- 1Division of Morphology, Anatomy and Physiology, Department of Medical Basics, Specialty and Education, Showa Medical University, Graduate School of Nursing and Rehabilitation Sciences, Yokohama, Japan
- 2Division of Neurological Science, Department of Rehabilitation, Showa Medical University, Graduate School of Nursing and Rehabilitation Sciences, Yokohama, Japan
- 3Division of Occupational Therapy and Mental Health, Department of Rehabilitation, Showa Medical University, Graduate School of Nursing and Rehabilitation Sciences, Yokohama, Japan
- 4Division of Cardiopulmonary Rehabilitation Science, Department of Rehabilitation, Showa Medical University, Graduate School of Nursing and Rehabilitation Sciences, Yokohama, Japan
- 5Division of Healthcare Management, Department of Medical Basics, Specialty and Education, Showa Medical University, Graduate School of Nursing and Rehabilitation Sciences, Yokohama, Japan
- 6Division of Clinical Engineering, Department of Medical Technology, Showa Medical University, Graduate School of Nursing and Rehabilitation Sciences, Yokohama, Japan
- 7Division of Clinical Radiology, Department of Medical Technology, Showa Medical University, Graduate School of Nursing and Rehabilitation Sciences, Yokohama, Japan
- 8Division of Health Science Education, Department of Medical Basics, Specialty and Education, Showa Medical University, Graduate School of Nursing and Rehabilitation Sciences, Yokohama, Japan
Introduction: Infection prevention and control education has traditionally been conducted in a lecture-based manner, and simulation-based educational strategies have become increasingly prevalent in the field of medical education in recent years. This systematic review aimed to compare the effectiveness of the simulation-based and traditional strategies of infection prevention and control education and to show the differences between these educational approaches. Furthermore, we identified the characteristics of simulation-based strategies for infection prevention and control education.
Method: Systematic reviews and meta-analyses were performed according to the Preferred Reporting Items for Systematic Reviews and Meta-Analyses guidelines. A systematic literature search was conducted using the CENTRAL, MEDLINE, and Scopus databases for articles published between January 1990 and September 2022. This study focused on students enrolled in medical and health professional courses. As such, healthcare professionals already working in clinical settings, as well as kindergarten and elementary school students were excluded from the study. The quality of the included studies and the risk of bias in each study were assessed. A total of 254 articles were identified; 21 underwent secondary screening. Ultimately, 10 articles were selected for the final review.
Results: Educational strategies between simulation- and lecture-based education showed improvements in knowledge acquisition. There was no significant difference in the rate of improvement between the two educational strategies. The characteristics of simulation-based educational strategies included confidence in skill performance, decision-making and problem-solving skills, emotional aspects related to infectious diseases (such as fear, empathy, self-reflection, and integration of complex information), and student satisfaction.
Conclusion: This systematic review suggests that simulation-based education is effective in developing students’ skills and attitudes, while traditional lecture-based methods are more suited for reinforcing students’ knowledge. Therefore, it is essential to choose educational strategies based on specific learning objectives and outcomes.
Systematic review registration: This systematic review protocol was preregistered in the Open Science Framework: https://osf.io/uj623/.
1 Introduction
The coronavirus disease 2019 (COVID-19) pandemic has caused fear of infection. It has resulted in a renewed awareness of the importance of hand hygiene and washing worldwide. Hand hygiene is one of the most common methods for preventing disease transmission (1). In addition to hand hygiene, healthcare professionals wear personal protective equipment (PPE) to treat patients and protect themselves from disease transmission and infection. Unfortunately, during the COVID-19 pandemic, a large number of healthcare professionals became infected and died (2, 3). Under these circumstances, it has become more important than ever to perform appropriate actions based on infection prevention and control and have appropriate education about infection, not only for healthcare professionals but also for students enrolled in medical, nursing, physical therapy, occupational therapy, and other related courses.
Participants in literature reviews of studies focusing on infection prevention and control education are often healthcare professionals (4–8). One reason for the need for infection prevention and control education for healthcare professionals is the prevention or reduction of healthcare-associated infections (HAIs; e.g. catheter-associated bloodstream infections, catheter-associated urinary tract infections, surgical site infections, and ventilator-associated pneumonia) and nosocomial infections (5, 6, 9). Although several studies on infection prevention and control education have focused on students, to the best of our knowledge, no systematic review reports exist on the results of these educational studies regarding infection prevention and control education. One report surveyed medical, dental, nursing, physical therapy, and occupational therapy students regarding their knowledge of infection prevention and control and their infection prevention measures during the COVID-19 pandemic. The report found that although these students had a high level of knowledge about infection prevention and control, they did not have sufficient ability to practice infection prevention and control actions, such as donning and doffing PPE and hand hygiene procedures (10). This means that students must acquire practical skills and knowledge during their student years before they work in clinical environments. Therefore, it is essential for the educational staff to develop evidence-based infection prevention and control strategies.
Simulation education is an educational strategy used to develop students’ practical skills. Simulation can be described as a continuum ranging from low-fidelity simulation (partial task trainers) to screen-based computer simulators, virtual reality (VR), role-playing (standardized patients), and high-fidelity simulation (full-scale simulation) (11). Simulation-based education strategies develop medical, nursing, and physical therapy students’ knowledge retention, clinical thinking, practical skills, confidence, and satisfaction compared to traditional strategies (12–15). Therefore, various simulation-based educational strategies can be adapted according to specific learning outcomes as well as educational and student levels. These systematic reports have described educational practices that mimic various clinical situations. However, the future challenges and limitations of simulation-based education primarily revolve around two key issues: (i) the significant costs involved in acquiring and maintaining advanced simulation equipment, and (ii) the need for educators to have the skills necessary to effectively utilize these simulators. Additionally, there is a requirement for the establishment of objective evaluation methods within simulation education (16). Specifically regarding objective evaluation in point (ii), organizations like the World Health Organization (WHO) have provided guidelines on proper procedures for putting on and removing PPE, as well as on hand hygiene. This presents an opportunity for objective evaluation in the field of infection prevention and control education through the use of checklists and other assessment tools within simulation-based education. However, our search for simulation-based education focused on practical training for infection control revealed that such training is predominantly offered to healthcare professionals in hospitals, with limited reports on its implementation in student education (17). Education on infection prevention and control requires the development of practical skills and knowledge. To effectively acquire both practical skills and knowledge, it is necessary to establish a simulation education strategy for infection prevention and control.
1.1 Aims
Our goal is to develop an infection prevention and control education strategy grounded in scientific evidence. To achieve this, the purpose of this study—serving as the first step—is to propose a simulation-based infection prevention and control education strategy. This approach is expected to effectively integrate students’ knowledge, skills, and attitudes, using systematic reviews and meta-analyses. The research questions for our systematic review and meta-analysis were as follows:
• Is infection prevention and control education based on a simulation strategy more effective than traditional educational strategies for students enrolled in medical, nursing, rehabilitation, and other related courses?
• What enhances learning satisfaction and the effectiveness of infection prevention and control education for students enrolled in medical, nursing, rehabilitation, and other related courses?
2 Methods
This systematic review was preregistered in the Open Science Framework Registry.1 This study followed the Preferred Reporting Items for Systematic Reviews and Meta-Analyses (PRISMA) guidelines (18). Additionally, a systematic meta-analysis was performed based on our previous protocol (17).
2.1 Study design
This study design was a meta-review of systematic reviews of articles on simulation and traditional infection prevention and control education for medical and healthcare students. Our study focused on articles published from 1990 to 2022. In a systematic review by Cant, R. P., it was reported that simulation education for medical and nursing students has been employed since 1999 (11). This suggests that simulation education has been used to teach students since the 1990s, and therefore, we have defined our study period as beginning in 1990. Systematic reviews included randomized clinical trials, pre-post designs, comparisons of two focus groups, or qualitative studies.
