- Department of Neurosurgery, Xijing Hospital, Fourth Military Medical University, Xi'an, China
Background: Cerebral cavernous malformations (CCMs) presenting with seizures can be treated with neurosurgery or radiosurgery, but the ideal treatment remains unclear. Currently, there is no adequate randomized controlled trial comparing surgical treatment and radiotherapy for epileptogenic CCMs. Therefore, we conducted a systematic review and meta-analysis of available data from published literature to compare the efficacy and safety of neurosurgery and radiosurgery for epileptogenic CCMs.
Methods: We performed a comprehensive search of the Ovid MEDLINE, Web of Science, PubMed, China Biological Medicine and China National Knowledge Infrastructure databases for studies published between January 1994 and October 2019. The search terms were as follows: “epilepsy,” “seizures,” “brain cavernous hemangioma,” “cerebral cavernous malformation,” “cerebral cavernous hemangioma,” “hemangioma, cavernous, central nervous system.” Two researchers independently extracted the data and reviewed all the articles. We compared the advantages and disadvantages of the two treatments.
Results: A total of 45 studies were included in our analysis. Overall, the seizure control rate was 79% (95% CI: 75–83%) for neurosurgery and 49% (95% CI: 38–59%) for radiosurgery. In the neurosurgery studies, 4.4% of patients experienced permanent morbidity, while no patients in the radiotherapy studies had permanent morbidity. In addition, the results of subgroup analysis showed that ethnicity, CCMs location and average lesion number are likely significant factors influencing the seizure outcome following treatment.
Conclusions: The epilepsy control rate after neurosurgery was higher than that after radiosurgery, but neurosurgery also had a relatively higher rate of permanent morbidity.
Introduction
Cerebral cavernous malformations (CCMs), also known as cavernous angiomas, have an incidence of 0.1–0.5% and account for 5–10% of cerebral and spinal vascular malformations (1–3). CCMs are benign vascular lesions that can occur anywhere in the brain parenchyma or leptomeninges but mainly occur in the supratentorial region. They are abnormal low-flow blood vessels in the brain consisting of expanded, thin-walled capillary clusters filled with hemosiderin deposits. CCMs can manifest as central nervous system bleeding and other neurological defects based on their location, and 40–70% of supratentorial cavernous malformations tend to have seizures as the first symptom (2–4). A total of 35–40% of CCM patients develop medically refractory epilepsy. The vascular morphology of CCMs is fragile and prone to repeated microbleeds, leading to reactive gliosis and hemosiderin deposition in adjacent brain tissues (2, 5, 6). Thus, the resulting ischemia, venous hypertension, glial hyperplasia, and inflammatory responses can all induce seizures and involve the brain parenchyma near these lesions. Of all cerebral vascular malformations, CCMs are the most common epileptic substrate. Seizures are the most common symptoms of supratentorial CCMs (7, 8). Epilepsy is known to significantly reduce quality of life and cause severe morbidity, and antiepileptic drugs (AEDs) often have undesirable side effects (9–11). Therefore, eliminating epilepsy is an important and often underestimated therapeutic goal in managing these lesions.
However, the ideal treatment remains unclear. Microsurgery is considered the standard treatment for intractable epilepsy caused by CCMs. Surgical removal can prevent seizures in 50–90% of patients (12). In the past few decades, with the application of advanced technology such as diffusion tensor imaging (DTI) and electrophysiological monitoring, surgical intervention had produced better results (13). Additionally, recent studies had confirmed that microsurgery could exhibit great seizure control rate (14, 15). However, the risk of surgical morbidity and mortality is high when the lesion is located in deep or eloquent areas (16–19). Stereotactic radiosurgery is another option for the treatment of CCMs, especially in high-risk patients (20, 21). In the treatment of epileptogenic CCMs, several authors have indicated that gamma knife radiosurgery (GKRS) can provide good seizure control (22–24). Currently, there is no adequate randomized controlled trial comparing surgical treatment and radiotherapy for epileptogenic CCMs. Therefore, we conducted a systematic review and meta-analysis of available data from published literature to compare the efficacy and safety of neurosurgery and radiosurgery for epileptogenic CCMs.
Methods
The present study was performed according to the Preferred Reporting Items for Systematic Reviews and Meta-Analyses guidelines (PRISMA) (25).
Search Strategy
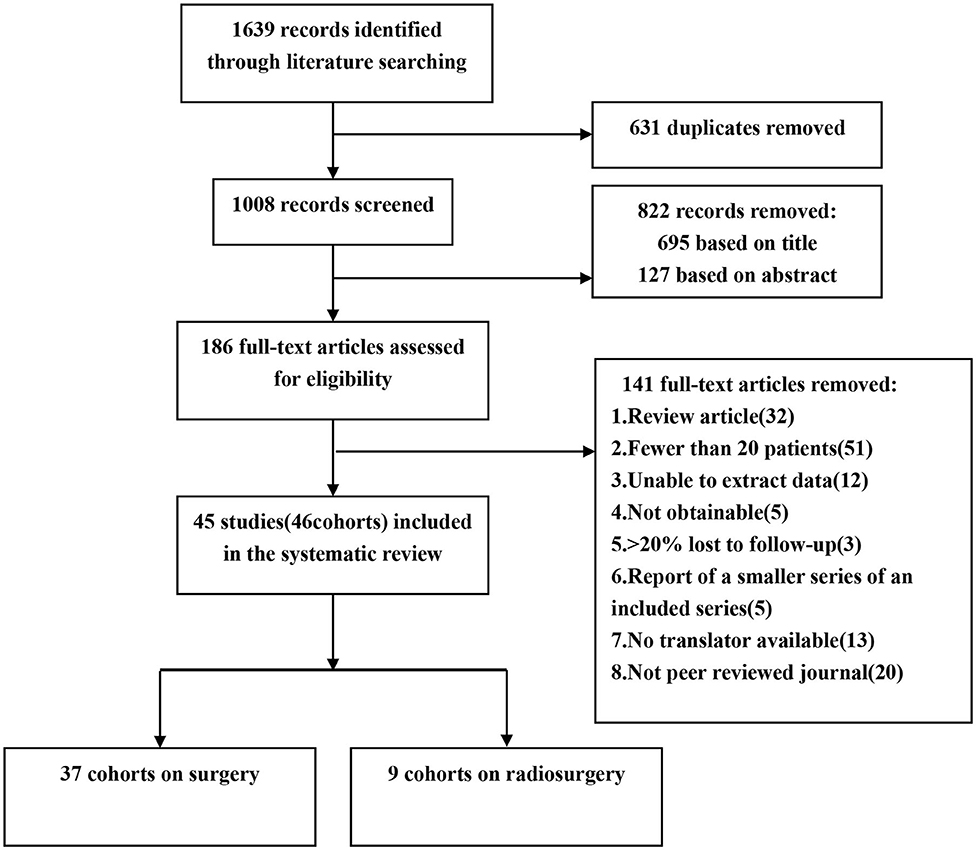
We performed a comprehensive search of the Ovid MEDLINE, Web of Science, PubMed, China Biological Medicine and China National Knowledge Infrastructure databases for studies published between January 1994 and October 2019. The search terms were as follows: “epilepsy,” “seizures,” “brain cavernous hemangioma,” “cerebral cavernous malformation,” “cerebral cavernous haemangioma,” “hemangioma, cavernous, central nervous system.” We retrieved the original articles of cohort studies published in peer-reviewed journals. We included eligible studies published in Chinese and English, while studies in other languages were excluded because we did not have translators (Figure 1).
Assessment of Eligibility
Two independent reviewers selected eligible studies based on the Patient, Intervention, Comparison, Outcome, and Study design (PICOS) guidelines (23): (1) Participants: patients' CCMs had to be confirmed by MRI or pathological examination; (2) Interventions: neurosurgery or radiosurgery; (3) Comparison: not applicable; (4) Outcome: seizure outcome estimated by Engel's classification; (5) Study designs: retrospective cohort study; the sample sizes of the studies had to be >20; studies must have described the follow-up time, and the follow-up rate had to be >80%. If the institution or author published multiple studies using the same cohort, only the report with the largest sample size was included for analysis. Case reports, reviews, meta-analyses, letters and conference articles were excluded.
