); 3.) ancestry (AA vs. EA) based on self-identification, 4.) ethnicity (all non-Hispanic); 5.) body mass index (BMI, kg/m2); 6.) diabetes mellitus status (type 1 diabetes, type 2 diabetes (T2DM), no diabetes); 7.) smoking (current, former, never); 8.) COAD tumor location (right defined as cecum, ascending colon, hepatic flexure, transverse colon; left defined as including splenic flexure, descending colon, sigmoid, rectum); 9.) COAD stage (1-4); 10.) MMR-d/MSI-H vs. MMR-p/MSI-L+MSS status classified primarily by immunohistochemistry (IHC); 11.) insurance status (Commercial/Medicare; Medicaid Mgd; Medicaid/Self-Pay).
2.3 RT-qPCR analysis of COAD-READ FFPE samples.
Total RNA was extracted from 5 µm COAD FFPE curls using the RecoverAll™ Total Nucleic Acid Isolation Kit (Thermo Fisher Scientific Inc, Waltham, MA) according to the manufacturer’s recommendation, except paraffin was removed by xylene washes, the protease digestion was extended to 3 hours at 50°C. 200–500 ng of total bulk RNA was reverse transcribed using Superscript IV™ VILO™ cDNA kit (Thermo Fisher Scientific Inc, Waltham, MA) according to the manufacturer’s recommendation qPCR was performed using the Applied Biosystems QuantStudio 3 Real Time PCR System (Thermo Fisher Scientific Inc., Waltham, MA). The 20 μl dual probe (target immune gene/reference gene) PCR reactions included 1-2 μl cDNA (corresponding to 25 ng of RNA), 1 μl 1× TaqMan Universal PCR master mix, 1 μl for each primers/pre mix (for target and reference gene) The reactions, run in triplicate, were incubated in a 96-well optical plate at 95 °C for 10 min, followed by 40 cycles of 95 °C for 15 s and 60°for 10 min. The threshold cycle (Ct) was defined as the fractional cycle number at which the fluorescence passes the fixed threshold. The Ct data were determined using default threshold settings. Taqman® primer probe set IDs for the target genes were: CXCL10 (HS00171042), CD45 (HS04189704) and CD3D (HS00174158). The Taqman® primer probe set IDs for the reference genes were: RAB7A (HS01115139) and C1ORF43 (HS00367486). A previous study reported that RAB7a and C1ORF43 were best suited for normalizing RT-qPCR assays of COAD/READ samples (27), particularly because of the low covariance exhibited by these two reference genes. These commercial probe/primer sets have been used extensively in previous publications including the study evaluating the two COAD reference genes (27). The ΔCt were calculated as reference gene Ct – target gene Ct to estimate the log transformation of the ratio of target gene/reference gene templates in the reactions.
2.4 Statistical analysis
TCGA CXCL10 outcomes were expressed as CXCL10 log2TPM. The RT-qPCR CXCL10 values were expressed as C1ORF43 Ct - CXCL10 Ct and RAB7A Ct - CXCL10 Ct. CD45 values were expressed as C1ORF43 Ct – CD45 Ct and RAB7A Ct – CD45 Ct, and CD3D values were expressed as C1ORF43 Ct – CD3D Ct and RAB7A Ct – CD3D Ct. Spearman’s correlation was used to examine the linear correlation between CXCL10 and continuous variables such as age, CD45 and CD3D values. The Wilcoxon rank sum test (for variables with 2 levels) or Kruskal-Wallis test (for variables with ≥ 3 levels) was utilized to examine the marginal difference in outcomes among categorical variables. For the Kruskal Wallis test, a Dunn’s post-hoc test was used to compare individual groups with each other. Multiple linear regression models were then utilized to examine whether there was a difference in the ancestry level or MMR status after adjusting for COAD/READ location and COAD/READ stage. 134 independent human COAD/READ FFPE tissue samples are expected to have 90% power to detect an increase in R2 being 6.5% while the R2 of model using covariates alone being 11.5% based on a multiple regression full-versus-reduced-model F-test with a Type I error rate of 0.05 (28). Both R2s in the sample size justification are estimated from TCGA data. Statistical analysis was performed using GraphPad Prism 10 (for some univariate analyses), by using the cor.test () function in R version 4.44 to calculate correlation coefficients and SAS 9.4 (SAS Institute Inc., Cary, NC). Significance level was set at 0.05.
3 Results
3.1 CXCL10 transcript expression is lower in AA vs. EA in two independent COAD-READ tumor bulk RNA-sequence datasets
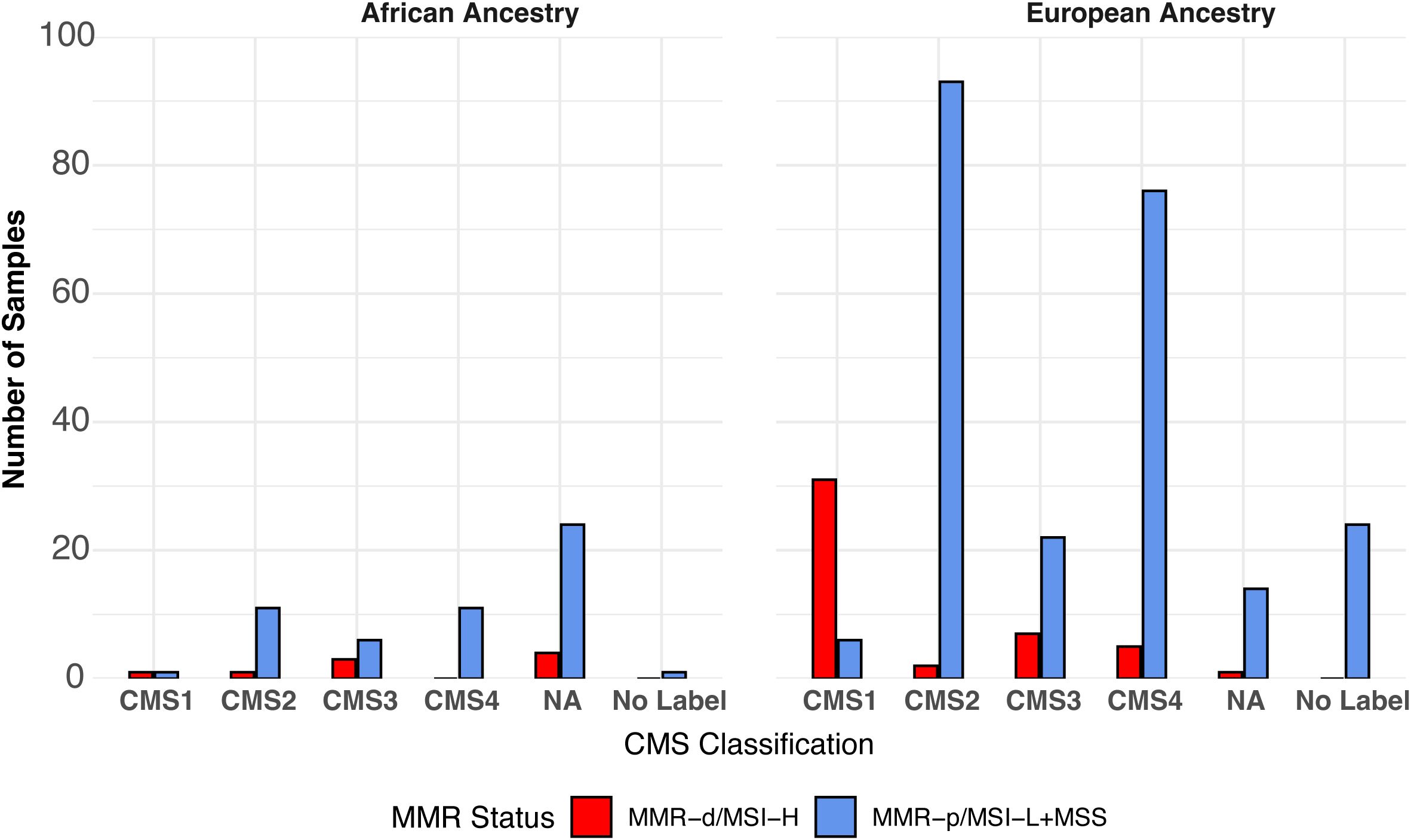
As shown in Figure 1, CXCL10 was identified as AA vs. EA differentially expressed genes (DEGs), which were expressed at a lower level in AA vs. EA COAD/READ samples in both the TCGA-COAD-READ (64 AA vs. 284 EA) and a smaller SUNY Downstate/Stony Brook (15 AA vs. 18 EA) bulk RNA sequence datasets, using edgeR (22, see Supplementary Table S1).
