- 1Department of Anesthesiology, Beijing Tiantan Hospital, Capital Medical University, Beijing, China
- 2Department of Neurosurgery, Beijing Tiantan Hospital, Capital Medical University, Beijing, China
Background: Chordoma is a malignant bone and soft tissue tumor derived from embryonic notochord remnants, and skull base chordoma accounts for ~1/3 of all chordoma cases. Skull base chordoma is closely related to the brainstem and cranial nerves and has a high recurrence rate. The purpose of this study was to investigate the influence of the timing of tracheal extubation on perioperative pulmonary complications. We also aimed to explore predictors of postoperative artificial airway (AA) retention in patients with skull base chordoma.
Methods: This was a single-center, retrospective cohort study. The study population included all skull base chordoma patients undergoing surgical treatment between January 2019 and December 2021 at Beijing Tiantan Hospital. The primary outcome was the incidence of postoperative pulmonary complications. Several patient characteristics were evaluated for potential associations with AA retention.
Results: A total of 310 patients with skull base chordoma were enrolled. The frequency of AA retention after surgery for skull base chordoma was 30.97%. The incidence of postoperative pulmonary complications was much lower in those without AA retention (3.74 vs. 39.58%, P < 0.001). Factors with the highest point estimates for the odds of AA retention included body mass index, cranial nerve involvement, maximum tumor diameter, operative method, hemorrhage volume, operative duration and intraoperative mechanical ventilation duration.
Conclusions: In this retrospective cohort study, most of the factors associated with postoperative airway retention were closely related to the patient's tumor characteristics. These data demonstrate that respiratory management in patients with skull base chordoma remains an ongoing concern.
Introduction
Chordoma is a rare malignant bone and soft tissue tumor derived from embryonic notochord remnants. The incidence of chordoma has been reported as 0.08 per 100,000, with skull base chordoma accounting for ~1/3 of all chordoma cases (1, 2). Skull base chordoma is closely related to the brainstem and cranial nerves and has a high recurrence rate. The 5-year survival rate is only 60–70% (3). Chordoma is not sensitive to conventional low-dose radiation, and high-dose radiation may damage surrounding brain tissue and nerves (2, 4). Treatment of chordoma has been based on surgical resection and radiotherapy. A growing body of evidence to support the particles-ion radiotherapy is an effective treatment.
The growth rate of skull base chordoma tumors is slow, and the clinical manifestations are mainly mass effect and compression symptoms. Compression of cranial nerves by the tumor can result in preoperative neurological dysfunction, with clinical manifestations including dysphagia, choking on water, and decreased pharyngeal reflex. There are 9–12 pairs of posterior cranial nerves, including the glossopharyngeal nerve, vagus nerve, accessory nerve, and hypoglossal nerve. La Corte et al. conducted a retrospective study of 59 skull base chordoma patients and found that the preoperative clinical symptoms, tumor resection degree, surgeon's experience, and postoperative complications were significant factors affecting the prognosis (5). Additionally, long-term artificial airway (AA) retention may lead to pulmonary complications such as respiratory infection. However, in the case of damage to the posterior cranial nerves, early active extubation can lead to aspiration pneumonia due to the weakened protective airway reflex and increase the incidence of perioperative pulmonary complications. Therefore, choosing the appropriate endotracheal extubation time is particularly important. To date, there have been no studies on predictors of postoperative AA retention in patients with skull base chordoma.
This study aimed to explore predictors of postoperative AA retention in patients with skull base chordoma using retrospective observational data from Beijing Tiantan Hospital. We also aimed to investigate the influence of the timing of tracheal extubation on perioperative pulmonary complications.
Materials and methods
This was a single-center, retrospective cohort study conducted at Beijing Tiantan Hospital. The trial protocol was approved by the Clinical Research Ethics Committee of Beijing Tiantan Hospital (approval no. KY2021-112-02), and the requirement for informed consent was waived.
Participants
The study population included all skull base chordoma patients undergoing surgical treatment between January 2019 and December 2021 at Beijing Tiantan Hospital. Patients younger than 18 years of age and patients without anesthesia records were excluded.
Data collection and outcome assessment
All patients underwent standardized preoperative preparation according to our hospital. Anticoagulants and antiplatelet drugs were discontinued for a specified period of time and heparin bridging therapy was performed as needed. Baseline data included demographic characteristics, preoperative comorbidities, smoking and alcohol history, and laboratory test results. Intraoperative data included the types and doses of anesthetics/medications, vital signs, fluid balance and blood transfusions, intraoperative mechanical ventilation duration, and operative duration. In addition, unplanned secondary endotracheal intubation and unplanned secondary operations were recorded. The patients were divided into two groups according to whether the AA was retained postoperatively: patients with AA retention (AA group) and without AA retention (WOAA group). AAs included those present after oral endotracheal intubation, nasal endotracheal intubation, and tracheotomy. Tumor diameter was measured by a senior professional radiologist based on enhanced magnetic resonance imaging of the head.
