- 1Department of Physical Medicine and Rehabilitation, Harvard Medical School, Boston, MA, United States
- 2Spaulding Rehabilitation Hospital, Charlestown, MA, United States
- 3Spaulding Research Institute, Charlestown, MA, United States
- 4MassGeneral Hospital for Children Sports Concussion Program, Boston, MA, United States
- 5Home Base, A Red Sox Foundation and Massachusetts General Hospital Program, Charlestown, MA, United States
- 6Sydney Partnership for Health, Education, Research and Enterprise (SPHERE), Sydney, NSW, Australia
- 7School of Medical Sciences, University of New South Wales, Randwick, NSW, Australia
- 8Priority Research Centre for Stroke and Brain Injury, School of Medicine and Public Health, University of Newcastle, Callaghan, NSW, Australia
- 9Hunter New England Local Health District Sports Concussion Program, Waratah, NSW, Australia
Background: There is considerable interest in determining whether later-in-life depression is associated with lifetime history of concussions or the duration of a career in professional contact and collision sports. Rugby league is a high-intensity collision sport involving a large number of tackles per game and a high rate of concussions. We examined predictors and correlates of depression in retired elite level rugby league players in Australia.
Methods: Retired elite level rugby league players (N = 141, age: M = 52.6, SD = 13.8; Range = 30–89 years) completed the Depression, Anxiety, and Stress Scale (DASS), Brief Pain Inventory, Connor-Davidson Resilience Scale (CD-RISC), and Epworth Sleepiness Scale; they also reported on lifetime history of concussions. The DASS depression score was regressed on age, total number of self-reported concussions, years played professionally, CD-RISC score, BPI pain interference score, and ESS score.
Results: The retired players reported a median of 15 total lifetime concussions [interquartile range (IQR) = 6–30], and a median of 8 years playing professional sports (IQR = 3.5–11). The proportion of the sample endorsing at least mild current depression was 29%. The DASS depression score was positively correlated with the DASS anxiety (r = 0.54) and DASS stress scores (r = 0.58). The CD-RISC score was negatively correlated with the depression score (r = −0.53). Depression scores were not significantly correlated with pain severity (r = 0.14), and were weakly correlated with life interference due to pain (r = 0.20) and years playing professional sports (r = −0.17). Depression scores were not significantly correlated with lifetime history of concussions (r = 0.14). A multiple regression model, with age, total number of self-reported concussions, years played professionally, the CD-RISC, Brief Pain Inventory-pain interference score, and Epworth Sleepiness Scale score as predictors was significant, with 35% of the variance in DASS depression accounted for. The two significant independent predictors of depression were lower resilience and greater life interference due to pain.
Conclusions: This is the first large study of depression in retired rugby league players. Depression in these retired players was not meaningfully associated with lifetime history of concussions or number of years playing elite level collision sport. Depression was associated with current anxiety, stress, resilience, and life interference due to chronic pain.
Introduction
Some retired professional athletes suffer from depression (1–12). There is considerable interest in whether repetitive neurotrauma, either in the form of concussions, or so-called subconcussive impacts, is associated with later in life mental health problems in former amateur and professional contact, collision, and combat sport athletes (13–16). Researchers have reported an association between a greater number of self-reported concussions and greater symptoms of later-in-life depression (17–22). The duration of a professional career is sometimes used as a proxy for exposure to low-level repetitive mild neurotrauma (23). The literature on the association between career duration and later in life depression is mixed, with some studies reporting a positive association (24) and some not (8, 25). In recent years, researchers have asserted that depression and suicidality are clinical features of chronic traumatic encephalopathy (CTE) (26–34), although the evidence for this assertion is limited (35–39), and depression and suicidality were not considered to be clinical features of CTE between 1929 and 2009 (40, 41). Nonetheless, this assertion amplifies the importance of studying depression in retired professional contact and collision sport athletes.
Depression in the General Population
The lifetime prevalence of depression in men born in the United States is ~20–28% (42). In the general population, it is understood that depression arises from the cumulative effects (43–45) of (i) genetics (46–49), (ii) adverse events in childhood (50–53) such as abuse and neglect, and (iii) current life stressors (54–57) such as relationship problems (58–60), employment instability (61–63), and financial problems (61, 62, 64, 65). Retired professional athletes can be affected by any of those factors.
Chronic Pain and Depression
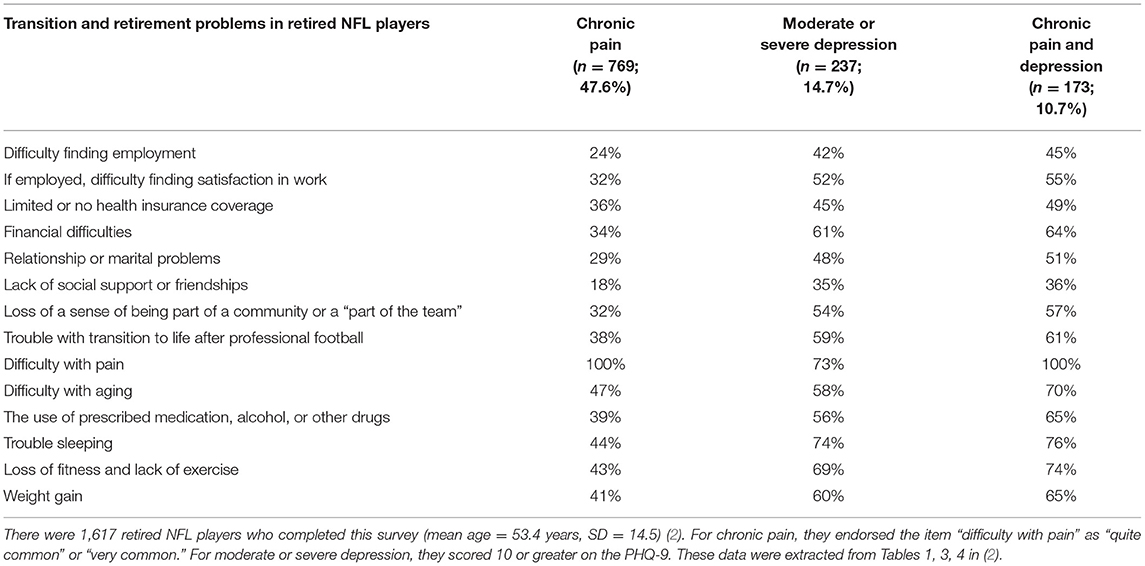
Importantly, former professional athletes also suffer from chronic pain (2, 3, 15, 66), and chronic pain is a well-established risk factor for and correlate of depression (67). Chronic pain is bidirectionally associated with depression (68–72) in that those with depression are more likely to have chronic pain and those with chronic pain are more likely to develop depression—and the two conditions might magnify each other. People with chronic pain are also at increased risk for suicidal ideation (73) and suicide (74). There is an association between chronic pain and depression in former professional soccer players (8) and NFL players (66). In former NFL players, there is an association between pain catastrophizing and depression (3). Moreover, in retired NFL players, the association between chronic pain and depression appears to be partially mediated by worsening physical functioning and other functional limitations (75). In a survey that sampled former NFL players with chronic pain, depression, or both, many reported difficulties related to their retirement transition away from football, such as financial trouble, sleep difficulties, weight gain, relationship problems, and more (2). These findings are summarized in Table 1.
Resilience and Depression
There is considerable interest in the role resilience might play regarding both depression and chronic pain (76–80). Resilience underlies a person's ability to cope with, adapt to, or overcome adversity. Resilience is manifested through adaptive behavior (81), a positive view of one's self, the world, and the future (82), and positive emotions, even in stressful situations (83). Greater resilience is associated with fewer symptoms of depression in older adults in general (84), less severe self-reported depression in older adults who are experiencing major depressive disorder (85), and a greater response to medication treatment for depression (86).