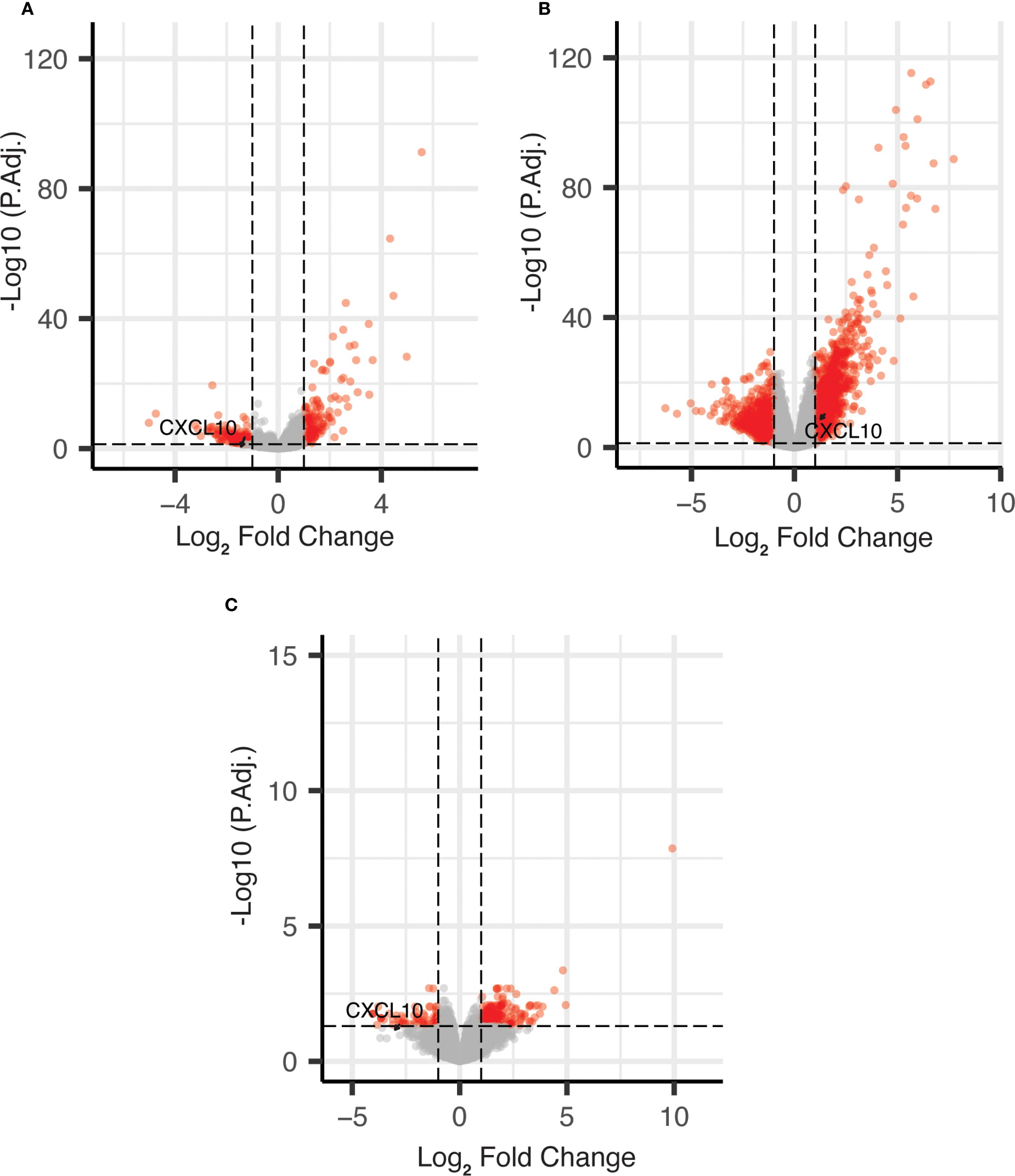
Figure 1. Volcano plots of DEGs for African vs. European ancestry and MMR-d/MSI-H using edgeR. (A) African vs. European ancestry DEGs in TCGA COAD dataset; (B) MMR-d/MSI-H vs. MMR-p/MSI-L+MSS DEGs in TCGA COAD dataset; (C) African vs. European ancestry DEGs in SUNY Downstate/Stony Brook dataset.
3.2 Categorization of MMR/MSI status between AA and EA TCGA-COAD-READ samples
MMR/MSI-status of the TCGA-COAD samples was obtained by downloading the TCGA-COAD-READ metadata and the MSI status reported previously for 327/348 samples (20). Of the 21 samples lacking MSI status values, 17 were categorized by using the MANTIS score (21). No information on the MMR/MSI status was provided for the smaller SUNY Downstate/Stony Brook RNA-seq dataset (7). The distribution of consensus molecular subtype (CMS1, CMS2, CMS3, CMS4, No Label) previously assigned to the TCGA-COAD-READ samples (24) for:1.) AA MMR-p/MSI-L+MSS; 2.) AA MMR-d/MSI-H; 3.) AA MMR undetermined; 4.) EA MMR-p/MSI-L+MSS; 5.) EA MMR-d/MSI-H vs. MMR-p/MSIL+MSS are shown in Figure 2. CMS1 has been associated with high expression of immune-related genes and MMR-d/MSI-H (22). CMS2 has been associated with a differentiated epithelial cell phenotype. CMS3 has been termed the metabolic subtype because of dysregulated metabolic genes. CMS4 is associated with a high stromal content. Some of the COAD samples could not be readily assigned to a single CMS and have been termed No Label. Thirty-seven (13%) of the 284 EA samples were labeled as CMS1. Thirty-one (84%) of the 37 EA CMS1 samples were also MMR-d/MSI-H. Only two (3%) of 64 AA samples were labeled as CMS1. Only one (50%) of two AA CMS1 samples was also MMR-d/MSI-H.
Overlap between TCGA-COAD-READ AA vs. EA DEGs and MMR-d/MSI-H vs. MMR-p/MSI-L+MSS DEGs
To reduce the number of false positive DEGs, the Wilcoxon rank sum test was used to determine the overlap between the AA vs. EA DEGs and the MMR-d/MSI-H vs. MMR-p/MSI-L+MSS DEGs (23). The number of AA vs. EA DEGs was reduced to 39 from 420, and the number of MMR-d/MSI-H vs. MMR-p/MSI-L+MSS DEGs was reduced to 738 from 2177 (see Supplementary Table S1). The overlap between the 39 AA vs. EA DEGs and the 738 MMR-d/MSI-H vs. MMR-p/MSI-L+MSS DEG lists consists of 7 genes (CXCL10, ALOX15B, IDO1, HCAR2, MARCO, OR2I1P and MTND4P24. Six of seven DEGs were decreased in the AA group and increased in the MMR-d/MSI-H group (CXCL10, ALOX15B, IDO1, HCAR2, MARCO and OR2I1P). The first five DEGs have been linked to macrophage function and in some instances with COAD/READ (29–34). OR2I1P is a pseudogene with unknown function. MTND4P24, which is increased in AA vs. EA and decreased in the MMR-d/MSI-H vs. MMR-p/MSI-L+MSS groups, is a pseudogene with unknown function.
Analysis of variables affecting CXCL10 mRNA expression in the TCGA-COAD dataset
Further analysis of the effects of AA and MMR-d/MSI-H status focused on CXCL10 log2TPM as the outcome because this gene plays a key role in regulating COAD/READ tumor microenvironment in MMR-d/MSI-H samples (14, 15). Differences in CXCL10 values were significantly associated with ancestry, MMR/MSI status, COAD/READ location, COAD/READ stage, but not sex (see Table 1). Age was not significantly correlated with CXCL10 levels. Multiple linear regression models were used to examine associations to CXCL10 expression while adjusting for COAD/READ stage, and with and without COAD/READ location, because of the number of missing location values. As shown in Table 1, CXCL10 values were lower in AA vs. EA (p -value < 0.0001) and higher in MMR-d/MSI-H vs. MMR-p/MSI-L+MSS (p-value < 0.0001), while controlling for COAD/READ stage and location. Neither COAD/READ stage nor location were significant, while controlling for ancestry and MMR/MSI status. Although MMR-d/MSI-H status has been previously correlated with right colon location (35), no significant multicollinearity was detected between the co-variables (results not shown). Estimated differences in CXCL10 due to ancestry across MMR/MSI status were not significant (see Table 2). Consistent with CXCL10’s role as a T-cell attractant was the significant correlation (Spearman’s correlation coefficient r= 0.44, p-value <0.0001) detected between CXCL10 log2TPM values and T-cell abundance estimated by CIBERSORT (see Supplementary Figure S1).
