- 1Epilepsy Center Frankfurt Rhine-Main and Department of Neurology, Goethe-University Frankfurt, Frankfurt am Main, Germany
- 2Epilepsy Center Hessen and Department of Neurology, Philipps-University Marburg, Marburg, Germany
- 3LOEWE Center for Personalized Translational Epilepsy Research (CePTER), Goethe-University Frankfurt, Frankfurt am Main, Germany
- 4Department of Clinical Neurosciences, University of Calgary, Calgary, AB, Canada
- 5Epilepsy Center Greifswald and Department of Neurology, Ernst-Moritz-Arndt-University Greifswald, Greifswald, Germany
Editorial on the Research Topic
Burden of Illness in People With Epilepsy: From Population-Based Studies to Precision Medicine
Epilepsy is a common and chronic neurological disease that is characterized by recurrent seizures which impose a major burden on patients, their caregivers, and society (1, 2). The aim of this Research Topic was thus to provide evidence that personalized translational epilepsy research will benefit patients through targeted experimental (3), clinical and network research (4, 5). There is a fast growing number of publications that deal with personalized or precision approaches for the treatment of epilepsy, Figure 1.
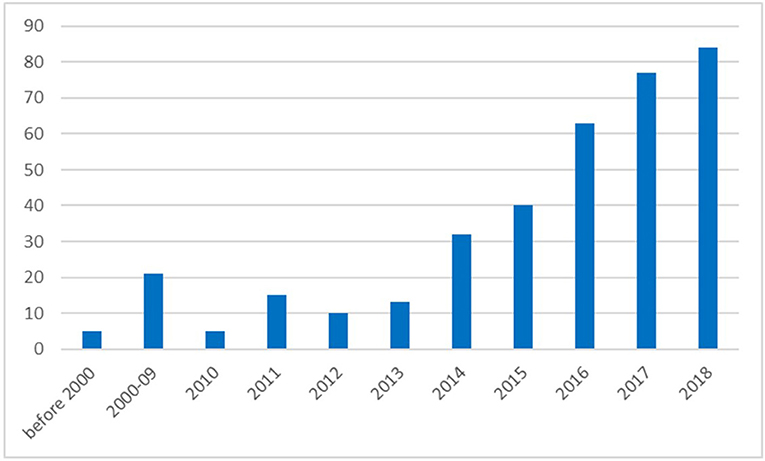
Figure 1. Number of publications listed in PubMed referring to search terms “Epilepsy” and “personalized” or “precision medicine” (PubMed query on September 13th 2018).
People with epilepsy face disease-specific restrictions concerning self-sufficiency, mobility, career choice, family planning, and other social aspects (6, 7). An analysis of patients with severe drug-refractory epilepsy showed a seven-fold increase in mortality, along with high costs and frequent epilepsy-related accidents and injuries (Strzelczyk et al.). The authors used a German health insurance database to administer a top-down approach, drawing patients from a representative cohort and matched them to a cohort that was not affected. Comorbidities, like depression and vascular disorders, were significantly increased in patients with epilepsy (Strzelczyk et al.). Focusing on epilepsy-related accidents and injuries, Willems et al. used a bottom-up approach in a cross-sectional study, and it showed that there was a possibility of a reduced quality of life and increased depression scores in affected patients (Willems et al.). The presented data in both studies fits well with other recent burden-of-disease studies that showed the costs for hospital treatment and anticonvulsants as being major cost drivers (8–11) and that persisting seizures were also associated with a reduced quality of life (12, 13).
While the use of newer anticonvulsants may be associated with increased costs, it also has the potential to significantly reduce the seizure burden. Brivaracetam is the latest anticonvulsant that has been approved as an add-on therapy for the treatment of focal-onset seizures (14). A single-center study from Marburg in Germany (Zahnert et al.) shows promising post-marketing results in a cohort of mainly drug-refractory patients, while another multi-center study focused on patients with epileptic encephalopathies (Willems et al.). In both studies, 50% responder rates of 35 to 45% were achieved, which were well in line with other postmarketing results (15–17).
The initial response to anticonvulsants is explored in patients with newly diagnosed epilepsy, and showed that the initial 6-month response, as well as the number of seizures prior to treatment and brain-imaging abnormalities, are important prognostic factors (Xia et al.).
Lifestyle-dependent factors are important, especially in genetic generalized epilepsies. Until now, it was unclear as to whether alcohol consumption has an impact on epilepsy in these patients (18). Even if the risk is generally increased in patients with epilepsy, patients with genetic generalized epilepsies have a particularly high risk of alcohol related-seizures after the consumption of a large amount of alcohol. This can also be attributed to accompanying factors, such as altered sleep architecture or impaired adherence to antiepileptic medication (Hamerle et al.).