Purpose and Hypotheses
For the past 8 years, a study of the brain health of retired elite level rugby league players from Australia has been underway (87–90). This study was approved by the Institutional Human Ethics Committee. Rugby league is a high-intensity collision sport involving a large number of tackles per game (91, 92) and a fairly high rate of concussions (93). The purpose of the current study is to examine predictors and correlates of depression in retired elite level rugby league players. We hypothesized that (i) a small subgroup of retired players would endorse symptoms consistent with depression. In terms of simple bivariate relationships, we hypothesized that (ii) a greater number of past concussions would be associated with more symptoms of current depression, (iii) more years of exposure to professional sport would be associated with more symptoms of depression, (iv) greater resilience would be associated with fewer symptoms of depression, and (v) greater chronic pain would be associated with more symptoms of depression. However, these variables are likely interrelated in retired elite level rugby league players, and we were ultimately interested in the strongest overall predictor(s) of depressive symptoms among the larger set of correlates. Consequently, in a multivariate model predicting depression from the following variables: age, lifetime history of concussions, years playing professional rugby league, resilience, chronic pain severity, and subjective sleepiness, we hypothesized that only resilience and chronic pain severity would be significant independent predictors.
Materials and Methods
Participants
Participants were retired elite level rugby league players. They included players that competed at the first grade level in the New South Wales Rugby League (NSWRL, 1908–1994), Australian Rugby League (1995–1997), Super League (1997), and/or National Rugby League (1998–present). These men were recruited in two ways. First, they were recruited through communication via club “old boys” (alumni) networks, who distributed study information to their members. Second, they were recruited through direct and indirect referrals from the National Rugby League and the Men of League Foundation, who also distributed information pertaining to the study to their members. Potential participants were excluded if they reported a history of neurosurgery or of a brain tumor requiring radiation treatment. We analyzed the data from the first 145 retired players. For this study, we excluded four of these men because they did not complete the self-report measure of depression (three of whom had dementia, which precluded their full participation in the study).
Procedures
This study, called The Retired Professional Rugby League Players Brain Health Research Program, has been running since 2012, and has been modified over the years. In its present form, the study incorporates a health survey, an in-person clinical evaluation, multi-modal experimental neuroimaging, blood biomarkers and genetic testing, and brain and spinal cord donation. Participants may opt in or out of any aspect of the research protocol. All participants completed a clinical interview, which was immediately followed by neurocognitive testing with a clinical neuropsychologist (i.e., author AG). The clinical interview collected data pertaining to demographic information and medical and concussion history, together with patient reported outcome measures. The interview and neurocognitive testing took ~2 h and 30 min in total. All variables used in this study were collected during the clinical interview and on questionnaires.
Measures
Exposure Variables
Concussion history was based on self-report. During an interview, a definition of concussion was provided to the participants (from the Consensus statement on concussion in sport, 2012 definition) (94). Participants were allowed to ask questions in order to clarify the definition. They reported the number of sport-related and non-sport-related concussions they sustained throughout their lives; these two values were summed in order to determine the total number of lifetime concussions for each participant. This variable was used for all lifetime concussion analyses in this manuscript. Number of years played at the elite level and number of games played at the elite level were also based on self-report.
Questionnaires
The Depression, Anxiety, Stress Scale 21-item (DASS-21) (95) is a shortened version of the original 42-item version (96). Each item is a statement about a negative emotional symptom and is rated by the participant on a 0–3 scale based on the extent to which they experienced that symptom over the past week. The scores for each of the three scales (i.e., depression, anxiety, and stress) are derived by summing the scores for the seven items that comprise that scale and multiplying the sum by 2. Higher scores reflect more symptoms. The total score for each scale is converted to a classification (i.e., normal, mild, moderate, severe/extremely severe) using the DASS Manual (97). Internal consistency (Cronbach's alpha) is high for each scale (depression = 0.94, anxiety = 0.87, Stress = 0.91) (95).
The Connor-Davidson Resilience Scale (CD-RISC) (98) is a 25-item measure that evaluates resilience without specifying a particular time interval. Each item is rated on a 0–4 scale (i.e., “not at all true” to “true nearly all of the time”), with a total score range from 0 to 100. Higher scores reflect greater resilience. Factor analysis of this scale yielded five factors, which were broadly interpreted as (1) personal competence/tenacity, (2) trust in one's instincts/tolerance of negative affect, (3) positive acceptance of change, (4) control, and (5) spiritual influences. It has high internal consistency (Cronbach's alpha = 0.89) in the general population (98).
The Epworth Sleepiness Scale (ESS) (99) is an 8-item self-report scale that assesses how likely the participant is to fall asleep during a variety of different situations (e.g., “sitting and reading,” “watching TV”). There is no specified time interval for the participant to consider. Each item is rated on a 0–3 scale (i.e., would never doze, slight chance of dozing, moderate change of dozing, high chance of dozing), with a total score range of 0–24. The questionnaire has a high level of internal consistency (Cronbach's alpha = 0.88) (100). Test-retest reliability (i.e., intra-class correlation coefficient) was 0.88 in a large sample of high school students (101).
The Brief Pain Inventory (BPI), Short Form (102, 103) is a self-report scale that measures the severity of pain and how it has interfered with activities over the past week. One subscale measures Pain Severity, which is the average of four items that assess pain at its worst, least, on average, and currently; each item is rated 0–10, from “no pain” to “pain as bad as you can imagine.” The second subscale measures Pain Interference, which is the average of seven items that assess the degree to which the pain interferes with general activity, mood, walking ability, sleep, etc.; each item is rated 0–10, from “does not interfere” to “completely interferes.” Higher scores indicate greater severity/interference. Internal consistency and test-retest reliability are consistently high across studies (104).
The Alcohol Use Disorders Identification Test (AUDIT): Self-Report Version (105, 106) is a 10-item instrument developed by the World Health Organization to identify harmful alcohol consumption by assessing frequency/amount of alcohol use (Questions 1–3), alcohol dependence (Questions 4–6), and alcohol-related problems (Questions 7–10). Various time intervals are assessed (e.g., weekly use of alcohol, consumption in the past year). Each item is rated on a 0–4 scale, with score ranges from 0 to 40 (higher = more hazardous alcohol use). A systematic review of its psychometric properties indicated a test-retest reliability over 0.8 on most studies, as well as a Cronbach's alpha of 0.81–0.93 (107). Risk level was classified based on the total score (0–7 = low risk; 8–15 = risky/hazardous; 16–19 = high-risk/harmful; ≥20 = high-risk) based on the manual (106).
Statistical Analyses
Descriptive statistics were computed for all variables used in the analyses. Most variables were non-normally distributed, so non-parametric statistics were used where appropriate. Spearman correlations were conducted between DASS depression, anxiety, and stress scores, as well as between these three variables and (i) the CD-RISC score, (ii) the BPI pain severity and pain interference scores, (iii) the AUDIT score, and (iv) the ESS score. Spearman correlations were also conducted between the DASS depression score and (i) total number of self-reported concussions and (ii) contact sport exposure (years playing rugby professionally and number of professional games played).
A simultaneous multiple regression was modeled, with the DASS depression score as the outcome and the following variables as predictors: age, total number of self-reported concussions, years played professionally, CD-RISC score, BPI pain interference score, and ESS score. Plots of standardized predicted values against standardized residuals were visually inspected to evaluate normality and homoscedasticity. Standardized residuals (with values ±1.96 reflecting unusual cases) and Cook's distance (with >1 defining problematic influential cases) were used to examine outliers. Multicollinearity was defined as correlations among predictors >0.8, variance inflation factor (VIF) values >10, or tolerance values <0.1. Model cross-validation was assessed by examining adjusted R2 in addition to standard R2. Data were analyzed with SPSS version 27.0.
For the hypothesis-based correlational analyses, we used an online calculator to compute the False Discovery Rate. This method controls for Type I error, with alpha set at p < 0.05 (two-tailed tests), which decreases the odds of finding a false positive result while maintaining high statistical power compared to other methods used to correct for multiple comparisons [e.g., Bonferroni correction; (108)].