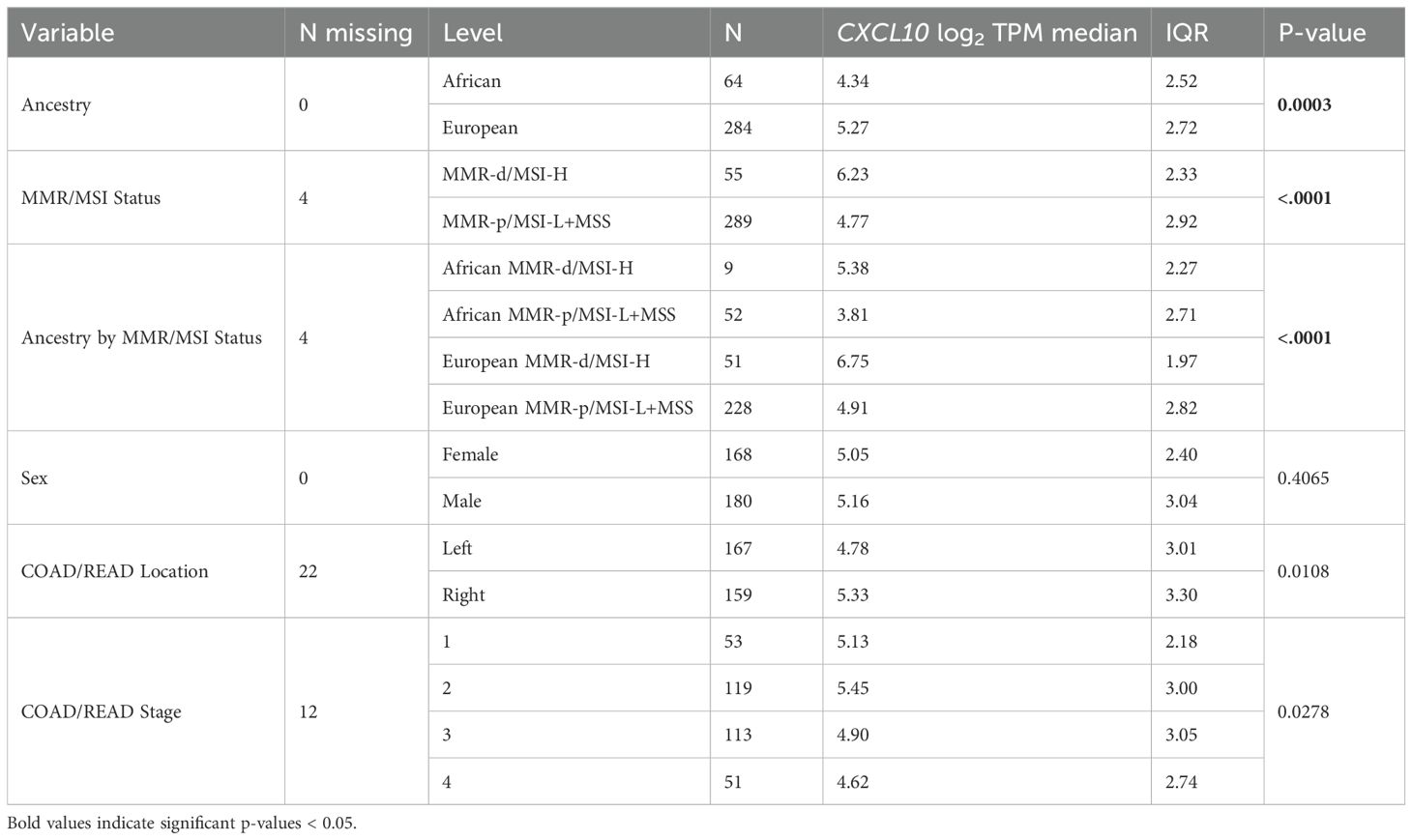
Table 1. Univariate analysis of CXCL10 log2TPM values from the TCGA-COAD-READ dataset with co-variables.
Table 2. Multiple linear regression models of estimated differences in TCGA-COAD CXCL10 log2TPM values with 95% confidence interval (CI).
Exploratory analysis comparing CXCL10 log2TPM values to CMS labels within each ancestry group (see Supplementary Figure S2), detected no significant difference between CMS labels within the AA group. In contrast, significant differences were detected between CMS labels in the EA group (p-value <0.0001). Dunns post-hoc test detected significantly increased CXCL10 expression in the EA CMS1 group compared with both CMS2 (p-value <0.0001) and CMS3 groups (p-value<0.0001), but not CMS4 or No Label groups. Also, CXCL10 log2 TPM values were significantly higher in EA CMS4 compared with both CMS2 (p-value<0.0001) and CMS3 (p-value=0.0002) groups, but not CMS1 or No Label groups.
RT-qPCR results from an independent set of COAD/READ FFPE samples enriched for AA MMR-d/MSI-H COAD samples
Because only 9 of the AA TCGA COAD/READ samples were MMR-d/MSI-H, an independent set of 134 COAD FFPE samples was assembled from three medical centers that was composed of roughly equal numbers of AA MMR-d/MSI-H, AA MMR-p/MSI-L+MSS, EA MMR-d/MSI-H, EA MMR-p/MSI-L+MSS. Amplifiable RNA by RT-qPCR was recovered from 118 (88%) of the samples. CXCL10 expression was normalized relative to two reference genes as C1ORF43 Ct – CXCL10 Ct and RAB7A Ct – CXCL10 Ct (see Figure 3). Loss of 12% of the original 134 samples resulted in the expected power being reduced from 90% to 87%. Univariate analyses of both values confirmed that CXCL10 values were significantly higher in MMR-d/MSI-H vs. MMR-p/MSI-L+MSS (see Tables 2, 3). In contrast to the TCGA-COAD CXCL10 log2 TPM values, the RT-qPCR CXCL10 values relative to both reference genes trended slightly higher in AA vs. EA but these differences did not reach significance. Differences in C1ORF43 Ct – CXCL10 Ct values were associated with COAD/READ location but not with COAD/READ stage, and differences in RAB7A Ct – CXCL10 Ct values were associated with COAD/READ stage but not with COAD/READ location. Neither RT-qPCR CXCL10 values were significantly associated with age or sex. When the same multivariable model used to analyze the TCGA CXCL10 log2 TPM results was applied to the RT-qPCR results (Tables 3–6), AA C1ORF43 Ct - CXCL10 Ct (p = 0.0438) and RAB7A Ct – CXCL10 Ct (p-value = 0.0497) values were higher than EA values, MMR-d/MSI-H C1ORF43 Ct – CXCL10 Ct (p-value = 0.019) and RAB7A Ct - CXCL10 Ct (p-value = 0.093) values were higher or trended higher than MMR-p/MSI-L+MSS values, while controlling for COAD/READ stage and location.
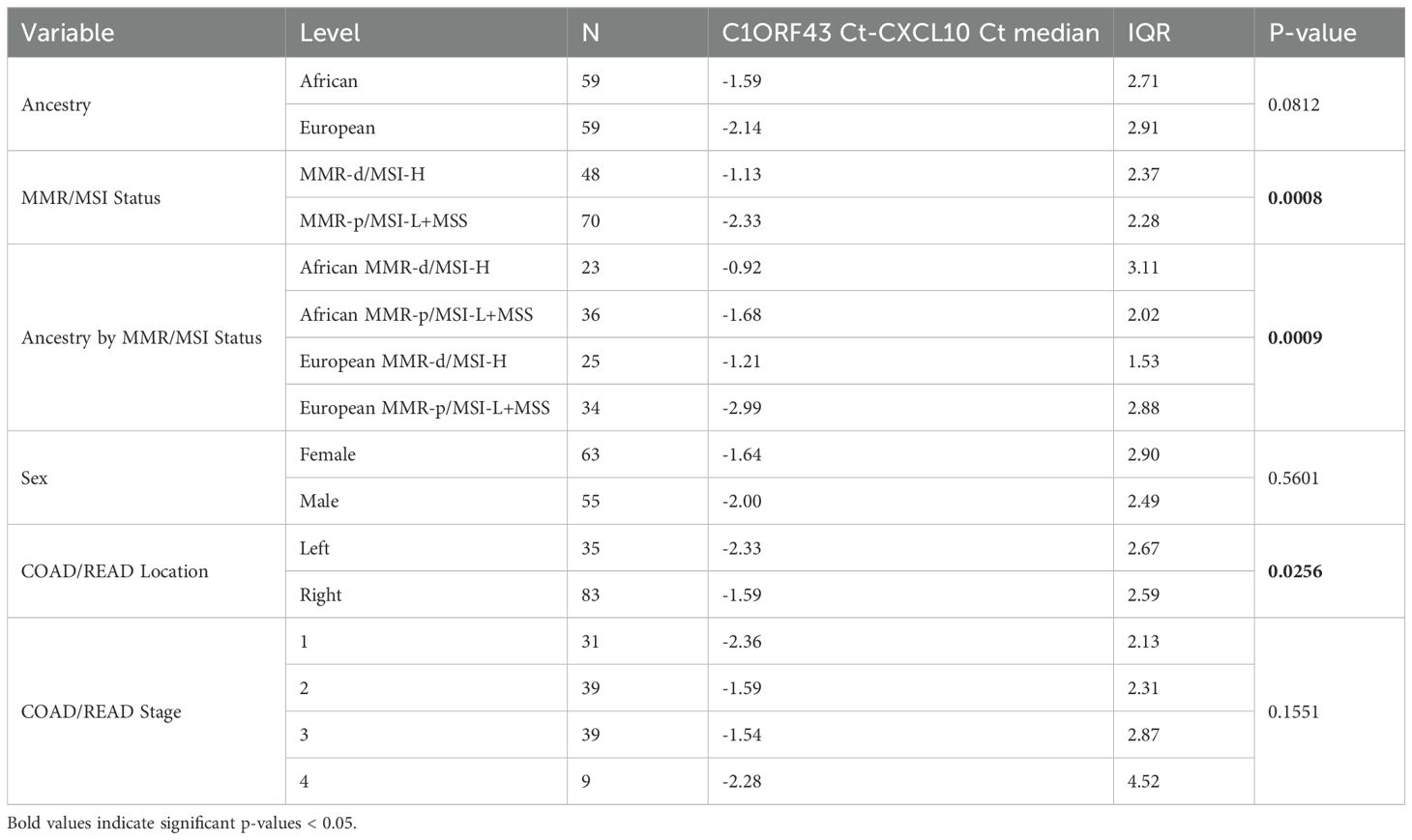
Table 3. Univariate analysis of RT-qPCR C1ORF43 Ct – CXCL10 Ct results from an independent set enriched for MMR-d/MSI-H COAD/READ FFPE samples.
