- 1Leidos, San Diego, CA, United States
- 2Deployment Health Research Department, Naval Health Research Center, San Diego, CA, United States
Introduction: Although previous research suggests that overpressure exposure from either high-level blast (HLB) or low-level blast (LLB) are harmful to health, to date no large-scale studies with representative samples of military personnel have utilized prospective designs and self-reported measures to examine the relationships between blast exposure and health conditions. To address these limitations, this analysis of data from the Millennium Cohort Study (MCS), the largest and longest running study of U.S. service members and veterans, examined (1) whether single or repeated HLB exposure is associated with self-reported diagnoses of illness and injury, (2) whether repeated HLB is associated with greater risk than single HLB, (3) potential adverse consequences of LLB exposure using military occupation as a proxy, and (4) the combined effects of single or repeated HLB and LLB exposure.
Method: MCS participants who completed the 2011–2013 survey (N = 138,949) were classified as having been exposed to “no,” “single,” or “repeated” HLB exposure, and into low or high risk of exposure to LLB based on occupation. Participants self-reported diagnosis of 45 medical conditions; newly reported diagnoses were regressed on single and repeated (vs. no) HLB, occupational risk of LLB, and relevant interactions using logistic regression.
Results: Single and repeated HLB were associated with new onset of 25 and 29 diagnoses, respectively; repeated HLB exposure was associated with greater risk than single HLB exposure for five diagnoses (e.g., PTSD, depression). Occupational risk of LLB was associated with 11 diagnoses (e.g., PTSD, significant hearing loss). Additionally, 14 significant interactions were detected across 11 diagnoses.
Discussion: Findings suggest that overpressure exposure (including single HLB, repeated HLB, and occupational risk of LLB) may increase the risks of self-reporting clinical diagnoses of PTSD, hearing loss, chronic fatigue syndrome, neuropathy-caused reduced sensation in the hands and feet, depression, vision loss, sinusitis, reflux, and anemia. Furthermore, the combination of HLB and LLB exposure may be associated with greater risk of migraines, PTSD, and impaired fecundity. These findings provide further evidence of the potential adverse consequences associated with overpressure exposure and underscore the necessity of public health surveillance initiatives for blast exposure and/or safety recommendations for training and operational environments.
1. Introduction
Members of the U.S. Armed Forces may be exposed to blast, also known as overpressure, as part of their routine occupational duties (1–3). Blast overpressure exposure can come from either incoming munitions (e.g., improvised explosive devices) or outgoing munitions (e.g., Carl Gustaf recoilless rifle) (4). Research to date suggests that both forms of blast overpressure exposure are harmful to health (1, 2, 5).
High-level blast (HLB) refers to overpressure generated by incoming munitions and was identified as the leading cause of deployment-related injuries, morbidity, and mortality during the Global War on Terror (4, 6, 7). A greater number of service members returned from combat deployments with mild to severe HLB-induced injuries that were ultimately not fatal due to advances in personal protective equipment and combat casualty care (8). Furthermore, as treatment of HLB-related injuries improved over time, more warfighters were able to return to battle where subsequent exposures to repeated HLB may occur. Although previous research has suggested an association between HLB exposure and a range of injuries including traumatic amputation, traumatic brain injury, organ damage, lung injury, auditory injury, and adverse mental health conditions (2, 9, 10), more research is needed to understand the consequences of repetitive HLB exposure.
Low-level blast (LLB), on the other hand, refers to overpressure generated by outgoing munitions (4). Although exposure to overpressure generated by such munitions is generally lower in intensity than HLB, recent literature reviews suggest that LLB may be associated with adverse health outcomes such as subclinical neurological and auditory symptomology, particularly among service members who experience cumulative exposures due to occupational duties (e.g., instructors leading training courses) (1, 11, 12). While much of this previous research was based on small-scale studies of various training programs, epidemiological investigations suggest military occupations with repetitive LLB exposure (e.g., from firing specific weapons systems known to generate overpressure) have elevated risks of traumatic brain injury diagnoses, particularly concussion and moderate TBI, tinnitus, and other neurological and auditory symptoms (13–17).
This emerging body of research has notable limitations. Previous studies predominantly employed retrospective study designs, rarely examined the effects of both HLB and LLB simultaneously within the same statistical model, or relied on archival medical and career records (13–17). No large-scale efforts to date utilized prospective designs and self-reported measures of exposures and/or outcomes. Additionally, nearly all human studies focused exclusively on active duty populations or law enforcement personnel, which are not necessarily representative of the broader military community (1, 18). For example, Reservists and National Guard personnel regularly deploy and may be exposed to blast in training and operational environments, yet were rarely included in research to date. As the effects of LLB are hypothesized to be cumulative in nature with latent outcomes emerging with age (1, 11, 12, 19, 20), there is a need to examine the effects of overpressure exposure even after leaving military service. Furthermore, limited research to date has directly examined the distinction between single and repetitive HLB, despite earlier work suggesting that outcomes may be more severe for those with repetitive HLB exposure (21–23).
