- 1Department of Rehabilitation Medicine, The Jikei University School of Medicine, Tokyo, Japan
- 2Department of Rehabilitation Medicine, Nishi-Hiroshima Rehabilitation Hospital, Hiroshima, Japan
- 3Department of Rehabilitation Medicine, Kawakita Rehabilitation Hospital, Tokyo, Japan
In Japan, the national medical insurance system and long-term care insurance (LTCI) system cover rehabilitation therapy for patients with acute, convalescent, and chronic stroke. Medical insurance covers early and multidisciplinary rehabilitation therapy during acute phase hospitalizations. Patients requiring assistance in their activities of daily living (ADL) after hospitalization are transferred to kaifukuki (convalescent) rehabilitation wards (KRW), which the medical insurance system has also covered. In these wards, patients can receive intensive and multidisciplinary rehabilitation therapy to improve their ADL and transition to a smooth home discharge. After discharge from these hospitals, elderly patients with stroke can receive outpatient (day-care) rehabilitation and home-based rehabilitation using the LTCI system. The Japanese government has proposed building a community-based integrated care system by 2025 to provide comprehensive medical services, long-term care, preventive care, housing, and livelihood support for patients. This policy aims to promote smooth coordination between medical insurance services and LTCI providers. Accordingly, the medical insurance system allows hospitals to receive additional fees by providing patient information to rehabilitation service providers in the LTCI system. A comprehensive database on acute, convalescent, and chronic phase stroke patients and seamless cooperation between the medical care system and LTCI system is expected to be established in the future. There are only 2,613 board-certified physiatrists in Japan, and many medical schools lack a department for rehabilitation medicine; establishing such a department at each school is encouraged to teach students efficient medical care procedures, to conduct research, and to facilitate the training of personnel in comprehensive stroke rehabilitation.
Introduction
Historically, stroke has been the number one cause of death among Japanese people, but has shifted to the fourth most common cause in recent years due to decreasing mortality rates, with cancer as the first, heart disease second, and senility third. These numbers reflect fewer deaths due to improved emergency medical services and advances in treatment methods, such as the use of recombinant tissue-type plasminogen activators (rt-PA) and mechanical thrombectomy. However, the overall number of patients with stroke remains high. In Japan, ~220,000 people experience a new stroke and ~290,000 people have recurring strokes annually (1). Endovascular treatment or neurosurgery is administered to 9.1% of patients, and 73% of patients receive rehabilitation. Another characteristic of stroke is that the number of patients affected increases with age. According to the 2019 surveys from the Ministry of Health, Labor, and Welfare, cerebrovascular disease accounted for 16.1% of primary causes, requiring long-term care (2). These diseases are serious problems for public life and health, despite being preventable, to a certain extent, through lifestyle improvements.
The clinical importance of rehabilitation therapy for patients with stroke is well-established. Rehabilitation must be provided in a timely and appropriate manner during acute, convalescent, and chronic phases. It is also important to transition seamlessly between the treatments for each phase to improve and maintain the function of patients with stroke. In Japan, the national medical insurance system and long-term care insurance (LTCI) system were established to provide rehabilitation services for patients with stroke (Figure 1). In fact, Japan's insurance system is unique. Furthermore, the length of hospital stay for patients with acute stroke in Japan is longer than in other countries, and medical costs are higher. It would be useful to introduce the transitional and long-term care system for rehabilitation of patients with stroke in Japan, where the population is aging to consider the adequate transitional and long-term care strategies after stroke in different health care systems.
