- 1Department of Otorhinolaryngology–Head and Neck Surgery, University Medical Center Utrecht, Utrecht, Netherlands
- 2University Medical Center Utrecht Brain Center, University Medical Center Utrecht, Utrecht, Netherlands
Objectives: With this systematic review we aim to provide an overview of the evidence of the effect of Mindfulness Based Interventions (MBIs) on (1) tinnitus distress and (2) anxiety and/or depression in tinnitus patients.
Methods: We conducted a systematic search in PubMed Medline, EMBASE and PsycInfo combining the terms and synonyms of “Tinnitus” and “Mindfulness.” The most recent search was performed on December 4th 2018. We wrote this systematic review according to the Preferred Reporting Items for Systematic Reviews and Meta-Analyses (PRISMA). Two independent authors identified studies, assessed the risk of bias and extracted data. Studies were considered eligible if they included adults with tinnitus, performed a protocolled MBI and measured tinnitus distress with validated questionnaires. Studies were appraised with either the Cochrane Risk of Bias tool or the MINORS criteria, depending on their design.
Results: The systematic search yielded seven articles (425 patients). Three randomized controlled trials (RCTs), three cohort studies and one comparative controlled trial. Different types of MBIs, including MBCT and MBSR, were assessed with various questionnaires. Two of three RCTs showed a statistically significant decrease in tinnitus distress scores directly after treatment in the mindfulness group compared to the control group. Six of seven studies showed statistically significant decrease in tinnitus distress scores directly after mindfulness therapy. One of three RCTs showed a statistically significant improvement of depression questionnaire scores after MBI compared to the control group directly post treatment.
Conclusions: A decrease of tinnitus distress scores in MBIs can be observed directly post-therapy based on moderate to high quality studies. This was found regardless of the heterogeneity of patients, study design, type of MBI and outcome assessment. Two out of three RCTs found clinically relevant decreases in tinnitus distress scores. No effect of MBIs was observed for depression and anxiety in tinnitus patients. Long term effects remain uncertain. Mindfulness may have a place in tinnitus therapy, although the long term effects need to be studied.
Introduction
Tinnitus is the awareness of a ringing, buzzing or hissing sound in the ears or head without an external stimulus (1). The reported prevalence ranges between 10 and 15% (1). However, the experienced hindrance of tinnitus differs among patients: whilst some consider it negligible and grow accustomed to it, others are distressed and cope with a high level of disease. In 5% of the population mild to moderate disturbance by tinnitus is reported, while quality of life is severely reduced in 1–2% of tinnitus sufferers (1–4).
Tinnitus distress is described as a “multidimensional phenomenon that can be associated with problems such as difficulties with concentration, insomnia, or negative thinking which can amplify it in vicious cycles” (5)p1. Furthermore, suffering patients report hopelessness, exhaustion, feeling overwhelmed and even suicidal thoughts (2). Considering the broad range of difficulties patients with tinnitus experience and the diversity in associated co-morbidities, tinnitus perceptions (e.g., loudness, location), causal risk factors and levels of distress, tinnitus is considered a heterogeneous condition (6).
Rationale
No curative treatment for tinnitus has been found thus far, and evidence for therapy that diminishes tinnitus distress is limited (7). Cognitive Behavioral Therapy(CBT) has been proven effective in improving quality of life in tinnitus patients (8). CBT is a structured, time limited psychological therapy which is based on the idea that a person's perception is influenced by personal experiences (8). It encourages patients to use cognitive and behavioral tasks to modify their response to thoughts and situations (9). There is great variation within the CBT approaches for tinnitus, even though common elements are found. One of these approaches is Relaxation Therapy (RT), based on the work by Lars-Göran Ost. It teaches patients to relax rapidly, in order to reduce anxiety (10). In recent years the so-called third wave of CBT has gained more interest. Third-wave methods focus more on the patient's relationship to thoughts and emotions than on thought content, emphasizing acceptance and mindfulness (11).
Mindfulness can be defined as: “the effort to intentionally pay attention, non-judgementally, to present-moment experience and sustain this attention over time” (12)p123. It is the practice of intentionally and openly attending to what is happening in the present; to not lose focus because of thoughts or sensations, nor to judge them (13, 14). Mindfulness was introduced to modern western medicine in 1979 by Jon Kabat-Zinn (15). He adapted and adopted traditional ‘eastern' meditative techniques into a program systematically training mindfulness, known as Mindfulness Based Stress Reduction (MBSR) (15, 16). Since the introduction of MBSR, different types of courses that integrate mindfulness techniques in contemporary psychological practice have been developed. These are collectively referred to as Mindfulness-Based Interventions (MBIs) (17). MBIs emphasize formal meditation and aim to help incorporate mindfulness in daily life (17). It involves control of attention and acceptance of present moment experiences (14). Segal et al. adapted the MBSR program to combine CBT and mindfulness techniques in order to treat relapsing depression; this was called Mindfulness Based Cognitive Therapy (MBCT) (18, 19). Both interventions (MBSR and MBCT) consist of 8 weekly group classes that last 2–2.5 h with a potential, one-time, all-day retreat. Homework and exercises to integrate mindfulness technique in normal daily life play an important role in both interventions (17). MBIs have been proven effective in treating several conditions such as stress, anxiety, depression, and chronic pain, all symptoms that are also associated with tinnitus (20–23).
Mindfulness is thought to work by changing the perception of negative experiences, making them less emotionally destructive. Patients are believed to become more aware and less preoccupied by physical or mental sensations after a MBI (14, 24). Avoidance is associated with tinnitus severity and distress. Acceptance, a key element of mindfulness, is the exact opposite of avoidance, which could help tinnitus sufferers to benefit from a MBI (25, 26).
Objectives and Research Question
The primary objective of this study is to systematically assess the effect of MBIs on tinnitus distress in the literature. Our secondary objective is to assess the effect of MBIs on depression and/or anxiety in tinnitus patients.
Methods
Study Design
We considered randomized controlled trials (RCTs), and observational studies [retrospective and prospective cohort studies and case series (n ≥ 5)]. We included studies if they included adults with tinnitus, with all types of protocolled MBIs.