In order to address the limitations of prior work, the present research examined Millennium Cohort Study data to estimate the effects of HLB and LLB exposure, both independently and jointly, on a variety of self-reported new-onset diagnoses of illness and injury. The purpose of this exploratory research was to examine whether HLB exposure (either single or repeated) is associated with self-reported diagnoses of illness and injury, examine whether repeated HLB is associated with greater risk than single HLB, and examine the potential adverse consequences of LLB exposure using MOS as a proxy for LLB. We hypothesized that both HLB and LLB exposures would be associated with elevated risks of neurological, hearing-related, and mental health diagnoses. We further speculated that the effects of HLB may be heterogeneous across occupational risk levels of LLB. Drawing on previous research in animals and humans, we primarily expected these interactions with regard to post-traumatic stress disorder (PTSD) and migraines, respectively (1, 11–13).
2. Materials and methods
The Millennium Cohort Study is the largest and longest-running prospective health study of members of the U.S. Armed Forces (24, 25) and was designed to investigate the long-term effects of military service on service member and veteran health (25). Thorough descriptions of the Study are available elsewhere (26, 27). Briefly, the Study uses a multi-panel multi-wave design with participants representing all branches of service, components, paygrades, and occupations. After providing informed consent, participants are requested to complete a self-administered survey every 3–5 years, even after separation from service, and responses can be linked with a variety of other data sources.
2.1. Study population
The present investigation utilized data from participants enrolled in Panels 1–4 (recruited in 2001, 2004, 2007, and 2011, respectively) who completed the 2011–2013 survey data collection (henceforth referred to as 2013 survey) (N = 138,949; see Figure 1).
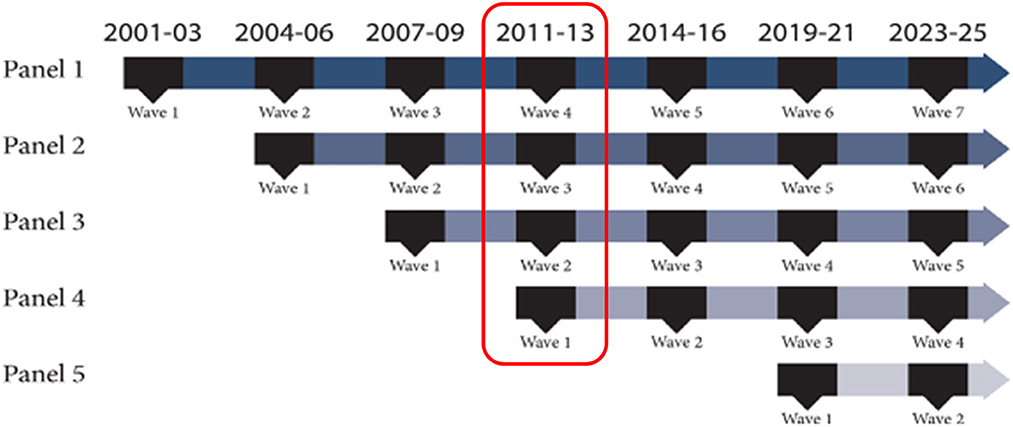
Figure 1. Depiction of the Millennium cohort study's multi-panel, multi-wave design. The red box identifies data utilized for the present research.
2.2. Measures
2.2.1. High-level blast
Exposure to HLB was first assessed in the 2013 survey. Specifically, the survey asked whether participants were ever injured from training or sports injuries, blast/explosion/bullet, and motor vehicle accident/crash. Participants indicated whether an injury occurred, occurred while deployed, and/or occurred while not deployed. If participants indicated that they were injured, they were then asked to report the total number of injury events using a two-digit textbox. Participants who indicated that they were injured from a blast/explosion/bullet while deployed and/or not deployed were categorized as having been exposed to HLB and were further categorized into groups reflecting either single or repeated HLB using the self-reported number of injury events.
2.2.2. Low-level blast
Consistent with previous research (14–17), occupational risk for LLB was determined using self-reported military occupation as a proxy. Millennium Cohort surveys assessed occupation at the time of survey completion; response options for enlisted personnel and officers or warrant officers were consistent with official DoD military occupational coding schemes, while response options for civilians were consistent with categories provided by the Bureau of Labor Statistics. Participants were categorized into high vs. low risk of repetitive LLB if they reported ever having worked in occupations determined to be high risk on any survey administered between 2001 and 2013. Enlisted high-risk occupations included infantry; armor or amphibious; combat engineering; artillery/gunnery, rockets, or missiles; air crew; seamanship; installation security; medical care; ancillary medical support; and law enforcement. Officer or Warrant Officer high-risk occupations included fixed wing fighter or bomber pilot, helicopter pilot, and aircraft crew. All remaining occupational categories, including all civilian categories, were considered low-risk occupations.
2.2.3. Self-reported diagnoses
The Millennium Cohort survey asked participants to indicate whether they had ever been told (at baseline) or in the past 3 years (at follow-up) by a doctor or other health professional that they have had any of 45 different self-reported conditions. Although we examined all available conditions for exploratory purposes, we hypothesized a priori that 11 conditions would be most likely to show associations with blast exposure (chronic fatigue syndrome, depression, significant hearing loss, manic-depressive disorder, migraine headaches, neuropathy-caused reduced sensation in hands or feet, PTSD, schizophrenia/psychosis, stroke, seizures, tinnitus/ringing of the ears).