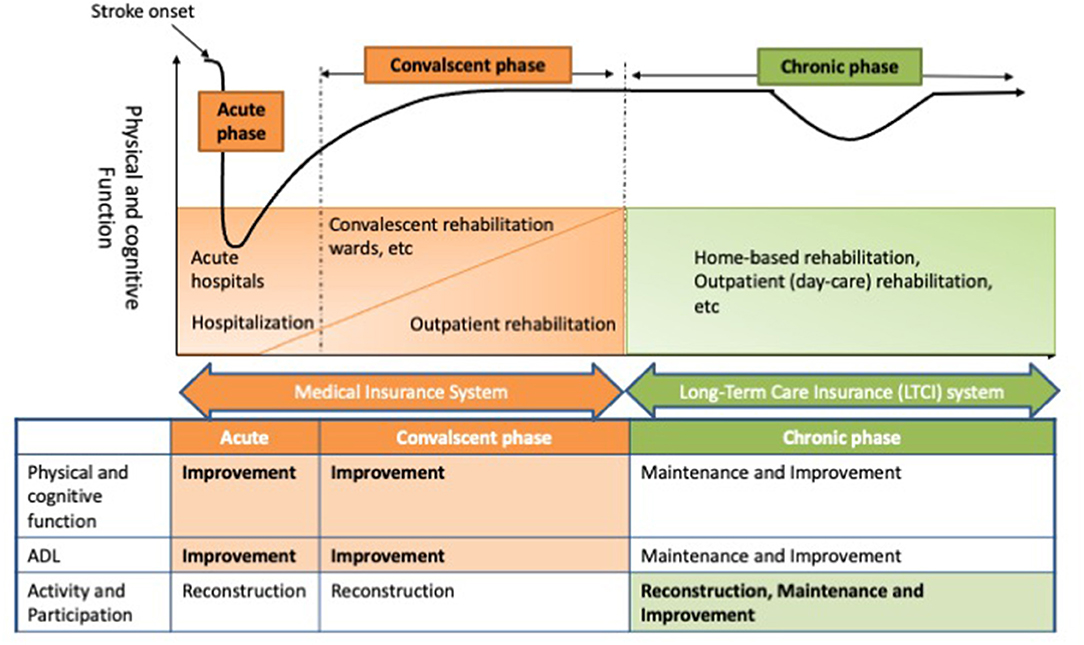
Figure 1. Transitional and long-term care system for rehabilitation of patients with stroke in Japan. In Japan, the medical insurance system covers rehabilitation services for stroke patients in acute and convalescent phases, while the long-term care insurance (LTCI) system covers chronic phase rehabilitation services. In the acute and convalescent phases, the main purpose of rehabilitation is to improve functional recovery and activities of daily living (ADL) of patients with stroke. In the chronic phase, the main aim of rehabilitation services is to maintain physical and cognitive functions and ADL, while improving the engagement of patients with stroke.
The purpose of this mini-review is to outline the transitional and long-term care system in Japan and the current challenges for the rehabilitation of patients with stroke at each phase.
Acute Phase
The main purpose of acute rehabilitation treatment for stroke is to prevent complications associated with immobility, to prevent systemic complications, and to promote functional reorganization of the brain. For this reason, mobilization, basic movement training, gait training, and activities of daily living (ADL) training are implemented as early rehabilitation. In Japan, in recent years, the importance of early rehabilitation for the treatment of acute stroke has been increasingly recognized, and its practice has become widespread. Evidence for these treatments is being collected, which leads to improved knowledge about early rehabilitation therapy (3). In observational studies from Japan (4, 5), very early mobilization was associated with functional recovery of patients with stroke. Initiating rehabilitative care within 24 h of stroke is safe and useful if provided by skilled therapists under physiatrist supervision. Using the Japanese Diagnosis Procedure Combination database, a cohort study analyzed 100,719 consecutive patients with ischemic stroke (6). Their results suggested that early and intensive rehabilitation improved patient ADL during hospitalization. Another study using the Diagnosis Procedure Combination database analyzed 4,266 patients with acute stroke who received intravenous thrombolysis using rt-PA (7). The results showed that a good prognosis at discharge was more likely in the group of patients who started rehabilitation treatment on the day of or after admission. In addition to timing (how early to start), the frequency (how often care is provided) is also important in early rehabilitation treatment (8). Using the Japan Rehabilitation Database, a cohort study of 8,033 patients with the acute cerebrovascular disease showed that high-frequency rehabilitation care (7 days a week for patients with early-onset acute stroke) was associated with better functional recovery (9). In fact, in most cases, rehabilitation was started the day after the onset of symptoms. The percentage of patients receiving rehabilitation 7 days a week was 35.%. The average length of rehabilitation provided per day was 76.7 min. In addition, the average length of stay in the hospital was 29.5 days (10). Based on these results, the medical insurance system can facilitate early rehabilitation therapy for patients with acute stroke in hospitals. Hospitals can charge an additional fee if they provide rehabilitation earlier in the course of the disease. The medical insurance system also assigns rehabilitation staff to intensive care units.