Risk of Bias Assessment
The Newcastle-Ottawa Scale (NOS) was used to assess the quality of the included studies. The NOS score is used to assess three major components: selection, comparability, and exposure. Studies are defined as high quality when scoring ≥5. Two reviewers independently evaluated the quality of the studies and resolved disagreements by discussion.
Data Extraction
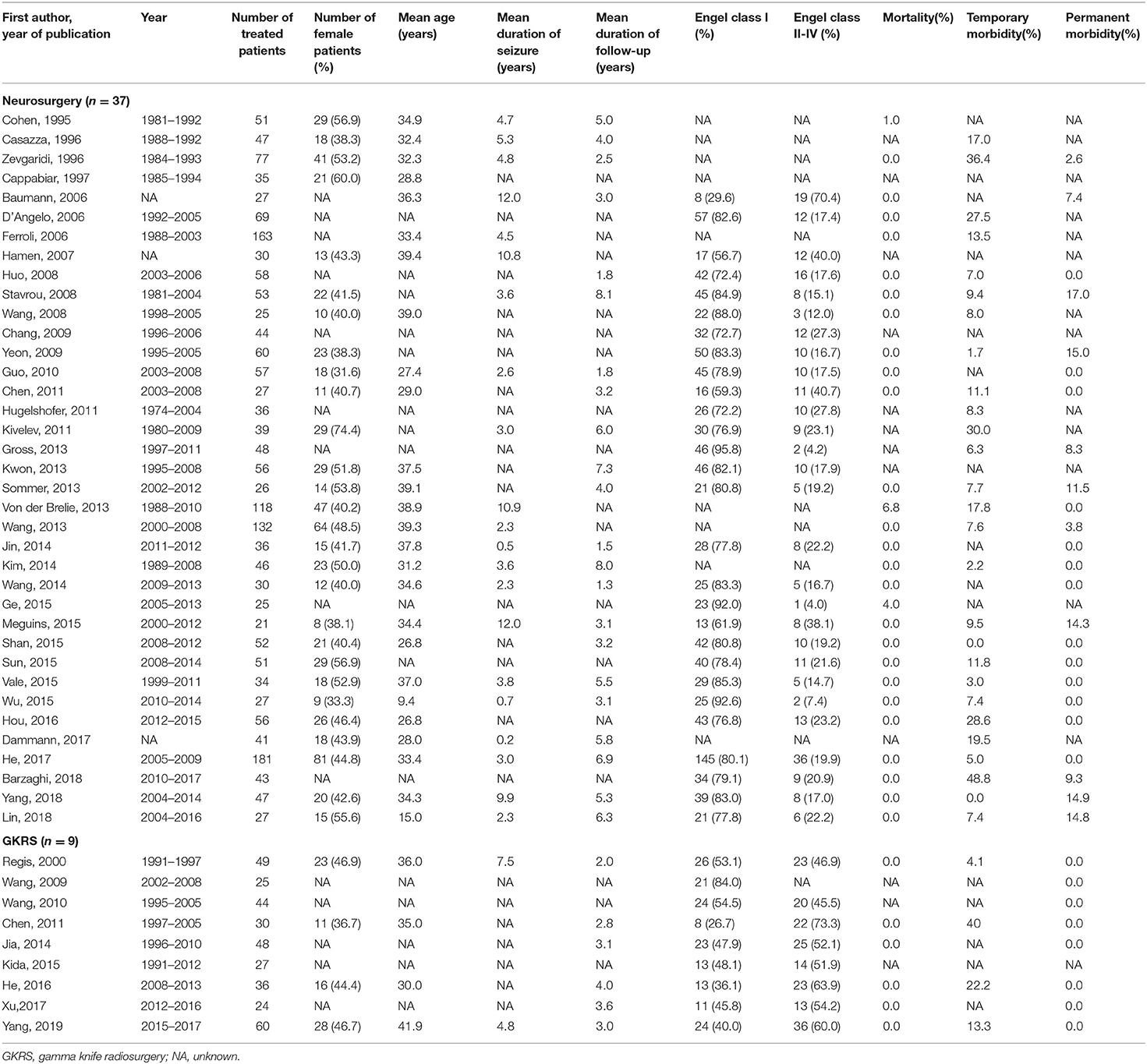
A total of 1,639 articles were retrieved in our initial search. Two researchers (Xiangyu Gao and Peng Luo) independently extracted the data and reviewed all the articles. First, two researchers screened the titles and abstracts of the retrieved literature. They then evaluated the full-texts of relevant articles to determine their eligibility. Opinion was sought from a senior investigator (Xiaofan Jiang) if the two researchers could not reach an agreement. Finally, 45 of 1,639 articles met the inclusion criteria. Two investigators extracted the following data from each eligible study: first author's last name, publication date, year of patients, total number of patients, number of female patients, mean follow-up time, mean age, mean duration of epilepsy, lesion location, post-operative seizure outcome, mortality, temporary morbidity and permanent morbidity (6, 24, 26–68) (Table 1). The term “mortality” is defined as patients' death attributed to CCMs or treatment. Temporary morbidity includes transient brain edema after surgery, new or worse neurological deficits, and a range of other complications, all of which can eventually be fully cured. Permanent morbidity includes memory deficits and persistent focal neurological deficits.
Statistical Analysis
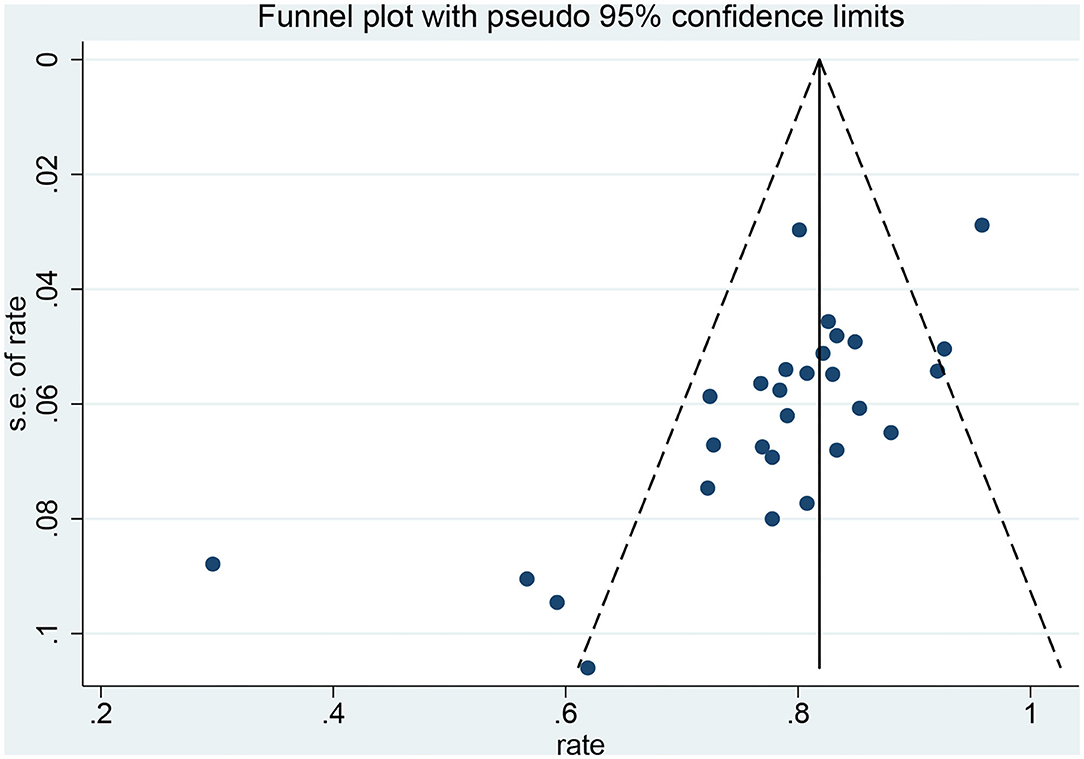
We pre-specified the following characteristics of the included cohorts as the baseline covariates of interest: mean duration of epilepsy, cohort midyear (defined as the middle of the year in which the treatment occurred), mean age of the patients, percentage of female patients, CCM location, percentage of patients who died, percentage of patients with temporary morbidity and percentage of patients with permanent morbidity. We used the Mann-Whitney U-test to evaluate the difference in the proportion of these characteristics between the neurosurgery and radiosurgery groups, with a p-value < 0.05 indicating a significant difference. The seizure outcome data were estimated by Engel's classification. Engel class I represented complete freedom from seizures since the operation, and Engel classes II-IV represented not seizure-free. To standardize the evaluation of the study results, we calculated the proportion of patients in Engel class I in each group. Meta-analysis software (version 14.2, Stata) was used to calculate the overall proportions. Statistical heterogeneity was evaluated by the I2 statistic. If I2 > 50%, we used a random effects model to analyze the assumption. Otherwise, we used a fixed effects model. Sensitivity analysis was performed to investigate the impact of an individual study on the overall risk assessment by omitting one study at a time. Publication bias was evaluated qualitatively examining the funnel plot and quantitatively by Egger's test, which was considered statistically asymmetrical when the p-value < 0.1.