Results
Demographic Characteristics and Exposure History
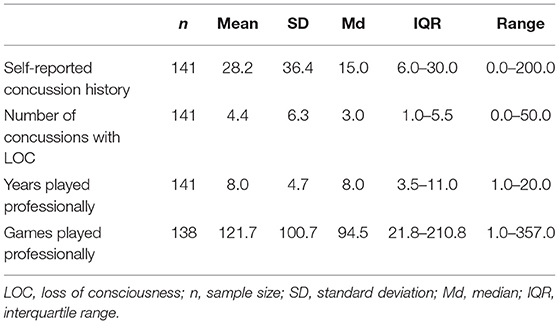
The mean age of the sample was 52.6 years (SD = 13.8, Range = 30–89) and the mean years of education was 11.9 (SD = 2.6, Range = 7.0–18.0). Approximately 71.6% of the retired players were married, 17.0% were divorced, 7.8% reported their marital status as single, 2.1% were cohabitating, and 1.4% were separated. The retired players reported their employment status as follows: employed full-time = 77.3%, employed part-time = 2.8%, retired = 18.4%, or unemployed = 1.4%. The median number of past concussions reported was 15.0, with 50% of the sample reporting between 6.0 and 30.0 prior concussions (Table 2). The median number of years competing at the elite level was 8.0 (IQR = 3.5–11.0).
Health History and Self-Report Measures
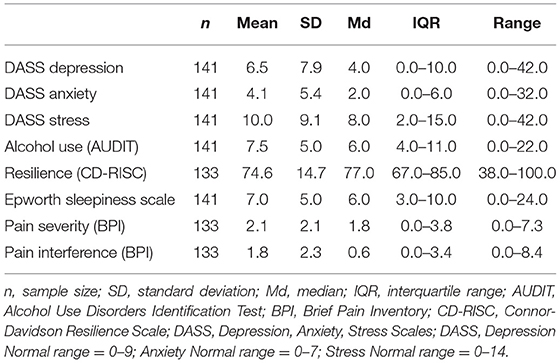
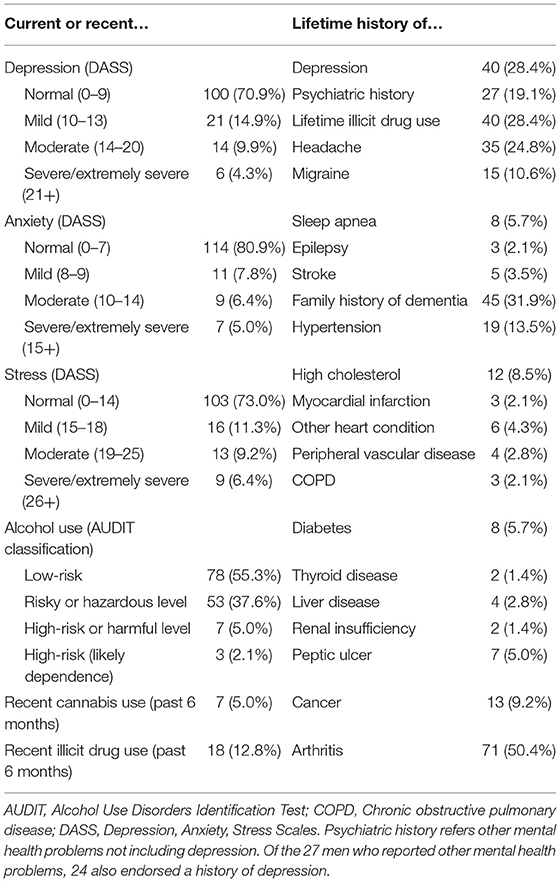
Descriptive statistics for the self-report measures are provided in Table 3. The mean scores for the sample on the depression, anxiety, and stress measures (DASS) were in the “normal classification range.” A lifetime history of depression was reported by 28.4% of the sample (Table 4). A lifetime history of drug use was reported by 28.4%. Regarding current psychological distress on the DASS, 29.1% of the retired players reported at least mild depression, 19.2% reported at least mild anxiety, and 27.0% reported at least mild stress. The breakdown of participants by DASS Depression classification ranges was as follows: Broadly Normal = 70.9%, Mild = 14.9%, Moderate = 9.9%, and Severe/Extremely Severe = 4.3%.
Bivariate Predictors of, and Correlates With, Depression
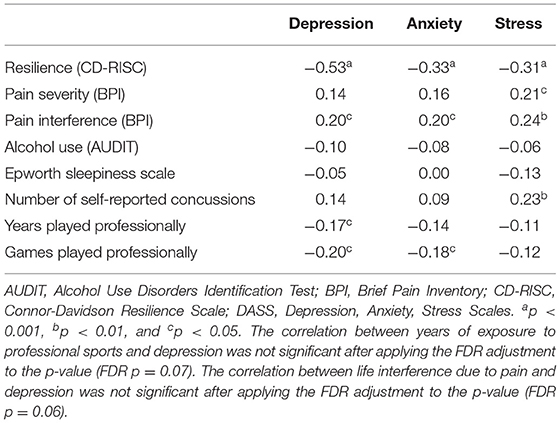
The DASS depression, anxiety, and stress subscales were positively correlated with one another (r = 0.54–0.58). Correlations between DASS depression, anxiety, and stress scores and other variables of interest are presented in Table 5.
Hypotheses (ii)–(v) relate to the associations between symptoms of depression and concussion history, years of exposure to professional sports, resilience, and chronic pain (both severity and life interference). There was no significant correlation between lifetime history of concussions and depression. There was a small significant negative correlation (r = −0.17, p = 0.04) between years of exposure to professional sports and depression (although this was not significant after applying the FDR p-value adjustment for the five hypothesis-based correlations: FDR p = 0.07). The resilience score (i.e., CD-RISC) was negatively correlated with depression (r = −0.53; p < 0.001), with a large effect size, indicating that higher levels of resilience are related to lower depression. Pain severity was not significantly correlated with depression. There was a small, significant (r = 0.20; p = 0.02) correlation between life interference due to pain and depression, but this association was not significant after applying the FDR adjustment to the p-value (FDR p = 0.06).
Multivariable Prediction Model
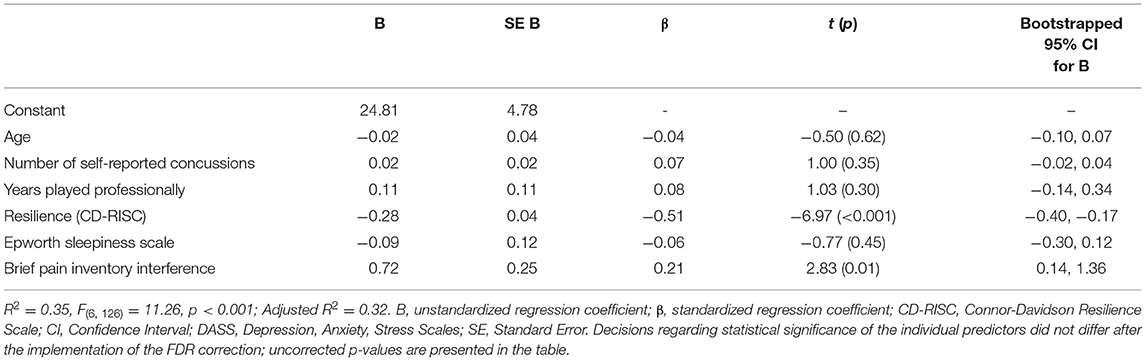
When evaluating the statistical assumptions for the regression, no Cook's distances exceeded 1. Only five cases (3.5% of the sample) had standardized residuals of ±1.96, suggesting that influential cases were not an issue in the model. Multicollinearity was also not a problem because the correlations between predictors were all well below 0.8, VIF values were all <1.1, and tolerance values were all >0.95. Assumptions of normality and homoscedasticity may not have been met for all variables, based on plots of standardized predicted values against standardized residuals. However, results from bootstrapped parameters (1,000 samples) did not differ from the initial results, suggesting no undue influence on model parameters.
Results of the regression are presented in Table 6. The model was significant (p < 0.001), with 35% of the variance in DASS depression accounted for by the set of predictors. After adjusting for model cross-validation, R2 was reduced to 0.32. Consistent with hypothesis (vi), the only significant predictors of DASS depression were resilience (the CD-RISC), β = −0.51, t = −6.97, p < 0.001 and BPI pain interference, β = 0.21, t = 2.83, p < 0.01. Age, number of self-reported concussions, years played at the elite level, and sleepiness were not significant.
