- Department of Neurology, Chungnam National University Hospital, Chungnam National University School of Medicine, Daejeon, South Korea
Many investigations have found common occurrences of benign paroxysmal positional vertigo (BPPV) in women, and clinical experience has shown that BPPV can develop due to increased hormonal fluctuations, especially during menopause. Therefore, knowledge about neurochemicals and their involvement with BPPV is imperative for the management of neurological issues in women. This review will discuss appropriate gender-based considerations of BPPV based on experimental and clinical evidence. The studies describe 2 lines of evidence regarding the association of perimenopause in women and the development of BPPV: (1) experimental evidence: the existence of estrogen receptors in the inner ear, otoconial malformations in osteopenic/osteoporotic rats, changes in otoconin 90 caused by hormone replacement therapy, and impaired calcium absorption following estrogen deprivation corrected by estrogen replacement therapy and (2) clinical evidence: epidemiological aspects, osteoporosis and estrogen deficiency. Future studies are necessary to validate the effects of hormonal replacement therapy and phytoestrogen in women with recurrent BPPV.
Introduction
Known as the most common cause of recurrent vertigo (1), benign paroxysmal positional vertigo (BPPV) is an important health problem affecting more than 420 million adults worldwide, based on an international consensus that BPPV has a lifetime prevalence of 10% (2). BPPV increases with age, especially during menopause, in a ratio of 2-3.2:1 for women and men aged 40–60 years (3–8). In particular, hormonal changes, external estrogens, and pregnancy exposure are only experienced by women. Further understanding of possible contributors to the predominance of BPPV in women could make a significant contribution to our understanding of the causes of BPPV and may provide new methods for prevention. Therefore, the present study will review the current state of knowledge on BPPV risk factors specific to women.
Perimenopause Period
There are three stages of perimenopause in the executive summary of the Stages of Reproductive Aging Workshop: “early menopausal transition (early perimenopause), characterized by irregularities in the menstrual cycle, late menopausal transition (late perimenopause), characterized by an interval of more than 60 days of amenorrhea in the previous 12 months; and early postmenopause, which is the first year following the last menstrual period (9).” Physiologically, estrogen declines sharply during this period, which occurs over several years and is characterized by marked fluctuations in sex hormone levels. The fluctuations during this period are more severe than those during the menstrual cycle (10). Regarding personal aspects, menopause occurs during the time in life when women are actively involved in raising a family and/or full-time work, during which time women may also be responsible for caring for elderly parents. Most menopausal women experience uncomfortable symptoms, and menopause is related to an increased risk for metabolic syndrome, in addition to obesity and osteoporosis (11). In the field of gynecology, menopausal symptoms are assessed using the “Kupperman rating scale” (Table 1) (12–14). The inclusion of vertigo items in one menopausal symptom index suggests that vertigo is also a frequent complaint in gynecology clinics. Although the nature of vertigo has not been precisely elucidated, postmenopausal hormone replacement therapy (HRT) was superior to placebo when assessed by the “Kupperman scale including the item addressing vertigo (15).” Additionally, many neurotology studies have shown an increased incidence of BPPV in women, and experience with older people suggests that hormonal fluctuations, particularly during menopause, may increase, resulting in the development of BPPV (3–8). Cooperative management between neurotologists and gynecologists could be helpful in the management of dizziness in women who experience it.
Experimental Evidence
Anatomical Differences
Differences in the peripheral vestibular system between men and women have been reported. To our knowledge, no reports have described the direct comparison of otoconial morphology between women and men. However, in the anteroposterior dimension, the width of the peripheral vestibular system is significantly smaller in women (16), which could suggest a difference in otoconial morphology, such as differences in the bones according to sex. Further validation studies are needed.
Hormone Changes
Physiologically, testosterone levels are more stable than estrogen levels throughout a woman's life and are relatively constant at ages 30–70 (17). Estrogen decreases steeply during the climacteric period. The female sex hormone estrogen 17β-estradiol (E2) is well-known to perform many tasks and contributes to various roles, such as reproductive organ differentiation and function, memory processes and bone metabolism (18, 19). Clinically, E2 and progesterone levels are clearly reduced in women with BPPV (20, 21); however, no difference in testosterone was found between the postmenopausal and control groups (21). Similar to other sex steroids, estrogen acts on target cells by attaching to nuclear hormone receptors such as estrogen receptor (ER)α and β (22). Thus, the ER level is an important determinant that influences estrogen signaling to the cell.