The primary outcome measure was tinnitus distress measured with a validated questionnaire. The secondary outcome measures were depression and/or anxiety measured with a validated questionnaire.
Participants, Interventions, Comparators
We searched for studies in accordance with the PICO search method (Patients, Intervention, Comparison, and Outcome). P: adults with tinnitus, I: protocolled MBI, C: any other therapy or no therapy and O: tinnitus distress, depression and/or anxiety measured with validated questionnaires. Only articles with original data were included for full text screening.
Systematic Review Protocol
We did not create a review protocol. This review was written according to the Preferred Reporting Items for Systematic Reviews and Meta-Analyses (PRISMA) (27).
Search Strategy
We conducted a systematic search on December 4th, 2018. The search was created and conducted by the review team (MR, KH, DS, IS). There were no restrictions regarding publication year, language, or publication status.
Electronic database searches were performed in PubMed, EMBASE, and PsycInfo. The search terms can be found in Supplementary Material. Search terms were based on the PICO search method, in which a combination of synonyms for the P (patients) and the I (interventions) were searched. Reference lists and citations of included articles were scanned to identify possible relevant studies. ClinicalTrials.org was searched for ongoing trials and protocols.
Data Sources, Studies Sections, and Data Extraction
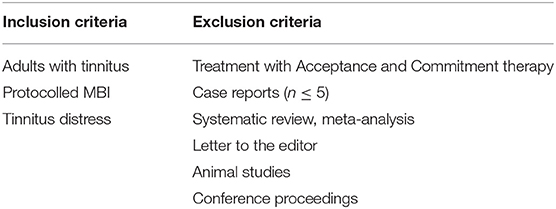
Two authors (MR and KH) selected applicable studies. Title-abstract and full-text screening were performed by two independent authors (MR and KH) and based on predefined inclusion and exclusion criteria (Table 1).
Original data from included articles were extracted by two authors (MR and IS). The following data was extracted, if provided: (1) total number of participants in each study, (2) total number of patients in each group, (3) intervention type and frequency, (4) outcome data pre-intervention, post-intervention and at 3 and 6 months follow up, (5) mean difference and p-values. If data was not provided, it was extracted from figures if possible. If mean differences were not provided, they were calculated if possible.
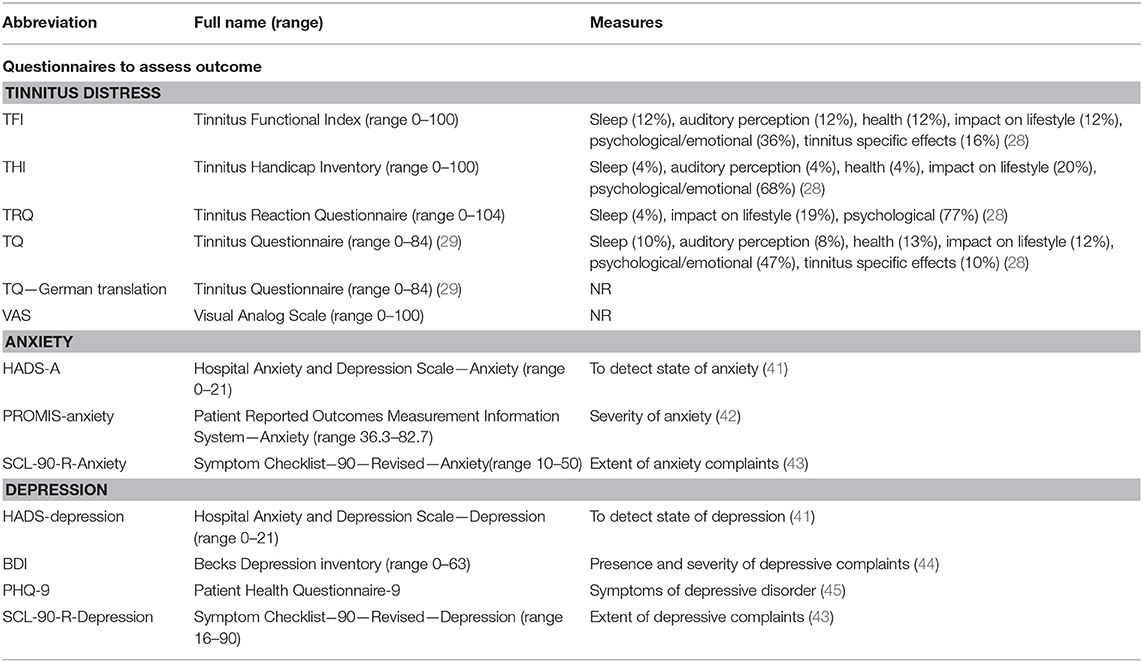
Differences on the questionnaires were considered clinically relevant if they reached a published minimal clinical important difference (MCID) [German Tinnitus Questionnaire (TQ) 12 points, Tinnitus Handicap Inventory (THI) 7 points, Tinnitus Functional Index (TFI) 13 points] (28–30).
Selected studies were critically appraised by two independent authors (MR and KH). Disagreements were solved by discussion. We included RCTs and observational studies. The RCTs were assessed with the Cochrane Risk of Bias Tool (31). The observational and the comparative controlled trial were assessed with the MINORS tool. Items were scored as 0 (not reported), 1 (reported but inadequate) or 2 (reported and adequate) (32).
Data Analysis
Meta-analyses were performed in case of homogenous outcomes.
