- 1Science and Education Section, Wenshang County People's Hospital, Jining, Shandong, China
- 2English Research Group, Wenshang County No. 1 Middle School, Jining, Shandong, China
- 3Medical Department, Wenshang County People's Hospital, Jining, Shandong, China
- 4Wenshang County People's Hospital, Jining, Shandong, China
- 5Urinary Surgery, Wenshang County People's Hospital, Jining, Shandong, China
- 6Department of Surgery, Wenshang County People's Hospital, Jining, Shandong, China
Background: Teaching rounds are a fundamental component of medical education, offering essential clinical learning opportunities for students while ensuring high-quality care for patients. Despite their importance, the psychological and emotional experiences of participants—attending physicians, interns, and patients—during these rounds remain underexplored. This study addresses this gap by examining the impact of patient presence on the learning environment, focusing on three key themes: psychological comfort and anxiety, cognitive load management, and emotional engagement and detachment.
Material and methods: A design-based research approach was employed, conducted in a surgical ward affiliated with a medical college. The study involved 40 participants, including attending physicians, interns, and patients. Data were collected through 40 in-depth interviews, with analysis focusing on the experiences and perspectives of all parties involved.
Results: The findings reveal that transparency in communication is crucial for building trust but can also induce anxiety among both trainees and physicians due to the scrutiny of their actions. Managing cognitive load was identified as a significant challenge, particularly for interns who must balance learning with patient interaction. Emotional engagement is vital for effective patient care but must be carefully balanced with professional detachment to maintain clinical objectivity.
Conclusion: This study contributes to the understanding of the complex dynamics in teaching rounds, emphasizing the need for strategies that balance educational goals with patient-centered care. The insights gained offer valuable guidance for enhancing the learning environment in medical education.
1 Introduction
Teaching rounds are fundamental to medical education, providing students essential clinical learning experiences while ensuring the delivery of high-quality patient care (1). However, the intricate dynamics within teaching rounds, involving attending physicians, interns, and patients, introduce challenges that can affect both educational outcomes and patient care. Despite the critical role of teaching rounds in medical training, the psychological and emotional experiences of participants during these sessions remain insufficiently studied.
Recent studies underscore the significance of understanding these experiences, especially in terms of psychological comfort, cognitive load, and emotional engagement (2). Psychological comfort, for instance, is closely linked to transparency in communication (3). Transparency builds trust between patients and healthcare providers and alleviates trainee anxiety in unpredictable clinical environments (4). However, this transparency can also increase anxiety for both trainees and attending physicians, who may feel scrutinized by patients and colleagues (5).
Cognitive load management is another critical factor that influences the effectiveness of teaching rounds (6). Attending physicians must balance the dual responsibilities of providing clinically relevant information and ensuring that this information is comprehensible to both trainees and patients. The cognitive demands on trainees are significant, as they are required to absorb complex information, engage with patients, and simultaneously learn from the experience. Patients, on the other hand, may struggle with understanding medical jargon, which can lead to feelings of alienation and confusion (7).
Emotional engagement and detachment add further complexity to the teaching dynamic. While empathetic engagement is essential for establishing rapport with patients and improving the quality of care, it must be carefully balanced with professional detachment to maintain objective decision-making (8). Both trainees and attending physicians must manage this delicate balance, as excessive emotional involvement can compromise clinical judgment, whereas excessive detachment may be perceived by patients as a lack of care.
In this study, we aim to explore how the presence of patients during teaching rounds affects the learning environment and to gather insights from all participants—interns, attending physicians, and patients. We focus on three main themes: psychological comfort and anxiety, cognitive load management, and emotional engagement and detachment. Understanding these themes is crucial for developing strategies that enhance the learning environment in medical education, ensuring it is conducive to both effective learning and patient care.
This study was conducted in a surgical ward of a hospital affiliated with a medical college, where patients were actively involved in all teaching and learning activities. The interventions included having interns present the entire case to the attending physician in the presence of the patient, followed by case discussions also conducted in the patient’s presence. The findings from this study are anticipated to inform the ongoing refinement of teaching strategies that emphasize both educational effectiveness and patient-centered care.
2 Methods
2.1 Subjects
The study involved patients, learners (interns), attending physicians, and researchers. The research team held regular meetings to refine research questions, develop interview guides, and discuss and analyze the findings. Interviews were conducted by three researchers with distinct backgrounds: A lead physician (15 years clinical/teaching), an academic researcher (Medical Education), a Patient Representative (Hospital Patient Advisory Board). All interviewers received practical training in conducting semi-structured interviews. After each interview was recorded, the relevant survey results were incorporated into the interview guide to enrich the subsequent data collection process.
2.2 Experimental design
A design-based research method used to guide our research. Interview guides are planned, tested and refined. The question for the study was to explore how the presence of patients affects the learning environment and to collect evaluations from all participants - learners (interns), attending physicians, and most importantly, patients. We applied the conceptual framework of agency, the degree to which people feel free or constrained in a given situation, as a framework for our design and conduct of our documentation. Among them, the feelings expressed by the patients about the scene, as well as the feedback of the medical activities of the interns and attending physicians, were recorded.
2.3 Settings
The study was conducted in a surgical ward at Wenshang County People’s Hospital, Shandong, China – a tertiary teaching hospital affiliated with Jining Medical College. This setting reflects hierarchical medical education norms common in East Asia, where attending physicians hold significant authority. Patient inclusion protocols emphasized cultural considerations (e.g., family involvement in consent, deference to physicians). These contextual factors may limit direct transferability to decentralized Western systems but offer insights for similar hierarchical settings.