Estrogen Receptors in the Inner Ear
Estrogen functions have been suggested to influence hearing and vestibular function (23, 24). In addition, the expression of ERα and β decreases with increasing age (25). A previous double-staining study found that in the inner ear, ERα and β were generally co-expressed (25). However, ERβ predominates in type II spiral ganglion neurons or inner ear strial marginal cells (24, 26–28). These findings support the role of estrogen in the inner ear.
TRPV6 and Estrogen
BPPV is described as the process of otoconia debris removal from the otoconial membrane (29). Because otoconia are calcium carbonate crystals, initial crystal formation in the proteinaceous core needs a local increase in Ca2+ and carbonate () concentrations (30). Importantly, low Ca2+ levels must be maintained in the endolymph of vestibular organs to prevent unnecessary mineralization (31). Several Ca2+ channel structures primarily act on the temporospatial control of Ca2+ concentrations in the endolymph to preserve a circumstance suitable for stable Ca2+ equilibrium. Previous reports indicate that the epithelial Ca2+ channels TRPV5 and TRPV6 manifest in the semicircular canal, which are important Ca2+-binding proteins for the maintenance of low Ca2+ concentrations in the endolymph. Moreover, ERα has been demonstrated to tightly regulate uterine TRPV6 transcription. An experimental study also showed that E2 regulates TRPV6 through an ERα-dependent pathway (32). In a previous study, decreased ERα levels in aged animals could induce a decrease in TRPV6, resulting in otoconial malformation and a decrease in the number of otoconia (25). Therefore, a sharp decrease in estrogen during menopause, especially a decrease in ERα, may impair otoconial metabolism and lead to a higher prevalence of BPPV (25).
Estrogen and Otoconia
Estrogen may also play an important role in otoconial metabolism. Bilateral ovariectomized osteopenic/osteoporotic rats had larger otoconia with a reduced density compared to controls (33).
Estrogen and Otoconin 90
An animal study conducted by Yang et al. demonstrated that bilateral ovariectomy in rats receiving female HRT reversed the reduction in the level of otoconin 90, the main protein that preserves the normal morphology and growth of otoconia (20, 34).
Estrogen and Vitamin D
Recent reports have shown that reduced serum levels of vitamin D are associated with the occurrence of BPPV (4, 35–40), and supplementation of vitamin D with/without calcium reduces recurrent events in BPPV patients (41–44). Estrogen treatment prevents the loss of intestinal Ca2+ absorption and bone density caused by ovariectomy in the premenopausal period (45). Experimental studies have shown that impaired Ca2+ absorption following estrogen deprivation is caused by a decreased response to 1,25 dihydroxycholecalciferol, the main regulator of intestinal absorption, and that estrogen treatment, rather than short-term replacement with 1,25 dihydroxycholecalciferol, can amend this abnormality. Therefore, combined hormone replacement and vitamin D management could be more effective for the prevention of further attacks of vertigo in perimenopausal women with BPPV. However, further validation studies are needed (45).
Clinical Evidence
Susceptibility of Women to BPPV
Several factors increase the susceptibility to BPPV, including older age, head and neck trauma, inactivity, and other ear problems or surgery. Many studies have shown a common occurrence in women, and clinical experience with older people has shown that BPPV can develop due to increased hormonal fluctuations, especially during menopause (3–8).
BPPV and Oral Contraceptives
A previous study reported that recurrent BPPV was related to oral contraceptives (46). It has been postulated that oral contraceptives may induce disturbances in the water and electrolyte balance, variances in endolymph pH and abnormalities in carbohydrate or lipid metabolism, which may cause otoconial degeneration and subsequent otoconial detachment and BPPV (46).
BPPV in Pregnancy
Although the link between BPPV and pregnancy is still unclear, some pregnant women have been first diagnosed with BPPV during pregnancy (47).