The primary outcome was the incidence of postoperative pulmonary complications. The definition of perioperative pulmonary complications included respiratory infection, respiratory failure, pleural effusion, atelectasis, pneumothorax, bronchospasm, and aspiration pneumonia. The Clavien–Dindo classification was used to categorize pulmonary lesions. Complications of grade II or above were used to calculate the incidence rate (6). Secondary outcomes included the incidence of extrapulmonary complications, postoperative length of hospital stay, postoperative length of intensive care unit (ICU) stay, and rate of unplanned secondary endotracheal intubation. Postoperative extrapulmonary complications were defined as new events outside the respiratory system, including neurovascular complications (stroke, transient ischemic accident), cardiovascular complications (acute coronary syndrome, circulatory insufficiency, congestive heart failure, new-onset arrhythmia), thromboembolic complications (pulmonary embolism, deep venous thrombosis), gastrointestinal complications (gastrointestinal hemorrhage, acute pancreatitis, ileus), surgical complications (surgical-site infection, surgical bleeding), infectious complications (sepsis, septic shock), and liver and kidney complications (acute hepatic injury, acute kidney injury) (6). The diagnosis of all postoperative complications was confirmed by two senior specialists. Surgical site infection is defined as infection related to an operative procedure, occurred at or near the surgical incision within 30 days of the procedure or cerebrospinal fluid tests confirm an intracranial infection (6). A poor prognosis was defined as death during hospitalization or Glasgow score of eight or less at discharge.
Statistical analysis
EmpowerStats software and R software (R version 4.2.0) were used for statistical analysis. The Kolmogorov–Smirnov test was applied for continuous variables with a normal distribution. Data conforming to a normal distribution are represented as the mean ± standard deviation (SD). Nonnormally distributed data are expressed as medians and interquartile ranges. The independent T-test or Mann–Whitney U test was performed according to the data distribution. Classification variables are expressed as a percentage and were analyzed using the chi-square test or Fisher's exact test. Based on the univariate logistic regression analysis, possible factors influencing postoperative pulmonary complications were found, and variables with a P < 0.05 were included in the multiple regression analysis. By logistic regression, odds ratios (ORs) and 95% confidence intervals (CIs) were calculated to evaluate the factors associated with postoperative AA retention. According to the multivariate analysis, continuous variables related to postoperative AA retention were selected to draw receiver operating characteristic (ROC) curves. P < 0.05 was considered statistically significant.
Results
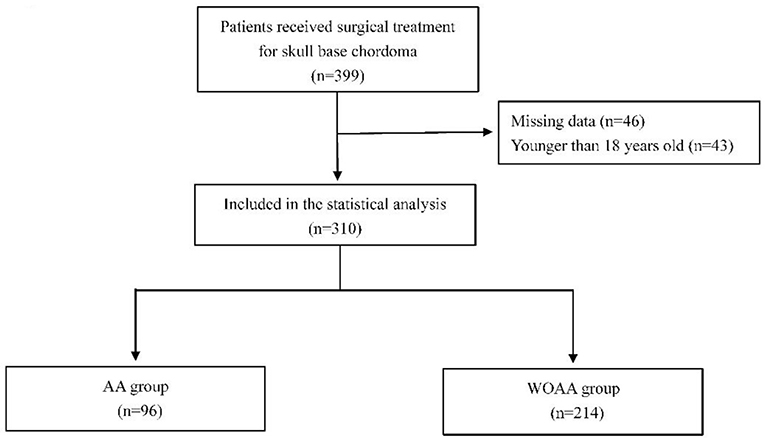
From January 2019 to December 2021, 399 patients underwent surgical treatment for skull base chordoma at Beijing Tiantan Hospital. Among them, 43 patients were younger than 18 years, and anesthesia data were unavailable for 46 patients. Thus, a total of 310 patients were included in the statistical analysis (Figure 1).