2.3. Statistical analysis
After calculating descriptive statistics among all 2013 survey responders, the likelihood of newly self-reported physician diagnosis was regressed on frequency of self-reported HLB exposure, occupational risk of LLB, and their interaction using separate logistic regressions for each condition. Sample sizes for each analysis differed because those who reported the diagnosis on surveys administered before 2013 were excluded. Newly-reported kidney failure requiring dialysis was excluded due to a relatively small number of cases. For these analyses, single and repeated HLB were dummy coded and entered separately with no HLB exposure as the referent. Additionally, occupational risk of LLB was dummy coded with low occupational risk of LLB exposure as the referent. Finally, to assess potential effect measure modification, interaction terms between single and repeated HLB and LLB, respectively, were included in models for each health condition. When significant interactions emerged, analyses were repeated stratified by occupational risk of LLB. Additionally, logistic regression analyses were repeated where different combinations of HLB and LLB were compared against a consistent referent of no HLB exposure and low LLB risk. Analyses adjusted for sex, birth year, race, ethnicity, component, paygrade, branch of service, deployment with and without combat experience, and panel. A threshold of p ≤ 0.05 was used to determine statistical significance; analyses were conducted using IBM SPSS Software Version 25.
3. Results
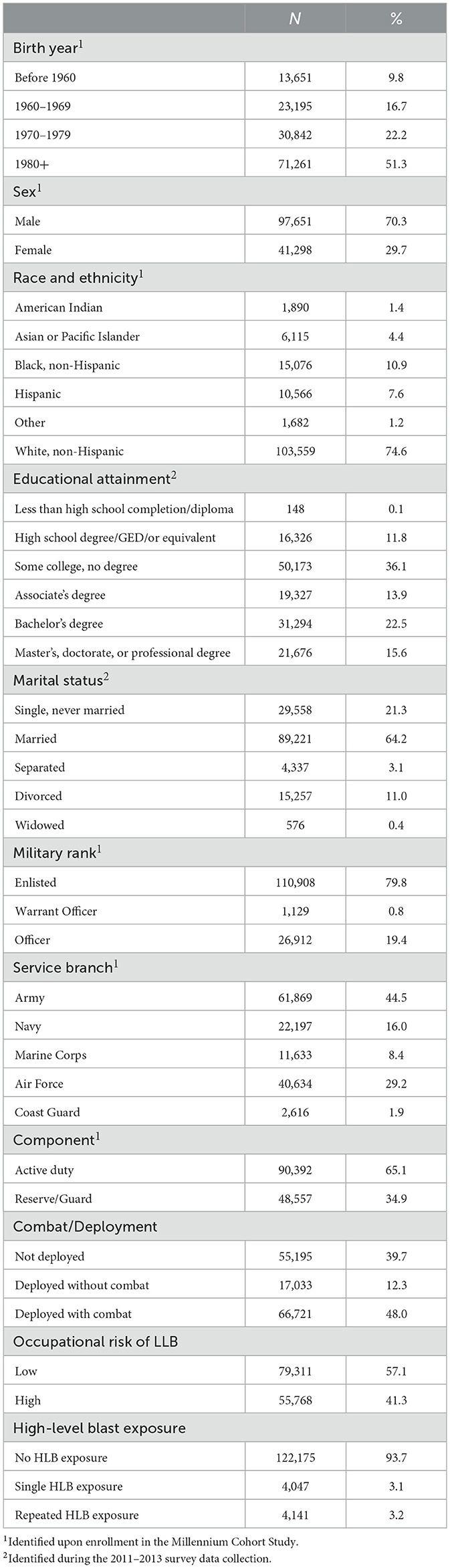
Overall, the sample was predominantly born after 1980, male, non-Hispanic White, married, served in the Army, part of the active duty component and enlisted pay grade (Table 1). Half had at least an Associate's degree as of the 2013 survey. Approximately 40% did not deploy, 12% deployed without combat, and 48% deployed with combat prior to the 2013 survey. Furthermore, 41% reported ever being in an occupation with high LLB exposure prior to or during the completion of the 2013 survey, while 3% reported single HLB and 3% reported repeated HLB exposure. The analytic sample sizes for each condition differed because of the restriction to newly-reported diagnosis (Table 2), but these overall descriptive distributions remained in the subsamples.