Osteoporosis
A characteristic feature of osteoporosis is a decrease in bone mass due to an imbalance between bone resorption and formation. Loss of reproductive function and aging are the two most significant factors developing this condition. After ~30–40 years, both women and men experience 0.3–0.5% bone loss per year (48, 49). After menopause, the rate of bone loss can increase 10 fold. In Western countries, one-third of women with menopause experience osteoporosis (50). There are two types of osteoporosis: primary osteoporosis and secondary osteoporosis (51). Type I primary osteoporosis occurs during the postmenopausal period when estrogen output and the bone formation rate are reduced and bone loss is accelerated (51). Type II primary osteoporosis is a senile process with a reduction in the synthesis of active vitamin D in the elderly, which reduces gastrointestinal absorption of Ca2+, bone cell activity and bone development. Secondary osteoporosis is caused by specific conditions and drugs and occurs in all age groups irrespective of sex. Fractures and injuries due to osteoporosis could harm a person's life and incapacitate their ability to live independently. Therefore, bone fractures related to decreased bone density can increase mortality (51). In addition, decreased bone mineral density is related to the occurrence/recurrence of BPPV. Patients with BPPV had lower bone density among both women and men compared to controls (52). Although both men and women may develop osteoporosis, women are more susceptible to osteoporosis than men due to their smaller size with lower bone mass and decreased estrogen secretion during menopause (53, 54). In a previous study on bone mineral density and BPPV, women over the age of 45 in the relapse group had lower T scores than those in the de novo group (52). To examine osteoporosis in menopausal women, ovariectomized rats have been investigated in several studies (55, 56). Estrogen spares the human skeleton from bone loss by slowing down the process of bone remodeling and maintaining an equilibrium between bone formation and absorption (57, 58). In women undergoing rapid bone loss after menopause (59, 60), bone resorption and urinary Ca2+ excretion are increased, and these changes are reversed by estrogen replacement therapy (61, 62). Considering that estrogen loss is a causal factor for bone loss during perimenopause, a specific ER modulator could be used to treat postmenopausal BPPV patients.
Hormone Replacement Therapy
HRT to combat estrogen depletion in menopause has also been successfully used to treat vasomotor symptoms and is assumed to be neuroprotective compared to women not using HRT. Although the nature of vertigo has not been precisely elucidated, women using postmenopausal HRT had better scores than the placebo group on the “Kupperman scale” (sweating, hot flashes, myalgia, and vertigo) (15). The hormonal fluctuation of ovarian neurosteroids might trigger the occurrence/recurrence of BPPV during the perimenopausal period. In the Taiwanese population, a study revealed that the incidence of BPPV was significantly lower in patients taking estrogen for menopausal syndrome in two age groups (ages 45–65 and ages 65 and over) (6). These findings support the efficacy of estrogen supplementation to decrease the occurrence of BPPV in women with menopause. The possible mechanisms include complete, more reliable estrogen blood levels that induce protective effects, estrogen effects on autophagy and possible epigenetic modulation (5, 6, 20, 63). However, chronic use of HRT increases the risk of breast cancer (64), stroke (64), and venous thrombosis. Therefore, many postmenopausal women rely on other non-steroidal estrogen mimetics or natural remedies to solve the problems associated with the symptoms of estrogen deficiency. Phytoestrogen could be an alternative to HRT. Phytoestrogens, including soy isoflavones, are non-steroidal, diphenolic substances that can bind to ERs and have activity similar to that of estrogen (65). To date, there have been no reports on the effectiveness of phytoestrogens on BPPV recurrence.
Conclusion
The biochemical pathway is a key factor in some medical illnesses. Thus, investigation into the biochemical causes of neurotological problems could be guaranteed to produce results and can be cost effective. In particular, hormonal changes, external estrogens, and pregnancy exposure are only experienced by women. It is not fully understood why postmenopausal women show a higher prevalence of BPPV. However, in menopause, the rapid decrease in ERs, especially ERα, due to the sudden decrease in estrogen can lead to the disturbance of otoconial metabolism, which can increase the prevalence of BPPV. Additionally, HRT can reverse the low otoconin 90 levels and reduce the incidence of BPPV (Table 2). Adoption of a customized approach considering the neurochemical changes in perimenopause will be extremely helpful for the management of BPPV in women. Cooperative management among neurotologists, endocrinologists, and gynecologists is also important as a focus for neurotological disorders, including BPPV, in women.
