- Department of Neurology, University of Ulm, Ulm, Germany
Recanalization methods in ischemic stroke have been progressively expanded over the past years. In addition the continuous development of specialized mechanical devices for thrombectomy a broad spectrum of new drugs has been tested: Both options, novel drugs as well as new devices, can be employed independently of each other, but in most cases a combination of the two with the standard treatment of intravenous fibrinolysis is applied. Until recently, a large number of case series have been performed to investigate the effects of various drugs and interventions, but only a few trials have been conducted to determine the optimal conditions for combining both procedures. This review surveys the different systemic and endovascular vessel reopening practices and their major bridging techniques.
Background and Purpose
Reperfusion is the primary therapeutic goal during acute ischemic stroke. By restoring blood flow to the affected vessel, reperfusion therapies save penumbral tissue, reduce final infarct size and result in an improved clinical outcome. The standard reperfusion method – intravenous recombinant tissue-type plasminogen activator (I.V.-rtPA) is the quickest way to initiate thrombolysis for acute ischemic stroke. At present treatment is recommended within the first 3 h after symptom onset, but the time window can be extended to 4.5 h based on the increasing evidence of benefit in patients treated within this interval (Hacke et al., 2008; Wahlgren et al., 2008). The effect of fibrinolysis depends chiefly on recanalization, which increases the probability of a favorable clinical outcome by a four- to fivefold factor. Intravenous fibrinolysis however reopens an occluded vessel in less than half of all cases (Rha et al., 2007). Moreover it recanalizes only one out of three patients with an occlusion of the proximal middle cerebral artery and only about one out of 10 patients in cases of thrombosis of the internal carotid artery (ICA; Mori et al., 1992; Wolpert et al., 1993; Tomsick et al., 1996; IMS Study Investigators, 2004). Therefore, particularly the prognosis of patients with clinically severe ischemic strokes caused by occlusions in the proximal vascular bed remains relatively poor. In these cases endovascular methods clearly provide higher recanalization rates at the expense of a longer delay in treatment initiation. The time to recanalization however is in itself a very substantial predictor of clinical outcome (Ringelstein et al., 1992; Heiss et al., 1998; Christou et al., 2000). Thus procedures such as intra-arterial thrombolysis (IAT) and mechanical thrombectomy improve recanalization rates considerably, but there is substantial doubt with regard to the ultimate superiority of their clinical efficacy. To avoid low recanalization rates by I.V.-rtPA or delayed reopening by IAT a bridging approach of both methods is more auspicious than one single method in isolation. The combination of both methods provides the advantages of early treatment initiation via I.V.-rtPA as well as higher recanalization rates by subsequently processing IAT and/or mechanical intra-arterial procedures. Yet despite a considerable number of different techniques the optimal crossover between intravenous and intra-arterial measures is still unavailable. Here we summarize the current data for the major recanalization-techniques and the various options for combining them. Finally, we propose a protocol for an actual bridging practice.
Intravenous Thrombolysis
Intravenous Recombinant Tissue-Type Plasminogen Activator
After a number of studies involving intravenous application of streptokinase attempted to resolve the therapeutic nihilism in ischemic stroke (MAST-I, 1995; Donnan et al., 1996; MAST-E, 1996), the NINDS-study group, in 1995, published their landmark-findings from a study of 624 patients with acute ischemic stroke (National Institute of Neurological Disorders, and Stroke rt-PA Stroke Study Group, 1995). In this study patients received 0.9 mg/kg/body weight (BW) of alteplase within 3 h of symptom onset. Patients in the treatment group were at least 30% more likely to have minimal or no disability at 3 months than those who received a placebo.
By comparison, two European trials: the European Cooperative Acute Stroke Study I (ECASS I) and ECASS II, investigated a time window of up to 6 h but failed to show the efficacy of thrombolytic treatment, as defined by each trial (Hacke et al., 1995, 1998). Nevertheless, the results from an extensive review (Wardlaw et al., 2003) of 18 fibrinolytic trials suggested a positive effect for rtPA given up to 6 h. Furthermore, a pooled analysis of the common data elements from six randomized placebo-controlled trials, including ATLANTIS (Part A and B), ECASS (both trials), and NINDS (Part 1 and 2) which investigated thrombolysis with rtPA for ischemic stroke, reported favorable outcomes even when therapy was administered between 3.0 and 4.5 h after symptom onset (Hacke et al., 2004). In 2008, the ECASS-3 trial confirmed this finding (Hacke et al., 2008).
In ECASS I, using 1.1 mg/kg/BW rtPA, resulted in a substantial number of intracranial hemorrhages, whereas most of the other randomized trials used 0.9 mg/kg/BW rtPA. On the other hand a lower dosage of rtPA may prove to be comparably effective. Two recent Japanese trials have shown that in an Asian population a similar outcome may be reached by two thirds of the standard rtPA dose in Caucasians (Yamaguchi et al., 2006; Mori et al., 2010). Meanwhile, the dosage of 0.9 mg/kg/BW has not only been proved to be safe in randomized trials but also in clinical practice as shown in a large register with 6483 patients (Wahlgren et al., 2007). At present I.V. thrombolysis with 0.9 mg/kg/BW rtPA has been approved in most countries.
Nevertheless even in industrialized countries only the minority (Albers and Olivet, 2007; Katzan et al., 2004; ) of all ischemic stroke patients receives rtPA therapy. The major reason for its restricted application is its reportedly narrow time window (Lees et al., 2006; Harrer, 2010), compounded by the necessity of cerebral imaging to exclude intracerebral hemorrhage. Since the late 1990’s (Schlaug et al., 1999), there have been attempts to prolong this short therapeutic interval by implementing an approach to predict the clinical success of recanalization by imaging the penumbra via the so-called “diffusion–perfusion mismatch.” Particularly in cases of proximal artery occlusion screening for this mismatch may help to increase the proportion of patients eligible for thrombolysis and as many as 70–80% show potentially salvageable tissue for more than 9 h (Copen et al., 2009). Although several phase II-studies (Hacke et al., 2005; Albers et al., 2006; Furlan et al., 2006) and a retrospective analysis of ATLANTIS, ECASS, and NINDS (Thomalla et al., 2006) have confirmed this concept, a prospective Phase 3 study that used this approach (Hacke et al., 2009) failed to demonstrate any benefit.