Discussion
We examined predictors and correlates of depression in retired elite level rugby league players. A lifetime history of depression was reported by 28.4% of the sample. Half of the retired players reported having arthritis (50.4%). Some degree of alcohol misuse was reported by 44.7% of the sample, and 12.8% reported recent drug use. Current moderate to severe depression (14.8%), anxiety (11.4%), and stress (15.6%) was reported by a small percentage of the sample. Greater resilience was associated with lower levels of depression, anxiety, and stress. There was a small positive correlation between life interference due to pain and depression. There was no association between lifetime history of concussions and current depression. There was a very weak negative correlation between exposure to professional sports (years played and games played) and current symptoms of depression, meaning that greater exposure was associated with fewer symptoms of depression. Finally, a multivariate model regressing depression on age, lifetime history of concussions, years playing elite rugby league, resilience, life interference due to chronic pain, and sleepiness accounted for 35% of the variance in depression. The only statistically significant independent predictors of depression were resilience and life interference due to pain.
Correlates of Depression in Former Elite and Professional Athletes
Some former professional contact and collision sport athletes experience depression (1–4, 7–12, 109). There are many reasons why former professional athletes might experience depression. The transition to retirement is often difficult and it can be associated with a tremendous sense of loss (110), a void in meaning and purpose (111, 112), and even financial hardship (113). Those former athletes who retire due to injury tend to have more difficulty with psychological adjustment to retirement than those who are more in control of their retirement decision (8). Most elite athletes have a strong sense of athletic identity (8, 114), which refers to the degree to which they identify very strongly with their athlete role as a core part of their fundamental sense of self, and look to others for acknowledgment and validation of that identity. Greater athletic identity has been associated with greater symptoms of depression in some retired professional athletes (8). In a study of former professional soccer players, screening positively for depression was associated with being younger, more recently retired, having higher athletic identity, and citing injury as the main reason for retirement (8). That said, in large-scale cohort study comparing former professional soccer players (n = 7,676) to matched general population control subjects (n = 23,028), hospital admissions for common mental health disorders were lower for the former players than the population controls (115).
Chronic pain (2) and osteoarthritis (116) are associated with depression and psychological distress in elite and professional athletes. In the present study, half (50.4%) reported arthritis and we found a weak association that approached significance between life interference due to chronic pain and current symptoms of depression. In the general population, there is a strong association between chronic pain and depression (67–72). In studies of retired NFL players (2, 3, 66, 75) and former athletes in other contact sports (8), chronic pain is associated with symptoms of depression. In one study of former NFL players (3), the correlation between symptoms of depression, measured using the CES-D, and pain intensity (r = 0.43) and life interference due to pain (r = 0.58) were considerably higher than correlations in the present study between symptoms of depression measured on the DASS and pain severity (r = 0.14) and life interference due to pain (r = 0.29).
In the present study, we found a strong negative association between resilience and depression. Although prior studies with retired elite and professional athletes have examined the prevalence and correlates of depression (15) and common mental disorders (9), the association between resilience and depression has not, to our knowledge, been explored. Nonetheless, researchers have recommended developing interventions for retired athletes that improve psychological resilience (9). In the general population, greater resilience is associated with fewer symptoms of depression in older adults (84), less severe self-reported depression in older adults who are experiencing major depressive disorder (85), and a greater response to medication treatment for depression (86).
Association Between Depression and Exposure to Neurotrauma
In the present study, a greater lifetime history of concussions and a greater history of exposure to elite-level collision sports were not associated with current symptoms of depression. This study is inconsistent with survey studies of former elite and professional athletes that have shown an association between a greater number of prior concussions and current symptoms of depression (17–22). Those studies were conducted prior to the greatly increased awareness of, and sensitivity to, concussions. Additionally, subjects in those studies reported far fewer past concussions than the subjects in the present study, and the effects of this reporting difference are unknown. Our results are also inconsistent with a small clinical study of retired NFL players that showed a significant correlation of r = 0.43 between lifetime number of concussions and Beck Depression Inventory-Second Edition scores (117). The results of this study also differ from other clinical studies of retired NFL players that have shown an association between a greater number of years played professionally and current symptoms of depression (24). These results align, however, with other studies of retired elite or professional athletes that have not found an association between concussion history (118) or greater number of years of exposure (8, 25) and current symptoms of depression or psychological distress.
Limitations
This study has several limitations. First, the study design was cross sectional and, therefore, no casual inference is permitted. Second, the sample consisted of male retired professional rugby league players, a narrow demographic group, which limits generalizability to other populations (e.g., women, amateur athletes, athletes from other sports). Third, it is possible that sampling bias may have led to the recruitment of healthier and higher functioning participants because they are more likely to be connected with alumni organizations and were informed about this research. Fourth, both lifetime concussion history and contact sport exposure were assessed via self-report. Consequently, these data may be subject to biases and memory failures associated with retrospective recall. Fifth, the various self-report measures used in this study assessed symptoms over somewhat different time intervals. Therefore, it was not possible to evaluate long-standing (or lifetime) health issues for those variables that only evaluated a more recent time interval. For example, the DASS and BPI measure symptoms of depression, anxiety, stress, and pain over the past week, and the CD-RISC and ESS evaluate resilience and sleepiness in general, without specifying a particular time period. There may be limited associations among the variables, given that psychological and other health factors can fluctuate over time. Sixth, we did not use structured psychiatric interviews to assess the full criteria for psychiatric disorders. Finally, the goal of this study was to examine the association between indices of past neurotrauma (i.e., history of concussions and duration of exposure to elite level sports) and current depressive symptoms. We included a small number of other variables that have previously been associated with depression symptoms. Our goal was not to try to comprehensively explain the variance in depressive symptoms, and we did not include other variables in the model that may be related to depressive symptoms such as alcohol/drug use, or disability status. A future study with a larger sample size could include more demographic and clinical variables in the model.
Conclusions
Researchers have reported that correlates of depression and psychological distress in retired elite and professional athletes include retirement due to injury (8), greater athletic identity (8), a higher level of career dissatisfaction (11, 119), current adverse life events (11, 12, 119), chronic pain (2, 3, 66, 75), osteoarthritis (116), and lifetime history of prior concussions (17–22). In the present study, neither lifetime history of concussions nor contact sport exposure were meaningfully related to depression in retired elite level rugby league players. Resilience was found to be a particularly strong correlate of depression. Future researchers should examine longitudinal predictors of depression in order to better delineate the developmental trajectory of depression during and after rugby league participation.
Data Availability Statement
The original contributions presented in the study are included in the article, further inquiries can be directed to the corresponding author. The statistical code, syntax, output, and analyses are available to qualified researchers upon request. Requests for this information should be directed to Andrew J. Gardner, QW5kcmV3LkdhcmRuZXJAbmV3Y2FzdGxlLmVkdS5hdQ==.
Ethics Statement
The studies involving human participants were reviewed and approved by the University of Newcastle Human Ethics Committee. The patients/participants provided their written informed consent to participate in this study.
Author Contributions
GI conceptualized the study and wrote portions of the manuscript. RV, GI, and DT conceptualized the statistical analyses. RV performed the statistical analyses and prepared the first draft of the Results section. CL assisted with securing funding. AG is the overall principal investigator, secured funding for the larger parent study, directed that study, collected all of the data, managed the database, helped conceptualize this study, and wrote portions of the manuscript. All authors critically reviewed the manuscript, read, and approved the last version of this manuscript.
Funding
This study was funded in part by the NSW Sporting Injuries Committee, the Brain Foundation, Australia, and the Priority Research Centre for Stroke and Brain Injury. Unrestricted philanthropic support was provided by the National Rugby League, ImPACT Applications, Inc., the Mooney-Reed Charitable Foundation, and the Spaulding Research Institute. The funders were not involved in the study design, collection, analysis, interpretation of data, the writing of this article or the decision to submit it for publication.