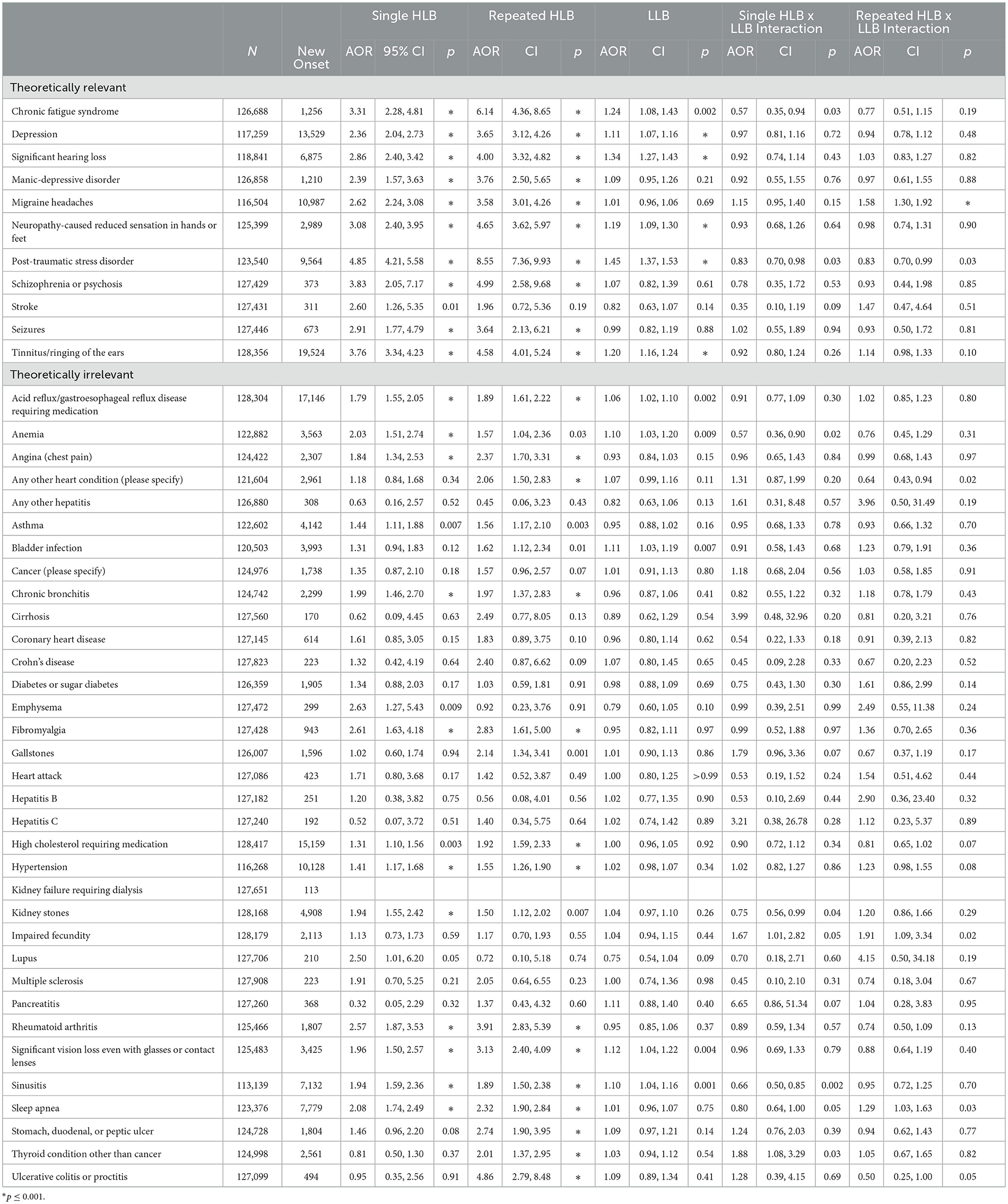
Findings are presented in order of the associations tested within each model. The five largest magnitudes of association are highlighted in the text and are occasionally supplemented with additional significant findings that were a priori hypothesized to be associated with blast exposure (see Table 2 for all adjusted associations). At least one significant association emerged for 34 of the 45 diagnoses examined, leaving 11 with no significant associations for single or repeated HLB, LLB, and their respective interactions. These 11 diagnoses included coronary heart disease, heart attack, pancreatitis, diabetes, hepatitis B, hepatitis C, any other hepatitis, cirrhosis, multiple sclerosis, Crohn's disease, and cancer.
3.1. Results for the effects of single and repeated HLB
Single HLB exposure was significantly associated with 25 of 45 self-reported diagnoses including all 11 of the conditions hypothesized a priori to be affected by blast (Table 2). The highest magnitudes of association for single vs. no HLB were observed for PTSD (adjusted odds ratio [AOR] = 4.85), schizophrenia or psychosis (3.83), tinnitus (3.76), chronic fatigue syndrome (3.31), and neuropathy-caused reduced sensation in the hands and feet (3.08). Repeated (vs. no) HLB exposure was significantly associated with 29 of 45 self-reported diagnoses and 10 of the conditions hypothesized a priori to be affected by blast. AORs for repeated HLB vs. no HLB were highest for PTSD (8.55), chronic fatigue syndrome (6.14), schizophrenia or psychosis (4.99), ulcerative colitis or proctitis (4.86), neuropathy-caused reduced sensation in the hands or feet (4.65), tinnitus (4.58), and significant hearing loss (4.00).
Of particular note, there were five significant differences between single and repeated HLB exposure (see Table 2). Repeated HLB exposure was associated with significantly greater risk than single HLB exposure for PTSD (AORsingle = 4.85, AORrepeated = 8.55), depression (AORsingle = 2.36, AORrepeated = 3.65), and high cholesterol requiring medication (AORsingle = 1.31, AORrepeated = 1.92). Additionally, whereas repeated blast exposure was significantly associated with ulcerative colitis and thyroid conditions other than cancer (AORsrepeated = 4.86 and 2.01, respectively), single HLB exposure was not.