Result
Study Selection and Characteristics
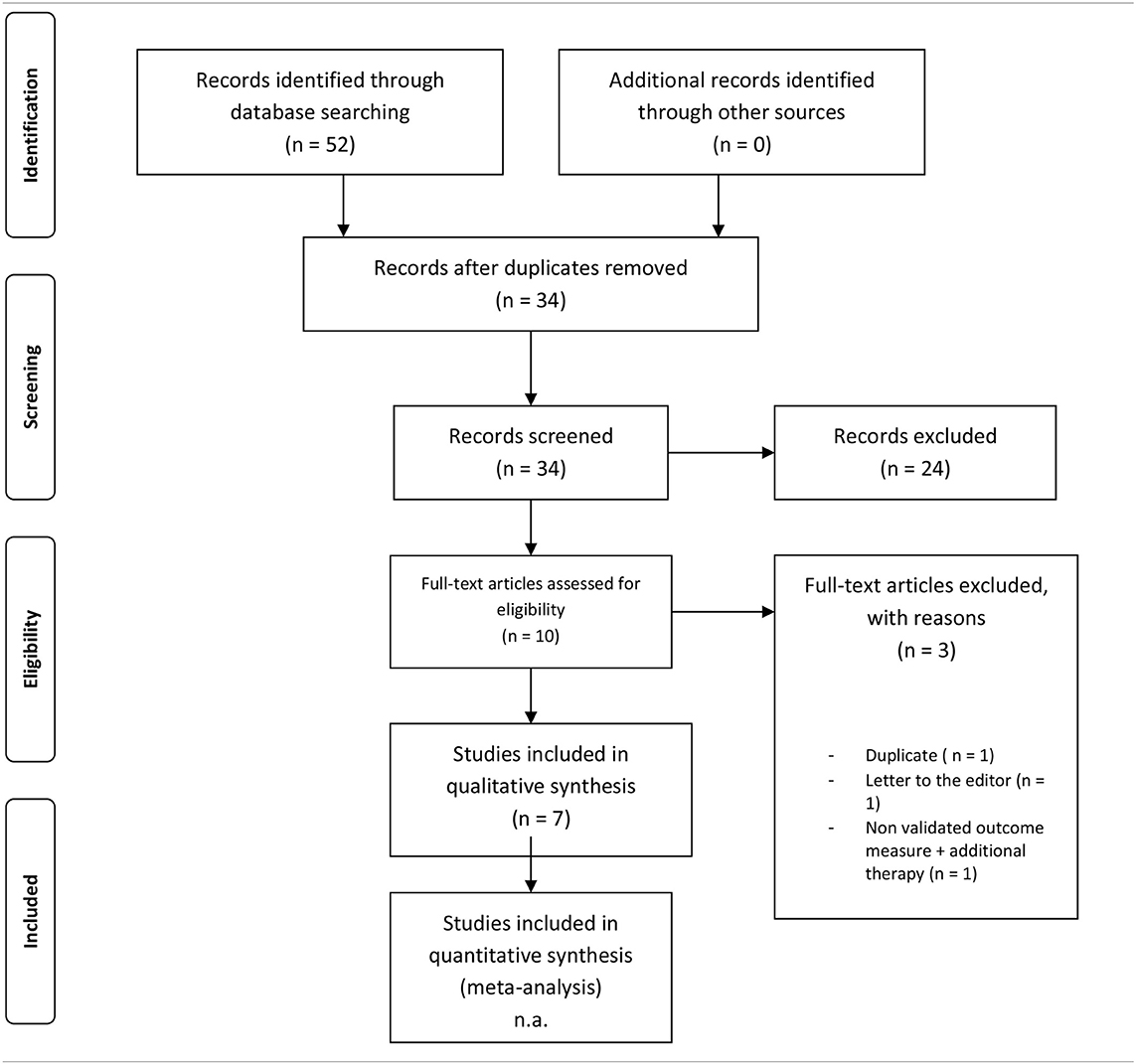
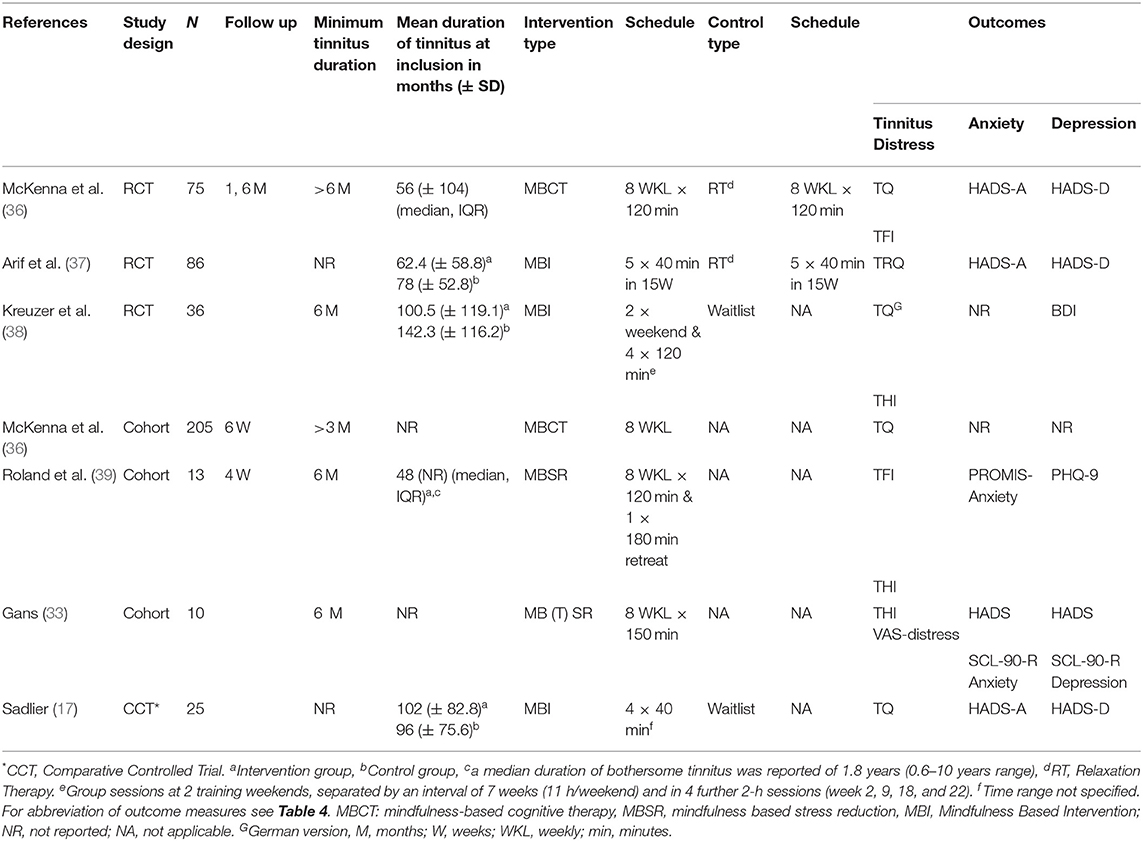
The electronic search of PubMed, EMBASE, and PsycInfo yielded 52 results. After removal of 18 duplicates, 34 studies were screened on title and abstract. Title/abstract screening resulted in 10 articles. Three articles were excluded: one was a duplicate (33), one was a letter to the editor (34), and one did not use a validated outcome measure in addition to including supplementary therapy to a MBI (35). We included 7 studies in this review (n = 425 patients, range of 8–182 patients per study) published between 2007 and 2017 (13, 24, 36–40) (Table 2).