For acute rehabilitation, multidisciplinary cooperation is important for the functional recovery of patients with stroke. For example, early assessment of swallowing function after the stroke onset helps prevent aspiration pneumonia and to promote early oral intake (11). Aoki et al. (12) reported that the activities of a multidisciplinary swallowing team, consisting of nurses, speech therapists, occupational therapists, audiologists, dieticians, dental hygienists, and pharmacists, reduced the incidence of pneumonia in patients with acute cerebrovascular disease. Such a multidisciplinary team, facilitated by the medical insurance system, should be able to assess and manage swallowing function during the acute stroke phase.
Convalescent Phase
After acute hospitalization, patients who require ADL assistance are transferred to the kaifukuki (convalescent) rehabilitation wards (KRW), which have been covered by the medical insurance system since 2000 (13, 14). Patients with disabling conditions, including stroke, traumatic brain injury, and other neurological diseases, as well as orthopedic diseases, such as hip fractures, are eligible for KRW admission. Under the health insurance system in Japan, rehabilitation therapy (physical, occupational, and speech therapy) is limited to 3 h per day, and the maximum length of stay for patients with stroke in the KRW is limited to 150 days. When rehabilitation goals are met and home or institutional care services are available, the physiatrist can decide to discharge a patient from the KRW. The basic hospitalization fee for the KRW stay is based on the number of medical staff, the provision of rehabilitation on holidays, the percentage of seriously ill patients, the home discharge rate, and motor Functional Independence Measure (FIM) efficiency adjusted by the length of the hospital stay.
The KRW association annual survey reported almost 85,000 KRW beds in 1,500 hospitals in 2019 (15), with an average patient stay length of 67.5 days. The mean patient age was 76.6 years, and 57.8% of patients were female. Stroke was the cause of 36.9% of cases in the KRW. The average time from the stroke onset to the admission to the KRW was 24.2 days. An average of 137.4 min of rehabilitation therapy was provided per day. When the ADL gain of patients with stroke was analyzed in terms of the change in FIM between admission and discharge, the average FIM was determined to be 61.5 points at admission and 84.6 points at discharge, with an average FIM improvement of 23.1 points. Of these, 60.6% of patients were discharged to their homes.
A variety of cutting-edge rehabilitation therapies have been developed and practiced in the KRW. According to a cohort study analyzing 2,325 patients (16), intensive rehabilitation therapy, defined as rehabilitation therapy for more than 15 h per week,was provided for 862 patients (37.1%). Intensive rehabilitation therapy was significantly associated with increased functional gain in elderly patients with stroke in the KRW. Regarding the collaboration between acute care and convalescent rehabilitation, a shorter interval between the stroke onset and admission to the KRW contributes to improved outcomes in patients with ischemic stroke, including ADL, dysphagia, and home discharge rate (17). Prognostic predictions based on a large database have been developed to assess outcomes of patients with stroke (18, 19). Multidisciplinary collaboration from the International Classification of Functioning, Disability, and Health is also practiced according to patient assessment and information sharing (20, 21). Furthermore, innovative rehabilitation using advanced technology, such as robotics, is also becoming more widely developed and practiced (22). Therefore, IRT, collaborations between acute and chronic phase rehabilitation practices, and rehabilitation using innovative techniques are being developed and conducted in KRWs to improve the function of patients with stroke.