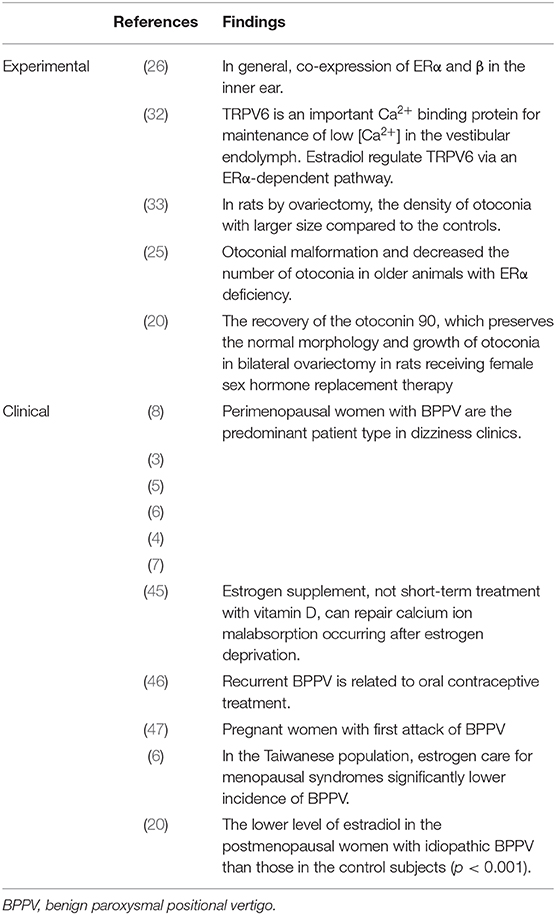
Table 2. Evidence of the relationship of estrogen to the pathogenesis of benign paroxysmal positional vertigo.
Author Contributions
S-HJ acquired and analyzed the data, and drafted the manuscript.
Funding
This research was supported by the Basic Science Research Program through the National Research Foundation of Korea (NRF), funded by the Ministry of Science, ICT and Future Planning (NRF-2017R1C1B50 77010).
Conflict of Interest
The author declares that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
References
1. Kim HJ, Lee JO, Choi JY, Kim JS. Etiologic distribution of dizziness and vertigo in a referral-based dizziness clinic in South Korea. J. Neurol. (2020) 267:2252–59. doi: 10.1007/s00415-020-09831-2
2. von Brevern M, Radtke A, Lezius F, Feldmann M, Ziese T, Lempert T, et al. Epidemiology of benign paroxysmal positional vertigo: a population based study. J. Neurol. Neurosurg. Psychiatry. (2007) 78:710–5. doi: 10.1136/jnnp.2006.100420
3. Vibert D, Kompis M, Hausler R. Benign paroxysmal positional vertigo in older women may be related to osteoporosis and osteopenia. Ann. Otol. Rhinol. Laryngol. (2003) 112:885–9. doi: 10.1177/000348940311201010
4. Han W, Fan Z, Zhou M, Guo X, Yan W, Lu X, et al. Low 25-hydroxyvitamin D levels in postmenopausal female patients with benign paroxysmal positional vertigo. Acta Otolaryngol. (2018) 138:443–6. doi: 10.1080/00016489.2017.1416168
5. Ogun OA, Buki B, Cohn ES, Janky KL, Lundberg YW. Menopause and benign paroxysmal positional vertigo. Menopause. (2014) 21:886–9. doi: 10.1097/GME.0000000000000190
6. Liu DH, Kuo CH, Wang CT, Chiu CC, Chen TJ, Hwang DK, et al. Age-related increases in benign paroxysmal positional vertigo are reversed in women taking estrogen replacement therapy: a population-based study in Taiwan. Front. Aging Neurosci. (2017) 9:404. doi: 10.3389/fnagi.2017.00404
7. Smith PF, Agrawal Y, Darlington CL. Sexual dimorphism in vestibular function and dysfunction. J. Neurophysiol. (2019) 121:2379–91. doi: 10.1152/jn.00074.2019
8. Mizukoshi K, Watanabe Y, Shojaku H, Okubo J, Watanabe I. Epidemiological studies on benign paroxysmal positional vertigo in Japan. Acta Otolaryngol. (1988) 447:67–72. doi: 10.3109/00016488809102859
9. Harlow SD, Gass M, Hall JE, Lobo R, Maki P, Rebar RW, et al. Executive summary of the stages of reproductive aging workshop + 10: addressing the unfinished agenda of staging reproductive aging. J. Clin. Endocrinol. Metab. (2012) 97:1159–68. doi: 10.1210/jc.2011-3362
10. Woods NF, Mitchell ES. Symptoms during the perimenopause: prevalence, severity, trajectory, and significance in women's lives. Am. J. Med. (2005) 118(Suppl. 12B):14–24. doi: 10.1016/j.amjmed.2005.09.031
11. Udo T, McKee SA, White MA, Masheb RM, Barnes RD, Grilo CM. Menopause and metabolic syndrome in obese individuals with binge eating disorder. Eat. Behav. (2014) 15:182–5. doi: 10.1016/j.eatbeh.2014.01.003
12. Lobo RA. Hormone-replacement therapy: current thinking. Nat. Rev. Endocrinol. (2017) 13:220–31. doi: 10.1038/nrendo.2016.164