Patient characteristics
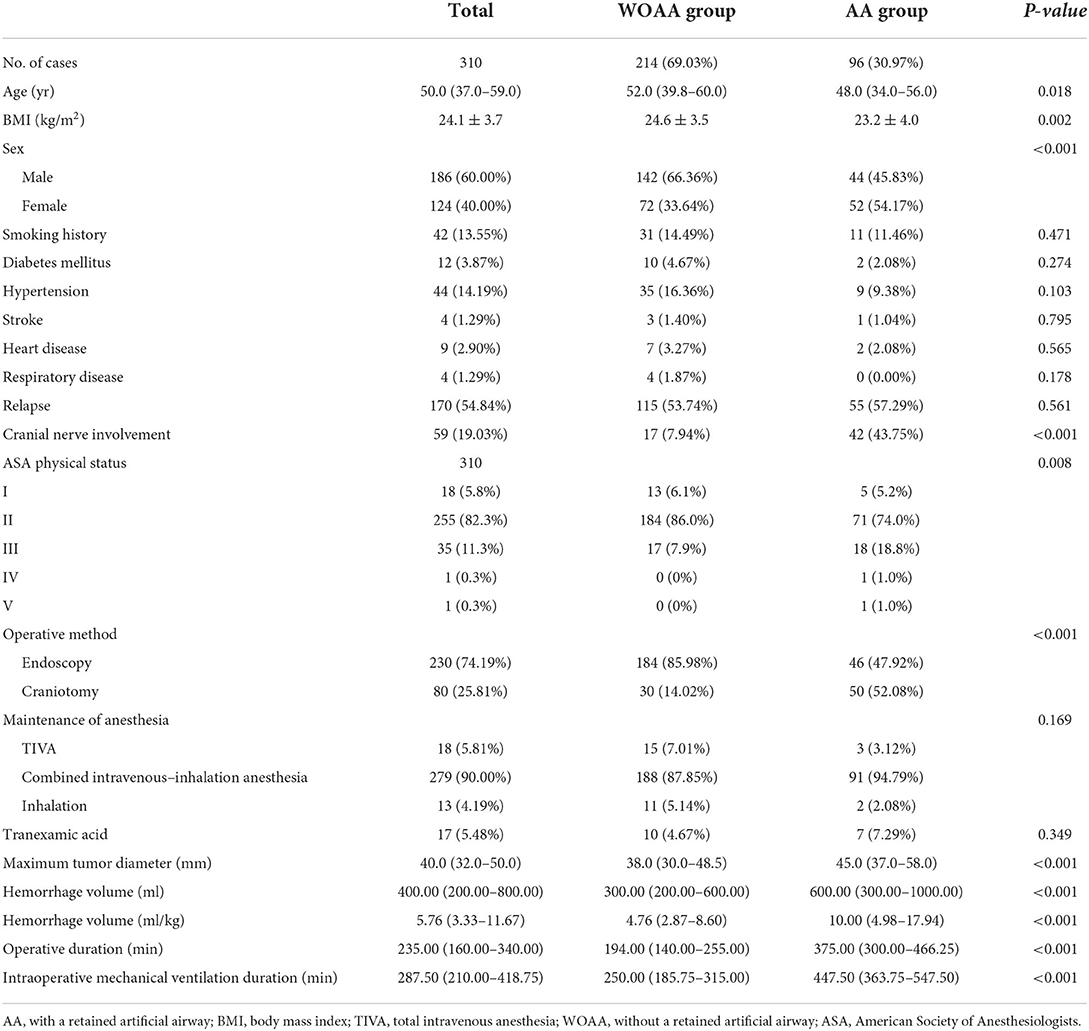
The baseline characteristics of the patients in the two groups are shown in Table 1. There were no significant differences between the two groups in terms of smoking history, diabetes mellitus, hypertension, stroke history, heart disease, respiratory disease, recurrence, or maintenance of anesthesia. The operative duration, intraoperative mechanical ventilation duration, maximum tumor diameter, and hemorrhage volume were significantly greater in those with than those without AA retention. In addition, there were significant differences in age, body mass index (BMI), sex, posterior cranial nerve involvement, ASA physical status and the operative method between the two groups.
Postoperative outcomes
In this study, we found that the rate of AA retention after surgery for skull base chordoma was 30.97%; buccal endotracheal intubation was maintained in 55 patients, nasal endotracheal intubation in 22 patients, and tracheotomy in 19 patients.
