- 1Physical Medicine and Rehabilitation Unit, Department of Neurosciences, ASST Carlo Poma, Mantova, Italy
- 2Physical and Rehabilitative Medicine, Department of Health Sciences, University of Eastern Piedmont, Novara, Italy
- 3Translational Medicine, Dipartimento Attività Integrate Ricerca e Innovazione (DAIRI), Azienda Ospedaliera SS. Antonio e Biagio e Cesare Arrigo, Alessandria, Italy
- 4Department of Medical and Surgical Sciences, University of Catanzaro “Magna Graecia”, Catanzaro, Italy
- 5Institute of Neurology, Department of Medical and Surgical Sciences, University of Catanzaro “Magna Graecia”, Catanzaro, Italy
- 6Department of Medical, Oral and Biotechnological Sciences, G. D'Annunzio University of Chieti-Pescara, Chieti, Italy
- 7Institute of Health Sciences, College of Medical Sciences of the University of Rzeszow, University of Rzeszow, Rzeszow, Poland
Multiple sclerosis (MS) is one of the most common causes of neurological progressive disease and can lead to loss of mobility, walk impairment, and balance disturbance. Among several rehabilitative approaches proposed, exergaming and virtual reality (VR) have been studied in the recent years. Active video game therapy could reduce the boredom of the rehabilitation process, increasing patient motivation, providing direct feedback, and enabling dual-task training. Aim of this systematic review was to assess the efficacy of exergaming and VR for balance recovery in patients with MS. PubMed, Scopus, and Web of Science were systematically searched from the inception until May 14, 2021 to identify randomized controlled trials (RCTs) presenting: patients with MS as participants, exergaming and VR as intervention, conventional rehabilitation as comparator, and balance assessment [Berg Balance Scale (BBS)] as outcome measure. We also performed a meta-analysis of the mean difference in the BBS via the random-effects method. Out of 93 records, this systematic review included and analyzed 7 RCTs, involving a total of 209 patients affected by MS, of which 97 patients performed exergaming or VR and 112 patients underwent conventional rehabilitation. The meta-analysis reported a significant overall ES of 4.25 (p < 0.0001), showing in the subgroup analysis a non-significant ES of 1.85 (p = 0.39) for the VR and a significant ES of 4.49 (p < 0.0001) for the exergames in terms of the BBS improvement. Taken together, these findings suggested that balance rehabilitation using exergames appears to be more effective than conventional rehabilitation in patients affected by MS.
Introduction
Multiple sclerosis (MS) is one of the most common causes of progressive neurological disability among young adults (1). Upper limb impairments, muscle weakness, spasticity, reduced functional performance, and fatigue are common clinical manifestations in patients with MS (2–6). A crucial impairment that might be often showed by patients with MS is balance disturbance, which could result in a higher risk of falling and reduced independence in the activities of daily living (ADLs) (7–10). To overcome these highly disabling issues, different rehabilitative approaches have been proposed so far in the literature (11, 12). In addition to conventional physiotherapy and rehabilitation interventions, technological devices are a promising therapeutic intervention in the complex framework of MS treatment. In this scenario, virtual reality (VR) approaches are suggested as potentially useful tools in several rehabilitative pathological conditions (13). Indeed, VR might enhance the interaction with surrounding artificial environment created to appear similar to the original one, allowing a multisensorial feedback training that might further increase the rehabilitation efficacy. Indeed, human balance control is the results of multiple sensory system inputs, integrated into a complex mechanism of constant reweight and adjustments, as visual, vestibular, and proprioception signals are continuously converted to corrective motor actions (14). Hence, a multisensorial augmented reality might be a particularly effective rehabilitation approach in MS balance impairments.
Moreover, it is provided though a display that can be also head-mounted, with complementary motion tracking devices, sound effects, and eventually end-effectors such as joysticks or sensors able to capture even muscle and brain signals (15). VR has been integrated in several neurological diseases rehabilitative protocols, including patients affected by MS, with promising results (13, 16–18). As a complementary tool of VR in rehabilitation programs (19), patients could also perform exergames, defined as the activity of playing video games that involve physical exertion (20). In the recent years, exergaming has been widely used in several rehabilitative programs and clinical study (21–23). Active video game therapy could reduce the boredom of the rehabilitation process, increasing patient motivation, providing direct feedback, and enabling dual-task training. In this study, commercially available exergames (e.g., Nintendo Wii and Microsoft Kinect) have successfully transformed living rooms into playful training environments for about 10 years (24). Clinical and home trials have been conducted to investigate the effectiveness of Nintendo Wii Fit in patients with MS, focusing on balance and gait improvement, but the results are controversial (25). In the recent years, researchers started to evaluate exergames as a rehabilitation tool for patients with MS (26). Exergaming has proved to be an acceptable, feasible, safe, fun, stimulating, and self-motivating tool (27). However, there is limited evidence of its efficacy among neurological pathologies, in particular, in patients with Parkinson's disease, stroke, and hereditary sensory motor neuropathy (28–30). To the best of our knowledge, few randomized controlled trials (RCTs) investigated the efficacy of exergaming in MS. Therefore, in systematic review and meta-analysis, we sought to evaluate the efficacy of exergames and VR compared with conventional rehabilitation treatment in terms of balance improvement in patients affected by MS.
Methods
Search Strategy
PubMed, Scopus, and Web of Science databases were systematically searched for English language articles published from the inception until May 14, 2021, according to each specific thesaurus, following the strategy depicted by Supplementary Table 1. This systematic review with meta-analysis was conducted according to the guidance of the Preferred Reporting Items for Systematic Reviews and Meta-Analyses (PRISMA) guidelines (31) and the Cochrane Handbook for Systematic Reviews of Interventions (32). Systematic review protocol has been registered on the International Prospective Register of Systematic Reviews (PROSPERO) (number: CRD42021257449).
Selection Criteria
After removing duplicates, two reviewers independently screened all the articles for eligibility. In case of disagreement, a consensus was reached with the opinion of a third reviewer. RCTs were considered eligible, if responding to the questions defined by the following the participants, intervention, comparator and outcome (PICO) model:
P) Participants: patients with MS.
I) Intervention: Exergames and/or VR.
C) Comparator: Conventional rehabilitation.
O) Outcome measure: Balance assessed by the Berg Balance Scale (BBS).
We included only RCTs with two groups (study group and control group) providing data at the end of the intervention (after 1 week later as maximum). We excluded: (1) studies including patients with MS aged <18 years; (2) studies including patients with MS with the Expanded Disability Status Scale (EDSS) score > 6; (3) cross-over study design; (4) studies written in a language different from English; (5) full-text unavailability (i.e., posters and conference abstracts); and (6) studies involving animals.
Data Extraction
Two reviewers independently extracted main data from the included RCTs through a customized data extraction model on a Microsoft Excel sheet. In case of disagreement, a consensus was obtained asking the opinion of another reviewer.
We extracted the following data: (1) First author; (2) Publication year; (3) Nationality; (4) Age of study participants; (5) Type of exergames and/or VR as intervention; (6) Type of control (placebo or sham treatment); (7) Population and number of patients included in the RCTs; (8) the BBS values as outcome measure; and (9) Main findings.