13. Kupperman HS, Blatt MH, Wiesbader H, Filler W. Comparative clinical evaluation of estrogenic preparations by the menopausal and amenorrheal indices. J. Clin. Endocrinol. Metab. (1953) 13:688–703. doi: 10.1210/jcem-13-6-688
14. Wiklund I, Holst J, Karlberg J, Mattsson LA, Samsioe G, Sandin K, et al. A new methodological approach to the evaluation of quality of life in postmenopausal women. Maturitas. (1992) 14:211–24. doi: 10.1016/0378-5122(92)90116-L
15. Bech P, Munk-Jensen N, Obel EB, Ulrich LG, Eiken P, Nielsen SP. Combined versus sequential hormonal replacement therapy: a double-blind, placebo-controlled study on quality of life-related outcome measures. Psychother. Psychosom. (1998) 67:259–65. doi: 10.1159/000012289
16. Marcus S, Whitlow CT, Koonce J, Zapadka ME, Chen MY, Williams DW III, et al. Computed tomography supports histopathologic evidence of vestibulocochlear sexual dimorphism. Int. J. Pediatr. Otorhinolaryngol. (2013) 77:1118–22. doi: 10.1016/j.ijporl.2013.04.013
17. Holmegard HN, Nordestgaard BG, Jensen GB, Tybjaerg-Hansen A, Benn M. Sex hormones and ischemic stroke: a prospective cohort study and meta-analyses. J. Clin. Endocrinol. Metab. (2016) 101:69–78. doi: 10.1210/jc.2015-2687
18. Pettersson K, Gustafsson JA. Role of estrogen receptor beta in estrogen action. Annu. Rev. Physiol. (2001) 63:165–92. doi: 10.1146/annurev.physiol.63.1.165
19. Losordo DW, Kearney M, Kim EA, Jekanowski J, Isner JM. Variable expression of the estrogen receptor in normal and atherosclerotic coronary arteries of premenopausal women. Circulation. (1994) 89:1501–10. doi: 10.1161/01.CIR.89.4.1501
20. Yang H, Gu H, Sun W, Li Y, Wu H, Burnee M, et al. Estradiol deficiency is a risk factor for idiopathic benign paroxysmal positional vertigo in postmenopausal female patients. Laryngoscope. (2018) 128:948–53. doi: 10.1002/lary.26628
21. Wang SF, Zhang L, Li GH, Zhang WW, Wang YP, Geng B. The change of female progesterone level and blood calcium concentration in perimenopausal women with benign paroxysmal positional vertigo. Zhonghua Er Bi Yan Hou Tou Jing Wai Ke Za Zhi. (2017) 52:287–90. doi: 10.3760/cma.j.issn.1673-0860.2017.04.010
22. Beato M, Klug J. Steroid hormone receptors: an update. Hum. Reprod. Update. (2000) 6:225–36. doi: 10.1093/humupd/6.3.225
23. Kuiper GG, Shughrue PJ, Merchenthaler I, Gustafsson JA. The estrogen receptor beta subtype: a novel mediator of estrogen action in neuroendocrine systems. Front. Neuroendocrinol. (1998) 19:253–86. doi: 10.1006/frne.1998.0170
24. Hultcrantz M, Simonoska R, Stenberg AE. Estrogen and hearing: a summary of recent investigations. Acta Otolaryngol. (2006) 126:10–4. doi: 10.1080/00016480510038617
25. Motohashi R, Takumida M, Shimizu A, Konomi U, Fujita K, Hirakawa K, et al. Effects of age and sex on the expression of estrogen receptor alpha and beta in the mouse inner ear. Acta Otolaryngol. (2010) 130:204–14. doi: 10.3109/00016480903016570