Conflict of Interest
GI serves as a scientific advisor for NanoDx™ (formerly BioDirection, Inc.), Sway Operations, LLC, and Highmark, Inc. He has a clinical and consulting practice in forensic neuropsychology, including expert testimony, involving individuals who have sustained mild TBIs (including athletes). He has received research funding from several test publishing companies, including ImPACT Applications, Inc., CNS Vital Signs, and Psychological Assessment Resources (PAR, Inc.). He has received research funding as a principal investigator from the National Football League, and salary support as a collaborator from the Harvard Integrated Program to Protect and Improve the Health of National Football League Players Association Members. DT serves as a consultant for REACT Neuro, Inc. CL serves as a consultant neurologist to the National Rugby League (NRL) providing a pro bono second opinion to current players regarding concussion assessment and management for the player's club doctor. AG serves as a scientific advisor for hitIQ, Ltd. He has a clinical practice in neuropsychology involving individuals who have sustained sport-related concussion (including current and former athletes). He has been a contracted concussion consultant to Rugby Australia since July 2016. He has received travel funding or been reimbursed by professional sporting bodies, and commercial organizations for discussing or presenting sport-related concussion research at meetings, scientific conferences, workshops, and symposiums. Previous grant funding includes the NSW Sporting Injuries Committee, the Brain Foundation (Australia), an Australian-American Fulbright Commission Postdoctoral Award, a Hunter New England Local Health District, Research, Innovation and Partnerships Health Research & Translation Centre and Clinical Research Fellowship Scheme, and the Hunter Medical Research Institute (HMRI), supported by Jennie Thomas, and the HMRI, supported by Anne Greaves. He is currently funded through an NHMRC Early Career Fellowship, and the University of Newcastle's Priority Research Centre for Stroke and Brain Injury. He has received research funding from the National Rugby League (NRL) for the Retired Players Brain Health research program.
The remaining author declares that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
Acknowledgments
The authors acknowledge and thank the Men of League Foundation for assistance with recruiting former players for this research program.
References
1. Weir DR, Jackson JS, Sonnega A. National Football League Player Care Foundation: Study of Retired NFL Players. Ann Arbor, MI: University of Michigan; Institute for Social Research (2009).
2. Schwenk TL, Gorenflo DW, Dopp RR, Hipple E. Depression and pain in retired professional football players. Med Sci Sports Exerc. (2007) 39:599–605. doi: 10.1249/mss.0b013e31802fa679
3. Mannes ZL, Ferguson EG, Perlstein WM, Waxenberg LB, Cottler LB, Ennis N. Negative health consequences of pain catastrophizing among retired National Football League athletes. Health Psychol. (2020) 39:452–62. doi: 10.1037/hea0000847
4. Mackinnon AL, Jackson K, Kuznik K, Turner A, Hill J, Davies MAM, et al. Increased risk of musculoskeletal disorders and mental health problems in retired professional jockeys: a cross-sectional study. Int J Sports Med. (2019) 40:732–8. doi: 10.1055/a-0902-8601
5. Jones ME, Davies MAM, Leyland KM, Delmestri A, Porter A, Ratcliffe J, et al. Osteoarthritis and other long-term health conditions in former elite cricketers. J Sci Med Sport. (2018) 21:558–63. doi: 10.1016/j.jsams.2017.10.013
6. Schuring N, Kerkhoffs G, Gray J, Gouttebarge V. The mental wellbeing of current and retired professional cricketers: an observational prospective cohort study. Phys Sportsmed. (2017) 45:463–9. doi: 10.1080/00913847.2017.1386069
7. Kilic O, Aoki H, Haagensen R, Jensen C, Johnson U, Kerkhoffs G, et al. Symptoms of common mental disorders and related stressors in Danish professional football and handball. Eur J Sport Sci. (2017) 17:1328–34. doi: 10.1080/17461391.2017.1381768
8. Sanders G, Stevinson C. Associations between retirement reasons, chronic pain, athletic identity, and depressive symptoms among former professional footballers. Eur J Sport Sci. (2017) 17:1311–8. doi: 10.1080/17461391.2017.1371795
9. Gouttebarge V, Kerkhoffs G. A prospective cohort study on symptoms of common mental disorders among current and retired professional ice hockey players. Phys Sportsmed. (2017) 45:252–8. doi: 10.1080/00913847.2017.1338497
10. Gouttebarge V, Aoki H, Kerkhoffs GM. Prevalence and determinants of symptoms related to mental disorders in retired male professional footballers. J Sports Med Phys Fitness. (2016) 56:648–54.
11. Gouttebarge V, Kerkhoffs G, Lambert M. Prevalence and determinants of symptoms of common mental disorders in retired professional Rugby Union players. Eur J Sport Sci. (2016) 16:595–602. doi: 10.1080/17461391.2015.1086819
12. Gouttebarge V, Frings-Dresen MH, Sluiter JK. Mental and psychosocial health among current and former professional footballers. Occup Med. (2015) 65:190–6. doi: 10.1093/occmed/kqu202
13. Gouttebarge V, Kerkhoffs G. Sports career-related concussion and mental health symptoms in former elite athletes. Neurochirurgie. (2020). doi: 10.1016/j.neuchi.2020.01.001
14. Manley G, Gardner AJ, Schneider KJ, Guskiewicz KM, Bailes J, Cantu RC, et al. A systematic review of potential long-term effects of sport-related concussion. Br J Sports Med. (2017) 51:969–77. doi: 10.1136/bjsports-2017-097791
15. Mannes ZL, Waxenberg LB, Cottler LB, Perlstein WM, Burrell LE 2nd, Ferguson EG, et al. Prevalence and correlates of psychological distress among retired elite athletes: a systematic review. Int Rev Sport Exerc Psychol. (2019) 12:265–94. doi: 10.1080/1750984X.2018.1469162
16. McAllister T, McCrea M. Long-term cognitive and neuropsychiatric consequences of repetitive concussion and head-impact exposure. J Athl Train. (2017) 52:309–17. doi: 10.4085/1062-6050-52.1.14
17. Terpstra AR, Vasquez BP, Colella B, Tartaglia MC, Tator CH, Mikulis D, et al. Comprehensive neuropsychiatric and cognitive characterization of former professional football players: implications for neurorehabilitation. Front Neurol. (2019) 10:712. doi: 10.3389/fneur.2019.00712
18. Kerr ZY, Thomas LC, Simon JE, McCrea M, Guskiewicz KM. Association between history of multiple concussions and health outcomes among former college football players: 15-year follow-up from the NCAA concussion study (1999-2001). Am J Sports Med. (2018) 46:1733–41. doi: 10.1177/0363546518765121