Other Fibrinolytics
Because of the disadvantages associated with rtPA there have been numerous attempts to find alternative fibrinolytic agents with a longer half life and a higher fibrin specificity to facilitate the application, to decrease the rates of hemorrhage, and to optimize the therapeutic effects. Tenecteplase, another plasminogen activator which can be administered in a bolus form has been investigated in two phase II trials (Haley et al., 2005, 2010). Both trials, however ended more or less at the dose finding level without demonstrating superiority or even equivalence to rtPA. Desmoteplase (DSPA), originally isolated from the saliva of a vampire bat, is a highly fibrin-specific plasminogen activator. Treatment with DSPA is of particular interest for thrombolysis after the 3-h time window owing to its potential to reduce intracranial hemorrhaging. In 2005, findings of the desmoteplase in acute ischemic stroke trial (DIAS I) in which I.V. DSPA was administered within 3–9 h of ischemic stroke onset in patients with perfusion/diffusion mismatch on MRI, were published (Hacke et al., 2005). One hundred and four patients with a National Institute of Health Stroke Scale (NIHSS) score of 4 to 20 were included. Outcome was rated by reperfusion on MRI 4–8 h after treatment, and clinical improvement after 3 months was assessed by using the NIHSS, the modified ranking scale (mRS), and Barthel index (BI). A significant advantage was found in terms of clinical as well as imaging parameters for DSPA, with the best results in the 125-μg/kg/BW group. A year later, the results of the dose escalation of desmoteplase for acute ischemic stroke trial (DEDAS), based on the same study protocol as the previous study, corroborated these findings (Furlan et al., 2006). However the consecutive follow-up trial DIAS II (Hacke et al., 2009) did not confirm the benefit by DSPA. It has been speculated that this was attributable to an uncommon spontaneous reopening rate of 50% in the placebo group, but the exact reasons for the discordant result are still unknown. Meanwhile a third DIAS-trial is on the way.
Similar to DSPA, ancrod, a substance which induces rapid defibrinogenation in humans by splitting fibrinopeptide A from fibrinogen, is derived from a non-human source. The purified fraction of the venom of the Malaysian spit viper has been investigated in acute ischemic stroke and has produced favorable outcomes in an initial randomized, placebo-controlled study (Sherman et al., 2000), in which 500 patients with an acute ischemic stroke were treated with ancrod versus a placebo. However several consecutive trials, in which ancrod was administered within a 3- or 6-h window, revealed inconsistent results. Finally Levy et al. (2009) failed to show an improvement in outcome in 500 randomized patients in the ASP-study, even after adjusting the timing and dosage regimes to the experiences of the preceding studies, and there was also still a trend to increased bleeding rates.
Glycoprotein IIB/IIIA Antagonists – Abciximab, Tirofiban, and Eptifibatide
The glycoprotein (GP) IIb/IIIa complex is the major integrin present on the platelet surface and plays a key role in platelet aggregation. The use of GP-IIb/IIIa antagonists is widespread and very common for cardiological purposes because of its efficacy in coronary interventions (Cura et al., 2000). Whereas Eptifibatide and Tirofiban as separate treatment options for ischemic stroke have only been investigated in retrospective case series (Martin-Schild et al., 2009) or in case reports (Liebeskind et al., 2002), Abciximab, the recombinant Fab fragment of a monoclonal anti-GP-IIb/IIIa antibody has been investigated more extensively. After encouraging Phase I and II trials (Abciximab in Ischemic Stroke Investigators, 2000; Abciximab Emergent Stroke Treatment Trial (AbESTT) Investigators, 2005) in ischemic stroke that demonstrated a trend toward better clinical outcomes without increasing hemorrhagic complications, a phase III trial was initiated (Adams et al., 2008). In addition to a cohort of patients within 6 h after stroke onset, a special cohort with “wake up strokes” was included. The clinical outcome was determined 3 months after admission using the mRS and the results were disappointing: whilst there was no difference in terms of good clinical outcome (33% of placebo-treated patients versus 32% of abciximab-treated patients), the rate of symptomatic or fatal intracranial hemorrhage increased significantly from 0.5% in the placebo group to 5.5% via inhibition of the GP-IIb/IIIa complex. As a result, the trial was terminated prematurely. In an alternative approach the CLEAR trial tested the combination of GP-IIb/IIIa-inhibitors, namely eptifibatide (75 μg/kg/BW bolus followed by a 0.75-μg/kg/BW/min infusion for 2 h), with a low dose rtPA regimen of either 0.30 mg/kg or 0.45 mg/kg/BW. The results were compared to a standard dose rtPA treatment (0.9 mg/kg; Pancioli et al., 2008). This approach appeared to be safe, but reports of a clinical amelioration are still lacking.
I.A.-Thrombolysis (IAT)
In IAT fibrinolytic drugs are applied directly into the occluding thrombus using microcatheter delivery systems. By means of this minimally invasive technique high local drug concentrations with lower systemic concentrations can be achieved, which, at least theoretically, reduces the risk of extracranial hemorrhagic complications. In addition this method provides precise imaging of the arterial anatomy, pathology, and collateral circulation. Furthermore, IAT includes the option of applying additional devices to disrupt the clot mechanically. In retrospective clinical case studies, IAT yielded higher rates of recanalization than I.V. therapy (Alexandrov et al., 2002; Higashida et al., 2003), with an estimated average recanalization rate of 70%, which has been confirmed in a recent meta-analysis (Lee et al., 2010). The method’s chief disadvantage, however, is the lag time during which fibrinolysis is initiated. The delay can be attributed to logistic as well as procedure-related technical reasons and is closely related to the progression of neuronal cell death in the ischemic brain, which has been shown to be strictly time dependent. Moreover the most effective thrombolytic drug for IAT has never been adequately tested. Although in the prolyse in acute cerebral thromboembolism (PROACT)-trials recombinant prourokinase has been used, r-proUK is unavailable routinely because it lacks FDA approval. As such, most recent investigations have utilized rtPA for practical reasons. Additionally, the ideal dosage for both drugs in IAT has not been tested. Patients were treated with either urokinase in a dosage up to 2 million U or with rtPA in a dosage up to 90 mg within 6 h of symptom onset. Comparisons between these trials are complicated because of the broad range of inclusion and exclusion criteria. The PROACT I study in 1995 was the first randomized double-blinded multicenter trial, in which safety, recanalization frequency, and clinical efficacy of IAT with r-proUK were compared with a placebo in patients with symptomatic MCA occlusion in a 6-h time window (del Zoppo et al., 1998). Eligible patients were randomized to receive a placebo or a fixed dose of 6 mg r-proUK administered over a 2-h period in the proximal third of the thrombus or close to the clot within the M1-segment. Mechanical disruption of the thrombus was prohibited. The degree of the recanalization was determined at the end of the procedure. Subsequently, patients were given I.V. heparin for 4 h. Because of severe hemorrhage rates in the first 16 patients with a high dose heparin regime, the heparin dose was later decreased. A CCT was performed in all patients after 24 h to control bleeding. Clinical outcome was rated by blinded physicians by the NIHSS, the mRS, and the BI 7, 30, and 90 days after treatment. Out of 40 patients, 26 received r-proUK, and 14 a placebo. In summary, there was a 10–12% absolute increase in positive outcomes in patients treated with r-proUK compared to those in the placebo group. Interestingly, heparin reduction resulted in a decreased recanalization rate from 82 to 40%, and, at the same time, hemorrhagic side-effects were also lower. The rate of symptomatic bleedings was 15% in the r-proUK group compared to 7% in the placebo group. Consequently in PROACT II (Furlan et al., 1999) the dosage of r-proUK was increased to 9 mg to improve the recanalization rates whereas only low dose heparin was administered. One hundred and eighty patients were randomized and 121 patients received r-proUK. Under this regimen, recanalization rate was 66% with an symptomatic hemorrhage rate of 10% for r-proUK treated patients. The absolute benefit was 15% and the relative benefit 58%. Within the last 15 years however only one further randomized trial of intra-arterial fibrinolysis (Ogawa et al., 2007) in ischemic stroke has been performed. Trials based on directly comparing intra-arterial and intravenous thrombolysis in terms of recanalization rates and especially in terms of clinical outcome have not been performed at all. Thus, intra-arterial fibrinolysis remains an individual treatment approach without approval by the FDA and it is not recommended generally.