2.2 Participants
The participants were undergraduate and graduate students enrolled in medical and health-related occupational courses (doctors, dentists, nurses, physical therapists, occupational therapists, pharmacists, and other medical-related fields).
2.3 Intervention
Infection prevention and control education using simulation-based learning and/or training.
2.4 Comparison
Infection education using traditional education methods.
2.5 Outcome
Critical thinking, skill performance, knowledge acquisition, decision-making and problem-solving skills, self-efficacy, clinical reasoning skills, self-confidence, communication skills, teamwork, improved clinical performance, leadership skills, and student satisfaction.
2.6 Search strategy
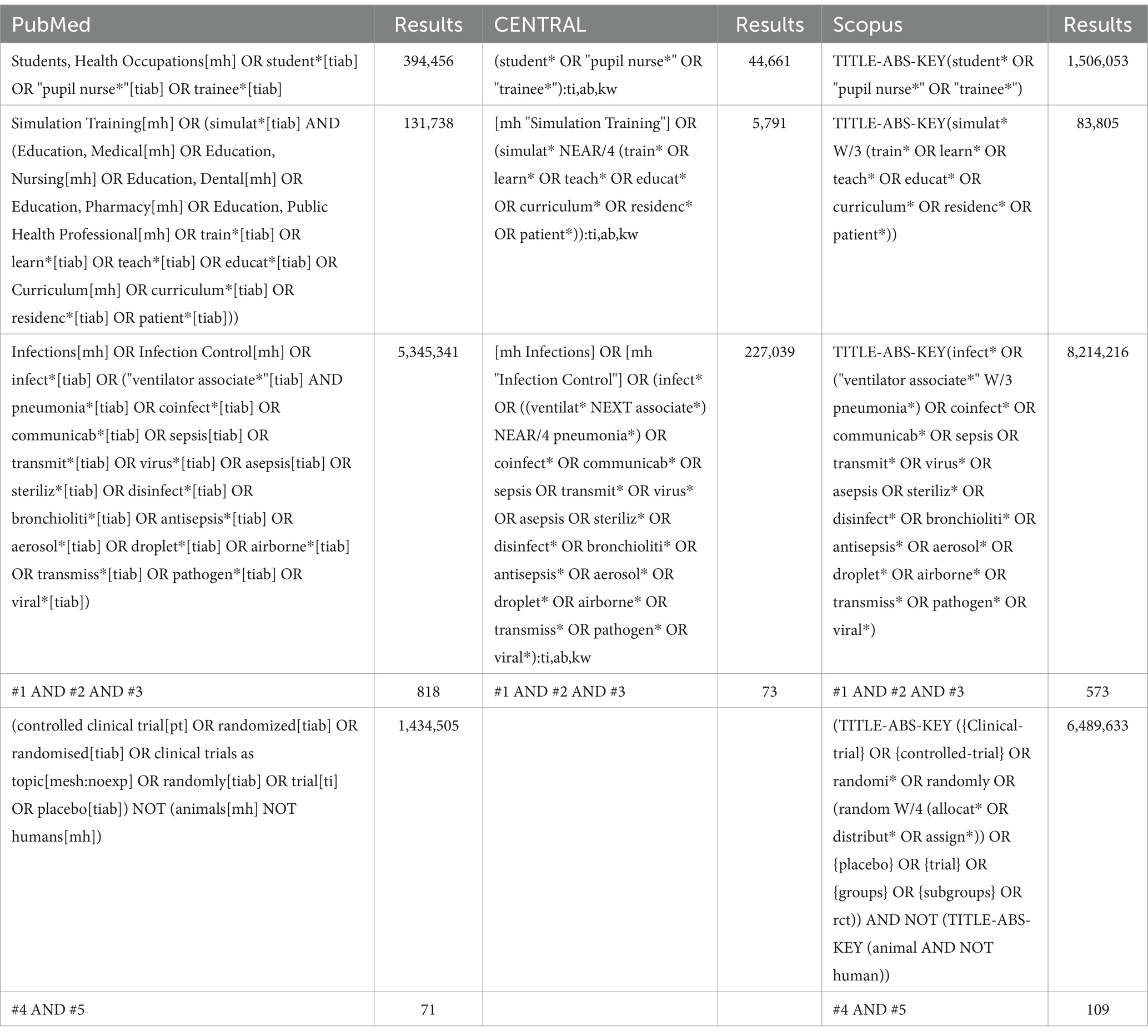
We conducted a search of the CENTRAL, MEDLINE, and Scopus databases, with the last search date set to January 13, 2023. Our approach involved the use of a combination of text keywords and Medical Subject Headings (MeSH) terms tailored to each database. The concepts we aimed to capture included Patients: students who want to become healthcare professionals, “students,” “health occupations,” and “pupil nurses”; Intervention: simulation-based infection prevention and control education, “simulation training,” “infection”; Comparison: Comparison with traditional infection control education, “randomized,” and “clinical trials.” The details are shown in Table 1. Readers can search for the relevant articles by copying and pasting each search term listed in Table 1 in each database.
2.7 Inclusion criteria
2.7.1 Types of studies
We included both controlled clinical trials and randomized controlled trials (RCTs) in this review. Furthermore, we supplemented these with observational studies (including cohort and case–control studies) to obtain practical reports.
2.7.2 Types of participants
The participants in the included studies comprised undergraduate and graduate students enrolled in medical and health-related occupational courses (medical doctors, dentists, nurses, physical therapists, occupational therapists, pharmacists, and other medical-related fields).
2.7.3 Types of outcome measures
The following outcome measures were considered when including the studies: critical thinking, skill performance, knowledge acquisition, decision-making and problem-solving skills, self-efficacy, clinical reasoning skills, self-confidence, communication skills, teamwork, improved clinical performance, leadership skills, and student satisfaction.
2.8 Exclusion criteria
This was a systematic review of simulation-based infection prevention and control education for students. Therefore, studies involving healthcare professionals, non-medical and healthcare-related occupational course students, non-university students (e.g., kindergarten and elementary school students), and the general public were excluded. Additionally, we included articles published between January 1990 and September 2022, and excluded those published outside of this time frame.
2.9 Data collection and analysis
2.9.1 Study selection
First, two investigators independently screened titles and abstracts using the text words and MeSH terms outlined previously in the initial literature search to determine whether articles potentially met the inclusion criteria. Articles that clearly did not meet the criteria were rejected. This double-blind study was conducted by two independent investigators using Rayyan software (19). In the primary screening phase, articles that did not match the review question were excluded based on an analysis of their titles and abstracts, and articles that could not be judged from their abstracts were retained. Next, the two reviewers independently reviewed the full texts of the remaining articles to determine their eligibility for review. In no case were the reviewers unable to extract all the required results for primary, secondary, and other outcomes from the included studies, and the authors were not contacted to explain the missing data in the studies. Disagreements at any stage were resolved through discussions between the two reviewers. If the reviewers failed to reach a consensus, a third reviewer was consulted for arbitration. The role of the third reviewer was to participate in discussions regarding any conflicts that arose. Before joining these discussions, the third reviewer independently reviewed the relevant articles. It is important to note that the third reviewer was not the final decision-maker. Instead, their role was to assist in reaching a consensus during the discussions.
2.9.2 Data extraction and management
The data extraction sheet was piloted among the reviewers before extraction to ensure that it was easy for the eight reviewers to use. Subsequently, data were independently extracted by two reviewers, recorded, and managed using standard Microsoft Excel data recording spreadsheets by eight reviewers. Data were extracted to obtain a complete record of methodology, study design, participants, interventions, outcome measures, and results. Maximal data extraction was planned to ensure that the findings were adequately followed without returning to the original dataset. The data to be extracted conformed to Cochrane recommendations.
