- 1Department of Emergency Medicine, The People’s Hospital of Atushi City, Atushi, China
- 2Department of Urology Surgery, The People’s Hospital of Atushi City, Atushi, China
- 3Department of Cardiovascular Medicine, The People’s Hospital of Atushi City, Atushi, China
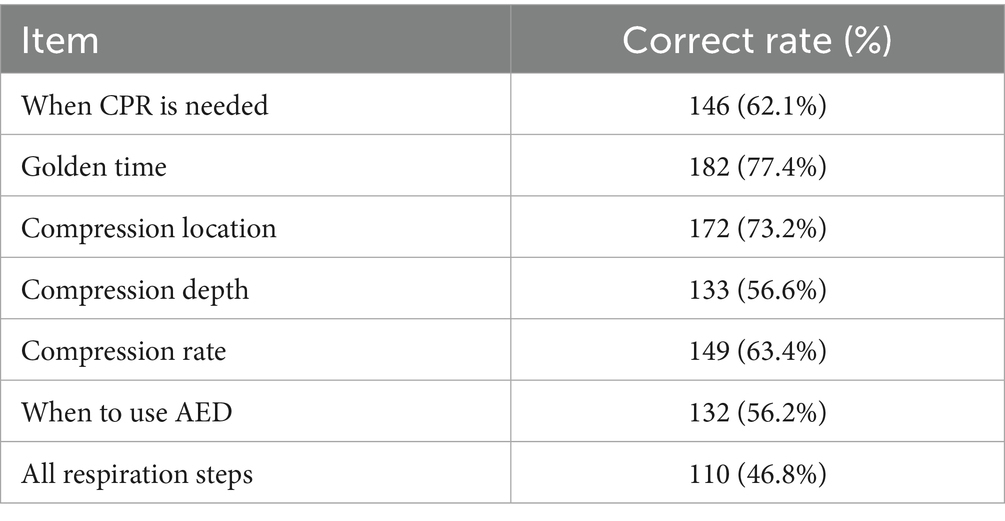
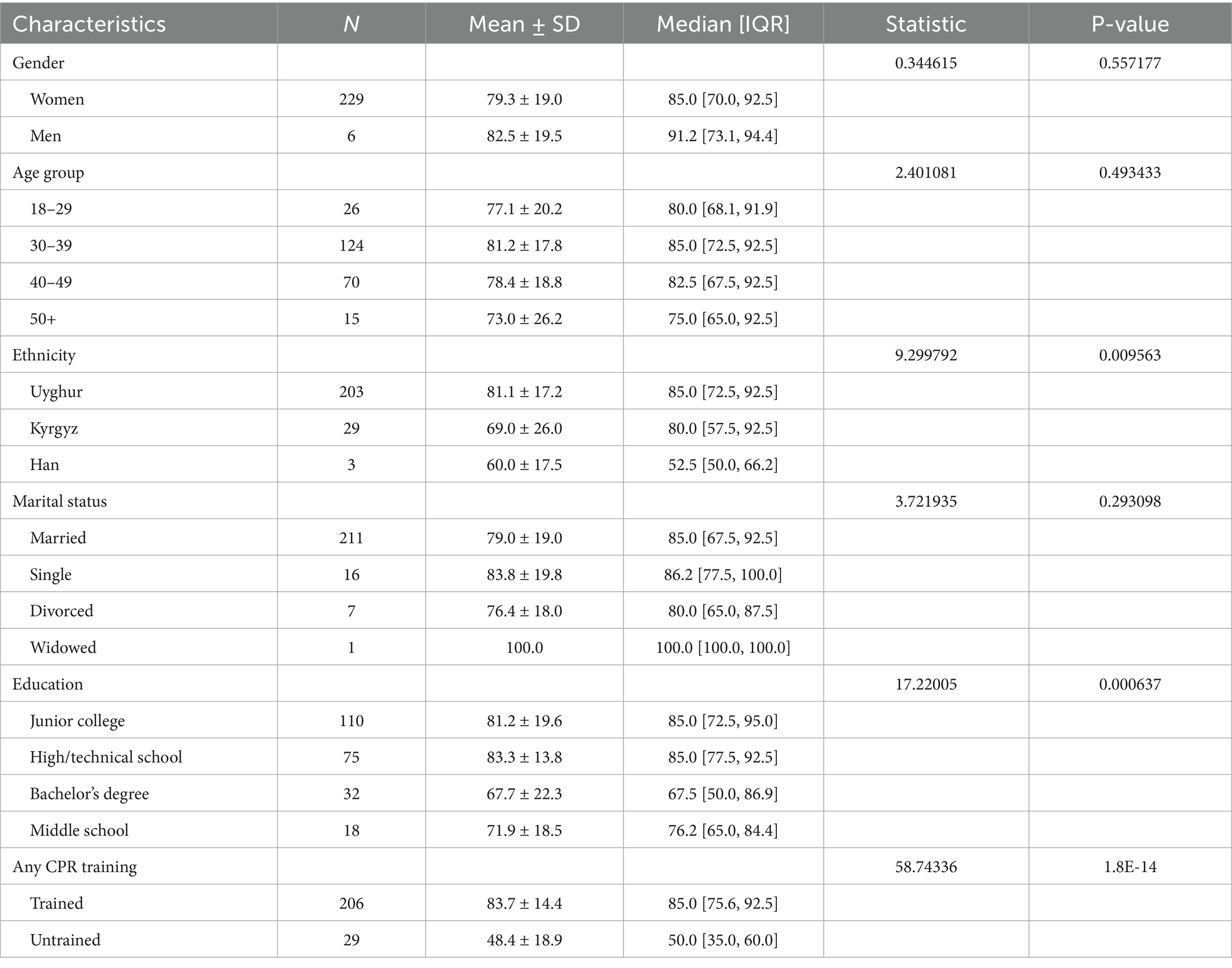
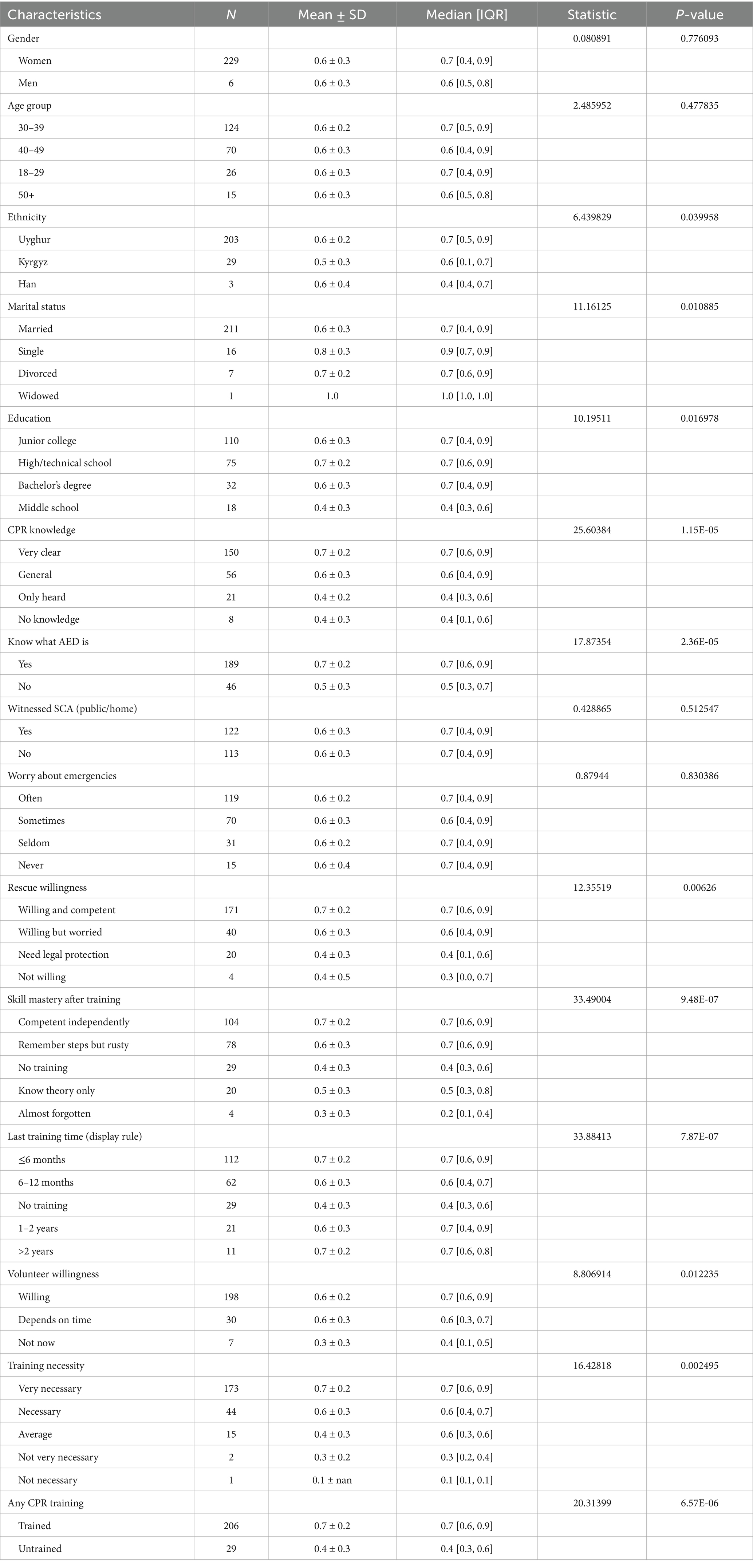
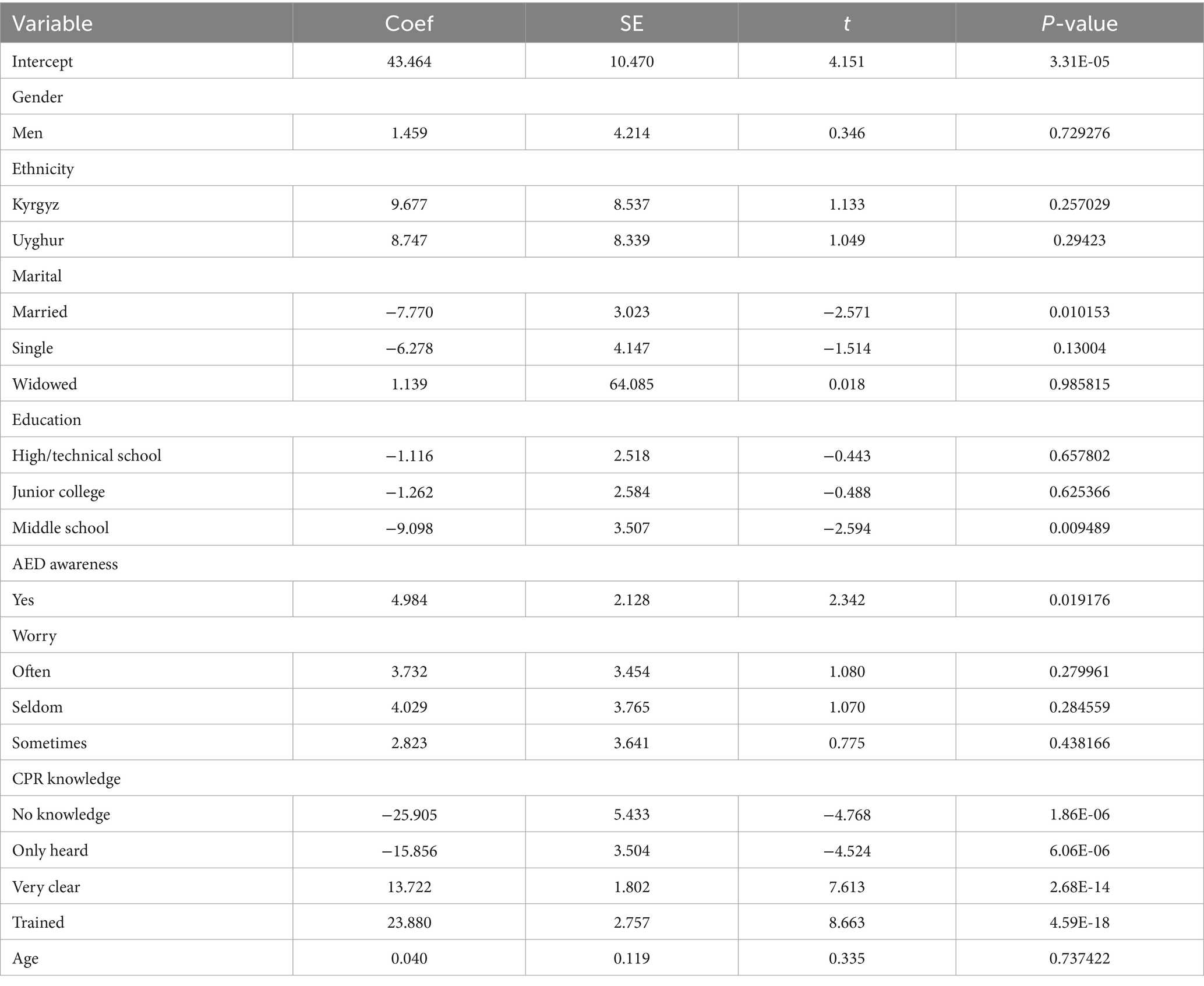
Out-of-hospital cardiac arrest (OHCA) survival depends on rapid recognition, high-quality chest compressions, and early use of an automated external defibrillator (AED). Township household health education instructors in rural China are grassroots healthcare workers and are often the first reachable trained personnel during emergencies; however, their readiness to perform cardiopulmonary resuscitation (CPR) is undercharacterized. We conducted a cross-sectional analysis of a programmatic survey involving 235 instructors in Xinjiang, China. The survey instrument captured demographics, training exposure and its recency, AED awareness, item-level CPR knowledge, rescue willingness, and preferences. We derived a composite readiness score (0–100) and a strict overall accuracy score by averaging seven item-level correctness indicators. Group differences were assessed using chi-squared, Fisher’s exact, or Kruskal–Wallis tests, with false discovery rate (FDR)-adjusted