26. Stenberg AE, Wang H, Sahlin L, Hultcrantz M. Mapping of estrogen receptors alpha and beta in the inner ear of mouse and rat. Hear. Res. (1999) 136:29–34. doi: 10.1016/S0378-5955(99)00098-2
27. Stenberg AE, Wang H, Sahlin L, Stierna P, Enmark E, Hultcrantz M. Estrogen receptors alpha and beta in the inner ear of the ‘Turner mouse' and an estrogen receptor beta knockout mouse. Hear. Res. (2002) 166:1–8. doi: 10.1016/S0378-5955(02)00310-6
28. Meltser I, Tahera Y, Simpson E, Hultcrantz M, Charitidi K, Gustafsson JA, et al. Estrogen receptor beta protects against acoustic trauma in mice. J. Clin. Invest. (2008) 118:1563–70. doi: 10.1172/JCI32796
29. Parnes LS, McClure JA. Free-floating endolymph particles: a new operative finding during posterior semicircular canal occlusion. Laryngoscope. (1992) 102:988–92. doi: 10.1288/00005537-199209000-00006
30. Hughes I, Thalmann I, Thalmann R, Ornitz DM. Mixing model systems: using zebrafish and mouse inner ear mutants and other organ systems to unravel the mystery of otoconial development. Brain Res. (2006) 1091:58–74. doi: 10.1016/j.brainres.2006.01.074
31. Yamauchi D, Raveendran NN, Pondugula SR, Kampalli SB, Sanneman JD, Harbidge DG, et al. Vitamin D upregulates expression of ECaC1 mRNA in semicircular canal. Biochem. Biophys. Res. Commun. (2005) 331:1353–7. doi: 10.1016/j.bbrc.2005.04.053
32. Lee GS, Jeung EB. Uterine TRPV6 expression during the estrous cycle and pregnancy in a mouse model. Am. J. Physiol. Endocrinol. Metab. (2007) 293:E132–8. doi: 10.1152/ajpendo.00666.2006
33. Vibert D, Sans A, Kompis M, Travo C, Muhlbauer RC, Tschudi I, et al. Ultrastructural changes in otoconia of osteoporotic rats. Audiol. Neurootol. (2008) 13:293–301. doi: 10.1159/000124277
34. Petko JA, Millimaki BB, Canfield VA, Riley BB, Levenson R. Otoc1: a novel otoconin-90 ortholog required for otolith mineralization in zebrafish. Dev. Neurobiol. (2008) 68:209–22. doi: 10.1002/dneu.20587
35. Jeong SH, Kim JS, Shin JW, Kim S, Lee H, Lee AY, et al. Decreased serum vitamin D in idiopathic benign paroxysmal positional vertigo. J. Neurol. (2013) 260:832–8. doi: 10.1007/s00415-012-6712-2
36. Buki B, Ecker M, Junger H, Lundberg YW. Vitamin D deficiency and benign paroxysmal positioning vertigo. Med. Hypotheses. (2013) 80:201–4. doi: 10.1016/j.mehy.2012.11.029
37. Talaat HS, Abuhadied G, Talaat AS, Abdelaal MS. Low bone mineral density and vitamin D deficiency in patients with benign positional paroxysmal vertigo. Eur. Arch. Otorhinolaryngol. (2015) 272:2249–53. doi: 10.1007/s00405-014-3175-3
38. Rhim GI. Serum vitamin D and recurrent benign paroxysmal positional vertigo. Laryngoscope Investig. Otolaryngol. (2016) 1:150–3. doi: 10.1002/lio2.35
39. Wu Y, Fan Z, Jin H, Guan Q, Zhou M, Lu X, et al. Assessment of bone metabolism in male patients with benign paroxysmal positional vertigo. Front. Neurol. (2018) 9:742. doi: 10.3389/fneur.2018.00742
40. Yang CJ, Kim Y, Lee HS, Park HJ. Bone mineral density and serum 25-hydroxyvitamin D in patients with idiopathic benign paroxysmal positional vertigo. J. Vestib. Res. (2018) 27:287–94. doi: 10.3233/VES-170625