Mechanical Thrombectomy
As an alternative to or as a supplementary tool for systemic or IAT mechanical thrombectomy provides higher recanalization rates – particularly in patients with occlusion of the carotid-, proximal media- or basilaric-artery. Endovascular thrombectomy devices remove the occluding clot from the affected vessel mechanically. In general three systems can be distinguished: initially distal systems have been developed, which permit retrieval of the clot by removing the thrombus on the way back after the thrombus has been passed by the system. A typical device is the mechanical embolus removal in cerebral ischemia (MERCI) Retrieval System. Results of the Phase 1 MERCI trial were published in 2004 (Gobin et al., 2004). In this study 28 patients with ICA, MCA, or occlusions of the basilar artery were treated within a median time of 6.15 h. In 43% of all patients, an effective recanalization could be achieved. No clinically significant bleeding occurred. Four years later, the final data of the Multi MERCI trial, a study with approximately the same inclusion criteria as the previous study but with treatment within 8 h, were released (Smith et al., 2008). One hundred and sixty-four patients were enrolled, and 131 were initially treated with the newer generation of MERCI L5 retriever. Recanalization by pure mechanical thrombectomy was achieved in 57.3%, whereas a recanalization rate of 68% was achieved after additional IAT. Even more importantly, the clinical outcome after 90 days was significantly (p < 0.001) improved. In turn, this clinical improvement correlated closely with success rates of recanalization. A pooled analysis of MERCI and Multi MERCI with a subinvestigation of patients with an acute stoke from intracranial ICA-occlusion confirmed this observation (Flint et al., 2007). Because of its promising results the MERCI Retriever was the first FDA-approved technical device used to restore blood flow.
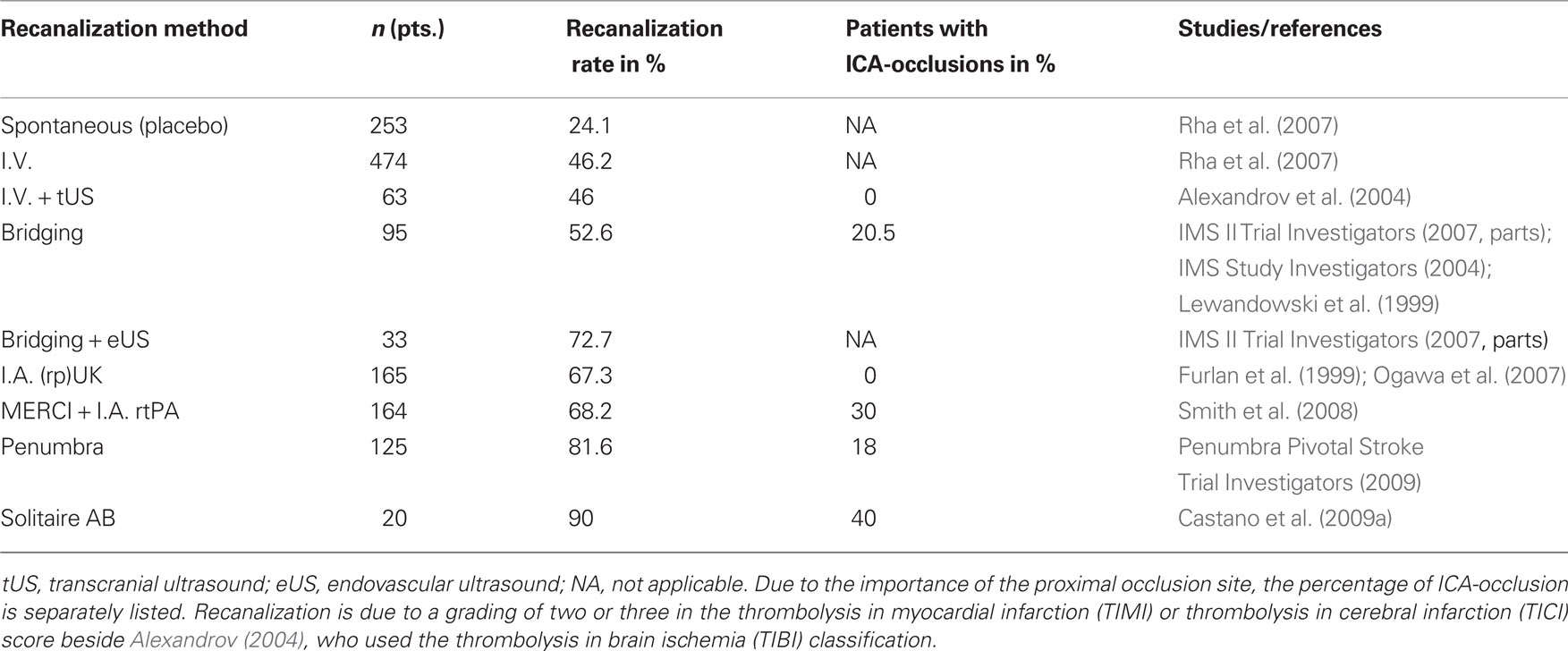
Alternatively to this method, a clot may be removed from the proximal side, e.g., by using aspiration techniques. In the process, the necessity of perforating the thrombus can be avoided, thereby reducing the risk of thrombus fragmentation and associated distal emboli. However a comparison of both methods (i.e., retrieval versus aspiration) reveals a higher recanalization rate for the distal thrombectomy systems (Gralla et al., 2006; see Table 1).
An even more advanced device is the Penumbra Stroke System, which was licensed by the FDA after it achieved a recanalization rate of 100% in a smaller pilot study (Bose et al., 2008) and even 81.6% in a subsequent larger prospective trial (Penumbra Pivotal Stroke Trial Investigators, 2009). In addition to an aspiration system, this device includes a mechanism for grasping the thrombus directly. In a similar manner, stents like the Solitaire-remodeling device, are capable of being delivered immediately to the side of the thrombus and removing the clot, while at the same time, being completely retrievable (Henkes et al., 2003; Castano et al., 2009b). Although only small case series are available, the Solitaire stent might be superior (Castano et al., 2009b) to distal retraction devices owing to its simplicity and speed, as well as its relatively protective properties for the vessel wall. In any event, a comparison of several recanalization procedures (Rha et al., 2007; Nogueira et al., 2009) and thrombectomy devices (Castano et al., 2009a, Serna-Candel et al., 2010) yields the highest recanalization success rates for distal thrombectomy devices, one the one hand, and the Solitaire stent on the other (see Table 1).
Bridging Therapy
I.V./I.A.-Combining I.V. and I.A.-rtPA
Time delay resulting from initiation and preparation of IAT and mechanical devices is the main drawback of this technique compared with I.V. thrombolysis.