Data Synthesis
The RCTs were synthesized describing extracted data and the study quality was independently assessed by two authors according to the PEDro scale (33). In case of disagreement, a third reviewer was asked to obtain a consensus. RCTs included were classified, according to the PEDro scale (33), as excellent (9–10 points), good (6–8 points), fair (4–5 points), or poor (<4 points) quality studies. Additionally, two authors assessed the risk-of-bias using the revised Cochrane risk-of-bias 2 (RoB 2) tool for randomized trials (34) and discussed any disagreements until consensus was reached with a third reviewer.
Statistical Analysis
The statistical analysis was performed on Stata version 15.0 (Stata, College Station, Texas, USA) and RevMan version 5.3. The heterogeneity among comparisons was estimated by the chi-squared and I2 statistic tests. An I2 > 50% determined significant heterogeneity across the articles. Effect size (ES) measure and a random-effects model were obtained to determine the pooled estimates with 95% CIs. Missing means and SDs were estimated from medians, ranges, and interquartile ranges (IQRs) using the method introduced by Hozo et al. (35). Then, we carried out a sensitivity analysis on the stability of the combined results. Lastly, we also performed a subgroup analysis on the intervention type to investigate the source of heterogeneity. The potential publication bias was assessed using a contour-enhanced funnel plot of effect size against its SE.
Results
Study Characteristics
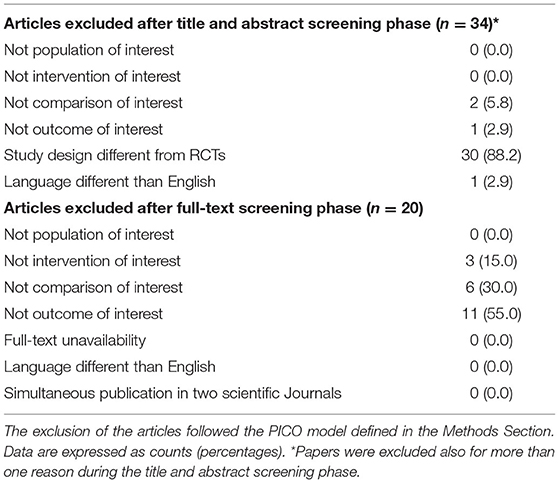
At the end of the search, 93 studies were identified, 61 of which were considered suitable for title and abstract screening, after the removal of duplicates. Out of these, 34 studies were excluded after the title and abstract screening, according to the PICO model. Thus, the selected articles were assessed for eligibility and 20 of them were excluded according to the following reasons: not intervention of interest (n = 3), not comparison of interest (n = 6), and not outcome of interest (n = 11) (see Table 1 for further details). Therefore, 7 RCTs (26, 36–41) were included in this systematic review, as shown by the PRISMA flowchart in Figure 1. The main characteristics of these studies are given in detail in Table 2. The included studies (26, 36–41) have been published in the last 7 years (from 2003 to 2020). Five (36, 37, 39–41) (71.4%) studies were conducted in Europe [one (36) study from Italy, two (37, 41) study from Spain, one (39) study from Hungary, one (40) study from Israel] and two (26, 38) (28.6%) studies were conducted in Eastern Mediterranean [one (26) study from Jordan, one (38) study from Iran]. A total of 209 subjects were analyzed and 97 subjects performed VR or exergaming as balance training, whereas 112 subjects were included in the control group (undergoing conventional balance training). Study cohorts of the RCTs included ranged from 11 (41) to 47 (37) patients, with a mean age ranging from 34.9 ± 8.9 (26) to 48.3 ± 10.8 years (41). Concerning the follow-up evaluations, only one RCT (38) performed a follow-up at 12 weeks from baseline. Five RCTs (26, 36–39) investigated the effectiveness of exergaming and two RCTs (40, 41) investigated the effectiveness of VR.
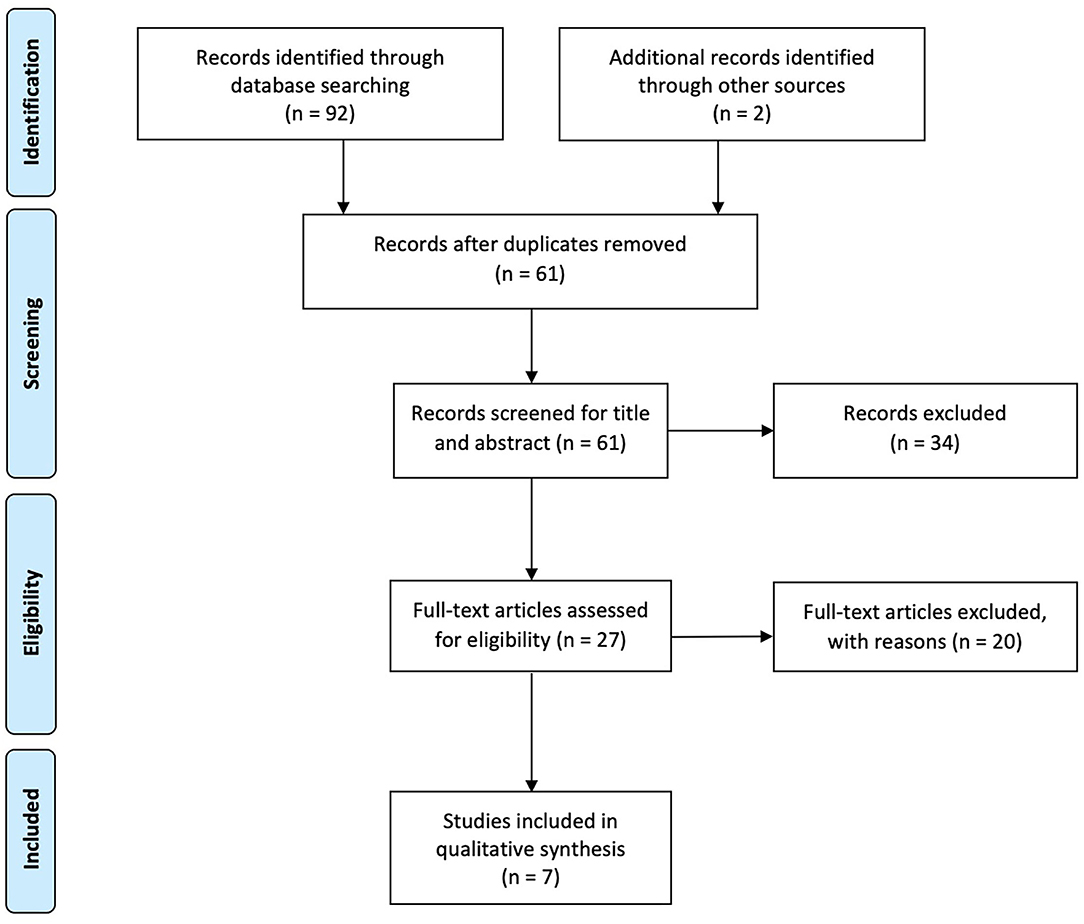
Figure 1. The Preferred Reporting Items for Systematic Reviews and Meta-Analyses (PRISMA) flow diagram.