Chronic Phase
Japan has an unprecedented aging population that affects health and long-term care systems. The LTCI system was introduced in Japan in 2000 to address the demands of older people with disabilities based on a user-oriented social insurance system supporting independence (23). Older people with certified LTCI service needs can utilize facility services, in-home services, and community-based services. Following its implementation, the mean length of stay for patients with stroke in rehabilitation hospitals decreased (24). Furthermore, the Japanese government proposed establishing a community-based integrated care system by 2025 to comprehensively provide health care, nursing care, preventive care, housing, and livelihood support for patients (25). This national policy promotes the smooth coordination between medical insurance services and LTCI providers.
There are two main types of rehabilitation services in the LTCI system: home-based rehabilitation and outpatient (day-care) rehabilitation (26, 27). Home-based rehabilitation is provided by rehabilitation staff who visit patient homes. In 2019, there were ~4,600 facilities and 115,000 recipients for home-based rehabilitation (28). Forty min a day, two times a week is a typical service provision for home-based rehabilitation. During outpatient (day-care) rehabilitation, nursing care services, such as meals and bathing, are provided along with hospital-based rehabilitation. In 2019, there were ~8,000 facilities and 600,000 recipients for outpatient (day-care) rehabilitation (29). The outpatient (day-care) rehabilitation is generally provided one time or two times a week for 6–7 h each time. In outpatient (day-care) rehabilitation, rehabilitation to improve physical functions, such as muscle strength training and gait training, is often conducted.
To use LTCI services, a person must be certified as needing long-term care based on their physical and cognitive functions, as well as the status of their nursing care and medical treatment. For certified patients, the system requires that they use LTCI rehabilitation services instead of medical insurance, except when they are hospitalized or in the early stages of their illness. In addition, the medical insurance also covers the outpatient rehabilitation for younger patients with stroke and elderly patients who were not certified as needing long-term care in the chronic phase. Among rehabilitation services after returning home from the KRW, outpatient rehabilitation through medical insurance, outpatient (day-care) rehabilitation through LTCI, and home-based rehabilitation through LTCI each account for ~10% of discharged patients (15).
In the LTCI system, using information and communication technology devices to collaborate with other professions is encouraged. If service providers provide information from medical insurance service centers to LTCI rehabilitation centers, they can charge an additional fee for linking the information using information and communication technology. Furthermore, holding conferences with other professionals within LTCI rehabilitation services is recommended, which also would allow the use of these technologies, such as video teleconferencing systems.
Scientific evidence is necessary to promote high-quality long-term care services. Therefore, the Japanese Ministry of Health, Labor, and Welfare launched a database for LTCI services, the Long-Term Care Information System for Evidence (LIFE), in April 2021. This database stores information on diseases, physical and cognitive functions, rehabilitation goals and interventions, ADL, instrumental ADL, and nutritional status. The purpose of this database is to provide feedback for users and facilities, as well as promote high-quality evidence-based services. Furthermore, by using the LIFE database, service providers can charge another additional fee within the LTCI system. Data from the LIFE database could allow the establishment of evidence for higher quality rehabilitation services for elderly patients, who also suffer from stroke. Although it is possible to link the National Database of medical claims data with the LIFE database in the LTCI system (30), there are no unified outcome measures for rehabilitation with medical insurance and LTCI. Moreover, since there are no standardized codes for individual rehabilitation interventions, it is difficult to clarify effective rehabilitation methods using a database. We hope comprehensive and standardized intervention methods and outcome measures are established for acute, convalescent, and chronic stroke phases.
Future Perspective
“The Cerebrovascular and Cardiovascular Disease Control Act” was enacted in December 2019 to control national cerebrovascular diseases. “The Japanese National Plan for Promotion of Cardiovascular Disease Control” based on this law set out three goals: prevention of cerebrovascular diseases and dissemination of correct knowledge; improvement of the service delivery system for health, medical care, and welfare; and promotion of research on cerebrovascular diseases (31, 32). By achieving these three goals, the basic plan thus aims to extend healthy life expectancy by 3 or more years and reduce the age-adjusted mortality rate for cerebrovascular diseases by 2040, which is when the elderly population in Japan will reach its peak. This law and basic plan state that coordination between the treatments for acute, convalescent, and chronic phases is important, and that appropriate services related to medical care, nursing care, and welfare should be provided. Since these require governments and prefectures to promote the control of cerebrovascular diseases, it is expected that the transitional and long-term care systems for stroke rehabilitation will be further developed.