Results
Systematic Literature Review
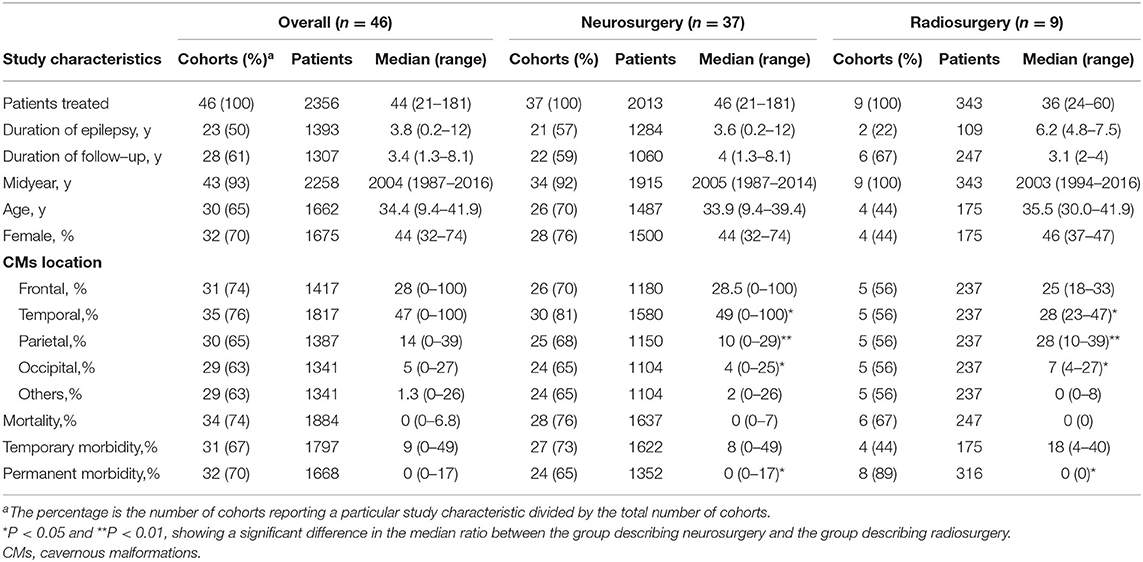
After screening, 45 studies (46 cohorts) involving 2,356 patients were identified. Thirty-seven studies described a total of 2013 patients who underwent neurosurgery, and nine studies described a total of 343 patients who underwent radiosurgery. Four (9%) cohorts examined patients from multiple centers, and the remaining 42 (91%) cohorts examined patients from a single center. Twenty-five (55%) cohorts were from Asia, 14 (30%) cohorts were from Europe, 5 (11%) cohorts were from North America, 1 (2%) cohort was from South America, and 1 (2%) cohort was from Oceania. All 45 studies were published between 1995 and 2019. Twenty-eight studies (62%) described the mean or median duration of follow-up. Thirty-seven studies (80%) described post-operative seizure outcomes. We found statistically significant differences in the CCM location and proportion of patients with permanent morbidity between the neurosurgery and radiosurgery groups. GKRS is more suitable for CCM lesions located in the parietal lobe and occipital lobe, while neurosurgery is more suitable for temporal lobe lesions. Compared with patients in the radiosurgery group, patients in the neurosurgery group had a higher incidence of permanent morbidity after surgery (Table 2).
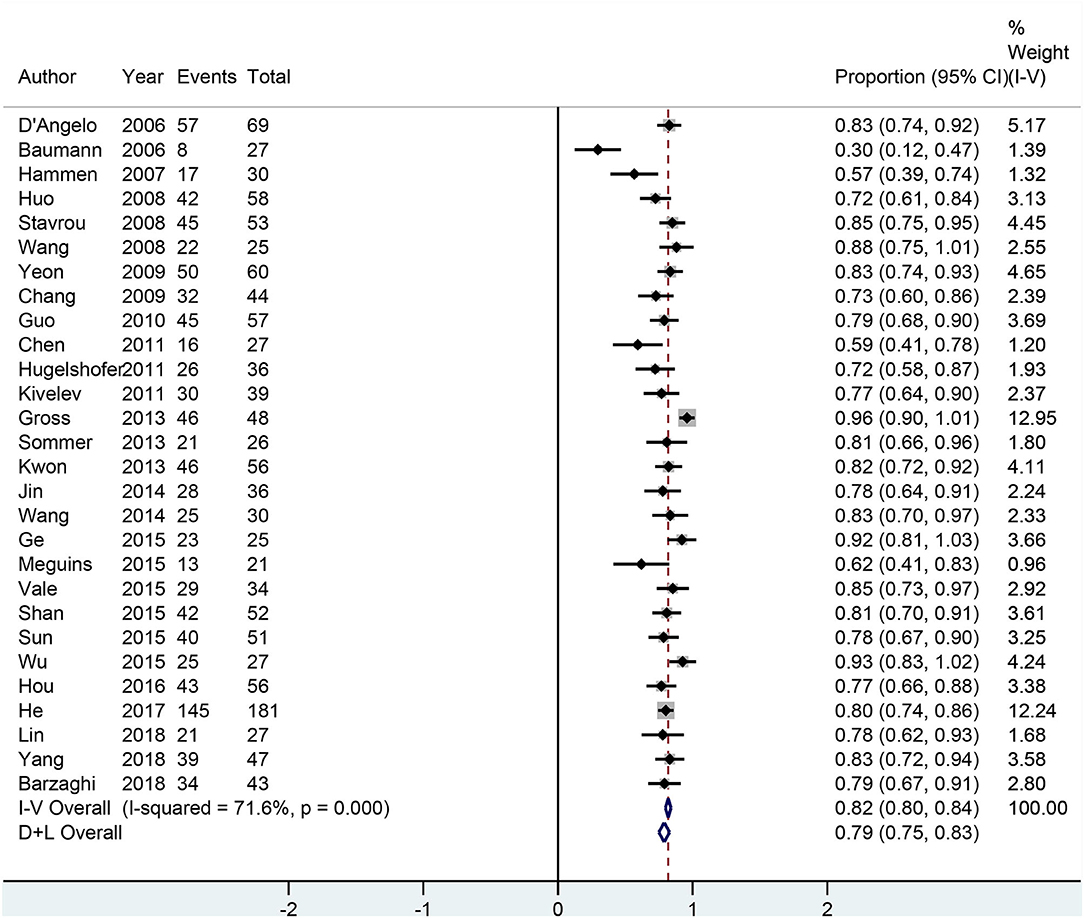
Seizure Outcomes
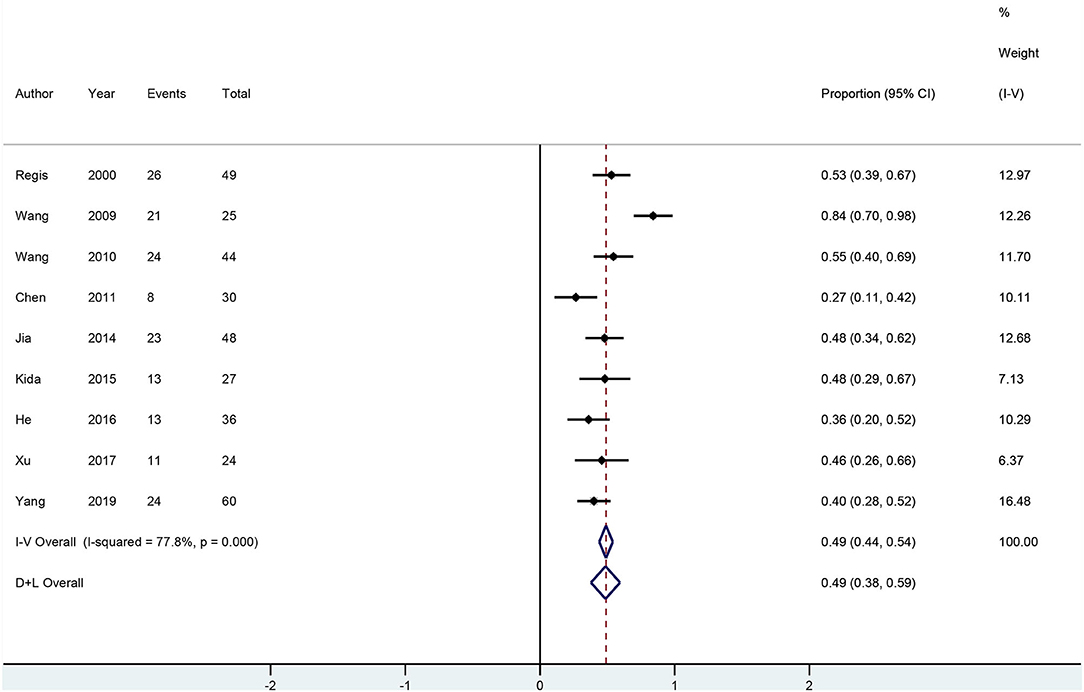
All 28 neurosurgery studies (except Baumann's study) showed that neurosurgery was an effective surgical treatment for seizures, with more than 50% of patients being classified as Engel class I. As shown in Figure 2, the overall proportion of patients in Engel class I was 0.79 (95% CI 0.75–0.83) across all 28 neurosurgery studies, which suggested that neurosurgery can significantly control seizures. Because I2 > 50%, we used a random effects model to analyze the data. The nine radiosurgery studies also demonstrated the efficacy of GKRS in the treatment of epileptogenic CCMs. As shown in Figure 3, the overall proportion of patients in Engel class I was 0.49 (95% CI 0.38–0.59). All radiosurgery studies were analyzed using a random effects model because I2 > 50%.
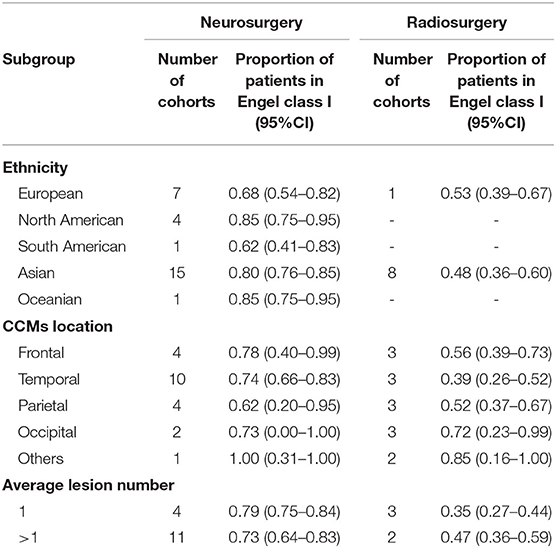
In addition, we performed subgroup analyses and the confounding factors in our studies were ethnicity, CCMs location and average lesion number (Table 3). Patients from North America (0.85, 95% CI 0.75–0.95), Asia (0.80, 95% CI 0.76–0.85) and Oceania (0.85, 95% CI 0.75–0.95) had higher proportions of favorable seizure outcomes in neurosurgery studies. When CCMs lesions were located in the frontal and temporal lobes, seizure outcomes of neurosurgery (0.78, 95% CI 0.40–0.99; 0.74, 95% CI 0.66–0.83; respectively) were significantly better than those of radiosurgery (0.56, 95% CI 0.39–0.73; 0.39, 95% CI 0.26–0.52; respectively). The effect of neurosurgery on single lesion (0.79, 95% CI 0.75–0.84) is better than that on multiple lesions (0.73, 95% CI 0.64–0.83). In contrast, the effect of neurosurgery on multiple lesions (0.47, 95% CI 0.36–0.59) is better than that on single lesion (0.35, 95% CI 0.27–0.44).
Mortality and Morbidity
Of the 37 neurosurgery studies, thirty-three (89%) studies reported on the mortality or morbidity. Two (0.1%) patients died post-operatively, 212 (13.1%) patients experienced temporary morbidity, and 60 (4.4%) patients experienced permanent neurological symptoms. Eight (88.9%) of the nine radiosurgery studies reported on the mortality or morbidity. No deaths or permanent complications occurred. Thirty (17.1%) patients experienced temporary morbidity.
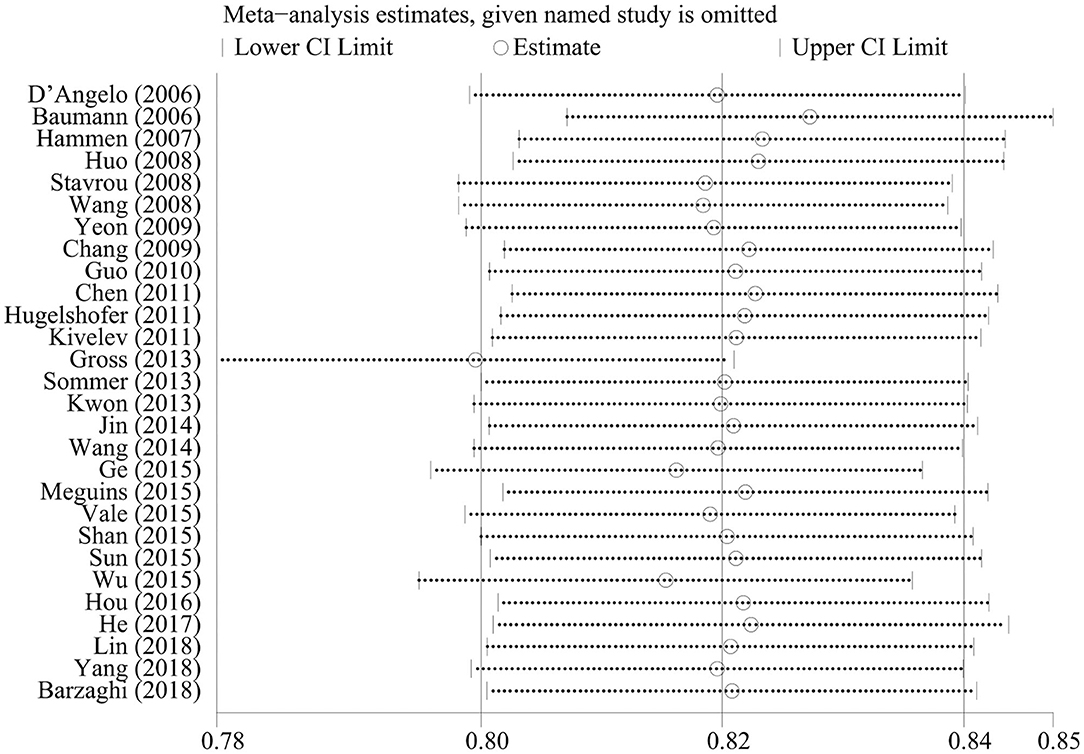