post hoc comparisons. Readiness correlates were examined using ordinary least squares (OLS) regression. The participants were predominantly women (97.4%) with a mean age of 37.4 ± 7.1 years; 86.4% were Uyghur, 12.3% Kyrgyz, and 1.3% Han. In total, 87.7% of the participants received CPR training, and 80.4% reported AED awareness. The mean readiness score was 79.4 ± 19.0, and the strict overall accuracy was 62.2 ± 25.6%. Item-level correct rates were as follows: “golden time,” 77.4%; compression location, 73.2%; compression rate, 63.4%; indication, 62.1%; compression depth, 56.6%; AED timing, 56.2%; and all respiration steps, 46.8%. The trained participants showed higher readiness (83.7 ± 14.4 vs. 48.4 ± 18.9; p < 0.0001) and accuracy (0.65 vs. 0.42; p < 0.0001) compared to the untrained participants. Readiness varied by ethnicity (p = 0.0096; Uyghur > Kyrgyz, FDR = 0.050) and education (p = 0.00064). In the OLS model, having any prior training (+23.9; p < 0.0001), self-rated “very clear” knowledge (+13.7; p < 0.0001), and AED awareness (+5.0; p = 0.019) independently increased readiness, whereas middle-school education (−9.10; p = 0.0095) and married status (−7.77; p = 0.010) decreased readiness. The findings indicate generally favorable readiness with identifiable gaps, supporting low-dose, high-frequency, bilingual, hands-on refresher training tailored to rural Xinjiang.