Providing appropriate rehabilitation for patients with stroke requires active physiatrist participation. Physiatrists are usually involved in the clinical management of a multidisciplinary rehabilitation team that consists of nurses, physical therapists, occupational therapists, speech therapists, and medical social workers (33). The physiatrist is expected to implement the management of patients with stroke as a leader of the rehabilitation team. Board-certificated physiatrists with sufficient knowledge and experience about stroke rehabilitation are recommended to be the primary care providers for patients with stroke. A retrospective cohort study with the Japan Rehabilitation Database identified that the clinical management provided by board-certified physiatrists in the form of early rehabilitation for patients with acute and convalescent stroke is a significant predictor of a good functional prognosis (10, 34). In Japan, however, stroke rehabilitation is not always provided by a board-certified physiatrist. At some hospitals or facilities, physicians with other specialties lead the rehabilitation team. This is, in part, due to a shortage in the number of board-certified physiatrists. There were only 2,613 in 2021, and many medical schools lack a department for rehabilitation medicine. Establishing such a department in each medical school would help teach students medicine and efficient medical care, enable research, and facilitate the training of personnel in comprehensive stroke rehabilitation.
Innovative neurorehabilitation techniques, such as non-invasive brain stimulation, are effective in functional recovery, primarily in patients with chronic stroke. Our group developed a combined protocol using repetitive transcranial magnetic stimulation (rTMS) and IRT that can effectively improve the function of patients with chronic stroke (35). This protocol is now being implemented in many facilities throughout Japan (36). Although the efficacy of non-invasive brain stimulation for patients with stroke in the acute and convalescent phases is controversial, it may be possible to perform it effectively according to brain condition, such as in the case of interhemispheric inhibition, by using functional brain imaging (37–39). We hope non-invasive brain stimulation and other neurorehabilitation techniques will become more widely implemented in the rehabilitation of patients with stroke for acute and convalescent phases.
Author Contributions
SK designed concept, drafted the manuscript with important intellectual input from TO and KM, and takes responsibility for whole work from inception to published article. MA provided technical and administrative support and critically assessed the manuscript. All authors have read and approved the final version of the submitted paper.
Conflict of Interest
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
Publisher's Note
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
Acknowledgments
We express our deepest gratitude to the staff of the Department of Rehabilitation Medicine at the Jikei University School of Medicine. We would like to thank Uni-edit (https://uni-edit.net/) for editing and proofreading this manuscript.
References
1. Takashima N, Arima H, Kita Y, Fujii T, Miyamatsu N, Komori M, et al. Incidence, management and short-term outcome of stroke in a general population of 14 million Japanese-Shiga Stroke Registry. Circ J. (2017) 81:1636–46. doi: 10.1253/circj.CJ-17-0177
2. Ministry of Health, Labour, andx1 Welfare. National Survey on Basic Living Conditions in 2019. (2019). Available online at: https://www.mhlw.go.jp/toukei/saikin/hw/k-tyosa/k-tyosa19/index.html (accessed April 3, 2021).