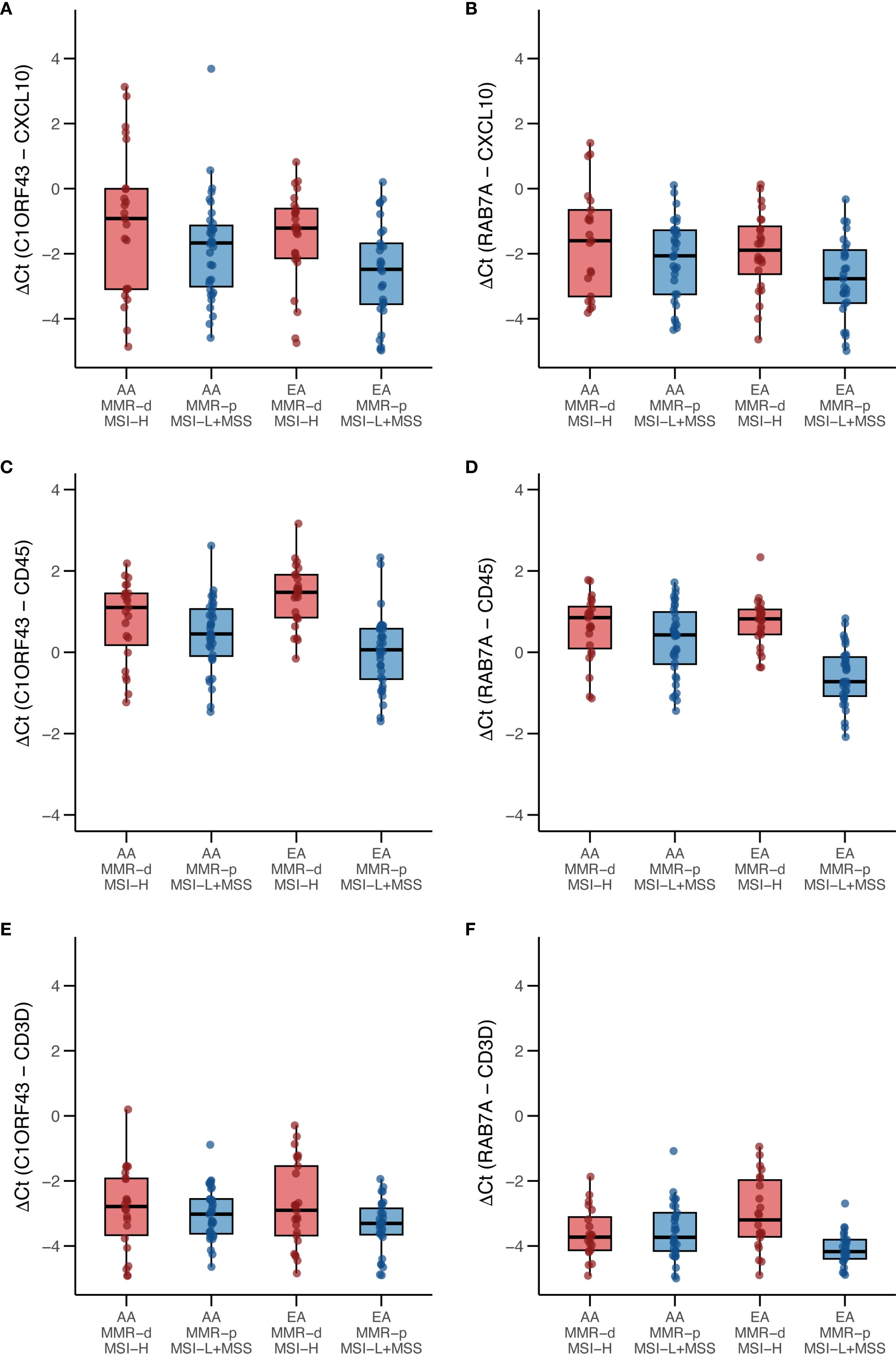
Figure 3. Box and whisker plots of RT-qPCR analysis of CXCL10, CD45 and CD3D expression in an independent set enriched for African ancestry (AA) MMR-d/MSI-H COAD FFPE samples. (A) C1ORF43 Ct - CXCL10 Ct; (B) RAB7A Ct – CXCL10 Ct; (C) C1ORF43 Ct – CD45 Ct; (D) RAB7A Ct – CD45 Ct, (E) C1ORF43 Ct – CD3D Ct, (F) RAB7A Ct – CD3D Ct.
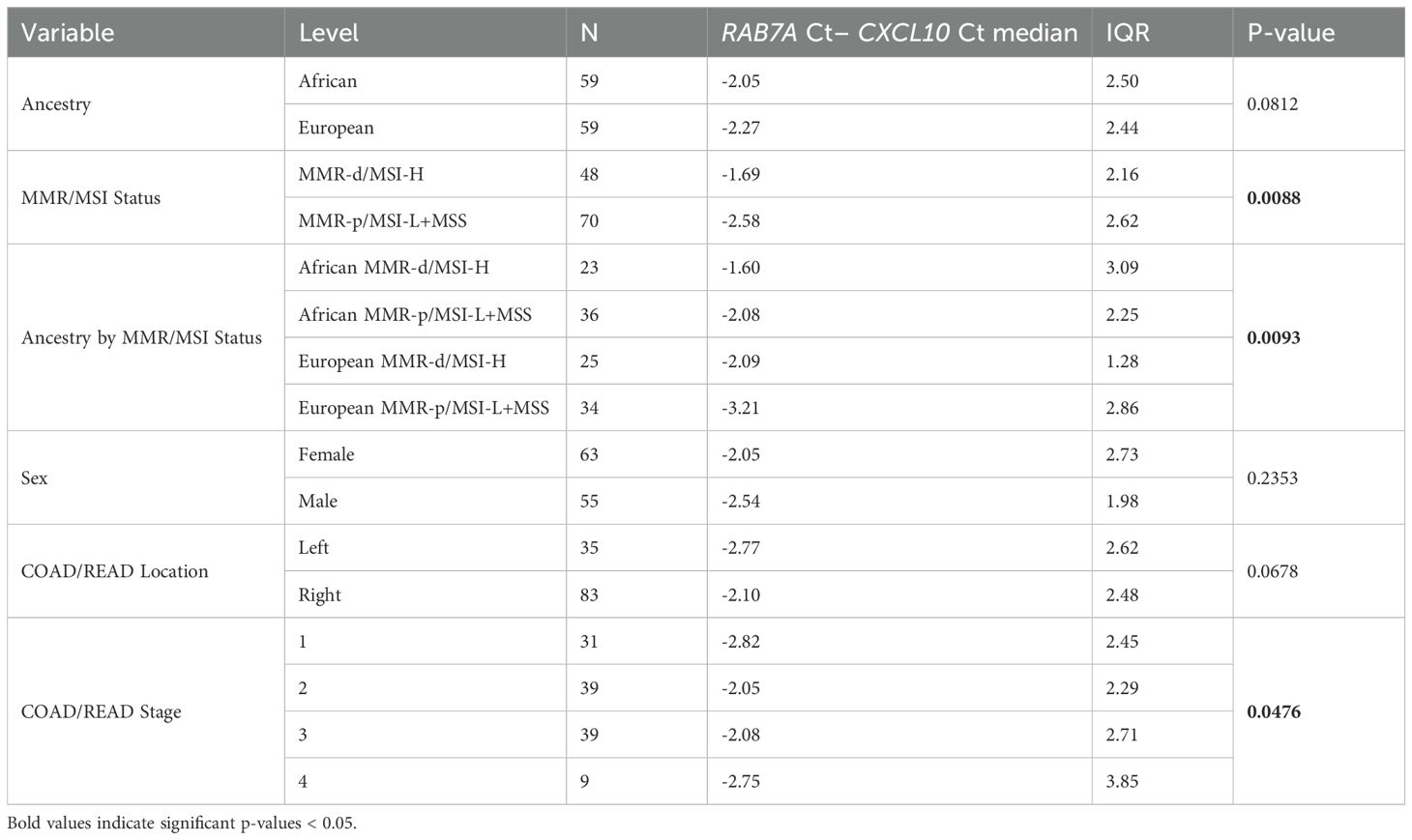
Table 4. Univariate analysis of RT-qPCR RAB7A Ct - CXCL10 Ct results from an independent set of COAD/READ FFPE samples.
