- State Key Laboratory of Complex Severe and Rare Diseases, Department of Dermatology, Peking Union Medical College Hospital, Chinese Academy of Medical Sciences and Peking Union Medical College, National Clinical Research Center for Dermatologic and Immunologic Diseases, Beijing, China
Background: Male genital dermatoses encompass a diverse range of infectious, inflammatory, and neoplastic conditions with overlapping clinical presentations, often leading to diagnostic challenges. Misdiagnosis can result in inappropriate management and significant patient distress, particularly given the sensitive nature of the anatomical site. Although histopathology remains the diagnostic gold standard, non-invasive tools such as dermoscopy are becoming increasingly valuable for preliminary evaluation. A thorough understanding of the clinical features associated with male genital dermatoses is essential for achieving accurate diagnoses.
Methods: Our retrospective study analyzed 572 histopathologically confirmed cases of lesions on the male external genitalia at Peking Union Medical College Hospital from 2015 to 2025. Data included demographics, disease duration, lesion distribution, dermoscopy results if exists, and clinical-dermatoscopic-pathological concordance.
Results: The cohort with a mean age of 47.6 years, exhibited distinct age-specific patterns: adolescents (1.2%) had inflammatory/autoimmune conditions; adults (70.6%) showed human papillomavirus-associated (Bowenoid papulosis, genital warts) and inflammatory diseases (lichen sclerosus); and elderly patients (28.1%) had higher malignancy rates (extramammary Paget’s disease, squamous cell carcinoma). Overall, inflammatory diseases (33.7%) and tumors (33.4%) were the most common diagnoses. Notably, diagnostic clinical-pathological discordance was observed in 34.6% of cases, particularly for lichen planus (4.9%) and extramammary Paget’s disease (2.8%).
Conclusion: This study highlights the diverse etiologies of male genital dermatoses and underscores the necessity of age-stratified evaluations. The use of dermoscopy improves diagnostic accuracy and minimizes the need for unnecessary biopsies. Conditions such as extramammary Paget’s disease, bowenoid papulosis, and lichen sclerosus require heightened awareness due to their potential for malignancy or diagnostic complexity. Integrating clinical, dermoscopic, and histopathological data is critical for effective management.
Introduction
Male genital dermatoses encompass a wide range of conditions with overlapping clinical manifestations, including infectious, inflammatory, and neoplastic disorders, which often lead to diagnostic challenges. These dermatoses may be localized to the genital area or represent a manifestation of a more widespread dermatologic condition. Misdiagnosis or delayed diagnosis can result in inappropriate management and significant psychological distress for patients. Patients often delay seeking medical attention owing to the sensitive location of lesions, increasing risks of delayed or incorrect diagnoses and subsequent therapeutic delays. Meanwhile, patients frequently worry that genital lesions may indicate sexually transmitted infections (STIs), a concern that can lead to significant psychological distress and social stigma. This highlights the crucial need for accurate differentiation between STI-related and non-STI-related dermatoses during clinical evaluations (1). Although histopathological examination remains the gold standard for diagnosis, biopsies of the external genitalia carry risks, including potential impacts on function, appearance, psychological well-being, and overall quality of life. To better understand the clinical characteristics of these conditions, we conducted a retrospective analysis of demographic data, disease profiles, lesion morphology, and clinical-dermatocopic-pathological diagnostic discrepancies in male external genitalia biopsies performed at our center over the past decade. This study aims to enhance the recognition of these conditions among dermatologists and urologists while reducing the likelihood of misdiagnosis.
Materials and methods
In this retrospective study, we analyzed 572 cases of histopathologically confirmed skin lesions of the male external genitalia (defined as involving the penis and/or scrotum) at Peking Union Medical College Hospital from March 2015 to March 2025. Only cases with clinical photographs, histopathological images, and comprehensive medical records were included. Data were extracted from electronic medical records, including demographics, disease duration, disease distribution, clinical presentation, symptoms, pathological diagnosis, and clinical diagnosis. All patients scheduled for skin biopsy will be screened for hepatitis B, hepatitis C, syphilis, and human immunodeficiency virus, as well as whole blood routine and coagulation tests. Additionally, for cases with available dermoscopy data, those findings were also incorporated into the analysis. All dermoscopic interpretations and histopathological evaluations were independently assessed and confirmed by two experienced dermatologists. The final histopathological results will refer to laboratory results, especially in the case of infectious diseases, for accurate diagnosis. The study was approved by the ethics committee of Peking Union Medical College Hospital (K 8437).