Three RCTs (35–37) one comparative controlled trial (13) and three cohort studies (24, 39, 40) were included in our review. Six out of the seven studies assessed the outcome only at the end of therapy, while one study had a follow up at 6 months (RCT) (36). Characteristics of the included studies are summarized in Table 3. Different types of questionnaires were used to measure outcomes of tinnitus distress, anxiety or depression; these are described in Table 4. In the article by Kreuzer et al. post therapy was considered to be the measurement after week 24 (38). Data on the TQ from Sadlier was deducted by manual measurements (13).
Two studies used MBCT (24, 36) and two studies used MBSR, all according to the general standards for these treatments (as stated in the section Introduction) (39, 40). Gans et al. adapted the MBSR program to Mindfulness Based Tinnitus Stress Reduction (MBTSR), where the central focus was placed on psychoeducation related to co-occurring complaints in tinnitus patients. Class-time was focused on the awareness of sound and tinnitus perception (40).
Three other studies used different MBIs (13, 37, 38). Of these, Arif et al. administered “mindfulness meditation” conducted by a single experienced therapist, which consisted of five (40 min) sessions over a period of 15 weeks. The therapy included in-session exercises and homework (37). Kreuzer et al. administered a “mindfulness- and body-psychotherapy based group treatment”, conducted by a single experienced therapist. Participants received 2 weekends (11 h per weekend, 7 weeks apart) of therapy (including self-massage, breathing exercises, mindfulness meditation). Two weeks after each weekend and 11 and 15 weeks after the second training there was a 2 h review meeting. Homework was encouraged (38). Sadlier et al. administered a “mindfulness meditation cognitive behavioral therapy approach,” which was based on the work of Kabat-Zinn (15). Patients received four therapy sessions of 40 min each. The therapy involved a blend of approaches using CBT and mindfulness meditation. Mindfulness was introduced in the third session (13).
Relaxation Therapy (RT) was used as control group in two of the included RCTs; (10, 36, 37) McKenna et al. applied the RT in eight weekly sessions, while Arif et al. provided five sessions of RT in 15 weeks (36, 37). In the RCT by Kreuzer et al. a waiting list served as the control group, which was similar to the included comparative controlled trial by Sadlier et al. (13) and Kreuzer et al. (38).
Risk of Bias Assessment
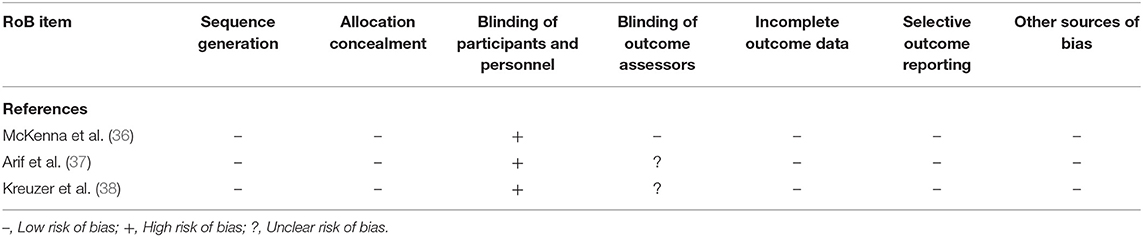
Cochrane Risk of Bias Assessment for Included RCTs
The items sequence generation, allocation concealment, incomplete outcome data, selective outcome reporting, and other sources of bias were scored as low risk of bias in all three RCTs (36–38). Blinding of participants and personnel scored high risk of bias in all three studies; this is inherent to the intervention. For outcome assessment McKenna et al. scored a low risk, the other two RCTs scored an unclear risk (Table 5).
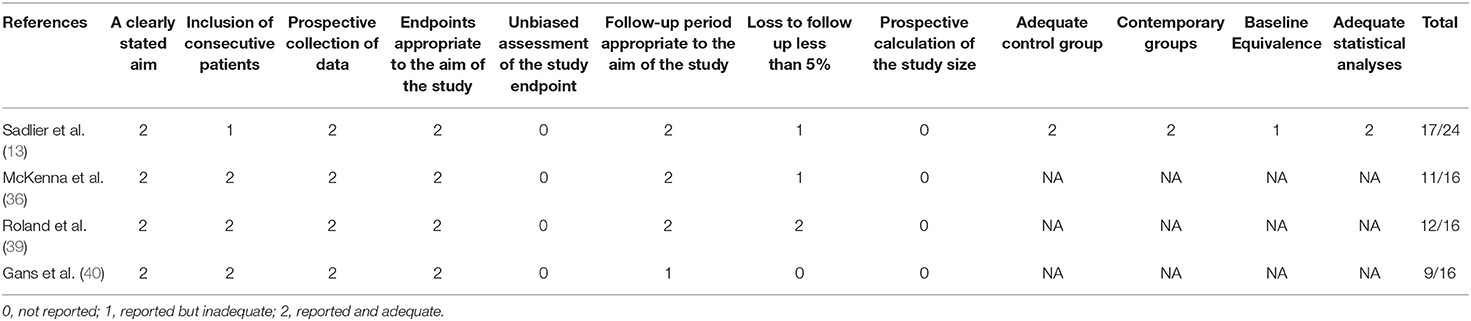
MINORS Criteria for Included Non-randomized Studies
“Reported and adequate” was scored for the items a clearly stated aim, prospective collection of data and endpoint appropriate to the aim of the study in all four included non-randomized studies (13, 24, 39, 40). “Reported and adequate” was scored on adequate control group, contemporary groups and adequate statistical analyses for Sadlier, where other studies scored “not applicable” (13). The items unbiased assessment of the study endpoint and prospective calculation of the study size were all scored as “not reported” (Table 6).