2.9.3 Assessment of risk of bias
To assess the possible risk of bias (RoB) for each study, we evaluated and reported on the methodological RoB for the included studies on the following individual elements for RCTs: random sequence generation, allocation sequence concealment, blinding (participants, personnel), blinding (outcome assessment), completeness of outcome data, selective outcome reporting, similar baseline characteristics, and similar baseline outcome measurements. However, some non-randomized studies were reported. For these studies, we used the Risk of Bias in Non-Randomized Studies of Interventions (ROBINS-I), which aims to assess the RoB of estimates of the effectiveness or safety (benefit or harm) of interventions from studies that do not use randomization to allocate the intervention (20). In all cases, two reviewers independently assessed the RoB of the included studies, with any disagreements resolved through discussion or by consulting a third reviewer who was expected to be consulted previously for arbitration until a consensus was reached. We judged each item as high, low, with some concerns in RoB, and low, moderate, serious, critical, and no information in ROBINS-I, as mentioned in the criteria.
2.9.4 Data synthesis and statistical analysis
Because statistical pooling was not possible, the findings from the quantitative and qualitative papers were consolidated into a single Microsoft Excel dataset with the following content:
• Author
• Population
• Country
• Type of study
• Student
• Intervention
• Comparison
• Outcome
• Key results
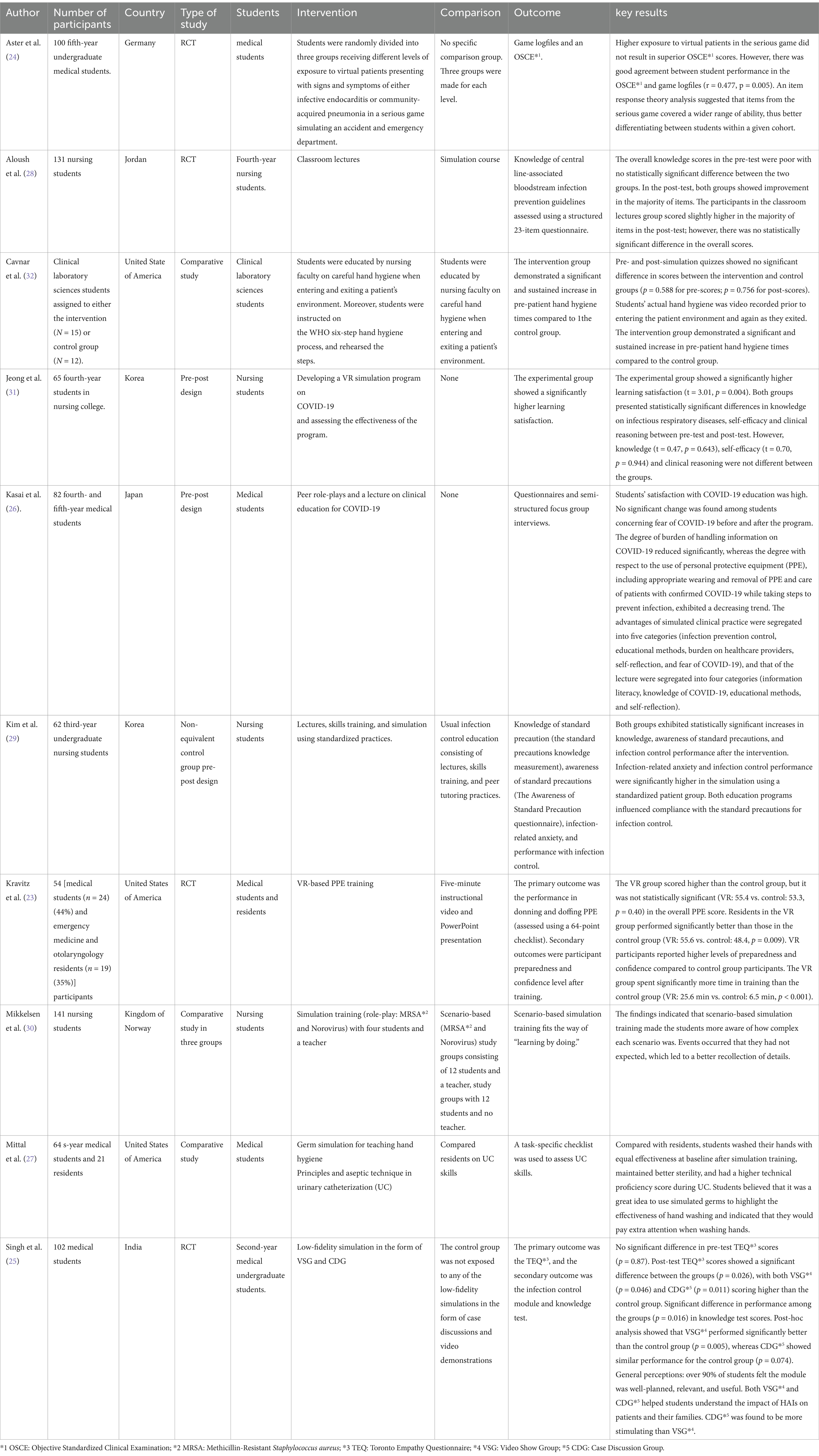
The diversity of the studies showed that a statistical meta-analysis was not feasible, so this review was presented using a narrative synthesis based on methodology. First, each investigator summarized the articles according to their theoretical perspective, using their individual knowledge and experience, and recorded this in an Excel sheet. This initial summary was done individually by each investigator. Next, the investigators collaborated to extract key themes relevant to the research questions from the appropriate papers and identified the content (21, 22).
3 Results
3.1 Characteristics of the study population (study selection)
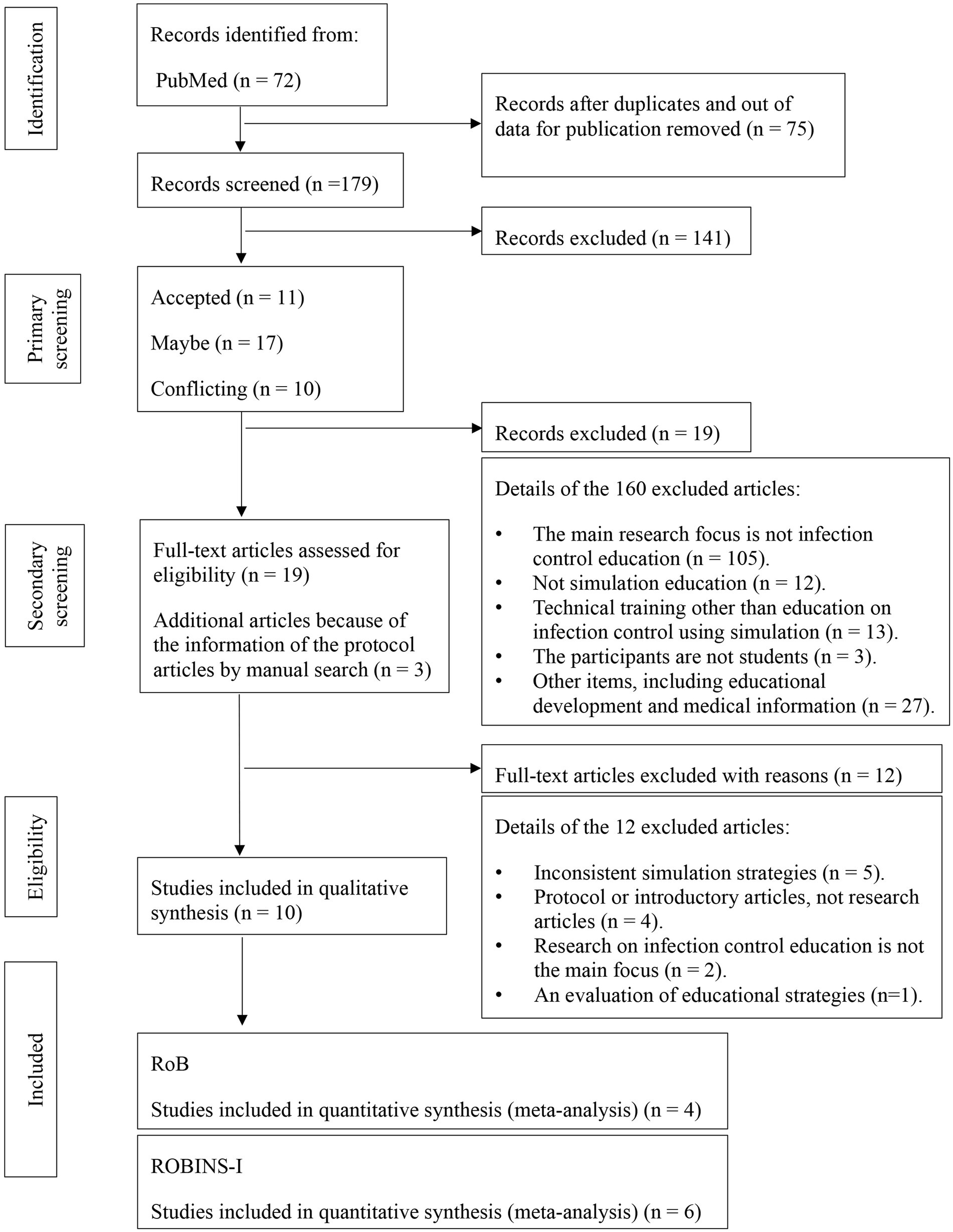
In total, 72, 73, and 109 articles were extracted from PubMed, CENTRAL, and Scopus, respectively. Out of these, 75 were duplicates and outdated publications; therefore, 179 were eligible for primary screening. Primary screening was assessed by title, keywords, and abstract, resulting in 11 acceptable, 17 maybe, and 10 conflicting articles, which were discussed among two investigators, and 19 articles were selected. During this process, three articles were added by manual search; thus, 21 articles in total were screened by a secondary process. As a result of the secondary screening, 10 articles were eligible for inclusion (Figure 1).