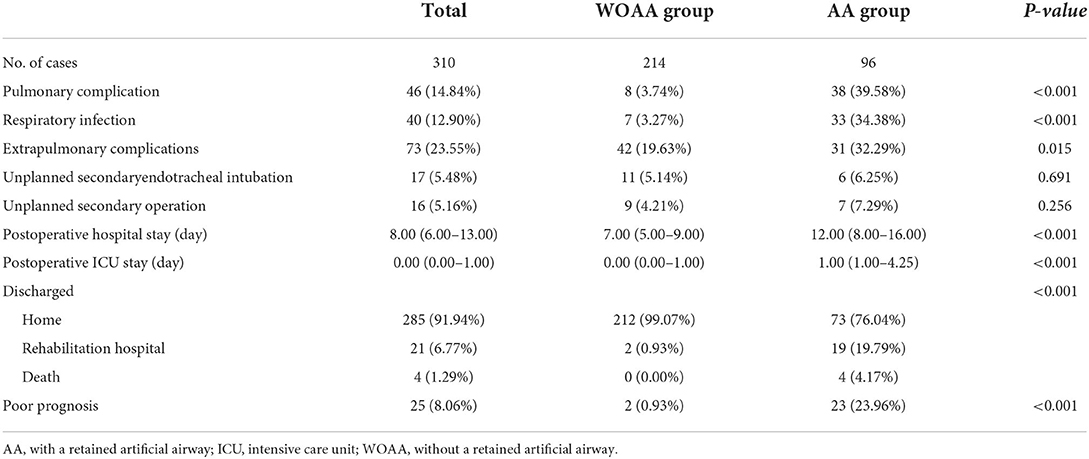
The outcomes of the patients are shown in Table 2. In this study, 46 patients developed perioperative pulmonary complications, including 38 patients with AA retention and eight without AA retention. The incidence of postoperative pulmonary complications was much lower in those without AA retention (3.74 vs. 39.58%, P < 0.001). The incidence of postoperative extrapulmonary complications was 32.29 and 19.63% in those with and without AA retention, respectively (P = 0.015). Both the length of postoperative hospital stay and the length of ICU stay were extended in the AA group (P < 0.001). There were two patients (0.93%) with an unfavorable prognosis in the WOAA group and 23 patients (23.96%) in the AA group (P < 0.001).
There was no significant difference between the two groups in terms of unplanned secondary endotracheal intubation and unplanned secondary surgery. Six patients in the AA group underwent secondary endotracheal intubation; causes of secondary endotracheal intubation included dyspnea, poor cough reflex, and respiratory infection. Eleven patients in the WOAA group underwent secondary endotracheal intubation; reasons for endotracheal intubation included the need for a second operation, postoperative local cerebral edema, reflux aspiration, and pulmonary infection. Of the 17 patients who underwent secondary endotracheal intubation, one died, and seven had a poor prognosis and required continued treatment in the rehabilitation hospital.
The artificial airway was retained for 20 h (15–219 h) after operation. The patients who retained the artificial airway after operation were divided into two groups: those who retained the artificial airway for <24 h after operation were in the short-term group, and the others were in the long-term group. There were 50 people in the short-term group and 46 people in the long-term group. Short-term group of postoperative artificial airway retention time is 15.5 h (13.0–17.0 h), long-term group is 230.0 h (144.8–321.0 h).
Predictors associated with postoperative AA retention
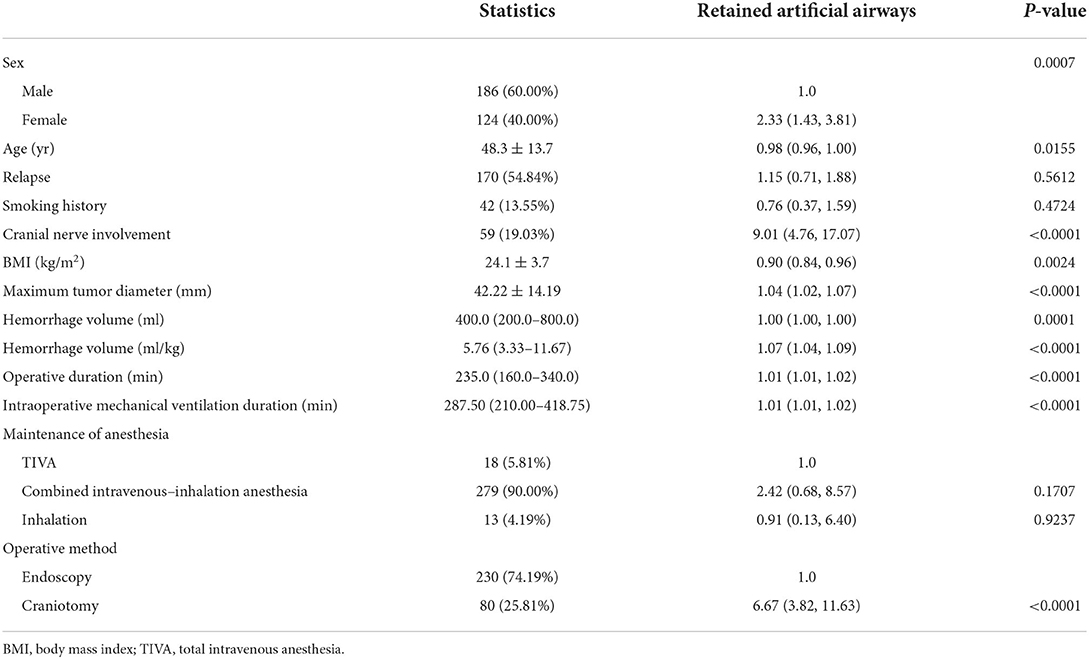
Univariate analysis showed that women were more likely than men to require AA retention postoperatively (OR = 2.33, 95% CI: 1.43–3.81; P = 0.0007). Patients with cranial nerve involvement were also more likely to require AA retention postoperatively (OR = 9.01, 95% CI: 4.76–17.07; P < 0.0001). Compared with endoscopic surgery, patients who underwent craniotomy had a higher risk of postoperative AA retention (OR = 6.67, 95% CI: 3.82–11.63; P < 0.0001) (Table 3). In addition, the maximum tumor diameter, intraoperative hemorrhage volume, operative duration, and intraoperative mechanical ventilation duration were related to postoperative AA retention.