Introduction
Out-of-hospital cardiac arrest (OHCA) represents a universally time-critical emergency where survival depends on rapid recognition, high-quality cardiopulmonary resuscitation (CPR), and early defibrillation (1–8). Despite advances in resuscitation science, substantial rural–urban disparities in OHCA survival persist worldwide (9–13). These disparities reflect not only differences in emergency medical service (EMS) response times—which can exceed 30 min in remote areas compared to 8–10 min in urban centers—but also gaps in bystander CPR rates and public-access defibrillator availability. Evidence from population studies and meta-analyses across multiple continents demonstrates that bystander CPR and timely automated external defibrillator (AED) use substantially improve neurological outcomes and survival. However, the implementation of these evidence-based interventions remains inconsistent in resource-limited and geographically isolated settings (14–26).
In rural and remote settings around the world, formal EMS systems face significant geographic and temporal barriers. When ambulance transport times exceed the critical 4–8-min window for effective resuscitation, community health workers (CHWs) become de facto first responders. These frontline personnel—known variously as Accredited Social Health Activists (ASHAs) in India (27–29), Health Extension Workers in Ethiopia (30, 31), Community Health Agents in Brazil (32), and village doctors in China—provide primary health education, chronic disease management, and emergency response in underserved populations. Current resuscitation guidelines emphasize comprehensive, customized CPR training; however, empirical data characterizing the preparedness of CHWs to recognize and manage cardiac arrest remain remarkably sparse, particularly in multiethnic and multilingual regions where cultural and linguistic factors may compound implementation challenges (33–35).
China’s tiered rural health system offers a valuable perspective for examining these global challenges. Township household health education instructors—community-based health educators who conduct home visits for chronic disease management and health promotion, functionally equivalent to CHWs in other contexts—represent the most accessible trained personnel during medical emergencies in villages that are often located hours away from the nearest hospital.
The Xinjiang Uyghur Autonomous Region in northwestern China exemplifies the severity of these challenges. Spanning 1.66 million km2, Xinjiang is characterized by vast distances, sparse population density (15 persons/km2 versus the national average of 145/km2), and profound ethnic and linguistic diversity. The population comprises Uyghur (45%), Han Chinese (42%), and Kyrgyz, along with other minority groups (13%). As a result, health education materials are needed in Uyghur, Kyrgyz, and Mandarin Chinese. In Atushi, a prefecture in southern Xinjiang bordering Kyrgyzstan, some villages are located 3–5 h by road from the nearest county hospital, and township health centers may employ only approximately 30 clinicians to serve areas with 10,000 residents (36, 37). Emergency response times routinely exceed 30 min, making township health education instructors the most readily available trained personnel during the critical first minutes following a cardiac arrest.
Therefore, we conducted this cross-sectional analysis with three objectives: (1) to characterize baseline CPR knowledge and readiness among township household health education instructors in rural Xinjiang; (2) to identify demographic and training-related factors associated with knowledge gaps; and (3) to inform the development of targeted, culturally appropriate CPR training programs for this workforce. In addition to characterizing this specific workforce, our findings may guide CPR training strategies for community health workers in other geographic and cultural contexts where similar barriers to emergency preparedness exist.
Materials and methods
Study design and setting
We conducted a cross-sectional analysis of a programmatic survey administered to township household health education instructors in Atushi, Xinjiang, China. These instructors are employed by township health centers or community health service centers and supervised by the public health department. Their primary responsibilities mirror those of CHWs globally: conducting household visits to provide health education on chronic disease management (hypertension, diabetes), infectious disease prevention, and emergency preparedness. Community members access services through instructor-initiated household visits or by seeking care at health centers. In medical emergencies, instructors are often contacted by community members before or concurrently with calls to formal emergency services, making them de facto first responders.
Participants and data collection
Eligible participants included all active township household health education instructors working in Atushi. The sample size was determined using a complete enumeration approach: all 235 active instructors in the region at the time of the survey were invited, and all consented, providing a census that eliminates sampling error within the defined population and ensures adequate power to detect effect sizes in group comparisons. The survey instrument was developed in Mandarin Chinese—the language of health education delivery in the region—although participants’ primary languages varied (Uyghur, Kyrgyz, or Chinese). Response options were aligned with international CPR guideline content, and responses were subsequently mapped to English labels for analysis and reporting.
The instrument collected information on demographics (gender, age, ethnicity, marital status, and education), training exposure indicators (any CPR training and recency), AED awareness, experience witnessing cardiac arrest, worry about emergencies, rescue willingness, perceived training necessity, and preferences for training formats and methods.
Measures and operational definitions
The survey instrument was developed using a multistage process based on the 2020 American Heart Association CPR guidelines and adapted for the Chinese context in consultation with emergency medicine specialists and public health educators. The Chinese-language instrument was tested through cognitive interviews with five township health workers to assess comprehension and cultural appropriateness, with minor wording adjustments made based on feedback. Although formal psychometric validation was not conducted due to resource constraints, content validity was ensured through expert review and alignment with international guidelines.
CPR knowledge items mirrored core adult basic life support concepts, including indications for initiating CPR, the “golden time” for intervention, chest-compression location, chest-compression depth, chest-compression rate, timing of AED use, and a multi-select list of artificial respiration steps. Single-choice items were scored as correct if they matched guideline-concordant responses. The respiration sequence was scored in two ways: a strict “all-correct” indicator and a partial score ranging from 0 to 1, proportional to the number of correct steps selected.
Training exposure was dichotomized as “Trained” if the respondents reported either formal training (e.g., hospital or Red Cross) or self-study via videos/books; otherwise, they were classified as “Untrained.” Training recency was categorized as “≤6 months,” “6–12 months,” “1–2 years,” and “>2 years,” with “No training” assigned if the respondent reported no training or did not report a training time.
We derived two summary outcomes. The strict overall knowledge accuracy score was the mean of seven item-level correctness indicators, covering indications, golden time, compression location, compression depth, compression rate, AED timing, and respiration steps. The composite readiness score (0–100) integrated self-rated CPR knowledge (maximum 30 points), training exposure (maximum 20 points), correctness on four key knowledge items (maximum 30 points), and rescue willingness (maximum 20 points).
Statistical analysis
Categorical variables were summarized using counts and percentages, while continuous variables were described with means and standard deviations and with medians and interquartile ranges as supplementary descriptors. Baseline comparisons between the trained and untrained participants were performed using chi-squared tests for categorical variables, Fisher’s exact test for sparse 2 × 2 tables, and the Kruskal–Wallis test for continuous variables. To assess group differences in readiness and strict overall accuracy for single-choice variables, the Kruskal–Wallis test was used and, when significant, the pairwise Mann–Whitney U test with Benjamini–Hochberg false discovery rate (FDR) adjustment was conducted. Item-level accuracy across subgroups (training status, gender, ethnicity, age group, education, and marital status) was compared using chi-squared or Fisher’s exact tests (Supplementary Table 1).
To identify independent correlates of readiness, an ordinary least squares (OLS) regression with HC3 robust standard errors was used. Predictors included training status, age, gender, ethnicity, marital status, education, AED awareness, worry about emergencies, and self-rated CPR knowledge. Statistical significance was defined as a two-sided p-value of < 0.05. Analyses were conducted using Python 3.9.