Results
Patient characteristics
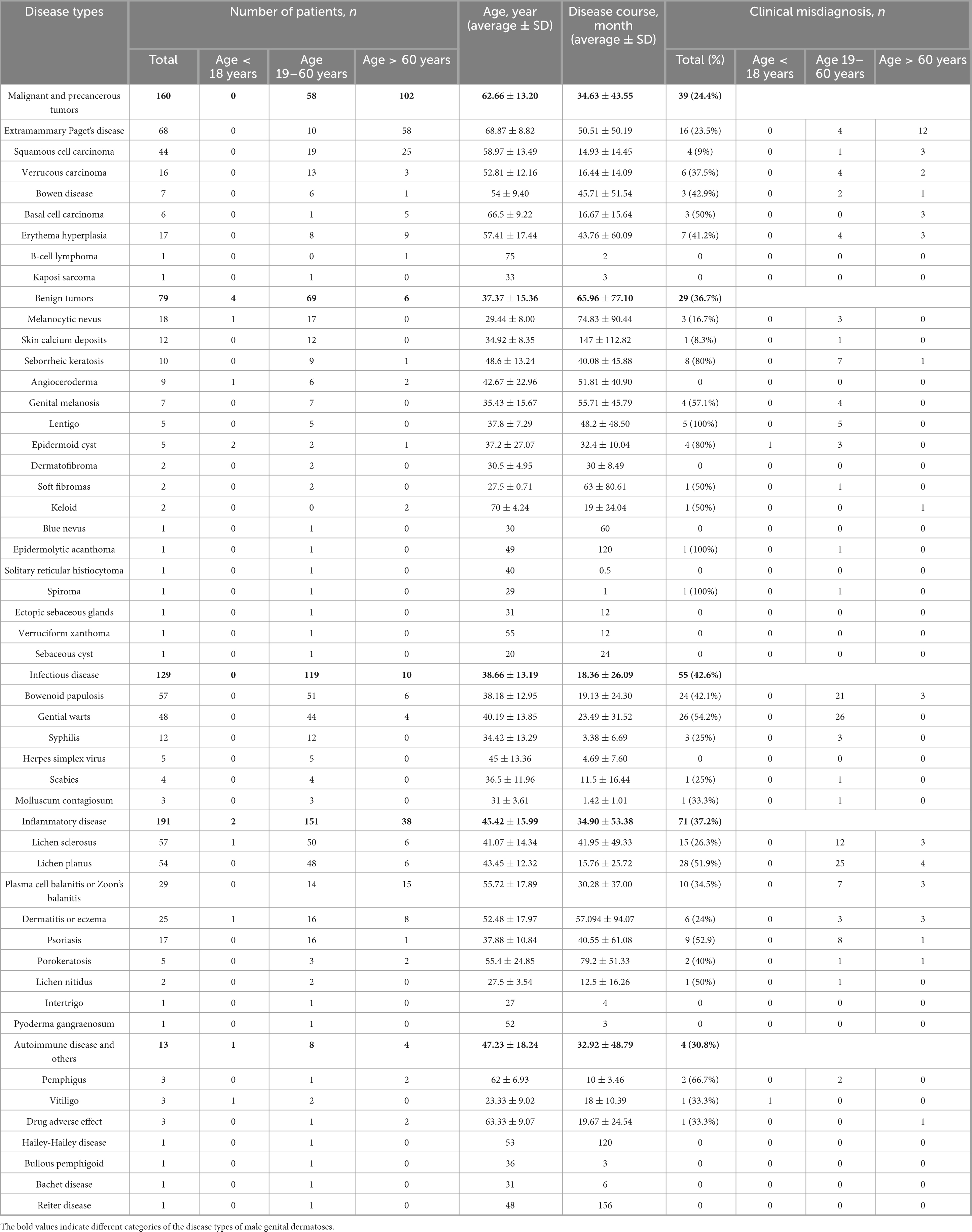
The mean age of the patients was 47.64 ± 17.6 years (range: 12–95 years), with 7 cases (1.2%) occurring in adolescents aged 18 and under, 404 (70.6%) in adults (19–60 years), and 161 (28.1%) in elderly patients (>60 years,70.34 ± 17.60 years). The distribution of patients across different disease is presented in Table 1.
Disease constitution, duration and anatomical distribution
The study identified 47 distinct pathological diagnoses. The mean disease duration was 35.2 ± 51.9 months, with cases categorized as follows: inflammatory diseases (191 cases, 33.4%), benign and malignant tumors (239 cases, 41.8%), infectious diseases (129 cases, 22.6%), and autoimmune diseases and other conditions (13 cases, 2.3%). The ten most prevalent diagnoses were extramammary Paget’s disease (EMPD) (68 cases, 11.9%), Bowenoid papulosis (BP) (57 cases, 10.0%), lichen sclerosus (LS) (57 cases, 10.0%), lichen planus (LP) (54 cases, 9.4%), genital warts (48 cases, 8.4%), squamous cell carcinoma (SCC) (44 cases, 7.7%), balanitis (29 cases, 5.0%), dermatitis or eczema (25 cases, 4.4%), melanocytic nevi (18 cases, 3.1%), and erythema hyperplasia (17 cases, 3.0%). Demographic information, disease distribution, disease course, and age distribution are summarized in Table 1.
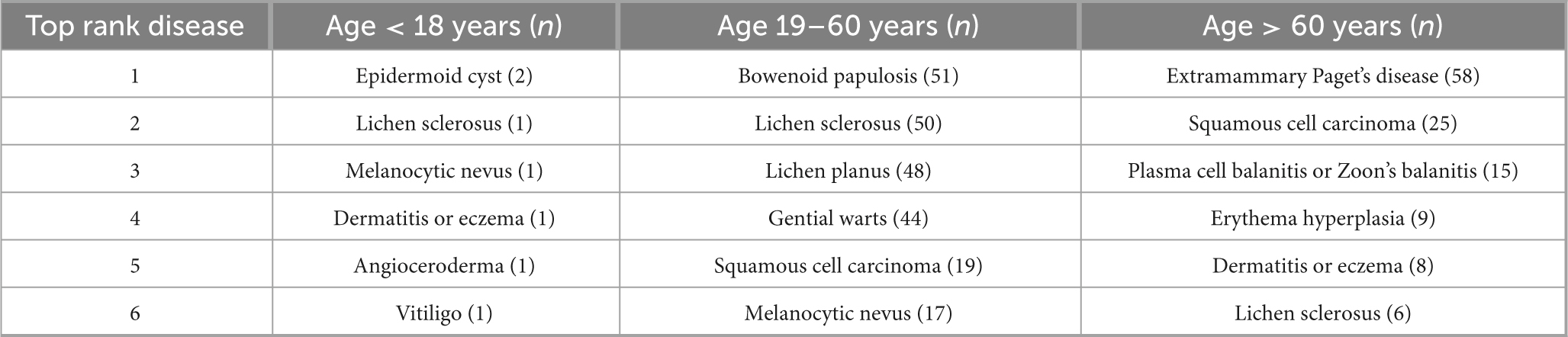
In the pediatric group, the mean disease duration was 38.6 ± 46.5 months. The most prevalent diagnosis was epidermoid cysts (2 cases, 28.6%), followed by vitiligo, angiokeratoma, dermatitis, LS and pigmented nevus (1 case each). Among adults, the mean disease duration was 35.5 ± 54.7 months, with infectious and inflammatory conditions predominating. The top five diagnoses in this group were BP (51 cases, 12.6%), LS (50, 12.4%), LP (47, 11.6%), genital warts (43, 10.6%), and SCC (19, 4.7%). In the elderly cohort, the mean duration was 34.5 ± 44.7 months, and there was a notable increase in the prevalence of malignancies. The top five diagnoses included EMPD (58 cases, 36.0%), SCC (25, 15.5%), balanitis (15, 9.3%), erythema hyperplasia (9, 5.6%), and dermatitis/eczema (8, 5.0%). The top five diseases across different age groups are summarized in Table 2.