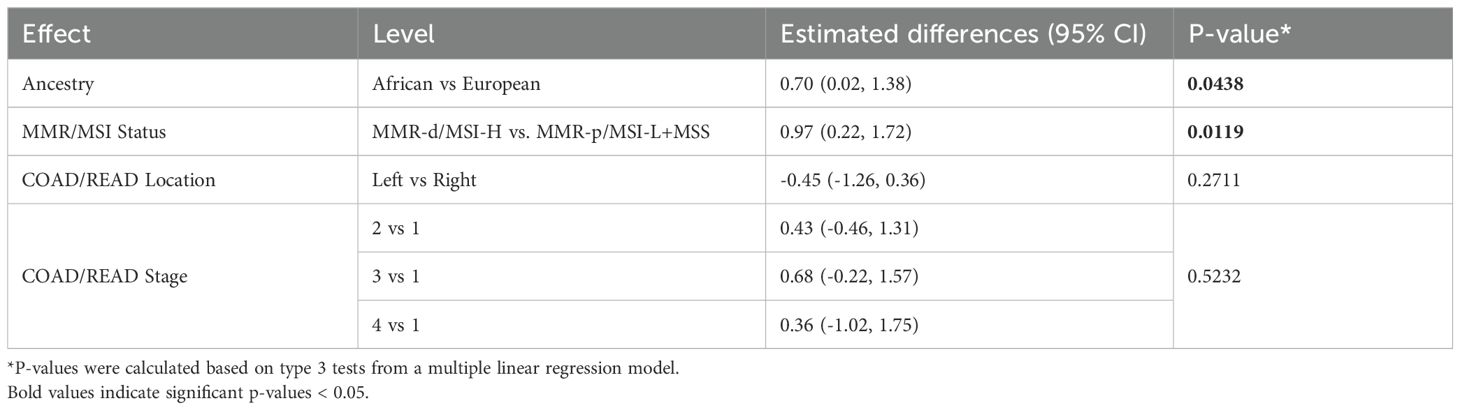
Table 5. Multivariable regression model of estimated differences in C1ORF43 Ct – CXCL10 Ct results with 95% CI from an independent set enriched for MMR-d/MSI-H COAD/READ FFPE samples.
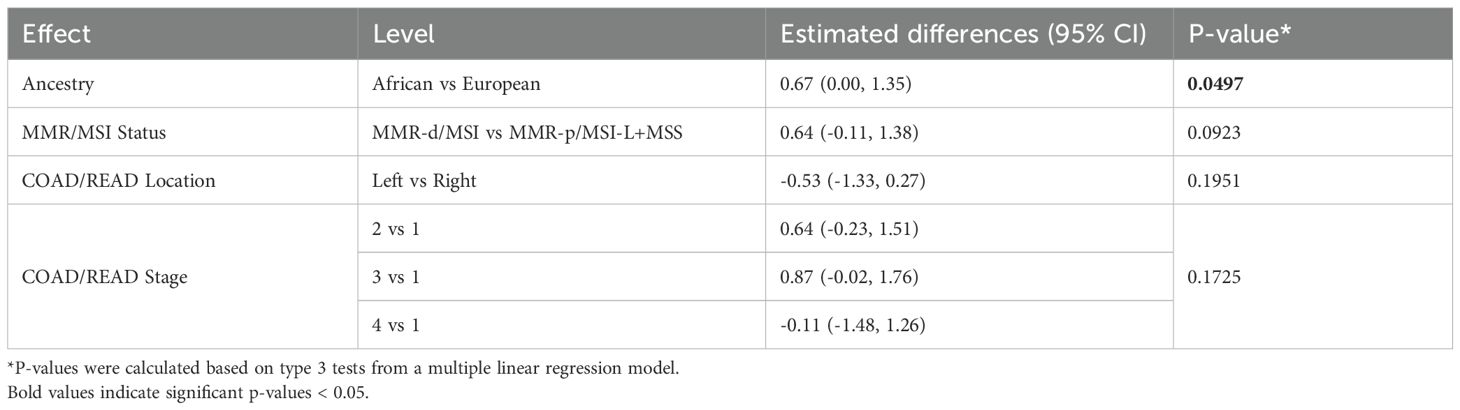
Table 6. Multivariable regression model of estimated differences in RAB7A Ct – CXCL10 Ct results with 95% CI from an independent set enriched for MMR-d/MSI-H COAD/READ FFPE samples.
Parallel RT-qPCR assays were conducted for CD45, a myeloid/general white cell marker, and CD3D, a T-cell marker in the independent set of COAD/READ FFPE samples (see Figure 3). In single cell RNA-sequence datasets, CXCL10 has been shown to be highly expressed in myeloid cell types (29). CXCL10 has been shown to be a T-cell attractant (36). Consistent with these reports are the strong positive correlations (see Figure 4) observed between C1ORF43 Ct - CXCL10 Ct and C1ORF43 Ct - CD45 Ct (Spearman correlation coefficient = 0.54, p-value < 0.0001), between RAB7A Ct - CXCL10 Ct and RAB7A Ct - CD45 Ct (Spearman correlation coefficient r =0.44, p-value < 0.0001), between C1ORF43 Ct- CXCL10 Ct and C1ORF43 Ct – CD3D Ct (Spearman correlation coefficient r = 0.51, p-value < 0.0001), and between RAB7A Ct - CXCL10 Ct and RAB7A Ct – CD3D Ct (Spearman correlation coefficient r = 0.34, p value < 0.0001).
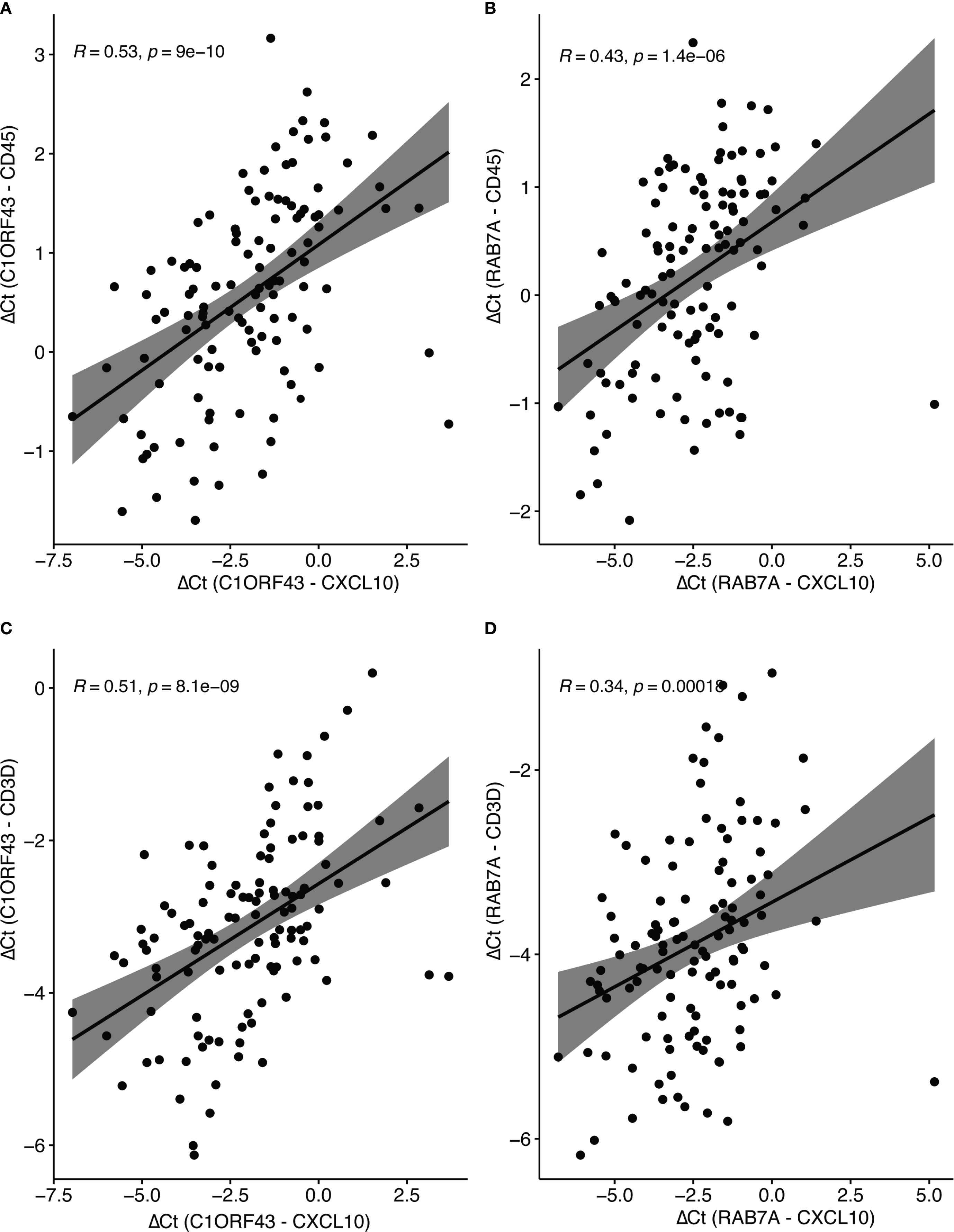
Figure 4. Spearman correlation of RT-qPCR CXCL10 and Immune Cell Type Markers (CD45 and CD3d). Scatter plots show correlations between ΔCt values of CXCL10 (normalized to reference genes C1ORF43 or RAB7A). (A) CXCL10 vs CD45 (C1ORF43 reference). (B) CXCL10 vs CD45 (RAB7A reference). (C) CXCL10 vs CD3D (C1ORF43 reference). (D) CXCL10 vs CD3D (RAB7A reference).