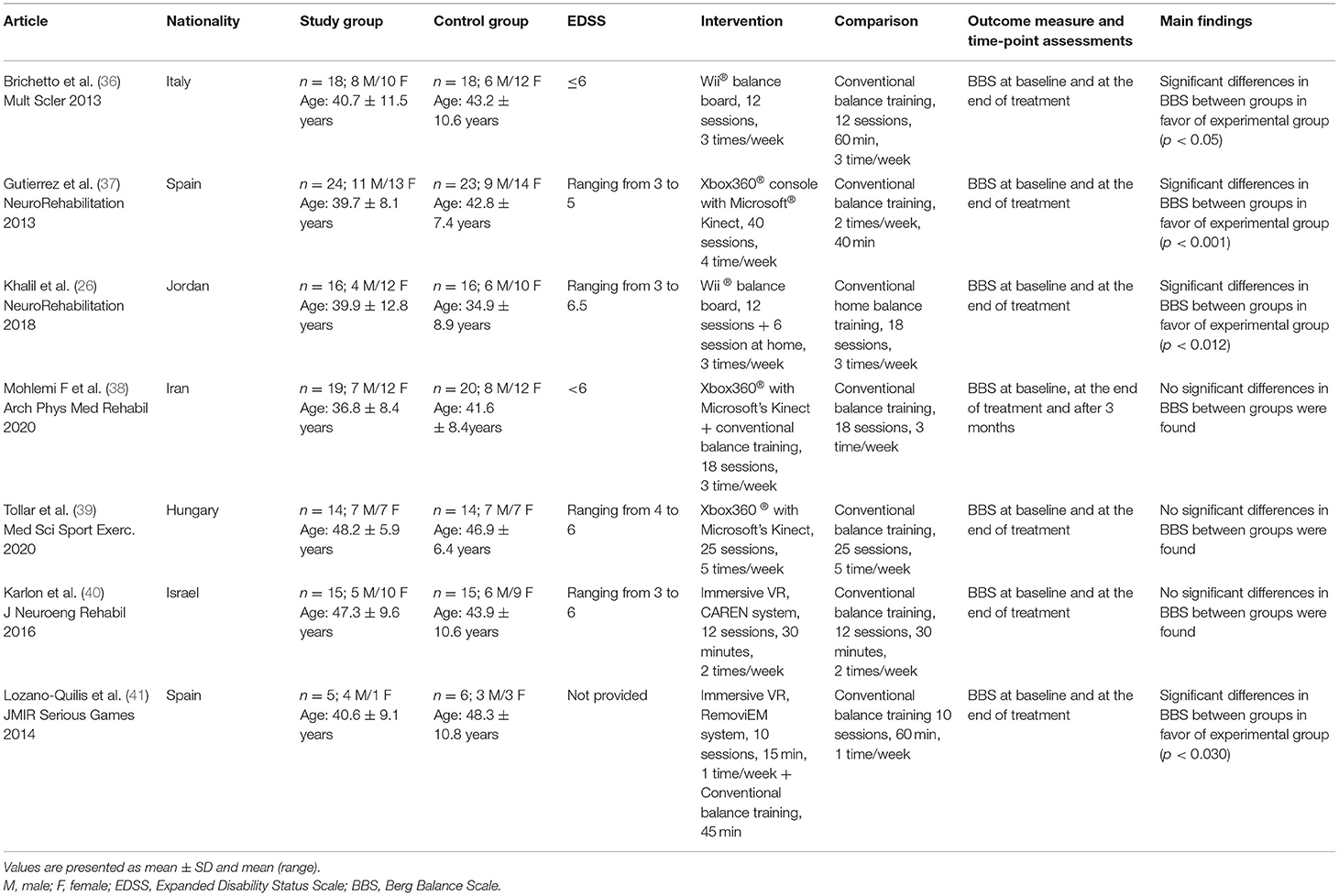
Table 2. Main characteristics of the randomized controlled trials included in the present systematic review.
Exergaming
Five RCTs (26, 36–39) assessed exergames as intervention compared with conventional balance training. Brichetto et al. (36) showed a significant improvement in the BBS in the experimental group after therapy (54.6 ± 2.2 vs. 49.7 ± 3.9; time × treatment: p < 0.05). Gutierrez et al. (37) reported a significant improvement in the BBS in the experimental group when comparing with control group at the end of the balance training (89.4 ± 6.6 vs. 81.9 ± 10.1; F = 29.896, p < 0.001). Similar results were found by Khalil et al. (26). They showed a significant difference between groups according to the balance score in favor of the experimental group (EG) (50.4 ± 3.7 vs. 45.1 ± 8.64; p = 0.012). On the other hand, Mohlemi et al. (38) investigated the efficacy of Xbox360® plus conventional balance training vs. conventional rehabilitation, showing an improvement in the BBS in both the groups at the end of the treatment (EG: 46.6 ± 3.9 vs. 52.4 ± 2.1; p < 0.001; control group (CG) 45.5 ± 7.2 vs. 49.9 ± 5.5; p < 0.001) and at follow-up (52.0 ± 2.7; p < 0.001; 49.0 ± 5.7; p = 0.01, respectively). However, no differences between group were showed (p = 0.32 at the end; p = 0.10 at the follow-up). Similar results were found by Tollar et al. (39). The authors showed significant differences within groups in terms of balance activity after exergaming training (study group: 6.1 ± 3.5; p < 0.005 vs. control group: 3.9 ± 2.3; p < 0.005), but improvements in the BBS did not differ between groups.
Virtual Reality
Two studies (40, 41) have investigated the effectiveness of VR vs. conventional balance training. Karlon et al. (40) in 2016 reported non-statistically significant differences between groups in the BBS score after treatment (47.9 ± 6.4 vs. 44.6 ± 4.9; F (p-value) = 1.794 (0.561)]. On the other hand, Lozano-Quilis et al. (41) used a kinect-based VR plus conventional balance training as intervention. A significant improvement in the BBS was found between groups in favor of the experimental group (50.3 ± 5.6 vs. 51.6 ± 5.8; p < 0.030).
Meta-Analysis
A meta-analysis was performed to highlight the efficacy of exergames and VR in improving balance (measured by the BBS) in patients affected by MS, showing an overall ES of 4.25 (95% CI = 3.14–5.36, p = 0.00001). The subgroup analysis reported a non-significant ES of VR in terms of the BBS improvement [1.85 (95% CI = 2.33–6.04), p = 0.39], whereas there was a significant improvement in the ES of the exergaming [4.49 (95% CI = 3.32–5.66), p = 0.00001], as shown by Figure 2. Given the low number of RCTs, a random-effects model was adopted. Moreover, the Begg's funnel plot analysis of publishing bias reported qualitatively symmetry in the RCTs included in this study, as shown in Figure 3.