Results
Participant characteristics
We analyzed 235 township household health education instructors (Table 1). The cohort was predominantly female (N = 229, 97.4%), with a mean age of 37.4 ± 7.1 years. The majority of the participants identified as Uyghur (N = 203, 86.4%), with smaller proportions identifying as Kyrgyz (N = 29, 12.3%) and Han Chinese (N = 3, 1.3%). The majority of the participants were married (N = 211, 89.8%), and educational attainment was primarily junior college (N = 110, 46.8%) or high/technical school (N = 75, 31.9%), with 13.6% holding a bachelor’s degree and 7.7% completing middle-school education. These characteristics reflect the staffing composition of village-level public health personnel in rural Xinjiang.
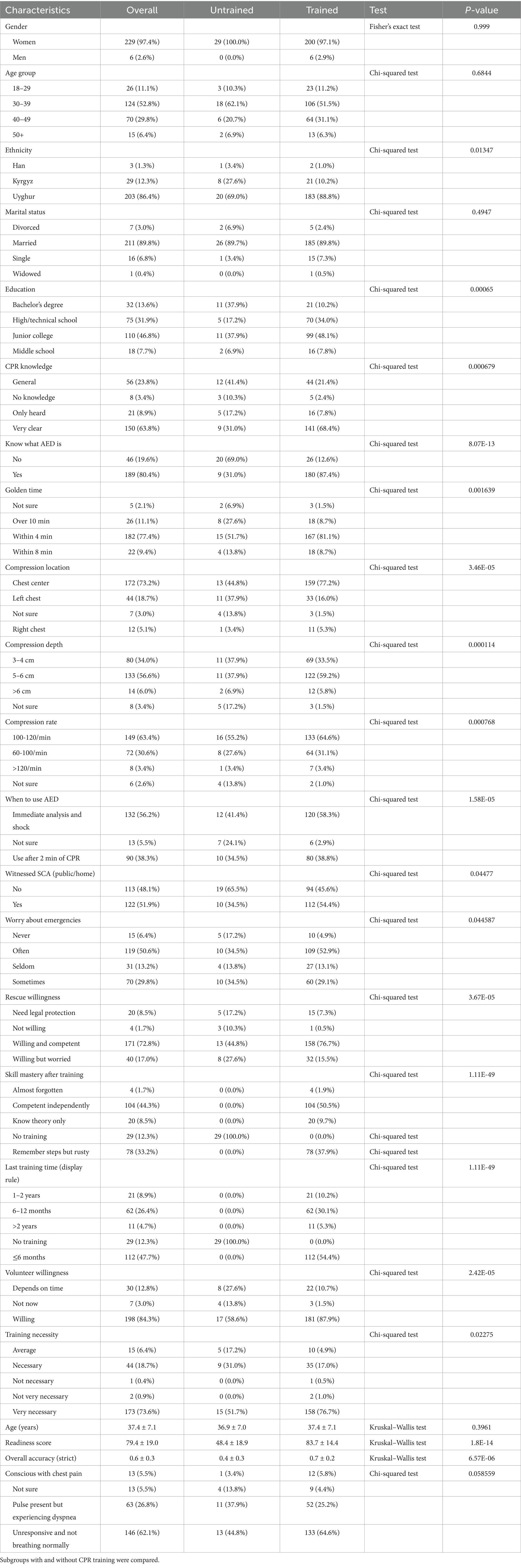
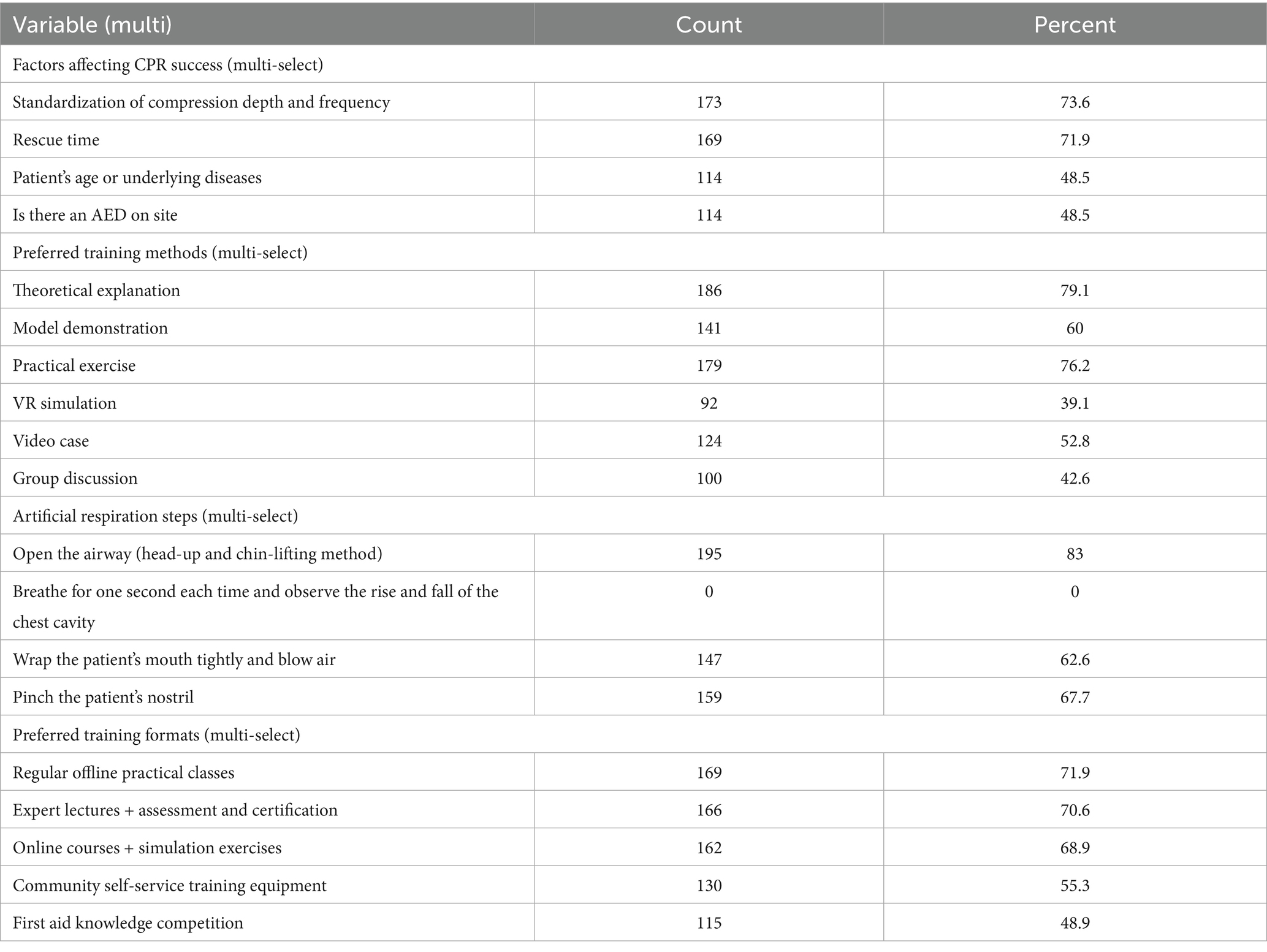
Table 1. Demographic information of the participants and the characteristics of the questionnaire (N = 235).
The proportion of CPR training was high: 87.7% reported any CPR training and 75.3% reported formal training (Table 1). Training recency was favorable, with 47.7% trained within the past 6 months, 26.4% within 6–12 months, 8.9% within 1–2 years, and 4.7% more than 2 years prior; 12.3% reported no training. AED awareness was reported by 80.4% of the respondents. The majority of the participants (N = 122, 51.9%) had witnessed a cardiac arrest in a public setting or at home. Rescue willingness was high, with 72.8% indicating they were willing and felt competent to act, 17.0% willing but worried, 8.5% willing only with legal protection, and 1.7% not willing. The majority of respondents (N = 173, 73.6%) considered CPR training “very necessary,” with 18.7% rating it “necessary.”