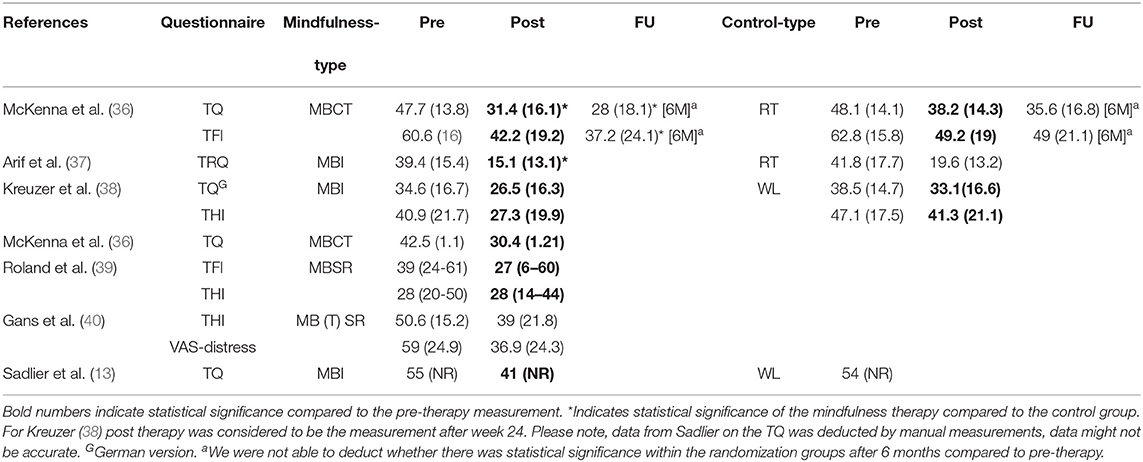
Primary Outcome
Two out of three RCTs showed a significantly higher decrease in tinnitus distress after treatment in the mindfulness therapy group compared to the control groups (36, 37). Of these, the RCT by McKenna et al. compared MBCT to RT and found a statistically significant improvement on the TQ of (adjusted mean difference, AMD)−6.3 points (95% CI −11.5 to −1.2, p = 0.016) compared to RT, while no statistically significant difference was seen between both treatments by usage of the TFI (AMD−4.8 points (95% CI −12.2 to 2.5), p = 0.199] (36). The second RCT by Arif et al. compared a MBI to RT using the Tinnitus Reaction Questionnaire (TRQ) and found a statistically significant improvement of tinnitus distress after MBI compared to the control group (mean difference−8.2 point (95% CI −16.4 to −0.1, p = 0.047) (37). Of these studies only McKenna et al. included an outcome assessment at 6 months follow-up, where a superior effect of MBI was still seen over RT for the TQ score (AMD−7.2 points (95% CI −12.3 to −2.1, p = 0.006) and the TFI score (AMD−9.6 points (95% CI −17 to −2.3, p = 0.011) (36). The third RCT by Kreuzer et al., comparing MBI to a waiting list, did not find a statistically significant difference between both groups after treatment for the TQ and THI (38) (Table 7).
Considering the effect of different mindfulness therapies, all seven randomized and non-randomized studies reported a lower score on the different tinnitus distress questionnaires post-treatment compared to pre-treatment scores. Six out of the seven studies demonstrated a statistically significant reduction after treatment with MBIs (Table 7).
Secondary Outcome
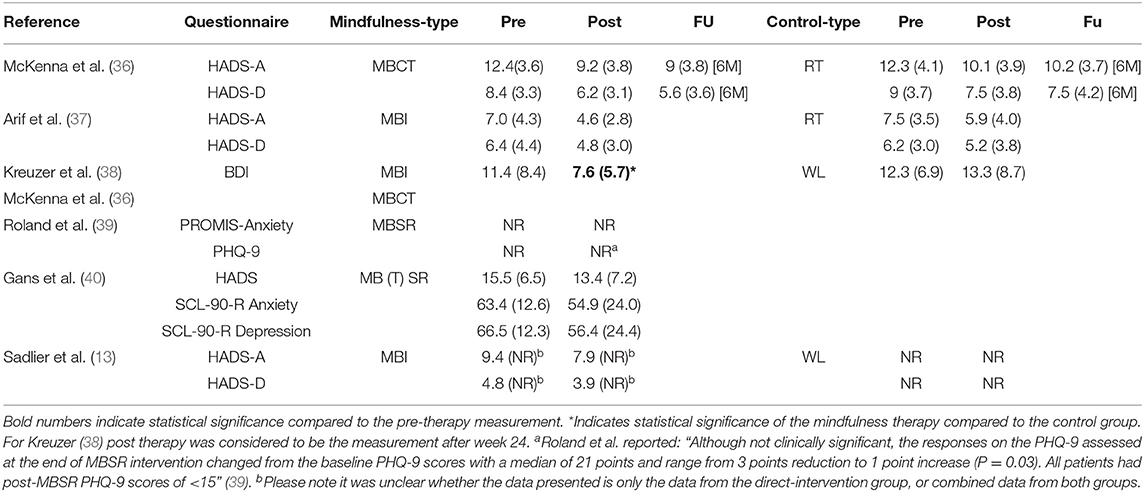
Six out of the seven included studies reported outcomes of anxiety and depression measurement.
Only one out of three RCTs showed a statistically significant decreased depression score (Becks Depression Inventory, BDI) in the MBI group compared to the control group (waiting list) directly after treatment (p = 0.035) (38).
Considering the effect post-treatment vs. pre-treatment, all six studies showed lower absolute scores for anxiety and depression outcomes after a MBI on different questionnaires (Table 8). Only one study showed a statistically significant decreased depression score (BDI) after MBI [p = 0.024, calculated mean difference−3.8 (95% CI −7.3 to −0.3)] (38). Due to heterogeneous designs, interventions and outcome measures, we were not able to pool the data nor conduct a meta-analysis.