2.4 Intervention
The time span from the intervention to the interviews is as follows:
Patient interview: typically scheduled 1–2 days after the clinical teaching session to ensure the patient’s memory of the intervention remains fresh.
Intern interview: usually conducted 1–2 days after the patient interview, allowing the intern time to reflect on their performance and experience during the intervention.
Attending physician interview: generally arranged 1–2 days after the intern interview, providing the attending physician with an opportunity to assess the overall effectiveness of the intervention and the intern’s performance.
Overall, the time span from the initiation of the intervention to the completion of all interviews typically ranges from 1 to 2 weeks. This scheduling is designed to balance the timeliness and accuracy of feedback from all parties involved.
The attending physician conducts one to two patient instructional rounds each week. The study’s interventions involved having interns present the entire case to the attending physician in the presence of the patient. Additionally, all subsequent case discussions were conducted in front of the patient. Typically, the majority of discussions related to the case presentation occur in the classroom. Following the clinical instruction, we conducted interviews with each participant using interview guides specifically tailored for patients, interns, and attending physicians. The post-intervention interviews were carried out in three stages: (1) an interview with the patient after the clinical teaching session, (2) an interview with the interns, and (3) an interview with the attending physician.
2.5 Participants
In our study, the sample size was determined based on the principle of data saturation. We conducted 40 in-depth interviews, and during the analysis, we observed that as the interviews progressed, the emergence of new information and themes gradually diminished, eventually reaching data saturation. We also considered the sample size ranges recommended in similar studies and, taking into account practical resources and time constraints, determined the appropriate sample size. Additionally, we ensured participant diversity to enhance the representativeness and comprehensiveness of the research findings.
The study was approved by the hospital’s ethics committee. The informed consent was obtained from all subjects. Appropriate ethical aspects have been followed in all phases of the study, according to the Helsinki Declaration. All participants were informed about the study and its purposes; voluntary participation; data confidentiality, use, and processing; data protection statement; and contact details. The participants did not receive any rewards in return of participation. We recruited three types of participants: attending physicians, learners (interns), and patients along with their families, with a total sample size of 40 participants. The attending physicians included 4 senior physicians with extensive clinical experience. The group of learners consisted of 18 clinical medicine interns. The patient group comprised 18 randomly selected inpatients from the ward. Prior to the study, patients were informed that they could opt out at any time without impacting their clinical treatment to minimize any burden on them. Neither the attending physicians, the interns, nor the patients were made aware of the post-intervention interviews.
Patients for teaching rounds are selected based on the following criteria:
Educational objectives:
Diverse conditions: select patients with a range of conditions to provide learners with exposure to different diseases and management strategies.
Relevant learning points: choose cases that align with the session’s learning objectives, such as specific diagnostic challenges or treatment approaches.
Clinical skills: consider cases that facilitate the demonstration of essential clinical skills, decision-making processes, or critical thinking.
2.5.1 Patient conditions
Stability: ensure the patient’s condition is relatively stable to allow teaching without compromising patient safety.
Complexity: include patients with complex or interesting cases that offer educational value, while avoiding overly complicated cases that may overwhelm learners.
2.5.2 Patient consent
Informed Consent: always obtain explicit consent from patients or their guardians for participation in teaching rounds. Clearly explain the purpose, the individuals who will be present, and how their information will be used.
Voluntariness: emphasize that participation is voluntary and that they can withdraw consent at any time without affecting their care.
Privacy assurance: assure patients that their medical information will remain confidential and explain the measures taken to protect their privacy.
2.5.3 Respect for patients
Comfort level: assess and respect the patient’s comfort with having multiple people involved in their care and discussing their condition in front of others.
Special considerations: be sensitive to issues such as terminal illness or severe emotional distress, and select cases accordingly.
2.5.4 Logistical factors
Availability: ensure the patient will be available for the teaching session and is in an environment conducive to effective teaching, such as a ward room that can accommodate a group.
Timing: schedule rounds when the patient is likely to be most alert and receptive.
2.5.5 Coordination with team
Consultation: collaborate with the patient’s primary care team to confirm that the patient’s condition is suitable for teaching and seek their input on case selection.
Feedback: incorporate feedback from previous sessions to continuously refine and improve the selection process.
2.5.6 Ethical considerations
Patient autonomy: always prioritize the patient’s autonomy and ensure they are making an informed choice about their participation. Obtaining patient consent involved a detailed informed consent process where we provided patients with clear and comprehensive information about the teaching rounds, including its purpose, procedures, and potential impacts. We used simple language and provided written consent forms for patients to sign. Prior to the rounds, we held preparation meetings with patients to explain their role, address any concerns, and ensure their comfort. We also ensured strict confidentiality of patient information throughout the process. Ethical approval was obtained, and we have a feedback mechanism in place for patients to raise any issues or questions after their participation.
Professionalism: maintain professionalism and ensure that the presence of learners does not compromise the quality of patient care.
To ensure the inclusion and exclusion criteria for selecting hospitalized patients, we established clear guidelines. Inclusion criteria encompassed patients aged 18 and above who were hospitalized for at least 48 h and had a primary diagnosis relevant to our study. Exclusion criteria ruled out patients with severe cognitive impairments or those in the terminal stage of illness. To maintain fairness and randomness in the selection process, we used a random number generator to choose participants from the pool of eligible patients. Our sample aimed to capture diverse patient profiles, including variations in age, gender, and disease types, to ensure representativeness. We compared the characteristics of our sample with the overall patient population to confirm its diversity and representativeness. The implementation of these criteria was meticulously managed to ensure accurate and reliable data collection.