3.2. Results for the effect of LLB
Occupational risk of LLB exposures was significantly associated with 11 of the 45 diagnoses examined, including 6 of the 11 conditions hypothesized a priori to be affected by blast. The highest magnitudes of association were observed for PTSD (1.45), significant hearing loss (1.34), chronic fatigue syndrome (1.24), tinnitus (1.20), neuropathy-caused reduced sensation in the hands and feet (1.19), significant vision loss (1.12), and depression (1.11).
3.3. Results for the interaction between HLB and LLB
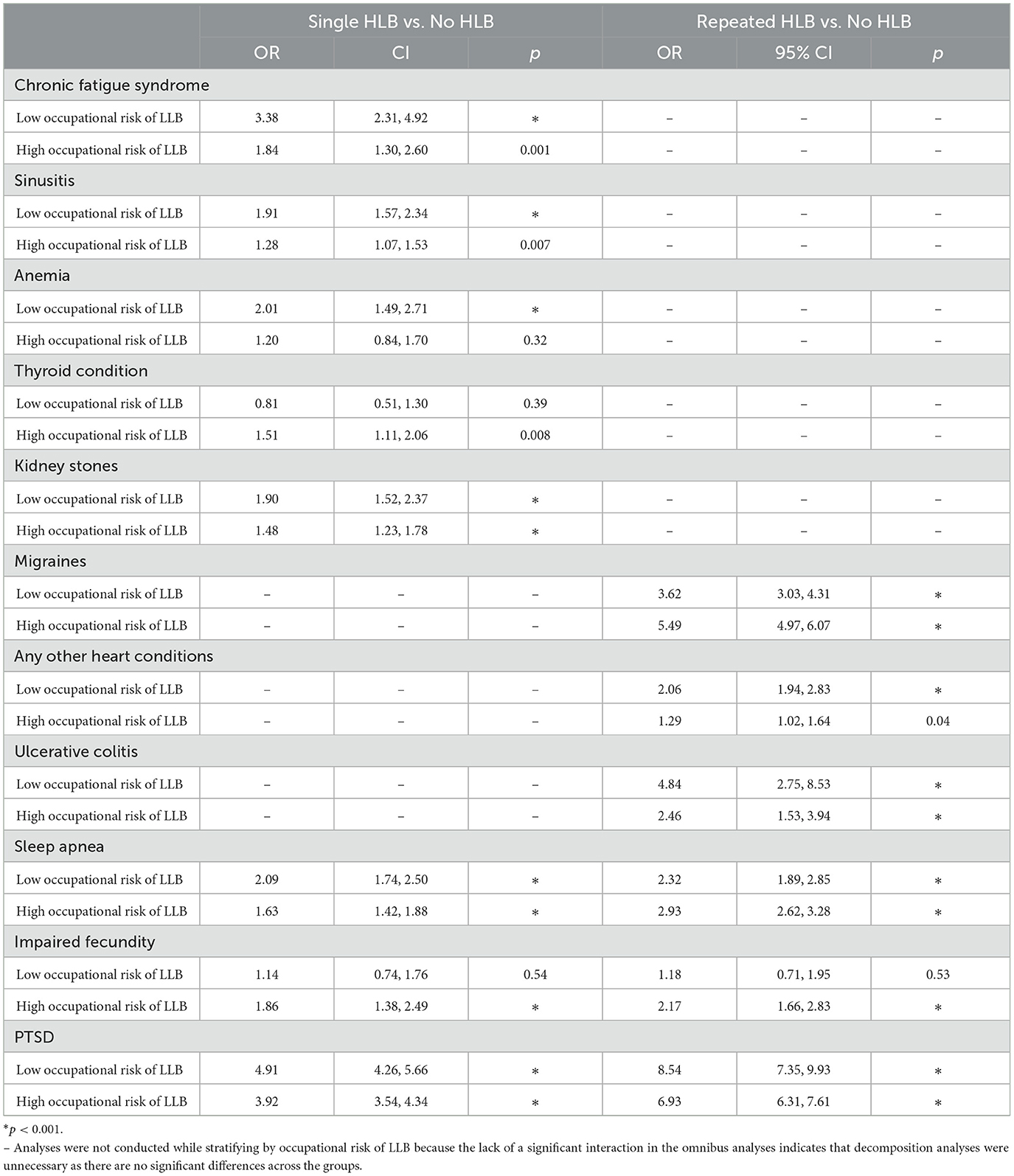
There were 14 significant interactions detected, including 8 single HLB by LLB interactions and 6 repeated HLB by LLB interactions across 11 diagnoses. Decomposition of the joint effect estimates are depicted in Table 3, which presents the AORs of single HLB vs. no HLB and repeated HLB vs. no HLB stratified by occupational risk for LLB. Table 4 presents the AORs of the combinations of blast exposure compared against a consistent referent of no HLB exposure and low LLB risk.