19. Gouttebarge V, Aoki H, Lambert M, Stewart W, Kerkhoffs G. A history of concussions is associated with symptoms of common mental disorders in former male professional athletes across a range of sports. Phys Sportsmed. (2017) 45:443–9. doi: 10.1080/00913847.2017.1376572
20. Kerr ZY, Evenson KR, Rosamond WD, Mihalik JP, Guskiewicz KM, Marshall SW. Association between concussion and mental health in former collegiate athletes. Inj Epidemiol. (2014) 1:28. doi: 10.1186/s40621-014-0028-x
21. Kerr ZY, Marshall SW, Harding HP Jr, Guskiewicz KM. Nine-year risk of depression diagnosis increases with increasing self-reported concussions in retired professional football players. Am J Sports Med. (2012) 40:2206–12. doi: 10.1177/0363546512456193
22. Guskiewicz KM, Marshall SW, Bailes J, McCrea M, Harding HP Jr, Matthews A, et al. Recurrent concussion and risk of depression in retired professional football players. Med Sci Sports Exerc. (2007) 39:903–9. doi: 10.1249/mss.0b013e3180383da5
23. Mez J, Daneshvar DH, Abdolmohammadi B, Chua AS, Alosco ML, Kiernan PT, et al. Duration of American football play and chronic traumatic encephalopathy. Ann Neurol. (2020) 87:116–31. doi: 10.1002/ana.25611
24. Roberts AL, Pascual-Leone A, Speizer FE, Zafonte RD, Baggish AL, Taylor H Jr, et al. Exposure to American Football and neuropsychiatric health in former national football league players: findings from the football players health study. Am J Sports Med. (2019) 47:2871–80. doi: 10.1177/0363546519868989
25. Clark MD, Varangis EML, Champagne AA, Giovanello KS, Shi F, Kerr ZY, et al. Effects of career duration, concussion history, and playing position on white matter microstructure and functional neural recruitment in former college and professional football athletes. Radiology. (2018) 286:967–77. doi: 10.1148/radiol.2017170539
26. Montenigro PH, Baugh CM, Daneshvar DH, Mez J, Budson AE, Au R, et al. Clinical subtypes of chronic traumatic encephalopathy: literature review and proposed research diagnostic criteria for traumatic encephalopathy syndrome. Alzheimers Res Ther. (2014) 6:68. doi: 10.1186/s13195-014-0068-z
27. McKee AC, Stein TD, Nowinski CJ, Stern RA, Daneshvar DH, Alvarez VE, et al. The spectrum of disease in chronic traumatic encephalopathy. Brain. (2013) 136:43–64. doi: 10.1093/brain/aws307
28. Stern RA, Daneshvar DH, Baugh CM, Seichepine DR, Montenigro PH, Riley DO, et al. Clinical presentation of chronic traumatic encephalopathy. Neurology. (2013) 81:1122–9. doi: 10.1212/WNL.0b013e3182a55f7f
29. Gavett BE, Stern RA, McKee AC. Chronic traumatic encephalopathy: a potential late effect of sport-related concussive and subconcussive head trauma. Clin Sports Med. (2011) 30:179–88, xi. doi: 10.1016/j.csm.2010.09.007
30. Stern RA, Riley DO, Daneshvar DH, Nowinski CJ, Cantu RC, McKee AC. Long-term consequences of repetitive brain trauma: chronic traumatic encephalopathy. Pm R. (2011) 3:S460–7. doi: 10.1016/j.pmrj.2011.08.008
31. Baugh CM, Stamm JM, Riley DO, Gavett BE, Shenton ME, Lin A, et al. Chronic traumatic encephalopathy: neurodegeneration following repetitive concussive and subconcussive brain trauma. Brain Imaging Behav. (2012) 6:244–54. doi: 10.1007/s11682-012-9164-5
32. Omalu BI, Bailes J, Hammers JL, Fitzsimmons RP. Chronic traumatic encephalopathy, suicides and parasuicides in professional American athletes: the role of the forensic pathologist. Am J Forensic Med Pathol. (2010) 31:130–2. doi: 10.1097/PAF.0b013e3181ca7f35
33. Omalu B. Chronic traumatic encephalopathy. Prog Neurol Surg. (2014) 28:38–49. doi: 10.1159/000358761
34. Mez J, Daneshvar DH, Kiernan PT, Abdolmohammadi B, Alvarez VE, Huber BR, et al. Clinicopathological evaluation of chronic traumatic encephalopathy in players of American Football. J Am Med Assoc. (2017) 318:360–70. doi: 10.1001/jama.2017.16687
35. Iverson GL. Chronic traumatic encephalopathy and risk of suicide in former athletes. Br J Sports Med. (2014) 48:162–5. doi: 10.1136/bjsports-2013-092935
36. Wortzel HS, Shura RD, Brenner LA. Chronic traumatic encephalopathy and suicide: a systematic review. Biomed Res Int. (2013) 2013:424280. doi: 10.1155/2013/424280
37. Maroon JC, Winkelman R, Bost J, Amos A, Mathyssek C, Miele V. Chronic traumatic encephalopathy in contact sports: a systematic review of all reported pathological cases. PLoS ONE. (2015) 10:e0117338. doi: 10.1371/journal.pone.0117338
38. Iverson GL. Suicide and chronic traumatic encephalopathy. J Neuropsychiatry Clin Neurosci. (2016) 28:9–16. doi: 10.1176/appi.neuropsych.15070172
39. Iverson GL. Retired National Football League players are not at greater risk for suicide. Arch Clin Neuropsychol. (2020) 35:332–41. doi: 10.1093/arclin/acz023
40. Roberts A. Brain Damage in Boxers: A Study of Prevalence of Traumatic Encephalopathy Among Ex-Professional Boxers. London: Pitman Medical Scientific Publishing Co. (1969).
41. Iverson GL, Gardner AJ, Shultz SR, Solomon GS, McCrory P, Zafonte R, et al. Chronic traumatic encephalopathy neuropathology might not be inexorably progressive or unique to repetitive neurotrauma. Brain. (2019) 142:3672–93. doi: 10.1093/brain/awz286
42. Gonzalez HM, Tarraf W, Whitfield KE, Vega WA. The epidemiology of major depression and ethnicity in the United States. J Psychiatr Res. (2010) 44:1043–51. doi: 10.1016/j.jpsychires.2010.03.017
43. Kendler KS, Thornton LM, Gardner CO. Genetic risk, number of previous depressive episodes, and stressful life events in predicting onset of major depression. Am J Psychiatry. (2001) 158:582–6. doi: 10.1176/appi.ajp.158.4.582
44. Kendler KS, Thornton LM, Gardner CO. Stressful life events and previous episodes in the etiology of major depression in women: an evaluation of the “kindling” hypothesis. Am J Psychiatry. (2000) 157:1243–51. doi: 10.1176/appi.ajp.157.8.1243
45. Monroe SM, Harkness KL. Life stress, the “kindling” hypothesis, and the recurrence of depression: considerations from a life stress perspective. Psychol Rev. (2005) 112:417–45. doi: 10.1037/0033-295X.112.2.417
46. Binder EB, Nemeroff CB. The CRF system, stress, depression and anxiety-insights from human genetic studies. Mol Psychiatry. (2010) 15:574–88. doi: 10.1038/mp.2009.141
47. Hauger RL, Risbrough V, Oakley RH, Olivares-Reyes JA, Dautzenberg FM. Role of CRF receptor signaling in stress vulnerability, anxiety, and depression. Ann N Y Acad Sci. (2009) 1179:120–43. doi: 10.1111/j.1749-6632.2009.05011.x
48. McGuffin P, Knight J, Breen G, Brewster S, Boyd PR, Craddock N, et al. Whole genome linkage scan of recurrent depressive disorder from the depression network study. Hum Mol Genet. (2005) 14:3337–45. doi: 10.1093/hmg/ddi363