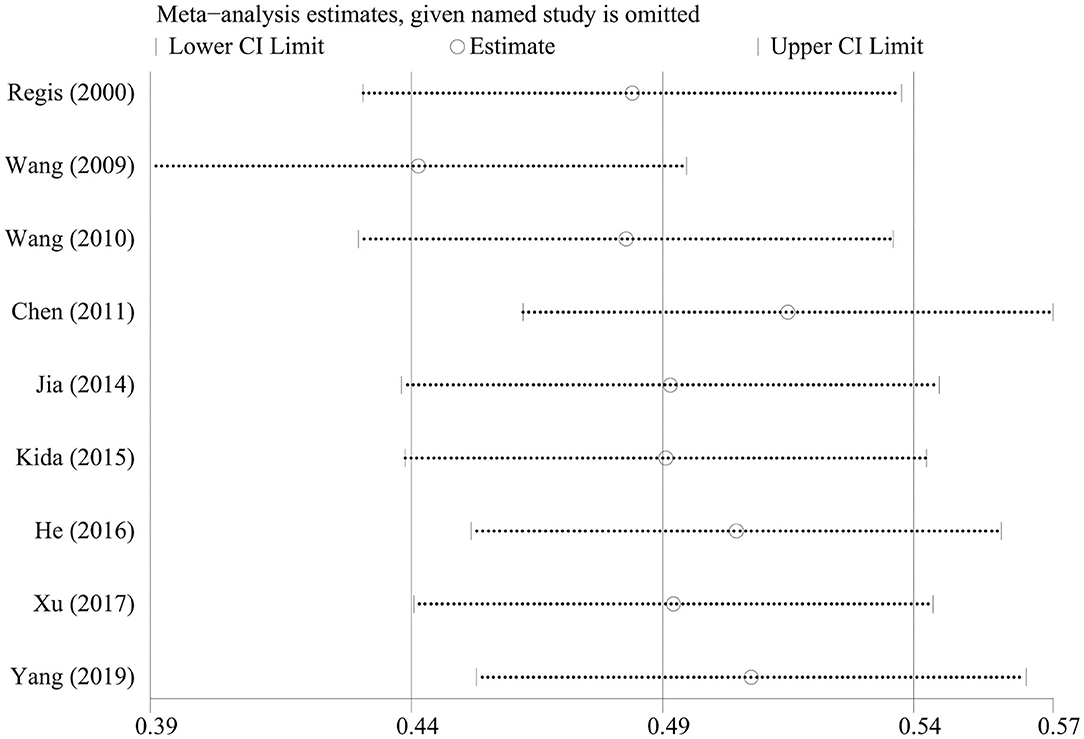
Sensitivity Analysis
We omitted one study at a time to investigate the influence of a single study on the pooled estimates. The comparison results in the radiosurgery group were not significantly altered, indicating that this group's results were statistically robust. In the neurosurgery group, Gross's study was shown to have a substantial influence on the pooled estimates due to its higher proportion of patients in Engel class I. However, Gross's study did not affect our conclusions (Figures 4, 5).
Publication Bias
Funnel plots and Egger's test were used to evaluate the publication bias. The p-values produced by Egger's test on the post-radiosurgery seizure outcomes and post-neurosurgery seizure outcomes were 0.778 and 0.000, respectively. Therefore, there was no publication bias in the radiosurgery studies, but publication bias might have influenced the results of the neurosurgery studies (Figures 6,7).
Discussion
Overall, our results indicate that the epilepsy control rate after neurosurgery was higher than that after radiosurgery, but neurosurgery also had a relatively higher rate of permanent morbidity. The effect of neurosurgery on multiple lesions is better than that on single lesion whereas radiotherapy was the opposite. The effect of neurosurgery on frontal lobe and temporal lobe lesions is significantly better than those of radiotherapy. Ethnicity affects the seizure outcome following the treatment. Radiosurgery is more suitable for CCM lesions located in the parietal lobe and occipital lobe, while neurosurgery is more suitable for temporal lobe lesions.
CCMs are low-flow vascular malformations that are usually static and can also bleed repeatedly and grow. CCMs are occult vascular malformations that are difficult to find on DSA. MRI has a high specificity and sensitivity for CCMs, which can be clearly diagnosed and characterized due to their nodular or circular appearance. There is generally no edema or placeholder effect around the lesion except when it is accompanied by bleeding (69). The mechanism of CCM-induced epilepsy is still not fully understood. CCMs do not contain nerve tissues and will not become the epilepsy initiation area by itself. Peripheral hemosiderin deposition and gliosis caused by recurrent microhemorrhage of malformed vessels are considered to be the main causes of epilepsy (70).
AEDs are the primary treatment for CCMs with epilepsy. For refractory epilepsy, neurosurgery or radiosurgery should be considered. Yang's research shows that surgery for intractable epilepsy can effectively control seizures. In addition, the appropriate operation scheme can be selected according to the location of CCMs and the responsiveness of patients to antiepileptic drugs to maximize the control of epilepsy and minimize post-operative neurological sequelae (68). He et al. also reported the effectiveness of neurosurgery for intractable epilepsy and pointed out that the shorter the duration of seizures before surgery, the better the control of seizures after surgery (67). Ruan et al. (14) conducted a meta-analysis and the result showed that patients who underwent surrounding hemosiderin excision could exhibit significantly improved seizure outcomes compared to patients without hemosiderin excision. Additionally, Shang-Guan's meta-analysis reported that extended lesionectomy does not contribute to better seizure control for patients with cerebral cavernous malformations with epilepsy (15). In addition, radiotherapy can also be used for the treatment of refractory epilepsy. There has been a considerable amount of research on its effectiveness. Regis et al. showed that GKRS can control seizures safely and effectively. When CCMs are located in a highly functional area, the risk of surgical treatment is higher, and GKRS treatment is more appropriate (24). However, the ideal treatment remains unclear.