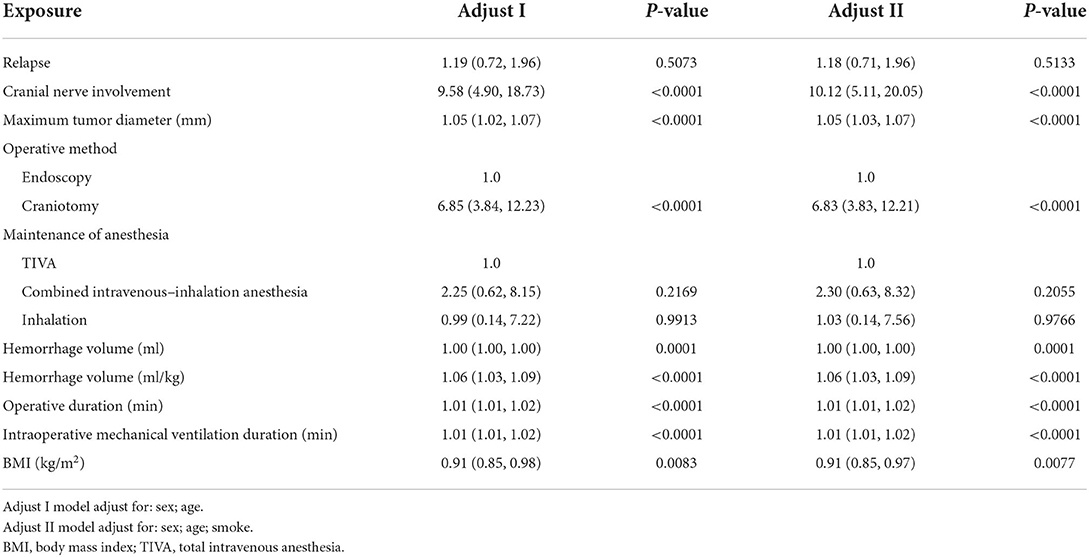
Two multifactor analysis models were established (Table 4). Model one was adjusted for sex and age, while model two was adjusted for sex, age, and smoking history. After adjusting for potential confounding factors, the multivariate analysis showed that BMI (OR = 0.91, 95% CI: 0.85–0.97; P = 0.0077), cranial nerve involvement (OR = 10.12, 95% CI: 5.11–20.05; P < 0.0001), maximum tumor diameter (OR = 1.05, 95% CI: 1.03–1.07; P < 0.0001), operative method (OR = 6.85, 95% CI: 3.84–12.21; P < 0.0001), hemorrhage volume (OR = 1.06, 95% CI: 1.03–1.09; P < 0.0001), operative duration (OR = 1.01, 95% CI: 1.01–1.02; P < 0.0001), and intraoperative mechanical ventilation duration (OR = 1.01, 95% CI: 1.01–1.02; P < 0.0001) were all associated with postoperative AA retention.
According to the multivariate analysis, continuous variables related to AA retention were selected for ROC curve analysis, and the results are shown in Figure 2. The area under the ROC curve (AUC) of the BMI was 0.61 (95% CI: 0.54–0.67). When the optimal threshold was 22.64, the specificity was 0.74, and the sensitivity was 0.49. The AUC of the maximum tumor diameter was 0.66 (95% CI: 0.59–0.73), with a specificity and sensitivity of 0.68 and 0.63, respectively, when the optimal threshold was 43.50 mm. The AUC of the operative duration was 0.85 (95% CI: 0.81–0.89), with a specificity and sensitivity of 0.83 and 0.83, respectively, when the optimal threshold was 282.50 min. The AUC of the intraoperative mechanical ventilation duration was 0.86 (95% CI: 0.82–0.91), with a specificity and sensitivity of 0.83 and 0.85, respectively, when the optimal threshold was 343.50 min. The AUC of the hemorrhage volume was 0.71 (95% CI: 0.64–0.77), when the optimal cutoff point was 8.63 ml/kg, with a specificity of 0.75 and sensitivity of 0.58.