49. Sullivan PF, Neale MC, Kendler KS. Genetic epidemiology of major depression: review and meta-analysis. Am J Psychiatry. (2000) 157:1552–62. doi: 10.1176/appi.ajp.157.10.1552
50. Bradley RG, Binder EB, Epstein MP, Tang Y, Nair HP, Liu W, et al. Influence of child abuse on adult depression: moderation by the corticotropin-releasing hormone receptor gene. Arch Gen Psychiatry. (2008) 65:190–200. doi: 10.1001/archgenpsychiatry.2007.26
51. Heim C, Newport DJ, Mletzko T, Miller AH, Nemeroff CB. The link between childhood trauma and depression: insights from HPA axis studies in humans. Psychoneuroendocrinology. (2008) 33:693–710. doi: 10.1016/j.psyneuen.2008.03.008
52. Heim C, Bradley B, Mletzko TC, Deveau TC, Musselman DL, Nemeroff CB, et al. Effect of childhood trauma on adult depression and neuroendocrine function: sex-specific moderation by CRH receptor 1 gene. Front Behav Neurosci. (2009) 3:1–10. doi: 10.3389/neuro.08.041.2009
53. Gatt JM, Nemeroff CB, Dobson-Stone C, Paul RH, Bryant RA, Schofield PR, et al. Interactions between BDNF Val66Met polymorphism and early life stress predict brain and arousal pathways to syndromal depression and anxiety. Mol Psychiatry. (2009) 14:681–95. doi: 10.1038/mp.2008.143
54. Farmer AE, McGuffin P. Humiliation, loss and other types of life events and difficulties: a comparison of depressed subjects, healthy controls and their siblings. Psychol Med. (2003) 33:1169–75. doi: 10.1017/S0033291703008419
55. Friis RH, Wittchen HU, Pfister H, Lieb R. Life events and changes in the course of depression in young adults. Eur Psychiatry. (2002) 17:241–53. doi: 10.1016/S0924-9338(02)00682-X
56. Kendler KS, Hettema JM, Butera F, Gardner CO, Prescott CA. Life event dimensions of loss, humiliation, entrapment, and danger in the prediction of onsets of major depression and generalized anxiety. Arch Gen Psychiatry. (2003) 60:789–96. doi: 10.1001/archpsyc.60.8.789
57. Kendler KS, Karkowski LM, Prescott CA. Causal relationship between stressful life events and the onset of major depression. Am J Psychiatry. (1999) 156:837–41. doi: 10.1176/ajp.156.6.837
58. Bodenmann G, Randall AK. Close relationships in psychiatric disorders. Curr Opin Psychiatry. (2013) 26:464–7. doi: 10.1097/YCO.0b013e3283642de7
59. Jaremka LM, Lindgren ME, Kiecolt-Glaser JK. Synergistic relationships among stress, depression, and troubled relationships: insights from psychoneuroimmunology. Depress Anxiety. (2013) 30:288–96. doi: 10.1002/da.22078
60. Bulloch AG, Williams JV, Lavorato DH, Patten SB. The relationship between major depression and marital disruption is bidirectional. Depress Anxiety. (2009) 26:1172–7. doi: 10.1002/da.20618
61. Dooley D, Fielding J, Levi L. Health and unemployment. Annu Rev Public Health. (1996) 17:449–65. doi: 10.1146/annurev.pu.17.050196.002313
62. Kessler RC, Bromet EJ. The epidemiology of depression across cultures. Annu Rev Public Health. (2013) 34:119–38. doi: 10.1146/annurev-publhealth-031912-114409
63. Gallo WT, Bradley EH, Siegel M, Kasl SV. Health effects of involuntary job loss among older workers: findings from the health and retirement survey. J Gerontol B Psychol Sci Soc Sci. (2000) 55:S131–40. doi: 10.1093/geronb/55.3.S131
64. Gonzalez G, Vives A. Work status, financial stress, family problems, and gender differences in the prevalence of depression in Chile. Ann Work Expo Health. (2019) 63:359–70. doi: 10.1093/annweh/wxy107
65. Richardson T, Elliott P, Roberts R. The relationship between personal unsecured debt and mental and physical health: a systematic review and meta-analysis. Clin Psychol Rev. (2013) 33:1148–62. doi: 10.1016/j.cpr.2013.08.009
66. Cottler LB, Ben Abdallah A, Cummings SM, Barr J, Banks R, Forchheimer R. Injury, pain, and prescription opioid use among former National Football League (NFL) players. Drug Alcohol Depend. (2011) 116:188–94. doi: 10.1016/j.drugalcdep.2010.12.003
67. Banks SM, Kerns RD. Explaining high rates of depression in chronic pain: a diathesis-stress framework. Psychol Bull. (1996) 119:95–110. doi: 10.1037/0033-2909.119.1.95
68. Atkinson JH, Slater MA, Patterson TL, Grant I, Garfin SR. Prevalence, onset, and risk of psychiatric disorders in men with chronic low back pain: a controlled study. Pain. (1991) 45:111–21. doi: 10.1016/0304-3959(91)90175-W
69. Fishbain DA, Cutler R, Rosomoff HL, Rosomoff RS. Chronic pain-associated depression: antecedent or consequence of chronic pain? A review. Clin J Pain. (1997) 13:116–37. doi: 10.1097/00002508-199706000-00006
70. Wilson KG, Eriksson MY, D'Eon JL, Mikail SF, Emery PC. Major depression and insomnia in chronic pain. Clin J Pain. (2002) 18:77–83. doi: 10.1097/00002508-200203000-00002
71. Campbell LC, Clauw DJ, Keefe FJ. Persistent pain and depression: a biopsychosocial perspective. Biol Psychiatry. (2003) 54:399–409. doi: 10.1016/S0006-3223(03)00545-6
72. McWilliams LA, Cox BJ, Enns MW. Mood and anxiety disorders associated with chronic pain: an examination in a nationally representative sample. Pain. (2003) 106:127–33. doi: 10.1016/S0304-3959(03)00301-4
73. Ilgen MA, Zivin K, McCammon RJ, Valenstein M. Pain and suicidal thoughts, plans and attempts in the United States. Gen Hosp Psychiatry. (2008) 30:521–7. doi: 10.1016/j.genhosppsych.2008.09.003
74. Tang NK, Crane C. Suicidality in chronic pain: a review of the prevalence, risk factors and psychological links. Psychol Med. (2006) 36:575–86. doi: 10.1017/S0033291705006859
75. Turner RW 2nd, Sonnega A, Cupery T, Chodosh J, Whitfield KE, Weir D, et al. Functional limitations mediate the relationship between pain and depressive symptoms in former NFL athletes. Am J Mens Health. (2019) 13:1557988319876825. doi: 10.1177/1557988319876825
76. Stonnington CM, Kothari DJ, Davis MC. Understanding and promoting resiliency in patients with chronic headache. Curr Neurol Neurosci Rep. (2016) 16:6. doi: 10.1007/s11910-015-0609-2
77. Sturgeon JA, Zautra AJ. Psychological resilience, pain catastrophizing, and positive emotions: perspectives on comprehensive modeling of individual pain adaptation. Curr Pain Headache Rep. (2013) 17:317. doi: 10.1007/s11916-012-0317-4
78. Ramirez-Maestre C, Esteve R. Disposition and adjustment to chronic pain. Curr Pain Headache Rep. (2013) 17:312. doi: 10.1007/s11916-012-0312-9
79. Waugh CE, Koster EH. A resilience framework for promoting stable remission from depression. Clin Psychol Rev. (2015) 41:49–60. doi: 10.1016/j.cpr.2014.05.004
80. Southwick SM, Vythilingam M, Charney DS. The psychobiology of depression and resilience to stress: implications for prevention and treatment. Annu Rev Clin Psychol. (2005) 1:255–91. doi: 10.1146/annurev.clinpsy.1.102803.143948