5 Discussion
Previous analyses of the AA vs. EA TCGA-COAD dataset have highlighted AA vs. EA DEGs, particularly lower expression of immune related genes in the African vs. European ancestry groups. The current study differs from the previous studies by using multivariable analysis to examine potentially confounding variables such as MMR/MSI status, rather than attempting to control for these factors by propensity matching. Differences in the DEGs identified in the current study from previous studies may relate to the use of unprocessed counts as opposed to processed counts as input, and use of different DEG platforms (edgeR and Wilcoxon rank sum test). The current study identified five AA vs. EA immune related genes, including CXCL10 that were expressed at lower levels in the AA, but expressed at higher level in MMR-d/MSI-H group. CXCL10 is part of the CXCL9, 10, 11-CXCR3 axis, which plays an important role in tumor immune microenvironment remodeling (36). CXCL10 has been positively correlated with COAD/READ survival (37, 38).
The percentages of MMR-d/MSI-H in the TCGA-COAD-READ AA vs. EA samples were 14.1% vs. 16.0%, consistent with previous reports that the prevalence of MSI-d/MSI-H is lower in the AA vs. EA cohort (18). This small difference in prevalence does not explain the greater than 2-fold difference in CXCL10 expression between the two groups. Multivariable models confirmed that TCGA-COAD-READ CXCL10 expression values were lower in AA vs. EA, and higher in MMR-d/MSI-H vs. MMR-p/MSI-Low, while controlling for COAD/READ location and COAD/READ stage. Neither COAD/READ location nor stage were significantly associated with TCGA CXCL10 levels, when controlling for ancestry and MMR/MSI status. The total number of AA MMR-d/MSI-H samples was only 9 of 348 total samples, which clearly restricted the ability to detect statistically significant differences in CXCL10 expression across groups stratified by both ancestry and MMR/MSI-status.
The consensus molecular subtype (CMS) classification is the most widely accepted gene expression based categorization of transcriptional profiles. It was based on applying machine learning (random forest) to five publicly accessible COAD/READ bulk RNA sequencing datasets, including the TCGA dataset (24). Our results demonstrate that the distribution of CMS1 labels in the AA cohort is very different from that of the EA cohort. Only in the EA cohort is the high association between CMS1 classification and MMR-d/MSI status observed. Furthermore, the significantly increased CXCL10 expression values in the CMS1 group compared to CMS2 and CMS3 groups is observed only in the EA cohort and not in the AA cohort. If the public datasets used to develop the CMS classifications had poor representation of self-identified African ancestry COAD/READ samples, this could explain the different distributions of CMS labels between the two ancestry groups. Associations of the CMS3 classification and African ancestry and obesity has recently been reported (39, 40). Because obesity has been reported to be most prevalent in US self-identified African ancestry AA group (41), it may be important to control for obesity as a potentially confounding variable. Unfortunately, many of the TCGA-COAD-READ samples are missing body mass index (BMI) values.
The limited number of AA MMR-d/MSI-H samples in TCGA-COAD combined with the lack of AA samples annotated for MMR/MSI status from commercial vendors underscores the need for ancestrally diverse cohorts with robust clinical annotations. To further investigate the effect of African ancestry across MMR/MSI status, an independent set of COAD/READ FFPE samples was assembled from three medical centers that was enriched for AA and MMR-d/MSI-H samples. Approximately 2% of MMR-d/MSI COAD/READ have germline mutations or Lynch syndrome, but COAD/READ samples with germline MMR mutations were excluded from this independent set of samples. The relative proportion of the AA group was increased to match the number of EA group, and the percentage of MMR-d/MSI-H samples increased to 39% in the AA group and 42% in the EA group of the independent set of COAD FFPE samples. Normalized CXCL10 mRNA expression (see Tables 1, 3, 4) was significantly higher in the MMR-d/MSI-H group vs. the MMR-p/MSI-L+MSS groups for both the TCGA-COAD-READ RNA-sequence data set (p-value=0.0003) and the independent FFPE RT-qPCR datasets (p-value =0.0003 for C1ORF43 as reference gene, p-value = 0.0008 for Rab7a as the reference gene). However, there were differences between the TCGA-COAD-READ RNA-sequence dataset and the independent FFPE RT-qPCR results, when normalized CXCL10 expression values were compared between African vs. European ancestry groups. While normalized CXCL10 mRNA expression was significantly lower in the AA vs. EA TCGA-COAD-READ RNA-sequence data set, no significant difference was observed between the AA vs. EA independent set RT-qPCR datasets using either of the two reference genes (see Tables 1, 3, 4). In fact, the normalized RT-qPCR CXCL0 mRNA values trended somewhat higher in the AA vs. EA group for both reference genes. The discordant AA vs. EA CXCL10 results between the TCGA-COAD-READ and the independent FFPE datasets could potentially relate to 1.) differences in the proportion of AA MMR-d/MSI-H, AA MMR-p/MSI-L+MSS, EA MMR-d/MSI-H, EA MMR-p/MSI-L+MSS samples; 2.) MSI PCR-capillary electrophoresis (CE) based classification of MMR-d/MSI-H for the TCGA-COAD-READ vs. MMR-immunohistochemical (IHC) based classification of MMR-d; 3.) difference in the quality of the RNA extracted from frozen vs. FFPE tissues, 4.) differences in normalization for RNA-sequence vs. RT-qPCR measurements of mRNA expression, 5.) differences in correlations between self-identification of African ancestry and genomic estimates of African/European ancestry admixture. In the US the average genomic based estimate of African ancestry admixture is 73% in the self-identified African ancestry population (42), however the variation in African ancestry admixture compared to a reference Nigerian population can range from 30% to close to 100% (43). The sizes of the four ancestry MMR/MSI status groups were very unbalanced in the TCGA-COAD-READ group compared to the independent set of FFPE samples. With only 9 AA MMR-d/MSI-H samples in the TCGA-COAD-READ group, sampling bias particularly with respect to genomic estimates of African/European ancestry admixture could be the basis for discordant results between the TCGA-COAD-READ and the independent set of FFPE samples assembled from three medical centers. Because concordance between MMR-IHC and MSI PCR-CE has been reported to be 98% (44), it is unlikely that using two separate methods for classifying MMR-d/MSI-H explains the discordant results between the TCGA-COAD-READ and the independent FFPE set of tissues. The quality of the RNA recovered from FFPE samples is poor (RIN ~2) compared to frozen tissue (RIN >6) and typically exhibits higher Ct values in RT-qPCR assays compared to parallel frozen samples (45). It has been shown that while RT-qPCR and RNA-sequence results correlate, the correlation is surprisingly modest with r ~0.6 (45). For RNA-sequence data normalization is conducted using multiple genes. In contrast, RT-qPCR results are normalized against a single reference gene. For this reason, we selected Taqman primer probe sets for two reference genes that had been previously vetted for RT-qPCR analysis of COAD/READ RNA (27). To compare RNA-sequencing with RT-qPCR and to identify additional AA vs. EA DEGs, we are submitting this independent FFPE RNA sample set for parallel RNA-sequencing enriched by exome capture (46) and plan to continue to increase the size of the independent FFPE set of samples.
In summary, this study did not detect a significant ancestry effect on CXCL10 expression across MMR status but confirmed that CXCL10 mRNA expression is higher in MMR-d/MSI-H than MMR-p/MSI-L+MSS COAD/READ. Disentangling the effect of African ancestry from other co-variables such as MMR/MSI status requires increasing representation of minority samples across MMR/MSI status, genomic based estimation of ancestry admixture and rigorous collection of potential confounding metadata variables for all samples.
Data availability statement
The original contributions presented in the study are included in the article/Supplementary Material. Further inquiries can be directed to the corresponding author.
Ethics statement
The studies involving humans were approved by Stony Brook Institutional Review Board. The studies were conducted in accordance with the local legislation and institutional requirements. The human samples used in this study were acquired from a by- product of routine care or industry. Written informed consent for participation was not required from the participants or the participants’ legal guardians/next of kin in accordance with the national legislation and institutional requirements.