Discussion
Summary of Main Findings
In this study we assessed the effect of MBIs on tinnitus distress. Our search yielded seven articles, consisting of three RCTs, three cohort studies, and one comparative controlled trial. The three RCTs had a low risk of bias; the cohort studies and the comparative controlled trial had medium risk of bias.
Two out of three RCTs showed a statistically significant reduction in tinnitus distress directly after treatment in the mindfulness group compared to the control group (both RT).The observed changes in TFI scores in the RCTs by McKenna et al. and Arif et al. are considered clinically relevant by exceeding the MCID on the TFI (13 points) (28, 36, 37). Interestingly, the third RCT comparing the effect of a MBI to a waiting list group didn't show statistically significant differences (38). Besides differences in the comparison, we observed differences in timing and scheduling of MBIs. However, to what extent this can explain differences in outcome cannot be answered by our review.
In six out of seven included studies, a statically significant decrease of tinnitus distress scores was observed directly post treatment, regardless of MBIs, study designs and type of questionnaire (13, 24, 36–39). These decreases reached MCID in three out of six studies (36, 38, 40).
Long term outcome (6 months) was only assessed by one RCT (36). A persistent statistically significant decrease in tinnitus distress scores was observed after 6 months, compared to pre- and directly posttreatment scores (36). In an additional letter to the editor, Gans et al. reported a sustained effect of the MB (T) SR therapy 1 year after treatment in a small set of patients attending, subsequent follow-up assessment (34). This limited insight in the long term results of MBI on tinnitus distress hinders strong conclusions and needs further exploration.
There are several overlapping psychological, theoretical frameworks that attempt to explain the mechanisms of improved tolerance of tinnitus (9, 26, 46). The use of CBT, including third-wave approaches, is generally based on these models. These include habituation and cognitive techniques that intervene in dysfunctional responses (26). Tinnitus severity is associated with negative cognitions (47). Mindfulness is believed to increase cognitive and metacognitive awareness, whereby negative thoughts will become less emotionally destructive in tinnitus patients (9, 36). Additionally, the persistence of tinnitus can lead to conditioned fear responses such as avoidance, which is associated with tinnitus severity and distress (25, 26). By advocating acceptance rather than avoidance, mindfulness might be beneficial to tinnitus patients to lower tinnitus distress (26, 48).
In regard to the secondary outcome of anxiety and depression, one out of the three RCTs showed statistically significant decreased depression scores after MBI compared to the control group (waiting list) (38). Only one out of the six studies demonstrated a statistically significant reduction of scores on a depression questionnaire after MBI compared to the pre-treatment condition (38). Regardless of treatment group (mindfulness or control), the scores on the different anxiety/depression questionnaires were all relatively low at the pre-treatment measurement (reported range of pre-treatment HADS-A: 7.0–12.4, HADS-D: 4.8–8.4 (norm range 0–21, 8–10 = possible anxiety/depression)/pre-treatment BDI 11.4 (norm range 0–63, 0–13 = minimal depression) (Table 4).
In literature MBIs have been demonstrated to be effective in reducing depressive symptoms and anxiety for non-tinnitus patients (18). This can be beneficial for tinnitus patients as these symptoms are often related to the tinnitus complaints. No effects of MBIs were observed in our study, potentially due to the low anxiety and depression scores pre-treatment. A meta-analysis by Hofmann et al. showed that in patients with elevated levels of anxiety and depression but with other primary complaints, the effect size after a MBI is smaller than in patients with anxiety or depression as their primary complaint (21). This could also possibly explain the lack of effect of MBIs on anxiety and depression scores.
Some biases in the included studies need to be taken into consideration. Firstly, only one study investigated the effect of a MBI (MBCT) after 6 months. Even though the reduced tinnitus distress scores were maintained after 6 months, the effectiveness of MBIs over time remains uncertain (36). Secondly, there is a large heterogeneity in outcome measures used in the included studies, which hinders generalization of results. Even though all have been validated, each questionnaire addresses a slightly different domain of tinnitus and its impact (28). Nevertheless, the majority of included tinnitus distress questionnaires used in this review (TQ, TRQ, THI, and TFI) has a strong focus on the psychological/emotional domain. Thirdly, in this review the studied patient population is heterogeneous (e.g., minimum tinnitus duration at inclusion, mean tinnitus duration, different ranges of initial tinnitus distress at inclusion) with a large spread of outcomes after intervention. This also suggests a high heterogeneity in the different tinnitus patients and/or effects of therapy. Because one treatment will most likely not benefit all patients, a “subgroup” analysis might be needed to assess the therapeutical effects in relation to specific patient or disease related characteristics (6, 49). Fourthly, the heterogeneity in treatment protocols underlines the need for determining which elements are essential to successful MBIs for tinnitus.
Conclusions
In this systematic review we found beneficial effects of MBIs on decrease in tinnitus distress scores, regardless of the heterogeneity of tinnitus patients, study designs, interventions and outcome measures. Two out of three RCTs found clinically relevant decreases in tinnitus distress scores. The included studies were of moderate to high quality. No effects of MBIs were observed for depression and/or anxiety. Conclusions concerning long term effects cannot be drawn, we therefore advise future trials to include a longer follow up.
Author Contributions
MR, AS, KH, and IS designed the study, created and conducted the search. MR and KH selected the applicable studies, title-abstract, and full-text screening were performed by MR and KH. Original data from included articles were extracted by MR and IS. Risk of Bias was assessed by MR and KH. The manuscript was written by MR, KH, IS, RS, and AS critically revised the work and approved the final version to be published.