To compare the efficacy and safety of neurosurgery and radiosurgery for epileptogenic CCMs, we conducted a systematic review and meta-analysis of available data from published literature. The results of our systematic review showed that neurosurgery is more likely to be used in refractory epilepsy patients with CCM lesions located in the temporal lobe, while radiosurgery is more likely to be used in patients with CCM lesions located in the parietal lobe and occipital lobe. In addition, there was no significant difference in mortality and post-operative transient morbidity between the two treatments, but the proportion of patients with permanent complications was significantly higher in the neurosurgery group than in the radiosurgery group. Additionally, the results showed that 4.4% of patients in the neurosurgery studies experienced permanent morbidity, while no patients in the radiosurgery studies had permanent morbidity. We also found that the proportion of patients with temporary morbidity in the radiosurgery group (17.1%) was greater than that in the neurosurgery group (13.1%). After consulting the literature, we found that radiosurgery could cause to post-operative brain edema in patients, leading to a significantly higher proportion of patients suffering from temporary morbidity; however, brain edema will eventually subside over time.
The results of our meta-analysis showed that the seizure control rate was 0.79 (95% CI 0.75–0.83) for neurosurgery and 0.49 (95% CI 0.38–0.59) for radiosurgery. In terms of controlling epilepsy, the effect of neurosurgery is significantly better than that of radiosurgery. In addition, CCMs multiplicity and CCMs location are important factors affecting the prognosis of CCMs. Englot et al. (71) had reported that individuals with a single lesion received neurosurgery were more likely to attain post-operative seizure freedom. Some of the neurosurgery studies found CCMs locations were not related to seizure outcomes (38, 71). Wang et al. believed that radiosurgery is more effective for seizure caused by CCMs in frontal and parietal lobe than that caused in temporal lobe (40). Therefore, we performed subgroup analyses to summarize the influence of these confounding factors on the results. We observed that the effect of neurosurgery on single lesion (0.79, 95% CI 0.75–0.84) is better than that on multiple lesions (0.73, 95% CI 0.64–0.83), which further supported the conclusions of Englot et al. (71). On the contrary, we found that the effect of radiosurgery on multiple lesions (0.47, 95% CI 0.36–0.59) is better than that on single lesion (0.35, 95% CI 0.27–0.44). These data revealed that average lesion number is likely a factor influencing seizure outcome which needs further case-control trials. Consistent with previous studies, our results showed that there is little difference in the effect of neurosurgery on each site and radiotherapy was more effective for frontal (0.56, 95% CI 0.39–0.73) and parietal (0.52, 95% CI 0.37–0.67) CCMs than for temporal (0.39, 95% CI 0.26–0.52) CCMs. we also found that for lesions located in the frontal lobe and temporal lobe, neurosurgery (0.78, 95% CI 0.40–0.99; 0.74, 95% CI 0.66–0.83; respectively) is significantly superior to radiosurgery (0.56, 95% CI 0.39–0.73; 0.39, 95% CI 0.26–0.52; respectively). For CCMs lesions at other locations, the differences in seizure outcome between the two treatments were not significant.