A potential advantage of a combined I.V./I.A. approach is the rapid initiation and easy handling of I.V. treatment, combined with the potentially higher recanalization rates associated with I.A. therapy, to optimize clinical outcome. Lewandowski et al. (1999) published the findings of the emergency management stroke (EMS) Bridging Trial. This was a double-blinded, randomized, placebo-controlled multicenter trial that compared pure IAT to an I.V./I.A. approach. A total of 35 patients with acute ischemic stroke within 3 h after symptom onset were randomized. They received either a loading dose of 0.6 mg/kg/BW I.V. rtPA with 10% as bolus application (17 patients) or a placebo (18 patients) followed immediately by cerebral arteriography and local I.A.-rtPA with a maximal dose of 20 mg rtPA. The combined approach yielded significantly higher recanalization rates (55% I.V./I.A. versus 10% placebo/IAT) without producing a clinically significant improvement as measured by NIHSS, BI, mRS, and Glasgow Outcome Scale at days 1 and 7 and after 3 months. The obviously higher mortality rate in the I.V./I.A.-group seemed to be attributable to the very low numbers of patients included. In a very similar (but not placebo-controlled) approach, 80 severely affected patients (NIHSS ≥ 10) were treated in the interventional management of stroke single arm trial (IMS I) from 2004 (IMS Study Investigators, 2004). In this study the same I.V.-rtPA dosage was used, but the initial I.V.-bolus was slightly increased to 15% and the consecutive intra-arterial dosage was adapted to 22 mg rtPA. The 3-months outcome in these 80 subjects was matched to the outcome in the NINDS rtPA Stroke trial thus making it possible to compare standard intravenous fibrinolysis (I.V.-rtPA) with the I.V./I.A.-approach. Once again the asymptomatic hemorrhage rates increased significantly with the combination therapy (43 versus 6%), whereas symptomatic bleedings did not differ in between these two trials. The clinical outcome of the combined therapy did not differ from the purely intravenous procedure, although both methods substantially improved the clinical outcome compared to the placebo-treated patients in NINDS. In the subsequent single arm Interventional Management of Stroke II Study (IMS II Trial Investigators, 2007), 81 subjects with even more severe strokes and a median baseline NIHSS score of 19 were included. Fifty-five patients received the combined I.V./IAT. The results were similar to the IMS I trial with a mRS of 0–2 in 46% after 3 months, but the rate of symptomatic intracranial hemorrhages was increased from 6.3 in IMS I to 9.9% in IMS II. Nonetheless, it should be borne in mind that in the 2007 study, in 36 of the 55 I.A.-treated patients the approach was complemented by a small-vessel ultrasound infusion system (EKOS) to potentially accelerate thrombolysis. In a more clinical setting the “classical” bridging-version has been tested in both carotid artery distribution strokes (Ernst et al., 2000) and in very severely affected patients (Zaidat et al., 2002). In the event of persisting deficits, the I.V.-approach was shifted after 30 min to a IAT until the clot completely resolved or up to a maximum dosage of 0.9 mg/kg/BW. Although a recanalization could be achieved in four out of five patients with an ICA-occlusion, the mortality rate remained as high as 50%. Interestingly, an upside-down pathway has also been conducted. Keris et al. (2001) applied primarily IAT followed by I.V.-thrombolyis. In that study 45 patients with severe acute ischemic stroke within 6 h after symptom onset were investigated. Only 12 of them were randomized to the fibrinolysis group, whereas 33 patients were randomized to the conventional treatment group. Patients in the first group received 25 mg rtPA I.V. over 60 min after an intra-arterial injection of 25 mg rtPA over 5–10 min without mechanical clot disruption. Although clinical outcomes following treatment assessment at 1 and at 12 months were better, these results are clearly restricted by the very low number of patients studied.
Bridging Extended – I.V./I.A-Thrombolysis and Beyond
Despite inconclusive results and an astonishing lack of even a single study comparing a combined I.V./I.A. approach to the standard I.V.-rtPA scheme in a randomized trial, the “conventional” I.V./I.A.-combination approach has been extended in several ways. Some investigators used urokinase (UK) in addition to rtPA for synergistic and complementary effects. For example, in 24 patients with a median baseline NIHSS score of 18, Lee et al. (2004), administered a full dose I.V.-rtPA (0.9 mg/kg/BW) treatment followed by I.A. UK (300000 U initially, with a maximum overall dose of 1000000 U). Symptomatic hemorrhage rates remained low, although four patients also received I.V. abciximab when a reocclusion of the affected vessel was identified (Lee et al., 2004). In general, many studies have supplemented rtPA or UK with GP-IIb/IIIa-inhibitors. Eckert et al. (2005) combined I.V. abciximab (0.25 mg/kg bolus, followed by a 12-h infusion therapy with 0.125 μg/kg/min) with IAT (median dosage: 20 mg rtPA) in patients with basilar artery stroke. I.V. tirofiban combined with I.A. UK was studied by Mangiafico et al. (2005) – this time again in severely affected patients with a median NIHSS score of 21. The outcome after 3 months was compared with a retrospective cohort treated with I.A.-rtPA (median dosage: 40 mg). In view of the small numbers of subjects enrolled in these studies, definitive clinical conclusions cannot yet be drawn. It needs to be pointed out however, that despite a higher degree of hemorrhaging in general no significant differences in symptomatic bleedings have to be tolerated. This is also true when mechanical procedures are added to the pharmacological approach to enhance recanalization. Typically such protocols are gradated constructs, adding intra-arterial fibrinolysis, and mechanical procedures in the event of persistent occlusion after the preceding intravenous intervention. In 2009, the RECANALISE study (Mazighi et al., 2009) achieved a recanalization rate of 87% in this manner, although one fourth of the study population of more than 50 individuals in the I.V./endovascular approach had combined ICA/MCA-occlusions. Three years previously, the Multi MERCI Trial (Flint et al., 2007) had yielded a similarly high rate of effectiveness in a very similar group. Nevertheless, comparison with the pure intra-arterial PROACT II study did not reveal the superiority of this combined approach (Josephson et al., 2009) in terms of clinical outcome. It is worth mentioning that in the Multi MERCI trial, unlike the RECANALISE study, a full dose of I.V. fibrinolysis (0.9 mg/kg/BW) was administered. Intuitively, this regimen seems to be more prone to intracranial hemorrhages. In contrast, Shaltoni et al. (2007), in a retrospective data set from 69 patients with a median pretreatment NIHSS score of 18, showed that a consecutive IAT within a median time of 105 min after finalizing a full dose I.V.-treatment did not necessarily result in higher symptomatic intracranial hemorrhage rates. However, a direct comparison of the intracranial hemorrhage frequencies is difficult, as this study included mainly intra-arterial treatment with reteplase. Moreover the few patients treated with alteplase and UK received even lower fibrinolytic dosages compared to the PROACT and IMS-1 and -2 trials. Unfortunately the results of the randomized IMS-3 trial (Khatri et al., 2008), which includes the use of two different catheter devices, will be a long time in coming.