Conflict of Interest
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
Supplementary Material
The Supplementary Material for this article can be found online at: https://www.frontiersin.org/articles/10.3389/fneur.2019.01135/full#supplementary-material
References
1. Langguth B, Kreuzer PM, Kleinjung T, De Ridder D. Tinnitus: causes and clinical management. Lancet Neurol. (2013) 12:920–30. doi: 10.1016/S1474-4422(13)70160-1
2. Marks E, Smith P, McKenna L. Living with tinnitus and the health care journey: An interpretative phenomenological analysis. Br J Health Psychol. (2019) 24:250–64. doi: 10.1111/bjhp.12351
3. Fujii K, Nagata C, Nakamura K, Kawachi T, Takatsuka N, Oba S, et al. Prevalence of tinnitus in community-dwelling Japanese adults. J Epidemiol. (2011) 21:299–304. doi: 10.2188/jea.JE20100124
4. Henry JA, Dennis KC, Schechter MA. General review of tinnitus: Prevalence, mechanisms, effects, and management. J Speech Lang Hear Res. (2005) 48:1204–35. doi: 10.1044/1092-4388(2005/084)
5. Brüggemann P, Szczepek AJ, Rose M, McKenna L, Olze H, Mazurek B. Impact of multiple factors on the degree of tinnitus distress. Front Hum Neurosci. (2016) 10:341. doi: 10.3389/fnhum.2016.00341
6. Cederroth CR, Gallus S, Hall DA, Kleinjung T, Langguth B, Maruotti A, et al. Editorial: towards an understanding of tinnitus heterogeneity. Front Aging Neurosci. (2019) 11:53. doi: 10.3389/fnagi.2019.00053
7. McFerran DJ, Stockdale D, Holme R, Large CH, Baguley DM. Why is there no cure for tinnitus? Front Neurosci. (2019) 13:802. doi: 10.3389/fnins.2019.00802
8. Martinez-Devesa P, Perera R, Theodoulou M, Waddell A. Cognitive behavioural therapy for tinnitus. Cochrane Database Syst Rev. (2010). CD005233. doi: 10.1002/14651858.CD005233.pub3
9. McKenna L, Handscomb L, Hoare DJ, Hall DA. A scientific cognitive-behavioral model of tinnitus: Novel conceptualizations of tinnitus distress. Front Neurol. (2014) 5:196. doi: 10.3389/fneur.2014.00196
10. Öst LG. Applied relaxation: description of a coping technique and review of controlled studies. Behav Res Ther. (1987) 25:397–409. doi: 10.1016/0005-7967(87)90017-9
11. Hayes SC, Hofmann SG. The third wave of cognitive behavioral therapy and the rise of process-based care. World Psychiatry. (2017) 16:245–6. doi: 10.1002/wps.20442
12. Miller JJ, Fletcher K, Kabat-Zinn J. Three-year follow-up and clinical implications of a mindfulness meditation-based stress reduction intervention in the treatment of anxiety disorders. Gen Hosp Psychiatry. (1995) 17:192–200. doi: 10.1016/0163-8343(95)00025-M
13. Sadlier M, Stephens SDG, Kennedy V. Tinnitus rehabilitation: a mindfulness meditation cognitive behavioural therapy approach. J Laryngol Otol. (2008) 122:31–7. doi: 10.1017/S0022215107007438
14. Bishop SR, Lau M, Shapiro S, Carlson L, Anderson ND, Carmody J, et al. Mindfulness: a proposed operational definition. Clin Psychol Sci Pract. (2004) 11:230–41. doi: 10.1093/clipsy.bph077
15. Kabat-Zinn J. An outpatient program in behavioral medicine for chronic pain patients based on the practice of mindfulness meditation - theoretical considerations and preliminary-results. Gen Hosp Psychiatry. (1982) 4:33–47. doi: 10.1016/0163-8343(82)90026-3
16. Segal ZV, Williams JMG, Teasdale JD. Mindfulness Based Cognitive Therapy for Depression: A New Approach to Preventing Relapse. New York, NY: Guildford Press (2002).
17. Shapero BG, Greenberg J, Pedrelli P, de Jong M, Desbordes G. Mindfulness-based interventions in psychiatry. Focus. (2018) 16:32–9. doi: 10.1176/appi.focus.20170039
18. Creswell JD. Mindfulness interventions. Annu Rev Psychol. (2017) 68:491–516. doi: 10.1146/annurev-psych-042716-051139
19. Segal Z V, Walsh KM. Mindfulness-based cognitive therapy for residual depressive symptoms and relapse prophylaxis. Curr Opin Psychiatry. (2016) 29:7–12. doi: 10.1097/YCO.0000000000000216
20. Bohlmeijer E, Prenger R, Taal E, Cuijpers P. The effects of mindfulness-based stress reduction therapy on mental health of adults with a chronic medical disease: a meta-analysis. J Psychosom Res. (2010) 68:539–44. doi: 10.1016/j.jpsychores.2009.10.005
21. Hofmann SG, Sawyer AT, Witt AA, Oh D. The effect of mindfulness-based therapy on anxiety and depression: a meta-analytic review. J Consult Clin Psychol. (2010) 78:169–83. doi: 10.1037/a0018555
22. Morone NE, Greco CM, Weiner DK. Mindfulness meditation for the treatment of chronic low back pain in older adults: a randomized controlled pilot study. Pain. (2008) 134:310–9. doi: 10.1016/j.pain.2007.04.038
23. Yeung S, Wong S, Chan FWK, Wong RLP, Chu MC, Lam YYK, et al. Comparing the effectiveness of mindfulness-based stress reduction and multidisciplinary intervention programs for chronic pain a randomized comparative trial. Clin J Pain. (2011) 27:724–34. doi: 10.1097/AJP.0b013e3182183c6e
24. McKenna L, Elizabeth EM, Ovid VF. Mindfulness-based cognitive therapy for chronic tinnitus: evaluation of benefits in a large sample of patients attending a tinnitus clinicl link. Ear Hear. (2018) 39:359–66. doi: 10.1097/AUD.0000000000000491
25. Hesser H, Andersson G. The role of anxiety sensitivity and behavioral avoidance in tinnitus disability. Int J Audiol. (2009) 48:295–9. doi: 10.1080/14992020802635325
26. Cima RFF. Bothersome tinnitus: cognitive behavioral perspectives. HNO. (2018) 66:369–74. doi: 10.1007/s00106-018-0502-9
27. Moher D, Liberati A, Tetzlaff J, Altman DG, Altman D, Antes G, et al. Preferred reporting items for systematic reviews and meta-analyses: the PRISMA statement (Chinese edition). J Chin Integr Med. (2009) 7:889–96. doi: 10.3736/jcim20090918