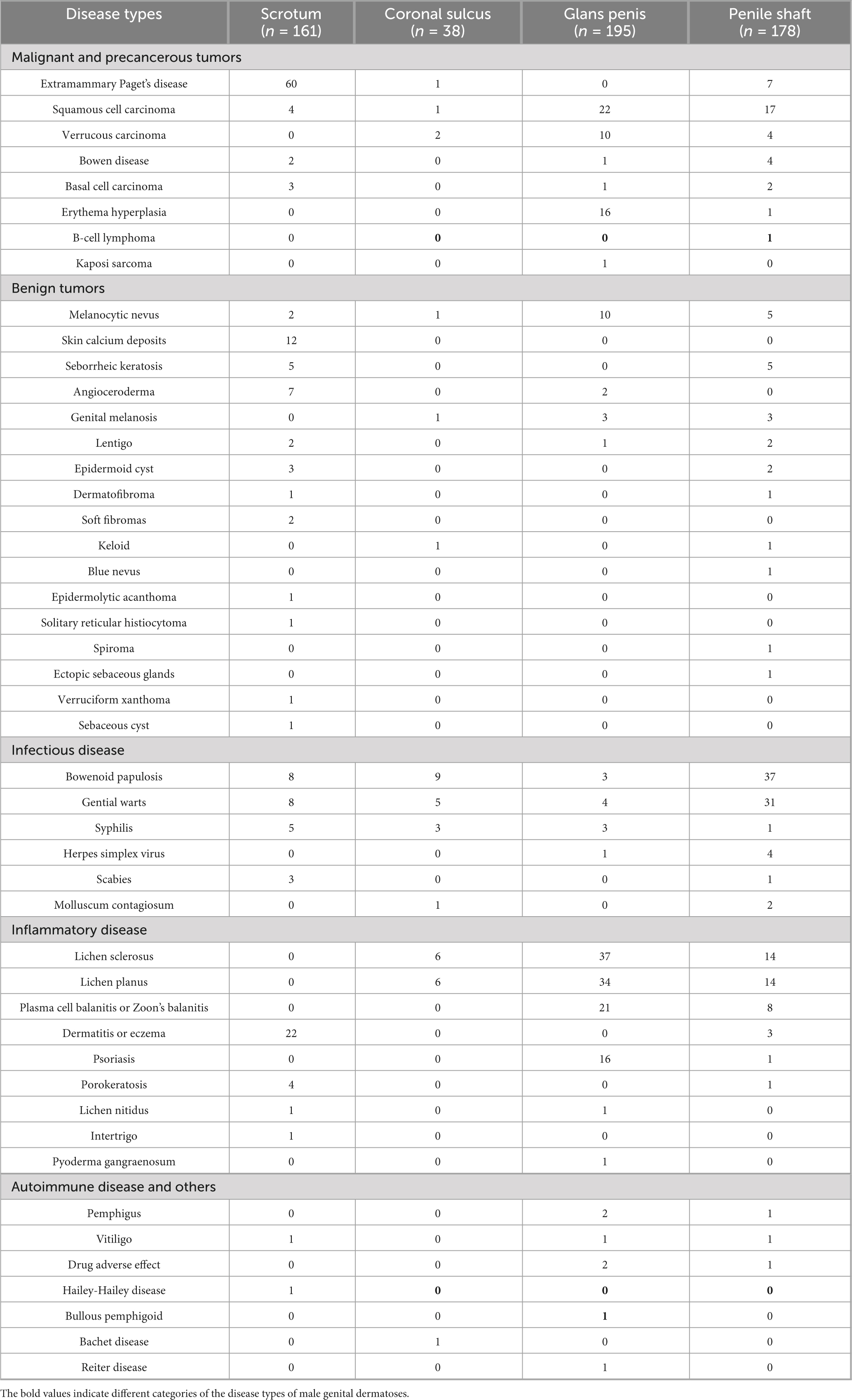
Based on the biopsy sites of skin lesions, the male genitalia area was divided into four anatomical regions: the scrotum, penile shaft, coronal sulcus, and glans penis. The glans penis was the most frequently biopsied site (195 cases), followed by the penile shaft (178 cases), scrotum (161 cases), and coronal sulcus (38 cases). Lesions involved multiple genital regions in 61 patients, with some cases also extending to extragenital areas (e.g., perianal region, perineum, and axillae). The distribution of these disease is presented in Table 3.