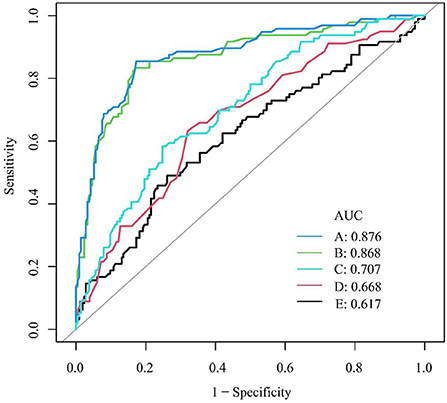
Figure 2. ROC curve for AA retention. (A) Duration of intraoperative mechanical ventilation (min); (B) operative duration (min); (C) hemorrhage volume (ml/kg); (D) maximum tumor diameter (mm); (E) BMI (kg/m2). AUC, area under the ROC curve; BMI, body mass index; ROC, receiver operating characteristic.
Discussion
Chordoma is a rare malignant and aggressive tumor with a poor prognosis. Skull base chordomas are often more complex than other chordomas (7, 8). This study retrospectively analyzed the incidence of postoperative pulmonary complications in patients with skull base chordoma and explored the risk factors for postoperative AA retention. Among them, 30.97% of patients required postoperative AA retention, which was found to be associated with an increased frequency of pulmonary complications and a poor prognosis. The results of this study are consistent with those of studies of nonneurosurgical patients (9–12). Prolonged AA retention can lead to complications, including lung infection, glottis narrowing, and difficulty swallowing (13). Postoperative pulmonary complications are also associated with an increased mortality rate, length of hospital stay, and cost of hospitalization (14–19).
In neurosurgical patients, prolonged surgery, substantial hemorrhage, diabetes mellitus, chronic obstructive pulmonary disease, preoperative leukocytosis, ASA≥3 classification, and skull base occupation are risk factors for postoperative pneumonia (20). Additionally, symptoms of cranial nerve involvement, prolonged surgery, long-term mechanical ventilation, decreased postoperative consciousness, and skull base surgery increase the incidence of pulmonary complications in neurosurgical patients during the perioperative period (21, 22). Furthermore, postoperative blood transfusions, posterior cranial nerve compression, prolonged ICU stay, and tracheotomy are independent predictors of postoperative pulmonary complications in skull base surgery (20). Furthermore, postoperative pulmonary complications are significantly associated with a poorer prognosis, including higher rates of secondary surgery, readmission, mortality, and extended hospitalization, after craniocerebral tumor surgery (20).
Retained AAs and mechanical ventilation can provide direct access to the lungs for pathogens and reduce the immune barrier function of the mucosa, which may increase the risk of postoperative pulmonary complications (10). We identified several risk factors for perioperative AA retention, and the possibility of AA retention is considerable for patients with specific characteristics. Posterior cranial nerve involvement, craniotomy for chordoma resection, BMI > 22.64 kg/m2, maximum tumor diameter > 43.5 mm, operative duration > 282.50 min, intraoperative mechanical ventilation duration > 343.50 min, and hemorrhage volume > 8.63 ml/kg were all independent risk factors for postoperative AA retention. Considering that most factors related to AA retention are tumor characteristics, few factors can be actively addressed. Therefore, clinical work may focus on reducing the incidence of pulmonary complications in high-risk patients who require AA retention. A meta-analysis of 178 randomized controlled studies found that exercise interventions and inspiratory muscle training reduced perioperative pulmonary complications in patients undergoing elective major surgery (23). Laurent et al. found that preoperative ventilator endurance training could improve respiratory muscle endurance and reduce the incidence of postoperative pulmonary complications (24).
More than 20% of complications in respiratory management occur during extubation, with severe consequences, including hypoxia and death (13). Although many guidelines focus on endotracheal intubation, there is limited literature on endotracheal extubation at the end of surgery. At the end of the surgery, endotracheal extubation or AA retention is necessary according to the patient's specific situation. In patients with skull base chordoma, cranial nerve involvement results in impaired cranial nerve function and poor protective airway reflexes. Therefore, caution is needed when considering whether to retain AAs. In addition, surgeons should minimize the operative duration and hemorrhage volume, and anesthetists should refine perioperative airway management methods. There are some limitations to this study. First, this was a single-center, retrospective study, and we could only determine the patient's condition through medical records. In addition, we could not collect intraoperative mechanical ventilation parameters, including the tidal volume, respiratory rate, airway pressure, and other data. Previous randomized controlled studies have found no significant difference in the incidence of pulmonary complications 7 days after surgery between adults patients ventilated with a low intraoperative tidal volume and those ventilated with a conventional tidal volume (25). There were significant differences in maximum tumor diameter, hemorrhage volume, operative duration, and intraoperative mechanical ventilation duration between the two groups. The above factors will affect the postoperative status of patients, making patients more sensitive to infection and other complications. It is difficult to draw a firm line between these factors as direct causes of poor prognosis or as reasons for the preservation of the artificial airway after surgery. However, the results of this study need to be validated by large prospective studies.