3.2 Methodological quality assessment of intervention studies
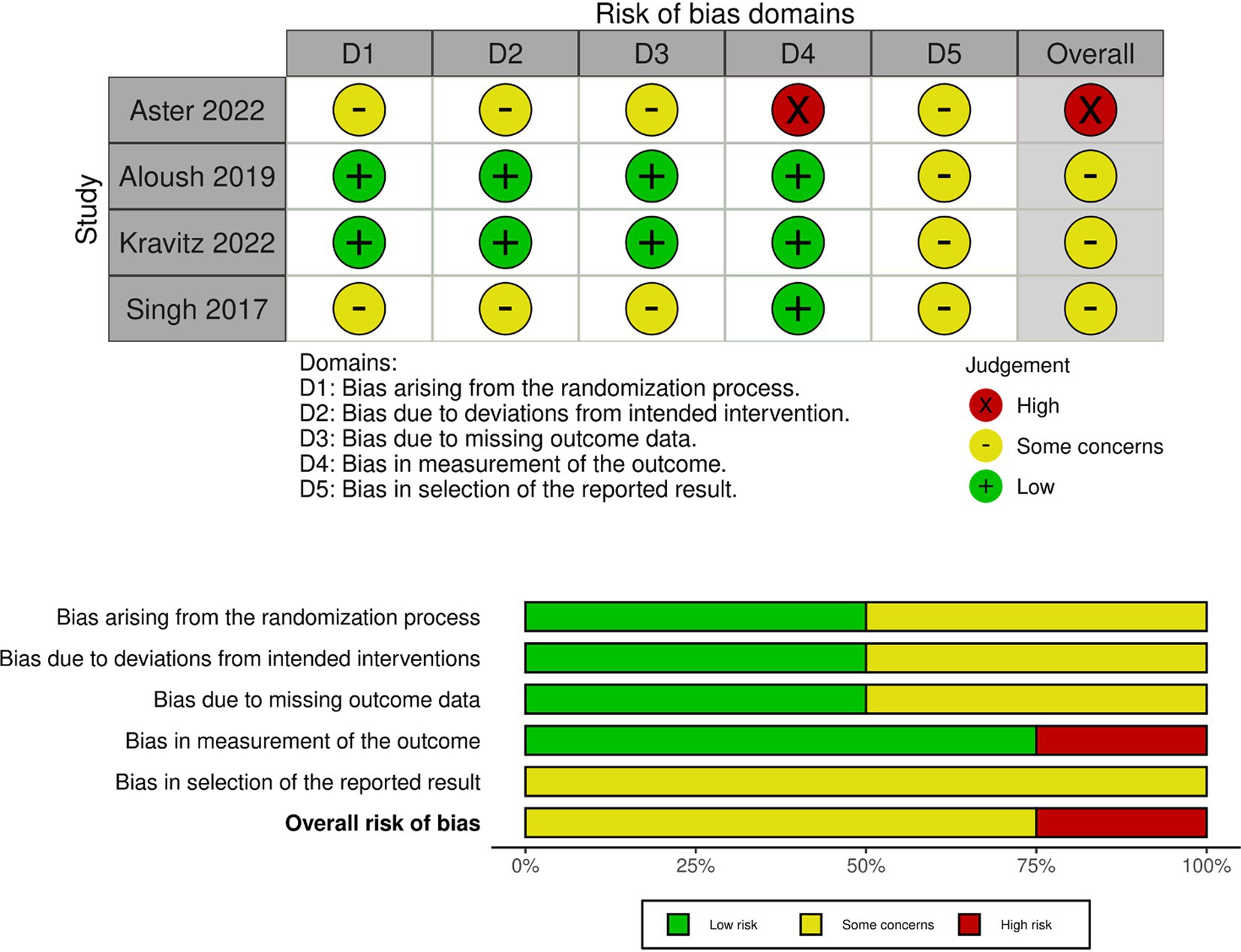
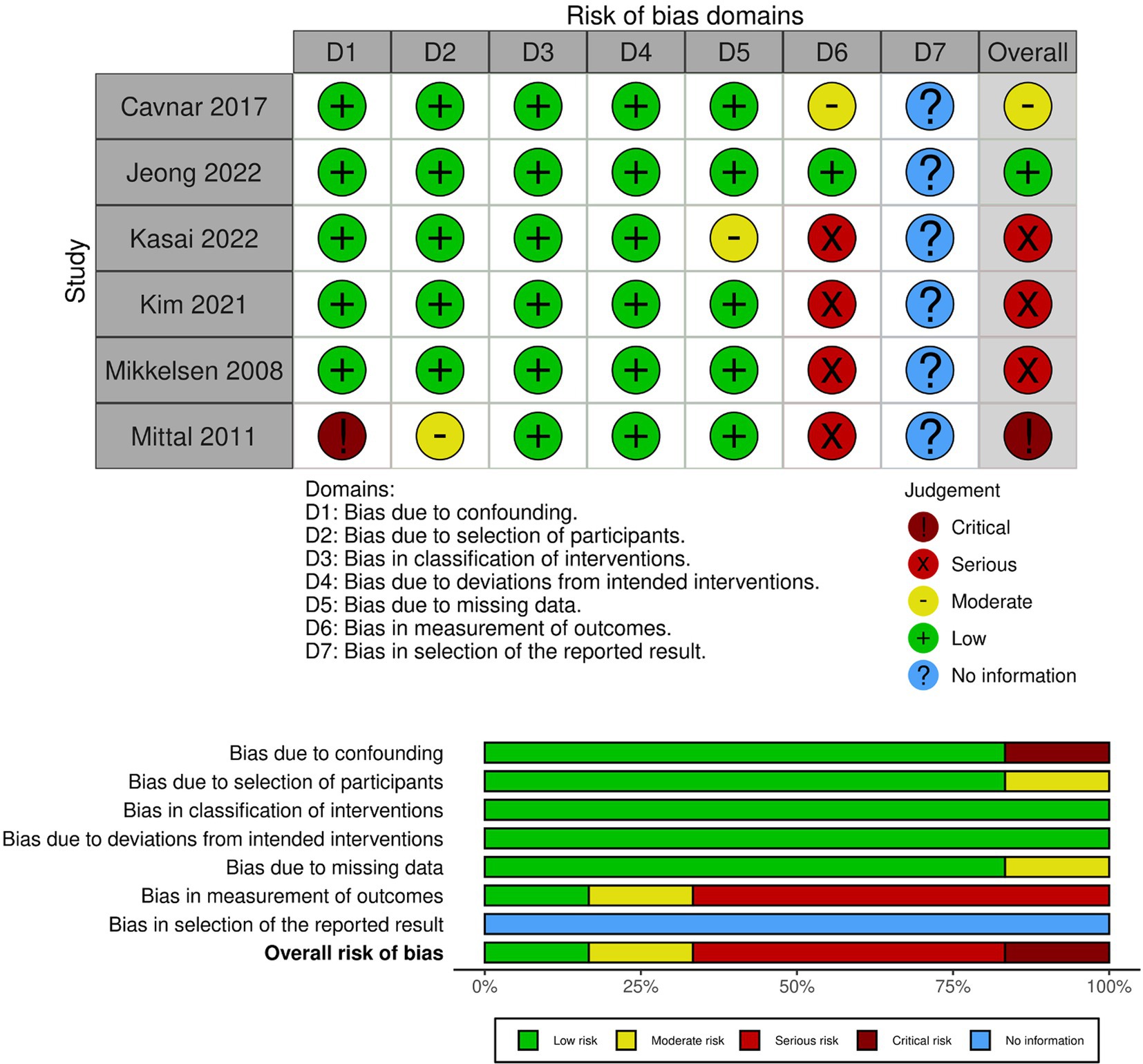
A study-level bias assessment was conducted for these articles. As four were RCT and six were non-RCT studies (pre-post or observational studies), the bias assessment was conducted using the RoB and ROBINS-I. In RoB, three out of four articles were rated as concerning, whereas the other resulted in a high risk (Figure 2 and Supplementary Figure 1). In ROBINS-I, one article was at low risk, one was at moderate risk, three were at serious risk, and one was at critical risk (Figure 3 and Supplementary Figure 2). These 10 articles showed the educational effectiveness of simulation-based infection prevention and control education for undergraduate and graduate students. A meta-analysis was not feasible in this study owing to substantial heterogeneity among the included studies in terms of study designs, interventions, and outcomes. Among the 10 studies included, four were RCTs, while the remaining six were non-RCTs, which included pre-post and observational studies. The methodological quality assessment indicated that three RCTs had “some concerns” regarding bias, while one had a “high risk” of bias. Among the six non-RCTs, three were classified as having a “serious risk,” and one was classified as having a “critical risk,” according to the ROBINS-I tool.
The simulation-based infection prevention and control education strategies varied significantly, encompassing not only those using low- and high-fidelity simulators but also VR, serious games, role-playing, and demonstrations as learning strategies. Additionally, the frequency, duration, and intensity of simulation training varied widely, contributing to the overall heterogeneity of the interventions.
Regarding outcome heterogeneity, a variety of assessment methods were employed across studies. For instance, one study utilized an objective structured clinical examination (OSCE) for technical assessment, while another applied a checklist based on Centers for Disease Control and Prevention guidelines or used its own developed assessment criteria. Interviews conducted revealed a diverse array of evaluation approaches. The combination of different study designs, the associated risk of bias, and varied outcomes further limited the feasibility of performing a meta-analysis.
3.3 Characteristics of research on infection prevention and control education using simulation for medical and healthcare students
Four studies conducted RCTs and six studies conducted non-RCTs, comparing simulation-based education before and after its implementation, or comparing it to traditional education. A total of 796 students participated in studies involving infection prevention and control education (Table 2).
Of the 10 articles in this review, five were aimed at medical students (23–27), four at nursing students (28–31), and one at clinical laboratory students (32). The definition of a simulation-based educational strategy varied across the literature: two studies used VR (23, 31), five studies used role-play or demonstrations (26, 27, 29, 30, 32), one study used low-fidelity simulators (25), one study used high-fidelity simulators (28), and one study used serious games (24).
Regarding infection prevention and control educational topics, four articles were related to the donning and doffing of PPE and hand hygiene (23, 29, 31, 32), three articles were related to HAIs (25, 27, 28), and three articles were related to the pathophysiology of infectious diseases (24, 26, 30).
To compare the educational effectiveness of simulation-based infection prevention/control education with traditional classroom lectures and viewing of video materials, knowledge tests, practical tests (such as the objective, standardized clinical examinations), and questionnaires were used as evaluation methods. However, the detailed content of these evaluation items depended on the individual, and there were no common evaluation items.