The difference of gene background in CCMs patients is closely related to clinical manifestation and prognosis. Different ethnic groups have different genetic backgrounds and different mutation sites (72). Previous cohort studies have not focused on this. Therefore, we did a subgroup analysis and our data indicated that North Americans (0.85, 95% CI 0.75–0.95), Asians (0.80, 95% CI 0.76–0.85) and Oceanians (0.85, 95% CI 0.75–0.95) benefited more from neurosurgery than Europeans (0.68, 95% CI 0.54–0.82) and South Americans (0.62, 95% CI 0.41–0.83). We speculated that ethnicity might be associated with prognosis and further random controlled trails were needed. Unfortunately, data on mortality and morbidity of the two treatment could not be subgroup analyzed as they were not provided in the majority of the included studies.
Lately, there is an emerging minimally invasive technique called stereotactic laser ablation (SLA) which is getting into focus. SLA could precisely ablate lesions with less collateral injury around lesions. A cohort study by Willie et al. (73) reported 17 patients receiving SLA, 14 (82%) of whom achieved Engel I after a year-long follow-up period. SLA has the same good seizure control rate as neurosurgery and is more tolerable for the patients. Therefore, SLA is expected to be a first-line minimally invasive therapy for CCMs-related epilepsy, but more case-control trials are still needed.
The NOS was used to assess the quality of the included studies, and each study had a moderate level of quality with an average score of 6. Our systematic review and meta-analysis has three limitations. First, all the included studies were retrospective studies. Therefore, randomized controlled trials are urgently needed. Second, neurosurgery was not consistent in all the included studies. Last, the experience of surgeons greatly affects the outcome of the operation.
Conclusion
In summary, our paper demonstrates that the epilepsy control rate after neurosurgery was higher than that after radiosurgery, but neurosurgery also had a relatively higher rate of permanent morbidity. Number of lesions, location and ethnicity are likely significant factors influencing the seizure outcome following treatment. Therefore, our data provide new ideas for clinical individualized precision medicine but further random controlled trials are still needed.
Data Availability Statement
All datasets presented in this study are included in the article/Supplementary Material.
Author Contributions
XG, KY, and JS contributed conception and design of the study. PL and XJ organized the database. YC performed the statistical analysis. XG wrote the first draft of the manuscript. BZ, HZ, SD, LZ, and PL wrote sections of the manuscript. All authors contributed to manuscript revision, read, and approved the submitted version.
Funding
This work was supported by the National Natural Science Foundation of China (nos. 81871023, 81671303, and 81771322) and the Military Youth talent lifting project (no. 17-JCJQ-QT-037).
Conflict of Interest
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
References
1. Amin-Hanjani S, Robertson R, Arginteanu MS, Scott RM. Familial intracranial arteriovenous malformations. Case report and review of the literature. Pediatr Neurosurg. (1998) 29:208–13. doi: 10.1159/000028723
2. Awad I, Jabbour P. Cerebral cavernous malformations and epilepsy. Neurosurg Focus. (2006) 21:e7. doi: 10.3171/foc.2006.21.1.8
3. Moriarity JL, Wetzel M, Clatterbuck RE, Javedan S, Sheppard JM, Hoenig-Rigamonti K, et al. The natural history of cavernous malformations: a prospective study of 68 patients. Neurosurgery. (1999) 44:1166–71. doi: 10.1227/00006123-199906000-00003
4. Del Curling O, Kelly DL, Elster AD, Craven TE. An analysis of the natural history of cavernous angiomas. J Neurosurg. (1991) 75:702–8. doi: 10.3171/jns.1991.75.5.0702
5. Bacigaluppi S, Retta SF, Pileggi S, Fontanella M, Goitre L, Tassi L, et al. Genetic and cellular basis of cerebral cavernous malformations: implications for clinical management. Clin Genetics. (2013) 83:7–14. doi: 10.1111/j.1399-0004.2012.01892.x
6. Cappabianca P, Alfieri A, Maiuri F, Mariniello G, Cirillo S, de Divitiis E. Supratentorial cavernous malformations and epilepsy: seizure outcome after lesionectomy on a series of 35 patients. Clin Neurol Neurosurg. (1997) 99:179–83. doi: 10.1016/S0303-8467(97)00023-1
7. Attar A, Ugur HC, Savas A, Yüceer N, Egemen N. Surgical treatment of intracranial cavernous angiomas. J Clin Neurosci. (2001) 8:235–9. doi: 10.1054/jocn.2000.0787
8. Porter PJ, Willinsky RA, Harper W, Wallace MC. Cerebral cavernous malformations: natural history and prognosis after clinical deterioration with or without hemorrhage. J Neurosurg. (1997) 87:190–7. doi: 10.3171/jns.1997.87.2.0190
9. Cascino GD. When drugs and surgery don't work. Epilepsia. (2008) 49(Suppl. 9):79–84. doi: 10.1111/j.1528-1167.2008.01930.x
10. Cramer JA, Mintzer S, Wheless J, Mattson RH. Adverse effects of antiepileptic drugs: a brief overview of important issues. Expert Rev Neurother. (2010) 10:885–91. doi: 10.1586/ern.10.71
11. Sheth RD. Adolescent issues in epilepsy. J Child Neurol. (2002) 17(Suppl. 2):2S23–7. doi: 10.1177/08830738020170020801
12. Bertalanffy H, Gilsbach JM, Eggert HR, Seeger W. Microsurgery of deep-seated cavernous angiomas: report of 26 cases. Acta Neurochir. (1991) 108:91–9. doi: 10.1007/BF01418515
13. Sandalcioglu IE, Wiedemayer H, Secer S, Asgari S, Stolke D. Surgical removal of brain stem cavernous malformations: surgical indications, technical considerations, and results. J Neurol Neurosurg Psychiatry. (2002) 72:351–5. doi: 10.1136/jnnp.72.3.351
14. Ruan D, Yu X, Shrestha S, Wang L, Chen G. The role of hemosiderin excision in seizure outcome in cerebral cavernous malformation surgery: a systematic review and meta-analysis. PLoS ONE. (2015) 10:e0136619. doi: 10.1371/journal.pone.0136619
15. Shang-Guan H, Wu Z, Yao P, Chen G, Zheng S, Kang D. Is extended lesionectomy needed for patients with cerebral cavernous malformations presenting with epilepsy? A meta-analysis. World Neurosurg. (2018) 120:e984–90. doi: 10.1016/j.wneu.2018.08.208
16. Gross BA, Batjer HH, Awad IA, Bendok BR. Brainstem cavernous malformations. Neurosurgery. (2009) 64:E805–18. doi: 10.1227/01.NEU.0000343668.44288.18
17. Mathiesen T, Edner G, Kihlström L. Deep and brainstem cavernomas: a consecutive 8-year series. J Neurosurg. (2003) 99:31–7. doi: 10.3171/jns.2003.99.1.0031
18. Monaco EA, Khan AA, Niranjan A, Kano H, Grandhi R, Kondziolka D, et al. Stereotactic radiosurgery for the treatment of symptomatic brainstem cavernous malformations. Neurosurg Focus. (2010) 29:E11. doi: 10.3171/2010.7.FOCUS10151