Conclusion
At present, intravenous fibrinolysis is the approved standard therapy in patients with acute ischemic stroke. Nevertheless, only a minority of all patients is treated with I.V.-rtPA, whereas recanalization – the most crucial factor for the clinical outcome – succeeds in only 50% of patients receiving this therapy. Intra-arterial procedures yield considerably higher recanalization rates for I.A.-rtPA and particularly for mechanical thrombectomy devices, although their clinical superiority over the systemic approach may depend on the time lag associated with the more complex technique. Accordingly, bridging this time lag by means of intravenous rtPA is a useful strategy. Most available data from randomized trials recommend a dosage of 0.6 mg/kg/BW rtPA and a time lag of 30 min as “intravenous to intra-arterial” needle time (Lewandowski et al., 1999; Ernst et al., 2000; Zaidat et al., 2002; IMS Study Investigators, 2004; IMS II Trial Investigators, 2007). Although superior clinical outcomes have not been proved yet, this regimen seems to be reasonable. Treatment confined to a dosage of 0.6 mg/kg/BW I.V.-rtPA is effective, at least in an Asian population (Yamaguchi et al., 2006; Mori et al., 2010), whereas the incidence of intracranial hemorrhages remains unchanged even when intra-arterial fibrinolysis is also performed. The 30-min time lag between I.V.-rtPA and the initiation of intra-arterial procedures is short, but this interval has to be as short as possible. In the event that, for logistical reasons, it is necessary to exceed the 30-min time limit, an intravenous fibrinolysis with 0.9 mg/kg/BW rtPA should be administered. The data to date in the field (Flint et al., 2007; Shaltoni et al., 2007) does not indicate that there are higher symptomatic bleeding rates if an intra-arterial procedure is performed immediately after a full dose I.V.-rtPA fibrinolysis.
In general subsequent endovascular intervention should be aimed at recanalizing persisting vessel-occlusions, as performed in several recent studies (Eckert et al., 2005; Mangiafico et al., 2005; Flint et al., 2007; Smith et al., 2008; Castano et al., 2009a; Mazighi et al., 2009). Depending on the preceding intravenous rtPA dosage, we propose a strategy based predominantly on a combination of an intra-arterial fibrinolysis and a mechanical device after an intravenous dosage of 0.6 mg/kg/BW rtPA, whereas a almost “pure” mechanical intervention, for example with the Solitaire stent, should be preferred following an intravenous full dose rtPA regimen. However, in our experience recanalization by an I.A. approach without any additional fibrinolytic agent is difficult. Therefore a small amount of rtPA is always used in our center.
Finally, all these approaches have to be able to demonstrate their clinical superiority when comparing their results with the gold standard, which up to now remains I.V.-rtPA. Therefore a randomized trial comparing intravenous fibrinolysis with a bridging therapy is desperately needed. In this study patients with a proximal artery occlusion and a large penumbra according to the MRI mismatch criteria should be treated either intravenously or by a bridging regimen, including intra-arterial fibrinolysis and/or mechanical thrombectomy.
Conflict of Interest Statement
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
References
Abciximab Emergent Stroke Treatment Trial (AbESTT) Investigators. (2005). Emergency administration of abciximab for treatment of patients with acute ischemic stroke: results of a randomized phase 2 trial. Stroke 36, 880–890.
Abciximab in Ischemic Stroke Investigators. (2000). Abciximab in acute ischemic stroke: a randomized, double-blind, placebo-controlled, dose-escalation study. Stroke 31, 601–609.
Adams, H. P., Jr. Effron, M. B., Torner, J., Davalos, A., Frayne, J., Teal, P., Leclerc, J., Oemar, B., Padgett, L., Barnathan, E. S., and Hacke, W. (2008). Emergency administration of abciximab for treatment of patients with acute ischemic stroke: results of an international phase III trial: abciximab in emergency treatment of stroke trial (AbESTT-II). Stroke 39, 87–99.
Albers, G. W., and Olivot, J. M. (2007). Intravenous alteplase for ischaemic stroke. Lancet 369, 249–250.
Albers, G. W., Thijs, V. N., Wechsler, L., Kemp, S., Schlaug, G., Skalabrin, E., Bammer, R., Kakuda, W., Lansberg, M. G., Shuaib, A., Coplin, W., Hamilton, S., Moseley, M., and Marks, M. P. (2006). Magnetic resonance imaging profiles predict clinical response to early reperfusion: the diffusion and perfusion imaging evaluation for understanding stroke evolution (DEFUSE) study. Ann. Neurol. 60, 508–517.
Alexandrov, A. V., and Grotta, J. C. (2002). Arterial reocclusion in stroke patients treated with intravenous tissue plasminogen activator. Neurology 59, 862–867.
Alexandrov, A. V., Molina, C. A., Grotta, J. C., Garami, Z., Ford, S. R., Alvarez-Sabin, J., Montaner, J., Saqqur, M., Demchuk, A. M., Moye, L. A., Hill, M. D., and Wojner, A. W. (2004). Ultrasound-enhanced systemic thrombolysis for acute ischemic stroke. N. Engl. J. Med. 351, 2170–2178.
Bose, A., Henkes, H., Alfke, K., Reith, W., Mayer, T. E., Berlis, A., Branca, V., and Sit, S. P. (2008). The Penumbra System: a mechanical device for the treatment of acute stroke due to thromboembolism. AJNR Am. J. Neuroradiol. 29, 1409–1413.
Castano, C., Dorado, L., Guerrero, C., Millan, M., Gomis, M., Perez de la Ossa, N., Castellanos, M., Garcia, M. R., Domenech, S., and Davalos, A. (2009a). Mechanical thrombectomy with the Solitaire AB device in large artery occlusions of the anterior circulation: a pilot study. Stroke 41, 1836–1840.
Castano, C., Serena, J., and Davalos, A. (2009b). Use of the new Solitaire (TM) AB device for mechanical thrombectomy when merci clot retriever has failed to remove the clot. A case report. Interv. Neuroradiol. 15, 209–214.
Christou, I., Alexandrov, A. V., Burgin, W. S., Wojner, A. W., Felberg, R. A., Malkoff, M., and Grotta, J. C. (2000). Timing of recanalization after tissue plasminogen activator therapy determined by transcranial doppler correlates with clinical recovery from ischemic stroke. Stroke 31, 1812–1816.
Copen, W. A., Rezai Gharai, L., Barak, E. R., Schwamm, L. H., Wu, O., Kamalian, S., Gonzalez, R. G., and Schaefer, P. W. (2009). Existence of the diffusion-perfusion mismatch within 24 hours after onset of acute stroke: dependence on proximal arterial occlusion. Radiology 250, 878–886.
Cura, F. A., Bhatt, D. L., Lincoff, A. M., Kapadia, S. R., L’Allier, P. L., Ziada, K. M., Wolski, K. E., Moliterno, D. J., Brener, S. J., Ellis, S. G., and Topol, E. J. (2000). Pronounced benefit of coronary stenting and adjunctive platelet glycoprotein IIb/IIIa inhibition in complex atherosclerotic lesions. Circulation 102, 28–34.
del Zoppo, G. J., Higashida, R. T., Furlan, A. J., Pessin, M. S., Rowley, H. A., and Gent, M. (1998). PROACT: a phase II randomized trial of recombinant pro-urokinase by direct arterial delivery in acute middle cerebral artery stroke. PROACT investigators. Prolyse in acute cerebral thromboembolism. Stroke 29, 4–11.