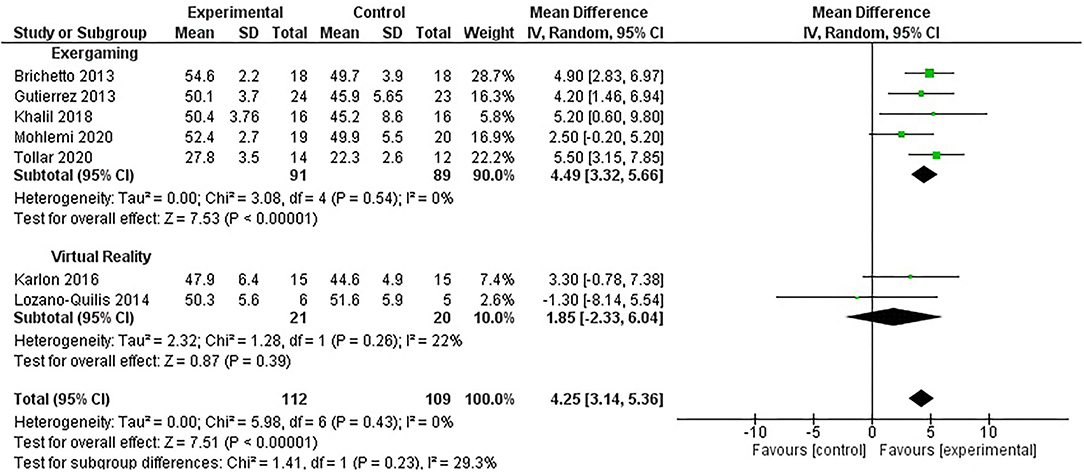
Figure 2. Forest plot illustrating the comparison between exergaming and virtual reality interventions vs. conventional rehabilitation through a meta-analysis.
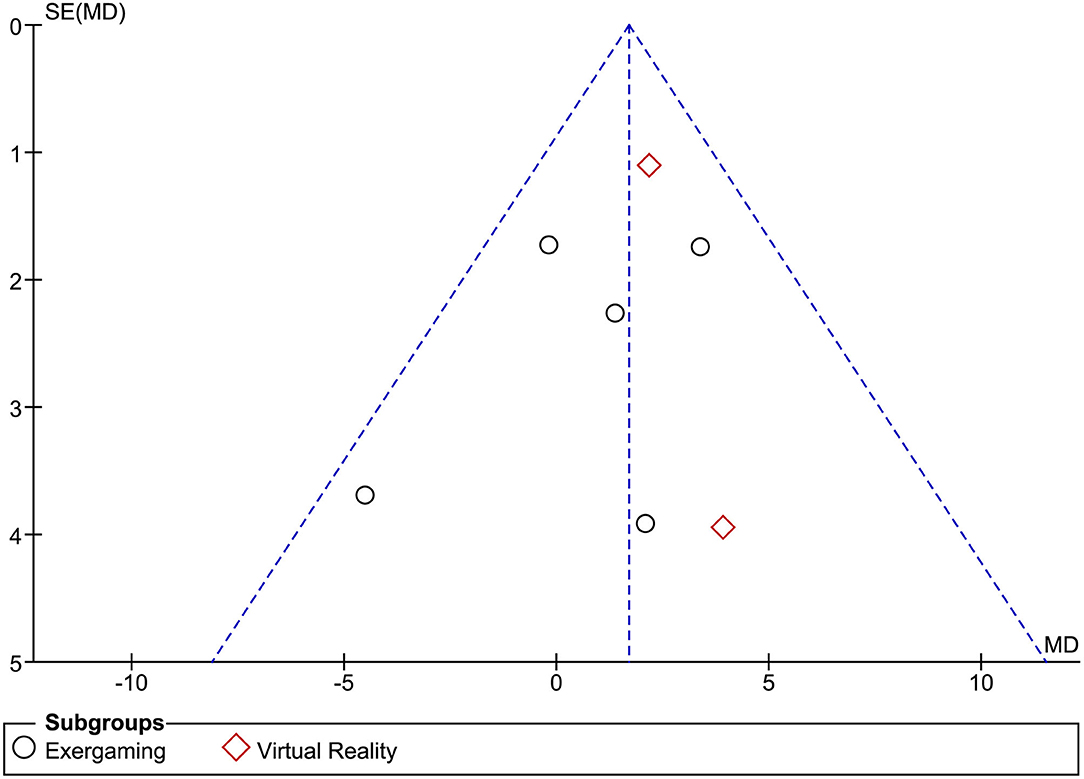
Figure 3. Begg's funnel plot analysis of publishing bias in the studies included in the present systematic review.
Risk-of-Bias
The risk-of-bias among the RCTs analyzed was estimated using the RoB 2 (42) (see Figure 4 for further details). With respect to the selection bias, six studies (85.7%) ensured a correct randomization (26, 36–40). Five RCTs (71.4%) (26, 36–39) excluded performance bias. On the other hand, six studies (85.7%) (26, 36, 38–41) provided guarantees on blinding of outcome assessment and six studies (85.7%) (26, 36–40) adequately assessed attrition bias.
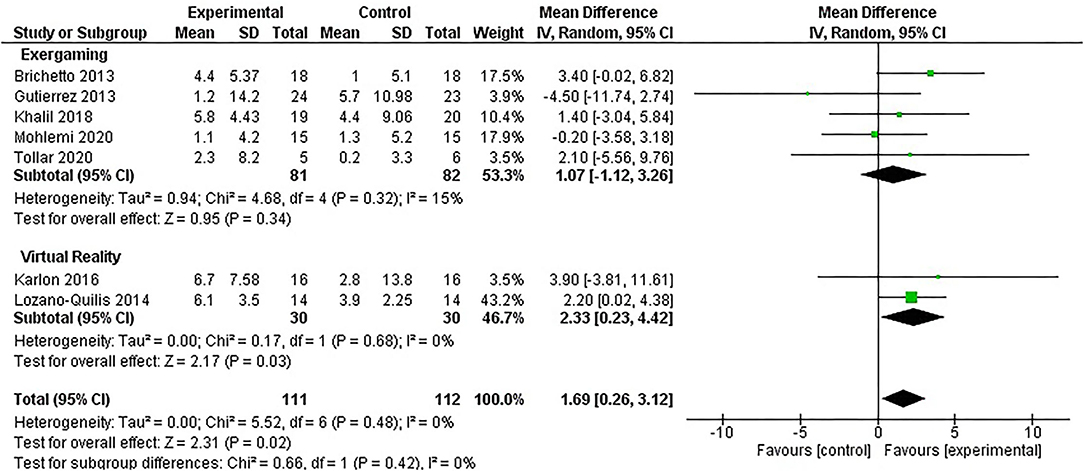
Figure 4. Risk-of-bias assessed by the version 2 of the Cochrane risk-of-bias 2 (RoB 2) tool for randomized trials.
Discussion
Virtual reality has recently emerged as a promising intervention in the rehabilitation of several neurological diseases (28–30, 43). This intriguing and complex technique can evoke brain behavioral responses that mimic real-world interaction, acting in real-time but in a safe environment. Exergaming consists of whole-body physical exercises comparable to a moderate intensity training, performed through active video games (44). It has been used in the rehabilitation of several neurological diseases to enhance both the cognitive and physical function and improve balance (45–47), as it offers task-oriented exercises enhancing motor learning and neural plasticity (48). Our findings are in line with previous evidence in the neurorehabilitation field, reporting that VR and exergaming are cumulatively effective on gait and balance in Parkinson's disease (49, 50), patients with poststroke (51), traumatic brain injury (52), and cerebral palsy (53). Despite the overall significance demonstrated for these two rehabilitation approaches (p = 0.00001), it should be noted that in the subgroup analysis, only exergames reported a significant effect size (p = 0.00001) compared to VR (p = 0.39).