19. Wang CC, Liu A, Zhang JT, Sun B, Zhao YL. Surgical management of brain-stem cavernous malformations: report of 137 cases. Surg Neurol. (2003) 59:444–54. doi: 10.1016/S0090-3019(03)00187-3
20. Hasegawa T, McInerney J, Kondziolka D, Lee JY, Flickinger JC, Lunsford LD. Long-term results after stereotactic radiosurgery for patients with cavernous malformations. Neurosurgery. (2002) 50:1190–7. doi: 10.1227/00006123-200206000-00003
21. Karlsson B, Kihlström L, Lindquist C, Ericson K, Steiner L. Radiosurgery for cavernous malformations. J Neurosurg. (1998) 88:293–7. doi: 10.3171/jns.1998.88.2.0293
22. Bartolomei F, Régis J, Kida Y, Kobayashi T, Vladyka V, Liscàk R, et al. Gamma Knife radiosurgery for epilepsy associated with cavernous hemangiomas: a retrospective study of 49 cases. Stereotact Funct Neurosurg. (1999) 72(Suppl. 1):22–8. doi: 10.1159/000056435
23. Liu KD, Chung WY, Wu HM, Shiau CY, Wang LW, Guo WY, et al. Gamma knife surgery for cavernous hemangiomas: an analysis of 125 patients. J Neurosurg. (2005) 102:81–6. doi: 10.3171/sup.2005.102.s_supplement.0081
24. Regis J, Bartolomei F, Kida Y, Kobayashi T, Vladyka V, Liscak R, et al. Radiosurgery for epilepsy associated with cavernous malformation: retrospective study in 49 patients. Neurosurgery. (2000) 47:1091–7. doi: 10.1097/00006123-200011000-00013
25. Liberati A, Altman D, Tetzlaff J, Mulrow C, Gøtzsche P, Ioannidis J, et al. The PRISMA statement for reporting systematic reviews and meta-analyses of studies that evaluate healthcare interventions: explanation and elaboration. BMJ. (2009) 339:b2700. doi: 10.1136/bmj.b2700
26. Cohen DS, Zubay GP, Goodman RR. Seizure outcome after lesionectomy for cavernous malformations. J Neurosurg. (1995) 83:237–42. doi: 10.3171/jns.1995.83.2.0237
27. Casazza M, Broggi G, Franzini A, Avanzini G, Spreafico R, Bracchi M, et al. Supratentorial cavernous angiomas and epileptic seizures: preoperative course and postoperative outcome. Neurosurgery. (1996) 39:26–32. doi: 10.1097/00006123-199607000-00007
28. Zevgaridis D, van Velthoven V, Ebeling U, Reulen HJ. Seizure control following surgery in supratentorial cavernous malformations: a retrospective study in 77 patients. Acta Neurochir. (1996) 138:672–7. doi: 10.1007/BF01411470
29. Baumann CR, Schuknecht B, Lo Russo G, Cossu M, Citterio A, Andermann F, et al. Seizure outcome after resection of cavernous malformations is better when surrounding hemosiderin-stained brain also is removed. Epilepsia. (2006) 47:563–6. doi: 10.1111/j.1528-1167.2006.00468.x
30. D'Angelo VA, De Bonis C, Amoroso R, Cali A, D'Agruma L, Guarnieri V, et al. Supratentorial cerebral cavernous malformations: clinical, surgical, and genetic involvement. Neurosurg Focus. (2006) 21:e9. doi: 10.3171/foc.2006.21.1.10
31. Ferroli P, Casazza M, Marras C, Mendola C, Franzini A, Broggi G. Cerebral cavernomas and seizures: a retrospective study on 163 patients who underwent pure lesionectomy. Neurol Sci. (2006) 26:390–4. doi: 10.1007/s10072-006-0521-2
32. Hammen T, Romstock J, Dorfler A, Kerling F, Buchfelder M, Stefan H. Prediction of postoperative outcome with special respect to removal of hemosiderin fringe: a study in patients with cavernous haemangiomas associated with symptomatic epilepsy. Seizure. (2007) 16:248–53. doi: 10.1016/j.seizure.2007.01.001
33. Huo L, Wu L, Zhang MY, Hou YH, Ding XP, Fang JS. Electrocorticography monitoring in microsurgical treatment of solitary cavernous angiomas. Zhong Nan Da Xue Xue Bao Yi Xue Ban. (2008) 33:448–51. doi: 10.3321/j.issn:1672-7347.2008.05.014
34. Stavrou I, Baumgartner C, Frischer JM, Trattnig S, Knosp E. Long-term seizure control after resection of supratentorial cavernomas: a retrospective single-center study in 53 patients. Neurosurgery. (2008) 63:888–96. doi: 10.1227/01.NEU.0000327881.72964.6E
35. Wang ZZ, zhuge QC, Ye S, Lin C, Zhang Y, Wu ZB, et al. Microsurgical treatment of supratentorial intracranial cavernous malformation associated with epilepsy. Chin J Neurosurg. (2008) 8:593–6. doi: 10.3321/j.issn:1001-2346.2008.08.011
36. Chang EF, Gabriel RA, Potts MB, Garcia PA, Barbaro NM, Lawton MT. Seizure characteristics and control after microsurgical resection of supratentorial cerebral cavernous malformations. Neurosurgery. (2009) 65:31–8. doi: 10.1227/01.NEU.0000346648.03272.07
37. Wang HW, Zhang GR, Zhu LF, Qi Y, Li MS. Diagnosis of cerebral cavernous angioma and its treatment by gamma knife. Inn Mong Med J. (2009) 41:553–5. doi: 10.3969/j.issn.1004-0951.2009.05.017
38. Yeon JY, Kim JS, Choi SJ, Seo DW, Hong SB, Hong SC. Supratentorial cavernous angiomas presenting with seizures: surgical outcomes in 60 consecutive patients. Seizure. (2009) 18:14–20. doi: 10.1016/j.seizure.2008.05.010
39. Guo Q, Zhu D, Wu J, Hua G, Tan JL, Jin X. Surgical strategy of supratentorial cavernous angiomas associated with epilepsy (a report of 57 cases). Chin J Stereotact Funct Neurosurg. (2010) 1:20–2. doi: 10.3210/j.issn:1008-2425.2010.01.020
40. Wang P, Zhang FC, Zhang HY, Zhao HY. Gamma knife radiosurgery for intracranial cavernous malformations. Clin Neurol Neurosurg. (2010) 112:474–7. doi: 10.1016/j.clineuro.2010.03.012
41. Chen GX, Xu LS, Xu MH, Shen GJ. Therapeutic effect of two methods on seizures induced by supratentorial cavernous hemangioma. Chin J Clin Neurosurg. (2011) 16:420–1. doi: 10.3969/j.issn.1009-153X.2011.07.012
42. Hugelshofer M, Acciarri N, Sure U, Georgiadis D, Baumgartner RW, Bertalanffy H, et al. Effective surgical treatment of cerebral cavernous malformations: a multicenter study of 79 pediatric patients. J Neurosurg Pediatr. (2011) 8:522–5. doi: 10.3171/2011.8.PEDS09164
43. Kivelev J, Niemela M, Blomstedt G, Roivainen R, Lehecka M, Hernesniemi J. Microsurgical treatment of temporal lobe cavernomas. Acta Neurochir. (2011) 153:261–70. doi: 10.1007/s00701-010-0812-5
44. Gross BA, Smith ER, Goumnerova L, Proctor R, Madsen JR, Scott RM. Resection of supratentorial lobar cavernous malformations in children. J Neurosurg Pediatr. (2013) 12:367–73. doi: 10.3171/2013.7.PEDS13126
45. Kwon CS, Sheth SA, Walcott BP, Neal J, Eskandar EN, Ogilvy CS. Long-term seizure outcomes following resection of supratentorial cavernous malformations. Clin Neurol Neurosurg. (2013) 115:2377–81. doi: 10.1016/j.clineuro.2013.08.024
46. Sommer B, Kasper BS, Coras R, Blumcke I, Hamer HM, Buchfelder M, et al. Surgical management of epilepsy due to cerebral cavernomas using neuronavigation and intraoperative MR imaging. Neurol Res. (2013) 35:1076–83. doi: 10.1179/016164113X13801151880551
47. von der Brelie C, Malter MP, Niehusmann P, Elger CE, von Lehe M, Schramm J. Surgical management and long-term seizure outcome after epilepsy surgery for different types of epilepsy associated with cerebral cavernous malformations. Epilepsia. (2013) 54:1699–706. doi: 10.1111/epi.12327