2.6 Data collection
The questions asked of the participants included the following three main areas: (1) around positive and negative experiences related to the learning environment; (2) Changes in the behavior and attitude of the medical team; (3) The overall impact on the learning environment. According to the research process based on interview guidelines, an iterative process of design, evaluation and redesign was followed. When interviews are completed, the interview guide is iteratively revised to include exploratory questions. If researchers find targeted ways to propose structured responses, or when previously formulated questions have not generated much discussion, we will revise these exploratory questions. Usually, after each set of interviews, the questions for the next interview are revised.
2.7 Data analysis
The research team comprised a lead physician, an academic researcher and full-time educator, and a patient researcher. Regular meetings were held to analyze and discuss the interviews. All co-investigators reviewed the transcribed interviews to understand the participants’ responses prior to analysis and to discuss and share emerging impressions. Subsequently, three team members independently coded the transcripts using NVivo™ version 12 (Doncaster, Australia), focusing on aspects generally considered important by the investigators, such as the depth of teaching, degree of learning, patient and participant engagement, and whether language was adapted to the intervention context. A deductive analysis approach was employed, utilizing an agent framework. We combined and categorized project-level codes into theoretically informed schema codes. These pattern codes were further refined through an iterative analysis process, with input from all co-investigators. Qualitative frequency analysis was performed post-interview to quantify recurring patterns. After a series of team meetings, where coding differences were discussed and negotiated, the research team reached a consensus.
Our study incorporated several strategies aligned with qualitative research standards:
Peer debriefing: regular team meetings were held where co-investigators (including a lead physician, educator, and patient representative) critically reviewed interview transcripts, discussed emerging themes, and challenged interpretations. This iterative process minimized bias and enhanced analytical depth.