Overall readiness and knowledge performance
The composite readiness score averaged 79.4 ± 19.0, with a median of 85.0 and an interquartile range of 70.0 to 92.5 (Table 1, Figure 1A). The strict overall knowledge accuracy score averaged 62.2 ± 25.6%, with a median of 70% and an interquartile range of 40%–90% (Table 2). Correct identification of the “golden time” (77.4%) and adult compression location (73.2%) was relatively strong. Correct selection of the compression rate was 63.4% and of the indication to initiate CPR was 62.1%. Lower correct rates were observed for compression depth (56.6%) and AED timing (56.2%). The strict all-correct score for artificial-respiration steps was 46.8%.
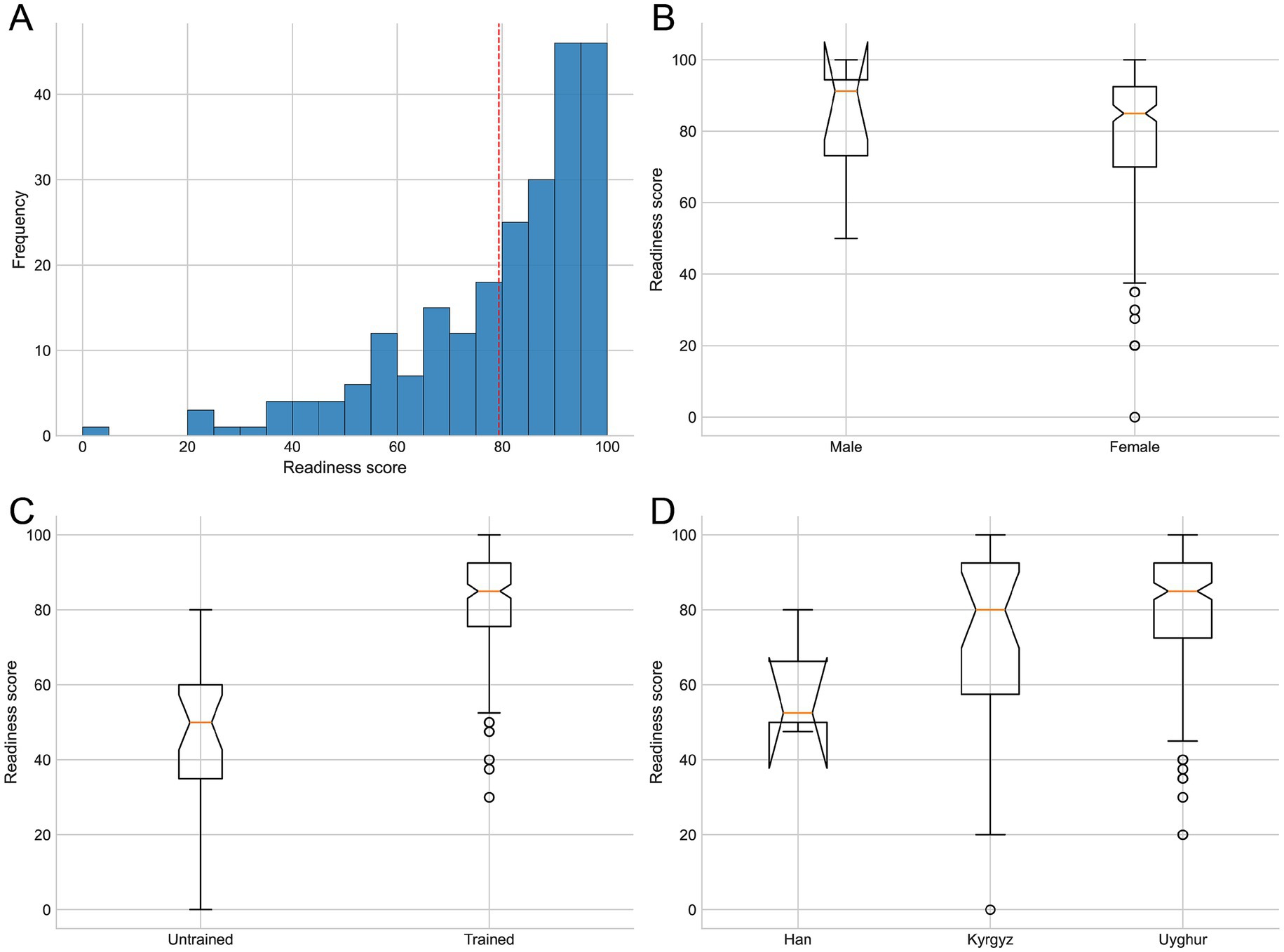
Figure 1. Statistical analysis of CPR readiness scores. (A) Overall distribution (histogram). (B) Group comparisons by gender. (C) Group comparisons by training status. (D) Group comparisons by ethnicity.
Comparisons by training status
The trained participants outperformed the untrained peers across primary outcomes (Table 1). The readiness score was 83.7 ± 14.4 among the trained respondents versus 48.4 ± 18.9 among the untrained respondents, representing a highly significant difference by the Kruskal–Wallis test (p < 0.0001). The strict overall knowledge accuracy score was correspondingly higher among the trained respondents than among the untrained respondents (0.65 vs. 0.42; p < 0.0001). At the item level, training status was associated with higher correct rates for several knowledge items. Correct recognition of the “golden time” was 81.1% among the trained participants compared to 51.7% among the untrained participants (chi-squared, p = 0.00040). Correct identification of the compression location was 77.2% versus 44.8% (p = 0.00023). Correct indication for initiating CPR was 64.6% versus 44.8% (p = 0.040), compression depth 59.2% versus 37.9% (p = 0.030), and all-correct respiration steps 51.0% versus 17.2% (p = 0.00065). Differences between the trained and untrained participants were smaller for the compression rate (64.6% vs. 55.2%; p = 0.326) and AED timing (58.3% vs. 41.4%; p = 0.086). Training recency showed a graded association: readiness was highest among those trained within 6 months (87.2 ± 12.5) and lowest in the no-training group (48.4 ± 18.9), with an overall p-value of < 0.0001 (Kruskal–Wallis). Strict overall accuracy also differed by training recency (p < 0.0001).
Group differences across demographic subgroups
Readiness varied by ethnicity (Kruskal–Wallis, p = 0.0096), with pairwise Mann–Whitney contrasts demonstrating higher readiness among the Uyghur respondents than the Kyrgyz respondents (mean 81.1 vs. 69.0; raw p = 0.0167; false discovery rate-adjusted p = 0.050) (Tables 3, 4, Figure 1). Although the Han respondents had a small sample size (n = 3) and hence imprecise estimates, their mean readiness was 60.0 ± 17.5. Strict overall accuracy also differed by ethnicity (p = 0.03996); pairwise comparisons showed that the Uyghur respondents outperformed the Kyrgyz respondents (FDR-adjusted p = 0.036). Education was associated with readiness (p = 0.0006368) and strict overall accuracy (p = 0.01698), with lower scores observed for the participants with a middle-school education compared to the junior college and high/technical groups. In contrast, neither gender nor age group was associated with readiness or strict overall accuracy.