Although students’ knowledge test scores improved after both simulation and traditional education, most studies found no significant differences between these two educational strategies. The benefits of simulation education were confidence in skill performance (23, 27, 32), decision-making and problem-solving skills (25, 27, 28), emotional aspects related to infectious diseases (fear, empathy, self-reflection, integration of complex information) (25, 26, 29, 31), and student satisfaction with simulation-based infection prevention and control education (26, 31). A summary of this is presented in Table 3.
4 Discussion
This systematic review compared the educational effectiveness of the simulation-based traditional education strategies for infection prevention and control and showed the differences between these educational approaches. Furthermore, we identified the characteristics of simulation-based strategies for infection prevention and control education.
During the COVID-19 pandemic, nursing students reported feeling a strong desire to help others; however, they were conflicted by their lack of knowledge and skills related to infection prevention and control, as well as their own fear of infection (33, 34). Furthermore, reports on the knowledge and skills of nursing students regarding hand hygiene indicated that, although they have higher infection-related knowledge than general students, they have significantly less clinical experience than practicing nurses in clinical situations. This lack of experience increases the risk of infection in clinical practice (35). These reports highlight the deficiency in infection prevention and control education prior to clinical practice. Regarding students’ knowledge and behaviors related to infection control and prevention, several articles reported that medical students have low awareness of hand hygiene (36). Evaluations of hand hygiene knowledge among students in medical, dental, and nursing schools revealed that their knowledge level was low-to-moderate (37), and female students had a higher awareness of hand hygiene practices than male students (38). These reports reveal the current state of infection prevention and control knowledge and practical skills of the students. Hence, the importance of infection prevention and control education for students has been reaffirmed, and there is a recognized need to provide scientific information to educational staff on infection prevention and control educational strategies and their effectiveness. These aspects had been previously noted in the field of medical education, prior to the COVID-19 pandemic. However, the COVID-19 pandemic has led to the identification of more specific issues within medical education settings, such as those pertaining to infection prevention and control education, related to PPE (23, 26, 31). Personal protective equipment techniques are considered one of the most basic infection control education skills. However, this systematic review suggests that the COVID-19 pandemic has significantly increased the importance of ensuring that students acquire such PPE knowledge and skills. Additionally, simulation-based infection prevention and control education focused on awareness of the COVID-19 pandemic led to a decrease in anxiety in some students, while anxiety increased in others (26). Confronting the global fear of COVID-19 without the correct knowledge increases fear among students. A suggested method to alleviate this fear is the acquisition of accurate pathological knowledge alongside the necessary PPE accurate techniques (29, 39). These findings suggest that, through this systematic review, infection prevention and control education using simulation as an educational strategy may have been transformed by the COVID-19 pandemic into more specific learning content, such as pathological knowledge of COVID-19, and donning and doffing PPE, including the hand hygiene techniques, as a way to protect oneself when working with patients.