3. AVERT Trial Collaboration group. Efficacy and safety of very early mobilisation within 24 h of stroke onset (AVERT): a randomised controlled trial. Lancet. (2015) 386:46–55. doi: 10.1016/S0140-6736(15)60690-0
4. Kinoshita T, Nishimura Y, Nakamura T, Hashizaki T, Kojima D, Kawanishi M, et al. Effects of physiatrist and registered therapist operating acute rehabilitation (PROr) in patients with stroke. PLoS ONE. (2017) 12:e0187099. doi: 10.1371/journal.pone.0187099
5. Kinoshita T, Yoshikawa T, Nishimura Y, Kamijo Y, Arakawa H, Nakamura T, et al. Mobilization within 24 hours of new-onset stroke enhances the rate of home discharge at 6-months follow-up: a prospective cohort study. Int J Neurosci. (2020) 22:1–10. doi: 10.1080/00207454.2020.1774578
6. Yagi M, Yasunaga H, Matsui H, Morita K, Fushimi K, Fujimoto M, et al. Impact of rehabilitation on outcomes in patients with ischemic stroke: a nationwide retrospective cohort study in Japan. Stroke. (2017) 48:740–6. doi: 10.1161/STROKEAHA.116.015147
7. Momosaki R, Yasunaga H, Kakuda W, Matsui H, Fushimi K, Abo M. Very early versus delayed rehabilitation for acute ischemic stroke patients with intravenous recombinant tissue plasminogen activator: a nationwide retrospective cohort study. Cerebrovasc Dis. (2016) 42:41–8. doi: 10.1159/000444720
8. Bernhardt J, Churilov L, Ellery F, Collier J, Chamberlain J, Langhorne P, et al. Prespecified dose-response analysis for A Very Early Rehabilitation Trial (AVERT). Neurology. (2016) 86:2138–45. doi: 10.1212/WNL.0000000000002459
9. Kinoshita S, Momosaki R, Kakuda W, Okamoto T, Abo M. Association between 7 days per week rehabilitation and functional recovery of patients with acute stroke: a retrospective cohort study based on the Japan Rehabilitation Database. Arch Phys Med Rehabil. (2017) 98:701–6. doi: 10.1016/j.apmr.2016.11.004
10. Kinoshita S, Kakuda W, Momosaki R, Yamada N, Sugawara H, Watanabe S, et al. Clinical management provided by board-certificated physiatrists in early rehabilitation is a significant determinant of functional improvement in acute stroke patients: a retrospective analysis of Japan rehabilitation database. J Stroke Cerebrovasc Dis. (2015) 24:1019–24. doi: 10.1016/j.jstrokecerebrovasdis.2014.12.026
11. Momosaki R, Abo M, Kakuda W, Kobayashi K. Applicability of the two-step thickened water test in patients with poststroke dysphagia: a novel assessment tool for paste food aspiration. J Stroke Cerebrovasc Dis. (2013) 22:817–21. doi: 10.1016/j.jstrokecerebrovasdis.2012.05.011
12. Aoki S, Hosomi N, Hirayama J, Nakamori M, Yoshikawa M, Nezu T, et al. The multidisciplinary swallowing team approach decreases pneumonia onset in acute stroke patients. PLoS ONE. (2016) 11:e0154608. doi: 10.1371/journal.pone.0154608
13. Miyai I, Sonoda S, Nagai S, Takayama Y, Inoue Y, Kakehi A, et al. Results of new policies for inpatient rehabilitation coverage in Japan. Neurorehabil Neural Repair. (2011) 25:540–7. doi: 10.1177/1545968311402696
14. Okamoto T, Ando S, Sonoda S, Miyai I, Ishikawa M. “Kaifukuki Rehabilitation Ward” in Japan. Jpn J Rehabil Med. (2014) 51:629–33. doi: 10.2490/jjrmc.51.629
15. Kaifukuki Rehabilitation Ward Association. Annual Survey. (2019). Available online at: http://www.rehabili.jp/publications/download.html (accessed April 14, 2021).