Author contributions
DJ: Methodology, Writing – review & editing, Investigation, Formal analysis, Writing – original draft, Data curation. AF: Formal analysis, Writing – review & editing, Methodology, Investigation, Validation. RF: Methodology, Investigation, Validation, Writing – review & editing, Formal analysis. DS: Formal analysis, Validation, Writing – review & editing, Investigation, Methodology. JL: Project administration, Writing – review & editing, Methodology, Supervision, Data curation, Formal analysis. JC: Project administration, Writing – review & editing, Data curation. EL: Funding acquisition, Conceptualization, Project administration, Supervision, Writing – original draft, Writing – review & editing, Data curation, Investigation. YL: Investigation, Formal analysis, Writing – review & editing, Methodology. JY: Writing – review & editing, Methodology, Supervision, Formal analysis. QY: Data curation, Writing – review & editing. SA: Data curation, Writing – review & editing. OO: Data curation, Supervision, Writing – review & editing, Resources. BT: Data curation, Writing – review & editing, Resources. NS: Writing – review & editing, Investigation. BC: Writing – review & editing, Supervision, Funding acquisition. AG: Writing – review & editing, Supervision, Funding acquisition.
Funding
The author(s) declare financial support was received for the research and/or publication of this article. Funding for this project was supported in part by NCI R03CA283359-01A1 (A.G., PI) and an institutional American Cancer Society award (A.G., PI). D.F.J. was supported by administrative diversity supplements to R01GM145700 and R01GM134307, (PI B.C.).
Acknowledgments
We acknowledge the Biostatistics Shared Resource at the Stony Brook Cancer Center for providing statistical consultation, and the Stony Brook Cancer Center Tissue Analytics Shared Resource Henry Ford Translational and Clinical Research Center Biorepository for providing de-identified COAD FFPR samples and clinical metadata. We acknowledge Richard Kew, PhD Director of the Stony Brook Cancer Center Biobank and Maksim Agaranov MD Chief of Pathology at NYCH+H/KCH for serving as honest brokers in order to deidentify the COAD/READ FFPE samples at SBUH and NYCH+H/KHC respectively. We thank Dr. Agnieszka Bialkowska and Dr. Vincent Yang in the Division of Gastroenterology at the Renaissance School of Medicine at Stony Brook University for many helpful discussions. We thank Dr. Jela Bandovic in the Department of Pathology at the Renaissance School of Medicine at Stony Brook University for serving as a pathologist on this project and for their invaluable assistance in facilitating sample acquisition.
Conflict of interest
AG reports a National Cancer Institute grant R03CA283359 and a pilot grant from Institutional Research Grant 21-143-01-IRG from the American Cancer Society, and BC reports administrative diversity supplement R01GM14570003S1 and an administrative diversity supplement to R01 GM134307, during the conduct of this study. NS reports a National Cancer Institute grant R00CA263154.
The remaining authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
The author(s) declared that they were an editorial board member of Frontiers, at the time of submission. This had no impact on the peer review process and the final decision.
Generative AI statement
The author(s) declare that no Generative AI was used in the creation of this manuscript.
Any alternative text (alt text) provided alongside figures in this article has been generated by Frontiers with the support of artificial intelligence and reasonable efforts have been made to ensure accuracy, including review by the authors wherever possible. If you identify any issues, please contact us.
Publisher’s note
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
Supplementary material
The Supplementary Material for this article can be found online at: https://www.frontiersin.org/articles/10.3389/fgstr.2025.1638438/full#supplementary-material
Supplementary Figure 1 | Spearman correlation between CXCL10 log2TPM values and CIBERSORT estimate of T-cell abundance in the TCGA-COAD-READ RNA-sequence dataset.
Supplementary Figure 2 | Scatter plot of CXCL10 log2TPM values in (A) AA CMS1, CMS2, CMS3, CMS4 and No Labels groups; and (B) EA CMS1, CMS2, CMS3, CMS4 and No Labels groups.
Abbreviations
COAD, colon adenocarcinoma; READ, rectal adenocarcinoma; AA, African ancestry; EA, European ancestry; MMR, mismatch repair; MSI, microsatellite instability; TCGA, The Cancer Genome Atlas, c-GAS/STING, cyclic GMP-AMP synthase - stimulator of interferon genes; CXCL10, C-X-C motif chemokine 10; FFPE, formalin fixed paraffin embedded; NYCH+H, New York City Health+Hospitals; KCH, Kings County Hospital; MANTIS, Microsatellite Analysis for Normal Tumor InStability; DEGs, differentially expressed genes; RT-qPCR, reverse transcriptase-quantitative polymerase chain reaction; CE, capillary electrophoresis; IHC, immunohistochemical.
References
1. Siegel RL, Giaquinto AN, and Jemal A. Cancer statistics, 2024. CA Cancer J Clin. (2024) 74:12–49. doi: 10.3322/caac.21820
2. Carethers JM and Doubeni CA. Causes of socioeconomic disparities in colorectal cancer and intervention framework and strategies. Gastroenterology. (2020) 158:354–67. doi: 10.1053/j.gastro.2019.10.029
3. Li Y, Pang X, Cui Z, Zhou Y, Mao F, Lin Y, et al. Genetic factors associated with cancer racial disparity - an integrative study across twenty-one cancer types. Mol Oncol. (2020) 14:2775–86. doi: 10.1002/1878-0261.12799
4. Curran T, Sun Z, Gerry B, Findlay VJ, Wallace K, Li Z, et al. Differential immune signatures in the tumor microenvironment are associated with colon cancer racial disparities. Cancer Med. (2021) 10:1805–14. doi: 10.1002/cam4.3753
5. Myer PA, Kim H, Blümel AM, Finnegan E, Kel A, Thompson TV, et al. Master transcription regulators and transcription factors regulate immune-associated differences between patients of African and European ancestry with colorectal cancer. Gastro Hep Adv. (2022) 1:328–41. doi: 10.1016/j.gastha.2022.01.004
6. El Moheb M, Shen C, Kim S, Putman K, Zhang H, Ruff SM, et al. Stage-specific tumoral gene expression profiles of black and white patients with colon cancer. Ann Surg Oncol. (2025) 32:736–49. doi: 10.1245/s10434-024-16550-9
7. Paredes J, Zabaleta J, Garai J, Ji P, Imtiaz S, Spagnardi M, et al. Immune-related gene expression and cytokine secretion is reduced among African American colon cancer patients. Front Oncol. (2020) 10:1498. doi: 10.3389/fonc.2020.01498
8. Malik SA, Zhu C, Li J, LaComb JF, Denoya PI, Kravets I, et al. Impact of preoperative antibiotics and other variables on integrated microbiome-host transcriptomic data generated from colorectal cancer resections. World J Gastroenterol. (2021) 27:1465–82. doi: 10.3748/wjg.v27.i14.1465
9. Haskins IN, Wang BD, Bernot JP, Cauley E, Horvath A, Marks JH, et al. Genomics of Black American colon cancer disparities: An RNA sequencing (RNA-Seq) study from an academic, tertiary referral center. Surgery. (2021) 170:1160–7. doi: 10.1016/j.surg.2021.03.031
10. Yamada HY, Xu C, Jones KL, O’Neill PH, Venkateshwar M, Chiliveru S, et al. Molecular disparities in colorectal cancers of White Americans, Alabama African Americans, and Oklahoma American Indians. NPJ Precis Oncol. (2023) 7:79. doi: 10.1038/s41698-023-00433-5
11. Cancer Genome Atlas Network. Comprehensive molecular characterization of human colon and rectal cancer. Nature. (2012) 487:330–7. doi: 10.1038/nature11252
12. André T, Cohen R, and Salem ME. Immune checkpoint blockade therapy in patients with colorectal cancer harboring microsatellite instability/mismatch repair deficiency in 2022. Am Soc Clin Oncol Educ Book. (2022) 42:1–9. doi: 10.1200/EDBK_349557
13. Boissière-Michot F, Lazennec G, Frugier H, Jarlier M, Roca L, Duffour J, et al. Characterization of an adaptive immune response in microsatellite-instable colorectal cancer. Oncoimmunology. (2014) 3:e29256. doi: 10.4161/onci.29256
14. Mowat C, Mosley SR, Namdar A, Schiller D, and Baker K. Anti-tumor immunity in mismatch repair-deficient colorectal cancers requires type I IFN-driven CCL5 and CXCL10. J Exp Med. (2021) 218:e20210108. doi: 10.1084/jem.20210108