The WHO guidelines for infection prevention and control educational strategies for medical students suggest a combination of the following methods: (1) lectures and clinical placements, (2) online activities, (3) on-the-ward activities, (4) small group tutorial teaching, (5) problem-based learning, (6) simulation/skills laboratories, and (7) traditional tutorials.2 Among these educational strategies, we conducted a systematic review to compare traditional educational methods with simulation-based education, which has recently been recognized for its effectiveness. For undergraduate and graduate students enrolled in medical and healthcare-related occupational courses, simulation-based education has several benefits: (1) improved knowledge and skills, (2) a safe learning environment, (3) enhanced clinical judgment and decision-making, (4) increased self-confidence and satisfaction, (5) effective non-technical skills training, (6) reduced anxiety and increased confidence in technical skills, and (7) long-term retention (12, 40–42). However, simulation-based educational strategies face challenges such as high costs and resource intensiveness (requiring substantial resources, including dedicated space, equipment, and trained faculties) (42, 43).
The results of this systematic review indicate that the characteristics of simulation-based educational strategies included confidence in skill performance, decision-making and problem-solving skills, emotional aspects related to infectious diseases (such as fear, empathy, self-reflection, and integration of complex information), and student satisfaction. However, studies that utilized simulation education strategies also had their limitations. In strategies using VR, technical challenges in creating scenarios were noted (31). Furthermore, students participated only in brief or single-session VR scenarios, which resulted in limited interpretations of the evaluation outcomes concerning knowledge, skills, and attitudes (23, 31). In role-play strategies, several concerns have been raised, including the small number of participants and potential bias in participant recruitment (27, 29, 32). Additionally, there may be cultural bias present in the region where the study was conducted (26), and doubts regarding the generalizability of infection control education arising from research limited to a specific medical department (26). The simplicity of the infection control scenario also raises questions about whether the results can be applied to other infection control situations (29). The requirement for substantial human resources to conduct simulation education has also been emphasized (30). In educational research using low- and high-fidelity simulators, similar concerns have been noted, such as small sample sizes and potential cultural bias related to the study’s location. There is also a limitation in the focus solely on knowledge and skills, without a detailed analysis of the factors that enhance them (28). Additionally, the need for evaluation metrics that closely align with clinical practice has been highlighted. There is uncertainty about whether assessments conducted in simulation settings effectively translate to actual practice (25). In educational strategies using serious games, several issues have been identified, including participant drop-out, limited interpretation of results owing to the implementation being similar to VR in single sessions, and the need for more appropriate evaluation methods (24). It is essential to verify whether students are indeed capable of practicing their skills and demonstrating the appropriate attitudes, as questionnaire evaluations often rely on self-assessment (26).
To facilitate a comparison between traditional infection control education and the new educational strategy of simulation-based infection control education, we focused on articles published from 1990 to 2022. In our investigation, the earliest report on simulation-based infection control education was found to be from 2008. Regarding simulation education across all medical education, not just focused on infection prevention and control, McGaghie et al. have reported that various aspects of simulation education—including (i) fidelity, (ii) proficiency-based learning and outcome measurement, (iii) instructor training, (iv) curriculum development, and (v) the overall growth and maturation of instructor training—have significantly advanced over time (44). The strategy of simulation-based education helps students develop their skills and knowledge while gaining experience in a relatively safe and controlled environment. Simulation is recognized for providing a safe and relevant learning experience by operating “ex vivo,” meaning it does not involve real patients. However, a challenge remains in determining whether students who have undergone simulation education and acquired skills, knowledge, and attitudes can effectively apply these competencies in clinical practice (45). Simulation education is considered an effective method owing to the secure learning environment it creates. However, it can sometimes lead to a disconnect from real clinical settings, which may create a sense of deception for students (46). Therefore, educators must present clear learning objectives when conducting simulation education and provide thorough explanations for each scenario (44). It is also essential for educational research to investigate whether students’ knowledge, skills, and attitudes gained through simulation education are effectively utilized in clinical situations. Additionally, to implement simulation education successfully, educators may need to participate in seminars, such as Technician Training Programs, to learn about effective simulation strategies (47). Participation in such programs involves financial considerations, and the costs associated with acquiring and maintaining high-fidelity simulators can far exceed these expenses. To maximize educational effectiveness within limited resources, it is crucial to identify the specific benefits of simulation education and develop programs that enable students who have experienced simulation to fully realize their capabilities in clinical practice (48).
This systematic review indicated that traditional educational strategies, such as lectures, remain important in the acquisition of knowledge related to infection prevention and control. The integration of knowledge, skills, and attitudes is essential in both medical and general education (49). This suggests that, in infection prevention and control education, it is crucial to determine educational strategies based on specific educational objectives and learning outcomes. In light of these considerations, the necessity for standardization of education regarding the essential knowledge, as well as skills of donning and doffing PPE and hand hygiene has been supported (50). We propose two key initiatives to establish standardization in this area of education. Our primary challenge is the development of standardized evaluation methods. While various assessment techniques were used in this study to assess educational effectiveness, the significant variability in these evaluation methods prevented us from synthesizing and validating the findings across the individual studies. As a specific approach to simulation education in infection control, we recommend utilizing checklists based on WHO guidelines for hand hygiene3 and PPE.4 Additionally, we suggest developing knowledge assessment tests for students that are derived from these guidelines for hand hygiene and/or PPE checklists. Standardizing educational intervention protocols and adopting consistent outcome measurement criteria will allow for the implementation of high-quality RCTs. This method will facilitate future meta-analyses, improve researcher comparability, and contribute to identifying superior educational methods. Moreover, we propose conducting mid- and long-term outcome evaluations to determine whether students who have experienced simulation education can apply what they learned in clinical situations afterward. While many studies on simulation education focus on short-term outcomes, we, as educators, expect students to integrate their knowledge, skills, and attitudes into their clinical practice. Therefore, it is essential to assess changes in students’ behavior not only in the short term but also in the mid- and long term. Based on the results of this systematic review, we believe that effectively combining simulation with traditional lectures as educational strategies for infection prevention and control education will lead to the development of enhanced educational approaches.
4.1 Limitations
The evaluation of educational outcomes varied across studies; even when quantified, the assessed evaluation scores or items differed, and qualitative aspects such as interviews with students were also included. Consequently, integration between studies is not feasible, and future research will need to establish standardized metrics to indicate the effectiveness of infection prevention and control education. Additionally, it is important to consider the potential publication bias in educational research, as many studies have yielded positive results (51).
5 Conclusion
This systematic review aimed to establish a foundation for infection prevention and control educational strategies by comparing the effectiveness of simulation-based strategies and traditional educational strategies, specifically for undergraduate and graduate students enrolled in medical and healthcare-related occupational courses. Although both simulation and traditional education improve student knowledge, most studies found no significant differences between these two teaching strategies. The benefits of simulation education include confidence in skill performance, decision-making and problem-solving skills, emotional aspects related to infectious diseases, and student satisfaction with simulation-based infection prevention and control education. Infection prevention and control education require students to integrate knowledge, skills, and attitudes to develop practical competencies. This includes the use of simulation-based education, which excels in the acquisition of skills and attitudes alongside traditional lectures, which are effective for reinforcing knowledge.
Data availability statement
Data that support the findings of this study are available from the corresponding author upon request.
Author contributions
AY: Conceptualization, Data curation, Formal analysis, Funding acquisition, Investigation, Methodology, Project administration, Validation, Visualization, Writing – original draft, Writing – review & editing. HO: Data curation, Formal analysis, Investigation, Methodology, Validation, Writing – review & editing. KA: Data curation, Formal analysis, Investigation, Methodology, Validation, Writing – review & editing. NT: Conceptualization, Data curation, Formal analysis, Investigation, Methodology, Validation, Writing – original draft, Writing – review & editing. ST: Investigation, Validation, Writing – review & editing. KK: Investigation, Validation, Writing – review & editing. SN: Investigation, Validation, Writing – review & editing. MO: Investigation, Validation, Writing – review & editing. ME: Funding acquisition, Conceptualization, Project administration, Supervision, Writing – review & editing.