Clinical presentations
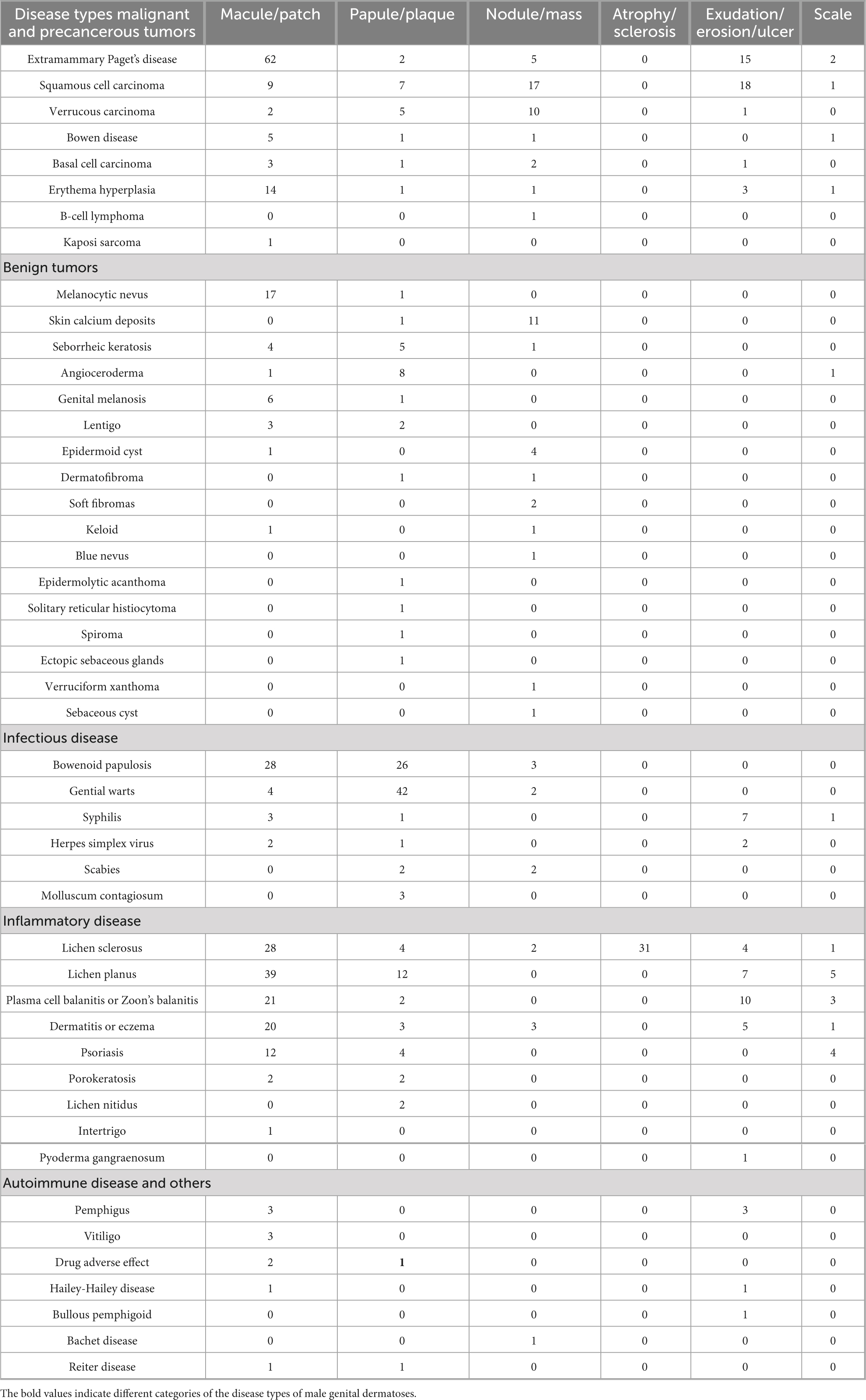
Dermatoses affecting the male external genitalia present a wide range of clinical manifestations. In our study, the manifestations of the skin diseases were consistent with previous findings. EMPD was characterized by persistent erythematous plaques, often accompanied by exudation, erosion, or ulceration. LS typically presented with localized sclerosis and epidermal atrophy, with severe cases progressing to frenular contracture and urethral stricture, resulting in functional impairment. Malignant neoplasms, including basal cell carcinoma (BCC), SCC, and verrucous carcinoma, typically manifested as nodules or indurated masses, sometimes with chronic non-healing ulcers.
Erosion and ulcers can also be seen in infectious skin diseases such as syphilis and herpes simplex, as well as in autoimmune bullous disease. Soft fibromas typically present as pedunculated skin tags. Papular lesions with variable coloration, size, and surface texture were observed in conditions such as BP, warts, lichen nitidus, and sebaceous hyperplasia. Scaling plaques were prominent in psoriasis and lichen planus, while erythroplasia of Queyrat and balanitis primarily presented as erythematous patches. Pruritus was a hallmark of inflammatory conditions (e.g., dermatitis, eczema, lichen simplex chronicus), whereas pain was strongly associated with ulcerative lesions. A summary of these clinical manifestations is summarized in Figure 1 and Table 4. The supplementary figures depict the typical dermoscopic (Supplementary Figure 1) and histopathological (Supplementary Figure 2) features of common male external genital skin diseases.

Figure 1. Clinical features of common male external genital skin diseases. (a) Extramammary Paget disease: Ill-defined erythematous plaque with exudation, erosion and scales involved the scrotum and penile shaft. (b) Bowenoid papulosis: Multiple pigmented maculopapular lesions with various sizes on the glans penis and penile shaft. (c) Lichen sclerosus: Porcelain-white atrophic plaques with epidermal fragility, and erosions on the glans penis. (d) Lichen planus: Violaceous polygonal papules with white reticular striae along the coronal sulcus and glans. (e) Genital warts: Multiple skin-colored to hyperpigmented cauliflower-like papulonodules distributed on the penile shaft. (f) Squamous cell carcinoma: An erythematous verrucous mass exhibiting central erosive ulceration surrounded by peripheral hyperkeratosis with serous crusting and collarette scaling on glans penis.