Donnan, G. A., Davis, S. M., Chambers, B. R., Gates, P. C., Hankey, G. J., McNeil, J. J., Rosen, D., Stewart-Wynne, E. G., and Tuck, R. R. (1996). Streptokinase for acute ischemic stroke with relationship to time of administration: Australian streptokinase (ASK) trial study group. JAMA 276, 961–966.
Eckert, B., Koch, C., Thomalla, G., Kucinski, T., Grzyska, U., Roether, J., Alfke, K., Jansen, O., and Zeumer, H. (2005). Aggressive therapy with intravenous abciximab and intra-arterial rtPA and additional PTA/stenting improves clinical outcome in acute vertebrobasilar occlusion: combined local fibrinolysis and intravenous abciximab in acute vertebrobasilar stroke treatment (FAST): results of a multicenter study. Stroke 36, 1160–1165.
Ernst, R., Pancioli, A., Tomsick, T., Kissela, B., Woo, D., Kanter, D., Jauch, E., Carrozzella, J., Spilker, J., and Broderick, J. (2000). Combined intravenous and intra-arterial recombinant tissue plasminogen activator in acute ischemic stroke. Stroke 31, 2552–2557.
Flint, A. C., Duckwiler, G. R., Budzik, R. F., Liebeskind, D. S., and Smith, W. S. (2007). Mechanical thrombectomy of intracranial internal carotid occlusion: pooled results of the MERCI and Multi MERCI Part I trials. Stroke 38, 1274–1280.
Furlan, A., Higashida, R., Wechsler, L., Gent, M., Rowley, H., Kase, C., Pessin, M., Ahuja, A., Callahan, F., Clark, W. M., Silver, F., and Rivera, F. (1999). Intra-arterial prourokinase for acute ischemic stroke. The PROACT II study: a randomized controlled trial. Prolyse in acute cerebral thromboembolism. JAMA 282, 2003–2011.
Furlan, A. J., Eyding, D., Albers, G. W., Al-Rawi, Y., Lees, K. R., Rowley, H. A., Sachara, C., Soehngen, M., Warach, S., and Hacke, W. (2006). Dose escalation of desmoteplase for acute ischemic stroke (DEDAS): evidence of safety and efficacy 3 to 9 hours after stroke onset. Stroke 37, 1227–1231.
Gobin, Y. P., Starkman, S., Duckwiler, G. R., Grobelny, T., Kidwell, C. S., Jahan, R., Pile-Spellman, J., Segal, A., Vinuela, F., and Saver, J. L. (2004). MERCI 1: a phase 1 study of mechanical embolus removal in cerebral ischemia. Stroke 35, 2848–2854.
Gralla, J., Schroth, G., Remonda, L., Nedeltchev, K., Slotboom, J., and Brekenfeld, C. (2006). Mechanical thrombectomy for acute ischemic stroke: thrombus-device interaction, efficiency, and complications in vivo. Stroke 37, 3019–3024.
Hacke, W., Albers, G., Al-Rawi, Y., Bogousslavsky, J., Davalos, A., Eliasziw, M., Fischer, M., Furlan, A., Kaste, M., Lees, K. R., Soehngen, M., and Warach, S. (2005). The desmoteplase in acute ischemic stroke trial (DIAS): a phase II MRI-based 9-hour window acute stroke thrombolysis trial with intravenous desmoteplase. Stroke 36, 66–73.
Hacke, W., Donnan, G., Fieschi, C., Kaste, M., von Kummer, R., Broderick, J. P., Brott, T., Frankel, M., Grotta, J. C., Haley, E. C., Jr., Kwiatkowski, T., Levine, S. R., Lewandowski, C., Lu, M., Lyden, P., Marler, J. R., Patel, S., Tilley. B. C., Albers, G., Bluhmki, E., Wilhelm, M., and Hamilton, S. (2004). Association of outcome with early stroke treatment: pooled analysis of ATLANTIS, ECASS, and NINDS rt-PA stroke trials. Lancet 363, 768–774.
Hacke, W., Furlan, A. J., Al-Rawi, Y., Davalos, A., Fiebach, J. B., Gruber, F., Kaste, M., Lipka, L. J., Pedraza, S., Ringleb, P. A., Rowley, H. A., Schneider, D., Schwamm, L. H., Leal, J. S., Sohngen, M., Teal, P. A., Wilhelm-Ogunbiyi, K., Wintermark, M., and Warach, S. (2009). Intravenous desmoteplase in patients with acute ischaemic stroke selected by MRI perfusion–diffusion weighted imaging or perfusion CT (DIAS-2): a prospective, randomised, double-blind, placebo-controlled study. Lancet Neurol. 8, 141–150.
Hacke, W., Kaste, M., Bluhmki, E., Brozman, M., Davalos, A., Guidetti, D., Larrue, V., Lees, K. R., Medeghri, Z., Machnig, T., Schneider, D., von Kummer, R., Wahlgren, N., and Toni, D. (2008). Thrombolysis with alteplase 3 to 4.5 hours after acute ischemic stroke. N. Engl. J. Med. 359, 1317–1329.
Hacke, W., Kaste, M., Fieschi, C., Toni, D., Lesaffre, E., von Kummer, R., Boysen, G., Bluhmki, E., Hoxter, G., and Mahagne, M. H. (1995). Intravenous thrombolysis with recombinant tissue plasminogen activator for acute hemispheric stroke. The European cooperative acute stroke study (ECASS). JAMA 274, 1017–1025.
Hacke, W., Kaste, M., Fieschi, C., von Kummer, R., Davalos, A., Meier, D., Larrue, V., Bluhmki, E., Davis, S., Donnan, G., Schneider, D., Diez-Tejedor, E., and Trouillas, P. (1998). Randomised double-blind placebo-controlled trial of thrombolytic therapy with intravenous alteplase in acute ischaemic stroke (ECASS II). Second European-Australasian acute stroke study investigators. Lancet 352, 1245–1251.
Haley, E. C., Jr., Lyden, P. D., Johnston, K. C., and Hemmen, T. M. (2005). A pilot dose-escalation safety study of tenecteplase in acute ischemic stroke. Stroke 36, 607–612.
Haley, E C., Jr., Thompson, J. L., Grotta, J. C., Lyden, P. D., Hemmen, T. G., Brown, D. L., Fanale, C., Libman, R., Kwiatkowski, T. G., Llinas, R. H., Levine, S. R., Johnston, K. C., Buchsbaum, R., Levy, G., and Levin, B. (2010). Phase IIB/III trial of tenecteplase in acute ischemic stroke: results of a prematurely terminated randomized clinical trial. Stroke 41, 707–711.
Harrer, J. U. (2010). Clinical applicability and the perfusion–diffusion mismatch theory: not yet a perfect match. Neurology 75, 1034–1035.
Heiss, W. D., Grond, M., Thiel, A., von Stockhausen, H. M., Rudolf, J., Ghaemi, M., Lottgen, J., Stenzel, C., and Pawlik, G. (1998). Tissue at risk of infarction rescued by early reperfusion: a positron emission tomography study in systemic recombinant tissue plasminogen activator thrombolysis of acute stroke. J. Cereb. Blood Flow Metab. 18, 1298–1307.