Although robotic rehabilitation effects on balance and gait have been recently investigated with positive results in patients with MS (54), few studies in literature addressed the effectiveness of VR and exergames compared with conventional treatment in patients with MS and in most cases only considering VR as a complementary tool in MS rehabilitation concerning balance. This could be related to the relative novelty of these devices and the difficult implementation in the clinical setting.
Firstly, Casuso-Holgado et al. (55), analyzed in a systematic review the effectiveness of VR on gait and balance in patients affected by MS, showing significant differences in comparison with no interventions and inconclusive evidence compared with standard treatment. However, the authors included several different outcome measures (i.e., walking speed and postural balance). Moreover, Cano Porras et al. (56) in a systematic review found only three studies focusing on the BBS as primary outcome in patients with MS and VR rehabilitation, with inconclusive results.
Evidence on the role of VR in rehabilitative management of patients with MS is scarce, even though, in 2016, Massetti et al. (57) performed a systematic review on the effects of VR in patients affected by MS, including also observational studies and considering mixed outcomes. Although this approach widened the number of studies included, the low quality of the studies precluded to perform a meta-analysis. Furthermore, a recent meta-analysis performed by Nascimento et al. (58) suggested that VR could induce benefits that can be similar or greater than conventional exercises in patients with MS. However, taken together, all these studies were unable to draw strong conclusion about the real impact of VR on balance improvement in patients with MS, even though the effects of this approach are promising, considering the evidence obtained in other chronic neurological disorders (59, 60).
Concerning exergames, Mura et al. (45), found that in mixed neurological pathologies, including MS, they might significantly improve executive functions and visuospatial perception compared with no intervention or standard rehabilitative treatment. Concerning balance, successive studies in mixed neurological diseases confirmed that exergames might be at least equivalent to conventional therapy (59) and are able to improve balance dysfunction (60).
In the present systematic review and meta-analysis, we found that VR and exergaming might significantly improve balance in terms of the BBS compared with standard treatment alone in patients affected by MS. Among balance assessment, we assessed the BBS as primary outcome, since it is widely used and recommended in different neurological settings for patients with MS with EDSS ranging from 0 to 7.5 (61). Given that the esteemed minimal clinically important difference for the BBS is 3 points (62), most of the selected studies showed a clinically significant difference between standard treatment and exergaming/VR interventions. Furthermore, VR and exergames might improve balance proposing simultaneous motor and cognitive tasks (63) that might also be addictive, improving both the motivation and treatment adherence (64). In this study, repetitive practice and observation are crucial for motor learning and VR might induce plastic changes in central nervous system that has been associated with mirror imagery in other neurological disorders such as stroke survivors through a facilitation effect on sensorimotor networks (65). The high adherence observed in patients performing exergaming might be due to the low practical barriers, high accessibility, low cost of the consoles, and the social impact because of the potential involvement of family members in multiplayer games (21). Moreover, exergames provide visual and auditory feedback, currently altered in patients affected by MS (66), thus improving the self-awareness of the patients during the training. Furthermore, Yazgan et al. (67) demonstrated a significant improvement in terms of fatigue and gait after exergaming treatment. The authors suggested that these improvements were obtained thanks to the less anxiety and greater confidence in the balance raised by the videogame approach and not a low energy expenditure compared to standard treatments.
This systematic review and meta-analysis have also some clinical implications for the rehabilitation clinical practice, considering that VR resulted to be an intriguing alternative for balance training in patients with MS, with psychological advantages that could enhance their motivation and treatment adherence (68). Clinicians should strike the right balance between too difficult and too easy tasks and as such keeping the motivation of the patients high. Objective progression and extrinsic feedback encourage robot-assisted rehabilitation that might play a critical role on neuroplasticity (69, 70). Lastly, it should be considered that VR might be home based, with a telerehabilitation approach, which is highly encouraged during coronavirus disease 2019 (COVID-19) pandemic, due to psychological and hospitalization issues (71–73).
We are aware that our systematic review considered only a small number of RCTs due to the limited evidence available in the literature. Hence, further high-quality studies investigating exergames and VR effects in improving balance in patients with MS compared with conventional rehabilitation treatment are still warranted and the use of relatively recent exergaming devices is not created specifically for neurorehabilitation. Moreover, to improve the strength of evidence on VR, future RCTs addressing this specific issue in patients with MS are warranted.
Conclusion
This study suggested that rehabilitative interventions using exergames and VR appear to be more effective than conventional rehabilitation to improve balance in patients with MS. More in detail, exergames showed to have a significant efficacy in improving balance outcomes and considering its safety and its effects on neuroplasticity, sensorimotor training, and motivation of the patients, it could be implemented as an effective technique in the complex rehabilitative treatment framework of neurological diseases including MS. Starting from these promising data, further evidence is warranted in the next future to focus on VR and its role in the rehabilitative approach to neurological disorders.
Data Availability Statement
The raw data supporting the conclusions of this article will be made available by the authors, without undue reservation.
Author Contributions
DC and AS contribute to the study design and conceptualization. AS contributes to the databases searching. DC, CC, and AC-S contribute to the data screening. AA, FFo, and AS contribute to the data extraction. DC, MI, and AS contribute to the data synthesis and interpretation. NM contributes to the statistical analysis. DC contributes to the manuscript drafting. MI and AS contribute to the critical revision, study supervision, and study submission. AA, NM, FFo, TP, FFe, CC, and AC-S contribute to the visualization. All the authors read and approved the final version of the manuscript.
Conflict of Interest
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
Publisher's Note
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
Acknowledgments
We would like to thank Matilde Zanini, PT for her support in this study.
Supplementary Material
The Supplementary Material for this article can be found online at: https://www.frontiersin.org/articles/10.3389/fneur.2021.773459/full#supplementary-material
References
1. McGinley MP, Goldschmidt CH, Rae-Grant AD. Diagnosis and Treatment of Multiple Sclerosis: A Review. JAMA. (2021) 325:765–79. doi: 10.1001/jama.2020.26858
2. Solaro C, de Sire A, Messmer Uccelli M, Mueller M, Bergamaschi R, Gasperini C et al. Efficacy of levetiracetam on upper limb movement in multiple sclerosis patients with cerebellar signs: a multicenter double-blind, placebo-controlled, crossover study. Eur J Neurol. (2020) 27:2209–16. doi: 10.1111/ene.14403
3. de Sire A, Mauro A, Priano L, Baudo S, Bigoni M, Solaro C. Effects of Constraint-Induced Movement Therapy on upper limb activity according to a bi-dimensional kinematic analysis in progressive multiple sclerosis patients: a randomized single-blind pilot study. Funct Neurol. (2019) 34:151–7.