Inconsistency between the clinical and pathological diagnosis
In our retrospective study, 198 cases (34.6%) exhibited discordance between the initial clinical diagnoses and the final pathological diagnoses. Our study revealed variable discordance rates across disease categories, with the highest rates observed in infectious diseases (42.6%), followed by inflammatory conditions (37.2%), benign tumors (36.7%), autoimmune and other disorders (30.8%), and malignant or premalignant lesions (24.4%). The discordance rate is presented in detailed in Table 1.
Inconsistency between the clinical and dermoscopy diagnosis
Using the patient names and medical record numbers, we systematically cross-referenced our institutional dermoscopic database with histopathological records, identifying 73 cases (16.9% of 433 histopathologically evaluated patients) with complete clinical photographs and dermoscopic records. Through analysis of characteristic dermoscopic patterns, we achieved definitive diagnoses of seborrheic keratosis, LS, psoriasis, angiokeratoma, melanocytic nevus, porokeratosis, balanitis, genital warts, LP, BP, and malignant conditions. Histopathological confirmation was obtained in 42 cases (57.5% diagnostic concordance rate). Eighteen cases (24.7%) exhibited non-specific dermoscopic patterns necessitating comprehensive differential diagnosis, encompassing inflammatory conditions (balanitis, LP, LS, dermatitis), infectious diseases (syphilis, BP), and neoplastic lesions including EMPD and erythroplasia of Queyrat. The dermoscopic diagnosis of 13 cases was different from the final pathological diagnosis, including the confusion between genital warts and BP, and the confusion between LS and LP.
Discussion
Our retrospective study evaluated 572 histopathologically confirmed cases from Peking Union Medical College Hospital, encompassing a comprehensive assessment of demographic data, disease duration, clinical manifestations, and diagnostic concordance between initial clinical impressions and definitive histological findings. STIs, including syphilis, herpes simplex virus (HSV) infection, and gonorrhea, represent the most prevalent conditions affecting the male external genitalia. In contrast, non-STI dermatoses of the male external genitalia encompass a wide spectrum of disease with varied etiologies. There are only a few comprehensive studies on the pattern of nonvenereal dermatoses in males (2, 3). To the best of our knowledge, our study is the largest single-center study of male external genitalia skin diseases in China to date. Our cohort demonstrated remarkable etiological diversity, incorporating infectious pathogens, immune-mediated conditions, chronic inflammatory disorders, and metabolic deposition diseases, thereby providing a representative cross-section of genital dermatopathology in male patients.
In our study, we observed significant differences in the disease spectrum among various age groups. Adolescents predominantly affected by inflammatory and autoimmune conditions, while sexually active adults showed a higher prevalence of human papillomavirus (HPV)-associated diseases. Notably, elderly patients had a significantly elevated risk of developing cutaneous tumors, emphasizing age as a critical oncogenic risk factor. These findings highlight the importance of age-stratified diagnostic approaches. In particular, for elderly populations, proactive tumor screening for genital lesions is strongly recommended to facilitate early detection and optimize clinical outcomes.
In our study, the most common biopsied skin disease was EMPD. EMPD is a rare cutaneous malignancy with metastatic potential, predominantly affecting elderly individuals in apocrine-rich regions such as the genital, perianal, and axillary areas. This dermatologic entity may either precede or coexist with underlying visceral malignancies (4). Clinically, EMPD can mimic common inflammatory and infectious dermatoses, leading to delays in diagnosis and potentially resulting in metastasis and a poor prognosis. In our study, EMPD was characterized by late onset, long disease duration, and a predilection for the scrotum. A panel of immunohistochemical staining, including AE1/AE3, CK7, CEA, EMA, S100, and periodic acid-Schiff staining, is useful for diagnosing EMPD (5). Additionally, other skin tumors can also occur in the male genitalia area. Mazzoni et al. reviewed a cohort of 1525 patients with genital premalignant and malignant diseases in Australia, providing further context to the range of conditions that can affect this region (6). In our study, premalignant or malignant lesions were identified in 5% of cases (74 cases), with penile intraepithelial neoplasia (57%), SCC (15%), and BP (12%) being the most common. These lesions exhibited distinct anatomical distributions: penile intraepithelial neoplasia and BP were found on the penile shaft, SCC on the glans, and BCC on the scrotum. The benign tumors in our cohort included seborrheic keratosis, angiokeratoma, dermatofibroma, acrochordon (soft fibroma), epidermolytic acanthoma, solitary reticular histiocytoma, keloid, and melanocytic nevus. Malignant neoplasms identified included Bowen’s disease, SCC, BCC, verrucous carcinoma, and cutaneous B-cell lymphoma. Histopathological examination is the golden standard for distinguishing these diseases. Our findings suggested that cutaneous neoplasms in the external genital region may develop either as primary lesions or as secondary manifestations of systemic malignancies.
In our research, the relatively low incidence of classic STIs can be attributed to two key factors. Firstly, these infections are typically diagnosed through serological tests, viral cultures, or nucleic acid amplification tests rather than histopathological examination. Secondly, biopsy is generally unnecessary for their clinical confirmation unless atypical presentations warrant histological evaluation. Therefore, our current study design cannot fully capture the true epidemiological profile of STIs diagnosed by standard laboratory methods. Some atypical manifestations of syphilis, such as Follmann balanitis, phagedenic chancres or multiple chancres, may be misdiagnosed or missed in the study if they were not clinically suspected and therefore not biopsied (7, 8). Among infectious etiologies in our cohort, the most prevalent diagnoses were BP, warts, syphilis, HSV infection, scabies and molluscum contagiosum. BP, a genital dysplasia induced by HPV infection, is characterized by multiple asymptomatic, well-demarcated, red-brown to violaceous papules with a flat, smooth, or verrucous surface. These lesions typically arise on the glans penis and foreskin in male patients and may coalesce into larger plaques (9). In our research, BP was found to have the highest incidence rate among adults aged 18–60 years. Despite its prevalence, we observed a 42% discordance rate between initial clinical impressions and final histopathological diagnoses, primarily due to its morphological similarity to other conditions such as condyloma acuminatum, viral warts, lichen planus, and seborrheic keratosis. Pathologically, BP needs to be differentiated from Bowen disease and erythroplasia of Queyrat. Although the transformation of BP into invasive SCC is rare, occurring in less than 1% of patients, it is still recommended to perform HPV subtyping tests to screen for potential carcinogenic HPV infections. Additionally, concurrent physical examinations and cytologic screening for sexual partners are recommended to ensure comprehensive management and prevention of disease progression (10).