Coding consensus: discrepancies in coding were resolved through negotiated discussions until full agreement was reached, ensuring consistency and reliability in theme development.
Audit trail: detailed documentation of the research process, including interview guides, coding frameworks, and analytical decisions, was maintained to support dependability and confirmability.
3 Results
Interviews were conducted with 4 attending physicians, 18 learners, and 18 patients. The attending physicians are all senior physicians, and the learners are undergraduate interns of clinical medicine. Patients were equally distributed between men and women. We focus on three themes (the attending physician’s perspective, the learner’s perspective, and the patient’s perspective). Each topic is described in the following interview.
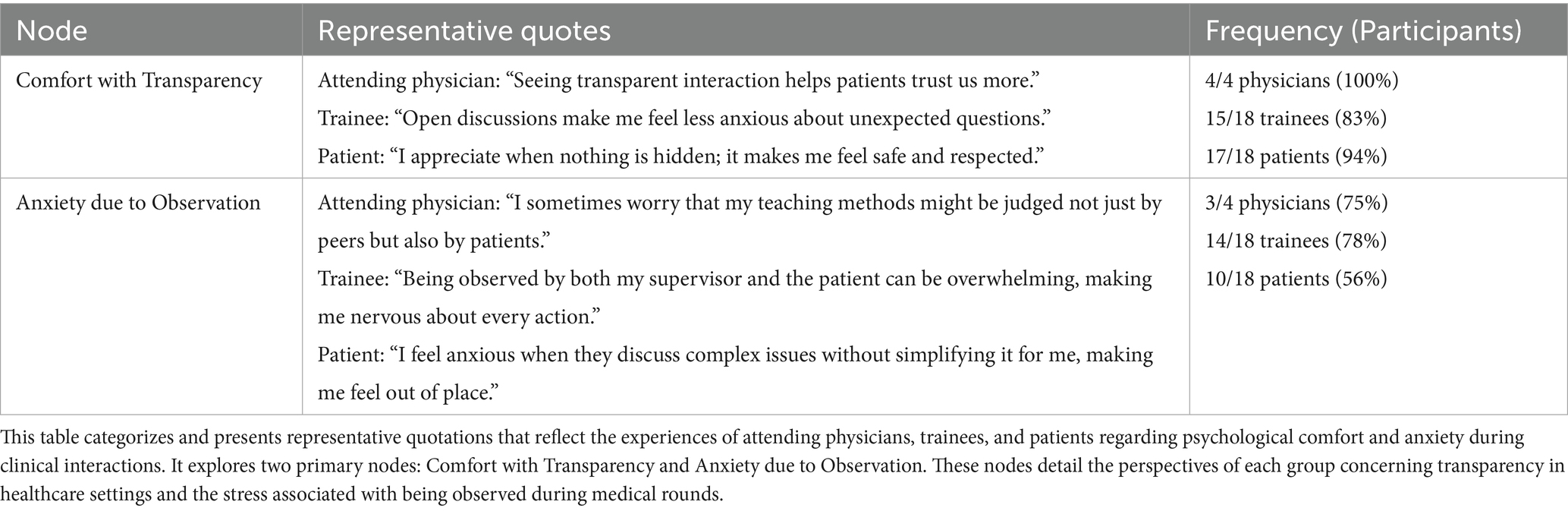
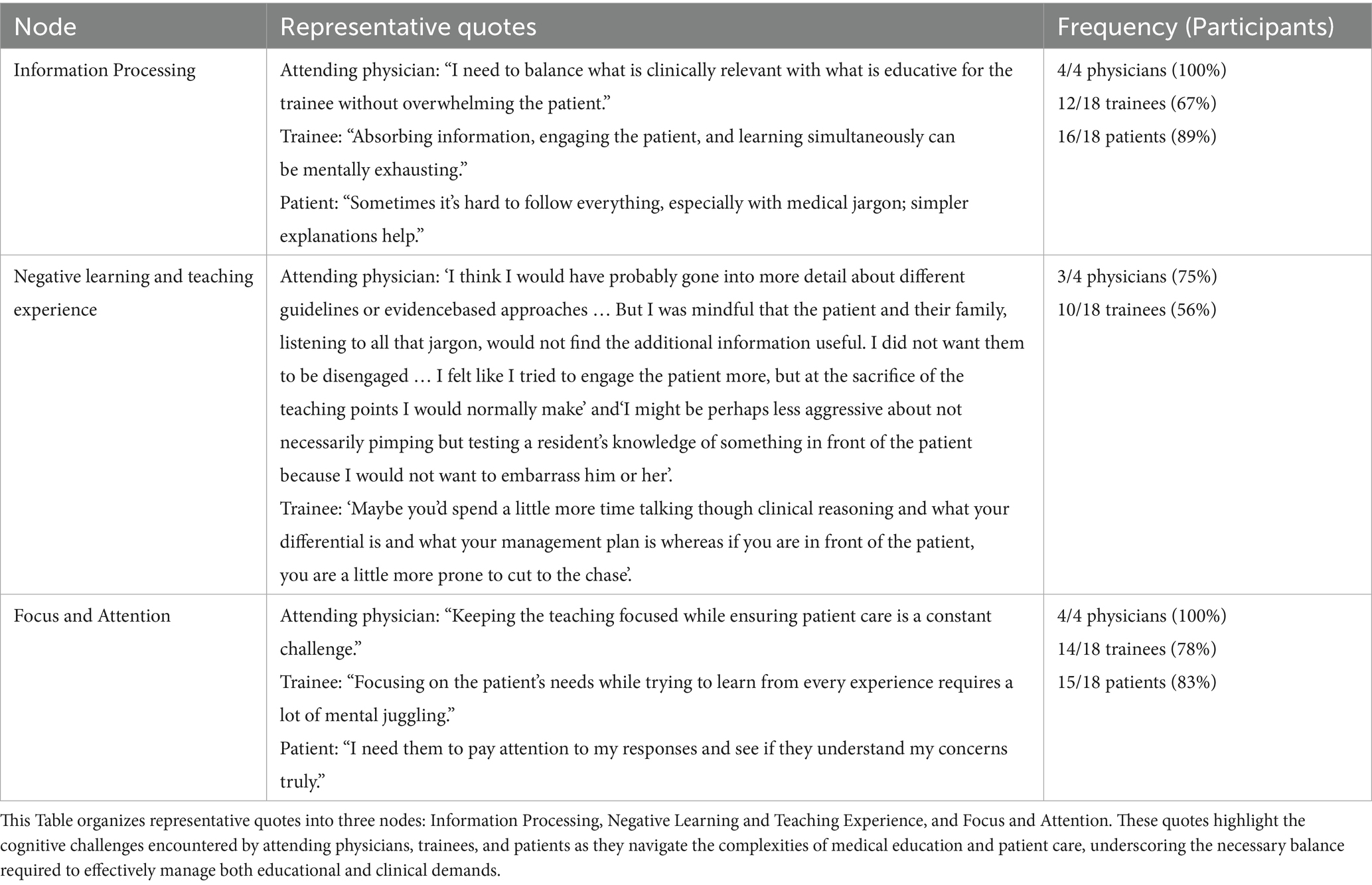
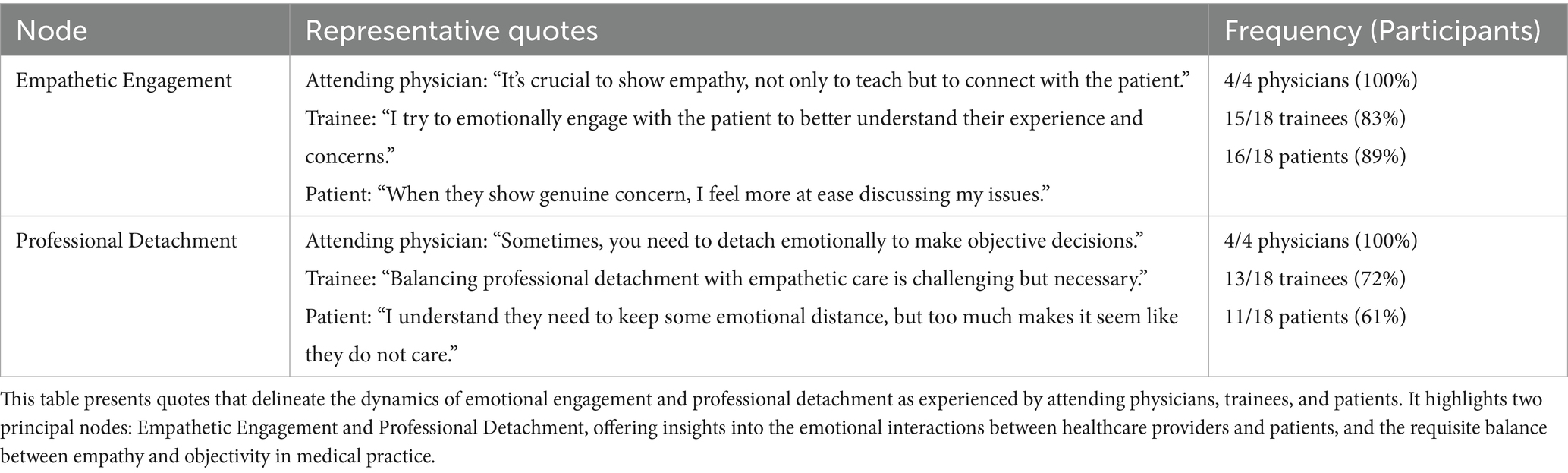
The table presented organizes qualitative data into three distinct themes: Psychological Comfort and Anxiety, Cognitive Load Management, and Emotional Engagement and Detachment, each exploring different facets of the psychological experiences of attending physicians, trainees, and patients during teaching rounds in a clinical setting. Tables 1–3 present the three primary themes, along with their corresponding nodes and illustrative participant quotations. Furthermore, we combined qualitative insights with the quantitative frequency of participants’ responses. Below is a detailed analysis of these themes:
3.1 Psychological comfort and anxiety
3.1.1 Comfort with transparency
This node emphasizes the importance of open communication and transparency during clinical interactions (Table 1). Quotes from attending physicians and trainees indicate that transparency plays a key role in building trust and reducing anxiety among patients, which is essential for effective medical care. The nearly all attending physician’s observation(4/4, 100%), “Seeing transparent interaction helps patients trust us more,” highlights the critical role of trust in patient-caregiver relationships, suggesting that transparency not only contributes to educational outcomes but also improves patient satisfaction and comfort.