16. Kamo T, Momosaki R, Suzuki K, Asahi R, Azami M, Ogihara H, et al. Effectiveness of intensive rehabilitation therapy on functional outcomes after stroke: a propensity score analysis based on Japan Rehabilitation Database. J Stroke Cerebrovasc Dis. (2019) 28:2537–42. doi: 10.1016/j.jstrokecerebrovasdis.2019.06.007
17. Yoshimura Y, Wakabayashi H, Momosaki R, Nagano F, Shimazu S, Shiraishi A. Shorter interval between onset and admission to convalescent rehabilitation wards is associated with improved outcomes in ischemic stroke patients. Tohoku J Exp Med. (2020) 252:15–22. doi: 10.1620/tjem.252.15
18. Kinoshita S, Abo M, Okamoto T. Tanaka N. Utility of the revised version of the ability for basic movement scale in predicting ambulation during rehabilitation in poststroke patients. J Stroke Cerebrovasc Dis. (2017) 26:1663–9. doi: 10.1016/j.jstrokecerebrovasdis.2017.02.021
19. Yang G, Gu R, Sato S, Zheng F, Sano M, Yashima C, et al. The ability for basic movement scale ii can predict functional outcome and discharge destination in stroke patients. J Stroke Cerebrovasc Dis. (2020) 29:104484. doi: 10.1016/j.jstrokecerebrovasdis.2019.104484
20. Kinoshita S, Abo M, Okamoto T, Kakuda W, Miyamura K, Kimura I. Responsiveness of the functioning and disability parts of the International Classification of Functioning, Disability, and Health core sets in postacute stroke patients. Int J Rehabil Res. (2017) 40:246–53. doi: 10.1097/MRR.0000000000000235
21. Kinoshita S, Abo M, Okamoto T. Effectiveness of ICF-based multidisciplinary rehabilitation approach with serial assessment and discussion using the ICF rehabilitation set in a convalescent rehabilitation ward. Int J Rehabil Res. (2020) 43:255–60. doi: 10.1097/MRR.0000000000000421
22. Tanaka N, Matsushita S, Sonoda Y, Maruta Y, Fujitaka Y, Sato M, et al. Effect of stride management assist gait training for poststroke hemiplegia: a single center, open-label, randomized controlled trial. J Stroke Cerebrovasc Dis. (2019) 28:477–86. doi: 10.1016/j.jstrokecerebrovasdis.2018.10.025
23. Yamada M, Arai H. Long-term care system in Japan. Ann Geriatr Med Res. (2020) 24:174–80. doi: 10.4235/agmr.20.0037
24. Miyoshi Y, Teraoka JK, Date ES, Kim MJ, Nguyen RT, Miyoshi S. Changes in stroke rehabilitation outcomes after the implementation of Japan's long-term care insurance system: a hospital-based study. Am J Phys Med Rehabil. (2005) 84:613–9. doi: 10.1097/01.phm.0000171007.76831.01
25. Song P, Tang W. The community-based integrated care system in Japan: health care and nursing care challenges posed by super-aged society. Biosci Trends. (2019) 13:279–81. doi: 10.5582/bst.2019.01173
26. Maruta M, Tabira T, Makizako H, Sagari A, Miyata H, Yoshimitsu K, et al. Impact of outpatient rehabilitation service in preventing the deterioration of the care-needs level among Japanese older adults availing long-term care insurance: a propensity score matched retrospective study. Int J Environ Res Public Health. (2019) 16:1292. doi: 10.3390/ijerph16071292
27. Tsuchiya-Ito R, Ishizaki T, Mitsutake S, Hamada S, Yoshie S, Iijima K, et al. Association of household income with home-based rehabilitation and home help service utilization among long-term home care service users. BMC Geriatr. (2020) 20:314. doi: 10.1186/s12877-020-01704-7
28. Ministry of Health, Labour, and Welfare. 182th Social Security Council, Long-Term Care Benefit Fee Divisional Meeting, Home-Based Rehabilitation. (2020). Available online at: https://www.mhlw.go.jp/stf/newpage_13021.html (accessed April 13, 2021).
29. Ministry of Health, Labour, and Welfare. 180th Social Security Council, Long-Term Care Benefit Fee Divisional Meeting, Outpatient (Day-Care) Rehabilitation. (2020). Available online at: https://www.mhlw.go.jp/stf/newpage_12499.html (accessed April 13, 2021).