Multivariable correlates of readiness
In OLS regression, independent correlates of readiness included training, self-rated knowledge, AED awareness, education, and marital status (Table 5). Any CPR training was associated with a 23.88-point increase in readiness (p < 0.0001) after adjusting for covariates. Self-rated “very clear” CPR knowledge was associated with a 13.72-point increase (p < 0.0001), whereas “only heard” and “no knowledge” categories were associated with 15.86- and 25.90-point decreases, respectively (both p < 0.0001), relative to reference categories. AED awareness (Yes) was associated with a 4.98-point increase in readiness (p = 0.019). Middle-school education was associated with a 9.10-point decrease relative to a bachelor’s degree (p = 0.0095). Married status was associated with a 7.77-point decrease relative to other categories (p = 0.010). Gender, age, and ethnicity were not significant after adjustment, indicating that the primary drivers of readiness were training exposure and knowledge-related factors, with education and marital status identifying subgroups potentially in need of additional support.
Training preferences and perceived helpful methods
Training preferences aligned with contemporary resuscitation education approaches. The respondents favored regular in-person practical sessions (71.9%), expert lectures with certification (70.6%), and online courses with simulated practice (68.9%), with additional interest in community self-training equipment (55.3%) and emergency knowledge competitions (48.9%) (Table 6). Perceived helpful training methods included theoretical instruction (79.1%), hands-on practice (76.2%), model demonstrations (60.0%), VR simulation (39.1%), video case studies (52.8%), and small-group discussions (42.6%).
Discussion
In this cross-sectional analysis of 235 township household health education instructors in Xinjiang, China, we found generally favorable CPR readiness and knowledge in the context of high training penetration, alongside clear, targeted gaps in procedural knowledge central to high-quality basic life support. These findings highlight a global challenge: bridging the “know-do gap” between international resuscitation guidelines and their implementation among frontline community health workers in resource-limited, culturally diverse settings.
Our finding that 87.7% of township household health education instructors had received any CPR training represents substantially higher coverage than previously reported for the general public in Chinese urban areas (6%–25.6%) (38). However, 12.4% of the trained participants relied on self-study via videos rather than hands-on practice with feedback, which lacks the deliberate practice necessary for procedural skill consolidation—a limitation observed across diverse CHW programs globally. Skill decay in CPR is well-documented internationally: psychomotor competencies deteriorate within 3–6 months without reinforcement, regardless of geographic or cultural context (39–41). Our finding that readiness decreased from 87.2 points among the participants trained ≤6 months to 48.4 points among the untrained participants aligns with this international evidence and underscores the need for spaced, high-frequency refresher training.
The workforce’s stated preferences for regular practical sessions (71.9%), expert-led certification (70.6%), and simulation-based VR (68.9%) align with international evidence on effective CHW training. Systematic reviews demonstrate that mastery learning approaches—where learners practice skills to a predefined competency threshold with deliberate feedback—yield superior retention compared to time-based training, regardless of setting (42). Low-dose, high-frequency training models, successfully piloted with community health agents in Ethiopia and Rwanda, maintain skill proficiency while minimizing workforce disruption (43–46).
Lower readiness among the Kyrgyz participants versus the Uyghur participants highlights the role of cultural and linguistic factors. Although all participants are proficient in Chinese, technical terminology and rapid instructions during demonstrations may impose additional cognitive load for those whose first language is Uyghur or Kyrgyz, leading to misunderstandings of critical parameters such as compression depth or rate ranges. Cultural norms around gender and physical contact may also affect training engagement and willingness to act: female instructors (97.4% of our sample) may face constraints when considering CPR delivery to male patients in conservative communities.
Systematic reviews and population studies have long shown the survival benefits of early bystander CPR and AED use (47–49), and guidelines emphasize compressions-first approaches, early defibrillation, and community training that is tailored to local contexts (50, 51). Educational science now favors mastery learning, debriefing, and spaced practice with feedback, strategies that are feasible at township or community health service centers (51, 52).
This study has several limitations. First, the cross-sectional design precludes causal inference. Second, self-reported knowledge may be subject to recall and social desirability bias; objective skill assessment using standardized manikin scenarios would provide more rigorous data. Third, the study population was drawn from a single region and had a highly skewed gender distribution. The extreme gender imbalance (97.4% women) reflects the occupational composition of township household health education instructors in this region, where women are preferentially recruited for roles involving household visits due to cultural norms around gender and home access. Fourth, we did not measure actual emergency response performance or patient outcomes. Fifth, the survey was administered in Chinese only, which may have disadvantaged participants whose primary language is Uyghur or Kyrgyz, despite their required Chinese proficiency. Finally, residual confounding from unmeasured variables cannot be ruled out.
Conclusion
Among township household health education instructors in Xinjiang, China, CPR readiness and knowledge were generally favorable, although clear gaps remained in ventilation sequencing, compression depth, and AED timing. To translate these findings into improved emergency preparedness, we recommend the following: (1) mandatory quarterly low-dose, high-frequency refresher sessions with feedback-enabled manikins; (2) development and dissemination of bilingual (Uyghur, Kyrgyz, Chinese) training modules with locally relevant scenarios and cultural adaptations; and (3) expansion of AED access, coupled with integration of quarterly AED drills into routine practice. It is also recommended to equip each township health center with AEDs co-located with training manikins and advocate for public AED placement in high-traffic community venues with multilingual signage. These evidence-based strategies can strengthen the capacity of rural grassroots healthcare workers to serve as effective first responders during cardiac emergencies, ultimately reducing rural–urban disparities in OHCA survival.
Data availability statement
The original contributions presented in the study are included in the article/Supplementary material, further inquiries can be directed to the corresponding author.
Ethics statement
The studies involving humans were approved by the Medical Ethics Committee of the People’s Hospital of Atushi City. The studies were conducted in accordance with the local legislation and institutional requirements. The participants provided their written informed consent to participate in this study.
Author contributions
JM: Formal analysis, Writing – review & editing, Project administration, Writing – original draft, Data curation, Investigation, Conceptualization. LK: Methodology, Data curation, Resources, Software, Writing – original draft. XZ: Software, Writing – original draft, Methodology, Validation, Resources. QT: Writing – original draft, Resources, Software, Data curation, Visualization, Validation. SL: Validation, Writing – original draft, Supervision, Software, Data curation, Visualization. WZ: Conceptualization, Writing – review & editing, Investigation, Writing – original draft, Project administration.
Funding
The author(s) declare that no financial support was received for the research and/or publication of this article.
Conflict of interest
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
Generative AI statement
The authors declare that no Gen AI was used in the creation of this manuscript.
Any alternative text (alt text) provided alongside figures in this article has been generated by Frontiers with the support of artificial intelligence and reasonable efforts have been made to ensure accuracy, including review by the authors wherever possible. If you identify any issues, please contact us.