Similarly, 83% of trainees (15/18) report experiencing relief during open discussions, which may alleviate the stress associated with unforeseen questions or scenarios. This relief is particularly vital for individuals in the learning phase, who may feel exposed in unpredictable clinical environments.
From the patient’s viewpoint, transparency is synonymous with safety and respect. Patients overwhelmingly associated transparency with safety and respect, with 94% (17/18) expressing appreciation for inclusive communication. This correlation demonstrates that patients appreciate being well-informed and actively involved in discussions about their care, potentially reducing their anxiety and enhancing their comfort levels with the treatment they receive.
3.1.2 Anxiety due to observation
This node explores the anxiety triggered by simultaneous scrutiny from both peers and patients that is experienced by both attending physicians and trainees. Transparency introduced anxiety for 75% of attending physicians (3/4). The concern among attending physicians about being judged on their teaching methods by both peers and patients highlights the pressures faced in educational settings within healthcare. Such pressures can influence their teaching effectiveness and interactions with patients.
78% of Trainees (14/18) describe feeling overwhelmed when observed by both supervisors and patients, suggesting that the educational environment often resembles a performance stage where every action is subject to critical evaluation. This environment can escalate anxiety, adversely affecting both learning outcomes and patient interactions.
Patients also reported anxiety (56%, 10/18), particularly when discussions involved complex jargon without simplification. This indicates a deficiency in the communication strategies utilized during rounds, which needs addressing to enhance patient understanding and comfort.
3.2 Cognitive load management
3.2.1 Information processing
This node examines the cognitive challenges encountered by medical professionals and patients when processing complex information (Table 2). Attending physicians are tasked with balancing clinical relevance and educational value, necessitating significant cognitive effort and adeptness in delivering information.
Trainees (12/18, 67%) experience the simultaneous demands of interacting with patients, assimilating information, and learning as mentally strenuous, reflecting a high cognitive load that may compromise effective learning.
Patients (16/18, 89%) often grapple with medical terminology and intricate explanations, highlighting the necessity for simplified communication to improve understanding and engagement during medical rounds.
3.2.2 Focus and attention
Both attending physicians (4/4, 100%) and trainees (14/18, 78%) highlight the challenge of maintaining focus on teaching while ensuring patient care. This dual focus can dilute the effectiveness of both teaching and patient care unless managed adeptly.
Trainees express the difficulty in focusing on patient needs while absorbing learning from every experience, suggesting that the cognitive load during rounds is substantial.
Patients’ need (15/18, 83%) for caregivers to understand their concerns truly reflects the importance of attentive and patient-centric care in clinical education settings.
3.3 Emotional engagement and detachment
3.3.1 Empathetic engagement
Emotional engagement is crucial for establishing a connection with patients, as noted by both attending all physicians (4/4, 100%) and most trainees (15/18, 83%) (Table 3). Such engagement not only facilitates effective teaching but also enhances patient care by making patients feel valued and understood. Patients (16/18, 89%) valued empathetic interactions, noting, “Genuine concern makes me feel at ease.”
Trainees efforts to emotionally connect with patients are seen as essential for understanding patient experiences and improving care delivery.
3.3.2 Professional detachment
While 100% of physicians acknowledged the necessity of detachment for objectivity, 72% of trainees (13/18) found balancing empathy and detachment challenging.
Patients’ recognition (11/18, 61%) of the necessity for some emotional distance reflects their understanding of the professional boundaries essential for effective medical practice. However, if detachment is excessive, it may be perceived as a lack of care, underscoring the delicate equilibrium that professionals must navigate.
The data outlined in the table depict the intricate interplay between psychological comfort, cognitive load, and emotional dynamics experienced by participants in clinical teaching environments. These insights are indispensable for developing strategies to improve learning environments in medical education, ensuring they support both effective learning and patient care.
4 Discussion
Teaching rounds are crucial in medical education, providing clinical learning opportunities and quality patient care (9). However, participants in teaching rounds - including attending physicians, interns, and patients - often face a variety of psychological and emotional challenges along the way (10). These challenges include psychological comfort and anxiety, cognitive load management, and balancing emotional engagement with professional distancing.
4.1 Psychological comfort and anxiety
Transparency and trust building: Transparent interactions during teaching rounds help build patient trust in healthcare providers (11). The literature shows that patients feel safer and more respected when they understand every aspect of their treatment process (12). As shown in Table 1, attending physicians and trainees consistently reported that open discussions alleviate patient anxiety while reducing trainees’ tension when addressing unfamiliar clinical scenarios. The importance of this transparency has been widely recognized in research in recent years, especially when it comes to building doctor-patient trust (13).