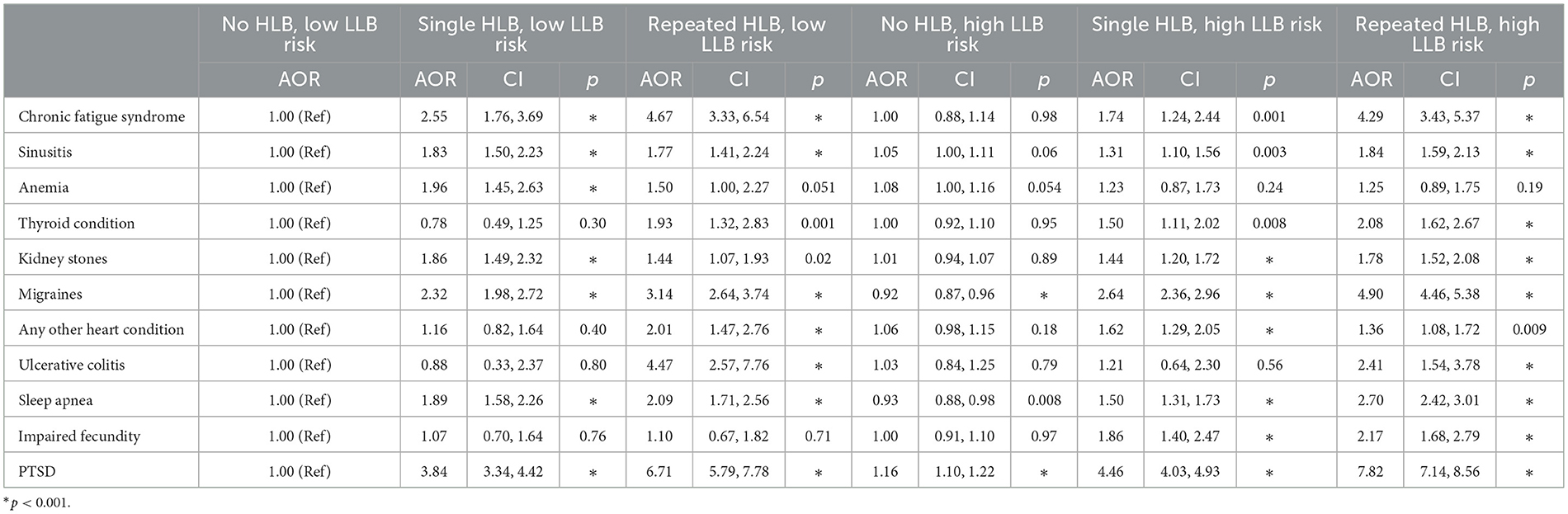
Table 4. AORs for levels of HLB and LLB exposure when compared against a consistent referent of no HLB and low LLB risk.
Significant interactions of single HLB and LLB were detected for anemia, chronic fatigue syndrome, kidney stones, sinusitis, thyroid condition, but no interactions for repeated HLB by LLB were detected for these conditions. Single (vs. no) HLB was associated with greater risk of anemia, chronic fatigue syndrome, kidney stones, and sinusitis among those in low risk occupations compared to high risk occupations. However, this pattern reversed for thyroid conditions such that single (vs. no) HLB was associated with greater risk of thyroid conditions among those in high vs. low risk occupations. However, interactions were not observed for repeated (vs. no) HLB.
Three diagnoses (any other heart conditions, migraine headaches, ulcerative colitis) had significant interactions for repeated HLB and LLB, but not single HLB and LLB. Repeated (vs. no) HLB was associated with greater risk of migraines among those in high risk compared to low risk occupations. However, any other heart conditions and ulcerative colitis showed the opposite pattern such that repeated (vs. no) HLB was associated with greater risk of these conditions among those in low vs. high risk occupations. Contrary to expectations, the joint AORs for repeated HLB and high LLB risk were not the largest AORs observed for any other heart conditions and ulcerative colitis (see Table 4).
Finally, significant interactions were detected for three diagnoses (impaired fecundity, PTSD, sleep apnea) for single (vs. no) HLB and repeated (vs. no) HLB with LLB, respectively. First, both single and repeated (vs. no) HLB were associated with greater risk of impaired fecundity among those in high-exposure occupations but not among those in low-exposure occupations. Second, the magnitudes of association for both single and repeated (vs. no) HLB on PTSD were relatively greater among those working in low vs. high risk occupations. As expected, the AORs for no, single, and repeated HLB consistently increased across both low and high LLB risk occupations. Although the AOR for high LLB risk and repeated HLB exposure was the largest AOR observed, it appeared to be lower than expected (see Table 4). Close inspection of the data suggests that prevalence of PTSD was greater among those in high risk occupations in both the presence and absence of HLB. Specifically, among those working in low-risk occupations, 4.2% of those with no HLB exposure, 24.3% of those with single HLB exposure, and 36.4% of those with repeated HLB exposure self-reported PTSD. In contrast, these numbers rise to 6.7, 30.8, 46.1%, respectively, among those working in high-risk occupations (see Figure 2). Third, for sleep apnea the effect of single (vs. no) HLB was greater for those in low- compared with high-exposure occupations. However, this pattern reversed for repeated (vs. no) HLB such that risk for sleep apnea was greater among high- vs. low-exposure occupations.