Publisher’s note
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
Supplementary material
The Supplementary material for this article can be found online at: https://www.frontiersin.org/articles/10.3389/fmed.2025.1697798/full#supplementary-material
References
1. Abate, SM, Nega, S, Basu, B, Mesfin, R, and Tadesse, M. Global burden of out-of-hospital cardiac arrest in children: a systematic review, meta-analysis, and meta-regression. Pediatr Res. (2023) 94:423–33. doi: 10.1038/s41390-022-02462-5
2. Kumar, A, Avishay, DM, Jones, CR, Shaikh, JD, Kaur, R, Aljadah, M, et al. Sudden cardiac death: epidemiology, pathogenesis and management. Rev Cardiovasc Med. (2021) 22:147–58. doi: 10.31083/j.rcm.2021.01.207
3. Sawyer, KN, Camp-Rogers, TR, Kotini-Shah, P, del Rios, M, Gossip, MR, Moitra, VK, et al. Sudden cardiac arrest survivorship: a scientific statement from the American Heart Association. Circulation. (2020) 141:e654–85. doi: 10.1161/CIR.0000000000000747
4. Al-Khatib, SM, Stevenson, WG, Ackerman, MJ, Bryant, WJ, Callans, DJ, Curtis, AB, et al. 2017 AHA/ACC/HRS guideline for management of patients with ventricular arrhythmias and the prevention of sudden cardiac death: a report of the American College of Cardiology/American Heart Association task force on clinical practice guidelines and the Heart Rhythm Society. Heart Rhythm. (2018) 15:e73–e189. doi: 10.1016/j.hrthm.2017.10.036
5. Myat, A, Song, KJ, and Rea, T. Out-of-hospital cardiac arrest: current concepts. Lancet. (2018) 391:970–9. doi: 10.1016/S0140-6736(18)30472-0
6. Rao, P, and Kern, KB. Improving community survival rates from out-of-hospital cardiac arrest. Curr Cardiol Rev. (2018) 14:79–84. doi: 10.2174/1573403X14666180507160555
7. Riva, G, and Hollenberg, J. Different forms of bystander cardiopulmonary resuscitation in out-of-hospital cardiac arrest. J Intern Med. (2021) 290:57–72. doi: 10.1111/joim.13260
8. Lee, OH, Heo, SJ, Bae, SA, Kim, MH, Park, JW, Kim, M, et al. Impact of emergency medical services call-to-hospital arrival time on outcomes of cardiac arrest: a Nationwide prospective cohort. Mayo Clin Proc. (2025) 100:1719–30. doi: 10.1016/j.mayocp.2025.06.025
9. Hsu, YC, Wu, WT, Huang, JB, Lee, KH, and Cheng, FJ. Association between prehospital prognostic factors and out-of-hospital cardiac arrest: effect of rural-urban disparities. Am J Emerg Med. (2021) 46:456–61. doi: 10.1016/j.ajem.2020.10.054
10. Hart, J, Vakkalanka, JP, Okoro, U, Mohr, NM, and Ahmed, A. Rural out-of-hospital cardiac arrest patients more likely to receive bystander CPR: a retrospective cohort study. Prehosp Emerg Care. (2025) 29:1104–10. doi: 10.1080/10903127.2024.2443478
11. Cheek, L, Schmicker, RH, Crowe, R, Goren, E, West, A, McMullan, J, et al. Rurality and area deprivation and outcomes after out-of-hospital cardiac arrest. JAMA Netw Open. (2025) 8:e253435. doi: 10.1001/jamanetworkopen.2025.3435
12. Brown, TP, Booth, S, Hawkes, CA, Soar, J, Mark, J, Mapstone, J, et al. Characteristics of neighbourhoods with high incidence of out-of-hospital cardiac arrest and low bystander cardiopulmonary resuscitation rates in England. Eur Heart J Qual Care Clin Outcomes. (2019) 5:51–62. doi: 10.1093/ehjqcco/qcy026
13. Toy, J, Bosson, N, Schlesinger, S, and Gausche-Hill, M. Racial and ethnic disparities in the provision of bystander CPR after witnessed out-of-hospital cardiac arrest in the United States. Resuscitation. (2023) 190:109901. doi: 10.1016/j.resuscitation.2023.109901
14. Ewy, GA. Cardiopulmonary resuscitation--strengthening the links in the chain of survival. N Engl J Med. (2000) 342:1599–601. doi: 10.1056/NEJM200005253422109
15. Bobrow, BJ, Panczyk, M, and Subido, C. Dispatch-assisted cardiopulmonary resuscitation: the anchor link in the chain of survival. Curr Opin Crit Care. (2012) 18:228–33. doi: 10.1097/MCC.0b013e328351736b
16. Ong, MEH, Perkins, GD, and Cariou, A. Out-of-hospital cardiac arrest: prehospital management. Lancet. (2018) 391:980–8. doi: 10.1016/S0140-6736(18)30316-7
17. Vallianatou, L, Kapadohos, T, Polikandrioti, M, Sigala, E, Stamatopoulou, E, Kostaki, EM, et al. Enhancing the chain of survival: the role of smartphone applications in cardiopulmonary resuscitation. Cureus. (2024) 16:e68600. doi: 10.7759/cureus.68600
18. Bunch, TJ, Hammill, SC, and White, RD. Outcomes after ventricular fibrillation out-of-hospital cardiac arrest: expanding the chain of survival. Mayo Clin Proc. (2005) 80:774–82. doi: 10.1016/S0025-6196(11)61532-2
19. Berdowski, J, Berg, RA, Tijssen, JGP, and Koster, RW. Global incidences of out-of-hospital cardiac arrest and survival rates: systematic review of 67 prospective studies. Resuscitation. (2010) 81:1479–87. doi: 10.1016/j.resuscitation.2010.08.006
20. Herlitz, J, Svensson, L, Holmberg, S, Ängquist, KA, and Young, M. Efficacy of bystander CPR: intervention by lay people and by health care professionals. Resuscitation. (2005) 66:291–5. doi: 10.1016/j.resuscitation.2005.04.003
21. Pagura, L, Fabris, E, Rakar, S, Gabrielli, M, Mazzaro, E, Sinagra, G, et al. Does extracorporeal cardiopulmonary resuscitation improve survival with favorable neurological outcome in out-of-hospital cardiac arrest? A systematic review and meta-analysis. J Crit Care. (2024) 84:154882. doi: 10.1016/j.jcrc.2024.154882
22. Do, SN, Luong, CQ, Pham, DT, Nguyen, CV, Ton, TT, Pham, TT, et al. Survival after out-of-hospital cardiac arrest, Viet Nam: multicentre prospective cohort study. Bull World Health Organ. (2021) 99:50–61. doi: 10.2471/BLT.20.269837
23. Nishiyama, C, Kiguchi, T, Okubo, M, al-Araji, R, Amorim, E, Alihodžić, H, et al. Characteristics of out-of-hospital cardiac arrest from 2018 to 2021 across the world: third report from the international liaison committee on resuscitation (ILCOR) research and registries committee. Resuscitation. (2025) 2025:110852. doi: 10.1016/j.resuscitation.2025.110852
24. Grasner, JT, Herlitz, J, Tjelmeland, IBM, Wnent, J, Masterson, S, Lilja, G, et al. European resuscitation council guidelines 2021: epidemiology of cardiac arrest in Europe. Resuscitation. (2021) 161:61–79. doi: 10.1016/j.resuscitation.2021.02.007
25. Tabi, M, Perel, N, Taha, L, Amsalem, I, Hitter, R, Maller, T, et al. Out of hospital cardiac arrest – new insights and a call for a worldwide registry and guidelines. BMC Emerg Med. (2024) 24:140. doi: 10.1186/s12873-024-01060-4
26. Pena-Pinedo, G, and Hernandez-Patino, I. CPR knowledge in future physicians: evidence to strengthen undergraduate medical training. Front Med (Lausanne). (2025) 12:1630153. doi: 10.3389/fmed.2025.1630153
27. Das, VN, Pandey, RN, Kumar, V, Pandey, K, Siddiqui, NA, Verma, RB, et al. Repeated training of accredited social health activists (ASHAs) for improved detection of visceral leishmaniasis cases in Bihar, India. Pathog Glob Health. (2016) 110:33–5. doi: 10.1080/20477724.2016.1156902