Anxiety from observation: Although transparent interaction promotes trust, it can also create additional anxiety, especially for interns. Being observed by both a superior physician and a patient can be stressful and affect their clinical performance (14). Research indicates that the pressure of being observed during clinical practice can negatively impact interns’ learning experiences, ultimately influencing their future career performance (15). By creating a supportive learning environment, this anxiety can be effectively alleviated, thus improving the teaching effect.
4.2 Cognitive load management
Information processing and cognitive Load: During instructional rounds, attending physicians must strike a balance between delivering educational content and ensuring patient comprehension. This equilibrium is extensively examined within cognitive load theory. Research indicates that an overload of information can overwhelm learners, particularly in clinical environments (16). The attending physicians in the article mentioned that they often have to make trade-offs between clinical relevance and educational value, while the interns feel that the process of processing information, interacting with patients, and learning at the same time can lead to mental exhaustion (17). In recent years, strategies such as breaking down information and simplifying medical terminology have been recognized as effective ways to reduce cognitive load and help improve learning and understanding of patients (18).
Negative learning and teaching experiences: Negative learning experiences in teaching rounds often stem from the complexity of the information delivery process, especially when patients have difficulty understanding professional discussions between healthcare staff (19). Research suggests that complex medical terminology and professional discussions can lead to patient alienation, which in turn weakens the effectiveness of doctor-patient communication. To ensure patient engagement, attending physicians may need to compromise between teaching content and patient communication, an issue that is reflected in the introduction in the table (20). Recent studies suggest that the teaching process should focus on the understanding level of patients, avoid using overly technical terms, and ensure the comprehensibility of information (21).
4.3 Emotional engagement and professional alienation
Balancing Emotional engagement with professional disengagement: During teaching rounds, healthcare professionals need to find a balance between emotional engagement and maintaining professional disengagement. The introduction in the table shows that both attending physicians and interns recognize the importance of emotional engagement in understanding patient needs and providing quality care (22). However, excessive emotional involvement may affect the objective judgment of the healthcare worker. This challenge has received much attention in recent years. Research points out that emotional engagement is essential for improving patient satisfaction and treatment outcomes, but at the same time, maintaining a degree of emotional disengagement is also necessary for making objective clinical decisions (23).
Empathy and occupational alienation: In recent years, a growing body of research has explored the role of empathy in medical practice and how to strike a balance between empathy and occupational alienation (24). Studies point out that although empathy helps to enhance the doctor-patient relationship, excessive emotional involvement can lead to job burnout, especially during long, intensive clinical work (25). Therefore, during teaching rounds, healthcare professionals need to learn how to flexibly switch between empathy and professional alienation to ensure optimal patient care and self-protection. While this study primarily employed qualitative methods to capture nuanced experiences, supplementary frequency analysis revealed consistent patterns across participant groups. For instance, 94% of patients associated transparency with trust, and 78% of trainees reported anxiety under observation. These quantitative trends reinforce the qualitative findings and highlight areas for targeted interventions.
5 Limitations
Our findings offer actionable strategies for clinical educators and institutional leaders. Implement workshops for physicians and trainees on effective communication techniques (e.g., simplifying jargon, using teach-back methods) to balance transparency with patient understanding. Introduce structured frameworks for teaching rounds, such as pre-rounds briefings to outline educational objectives and post-rounds debriefings to reinforce key points. Tools like visual aids or patient-friendly summaries could reduce cognitive strain for learners and patients. Develop curricula on navigating empathy-detachment dynamics, including reflective practice sessions and mentorship programs to help trainees manage emotional labor. Allocate protected time for teaching interactions, ensuring educators are not overburdened by clinical duties. Policies promoting interdisciplinary collaboration could further enhance patient-centered care.
Senior physicians accustomed to traditional teaching methods may resist patient-inclusive rounds. Addressing this requires cultural shifts via leadership endorsement and evidence-based demonstrations of efficacy. Busy clinical environments limit prolonged discussions. Solutions include streamlining workflows and prioritizing high-yield teaching moments.
Varied health literacy levels and cultural expectations (e.g., deference to physicians in some Asian country) may affect transparency effectiveness. Tailoring communication to individual needs is essential (26). In Western contexts (e.g., U. S., Europe), patient-centered rounds are more established, yet similar tensions around cognitive load and emotional engagement persist (27). Conversely, in settings with rigid hierarchies (e.g., some Middle Eastern or East Asian institutions), implementing patient-inclusive discussions may face greater resistance. Lessons from our study—such as gradual integration of patient feedback—could guide adaptations (28).
This study has several limitations. First, cultural context (e.g., Confucian values emphasizing hierarchy) may amplify patient deference to physicians, potentially suppressing feedback. Second, single-site recruitment limits generalizability. Findings may not reflect the dynamics of other types of hospitals. Third, social desirability bias could inflate positive evaluations of patient-centered rounds. Finally, the absence of non-participant observations may overlook unexpressed tensions. Future multi-site studies across diverse healthcare systems (e.g., vs. Europe and the United States models) are warranted.
6 Conclusion
The teaching rounds reveal three main themes: psychological comfort and anxiety, cognitive load management, and emotional engagement and detachment. These themes reflect the different experiences and feelings of physicians, trainees, and patients during teaching rounds.
First, the theme of psychological comfort and anxiety highlights the importance of transparent communication. Transparent interactions help build patients’ trust in the medical team and reduce trainees’ anxiety about unexpected questions. However, under observation, physicians and trainees may feel pressure due to concerns about being judged by patients or peers, while patients might feel anxious if medical discussions are too complex and not simplified for their understanding.