Conclusion
Postoperative AA retention in patients with skull base chordoma is associated with an increased incidence of pulmonary complications in the perioperative period. BMI, tumor compression of posterior cranial nerves, maximum tumor diameter, operative method, intraoperative hemorrhage volume, operative duration, and intraoperative mechanical ventilation duration are independent predictors of postoperative AA retention.
Data availability statement
The raw data supporting the conclusions of this article will be made available by the authors, without undue reservation.
Author contributions
All authors listed have made a substantial, direct, and intellectual contribution to the work and approved it for publication.
Funding
This study was supported by funding from Special Funding Support for Clinical Medicine Development (ZYLX201708 and DFL20180502) and the Beijing Municipal Science and Technology Commission (Z19110700660000).
Conflict of interest
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
Publisher's note
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
References
1. Bai J, Li M, Shi J, Jing L, Zhai Y, Zhang S, et al. Mid-term follow-up surgical results in 284 cases of clival chordomas: the risk factors for outcome and tumor recurrence. Neurosurg Rev. (2022) 45:1451–62. doi: 10.1007/s10143-021-01576-4
2. Teng C, Yang Q, Xiong Z, Ye N, Li X. Multivariate analysis and validation of the prognostic factors for skull base chordoma. Front Surg. (2021) 8:764329. doi: 10.3389/fsurg.2021.764329
3. Snyderman CH, Gardner PA. Current opinion in otolaryngology and head and neck surgery: clival chordoma and its management. Curr Opin Otolaryngol Head Neck Surg. (2020) 28:118–21. doi: 10.1097/MOO.0000000000000614
4. Li M, Shen Y, Xiong Y, Wang S, Li C, Bai J, et al. Loss of SMARCB1 promotes autophagy and facilitates tumour progression in chordoma by transcriptionally activating ATG5. Cell Prolif. (2021) 54:e13136. doi: 10.1111/cpr.13136
5. La Corte E, Broggi M, Raggi A, Schiavolin S, Acerbi F, Danesi G, et al. Peri-operative prognostic factors for primary skull base chordomas: results from a single-center cohort. Acta Neurochir. (2021) 163:689–97. doi: 10.1007/s00701-020-04219-7
6. Yan T, Liang XQ, Wang GJ, Wang T, Li WO, Liu Y, et al. Prophylactic penehyclidine inhalation for prevention of postoperative pulmonary complications in high-risk patients: a double-blind randomized trial. Anesthesiology. (2022) 136:551–66. doi: 10.1097/ALN.0000000000004159
7. Tian K, Zhang H, Ma J, Wang K, Ru X, Du J, et al. Factors for overall survival in patients with skull base chordoma: a retrospective analysis of 225 patients. World Neurosurg. (2017) 97:39–48. doi: 10.1016/j.wneu.2016.09.055
8. Rock AK, Opalak CF, Workman KG, Broaddus WC. Safety outcomes following spine and cranial neurosurgery: evidence from the national surgical quality improvement program. J Neurosurg Anesthesiol. (2018) 30:328–36. doi: 10.1097/ANA.0000000000000474
9. Gal J, Hunter S, Reich D, Franz E, DeMaria S, Neifert S, et al. Delayed extubation in spine surgery is associated with increased postoperative complications and hospital episode-based resource utilization. J Clin Anesth. (2022) 77:110636. doi: 10.1016/j.jclinane.2021.110636
10. Xu Y, Zuo Y, Zhou L, Hao X, Xiao X, Ye M, et al. Extubation in the operating room results in fewer composite mechanical ventilation-related adverse outcomes in patients after liver transplantation: a retrospective cohort study. BMC Anesthesiol. (2021) 21:286. doi: 10.1186/s12871-021-01508-1
11. McCarthy C, Fletcher N. Early extubation in enhanced recovery from cardiac surgery. Crit Care Clin. (2020) 36:663–74. doi: 10.1016/j.ccc.2020.06.005
12. Harris KC, Holowachuk S, Pitfield S, Sanatani S, Froese N, Potts JE, et al. Should early extubation be the goal for children after congenital cardiac surgery? J Thorac Cardiovasc Surg. (2014) 148:2642–7. doi: 10.1016/j.jtcvs.2014.06.093
13. Anastasian ZH, Kim M, Heyer EJ, Wang S, Berman MF. Attending handoff is correlated with the decision to delay extubation after surgery. Anesth Analg. (2016) 122:758–64. doi: 10.1213/ANE.0000000000001069