28. Abdel-All, M, Angell, B, Jan, S, Howell, M, Howard, K, Abimbola, S, et al. What do community health workers want? Findings of a discrete choice experiment among accredited social health activists (ASHAs) in India. BMJ Glob Health. (2019) 4:e001509. doi: 10.1136/bmjgh-2019-001509
29. Selvaraj, K, Sujiv, A, Banerjee, S, Bandyopadhyay, K, and Deshmukh, PR. Expanding roles of accredited social health activists (ASHAs) in the 2019 hepatitis E outbreak in a Peri-urban slum, Nagpur, India. Disaster Med Public Health Prep. (2022) 17:e270. doi: 10.1017/dmp.2022.232
30. Astale, T, Mesele, H, Pasquino, SL, Zewdie, A, Wolka, E, Endalamaw, A, et al. Capacity-building interventions for health extension workers in Ethiopia: a scoping review. PLoS One. (2025) 20:e0317198. doi: 10.1371/journal.pone.0317198
31. Yirsaw, AN, Lakew, G, Getachew, E, Kasaye, MD, Enyew, EB, Getachew, D, et al. Health extension workers job satisfaction and associated factors in Ethiopia: a systematic review and meta-analysis. BMC Health Serv Res. (2025) 25:144. doi: 10.1186/s12913-025-12298-4
32. Rahman, R, Pinto, RM, Zanchetta, MS, Lu, J, and Bailey, R. Community health agents, nurses and physicians conducting research in Brazil's family health program. Health Promot Int. (2019) 34:i92–i102. doi: 10.1093/heapro/daz015
33. Nabecker, S, de Raad, T, Abelairas-Gomez, C, Breckwoldt, J, Chakroun-Walha, O, Farquharson, B, et al. European resuscitation council guidelines 2025 education for resuscitation. Resuscitation. (2025) 215:110739. doi: 10.1016/j.resuscitation.2025.110739
34. du, L, Li, Y, Wang, Z, Zhang, G, Chen, X, Tian, Y, et al. A national survey on current state and development needs of clinical and academic emergency medicine in China. BMC Med Educ. (2024) 24:229. doi: 10.1186/s12909-024-05226-3
35. Hou, L, Wang, Y, and Wang, W. Prevention and control of cardiac arrest in healthy China. China CDC Wkly. (2021) 3:304–7. doi: 10.46234/ccdcw2021.076
36. Ma, J, Zhu, X, Tang, Q, Liu, S, Zhou, W, and Liu, S. Epidemiological characteristics of respiratory diseases in emergency department patients from different ethnic groups in the Atushi region, Xinjiang. Front Med (Lausanne). (2025) 12:1569629. doi: 10.3389/fmed.2025.1569629
37. Zhao, J, Zhang, Y, Zhang, H, Wang, S, He, H, Shi, G, et al. Epidemiological characteristics and spatiotemporal patterns of visceral Leishmaniasis in Xinjiang, China, during 2004-2021. Trop Med Infect Dis. (2024) 9:7. doi: 10.3390/tropicalmed9070153
38. Chen, M, Wang, Y, Li, X, Hou, L, Wang, Y, Liu, J, et al. Public knowledge and attitudes towards bystander cardiopulmonary resuscitation in China. Biomed Res Int. (2017) 2017:3250485. doi: 10.1155/2017/3250485
39. Sutton, RM, Niles, D, Meaney, PA, Aplenc, R, French, B, Abella, BS, et al. Low-dose, high-frequency CPR training improves skill retention of in-hospital pediatric providers. Pediatrics. (2011) 128:e145–51. doi: 10.1542/peds.2010-2105
40. Anderson, R, Sebaldt, A, Lin, Y, and Cheng, A. Optimal training frequency for acquisition and retention of high-quality CPR skills: a randomized trial. Resuscitation. (2019) 135:153–61. doi: 10.1016/j.resuscitation.2018.10.033
41. Mohan, SC, Bhatia, MB, Martinez, CR, Suria, N, Helenowski, I, Thakur, N, et al. Evaluation of a first responders course in rural North India. J Surg Res. (2021) 268:485–90. doi: 10.1016/j.jss.2021.07.023
42. McGaghie, WC, Issenberg, SB, Barsuk, JH, and Wayne, DB. A critical review of simulation-based mastery learning with translational outcomes. Med Educ. (2014) 48:375–85. doi: 10.1111/medu.12391
43. Tadesse, M, Hally, S, Rent, S, Platt, PL, Eusterbrock, T, Gezahegn, W, et al. Effect of a low-dose/high-frequency training in introducing a nurse-led neonatal advanced life support Service in a Referral Hospital in Ethiopia. Front Pediatr. (2021) 9:777978. doi: 10.3389/fped.2021.777978
44. Naz, A, Lakhani, A, Mubeen, K, and Amarsi, Y. Experiences of community midwives receiving helping baby breathe training through the low dose high-frequency approach in Gujrat, Pakistan. Midwifery. (2022) 105:103241. doi: 10.1016/j.midw.2021.103241
45. Kjaer, J, Milling, L, Brochner, AC, Lippert, F, Blomberg, SN, Christensen, HC, et al. Prehospital cardiac arrest resuscitation practices differ around the globe. Resusc Plus. (2025) 25:101017. doi: 10.1016/j.resplu.2025.101017
46. Tuyishime, E, Mossenson, A, Livingston, P, Irakoze, A, Seneza, C, Ndekezi, JK, et al. Resuscitation team training in Rwanda: a mixed method study exploring the combination of the VAST course with advanced cardiac life support training. Resusc Plus. (2023) 15:100415. doi: 10.1016/j.resplu.2023.100415
47. Sasson, C, Rogers, MAM, Dahl, J, and Kellermann, AL. Predictors of survival from out-of-hospital cardiac arrest: a systematic review and meta-analysis. Circ Cardiovasc Qual Outcomes. (2010) 3:63–81. doi: 10.1161/CIRCOUTCOMES.109.889576
48. Hasselqvist-Ax, I, Riva, G, Herlitz, J, Rosenqvist, M, Hollenberg, J, Nordberg, P, et al. Early cardiopulmonary resuscitation in out-of-hospital cardiac arrest. N Engl J Med. (2015) 372:2307–15. doi: 10.1056/NEJMoa1405796
49. Kragholm, K, Wissenberg, M, Mortensen, RN, Hansen, SM, Malta Hansen, C, Thorsteinsson, K, et al. Bystander efforts and 1-year outcomes in out-of-hospital cardiac arrest. N Engl J Med. (2017) 376:1737–47. doi: 10.1056/NEJMoa1601891
50. Merchant, RM, Topjian, AA, Panchal, AR, Cheng, A, Aziz, K, Berg, KM, et al. Part 1: executive summary: 2020 American Heart Association guidelines for cardiopulmonary resuscitation and emergency cardiovascular care. Circulation. (2020) 142:S337–57. doi: 10.1161/CIR.0000000000000918
51. Greif, R, Lockey, A, Breckwoldt, J, Carmona, F, Conaghan, P, Kuzovlev, A, et al. European resuscitation council guidelines 2021: education for resuscitation. Resuscitation. (2021) 161:388–407. doi: 10.1016/j.resuscitation.2021.02.016
Keywords: out-of-hospital cardiac arrest, external defibrillator, township household health education instructors, cardiopulmonary resuscitation, cross-sectional analysis
Citation: Ma J, Kuai L, Zhu X, Tang Q, Liu S and Zhou W (2025) CPR knowledge among rural grassroots healthcare workers in Xinjiang, China: a cross-sectional analysis. Front. Med. 12:1697798. doi: 10.3389/fmed.2025.1697798
Edited by:
Lynn Valerie Monrouxe, The University of Sydney, AustraliaReviewed by:
David Lopez, Loma Linda University, United StatesShajitha Thekke Veettil, Primary Health Care Corporation (PHCC), Qatar
Copyright © 2025 Ma, Kuai, Zhu, Tang, Liu and Zhou. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Weiwei Zhou, d2VpZ29vMTIyNEAxNjMuY29t
†These authors have contributed equally to this work
 Jin Ma
Jin Ma Liuniu Kuai2†
Liuniu Kuai2†