The genetic architecture of common non-lesional focal epilepsies was evaluated in a study that uses a customized panel of 21 well-known focal epilepsy genes (Tsai et al.). The study revealed that only 1.85% (11/593 patients) carried pathogenic or likely pathogenic variants in these genes, and this indicated that other yet to be discovered genes play a role as well.
Comorbidities, such as cognitive issues, are often present in patients with epilepsy (19). Gorny et al. showed that not all scales that were used to assess global cognitive function, work reliably in patients with epilepsy.
Structural abnormalities associated with clinical and neuropsychological characteristics in genetic epilepsies was evaluated in two studies on juvenile myoclonic epilepsy (JME) using MRI diffusion tensor imaging (DTI), and in benign childhood epilepsy, with centrotemporal spikes (BECTS), which used the graph theory analysis based on the cortical gyrification index, respectively (Domin et al.; Jiang et al.). In JME, the extent of microstructural abnormalities within the subcortical networks, including cortico-cortical, thalamo-frontal, and cortico-spinal connections, determined the clinical manifestation and subtype of JME in the individual patient, such as photoparoxysmal responses or seizures with predominant motor symptoms (Domin et al.). In contrast, abnormal cortical folding that was mainly in the central region is presumably the neuroanatomical basis for BECTS (Jiang et al.). The findings of both studies are important steps for the establishing of the pathophysiological concepts found in genetic epilepsies.
A step forward in the care for people with epilepsy could be through the introduction of technological therapies. Page et al. pointed out in their perspective article that there has been an increase in patient-triggered interventions, a finding based on automated monitoring of indicators and risk factors facilitated by technological advances. The main goal of such interventions would be the reduction of epilepsy-related mortality with SUDEP (Sudden Unexpected Death in Epilepsy) being the main reason for epilepsy-related deaths (20, 21).
An important point on this road is the development of an automatic computer-based detection algorithm of seizures. In their review, Baumgartner et al. described the use of potential bio signals, such as scalp EEG, ECG, and surface EMG, which can be combined for an algorithm and implemented into devices. The daily work of clinicians may be significantly improved by the use of an automated long-term EEG review. This was described by Koren et al. as an automatic critical care EEG pattern detection method that would be helpful in reducing review times.
This Research Topic presents a compilation of different studies which increases the visibility of the high burden associated with epilepsy, along with providing some directions as to how personalized or precision approaches may help to overcome this burden. In the coming years we will see a dramatic increase in personalized or precision medicine, Figure 1, that will significantly contribute to the management of epilepsy.
Author Contributions
All authors listed have made a substantial, direct and intellectual contribution to the work, and approved it for publication.
Conflict of Interest Statement
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
References
1. Josephson CB, Patten SB, Bulloch A, Williams JVA, Lavorato D, Fiest KM, et al. The impact of seizures on epilepsy outcomes: a national, community-based survey. Epilepsia (2017) 58:764–71. doi: 10.1111/epi.13723
2. Strzelczyk A, Reese JP, Dodel R, Hamer HM. Cost of epilepsy: a systematic review. Pharmacoeconomics (2008) 26:463–76. doi: 10.2165/00019053-200826060-00002
3. Bauer S, van Alphen N, Becker A, Chiocchetti A, Deichmann R, Deller T, et al. Personalized translational epilepsy research - Novel approaches and future perspectives: part II: experimental and translational approaches. Epilepsy Behav. (2017) 76:7–12. doi: 10.1016/j.yebeh.2017.06.040
4. Rosenow F, van Alphen N, Becker A, Chiocchetti A, Deichmann R, Deller T, et al. Personalized translational epilepsy research - Novel approaches and future perspectives: part I: clinical and network analysis approaches. Epilepsy Behav. (2017) 76:13–8. doi: 10.1016/j.yebeh.2017.06.041