14. Fernandez-Bustamante A, Frendl G, Sprung J, Kor DJ, Subramaniam B, Ruiz RM, et al. Postoperative pulmonary complications, early mortality, and hospital stay following noncardiothoracic surgery: a multicenter study by the perioperative research network investigators. JAMA Surg. (2017) 152:157–66. doi: 10.1001/jamasurg.2016.4065
15. Shander A, Fleisher LA, Barie PS, Bigatello LM, Sladen RN, Watson CB. Clinical and economic burden of postoperative pulmonary complications: patient safety summit on definition, risk-reducing interventions, and preventive strategies. Crit Care Med. (2011) 39:2163–72. doi: 10.1097/CCM.0b013e31821f0522
16. Marseu K, Slinger P. Peri-operative pulmonary dysfunction and protection. Anaesthesia. (2016) 71 Suppl 1:46–50. doi: 10.1111/anae.13311
17. Boden I, Skinner EH, Browning L, Reeve J, Anderson L, Hill C, et al. Preoperative physiotherapy for the prevention of respiratory complications after upper abdominal surgery: pragmatic, double blinded, multicentre randomised controlled trial. BMJ. (2018) 360:j5916. doi: 10.1136/bmj.j5916
18. Numata T, Nakayama K, Fujii S, Yumino Y, Saito N, Yoshida M, et al. Risk factors of postoperative pulmonary complications in patients with asthma and COPD. BMC Pulm Med. (2018) 18:4. doi: 10.1186/s12890-017-0570-8
19. Longo M, Agarwal V. Postoperative pulmonary complications following brain tumor resection: a national database analysis. World Neurosurg. (2019) 126:e1147–54. doi: 10.1016/j.wneu.2019.03.058
20. Zhao DW, Zhao FC, Zhang XY, Wei KY, Jiang YB, Liu D, et al. Association between postoperative hypoalbuminemia and postoperative pulmonary imaging abnormalities patients undergoing craniotomy for brain tumors: a retrospective cohort study. Sci Rep. (2022) 12:64. doi: 10.1038/s41598-021-00261-2
21. Zhang L, Xiong W, Peng Y, Zhang W, Han R. The effect of an intraoperative, lung-protective ventilation strategy in neurosurgical patients undergoing craniotomy: study protocol for a randomized controlled trial. Trials. (2018) 19:85. doi: 10.1186/s13063-018-2447-4
22. Sogame LC, Vidotto MC, Jardim JR, Faresin SM. Incidence and risk factors for postoperative pulmonary complications in elective intracranial surgery. J Neurosurg. (2008) 109:222–7. doi: 10.3171/JNS/2008/109/8/0222
23. Perry R, Herbert G, Atkinson C, England C, Northstone K, Baos S, et al. Pre-admission interventions (prehabilitation) to improve outcome after major elective surgery: a systematic review and meta-analysis. BMJ Open. (2021) 11:e050806. doi: 10.1136/bmjopen-2021-050806
24. Laurent H, Aubreton S, Galvaing G, Pereira B, Merle P, Richard R, et al. Preoperative respiratory muscle endurance training improves ventilatory capacity and prevents pulmonary postoperative complications after lung surgery. Eur J Phys Rehabil Med. (2020) 56:73–81. doi: 10.23736/S1973-9087.19.05781-2
25. Karalapillai D, Weinberg L, Peyton P, Ellard L, Hu R, Pearce B, et al. Effect of intraoperative low tidal volume vs conventional tidal volume on postoperative pulmonary complications in patients undergoing major surgery: a randomized clinical trial. JAMA. (2020) 324:848–58. doi: 10.1001/jama.2020.12866
Keywords: chordoma, artificial airway, postoperative pulmonary complications, anesthesiology, perioperative
Citation: Fu Y, Yu Y, Cui Y, Wang J, Ma B, Jian M, Yao J, Jing L, Bai J and Han R (2022) Factors associated with artificial airway retention after skull base chordoma resection: A retrospective cohort study. Front. Neurol. 13:992308. doi: 10.3389/fneur.2022.992308
Received: 12 July 2022; Accepted: 23 August 2022;
Published: 09 September 2022.
Edited by:
Shaan M. Raza, University of Texas MD Anderson Cancer Center, United StatesReviewed by:
Ziya Levent Gokaslan, Brown University, United StatesYongyu Yang, Southern Medical University, China
Copyright © 2022 Fu, Yu, Cui, Wang, Ma, Jian, Yao, Jing, Bai and Han. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Ruquan Han, cnVxdWFuLmhhbkBjY211LmVkdS5jbg==
†These authors have contributed equally to this work
 Yuxuan Fu
Yuxuan Fu Yun Yu1†
Yun Yu1† Minyu Jian
Minyu Jian Jiwei Bai
Jiwei Bai Ruquan Han
Ruquan Han