41. Talaat HS, Kabel AMH, Khaliel LH, Abuhadied G, El-Naga HAERA, Talaat AS. Reduction of recurrence rate of benign paroxysmal positional vertigo by treatment of severe vitamin D deficiency. Auris. Nasus. Larynx. (2016) 43:237–41. doi: 10.1016/j.anl.2015.08.009
42. Sheikhzadeh M, Lotfi Y, Mousavi A, Heidari B, Bakhshi E. The effect of serum vitamin D normalization in preventing recurrences of benign paroxysmal positional vertigo: a case-control study. Caspian J. Intern. Med. (2016) 7:173–7.
43. Califano L, Salafia F, Melillo MG, Mazzone S. Is hypovitaminosis D a risk factor for either the onset or the recurrence of Benign Paroxysmal Positional Vertigo? Frontiera ORL (2019). Available online at: http://www.frontieraorl.it/en/is-hypovitaminosis-d-risk-factor-for-either-the-onset-or-the-recurrence-of-benign-paroxysmal-positional-vertigo/
44. Carneiro de Sousa PJM, Abreu Pereira DM, Pereira CM, de Magalhaes P, Duarte DRS, da Silva T, et al. Vitamin D deficiency and benign paroxysmal positioning vertigo. Hearing Balance Commun. (2019) 17:179–81. doi: 10.1080/21695717.2019.1590988
45. Gennari C, Agnusdei D, Nardi P, Civitelli R. Estrogen preserves a normal intestinal responsiveness to 1,25-dihydroxyvitamin D3 in oophorectomized women. J. Clin. Endocrinol. Metab. (1990) 71:1288–93. doi: 10.1210/jcem-71-5-1288
46. Giacomini PG, Napolitano B, Alessandrini M, Di Girolamo S, Magrini A. Recurrent paroxysmal positional vertigo related to oral contraceptive treatment. Gynecol. Endocrinol. (2006) 22:5–8. doi: 10.1080/09513590500441614
47. Coban K, Yigit N, Aydin E. Benign paroxysmal positional vertigo in pregnancy. Turk Arch. Otorhinolaryngol. (2017) 55:83–6. doi: 10.5152/tao.2017.2079
48. Gallagher JC, Goldgar D, Moy A. Total bone calcium in normal women: effect of age and menopause status. J. Bone Miner. Res. (1987) 2:491–6. doi: 10.1002/jbmr.5650020605
49. Nordin BE, Need AG, Bridges A, Horowitz M. Relative contributions of years since menopause, age, and weight to vertebral density in postmenopausal women. J. Clin. Endocrinol. Metab. (1992) 74:20–3. doi: 10.1210/jc.74.1.20
50. Reginster JY, Burlet N. Osteoporosis: a still increasing prevalence. Bone. (2006) 38(2 Suppl. 1):S4–9. doi: 10.1016/j.bone.2005.11.024
51. Lips P, Cooper C, Agnusdei D, Caulin F, Egger P, Johnell O, et al. Quality of life in patients with vertebral fractures: validation of the Quality of Life Questionnaire of the European Foundation for Osteoporosis (QUALEFFO). Working Party for Quality of Life of the European Foundation for Osteoporosis. Osteoporos. Int. (1999) 10:150–60. doi: 10.1007/s001980050210
52. Jeong SH, Choi SH, Kim JY, Koo JW, Kim HJ, Kim JS. Osteopenia and osteoporosis in idiopathic benign positional vertigo. Neurology. (2009) 72:1069–76. doi: 10.1212/01.wnl.0000345016.33983.e0
53. Riggs BL, Khosla S, Melton LJ, III. Sex steroids and the construction and conservation of the adult skeleton. Endocr. Rev. (2002) 23:279–302. doi: 10.1210/edrv.23.3.0465
54. Seeman E. Growth in bone mass and size–are racial and gender differences in bone mineral density more apparent than real? J. Clin. Endocrinol. Metab. (1998) 83:1414–9. doi: 10.1210/jc.83.5.1414