Henkes, H., Flesser, A., Brew, S., Miloslavski, E., Doerfler, A., Felber, S., Monstadt, H., and Kuehne, D. (2003). A novel microcatheter-delivered, highly-flexible and fully-retrievable stent, specifically designed for intracranial use. Technical note. Interv. Neuroradiol. 9, 391–393.
Higashida, R., Furlan, A., Roberts, H., Tomsick, T., Connors, B., Barr, J., Dillon, W., Warach, S., Broderick, J., Tilley, B., and Sacks, D. (2003). Trial design and reporting standards for intraarterial cerebral thrombolysis for acute ischemic stroke. J. Vasc. Interv. Radiol. 14(Pt 2), S493–S494.
IMS Study Investigators. (2004). Combined intravenous and intra-arterial recanalization for acute ischemic stroke: the interventional management of stroke study. Stroke 35, 904–911.
IMS II Trial Investigators. (2007). The interventional management of stroke (IMS) II study. Stroke 38, 2127–2135.
Josephson, S. A., Saver, J. L., and Smith, W. S. (2009). Comparison of mechanical embolectomy and intraarterial thrombolysis in acute ischemic stroke within the MCA: MERCI and multi MERCI compared to PROACT II. Neurocrit. Care 10, 43–49.
Katzan, I. L., Hammer, M. D., Hixson, E. D., Furlan, A. J., Abou-Chebl, A., and Nadzam, D. M. (2004). Utilization of intravenous tissue plasminogen activator for acute ischemic stroke. Arch. Neurol. 61, 346–350.
Keris, V., Rudnicka, S., Vorona, V., Enina, G., Tilgale, B., and Fricbergs, J. (2001). Combined intraarterial/intravenous thrombolysis for acute ischemic stroke. AJNR Am. J. Neuroradiol. 22, 352–358.
Khatri, P., Hill, M. D., Palesch, Y. Y., Spilker, J., Jauch, E. C., Carrozzella, J. A., Demchuk, A. M., Martin, R., Mauldin, P., Dillon, C., Ryckborst, K. J., Janis, S., Tomsick, T. A., and Broderick, J. P. (2008). Methodology of the interventional management of stroke III trial. Int. J. Stroke 3, 130–137.
Lee, K. Y., Kim, D. I., Kim, S. H., Lee, S. I., Chung, H. W., Shim, Y. W., Kim, S. M., and Heo, J. H. (2004). Sequential combination of intravenous recombinant tissue plasminogen activator and intra-arterial urokinase in acute ischemic stroke. AJNR Am. J. Neuroradiol. 25, 1470–1475.
Lee, M., Hong, K. S., and Saver, J. L. (2010). Efficacy of intra-arterial fibrinolysis for acute ischemic stroke: meta-analysis of randomized controlled trials. Stroke 41, 932–937.
Lees, K. R., Zivin, J. A., Ashwood, T., Davalos, A., Davis, S. M., Diener, H. C., Grotta, J., Lyden, P., Shuaib, A., Hardemark, H. G., Wasiewski, W. W. (2006). NXY-059 for acute ischemic stroke. N. Engl. J. Med. 354, 588–600.
Levy, D. E., Del Zoppo, G. J., Demaerschalk, B. M., Demchuk, A. M., Diener, H. C., Howard, G., Kaste, M., Pancioli, A. M., Ringelstein, E. B., Spatareanu, C., and Wasiewski, W. W. (2009). Ancrod in acute ischemic stroke: results of 500 subjects beginning treatment within 6 hours of stroke onset in the ancrod stroke program. Stroke 40, 3796–3803.
Lewandowski, C. A., Frankel, M., Tomsick, T. A., Broderick, J., Frey, J., Clark, W., Starkman, S., Grotta, J., Spilker, J., Khoury, J., and Brott, T. (1999). Combined intravenous and intra-arterial r-TPA versus intra-arterial therapy of acute ischemic stroke: emergency management of stroke (EMS) bridging trial. Stroke 30, 2598–2605.
Liebeskind, D. S., Pollard, J. R., Schwartz, E. D., Cucchiara, B. L., McGarvey, M. L., and Hurst, R. W. (2002). Vertebrobasilar thrombolysis with intravenous tirofiban: case report. J. Thromb. Thrombolysis 13, 81–84.
Mangiafico, S., Cellerini, M., Nencini, P., Gensini, G., and Inzitari, D. (2005). Intravenous glycoprotein IIb/IIIa inhibitor (tirofiban) followed by intra-arterial urokinase and mechanical thrombolysis in stroke. AJNR Am. J. Neuroradiol. 26, 2595–2601.
Martin-Schild, S., Shaltoni, H., Abraham, A. T., Barreto, A. D., Hallevi, H., Gonzales, N. R., Grotta, J. C., and Savitz, S. I. (2009). Safety of eptifibatide for subcortical stroke progression. Cerebrovasc. Dis. 28, 595–600.
MAST-E. (1996). Thrombolytic therapy with streptokinase in acute ischemic stroke. The multicenter acute stroke trial – Europe study group. N. Engl. J. Med. 335, 145–150.
MAST-I. (1995). Randomised controlled trial of streptokinase, aspirin, and combination of both in treatment of acute ischaemic stroke. Multicentre acute stroke trial – Italy (MAST-I) group. Lancet 346, 1509–1514.
Mazighi, M., Serfaty, J. M., Labreuche, J., Laissy, J. P., Meseguer, E., Lavallee, P. C., Cabrejo, L., Slaoui, T., Guidoux, C., Lapergue, B., Klein, I. F., Olivot, J. M., Abboud, H., Simon, O., Niclot, P., Nifle, C., Touboul, P. J., Raphaeli, G., Gohin, C., Claeys, E. S., and Amarenco, P. (2009). Comparison of intravenous alteplase with a combined intravenous-endovascular approach in patients with stroke and confirmed arterial occlusion (RECANALISE study): a prospective cohort study. Lancet Neurol. 8, 802–809.
Mori, E., Minematsu, K., Nakagawara, J., Yamaguchi, T., Sasaki, M., and Hirano, T. (2010). Effects of 0.6 mg/kg intravenous alteplase on vascular and clinical outcomes in middle cerebral artery occlusion: Japan alteplase clinical trial II (J-ACT II). Stroke 41, 461–465.
Mori, E., Yoneda, Y., Tabuchi, M., Yoshida, T., Ohkawa, S., Ohsumi, Y., Kitano, K., Tsutsumi, A., and Yamadori, A. (1992). Intravenous recombinant tissue plasminogen activator in acute carotid artery territory stroke. Neurology 42, 976–982.
National Institute of Neurological Disorders, and Stroke rt-PA Stroke Study Group. (1995). Tissue plasminogen activator for acute ischemic stroke. N. Engl. J. Med. 333, 1581–1587.
Nogueira, R. G., Yoo, A. J., Buonanno, F. S., and Hirsch, J. A. (2009). Endovascular approaches to acute stroke, part 2: a comprehensive review of studies and trials. AJNR Am. J. Neuroradiol. 30, 859–875.
Ogawa, A., Mori, E., Minematsu, K., Taki, W., Takahashi, A., Nemoto, S., Miyamoto, S., Sasaki, M., and Inoue, T. (2007). Randomized trial of intraarterial infusion of urokinase within 6 hours of middle cerebral artery stroke: the middle cerebral artery embolism local fibrinolytic intervention trial (MELT) Japan. Stroke 38, 2633–2639.