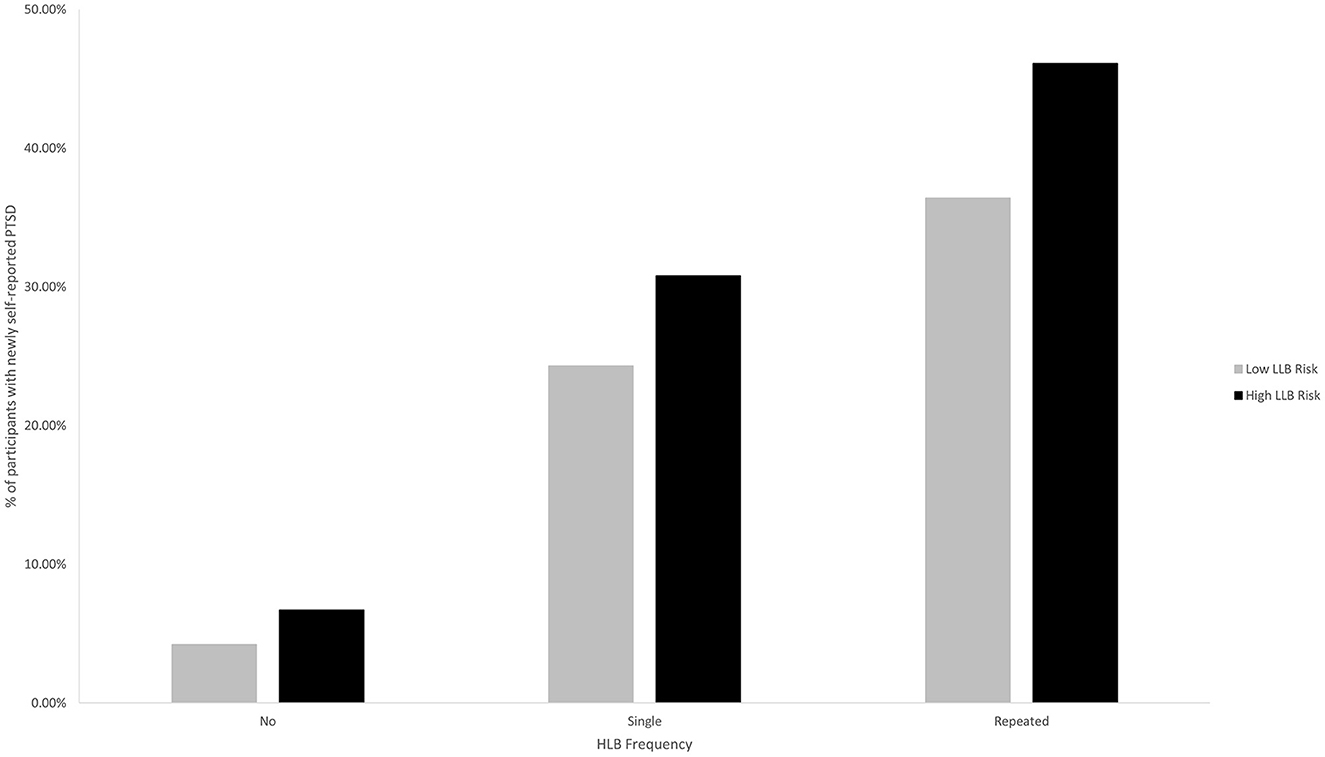
Figure 2. Percentage of participants with newly self-reported PTSD as a function of occupational risk of LLB and HLB frequency.
4. Discussion
This exploratory analysis of data from 138,949 members of the Millennium Cohort, representing active duty, Reserve, and National Guard personnel, estimated associations between single HLB, repeated HLB, and occupational risk of LLB on newly-reported diagnoses. Findings from this analysis suggest that overpressure exposure (including single HLB, repeated HLB, and occupational risk of LLB) may increase the risks of self-reporting clinical diagnoses of PTSD, hearing loss, chronic fatigue syndrome, tinnitus, neuropathy-caused reduced sensation in the hands and feet, depression, vision loss, sinusitis, reflux, and anemia. Additionally, both single and repeated HLB, but not LLB, were associated with schizophrenia, migraines, seizure, rheumatoid arthritis, fibromyalgia, manic depressive disorder, chronic bronchitis, sleep apnea, angina, hypertension, high cholesterol requiring medication, asthma, and kidney stones. Furthermore, repeated HLB was associated with greater risk above and beyond that of single HLB of PTSD, depression, high cholesterol requiring medication, ulcerative colitis, and thyroid conditions.
We were uniquely able to examine the interaction between HLB and LLB and identified interactions for eleven conditions, though we draw special attention to four here: migraines, sleep apnea, impaired fecundity, and PTSD. First, repeated (vs. no) blast exposure was associated with significantly greater risk of migraines for those working in high risk occupations compared to their lower risk counterparts. Although this association was restricted to the comparison of repeated HLB and was not replicated for single HLB, this finding extends previous research on the association between blast exposure and headaches (14, 28–32). Second, although respective interactions of single and repeated HLB and LLB were significant for sleep apnea, that the direction of the association switches for single and repeated HLB warrants caution. Third, the data suggest that although single and repeated HLB were not associated with impaired fecundity among those working in low risk occupations, those working in occupations marked by LLB were significantly more likely to report impaired fecundity following single or repeated HLB exposure. Fourth, the effect of HLB on PTSD was more pronounced among those who worked in low risk occupations, which reflects the fact that those working in high risk occupations were more likely to report PTSD in both the presence and absence of HLB.