4. de Sire A, Bigoni M, Priano L, Baudo S, Solaro C, Mauro A. Constraint-Induced Movement Therapy in multiple sclerosis: Safety and three-dimensional kinematic analysis of upper limb activity: a randomized single-blind pilot study NeuroRehabilitation. (2019) 45:247–54. doi: 10.3233/NRE-192762
5. Agostini F, Pezzi L, Paoloni M, Insabella R, Attanasi C, Bernetti A et al. Motor Imagery: A Resource in the Fatigue Rehabilitation for Return-to-Work in Multiple Sclerosis Patients-A Mini Systematic Review. Front Neurol. (2021) 12:696276. doi: 10.3389/fneur.2021.696276
6. Patti F, Chisari CG, D'Amico E, Annovazzi P, Banfi P, Bergamaschi R et al. Clinical and patient determinants of changing therapy in relapsing-remitting multiple sclerosis (SWITCH study). Mult Scler Relat Disord. (2020) 42:102124. doi: 10.1016/j.msard.2020.102124
7. Paolucci T, Bernetti A, Sbardella S, La Russa C, Murgia M, Salomè A et al. Straighten your back! Self-correction posture and postural balance in “non rehabilitative instructed” multiple sclerosis patients. NeuroRehabilitation. (2020) 46:333–41. doi: 10.3233/NRE-192987
8. O'Malley N, Clifford AM, Comber L, Coote S. Fall definitions, faller classifications and outcomes used in falls research among people with multiple sclerosis: a systematic review. Disabil Rehabil. (2020) 6:1–8. doi: 10.1080/09638288.2020.1786173
9. Cameron MH, Nilsagard Y. Balance, gait, and falls in multiple sclerosis. Handb Clin Neurol. (2018) 159:237–50. doi: 10.1016/B978-0-444-63916-5.00015-X
10. Kraft AK. Berger K. Quality of Care for Patients With Multiple Sclerosis-A Review of Existing Quality Indicators Front Neurol. (2021) 12:708723. doi: 10.3389/fneur.2021.708723
11. Amatya B, Khan F, Galea M. Rehabilitation for people with multiple sclerosis: an overview of Cochrane Reviews. Cochrane Database Syst Rev. (2019) 1:CD012732. doi: 10.1002/14651858.CD012732.pub2
12. Correale L, Buzzachera CF, Liberali G, Codrons E, Mallucci G, Vandoni M et al. Effects of Combined Endurance and Resistance Training in Women With Multiple Sclerosis: A Randomized Controlled Study. Front Neurol. (2021) 12:698460. doi: 10.3389/fneur.2021.698460
13. Maggio MG, Russo M, Cuzzola MF, Destro M, La Rosa G, Molonia F et al. Virtual reality in multiple sclerosis rehabilitation: A review on cognitive and motor outcomes. J Clin Neurosci. (2019) 65:106–11. doi: 10.1016/j.jocn.2019.03.017
14. Peterka RJ. Sensory integration for human balance control. Handb Clin Neurol. (2018) 159:27–42. doi: 10.1016/B978-0-444-63916-5.00002-1
15. Laver KE, George S, Thomas S, Deutsch JE, Crotty M. Virtual reality for stroke rehabilitation. Cochrane Database Syst Rev. (2015) 2015:CD008349. doi: 10.1002/14651858.CD008349.pub3
16. Abou L, Malala VD, Yarnot R, Alluri A, Rice LA. Effects of Virtual Reality Therapy on Gait and Balance Among Individuals With Spinal Cord Injury: A Systematic Review and Meta-analysis. Neurorehabil Neural Repair. (2020) 34:375–88. doi: 10.1177/1545968320913515
17. Kefaliakos A, Pliakos I, Kiekkas P, Charalampidou M, Diomidous M. Virtual Reality in the Rehabilitation of Patients with Neurological Disorders. Stud Health Technol Inform. (2016) 226:45–7.
18. Liao YY, Yang YR, Cheng SJ, Wu YR, Fuh JL, Wang RY. Virtual Reality-Based Training to Improve Obstacle-Crossing Performance and Dynamic Balance in Patients With Parkinson's Disease. Neurorehabil Neural Repair. (2015) 29:658–67. doi: 10.1177/1545968314562111
19. García-Bravo S, Cuesta-Gómez A, Campuzano-Ruiz R, López-Navas MJ, Domínguez-Paniagua J, Araújo-Narváez A et al. Virtual reality and video games in cardiac rehabilitation programs. A systematic review Disabil Rehabil. (2021) 43:448–57. doi: 10.1080/09638288.2019.1631892
20. O'Loughlin EK, Dutczak H, Kakinami L, Consalvo M, McGrath JJ, Barnett TA. Exergaming in Youth and Young Adults: A Narrative Overview. Games Health J. (2020) 9:314–38. doi: 10.1089/g4h.2019.0008
21. Marotta N, Demeco A, Indino A, de Scorpio G, Moggio L, Ammendolia A. Nintendo WiiTM versus Xbox KinectTM for functional locomotion in people with Parkinson's disease: a systematic review and network meta-analysis. Disabil Rehabil. (2020) 1:1–6. doi: 10.1080/09638288.2020.1768301
22. Khoury AR. Motion Capture for Telemedicine: A Review of Nintendo Wii, Microsoft Kinect, and PlayStation Move. J Int Soc Telemed EHealth. (2018) 6:e14 (1–9). doi: 10.29086/JISfTeH.6.e14
23. Chesser BT, Blythe SA, Ridge LD, Roskone Tomaszewski RE, Kinne BL. Effectiveness of the Wii for pediatric rehabilitation in individuals with cerebral palsy: a systematic review. Physical Therapy Reviews. (2020) 25:106–17. doi: 10.1080/10833196.2020.1740402
24. Givon Schaham N, Zeilig G, Weingarden H, Rand D. Game analysis and clinical use of the Xbox-Kinect for stroke rehabilitation. Int J Rehabil Res. (2018) 41:323–30. doi: 10.1097/MRR.0000000000000302
25. Zahra A, Sekhavat YA, Goljaryan S. A framework for rehabilitation games to improve balance in people with multiple sclerosis (MS). In: IEEE 2018 2nd National and 1st International Digital Games Research Conference: Trends, Technologies, and Applications (DGRC). (2018).