81. Wagnild GM, Young HM. Development and psychometric evaluation of the Resilience Scale. J Nurs Meas. (1993) 1:165–78.
82. Mak WW, Ng IS, Wong CC. Resilience: enhancing well-being through the positive cognitive triad. J Couns Psychol. (2011) 58:610–7. doi: 10.1037/a0025195
83. Tugade MM, Fredrickson BL. Resilient individuals use positive emotions to bounce back from negative emotional experiences. J Pers Soc Psychol. (2004) 86:320–33. doi: 10.1037/0022-3514.86.2.320
84. Wermelinger Avila MP, Lucchetti AL, Lucchetti G. Association between depression and resilience in older adults: a systematic review and meta-analysis. Int J Geriatr Psychiatry. (2017) 32:237–46. doi: 10.1002/gps.4619
85. Laird KT, Lavretsky H, Paholpak P, Vlasova RM, Roman M, St Cyr N, et al. Clinical correlates of resilience factors in geriatric depression. Int Psychogeriatr. (2019) 31:193–202. doi: 10.1017/S1041610217002873
86. Laird KT, Lavretsky H, St Cyr N, Siddarth P. Resilience predicts remission in antidepressant treatment of geriatric depression. Int J Geriatr Psychiatry. (2018) 33:1596–603. doi: 10.1002/gps.4953
87. Wright DK, Gardner AJ, Wojtowicz M, Iverson GL, O'Brien TJ, Shultz SR, et al. White matter abnormalities in retired professional Rugby League Players with a history of concussion. J Neurotrauma. (2020). doi: 10.1089/neu.2019.6886
88. Wojtowicz M, Gardner AJ, Stanwell P, Zafonte R, Dickerson BC, Iverson GL. Cortical thickness and subcortical brain volumes in professional rugby league players. Neuroimage Clin. (2018) 18:377–81. doi: 10.1016/j.nicl.2018.01.005
89. Gardner AJ, Iverson GL, Wojtowicz M, Levi CR, Kay-Lambkin F, Schofield PW, et al. MR spectroscopy findings in retired professional Rugby League players. Int J Sports Med. (2017) 38:241–52. doi: 10.1055/s-0042-120843
90. Guell X, Arnold Anteraper S, Gardner AJ, Whitfield-Gabrieli S, Kay-Lambkin F, Iverson GL, et al. Functional connectivity changes in retired Rugby League players: a data-driven functional magnetic resonance imaging study. J Neurotrauma. (2020) 37:1788–96. doi: 10.1089/neu.2019.6782
91. King D, Hume AP, Clark T. Video analysis of tackles in professional rugby league matches by player position, tackle height and tackle location. Int J Performance Anal Sport. (2010) 10:241–54. doi: 10.1080/24748668.2010.11868519
92. Gardner AJ, Howell DR, Levi CR, Iverson GL. Evidence of concussion signs in National Rugby League match play: a video review and validation study. Sports Med Open. (2017) 3:29. doi: 10.1186/s40798-017-0097-9
93. Gardner A, Iverson GL, Levi CR, Schofield PW, Kay-Lambkin F, Kohler RM, et al. A systematic review of concussion in rugby league. Br J Sports Med. (2015) 49:495–8. doi: 10.1136/bjsports-2013-093102
94. McCrory P, Meeuwisse WH, Aubry M, Cantu B, Dvorak J, Echemendia RJ, et al. Consensus statement on concussion in sport: the 4th International Conference on Concussion in Sport held in Zurich, November 2012. Br J Sports Med. (2013) 47:250–8. doi: 10.1136/bjsports-2013-092313
95. Antony MM, Bieling PJ, Cox BJ, Enns MW, Swinson RP. Psychometric properties of the 42-item and 21-item versions of the Depression Anxiety Stress Scales in clinical groups and a community sample. Psychol Assess. (1998) 10:176. doi: 10.1037/1040-3590.10.2.176
96. Lovibond PF, Lovibond SH. The structure of negative emotional states: comparison of the Depression Anxiety Stress Scales (DASS) with the Beck Depression and Anxiety Inventories. Behav Res Ther. (1995) 33:335–43. doi: 10.1016/0005-7967(94)00075-U
97. Lovibond SH, Lovibond PF. Manual for the Depression Anxiety Stress Scales. Sydney, NSW: Psychology Foundation (1995).
98. Connor KM, Davidson JR. Development of a new resilience scale: the Connor-Davidson Resilience Scale (CD-RISC). Depress Anxiety. (2003) 18:76–82. doi: 10.1002/da.10113
99. Johns MW. A new method for measuring daytime sleepiness: the Epworth sleepiness scale. Sleep. (1991) 14:540–5. doi: 10.1093/sleep/14.6.540
100. Johns MW. Reliability and factor analysis of the Epworth Sleepiness Scale. Sleep. (1992) 15:376–81. doi: 10.1093/sleep/15.4.376
101. Gibson ES, Powles AC, Thabane L, O'Brien S, Molnar DS, Trajanovic N, et al. “Sleepiness” is serious in adolescence: two surveys of 3235 Canadian students. BMC Public Health. (2006) 6:116. doi: 10.1186/1471-2458-6-116
102. Cleeland CS, Ryan KM. Pain assessment: global use of the Brief Pain Inventory. Ann Acad Med Singapore. (1994) 23:129–38.
103. Nicholas MK, Costa DSJ, Blanchard M, Tardif H, Asghari A, Blyth FM. Normative data for common pain measures in chronic pain clinic populations: closing a gap for clinicians and researchers. Pain. (2019) 160:1156–65. doi: 10.1097/j.pain.0000000000001496
104. Cleeland CS. The Brief Pain Inventory User Guide. Houston, TX: The University of Texas MD Anderson Cancer Center (2009).
105. Saunders JB, Aasland OG, Babor TF, de la Fuente JR, Grant M. Development of the Alcohol Use Disorders Identification Test (AUDIT): WHO collaborative project on early detection of persons with harmful alcohol consumption–II. Addiction. (1993) 88:791–804. doi: 10.1111/j.1360-0443.1993.tb02093.x
106. Babor TF, de la Fuente JR, Saunders J, Grant M. AUDIT. The Alcohol Use Disorders Identification Test. Guidelines for Use in Primary Health Care. Geneva: World Health Organization (1992).
107. de Meneses-Gaya C, Zuardi AW, Loureiro SR, Crippa JAS. Alcohol Use Disorders Identification Test (AUDIT): an updated systematic review of psychometric properties. Psychol Neurosci. (2009) 2:83–97. doi: 10.3922/j.psns.2009.1.12
108. Benjamini Y, Hochberg Y. Controlling the false discovery rate: a practical and powerful approach to multiple testing. J R Stat Soc Ser B. (1995) 57:289–300. doi: 10.1111/j.2517-6161.1995.tb02031.x
109. Park S, Lavallee D, Tod D. Athletes' career transition out of sport: a systematic review. Int Rev Sport Exer Psychol. (2013) 6:22–53. doi: 10.1080/1750984X.2012.687053
110. Demetriou A, Jago A, Gill PR, Mesagno C, Ali L. Forced retirement transition: a narrative case study of an elite Australian Rules football player. Int J Sport Exerc Psychol. (2020) 18:321–35. doi: 10.1080/1612197X.2018.1519839
111. Carless D, Douglas K. ‘We haven't got a seat on the bus for you' or ‘all the seats are mine': narratives and career transition in professional golf. Qual Res Sport Exerc. (2009) 1:51–66. doi: 10.1080/19398440802567949
112. McGillivray D, Fearn R, McIntosh A. Caught up in and by the beautiful game: a case study of Scottish professional footballers. J Sport Soc Issues. (2005) 29:102–23. doi: 10.1177/0193723504268730
113. Gaetz M. The multi-factorial origins of Chronic Traumatic Encephalopathy (CTE) symptomology in post-career athletes: the athlete post-career adjustment (AP-CA) model. Med Hypotheses. (2017) 102:130–43. doi: 10.1016/j.mehy.2017.03.023
114. Martin LA, Fogarty GJ, Albion MJ. Changes in athletic identity and life satisfaction of elite athletes as a function of retirement status. J Appl Sport Psychol. (2014) 26:96–110. doi: 10.1080/10413200.2013.798371
115. Russell ER, McCabe T, Mackay DF, Stewart K, MacLean JA, Pell JP, et al. Mental health and suicide in former professional soccer players. J Neurol Neurosurg Psychiatry. (2020) 91:1256–60. doi: 10.1136/jnnp-2020-323315
116. Turner AP, Barlow JH, Heathcote-Elliott C. Long term health impact of playing professional football in the United Kingdom. Br J Sports Med. (2000) 34:332–6. doi: 10.1136/bjsm.34.5.332
117. Didehbani N, Munro Cullum C, Mansinghani S, Conover H, Hart J Jr. Depressive symptoms and concussions in aging retired NFL players. Arch Clin Neuropsychol. (2013) 28:418–24. doi: 10.1093/arclin/act028
118. Kerr ZY, DeFreese JD, Marshall SW. Current physical and mental health of former collegiate athletes. Orthop J Sports Med. (2014) 2:2325967114544107. doi: 10.1177/2325967114544107
Keywords: retired athletes, sports, brain concussion, brain injury, depression, mental health
Citation: Iverson GL, Van Patten R, Terry DP, Levi CR and Gardner AJ (2021) Predictors and Correlates of Depression in Retired Elite Level Rugby League Players. Front. Neurol. 12:655746. doi: 10.3389/fneur.2021.655746
Received: 19 January 2021; Accepted: 10 March 2021;
Published: 01 April 2021.
Edited by:
Antonio Belli, University of Birmingham, United KingdomReviewed by:
Joseph Bleiberg, Independent Researcher, Bethesda, United StatesKimbra Kenney, Uniformed Services University of the Health Sciences, United States
Copyright © 2021 Iverson, Van Patten, Terry, Levi and Gardner. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Andrew J. Gardner, QW5kcmV3LkdhcmRuZXJAbmV3Y2FzdGxlLmVkdS5hdQ==
 Grant L. Iverson
Grant L. Iverson Ryan Van Patten
Ryan Van Patten Douglas P. Terry1,2,4,5
Douglas P. Terry1,2,4,5 Andrew J. Gardner
Andrew J. Gardner