Funding
The author(s) declare that financial support was received for the research and/or publication of this article. This study was supported by the School of Nursing and Rehabilitation Sciences, Showa University Research Fund (grant number: 2023No.3: AY) and by Grants-in-Aid for Scientifi Research (grant number: 24K13609, AY and ME) from the Japan Society for the Promotion of Science.
Acknowledgments
We would like to thank Tomoko Morimasa and Asae Ito (librarians, Showa University) for their advice on creating the MeSH terms. We thank Marina Fukao (staff at Showa University) for administrative and clerical support. Finally, we would like to thank Editage (www.editage.com) for the English language editing.
Conflict of interest
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
Generative AI statement
The author(s) declare that no Gen AI was used in the creation of this manuscript.
Publisher’s note
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
Supplementary material
The Supplementary material for this article can be found online at: https://www.frontiersin.org/articles/10.3389/fmed.2025.1529557/full#supplementary-material
Abbreviations
PRISMA, Preferred Reporting Items for Systematic Reviews and Meta-Analyses; HAI, Healthcare-associated infections; PPE, Personal protective equipment; RCT, Randomized controlled trials; RoB, Risk of bias; ROBINS-I, Risk of Bias in Non-Randomized Studies of Interventions; VR, Virtual reality.
Footnotes
2. ^https://www.who.int/publications/i/item/9789241598316
3. ^https://www.who.int/publications/i/item/9789241597906
4. ^https://www.who.int/teams/health-product-policy-and-standards/assistive-and-medical-technology/medical-devices/ppe
References
1. Huang, GK, Stewardson, AJ, and Grayson, ML. Back to basics: hand hygiene and isolation. Curr Opin Infect Dis. (2014) 27:379–89. doi: 10.1097/QCO.0000000000000080
2. Headquarters, W. (2021). The impact of COVID-19 on health and care workers: a closer look at deaths. World Health Organization. Available online at: https://iris.who.int/handle/10665/345300 (Accessed 1/11/2024).
3. Vera-Alanis, Y, Aranda-Sanchez, D, Cano-Verdugo, G, Gonzalez-Angulo, P, Rueda-Sanchez, CB, and Rojas-Martinez, A. Nursing staff mortality during the Covid-19 pandemic, scoping review. SAGE Open Nurs. (2022) 8:23779608221119130. doi: 10.1177/23779608221119130
4. Ward, DJ. The role of education in the prevention and control of infection: a review of the literature. Nurse Educ Today. (2011) 31:9–17. doi: 10.1016/j.nedt.2010.03.007
5. Zingg, W, Holmes, A, Dettenkofer, M, Goetting, T, Secci, F, Clack, L, et al. Hospital organisation, management, and structure for prevention of health-care-associated infection: a systematic review and expert consensus. Lancet Infect Dis. (2015) 15:212–24. doi: 10.1016/S1473-3099(14)70854-0
6. Mauger, B, Marbella, A, Pines, E, Chopra, R, Black, ER, and Aronson, N. Implementing quality improvement strategies to reduce healthcare-associated infections: a systematic review. Am J Infect Control. (2014) 42:S274–83. doi: 10.1016/j.ajic.2014.05.031
7. Martos-Cabrera, MB, Mota-Romero, E, Martos-Garcia, R, Gomez-Urquiza, JL, Suleiman-Martos, N, Albendin-Garcia, L, et al. Hand hygiene teaching strategies among nursing staff: a systematic review. Int J Environ Res Public Health. (2019) 16:3039. doi: 10.3390/ijerph16173039
8. Chow, A, Arah, OA, Chan, SP, Poh, BF, Krishnan, P, Ng, WK, et al. Alcohol handrubbing and chlorhexidine handwashing protocols for routine hospital practice: a randomized clinical trial of protocol efficacy and time effectiveness. Am J Infect Control. (2012) 40:800–5. doi: 10.1016/j.ajic.2011.10.005
9. Moralejo, D, El Dib, R, Prata, RA, Barretti, P, and Correa, I. Improving adherence to standard precautions for the control of health care-associated infections. Cochrane Database Syst Rev. (2018) 2018:CD010768. doi: 10.1002/14651858.CD010768.pub2
10. Modi, PD, Nair, G, Uppe, A, Modi, J, Tuppekar, B, Gharpure, AS, et al. COVID-19 awareness among healthcare students and professionals in Mumbai metropolitan region: a questionnaire-based survey. Cureus. (2020) 12:e7514. doi: 10.7759/cureus.7514
11. Cant, RP, and Cooper, SJ. Simulation-based learning in nurse education: systematic review. J Adv Nurs. (2010) 66:3–15. doi: 10.1111/j.1365-2648.2009.05240.x
12. Kim, J, Park, JH, and Shin, S. Effectiveness of simulation-based nursing education depending on fidelity: a meta-analysis. BMC Med Educ. (2016) 16:152. doi: 10.1186/s12909-016-0672-7
13. Mori, B, Carnahan, H, and Herold, J. Use of simulation learning experiences in physical therapy entry-to-practice curricula: a systematic review. Physiother Can. (2015) 67:194–202. doi: 10.3138/ptc.2014-40E
14. McGaghie, WC, Issenberg, SB, Cohen, ER, Barsuk, JH, and Wayne, DB. Does simulation-based medical education with deliberate practice yield better results than traditional clinical education? A meta-analytic comparative review of the evidence. Acad Med. (2011) 86:706–11. doi: 10.1097/ACM.0b013e318217e119
15. Shinnick, MA, and Woo, MA. The effect of human patient simulation on critical thinking and its predictors in prelicensure nursing students. Nurse Educ Today. (2013) 33:1062–7. doi: 10.1016/j.nedt.2012.04.004
16. Elendu, C, Amaechi, DC, Okatta, AU, Amaechi, EC, Elendu, TC, Ezeh, CP, et al. The impact of simulation-based training in medical education: a review. Medicine (Baltimore). (2024) 103:e38813. doi: 10.1097/MD.0000000000038813
17. Yoshikawa, A, Tashiro, N, Ohtsuka, H, Aoki, K, Togo, S, Komaba, K, et al. Protocol for educational programs on infection prevention/control for medical and healthcare student: a systematic review and meta-analysis. PLoS One. (2022) 17:e0276851. doi: 10.1371/journal.pone.0276851
18. Page, MJ, McKenzie, JE, Bossuyt, PM, Boutron, I, Hoffmann, TC, Mulrow, CD, et al. The PRISMA 2020 statement: an updated guideline for reporting systematic reviews. Syst Rev. (2021) 10:89. doi: 10.1186/s13643-021-01626-4
19. Ouzzani, M, Hammady, H, Fedorowicz, Z, and Elmagarmid, A. Rayyan-a web and mobile app for systematic reviews. Syst Rev. (2016) 5:210. doi: 10.1186/s13643-016-0384-4
20. Sterne, JA, Hernan, MA, Reeves, BC, Savovic, J, Berkman, ND, Viswanathan, M, et al. ROBINS-I: a tool for assessing risk of bias in non-randomised studies of interventions. BMJ. (2016) 355:i4919. doi: 10.1136/bmj.i4919
21. Sukhera, J. Narrative reviews: flexible, rigorous, and practical. J Grad Med Educ. (2022) 14:414–7. doi: 10.4300/JGME-D-22-00480.1
22. Ferrari, R. Writing narrative style literature reviews. Med Writing. (2015) 24:230–5. doi: 10.1179/2047480615Z.000000000329
23. Kravitz, MB, Dadario, NB, Arif, A, Bellido, S, Arif, A, Ahmed, O, et al. The comparative effectiveness of virtual reality versus E-module on the training of donning and doffing personal protective equipment: a randomized, simulation-based educational study. Cureus. (2022) 14:e23655. doi: 10.7759/cureus.23655