In our study, inflammatory dermatoses were the most common disease category, accounting for 191 out of 572 cases. Therefore, these conditions require particular clinical attention due to their potential for chronicity, functional impairment, and significant impact on quality of life. The predominant entities in our cohort included LS, LP, balanitis, and psoriasis. LS, also referred to balanitis xerotica obliterans, is a chronic inflammatory disorder that affects both genital and extragenital mucocutaneous tissues. In our research, it primarily affected the glans penis and prepuce. LS can present with hypopigmented lesions, erosions, or atrophy, and is characterized by debilitating symptoms such as pruritus, pain, dysuria, urinary stream obstruction, dyspareunia, and sexual dysfunction (11). Importantly, LS is associated with an increased risk of developing squamous cell carcinoma of penis, highlighting the need for vigilant monitoring and management of this condition (12). Early identification of LS is crucial for alleviating symptoms, preventing disease progression, and reducing the risk of malignant transformation. In contrast, psoriasis often presents as well-demarcated, erythematous plaques, with genital involvement affecting up to 63% of patients (13). However, in 2%–5% of patients, genital involvement may be the only manifestation of cutaneous psoriasis (14). This isolated presentation, particularly when it affects the glans penis and coronal sulcus, frequently exhibit atypical clinical features that complicate diagnosis. We observed a 53% discordance rate between initial clinical impressions of genital psoriasis and histopathological diagnoses. In such challenging cases, the presence of extragenital psoriatic features, such as nail pitting, arthropathy or classic skin lesions, often provides valuable diagnostic clues.
In addition, our study observed several rare conditions, including epidermolytic acanthoma, solitary reticular histiocytoma, verruciform xanthoma, and porokeratosis. However, the limited sample size of these cases presents certain limitations in our research findings. Despite these constraints, the identification of these rare conditions contributes to a broader understanding of dermatological disease spectrum.
In our study, 198 patients (34.6%) showed discrepancies between clinical and histological diagnoses. This inconsistency may be due to the clinical similarities among various male genital dermatoses. To address this challenge, dermoscopy and reflectance confocal microscopy (RCM), as non-invasive diagnostic tools, can be used to evaluate both melanocytic and non-melanocytic skin lesions, as well as a range of inflammatory and infectious skin diseases. Our analysis revealed a 57.5% diagnostic concordance rate (42/73) between dermoscopic features and histopathological confirmation, underscoring the clinical utility of dermoscopy in characterizing prototypical genital lesions such as LS, SCC, LP and melanocytic nevus. However, diagnostic discrepancies persisted in cases with atypical presentations or non-specific dermoscopic patterns (e.g., inflammatory dermatoses and early malignant transformations), necessitating multimodal integration of clinical-pathological correlation. Notably, the limited adoption of concurrent dermoscopic-histopathological evaluation (16.9%, 73/433 cases) highlights systemic gaps in real-world diagnostic workflows. By identifying characteristic patterns, dermoscopy and RCM significantly improve diagnostic accuracy and help to minimize the need for unnecessary invasive procedures. Extensive literature has documented the dermoscopic and RCM features of common genital diseases, providing valuable references for their diagnosis and differential diagnosis, thereby enhancing the precision of dermatological assessments (9, 15). We have reviewed and summarized the most common male external genital skin disorders in our study in the Table 5 (16–23). Given the unique nature of the anatomical area, some scholars have suggested using polarized, non-contact dermoscopy to prevent the spread of infectious diseases. Additionally, videodermatoscope can be used to avoid close contact between the examiner’s head and the patient’s genitals (16).
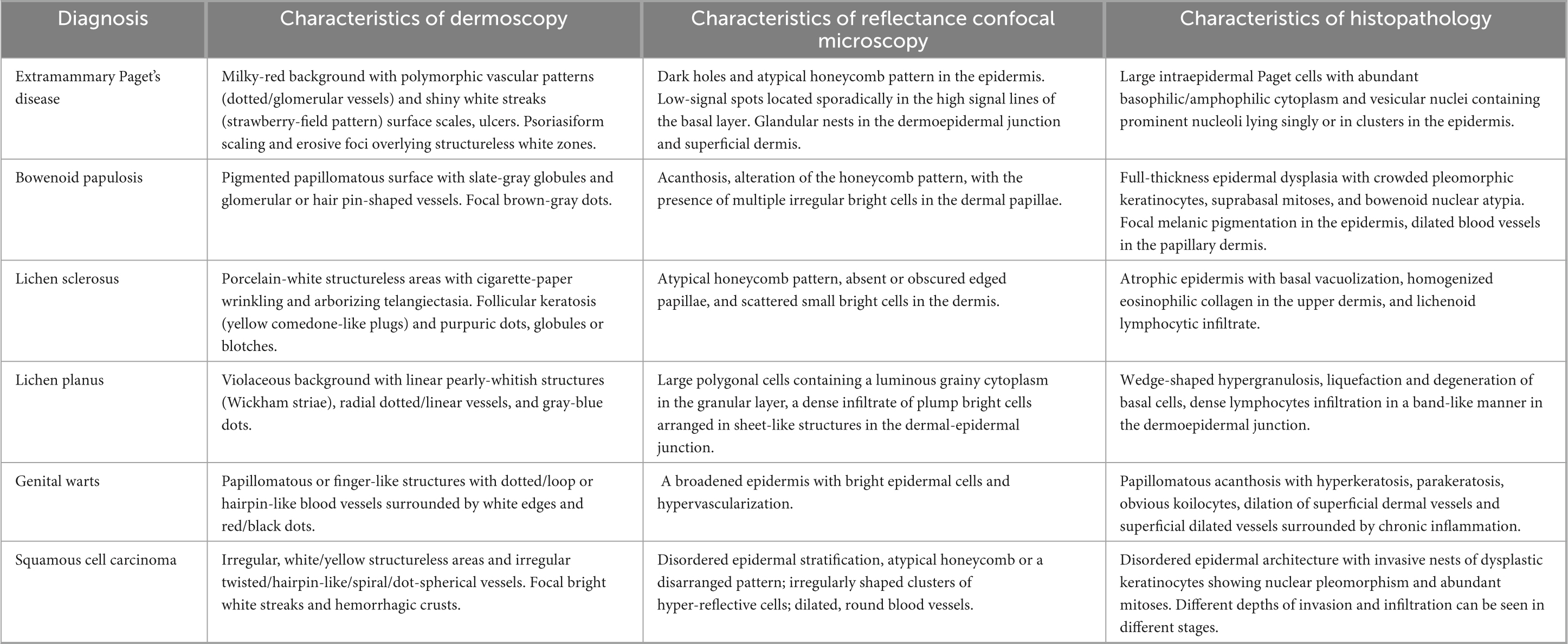
Table 5. Dermoscopic, reflectance confocal microscopic and histopathological characteristics of the most common six diseases in the study.