26. Khalil H, Al-Sharman A, El-Salem K, Alghwiri AA, Al-Shorafat D, Khazaaleh S, et al. The development and pilot evaluation of virtual reality balance scenarios in people with multiple sclerosis (MS): a feasibility study. NeuroRehabilitation. (2018) 43:473–82. doi: 10.3233/NRE-182471
27. Feys P, Straudi S. Beyond therapists: Technology-aided physical MS rehabilitation delivery. Mult Scler. (2019) 25:1387–93. doi: 10.1177/1352458519848968
28. Canning CG, Allen NE, Nackaerts E, Paul SS, Nieuwboer A, Gilat M. Virtual reality in research and rehabilitation of gait and balance in Parkinson disease. Nat Rev Neurol. (2020) 16:409–25. doi: 10.1038/s41582-020-0370-2
29. Costa MTS, Vieira LP, Barbosa EO, Mendes Oliveira L, Maillot P, Ottero Vaghetti CA et al. Virtual reality-based exercise with exergames as medicine in different contexts: A short review. Clin Pract Epidemiol Ment Health. (2019) 15:15–20. doi: 10.2174/1745017901915010015
30. Nguyen AV, Ong YA, Luo CX, Thuraisingam T, Rubino M, Levin MF et al. Virtual reality exergaming as adjunctive therapy in a sub-acute stroke rehabilitation setting: facilitators and barriers. Disabil Rehabil Assist Technol. (2019) 14:317–24. doi: 10.1080/17483107.2018.1447608
31. Moher D, Altman DG, Liberati A, Tetzlaff J. PRISMA statement. Epidemiology. 2011 22:128 author reply 128. doi: 10.1097/EDE.0b013e3181fe7825
32. Higgins JP, Thomas J, Chandler J, Cumpston M, Li T, Page MJ et al. Cochrane Handbook for Systematic Reviews of Interventions. USA:JohnWiley & Sons (2019). doi: 10.1002/9781119536604
33. Maher CG, Sherrington C, Herbert RD, Moseley AM, Elkins M. Reliability of the PEDro scale for rating quality of randomized controlled trials. Phys Ther. (2003) 83:713–21. doi: 10.1093/ptj/83.8.713
34. Sterne JAC, Savović J, Page MJ, Elbers RG, Blencowe NS, Boutron I, et al. RoB 2: a revised tool for assessing risk of bias in randomised trials. BMJ. (2019) 366:l4898. doi: 10.1136/bmj.l4898
35. Hozo SP, Djulbegovic B, Hozo I. Estimating the mean and variance from the median, range, and the size of a sample. BMC Med Res Methodol. (2005) 5:13. doi: 10.1186/1471-2288-5-13
36. Brichetto G, Spallarossa P, de Carvalho ML, Battaglia MA. The effect of Nintendo® Wii® on balance in people with multiple sclerosis: A pilot randomized control study. Mult Scler. (2013) 19:1219–21. doi: 10.1177/1352458512472747
37. Gutiérrez RO, Galán Del Río F, Cano-De La Cuerda R, Alguacil Diego IM, Diego A, González RA et al. A telerehabilitation program by virtual reality-video games improves balance and postural control in multiple sclerosis patients. NeuroRehabilitation. (2013) 33:545–54. doi: 10.3233/NRE-130995
38. Molhemi F, Monjezi S, Mehravar M, Shaterzadeh-Yazdi MJ, Salehi R, Hesam S et al. Effects of Virtual Reality vs Conventional Balance Training on Balance and Falls in People With Multiple Sclerosis: A Randomized Controlled Trial. Arch Phys Med Rehabil. (2021) 102:290–9. doi: 10.1016/j.apmr.2020.09.395
39. Tollár J, Nagy F, Tóth BE, Török K, Szita K, Csutorás B et al. Exercise Effects on Multiple Sclerosis Quality of Life and Clinical-Motor Symptoms. Med Sci Sports Exerc. (2020) 52:1007–14. doi: 10.1249/MSS.0000000000002228
40. Kalron A, Fonkatz I, Frid L, Baransi H, Achiron A. The effect of balance training on postural control in people with multiple sclerosis using the CAREN virtual reality system: a pilot randomized controlled trial. J Neuroeng Rehabil. (2016) 13:13. doi: 10.1186/s12984-016-0124-y
41. Lozano-Quilis JA, Gil-Gómez H, Gil-Gómez JA, Albiol-Pérez S, Palacios-Navarro G, Fardoun HM et al. Virtual rehabilitation for multiple sclerosis using a kinect-based system: randomized controlled trial. JMIR Serious Games. (2014) 2:e12. doi: 10.2196/games.2933
42. Higgins JP, Thompson SG, Deeks JJ, Altman DG. Measuring inconsistency in meta-analyses. BMJ. (2003) 327:557–60. doi: 10.1136/bmj.327.7414.557
43. de Araújo AVL, Neiva JFO, Monteiro CBM, Magalhães FH. Efficacy of Virtual Reality Rehabilitation after Spinal Cord Injury: A Systematic Review. Biomed Res Int. (2019) 2019:7106951. doi: 10.1155/2019/7106951
44. Bohil CJ, Alicea B, Biocca FA. Virtual reality in neuroscience research and therapy. Nat Rev Neurosci. (2011) 12:752–62. doi: 10.1038/nrn3122
45. Mura G, Carta MG, Sancassiani F, Machado S, Prosperini L. Active exergames to improve cognitive functioning in neurological disabilities: a systematic review and meta-analysis. Eur J Phys Rehabil Med. (2018) 54:450–62. doi: 10.23736/S1973-9087.17.04680-9
46. Kannan L, Vora J, Bhatt T, Hughes SL. Cognitive-motor exergaming for reducing fall risk in people with chronic stroke: A randomized controlled trial. NeuroRehabilitation. (2019) 44:493–510. doi: 10.3233/NRE-182683
47. Harris DM, Rantalainen T, Muthalib M, Johnson L, Duckham RL, Smith ST et al. Concurrent exergaming and transcranial direct current stimulation to improve balance in people with Parkinson's disease: study protocol for a randomised controlled trial. Trials. (2018) 19:387. doi: 10.1186/s13063-018-2773-6
48. Levin MF. Can virtual reality offer enriched environments for rehabilitation? Expert Rev Neurother. (2011) 11:153–5. doi: 10.1586/ern.10.201
49. Dockx K, Bekkers EM, Van den Bergh V, Ginis P, Rochester L, Hausdorff JM et al. Cochrane Movement Disorders Group Virtual reality for rehabilitation in Parkinson's disease. Cochrane Database Syst Rev. (2016) 12:CD010760. doi: 10.1002/14651858.CD010760.pub2
50. Harris DM, Rantalainen T, Muthalib M, Johnson L, Teo WP. Exergaming as a viable therapeutic tool to improve static and dynamic balance among older adults and people with idiopathic Parkinson's disease: a systematic review and meta-analysis. Front Aging Neurosci. (2015) 7:167. doi: 10.3389/fnagi.2015.00167
51. Rajaratnam BS, Gui Kaien J, Lee Jialin K, Sweesin K, Sim Fenru S, Enting L et al. Does the inclusion of virtual reality games within conventional rehabilitation enhance balance retraining after a recent episode of stroke? Rehabil Res Pract. (2013) 2013:649561. doi: 10.1155/2013/649561
52. Sessoms PH, Gottshall KR, Collins JD, Markham AE, Service KA, Reini SA. Improvements in gait speed and weight shift of persons with traumatic brain injury and vestibular dysfunction using a virtual reality computer-assisted rehabilitation environment. Mil Med. (2015) 180:143–9. doi: 10.7205/MILMED-D-14-00385
53. Brien M, Sveistrup H. An intensive virtual reality program improves functional balance and mobility of adolescents with cerebral palsy. Pediatr Phys Ther. (2011) 23:258–66. doi: 10.1097/PEP.0b013e318227ca0f