Pancioli, A. M., Broderick, J., Brott, T., Tomsick, T., Khoury, J., Bean, J., Del Zoppo, G., Kleindorfer, D., Woo, D., Khatri, P., Castaldo, J., Frey, J., Gebel, J., Jr., Kasner, S., Kidwell, C., Kwiatkowski, T., Libman, R, Mackenzie R., Scott, P., Starkman, S., and Thurman, R. J. (2008). The combined approach to lysis utilizing eptifibatide and rt-PA in acute ischemic stroke: the CLEAR stroke trial. Stroke 39, 3268–3276.
Penumbra Pivotal Stroke Trial Investigators. (2009). The penumbra pivotal stroke trial: safety and effectiveness of a new generation of mechanical devices for clot removal in intracranial large vessel occlusive disease. Stroke 40, 2761–2768.
Rha, J. H., and Saver, J. L. (2007). The impact of recanalization on ischemic stroke outcome: a meta-analysis. Stroke 38, 967–973.
Ringelstein, E. B., Biniek, R., Weiller, C., Ammeling, B., Nolte, P. N., and Thron, A. (1992). Type and extent of hemispheric brain infarctions and clinical outcome in early and delayed middle cerebral artery recanalization. Neurology 42, 289–298.
Schlaug, G., Benfield, A., Baird, A. E., Siewert, B., Lovblad, K. O., Parker, R. A., Edelman, R. R., and Warach, S. (1999). The ischemic penumbra: operationally defined by diffusion and perfusion MRI. Neurology 53, 1528–1537.
Serna-Candel, C., Lopez-Ibor, L., and Matias-Guiu, J. (2010). Endovascular treatment for acute stroke: an open field to begin. Neurologia 25, 273–278.
Shaltoni, H. M., Albright, K. C., Gonzales, N. R., Weir, R. U., Khaja, A. M., Sugg, R. M., Campbell, M. S., IIIrd, Cacayorin, E. D., Grotta, J. C., and Noser, E. A. (2007). Is intra-arterial thrombolysis safe after full-dose intravenous recombinant tissue plasminogen activator for acute ischemic stroke? Stroke 38, 80–84.
Sherman, D. G., Atkinson, R. P., Chippendale, T., Levin, K. A., Ng, K., Futrell, N., Hsu, C. Y., and Levy, D. E. (2000). Intravenous ancrod for treatment of acute ischemic stroke: the STAT study: a randomized controlled trial. Stroke treatment with ancrod trial. JAMA 283, 2395–2403.
Smith, W. S., Sung, G., Saver, J., Budzik, R., Duckwiler, G., Liebeskind, D. S., Lutsep, H. L., Rymer, M. M., Higashida, R. T., Starkman, S., Gobin, Y. P., Frei, D., Grobelny, T., Hellinger, F., Huddle, D., Kidwell, C., Koroshetz, W., Marks, M., Nesbit, G., and Silverman, I. E. (2008). Mechanical thrombectomy for acute ischemic stroke: final results of the multi MERCI trial. Stroke 39, 1205–1212.
Thomalla, G., Schwark, C., Sobesky, J., Bluhmki, E., Fiebach, J. B., Fiehler, J., Zaro Weber, O., Kucinski, T., Juettler, E., Ringleb, P. A., Zeumer, H., Weiller, C., Hacke, W., Schellinger, P. D., and Rother, J. (2006). Outcome and symptomatic bleeding complications of intravenous thrombolysis within 6 hours in MRI-selected stroke patients: comparison of a German multicenter study with the pooled data of ATLANTIS, ECASS, and NINDS tPA trials. Stroke 37, 852–858.
Tomsick, T., Brott, T., Barsan, W., Broderick, J., Haley, E. C., Spilker, J., and Khoury, J. (1996). Prognostic value of the hyperdense middle cerebral artery sign and stroke scale score before ultraearly thrombolytic therapy. AJNR Am. J. Neuroradiol. 17, 79–85.
Wahlgren, N., Ahmed, N., Davalos, A., Ford, G. A., Grond, M., Hacke, W., Hennerici, M. G., Kaste, M., Kuelkens, S., Larrue, V., Lees, K. R., Roine. R. O., Soinne, L., Toni, D., and Vanhooren, G. (2007). Thrombolysis with alteplase for acute ischaemic stroke in the safe implementation of thrombolysis in stroke-monitoring study (SITS-MOST): an observational study. Lancet 369, 275–282.
Wahlgren, N., Ahmed, N., Davalos, A., Hacke, W., Millan, M., Muir, K., Roine, R. O., Toni, D., and Lees, K. R. (2008). Thrombolysis with alteplase 3–4.5 h after acute ischaemic stroke (SITS-ISTR): an observational study. Lancet 372, 1303–1309.
Wardlaw, J. M., Zoppo, G., Yamaguchi, T., and Berge, E. (2003). Thrombolysis for acute ischaemic stroke. Cochrane Database Syst. Rev. 3, CD000213.
Wolpert, S. M, Bruckmann, H., Greenlee, R., Wechsler, L., Pessin, M. S., and del Zoppo, G. J. (1993). Neuroradiologic evaluation of patients with acute stroke treated with recombinant tissue plasminogen activator. The rt-PA acute stroke study group. AJNR Am. J. Neuroradiol. 14, 3–13.
Yamaguchi, T., Mori, E., Minematsu, K., Nakagawara, J., Hashi, K., Saito, I., and Shinohara, Y. (2006). Alteplase at 0.6 mg/kg for acute ischemic stroke within 3 hours of onset: Japan alteplase clinical trial (J-ACT). Stroke 37, 1810–1815.
Zaidat, O. O., Suarez, J. I., Santillan, C., Sunshine, J. L., Tarr, R.W., Paras, V. H., Selman, W. R., and Landis, D. M. (2002). Response to intra-arterial and combined intravenous and intra-arterial thrombolytic therapy in patients with distal internal carotid artery occlusion. Stroke 33, 1821–1826.
Keywords: fibrinolysis, bridging, thrombectomy, stroke
Citation: Knauer K and Huber R (2011) Fibrinolysis and beyond: bridging the gap between local and systemic clot removal. Front. Neur. 2:7. doi: 10.3389/fneur.2011.00007
Received: 06 September 2010;
Accepted: 02 February 2011;
Published online: 22 February 2011.
Edited by:
Shakir Husain Hakim, Max Institute of Neurosciences, IndiaReviewed by:
Amer Alshekhlee, St. Louis University, USAOssama Yassin Mansour, Alexandria University Hospital, Egypt
Copyright: © 2011 Knauer and Huber. This is an open-access article subject to an exclusive license agreement between the authors and Frontiers Media SA, which permits unrestricted use, distribution, and reproduction in any medium, provided the original authors and source are credited.
*Correspondence: Roman Huber, Department of Neurology, University of Ulm, Oberer Eselsberg 45, 89081 Ulm, Germany. e-mail:ci5odWJlckB1bmktdWxtLmRl
 K. Knauer
K. Knauer