15. Kaneta A, Nakajima S, Okayama H, Matsumoto T, Saito K, Kikuchi T, et al. Role of the cGAS-STING pathway in regulating the tumor-immune microenvironment in dMMR/MSI colorectal cancer. Cancer Immunol Immunother. (2022) 71:2765–76. doi: 10.1007/s00262-022-03200-w
16. Joseph DF. (2022). Deciphering molecular and cellular differences between black and white colorectal cancers through in-depth transcriptomic analyses (abstract A010, in: 15th AACR Conference on Cancer Health Disparities, Philadelphia, PA. Available online at: https://www.aacr.org/meeting/15th-aacr-conference-on-the-science-of-cancer-health-disparities-in-racial-ethnic-minorities-and-the-medically-underserved/abstracts/(Accessed September 19, 2025)
17. Myer PA, Lee JK, Madison RW, Pradhan K, Newberg JY, Isasi CR, et al. The genomics of colorectal cancer in populations with African and European ancestry. Cancer Discov. (2022) 12:1282–93. doi: 10.1158/2159-8290.CD-21-0813
18. Gutierrez C, Ogino S, Meyerhardt JA, and Iorgulescu JB. The prevalence and prognosis of microsatellite instability-high/mismatch repair-deficient colorectal adenocarcinomas in the United States. JCO Precis Oncol. (2023) 7:e2200179. doi: 10.1200/PO.22.00179
19. Colaprico A, Silva TC, Olsen C, Garofano L, Cava C, Garolini D, et al. TCGAbiolinks: an R/Bioconductor package for integrative analysis of TCGA data. Nucleic Acids Res. (2016) 44:e71. doi: 10.1093/nar/gkv1507
20. Liu Y, Sethi NS, Hinoue T, Schneider BG, Cherniack AD, Sanchez-Vega F, et al. Comparative molecular analysis of gastrointestinal adenocarcinomas. Cancer Cell. (2018) 33:721–735.e8. doi: 10.1016/j.ccell.2018.03.010
21. Kautto EA, Bonneville R, Miya J, Yu L, Krook MA, Reeser JW, et al. Performance evaluation for rapid detection of pan-cancer microsatellite instability with MANTIS. Oncotarget. (2017) 8:7452–63. doi: 10.18632/oncotarget.13918
22. Robinson MD, McCarthy DJ, and Smyth GK. edgeR: a Bioconductor package for differential expression analysis of digital gene expression data. Bioinformatics. (2010) 26:139–40. doi: 10.1093/bioinformatics/btp616
23. Li Y, Ge X, Peng F, Li W, and Li JJ. Exaggerated false positives by popular differential expression methods when analyzing human population samples. Genome Biol. (2022) 23:79. doi: 10.1186/s13059-022-02648-4
24. Guinney J, Dienstmann R, Wang X, de Reyniès A, Schlicker A, Soneson C, et al. The consensus molecular subtypes of colorectal cancer. Nat Med. (2015) 21:1350–6. doi: 10.1038/nm.3967
25. Chen B, Khodadoust MS, Liu CL, Newman AM, and Alizadeh AA. Profiling tumor infiltrating immune cells with CIBERSORT. Methods Mol Biol. (2018) 1711:243–59. doi: 10.1007/978-1-4939-7493-1_12
26. Fong C, Joseph D, Stanley S, Zhu Y, Zhu W, Grossman E, et al. Symptomatic colorectal cancer is associated with stage IV diagnosis in two disparate populations. Cureus. (2022) 14:e28691. doi: 10.7759/cureus.28691
27. Xu L, Luo H, Wang R, Wu WW, Phue JN, Shen RF, et al. Novel reference genes in colorectal cancer identify a distinct subset of high stage tumors and their associated histologically normal colonic tissues. BMC Med Genet. (2019) 20:138. doi: 10.1186/s12881-019-0867-y
28. PASS 2024 Power Analysis and Sample Size Software. Kaysville, Utah, USA: NCSS, LLC (2024). Available online at: ncss.com/software/pass(Accessed September 19, 2025)
29. Li L, Kanemitsu K, Ohnishi K, Yamada R, Yano H, Fujiwara Y, et al. CXCL10 expression in human colorectal cancer tissue and its correlation with serum levels of CXCL10. Cancer Genomics Proteom. (2024) 21:54–64. doi: 10.21873/cgp.20429
30. Pelka K, Hofree M, Chen JH, Sarkizova S, Pirl JD, Jorgji V, et al. Spatially organized multicellular immune hubs in human colorectal cancer. Cell. (2021) 184:4734–52. doi: 10.1016/j.cell.2021.08.003
31. Weigert A, Strack E, Snodgrass RG, and Brüne B. mPGES-1 and ALOX5/-15 in tumor-associated macrophages. Cancer Metastasis Rev. (2018) 37:317–34. doi: 10.1007/s10555-018-9731-3
32. Liu X, Yan G, Xu B, Yu H, An Y, and Sun M. Evaluating the role of IDO1 macrophages in immunotherapy using scRNA-seq and bulk-seq in colorectal cancer. Front Immunol. (2022) 13:1006501. doi: 10.3389/fimmu.2022.1006501
33. Graff EC, Fang H, Wanders D, and Judd RL. Anti-inflammatory effects of the hydroxycarboxylic acid receptor 2. Metabolism. (2016) 65:102–13. doi: 10.1016/j.metabol.2015.10.001
34. Dong Q, Zhang S, Zhang H, Sun J, Lu J, Wang G, et al. MARCO is a potential prognostic and immunotherapy biomarker. Int Immunopharmacol. (2023) 16:109783. doi: 10.1016/j.intimp.2023.109783
35. Boland CR and Goel A. Microsatellite instability in colorectal cancer. Gastroenterology. (2010) 138:2073–87. doi: 10.1053/j.gastro.2009.12.064
36. Tokunaga R, Zhang W, Naseem M, Puccini A, Berger MD, Soni S, et al. CXCL9, CXCL10, CXCL11/CXCR3 axis for immune activation - A target for novel cancer therapy. Cancer Treat Rev. (2018) 63:40–7. doi: 10.1016/j.ctrv.2017.11.007
37. Kistner L, Doll D, Holtorf A, Nitsche U, and Janssen KP. Interferon-inducible CXC-chemokines are crucial immune modulators and survival predictors in colorectal cancer. Oncotarget. (2017) 8:89998–90012. doi: 10.18632/oncotarget.21286
38. Song W, Yin H, Han C, Mao Q, Tang J, Ji Z, et al. The role of CXCL10 in prognosis of patients with colon cancer and tumor microenvironment remodeling. Med (Baltimore). (2021) 100:e27224. doi: 10.1097/MD.0000000000027224
39. Rhead B, Hein DM, Pouliot Y, Guinney J, de la Vega FM, and Sanford NN. Association of genetic ancestry with molecular tumor profiles in colorectal cancer. Genome Med. (2024) 16:99. doi: 10.1186/s13073-024-01373-w
40. Greene MW, Abraham PT, Kuhlers PC, Lipke EA, Heslin MJ, Wijaya ST, et al. Consensus molecular subtype differences linking colon adenocarcinoma and obesity revealed by a cohort transcriptomic analysis. PloS One. (2022) 17:e0268436. doi: 10.1371/journal.pone.0268436
41. Lofton H, Ard JD, Hunt RR, and Knight MG. Obesity among African American people in the United States: A review. Obes (Silver Spring). (2023) 31:306–15. doi: 10.1002/oby.23640
42. Bryc K, Durand EY, Macpherson JM, Reich D, and Mountain JL. The genetic ancestry of African Americans, Latinos, and European Americans across the United States. Am J Hum Genet. (2015) 96:37–53. doi: 10.1016/j.ajhg.2014.11.010
43. Mathias RA, Taub MA, Gignoux CR, Fu W, Musharoff S, O’Connor TD, et al. A continuum of admixture in the Western Hemisphere revealed by the African Diaspora genome. Nat Commun. (2016) 7:12522. doi: 10.1038/ncomms12522
44. Ye M, Ru G, Yuan H, Qian L, He X, and Li S. Concordance between microsatellite instability and mismatch repair protein expression in colorectal cancer and their clinicopathological characteristics: a retrospective analysis of 502 cases. Front Oncol. (2023) 13:1178772. doi: 10.3389/fonc.2023.1178772
45. Greytak SR, Engel KB, Bass BP, and Moore HM. Accuracy of molecular data generated with FFPE biospecimens: lessons from the literature. Cancer Res. (2015) 75:1541–7. doi: 10.1158/0008-5472.CAN-14-2378
Keywords: colorectal neoplasm, DNA mismatch repair, African continental ancestry group, European continental ancestry group, gene expression
Citation: Joseph DF, Fu A, Flores RE, Sharma DV, LaComb JF, Clark JM, Li E, Liao Y, Yang J, Yu Q, Adams S, Ogunwobi OO, Theisen B, Steele NG, Chen B and Guillaume A (2025) The effect of African ancestry and mismatch-repair enzyme deficiency/microsatellite instability-high on colorectal adenocarcinoma immune gene expression. Front. Gastroenterol. 4:1638438. doi: 10.3389/fgstr.2025.1638438
Received: 30 May 2025; Accepted: 11 September 2025;
Published: 03 October 2025.
Edited by:
Federica Rubbino, Humanitas Research Hospital, ItalyReviewed by:
Fabio Grizzi, Humanitas Research Hospital, ItalyXinna Du, Jiangsu Vocational College of Medicine, China
Copyright © 2025 Joseph, Fu, Flores, Sharma, LaComb, Clark, Li, Liao, Yang, Yu, Adams, Ogunwobi, Theisen, Steele, Chen and Guillaume. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Alexandra Guillaume, QWxleGFuZHJhLkd1aWxsYXVtZUBzdG9ueWJyb29rbWVkaWNpbmUuZWR1
 Dimitri F. Joseph
Dimitri F. Joseph Andrew Fu2
Andrew Fu2 Julie M. Clark
Julie M. Clark Ellen Li
Ellen Li Yunhan Liao
Yunhan Liao Seidu Adams
Seidu Adams Olorunseun O. Ogunwobi
Olorunseun O. Ogunwobi Bin Chen
Bin Chen Alexandra Guillaume
Alexandra Guillaume