55. Yang J, Pham SM, Crabbe DL. Effects of oestrogen deficiency on rat mandibular and tibial microarchitecture. Dentomaxillofac. Radiol. (2003) 32:247–51. doi: 10.1259/dmfr/12560890
56. Ames MS, Hong S, Lee HR, Fields HW, Johnston WM, Kim DG. Estrogen deficiency increases variability of tissue mineral density of alveolar bone surrounding teeth. Arch. Oral. Biol. (2010) 55:599–605. doi: 10.1016/j.archoralbio.2010.05.011
57. Manolagas SC. Birth and death of bone cells: basic regulatory mechanisms and implications for the pathogenesis and treatment of osteoporosis. Endocr. Rev. (2000) 21:115–37. doi: 10.1210/edrv.21.2.0395
58. Manolagas SC, Kousteni S, Jilka RL. Sex steroids and bone. Recent Prog. Horm. Res. (2002) 57:385–409. doi: 10.1210/rp.57.1.385
59. Parfitt AM, Mathews CH, Villanueva AR, Kleerekoper M, Frame B, Rao DS. Relationships between surface, volume, and thickness of iliac trabecular bone in aging and in osteoporosis. Implications for the microanatomic and cellular mechanisms of bone loss. J. Clin. Invest. (1983) 72:1396–409. doi: 10.1172/JCI111096
60. Eriksen EF, Hodgson SF, Eastell R, Cedel SL, O'Fallon WM, Riggs BL. Cancellous bone remodeling in type I (postmenopausal) osteoporosis: quantitative assessment of rates of formation, resorption, and bone loss at tissue and cellular levels. J. Bone. Miner. Res. (1990) 5:311–9. doi: 10.1002/jbmr.5650050402
61. Uebelhart D, Schlemmer A, Johansen JS, Gineyts E, Christiansen C, Delmas PD. Effect of menopause and hormone replacement therapy on the urinary excretion of pyridinium cross-links. J. Clin. Endocrinol. Metab. (1991) 72:367–73. doi: 10.1210/jcem-72-2-367
62. Lufkin EG, Wahner HW, O'Fallon WM, Hodgson SF, Kotowicz MA, Lane AW, et al. Treatment of postmenopausal osteoporosis with transdermal estrogen. Ann. Intern. Med. (1992) 117:1–9. doi: 10.7326/0003-4819-117-1-1
63. Marino G, Fernandez AF, Cabrera S, Lundberg YW, Cabanillas R, Rodriguez F, et al. Autophagy is essential for mouse sense of balance. J. Clin. Invest. (2010) 120:2331–44. doi: 10.1172/JCI42601
64. Lokkegaard E, Nielsen LH, Keiding N. Risk of stroke with various types of menopausal hormone therapies: a national cohort study. Stroke. (2017) 48:2266–9. doi: 10.1161/STROKEAHA.117.017132
Keywords: vertigo, estrogen, women, otoconia, perimenopause
Citation: Jeong S-H (2020) Benign Paroxysmal Positional Vertigo Risk Factors Unique to Perimenopausal Women. Front. Neurol. 11:589605. doi: 10.3389/fneur.2020.589605
Received: 31 July 2020; Accepted: 17 September 2020;
Published: 16 October 2020.
Edited by:
Augusto Pietro Casani, University of Pisa, ItalyReviewed by:
Francisco Carlos Zuma E. Maia, Pontifical Catholic University of Rio Grande do Sul, BrazilAlfonso Scarpa, University of Salerno, Italy
Mauro Gufoni, University of Pisa, Italy
Copyright © 2020 Jeong. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Seong-Hae Jeong, bXNlYWoxMDgxQGdtYWlsLmNvbQ==
 Seong-Hae Jeong
Seong-Hae Jeong