24. Aster, A, Scheithauer, S, Middeke, AC, Zegota, S, Clauberg, S, Artelt, T, et al. Use of a serious game to teach infectious disease Management in Medical School: effectiveness and transfer to a clinical examination. Front Med (Lausanne). (2022) 9:863764. doi: 10.3389/fmed.2022.863764
25. Singh, SP, Modi, CM, Patel, CP, and Pathak, AG. Low-fidelity simulation to enhance understanding of infection control among undergraduate medical students. Natl Med J India. (2017) 30:215–8. doi: 10.4103/0970-258X.218677
26. Kasai, H, Saito, G, Ito, S, Kuriyama, A, Kawame, C, Shikino, K, et al. COVID-19 infection control education for medical students undergoing clinical clerkship: a mixed-method approach. BMC Med Educ. (2022) 22:453. doi: 10.1186/s12909-022-03525-1
27. Mittal, MK, Morris, JB, and Kelz, RR. Germ simulation: a novel approach for raising medical students awareness toward asepsis. Simul Healthc. (2011) 6:65–70. doi: 10.1097/SIH.0b013e318206953a
28. Aloush, SM. Lecture-based education versus simulation in educating student nurses about central line-associated bloodstream infection-prevention guidelines. J Vasc Nurs. (2019) 37:125–31. doi: 10.1016/j.jvn.2018.11.006
29. Kim, E, Kim, SS, and Kim, S. Effects of infection control education for nursing students using standardized patients vs. peer role-play. Int J Environ Res Public Health. (2020) 18:18. doi: 10.3390/ijerph18010107
30. Mikkelsen, J, Reime, MH, and Harris, AK. Nursing students' learning of managing cross-infections--scenario-based simulation training versus study groups. Nurse Educ Today. (2008) 28:664–71. doi: 10.1016/j.nedt.2007.11.003
31. Jeong, Y, Lee, H, and Han, JW. Development and evaluation of virtual reality simulation education based on coronavirus disease 2019 scenario for nursing students: a pilot study. Nurs Open. (2022) 9:1066–76. doi: 10.1002/nop2.1145
32. Katie Cavnar JVDLaLH-B. Promoting patient safety through Interprofessional education simulation. Clin Lab Sci. (2017) 30:228–32. doi: 10.29074/ascls.30.4.228
33. Swift, A, Banks, L, Baleswaran, A, Cooke, N, Little, C, McGrath, L, et al. COVID-19 and student nurses: a view from England. J Clin Nurs. (2020) 29:3111–4. doi: 10.1111/jocn.15298
34. Thornton, TM, Decker, SA, and Roe, EA. Fear of contagion among nursing students in the era of COVID-19. J Nurs Educ. (2021) 60:404–7. doi: 10.3928/01484834-20210616-09
35. Chang, SO, Sohng, KY, Kim, K, Won, J, Chaung, SK, and Choi, MJ. How nursing students learn infection control education through undergraduate nursing programs: a phenomenographic research study. BMC Nurs. (2023) 22:297. doi: 10.1186/s12912-023-01465-9
36. Ergin, A, Bostanci, M, Onal, O, Bozkurt, AI, and Ergin, N. Evaluation of students' social hand washing knowledge, practices, and skills in a university setting. Cent Eur J Public Health. (2011) 19:222–7. doi: 10.21101/cejph.a3664
37. Thakker, VS, and Jadhav, PR. Knowledge of hand hygiene in undergraduate medical, dental, and nursing students: a cross-sectional survey. J Family Med Prim Care. (2015) 4:582–6. doi: 10.4103/2249-4863.174298
38. Alwan, N, Safwan, J, Kerek, R, and Ghach, W. Hand hygiene during the spread of COVID-19: a cross-sectional study of awareness and practices among academic institutions in Lebanon. Front Public Health. (2023) 11:1256433. doi: 10.3389/fpubh.2023.1256433
39. Norton, EJ, Georgiou, I, Fung, A, Nazari, A, Bandyopadhyay, S, and Saunders, KEA. Personal protective equipment and infection prevention and control: a national survey of UK medical students and interim foundation doctors during the COVID-19 pandemic. J Public Health (Oxf). (2021) 43:67–75. doi: 10.1093/pubmed/fdaa187
40. Labrague, LJ, McEnroe-Petitte, DM, Bowling, AM, Nwafor, CE, and Tsaras, K. High-fidelity simulation and nursing students' anxiety and self-confidence: a systematic review. Nurs Forum. (2019) 54:358–68. doi: 10.1111/nuf.12337
41. Jallad, ST, and Işık, B. The effectiveness of virtual reality simulation as learning strategy in the acquisition of medical skills in nursing education: a systematic review. Ir J Med Sci. (2022) 191:1407–26. doi: 10.1007/s11845-021-02695-z
42. Alharbi, A, Nurfianti, A, Mullen, RF, McClure, JD, and Miller, WH. The effectiveness of simulation-based learning (SBL) on students’ knowledge and skills in nursing programs: a systematic review. BMC Med Educ. (2024) 24:1099. doi: 10.1186/s12909-024-06080-z
43. Tong, LK, Li, YY, Au, ML, Ng, WI, Wang, SC, Liu, Y, et al. The effects of simulation-based education on undergraduate nursing students' competences: a multicenter randomized controlled trial. BMC Nurs. (2024) 23:400. doi: 10.1186/s12912-024-02069-7
44. McGaghie, WC, Issenberg, SB, Petrusa, ER, and Scalese, RJ. A critical review of simulation-based medical education research: 2003-2009. Med Educ. (2010) 44:50–63. doi: 10.1111/j.1365-2923.2009.03547.x
45. Cook, DA, Hatala, R, Brydges, R, Zendejas, B, Szostek, JH, Wang, AT, et al. Technology-enhanced simulation for health professions education: a systematic review and meta-analysis. JAMA. (2011) 306:978–88. doi: 10.1001/jama.2011.1234
46. Alinier, G, and Oriot, D. Simulation-based education: deceiving learners with good intent. Adv Simul (Lond). (2022) 7:8. doi: 10.1186/s41077-022-00206-3
47. Nestel, D, Bearman, M, Brooks, P, Campher, D, Freeman, K, Greenhill, J, et al. A national training program for simulation educators and technicians: evaluation strategy and outcomes. BMC Med Educ. (2016) 16:25. doi: 10.1186/s12909-016-0548-x
48. Maloney, S, and Haines, T. Issues of cost-benefit and cost-effectiveness for simulation in health professions education. Adv Simul (Lond). (2016) 1:13. doi: 10.1186/s41077-016-0020-3
49. Baartman, LKJ, and de Bruijn, E. Integrating knowledge, skills and attitudes: Conceptualising learning processes towards vocational competence. Educ Res Rev. (2011) 6:125–34. doi: 10.1016/j.edurev.2011.03.001
50. Barratt, R, and Gilbert, GL. Education and training in infection prevention and control: exploring support for national standards. Infect Dis Health. (2021) 26:139–44. doi: 10.1016/j.idh.2020.12.002
Keywords: infection prevention, infection control, infection education, simulation education, students, systematic review
Citation: Yoshikawa A, Ohtsuka H, Aoki K, Tashiro N, Togo S, Komaba K, Nogawa S, Osawa M and Enokida M (2025) Simulation-based infection prevention and control training for medical and healthcare students: a systematic review. Front. Med. 12:1529557. doi: 10.3389/fmed.2025.1529557
Edited by:
Preman Rajalingam, Mohammed Bin Rashid University of Medicine and Health Sciences, United Arab EmiratesReviewed by:
Yi Kong, Nanjing Drum Tower Hospital, ChinaHailemelekot Bekele Kebede, Epidemiology (Mph), Ethiopia
Copyright © 2025 Yoshikawa, Ohtsuka, Aoki, Tashiro, Togo, Komaba, Nogawa, Osawa and Enokida. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Akira Yoshikawa, eW9zaGktYWtpQG1lZC5zaG93YS11LmFjLmpw
 Akira Yoshikawa
Akira Yoshikawa Hiroyuki Ohtsuka2
Hiroyuki Ohtsuka2 Keiichiro Aoki
Keiichiro Aoki