54. Bowman T, Gervasoni E, Amico AP, Antenucci R, Benanti P, Boldrini P et al. “CICERONE” Italian Consensus Group for Robotic Rehabilitation. What is the impact of robotic rehabilitation on balance and gait outcomes in people with multiple sclerosis? A systematic review of randomized control trials J Phys Rehabil Med. (2021) 57:246–53. doi: 10.23736/S1973-9087.21.06692-2
55. Casuso-Holgado MJ, Martín-Valero R, Carazo AF, Medrano-Sánchez EM, Cortés-Vega MD, Montero-Bancalero FJ. Effectiveness of virtual reality training for balance and gait rehabilitation in people with multiple sclerosis: a systematic review and meta-analysis. Clin Rehabil. (2018) 32:1220–34. doi: 10.1177/0269215518768084
56. Cano Porras D, Siemonsma P, Inzelberg R, Zeilig G, Plotnik M. Advantages of virtual reality in the rehabilitation of balance and gait: Systematic review. Neurology. (2018) 90:1017–25. doi: 10.1212/WNL.0000000000005603
57. Massetti T, Trevizan IL, Arab C, Favero FM, Ribeiro-Papa DC, de Mello Monteiro CB. Virtual reality in multiple sclerosis - A systematic review. Mult Scler Relat Disord. (2016) 8:107–12. doi: 10.1016/j.msard.2016.05.014
58. Nascimento AS, Fagundes CV, Mendes FADS. Leal JC. Effectiveness of Virtual Reality Rehabilitation in Persons with Multiple Sclerosis: A Systematic Review and Meta-analysis of Randomized Controlled Trials. Mult Scler Relat Disord. (2021) 54:103128. doi: 10.1016/j.msard.2021.103128
59. Perrochon A, Borel B, Istrate D, Compagnat M, Daviet JC. Exercise-based games interventions at home in individuals with a neurological disease: A systematic review and meta-analysis. Ann Phys Rehabil Med. (2019) 62:366–78. doi: 10.1016/j.rehab.2019.04.004
60. Prosperini L, Tomassini V, Castelli L, Tacchino A, Brichetto G, Cattaneo D, et al. Exergames for balance dysfunction in neurological disability: a meta-analysis with meta-regression. J Neurol. (2021) 268:3223–37. doi: 10.1007/s00415-020-09918-w
61. Potter K, Cohen ET, Allen DD, Bennett SE, Brandfass KG, Widener GL et al. Outcome measures for individuals with multiple sclerosis: recommendations from the American Physical Therapy Association Neurology Section task force. Phys Ther. (2014) 94:593–608. doi: 10.2522/ptj.20130149
62. Gervasoni E, Jonsdottir J, Montesano A, Cattaneo D. Minimal Clinically Important Difference of Berg Balance Scale in People With Multiple Sclerosis. Arch Phys Med Rehabil. 2017 98:337–340.e2. doi: 10.1016/j.apmr.2016.09.128
63. Veldkamp R, Baert I, Kalron A, Tacchino A. D'hooge M, Vanzeir E et al. Structured Cognitive-Motor Dual Task Training Compared to Single Mobility Training in Persons with Multiple Sclerosis, a Multicenter RCT. J Clin Med. (2019) 8:2177. doi: 10.3390/jcm8122177
64. Yang CM, Chen Hsieh JS, Chen YC, Yang SY, Lin HK. Effects of Kinect exergames on balance training among community older adults: A randomized controlled trial. Medicine. (2020) 99:e21228. doi: 10.1097/MD.0000000000021228
65. Merians AS, Poizner H, Boian R, Burdea G, Adamovich S. Sensorimotor training in a virtual reality environment: does it improve functional recovery poststroke? Neurorehabil Neural Repair. (2006) 20:252–67. doi: 10.1177/1545968306286914
66. Craig JJ, Bruetsch AP, Lynch SG. Huisinga JM. Altered visual and somatosensory feedback affects gait stability in persons with multiple sclerosis Hum Mov Sci. (2019) 66:355–62. doi: 10.1016/j.humov.2019.05.018
67. Yazgan YZ, Tarakci E, Tarakci D, Ozdincler AR. Kurtuncu M. Comparison of the effects of two different exergaming systems on balance, functionality, fatigue, and quality of life in people with multiple sclerosis: a randomized controlled trial. Mult Scler Relat Disord. (2019) 39:101902. doi: 10.1016/j.msard.2019.101902
68. Robinson J, Dixon J, Macsween A, van Schaik P, Martin D. The effects of exergaming on balance, gait, technology acceptance and flow experience in people with multiple sclerosis: a randomized controlled trial. BMC Sports Sci Med Rehabil. (2015) 7:8. doi: 10.1186/s13102-015-0001-1
69. Calafiore D, Negrini F, Tottoli N, Ferraro F, Ozyemisci Taskiran O, de Sire A. Efficacy of robotic exoskeleton for gait rehabilitation in patients with subacute stroke: a systematic review with meta-analysis. Eur J Phys Rehabil Med. 2021 12. doi: 10.23736/S1973-9087.21.06846-5
70. de Sire A, Marotta N, Demeco A, Ammendolia A. Exoskeleton versus end-effector robot-assisted therapy for finger-hand motor recovery in stroke survivors: systematic review and meta-analysis. Top Stroke Rehabil. (2021) 21:1–12. doi: 10.1080/10749357.2021.1967657
71. de Sire A, Andrenelli E, Negrini F, Lazzarini SG, Patrini M, Ceravolo Ceravolo MG, International Multiprofessional Steering Committee of Cochrane Rehabilitation REH-COVER action. Rehabilitation and COVID-19: the Cochrane Rehabilitation 2020 rapid living systematic review. Update as of August 31st, 2020. Eur J Phys Rehabil Med. 2020 56:839–845. doi: 10.23736/S1973-9087.20.06614-9
72. Marotta N, Demeco A, Moggio L, Ammendolia A. Why is telerehabilitation necessary? A pre-post COVID-19 comparative study of ICF activity and participation Journal of Enabling Technologies. (2021) 15:117–21. doi: 10.1108/JET-11-2020-0047
73. Negrini F, Ferrario I, Mazziotti D, Berchicci M, Bonazzi M, de Sire A, et al. Neuropsychological Features of Severe Hospitalized Coronavirus Disease 2019 Patients at Clinical Stability and Clues for Postacute Rehabilitation. Arch Phys Med Rehabil. (2021) 102:155–8. doi: 10.1016/j.apmr.2020.09.376
Keywords: virtual reality, exergames, multiple sclerosis, balance, rehabilitation, meta-analysis
Citation: Calafiore D, Invernizzi M, Ammendolia A, Marotta N, Fortunato F, Paolucci T, Ferraro F, Curci C, Cwirlej-Sozanska A and de Sire A (2021) Efficacy of Virtual Reality and Exergaming in Improving Balance in Patients With Multiple Sclerosis: A Systematic Review and Meta-Analysis. Front. Neurol. 12:773459. doi: 10.3389/fneur.2021.773459
Received: 09 September 2021; Accepted: 12 November 2021;
Published: 10 December 2021.
Edited by:
Giovanni Morone, Santa Lucia Foundation (IRCCS), ItalyReviewed by:
Le Li, Northwestern Polytechnical University, ChinaLuca Prosperini, San Camillo-Forlanini Hospital, Italy
Copyright © 2021 Calafiore, Invernizzi, Ammendolia, Marotta, Fortunato, Paolucci, Ferraro, Curci, Cwirlej-Sozanska and de Sire. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Marco Invernizzi, bWFyY28uaW52ZXJuaXp6aUBtZWQudW5pdXBvLml0; Alessandro de Sire, YWxlc3NhbmRyby5kZXNpcmVAdW5pY3ouaXQ=
 Dario Calafiore
Dario Calafiore Marco Invernizzi
Marco Invernizzi Antonio Ammendolia
Antonio Ammendolia Nicola Marotta
Nicola Marotta Francesco Fortunato5
Francesco Fortunato5 Teresa Paolucci
Teresa Paolucci Francesco Ferraro
Francesco Ferraro Claudio Curci
Claudio Curci Agnieszka Cwirlej-Sozanska
Agnieszka Cwirlej-Sozanska Alessandro de Sire
Alessandro de Sire