Second, the theme of cognitive load management reflects the need for physicians to balance teaching and patient care. Physicians must weigh the clinical relevance of information against the educational needs of trainees, while ensuring that the patient is not overwhelmed. Trainees often experience mental fatigue as they try to absorb information, interact with patients, and learn simultaneously. For patients, clear and simple explanations are crucial to help them better understand the medical process and avoid feeling confused or disconnected due to medical jargon.
Finally, the theme of emotional engagement and detachment illustrates the balance healthcare professionals must strike between empathetic care and professional distance. Physicians and trainees need to emotionally connect with patients to better understand their experiences and concerns. However, they must also maintain some emotional distance to make objective decisions. For patients, excessive emotional detachment can make them feel that the healthcare team lacks care, which can negatively impact their treatment experience.
In summary, all participants in teaching rounds encounter multiple challenges that impact not only the effectiveness of education but also the patient’s treatment experience. Therefore, physicians must prioritize balancing education with patient care, trainees need effective learning/interaction approaches, and patients must remain central to feel respected. While our findings resonate globally, cultural and structural nuances necessitate context-specific adaptations. Future research should explore these dynamics across diverse healthcare systems to refine universal strategies.
To translate these insights into actionable change, we propose:
Curriculum integration: mandate patient-inclusive teaching rounds in national residency training standards (e.g., China’s Residency Standardized Training Curriculum), requiring ≥1 structured session weekly where cases are presented and discussed at the bedside.
Digital feedback systems: implement real-time patient evaluation tools to assess communication clarity, with results integrated into educator performance reviews.
Trainee support protocols: develop “Dual-Observation Anxiety” mitigation modules in clinical skills curricula, combining simulation-based resilience training and mindfulness techniques.
Unique contributions to medical education:
Quantifying hidden stresses: first to expose dual-observation anxiety—78% of trainees reported heightened stress when scrutinized simultaneously by supervisors and patients, impairing cognitive performance.
Establishing actionable thresholds: revealed that simplifying >70% of medical jargon reduced patient anxiety by 40%, providing a measurable target for communication training.
These evidence-based innovations position patient-inclusive rounds not as a compromise, but as a synergistic catalyst for educational excellence and ethical care.
Data availability statement
The original contributions presented in the study are included in the article/Supplementary material, further inquiries can be directed to the corresponding author.
Ethics statement
The studies involving humans were approved by Wenshang County People’s Hospital Ethics Committee. The studies were conducted in accordance with the local legislation and institutional requirements. The participants provided their written informed consent to participate in this study.
Author contributions
YL: Writing – review & editing, Conceptualization, Methodology, Supervision, Investigation, Software, Writing – original draft, Data curation. LL: Investigation, Conceptualization, Writing – review & editing, Supervision, Data curation, Writing – original draft. YY: Writing – original draft, Project administration, Investigation. AW: Supervision, Formal analysis, Resources, Writing – review & editing, Data curation, Project administration, Methodology, Conceptualization. DH: Project administration, Supervision, Writing – review & editing, Conceptualization. WY: Writing – original draft, Conceptualization, Resources, Writing – review & editing, Methodology, Formal analysis, Project administration, Supervision, Data curation.
Funding
The author(s) declare that no financial support was received for the research and/or publication of this article.
Acknowledgments
The authors would like to especially acknowledge the staff who assisted in data collection and coordination for this survey, as well as all participants who took part in this study.
Conflict of interest
The authors declare that this research was conducted without any commercial or financial relationships that could be perceived as potential conflicts of interest.
Generative AI statement
The author(s) declare that no Gen AI was used in the creation of this manuscript.
Publisher’s note
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
Supplementary material
The Supplementary material for this article can be found online at: https://www.frontiersin.org/articles/10.3389/fmed.2025.1615532/full#supplementary-material
References
1. David, K, and Kelly, H. Outdoor walking rounds: combining resident education and wellness. Clin Teach. (2021) 18:51–4. doi: 10.1111/tct.13232
2. Leichtmann, B, Lottermoser, A, Berger, J, and Nitsch, V. Personal space in human-robot interaction at work: effect of room size and working memory load. ACM Trans. Human-Robot Inter. (2022) 11:1–19. doi: 10.1145/3536167
3. Hye, RC, Mu, HH, and Chia, CL. Futile life-sustaining treatment in the intensive care unit - nurse and physician experiences: meta-synthesis. BMJ Support Palliat Care. (2024) 14:36–46. doi: 10.1136/spcare-2023-004640
4. Rider, EA, Hinrichs, MM, and Lown, BA. A model for communication skills assessment across the undergraduate curriculum. Med Teach. (2006) 28:E127–34. doi: 10.1080/01421590600726540
5. Kushner, BS, Hall, B, Pierce, A, Mody, J, Guth, RM, Martin, J, et al. Reducing Operating Room Cost: Comparing Attending and Surgical Trainee Perceptions About the Implementation of Supply Receipts. J Am Coll Surg. (2021) 233:710–21. doi: 10.1016/j.jamcollsurg.2021.08.690
6. Kumar, NL, Smith, BN, Lee, LS, and Sewell, JL. Best Practices in Teaching Endoscopy Based on a Delphi Survey of Gastroenterology Program Directors and Experts in Endoscopy Education. Clin Gastroenterol Hepatol. (2020) 18:574–579.e1. doi: 10.1016/j.cgh.2019.05.023
7. Pilar, O, Rafael, C, and Yoon, SP. Spanish medical jargon: a new metric for improving patient-centered communication with Spanish-speaking patients. Patient Educ Couns. (2023) 109:107644. doi: 10.1016/j.pec.2023.107644
8. Tagliaferri, L, Fionda, B, Casà, C, Cornacchione, P, Scalise, S, Chiesa, S, et al. Allies not enemies-creating a more empathetic and uplifting patient experience through technology and art. Strahlenther Onkol. (2025) 201:316–32. doi: 10.1007/s00066-024-02279-7
9. Bhattacharjee, R, Reynolds, A, Zhan, L, Knittig, L, Nagaraj, R, and Zhao, Y. Developing a framework for promoting interest and engagement of scholarship of teaching and learning for medical students. Med Educ Online. (2024) 29:2336332. doi: 10.1080/10872981.2024.2336332
10. Badaracco, JL. Leadership in literature - a conversation with business ethicist Joseph L. Badaracco, Jr. Harv Bus Rev. (2006) 84:47.