48. Wang X, Tao Z, You C, Li Q, Liu Y. Extended resection of hemosiderin fringe is better for seizure outcome: a study in patients with cavernous malformation associated with refractory epilepsy. Neurol India. (2013) 61:288–92. doi: 10.4103/0028-3886.115070
49. Jia G, Zhang JM, Ma ZM, Qiu B, Hou YH. Therapeutic effect of gamma knife on intracranial cavernous angioma. Zhong Nan Da Xue Xue Bao Yi Xue Ban. (2014) 39:1320–5. doi: 10.11817/j.issn.1672-7347.2014.12.016
50. Jin Y, Zhao C, Zhang S, Zhang X, Qiu Y, Jiang J. Seizure outcome after surgical resection of supratentorial cavernous malformations plus hemosiderin rim in patients with short duration of epilepsy. Clin Neurol Neurosurg. (2014) 119:59–63. doi: 10.1016/j.clineuro.2014.01.013
51. Kim J, Kim CH, Chung CK. Longitudinal changes in seizure outcomes after resection of cerebral cavernous malformations in patients presenting with seizures: a long-term follow-up of 46 patients. Acta Neurochir. (2014) 156:1539–47. doi: 10.1007/s00701-014-2121-x
52. Wang FL, Wang QH, Jin P. Microsurgical treatment of intracerebral cavernous angioma with epilepsy as first symptom in 30 cases. Chin J Stereotact Funct Neurosurg. (2014) 27:208–11. doi: 10.3210/j.issn:1008-2425.2014.04.004
53. Ge X. Surgical and non-surgical treatment of epilepsy associated with cavernous hemangioma. Chin J Mod Drug Appl. (2015) 9:98–9. doi: 10.14164/j.cnki.cn11-5581/r.2015.19.071
54. Kida Y, Hasegawa T, Iwai Y, Shuto T, Satoh M, Kondoh T, et al. Radiosurgery for symptomatic cavernous malformations: a multi-institutional retrospective study in Japan. Surg Neurol Int. (2015) 6(Suppl. 5):S249–57. doi: 10.4103/2152-7806.157071
55. Meguins LC, Rocha da Cruz Adry RA, da Silva Junior SC, Pereira CU, de Oliveira JG, de Morais DF, et al. Microsurgical treatment of patients with refractory epilepsy and mesial temporal cavernous malformations: clinical experience of a tertiary epilepsy center. Surg Neurol Int. (2015) 6:169. doi: 10.4103/2152-7806.169552
56. Shan YZ, Fan XT, Meng L, An Y, Xu JK, Zhao GG. Treatment and outcome of epileptogenic temporal cavernous malformations. Chin Med J. (2015) 128:909–13. doi: 10.4103/0366-6999.154289
57. Sun Z, Xie YF, Shi QH, Dan W, Yan Y, Lu B, et al. Treatment of supratentorial cerebral cavernous angioma associated with epilepsy as first symptom. Chin J Clin Neurosurg. (2015) 20:709–11. doi: 10.13798/j.issn.1009-153X.2015.12.002
58. Vale FL, Vivas AC, Manwaring J, Schoenberg MR, Benbadis SR. Temporal lobe epilepsy and cavernous malformations: surgical strategies and long-term outcomes. Acta Neurochir. (2015) 157:1887–95. doi: 10.1007/s00701-015-2592-4
59. Wu HJ, Yu Z, Zhao YL. Surgical treatment of intracranial cavernous angioma with epilepsy in children. J Int Neurol Neurosurg. (2015) 42:342–5. doi: 10.16636/j.cnki.jinn.2015.04.009
60. He ZB, Wang RJ, Wang HW. Factors influencing the curative effect of gamma knife on intracranial cavernous hemangioma with epilepsy as the first symptom. Chin J Nerv Ment Dis. (2016) 42:291–4. doi: 10.3969/j.issn.1002-0152.2016.05.008
61. Hou Z, Li W, An N, Shi XJ, Liu SY. Efficacy of surgical treatment for cerebral cavernous malformation related epilepsy: report of 56 cases. Acta Acad Med Militaris Tertiae. (2016) 38:1987–90. doi: 10.16016/j.1000-5404.201601171
62. Dammann P, Wrede K, Jabbarli R, Neuschulte S, Menzler K, Zhu Y, et al. Outcome after conservative management or surgical treatment for new-onset epilepsy in cerebral cavernous malformation. J Neurosurg. (2017) 126:1303–11. doi: 10.3171/2016.4.JNS1661
63. Xu WD, Quan JH, Gao JM. The curative effect of gamma knife therapy for intracranial cavernous hemangioma. Chin J Woman Child Health Res. (2017) 28:4. doi: 10.3316/j.issn.1673-5293.2017.03.001
64. Barzaghi LR, Capitanio JF, Giudice L, Panni P, Acerno S, Mortini P. Usefulness of ultrasound-guided microsurgery in cavernous angioma removal. World Neurosurg. (2018) 116:E414–20. doi: 10.1016/j.wneu.2018.04.217
65. Lin Q, Yang PF, Jia YZ, Pei JS, Xiao H, Zhang TT, et al. Surgical treatment and long-term outcome of cerebral cavernous malformations-related epilepsy in pediatric patients. Neuropediatrics. (2018) 49:173–9. doi: 10.1055/s-0038-1645871
66. Yang ZX, He ZB, Wang HW, Zhao XD, Wang YD, Zhang GR. The effect of gamma knife treatment on intracranial epileptogenic solitary cavernous angiomas. Chin J Stereotact Funct Neurosurg. (2019) 32:193–6. doi: 10.3210/j.issn:1008-2425.2019.04.193
67. He K, Jiang S, Song J, Wu Z, Chen L, Mao Y. Long-term outcomes of surgical treatment in 181 patients with supratentorial cerebral cavernous malformation-associated epilepsy. World Neurosurg. (2017) 108:869–75. doi: 10.1016/j.wneu.2017.08.095
68. Yang PF, Pei JS, Jia YZ, Lin Q, Xiao H, Zhang TT, et al. Surgical management and long-term seizure outcome after surgery for temporal lobe epilepsy associated with cerebral cavernous malformations. World Neurosurg. (2018) 110:e659–70. doi: 10.1016/j.wneu.2017.11.067
69. Wang KY, Idowu OR, Lin DDM. Radiology and imaging for cavernous malformations. Handb Clin Neurol. (2017) 143:249–66. doi: 10.1016/B978-0-444-63640-9.00024-2
70. Botterill JJ, Brymer KJ, Caruncho HJ, Kalynchuk LE. Aberrant hippocampal neurogenesis after limbic kindling: relationship to BDNF and hippocampal-dependent memory. Epilepsy Behav. (2015) 47:83–92. doi: 10.1016/j.yebeh.2015.04.046
71. Englot D, Han S, Lawton M, Chang E. Predictors of seizure freedom in the surgical treatment of supratentorial cavernous malformations. J Neurosurg. (2011) 115:1169–74. doi: 10.3171/2011.7.JNS11536
72. Davenport WJ, Siegel AM, Dichgans J, Drigo P, Mammi I, Pereda P, et al. CCM1 gene mutations in families segregating cerebral cavernous malformations. Neurology. (2001) 56:540–3. doi: 10.1212/WNL.56.4.540
Keywords: brain cavernous hemangioma, seizure, neurosurgery, radiosurgery, meta-analysis
Citation: Gao X, Yue K, Sun J, Cao Y, Zhao B, Zhang H, Dai S, Zhang L, Luo P and Jiang X (2020) Treatment of Cerebral Cavernous Malformations Presenting With Seizures: A Systematic Review and Meta-Analysis. Front. Neurol. 11:590589. doi: 10.3389/fneur.2020.590589
Received: 02 August 2020; Accepted: 25 September 2020;
Published: 26 October 2020.
Edited by:
Jose F. Tellez-Zenteno, University of Saskatchewan, CanadaReviewed by:
Antonina Sidoti, University of Messina, ItalyGiuseppe Lanzino, Mayo Clinic, United States
Copyright © 2020 Gao, Yue, Sun, Cao, Zhao, Zhang, Dai, Zhang, Luo and Jiang. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Peng Luo, cGVuZ2x1b0BmbW11LmVkdS5jbg==; Xiaofan Jiang, amlhbmd4ZkBmbW11LmVkdS5jbg==
†These authors have contributed equally to this work
 Xiangyu Gao
Xiangyu Gao Kangyi Yue†
Kangyi Yue† Lei Zhang
Lei Zhang Peng Luo
Peng Luo