28. Fackrell BYK, Hoare D. Questionnaires to measure tinnitus severity. ENT&Audiology News. (2014) 22:4–6.
29. Hall DA, Mehta RL, Argstatter H. Interpreting the Tinnitus Questionnaire (German version): what individual differences are clinically important? Int J Audiol. (2018) 57:553–7. doi: 10.1080/14992027.2018.1442591
30. Henry JA, Griest S, Thielman E, McMillan G, Kaelin C, Carlson KF. Tinnitus functional index: development, validation, outcomes research, and clinical application. Hear Res. (2016) 334:58–64. doi: 10.1016/j.heares.2015.06.004
31. Higgins J, Green S. Cochrane Handbook for Systematic Reviews of Interventions Version 5.1.0. The Cochrane Collaboration (2011). p. 1–739. Available online at: www.handbook.cochrane.org
32. Slim K, Nini E, Forestier D, Kwiatkowski F, Panis Y, Chipponi J. Methodological index for non-randomized studies (Minors): development and validation of a new instrument. ANZ J Surg. (2003) 73:712–6. doi: 10.1046/j.1445-2197.2003.02748.x
33. Gans J. P02.20. Mindfulness based tinnitus stress reduction (MBTSR) pilot study: a symptom perception shift program. BMC Complement Altern Med. (2012) 12:P76. doi: 10.1186/1472-6882-12-S1-P76
34. Gans JJ, Cole MA, Greenberg B. Sustained benefit of mindfulness-based tinnitus stress reduction (MBTSR) in adults with chronic tinnitus: a pilot study. Mindfulness. (2015) 6:1232–4. doi: 10.1007/s12671-015-0403-x
35. Philippot P, Nef F, Clauw L, Romrée M, Segal Z. A randomized controlled trial of mindfulness-based cognitive therapy for treating tinnitus. Clin Psychol Psychother. (2012) 19:411–9. doi: 10.1002/cpp.756
36. McKenna L, Marks EM, Hallsworth CA, Schaette R. Mindfulness-based cognitive therapy as a treatment for chronic tinnitus: a randomized controlled trial. Psychother Psychosom. (2017) 86:351–61. doi: 10.1159/000478267
37. Arif M, Sadlier M, Rajenderkumar D, James J, Tahir T. A randomised controlled study of mindfulness meditation versus relaxation therapy in the management of tinnitus. J Laryngol Otol. (2017) 131:501–7. doi: 10.1017/S002221511700069X
38. Kreuzer PM, Goetz M, Holl M, Schecklmann M, Landgrebe M, Staudinger S, et al. Mindfulness-and body-psychotherapy-based group treatment of chronic tinnitus: a randomized controlled pilot study. BMC Complement Altern Med. (2012) 12:235. doi: 10.1186/1472-6882-12-235
39. Roland LT, Lenze EJ, Hardin FM, Kallogjeri D, Nicklaus J, Wineland AM, et al. Effects of mindfulness based stress reduction therapy on subjective bother and neural connectivity in chronic tinnitus. Otolaryngol Head Neck Surg. (2015) 152:919–26. doi: 10.1177/0194599815571556
40. Gans JJ, O'Sullivan P, Bircheff V. Mindfulness based tinnitus stress reduction pilot study: a symptom perception-shift program. Mindfulness. (2014) 5:322–33. doi: 10.1007/s12671-012-0184-4
41. Zigmond AS SR. The hospital anxiety and depression scale. Acta Psychiatr Scand. (1983) 67:361–70. doi: 10.1111/j.1600-0447.1983.tb09716.x
42. Pilkonis PA, Choi SW, Reise SP, Stover AM, Riley WT, Cella D. Item banks for measuring emotional distress from the patient-reported outcomes measurement information system (PROMIS®): Depression, anxiety, and anger. Assessment. (2011) 18:263–83. doi: 10.1177/1073191111411667
43. Derogatis LR. SCL−90–R: Administration, Scoring, and Procedures Manual II. Baltimore: MD: Clinical Psychometric Research (1983).
44. Beck AT SR. Internal consistencies of the original and revised beck depression inventory. J Clin Psychol. (1984) 40:1365–7.
45. Kroenke K, Spitzer Rl WJ. The PHQ-9: validity of a brief depression severity measure. J Gen Intern Med. (2001) 16:606–13. doi: 10.1046/j.1525-1497.2001.016009606.x
46. Jastreboff PJ. Phantom auditory perception (tinnitus) - mechanisms of generation and perception. Neurosci Res. (1990) 8:221–54. doi: 10.1016/0168-0102(90)90031-9
47. Cima RFF, Crombez G, Vlaeyen JWS. Catastrophizing and fear of tinnitus predict quality of life in patients with chronic tinnitus. Ear Hear. (2011) 32:634–41. doi: 10.1097/AUD.0b013e31821106dd
48. Hesser H, Bånkestad E, Andersson G. Acceptance of tinnitus as an independent correlate of tinnitus severity. Ear Hear. (2015) 36:e176–82. doi: 10.1097/AUD.0000000000000148
Keywords: tinnitus, mindfulness, cognitive behavioral therapy, depression, anxiety, MBCT, MBSR
Citation: Rademaker MM, Stegeman I, Ho-Kang-You KE, Stokroos RJ and Smit AL (2019) The Effect of Mindfulness-Based Interventions on Tinnitus Distress. A Systematic Review. Front. Neurol. 10:1135. doi: 10.3389/fneur.2019.01135
Received: 16 July 2019; Accepted: 10 October 2019;
Published: 01 November 2019.
Edited by:
Agnieszka J. Szczepek, Charité Medical University of Berlin, GermanyReviewed by:
Petra Georgiewa Brueggemann, Charité Medical University of Berlin, GermanyNicolas Dauman, University of Poitiers, France
Copyright © 2019 Rademaker, Stegeman, Ho-Kang-You, Stokroos and Smit. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Maaike M. Rademaker, bS5tLnJhZGVtYWtlci0zQHVtY3V0cmVjaHQubmw=
 Maaike M. Rademaker
Maaike M. Rademaker Inge Stegeman
Inge Stegeman Krysten E. Ho-Kang-You
Krysten E. Ho-Kang-You Robert J. Stokroos
Robert J. Stokroos A. L. Smit
A. L. Smit