Conclusion
In conclusion, our research presents a comprehensive single-center retrospective study encompassing 572 histopathologically confirmed cases of male external genital skin lesions. The primary objective of this study was to enhance diagnostic accuracy and minimize misdiagnosis by thoroughly examining the demographic, clinical, and histopathological features of these conditions.
Data availability statement
The original contributions presented in this study are included in this article/Supplementary material, further inquiries can be directed to the corresponding author.
Ethics statement
The studies involving humans were approved by the Institutional Ethics Committee of Peking Union Medical College Hospital. The studies were conducted in accordance with the local legislation and institutional requirements. Written informed consent for participation in this study was provided by the participants’ legal guardians/next of kin. Written informed consent was obtained from the individual(s) for the publication of any potentially identifiable images or data included in this article.
Author contributions
Y-TQ: Software, Visualization, Data curation, Writing – original draft, Methodology, Investigation, Project administration, Validation. XM: Writing – original draft, Data curation, Investigation. J-YZ: Data curation, Investigation, Writing – original draft. J-WL: Supervision, Writing – original draft, Investigation, Validation. KF: Validation, Writing – original draft, Data curation. D-LM: Supervision, Resources, Data curation, Conceptualization, Writing – review & editing, Validation.
Funding
The author(s) declare that no financial support was received for the research and/or publication of this article.
Conflict of interest
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
Generative AI statement
The authors declare that no Generative AI was used in the creation of this manuscript.
Any alternative text (alt text) provided alongside figures in this article has been generated by Frontiers with the support of artificial intelligence and reasonable efforts have been made to ensure accuracy, including review by the authors wherever possible. If you identify any issues, please contact us.
Publisher’s note
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
Supplementary material
The Supplementary Material for this article can be found online at: https://www.frontiersin.org/articles/10.3389/fmed.2025.1630632/full#supplementary-material
Supplementary Figure 1 | Dermoscopic features of common male external genital skin diseases. (a) Extramammary Paget disease: Erythematous background with dotted and glomerular vessels interspersed with milky-white structureless areas with scales. (b) Bowenoid papulosis: Hyperkeratotic surface displaying slate-gray pigmentation in annular/granular patterns. (c) Lichen sclerosus: Porcelain-white structureless areas with “cigarette-paper” wrinkling, surrounded by arborizing telangiectasia and polymorphic vessels. (d) Lichen planus: Violaceous background, bright white linear structures, peripheral brown-gray peppering, and short linear vessels. (e) Genital warts: Papillomatous projections with central dotted/looped vessels encircled by whitish halos, small hemorrhagic spots, and a few white scales. (f) Squamous cell carcinoma: Erythematous background with disorganized irregular dotted/globular vessels, amidst focal bright white streaks, hemorrhagic crusts, and slightly scales.
Supplementary Figure 2 | Histopathological features of common male external genital skin diseases (haematoxylin-eosin stain, × 10). (a) Extramammary Paget disease: Intraepidermal proliferation of multiple large pale-staining Paget cells with abundant cytoplasm, arranged singly or in nests. (b) Bowenoid papulosis: Full-thickness epidermal dysplasia with multiple pleomorphic keratinocytes, atypical mitoses, and dilated papillary dermal capillaries. (c) Lichen sclerosus: Epidermal atrophy with basal vacuolization, hyalinization accompanied melanin incontinence in the papillary dermis, and perivascular lymphocytic infiltration below. (d) Lichen planus: Wedge-shaped hypergranulosis, basal layer liquefactive degeneration, and band-like lymphohistiocytic infiltrate obscuring the dermoepidermal junction. (e) Genital warts: Acanthosis with papillomatosis, hyperkeratosis, and koilocytic atypia, dilation of superficial dermal vessels and chronic inflammatory infiltration in the upper dermis. (f) Squamous cell carcinoma in situ: Full-thickness epidermal atypia with disordered maturation, dyskeratotic cells, and mitotic figures above the basal layer.
References
1. Saraswat PK, Garg A, Mishra D, Garg S. A study of pattern of nonvenereal genital dermatoses of male attending skin OPD at a tertiary care center. Indian J Sex Transm Dis AIDS. (2014) 35:129–34.