30. Mori T, Tamiya N, Jin X, Jeon B, Yoshie S, Iijima K, et al. Estimated expenditures for hip fractures using merged healthcare insurance data for individuals aged 75 years and long-term care insurance claims data in Japan. Arch Osteoporos. (2018) 13:37. doi: 10.1007/s11657-018-0448-2
31. Ministry Ministry of Health Labour Welfare. The Basic Plan for Controlling Cerebrovascular Diseases. (2020). Available online at: https://www.mhlw.go.jp/stf/newpage_14459.html (accessed May 17, 2021).
32. Kuwabara M, Mori M, Komoto S. Japanese National Plan for promotion of measures against cerebrovascular and cardiovascular disease. Circulation. (2021) 143:1929–31. doi: 10.1161/CIRCULATIONAHA.120.052737
33. Franceschini M, Caso V, Zampolini M, Negrini S, Giustini A. The role of the physiatrist in stroke rehabilitation: a European survey. Am J Phys Med Rehabil. (2009) 88:596–600. doi: 10.1097/PHM.0b013e3181aea225
34. Momosaki R, Kakuda W, Kinoshita S, Yamada N, Abo M. Clinical effectiveness of board-certificated physiatrists on functional recovery in elderly stroke patients during convalescence: a retrospective cohort study. Int J Gerontol. (2017) 1:7–11. doi: 10.1016/j.ijge.2016.05.005
35. Abo M, Kakuda W, Momosaki R, Harashima H, Kojima M, Watanabe S, et al. Randomized, multicenter, comparative study of NEURO versus CIMT in poststroke patients with upper limb hemiparesis: the NEURO-VERIFY Study. Int J Stroke. (2014) 9:607–12. doi: 10.1111/ijs.12100
36. Kakuda W, Abo M, Sasanuma J, Shimizu M, Okamoto T, Kimura C, et al. Combination protocol of low-frequency rTMS and intensive occupational therapy for post-stroke upper limb hemiparesis: a 6-year experience of more than 1,700 Japanese patients. Transl Stroke Res. (2016) 7:172–9. doi: 10.1007/s12975-016-0456-8
37. Tamashiro H, Kinoshita S, Okamoto T, Urushidani N, Abo M. Effect of baseline brain activity on response to low-frequency rTMS/intensive occupational therapy in poststroke patients with upper limb hemiparesis: a near-infrared spectroscopy study. Int J Neurosci. (2019) 129:337–43. doi: 10.1080/00207454.2018.1536053
38. Urushidani N, Kinoshita S, Okamoto T, Tamashiro H, Abo M. Low-Frequency rTMS and intensive occupational therapy improve upper limb motor function and cortical reorganization assessed by functional near-infrared spectroscopy in a subacute stroke patient. Case Rep Neurol. (2018) 10:223–31. doi: 10.1159/000492381
39. Kinoshita S, Tamashiro H, Okamoto T, Urushidani N, Abo M. Association between imbalance of cortical brain activity and successful motor recovery in sub-acute stroke patients with upper limb hemiparesis: a functional near-infrared spectroscopy study. Neuroreport. (2019) 30:822–7. doi: 10.1097/WNR.0000000000001283
Keywords: cerebrovascular disease, rehabilitation, long-term care insurance, acute phase, convalescent phase, chronic phase
Citation: Kinoshita S, Abo M, Okamoto T and Miyamura K (2022) Transitional and Long-Term Care System in Japan and Current Challenges for Stroke Patient Rehabilitation. Front. Neurol. 12:711470. doi: 10.3389/fneur.2021.711470
Received: 18 May 2021; Accepted: 09 December 2021;
Published: 11 January 2022.
Edited by:
Fenella Jane Kirkham, University College London, United KingdomReviewed by:
Yukio Mikami, Wakayama Medical University, JapanYukihide Nishimura, Iwate Medical University, Japan
Copyright © 2022 Kinoshita, Abo, Okamoto and Miyamura. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Shoji Kinoshita, a2lub3NoaXRhQGppa2VpLmFjLmpw
 Shoji Kinoshita
Shoji Kinoshita Masahiro Abo
Masahiro Abo Takatsugu Okamoto1,2
Takatsugu Okamoto1,2