5. Reif PS, Tsai MH, Helbig I, Rosenow F, Klein KM. Precision medicine in genetic epilepsies: break of dawn? Expert Rev Neurother. (2017) 17:381–92. doi: 10.1080/14737175.2017.1253476
6. Smeets VM, van Lierop BA, Vanhoutvin JP, Aldenkamp AP, Nijhuis FJ. Epilepsy and employment: literature review. Epilepsy Behav. (2007) 10:354–62. doi: 10.1016/j.yebeh.2007.02.006
7. Jacoby A. Stigma, epilepsy, and quality of life. Epilepsy Behav. (2002) 3:10–20. doi: 10.1016/S1525-5050(02)00545-0
8. Puka K, Smith ML, Moineddin R, Snead OC, Widjaja E. The influence of socioeconomic status on health resource utilization in pediatric epilepsy in a universal health insurance system. Epilepsia (2016) 57:455–63. doi: 10.1111/epi.13290
9. Riechmann J, Strzelczyk A, Reese JP, Boor R, Stephani U, Langner C, et al. Costs of epilepsy and cost-driving factors in children, adolescents, and their caregivers in Germany. Epilepsia (2015) 56:1388–97. doi: 10.1111/epi.13089
10. Willems LM, Richter S, Watermann N, Bauer S, Klein KM, Reese JP, et al. Trends in resource utilization and prescription of anticonvulsants for patients with active epilepsy in Germany from 2003 to 2013 - A ten-year overview. Epilepsy Behav. (2018) 83:28–35. doi: 10.1016/j.yebeh.2018.03.025
11. Strzelczyk A, Bergmann A, Biermann V, Braune S, Dieterle L, Forth B, et al. Neurologist adherence to clinical practice guidelines and costs in patients with newly diagnosed and chronic epilepsy in Germany. Epilepsy Behav. (2016) 64(Pt A):75–82. doi: 10.1016/j.yebeh.2016.07.037
12. Taylor RS, Sander JW, Taylor RJ, Baker GA. Predictors of health-related quality of life and costs in adults with epilepsy: a systematic review. Epilepsia (2011) 52:2168–80. doi: 10.1111/j.1528-1167.2011.03213.x
13. Kortland LM, Knake S, von Podewils F, Rosenow F, Strzelczyk A. Socioeconomic outcome and quality of life in adults after status epilepticus: a multicenter, longitudinal, matched case-control analysis from Germany. Front Neurol. (2017) 8:507. doi: 10.3389/fneur.2017.00507
14. Strzelczyk A, Klein KM, Willems LM, Rosenow F, Bauer S. Brivaracetam in the treatment of focal and idiopathic generalized epilepsies and of status epilepticus. Expert Rev Clin Pharmacol. (2016) 9:637–45. doi: 10.1586/17512433.2016.1156529
15. Steinhoff BJ, Bacher M, Bucurenciu I, Hillenbrand B, Intravooth T, Kornmeier R, et al. Real-life experience with brivaracetam in 101 patients with difficult-to-treat epilepsy-A monocenter survey. Seizure (2017) 48:11–4. doi: 10.1016/j.seizure.2017.03.010
16. Steinig I, von Podewils F, Moddel G, Bauer S, Klein KM, Paule E, et al. Postmarketing experience with brivaracetam in the treatment of epilepsies: a multicenter cohort study from Germany. Epilepsia (2017) 58:1208–16. doi: 10.1111/epi.13768
17. Strzelczyk A, Kay L, Bauer S, Immisch I, Klein KM, Knake S, et al. Use of brivaracetam in genetic generalized epilepsies and for acute, intravenous treatment of absence status epilepticus. Epilepsia (2018) 59:1549–56. doi: 10.1111/epi.14476
18. Samokhvalov AV, Irving H, Mohapatra S, Rehm J. Alcohol consumption, unprovoked seizures, and epilepsy: a systematic review and meta-analysis. Epilepsia (2010) 51:1177–84. doi: 10.1111/j.1528-1167.2009.02426.x
19. Helmstaedter C, Witt JA. Epilepsy and cognition - A bidirectional relationship? Seizure (2017) 49:83–9. doi: 10.1016/j.seizure.2017.02.017
20. Thurman DJ, Hesdorffer DC, French JA. Sudden unexpected death in epilepsy: assessing the public health burden. Epilepsia (2014) 55:1479–85. doi: 10.1111/epi.12666
Keywords: epilepsy, seizure, anticonvulsant, antiepileptic drug (AED), quality of life, imaging
Citation: Strzelczyk A, Klein KM and von Podewils F (2019) Editorial: Burden of Illness in People With Epilepsy: From Population-Based Studies to Precision Medicine. Front. Neurol. 9:1164. doi: 10.3389/fneur.2018.01164
Received: 16 September 2018; Accepted: 17 December 2018;
Published: 09 January 2019.
Edited and reviewed by: Fernando Cendes, Universidade Estadual de Campinas, Brazil
Copyright © 2019 Strzelczyk, Klein and von Podewils. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Adam Strzelczyk, c3RyemVsY3p5a0BtZWQudW5pLWZyYW5rZnVydC5kZQ==
 Adam Strzelczyk
Adam Strzelczyk Karl Martin Klein
Karl Martin Klein Felix von Podewils
Felix von Podewils