2. Acharya KM, Ranpara H, Sakhia JJ, Kaur C. A study of 200 cases of genital lesions of non-venereal origin. Indian J Dermatol Venereol Leprol. (1998) 64:68–70.
3. Khoo LS, Cheong WK. Common genital dermatoses in male patients attending a public sexually transmitted disease clinic in Singapore. Ann Acad Med Singap. (1995) 24:505–9.
4. Ishizuki S, Nakamura Y. Extramammary Paget’s disease: diagnosis, pathogenesis, and treatment with focus on recent developments. Curr Oncol. (2021) 28:2969–86.
5. Kang Z, Zhang Q, Zhang Q, Li X, Hu T, Xu X, et al. Clinical and pathological characteristics of extramammary Paget’s disease: report of 246 Chinese male patients. Int J Clin Exp Pathol. (2015) 8:13233–40.
6. Mazzoni D, Winkle D, Pool L, Hall A, Muir J. Genital premalignant and malignant diseases: a retrospective study of male genital skin biopsies. Int J Dermatol. (2021) 60:712–6.
7. Ciccarese G, Facciorusso A, Mastrolonardo M, Herzum A, Parodi A, Drago F. Atypical manifestations of syphilis: a 10-year retrospective study. J Clin Med. (2024) 13:1603.
8. Moris V, Laine E, Khan S, See LA. Unusual syphilis manifestation: from breast implant rupture to systemic erythroderma. IDCases. (2025) 39:e02170.
9. Seong SH, Jung JH, Kwon DI, Lee KH, Park JB, Baek JW, et al. Dermoscopic findings of genital keratotic lesions: bowenoid papulosis, seborrheic keratosis, and condyloma acuminatum. Photodiagnosis Photodyn Ther. (2021) 36:102448.
10. Chamli A, Zaouak A. Bowenoid Papulosis. In: StatPearls. Treasure Island (FL): StatPearls Publishing (2025).
11. Panou E, Panagou E, Foley C, Kravvas G, Watchorn R, Alnajjar H, et al. Male genital lichen sclerosus associated with urological interventions and microincontinence: a case series of 21 patients. Clin Exp Dermatol. (2022) 47:107–9.
12. Kravvas G, Shim TN, Doiron PR, Freeman A, Jameson C, Minhas S, et al. The diagnosis and management of male genital lichen sclerosus: a retrospective review of 301 patients. J Eur Acad Dermatol Venereol. (2018) 32:91–5.
13. Yao XJ, Zhang TD. Psoriasis localized to the glans penis in a 37-year-old man. CMAJ. (2018) 190:E747.
14. Zubrzycki N, Leow LJA. Case of male genital psoriasis without involvement of the glans penis. Case Rep Dermatol. (2022) 14:66–70.
15. Licata G, Tancredi V, Giorgio CM, Arisi M, Damiani L, Benvenuto P, et al. Pigmented nonmelanoma skin cancers of the genital area: a diagnostic and therapeutic challenge - monocentric experience and review of the literature. Int J Dermatol. (2024) 63:1477–83.
16. Lacarrubba F, Borghi A, Verzì AE, Corazza M, Stinco G, Micali G. Dermoscopy of genital diseases: a review. J Eur Acad Dermatol Venereol. (2020) 34:2198–207.
17. Guitera P, Scolyer RA, Gill M, Akita H, Arima M, Yokoyama Y, et al. Reflectance confocal microscopy for diagnosis of mammary and extramammary Paget’s disease. J Eur Acad Dermatol Venereol. (2013) 27:e24–9.
18. Cozma EC, Celarel AM, Stoenica IV, Lupu M, Banciu LM, Voiculescu VM, et al. Correlations between histopathological and confocal reflectance microscopy aspects in a patient with bowenoid papulosis. Diagnostics (Basel). (2023) 13:1531.
19. Kantere D, Neittaanmäki N, Maltese K, Larkö AMW, Tunbäck P. Exploring reflectance confocal microscopy as a non-invasive diagnostic tool for genital lichen sclerosus. Exp Ther Med. (2022) 23:410.
20. Chen L, Wang Y, Wang J, Qin B, Li Q. Male genital lichen sclerosus in a pediatric case: a focus on the reflectance confocal microscopy presentation. Skin Res Technol. (2023) 29:e13304.
21. Wang ZY, Fei WM, Li CX, Cui Y. Comparison of dermoscopy and reflectance confocal microscopy accuracy for the diagnosis of psoriasis and lichen planus. Skin Res Technol. (2022) 28:480–6.
22. Cinotti E, Barbarossa L, Cortonesi G, Lamberti A, La Marca F, Tognetti L, et al. Non-invasive imaging for the diagnosis of genital warts and their imitators. J Clin Med. (2024) 13:1345.
Keywords: male external genitalia, skin diseases, histopathology, dermoscopy, diagnostic discrepancy
Citation: Qian Y-T, Ma X, Zhang J-Y, Liu J-W, Fang K and Ma D-L (2025) Male external genital skin disorders: a retrospective analysis from a tertiary hospital in China. Front. Med. 12:1630632. doi: 10.3389/fmed.2025.1630632
Received: 18 May 2025; Revised: 05 November 2025; Accepted: 10 November 2025;
Published: 03 December 2025.
Edited by:
Francesco Borgia, University of Messina, ItalyReviewed by:
Mohammed Abu El-Hamd, Sohag University, EgyptGiulia Ciccarese, San Martino Hospital (IRCCS), Italy
Copyright © 2025 Qian, Ma, Zhang, Liu, Fang and Ma. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Dong-Lai Ma, bWRvbmdsYWlAc29odS5jb20=
 Yue-Tong Qian
Yue-Tong Qian Xiao Ma
Xiao Ma Jia-Wei Liu
Jia-Wei Liu Dong-Lai Ma
Dong-Lai Ma