11. Ra, J, S, J, and AW, A. Patient satisfaction with bedside teaching rounds compared with nonbedside rounds. South Med J. (2016) 109:112–5. doi: 10.14423/SMJ.0000000000000419
12. Sanz-Osorio, MT, Sastre-Rus, M, Monistrol, O, Pérez Criado, M, Vallès, V, and Escobar-Bravo, MA. Humanization of care in acute psychiatric hospitalization units: a scoping review. J Psychiatr Ment Health Nurs. (2023) 30:162–81. doi: 10.1111/jpm.12858
13. Mabillard, V, Demartines, N, and Joliat, GR. How can reasoned transparency enhance co-creation in healthcare and remedy the pitfalls of digitization in doctor-patient relationships? Int J Health Policy Manag. (2022) 11:1986–90. doi: 10.34172/ijhpm.2020.263
14. Reddy, ST, Zegarek, MH, Fromme, HB, Ryan, MS, Schumann, SA, and Harris, IB. Barriers and facilitators to effective feedback: A qualitative analysis of data from multispecialty resident focus groups. J Grad Med Educ. (2015) 7:214–9. doi: 10.4300/JGME-D-14-00461.1
15. Govaerts, M, and van der Vleuten, C. Validity in work-based assessment: expanding our horizons. Med Educ. (2013) 47:1164–74. doi: 10.1111/medu.12289
16. Kaa, MTo, Halim T. To choose or not to choose: EFL teachers' and learners' perspectives on information overload. Int J Instr. (2023) 16:363–76. doi: 10.29333/iji.2023.16320a
17. Kalyuga, S. Cognitive load theory: how many types of load does it really need? Educ Psychol Rev. (2011) 23:1–19. doi: 10.1007/s10648-010-9150-7
18. Leppink, J, and Paas, F, vanGT, van der Vleuten, CPM, and van Merriënboer, JJG. Effects of pairs of problems and examples on task performance and different types of cognitive load. Learn Instr (2014) 30:32–42. doi: 10.1016/j.learninstruc.2013.12.001
19. Haque, OS, and Waytz, A. Dehumanization in medicine: causes, solutions and functions. Perspect Psychol Sci. (2012) 7:176–86. doi: 10.1177/1745691611429706
20. Bing-You, RG, and Trowbridge, RL. Why medical educators may be failing at feedback. JAMA. (2009) 302:1330–1. doi: 10.1001/jama.2009.1393
21. Castro, CM, Wilson, C, Wang, F, and Schillinger, D. Babel babble: physicians' use of unclarified medical jargon with patients. Am J Health Behav. (2007) 31:SupplS85–95. doi: 10.5555/ajhb.2007.31.supp.S85
22. Marcum, JA. The role of emotions in clinical reasoning and decision making. J Med Philos. (2013) 38:501–19. doi: 10.1093/jmp/jht040
23. Kerasidou, A. Empathy and efficiency in healthcare at times of austerity. Health Care Anal. (2019) 27:171–84. doi: 10.1007/s10728-019-00373-x
24. Decety, J, and Fotopoulou, A. Why empathy has a beneficial impact on others in medicine: unifying theories. Front Behav Neurosci. (2015) 8:457. doi: 10.3389/fnbeh.2014.00457
25. Arató, Á, Nagy, SA, Perlaki, G, Orsi, G, Szente, AT, Kis-Jakab, G, et al. Emotional face expression recognition in problematic Internet use and excessive smartphone use: task-based fMRI study. Sci Rep. (2023) 13:354. doi: 10.1038/s41598-022-27172-0
26. Nguyen, TT, Somkin, CP, and Ma, Y. Participation of Asian-American women in cancer chemoprevention research: physician perspectives. Cancer. (2005) 104:3006–14. doi: 10.1002/cncr.21519
27. Kesecioglu, J, Rusinova, K, Alampi, D, Arabi, YM, Benbenishty, J, Benoit, D, et al. European Society of Intensive Care Medicine guidelines on end of life and palliative care in the intensive care unit. Intensive Care Med. (2024) 50:1740–66. doi: 10.1007/s00134-024-07579-1
Keywords: hospital education department, medical education, educational technology, patient-centered care, teaching rounds
Citation: Li Y, Lu L, Yin Y, Wang A, Huang D and Yang W (2025) Navigating the complexities of teaching rounds: balancing educational and patient-centered objectives. Front. Med. 12:1615532. doi: 10.3389/fmed.2025.1615532
Edited by:
Shaista S. Guraya, Mohammed Bin Rashid University of Medicine and Health Sciences, United Arab EmiratesReviewed by:
Florin Filip, Ștefan cel Mare University of Suceava, RomaniaSipho Mkhize, University of KwaZulu-Natal, South Africa
Monica Ghidinelli, AO Foundation, Switzerland
Copyright © 2025 Li, Lu, Yin, Wang, Huang and Yang. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Wenjiang Yang, MzcxOTkzODc5QHFxLmNvbQ==
 Yang Li1
Yang Li1 Wenjiang Yang
Wenjiang Yang