These findings contribute to a growing body of research linking overpressure exposure with adverse health and wellbeing outcomes. As with previous research, the most consistent findings emerged primarily for conditions that were neurological, hearing-related, or mental health-related. Specifically, these findings provide yet more evidence of the association between overpressure exposure (including single HLB, repeated HLB, and occupational LLB exposure) and hearing loss and tinnitus diagnosis (1, 11–13, 17, 33–35). Additionally, this research builds on previous research reporting on the adverse reproductive health consequences of HLB in that it reports that such effects occur for those who work occupations at high (but not low) risk for occupational exposure to LLB (36, 37).
Furthermore, the current research extends previous research on the association between LLB and subclinical headaches (14, 28–32). Although there was a significant association between single and repeated HLB and migraines, occupational risk of LLB was not significantly associated with newly diagnosed migraines. This lack of a statistically significant association was surprising, but this may be an artifact of a social expectation of headaches following certain training exercises involving exposure to LLB, which may reduce service members' healthcare seeking behavior. Nonetheless, the observed interaction of LLB and repeated HLB suggests that the association between repeated HLB and migraines was stronger for those working in high (vs. low) risk occupations, providing further evidence of the association between overpressure exposure and a more severe form of headaches (38, 39).
It is also clear from previous research that exposure to HLB, which is inherently a traumatic event, is associated with increased risk of PTSD (40–42). However, the work presented herein is one of the first to suggest that exposure to repeated HLB is associated with elevated risk of PTSD compared to single HLB. Specifically, compared with those with no HLB exposure, the relative odds of reporting PTSD nearly doubled from 4.85 to 8.55 for those with single vs. repeated HLB, respectively. Furthermore, the current research extends previous findings with animals and archival medical records suggesting that occupational risk of LLB was also associated with significantly increased risk of PTSD (1, 40, 43–45). The significant interaction of HLB and LLB herein suggests that those with occupational risk of LLB may be at elevated risk for diagnoses of PTSD compared to their lower risk counterparts even in the absence of an HLB, but is more pronounced following HLB exposure. Taken together, these findings add to the growing body of evidence that overpressure exposure is associated with greater risk of PTSD, though the mechanism for this effect (e.g., physiological damage to the brain, psychological trauma, an inflammatory mechanism) has yet to be elucidated.
Whereas, previous findings with hearing loss, tinnitus, headaches/migraines, and PTSD have been clearly associated with overpressure exposure, only limited prior research has provided evidence of associations between overpressure and fatigue or depression (1, 11, 12, 46). Although prior research with animals documented an associated between overpressure and indicators of depression-like behaviors, there is not yet evidence of this pattern among humans (1, 11, 12). The current research suggests a similar pattern in humans, which may also inform our understanding of the possible associations between overpressure and suicide that has been posited elsewhere. Furthermore, this report is the first to document an association between overpressure exposure and self-reported diagnoses of chronic fatigue syndrome specifically, though again the mechanism for this effect is still unclear. For example, it is possible that subclinical symptoms arising from overpressure exposure may impair one's ability to get high-quality sleep. Alternatively, it is possible that the shockwaves associated with overpressure may damage certain regions of the brain like the thalamus, which has been implicated in sleep-wake cycles (47, 48). Given the importance of both suicide and sleep in military populations, understanding these associations more fully represents exciting avenues for future research (49–55).
4.1. Limitations
There are notable limitations that warrant mention. First, the measurement of blast exposure (both LLB and HLB) may have resulted in misclassification. For example, we used occupational risk as a proxy for repetitive exposure to LLB. However, merely working in one of these occupations at some point in one's military career does not necessarily equate to having sustained repeated exposure to LLB, nor does it allow for precise considerations of factors that might affect the relationship between such exposure and adverse health outcomes including proximity to the weapon system, type of weapon system, frequency or duration of exposure, personal protective equipment, etc. Additionally, the wording of the HLB exposure item also included exposure to bullets. It is also possible that some warfighters may have been referring to LLB exposure when self-reporting exposure to “blast/explosions.” Furthermore, the number of HLB exposures was forced to range between 0 and 99 due to survey design. Although these data were heavily skewed, it is not presumed to affect the results as logistic regression does not assume normality of predictors nor residuals (56, 57).
Second, there are several limitations associated with the use of self-reported physician diagnoses. Because of the project's exploratory nature, we examined all 45 available diagnoses and did not correct for multiple comparisons. While certain statistically significant effect estimates may be false-positive findings, we felt that this was appropriate due to the exploratory nature of the analysis. Additionally, the use of newly self-reported physician diagnoses may lead to censoring of some outcomes of interest, especially since HLB and LLB exposure was assessed on the 2011–2013 survey while participants in the first three enrollment panels had the opportunity to report on most outcomes of interest in previous surveys. The absence of validated dates of exposure limited our ability to precisely identify medical conditions that were truly new-onset. Our decision to use newly reported diagnoses (thereby excluding those who had previously reported the diagnosis) was motivated by the need to exclude prevalent conditions, but may result in underestimates of the association between blast exposure and diagnoses. Five of the conditions examined (i.e., high cholesterol requiring medication, kidney stones, acid reflux/gastroesophageal reflux disease requiring medication, tinnitus/ringing of the ears, and impaired fecundity) were added to the survey in 2011 and were thus assumed to be new-onset even though the conditions may have emerged earlier. Additionally, the present research used self-reported diagnoses by a physician rather than official medical records of diagnosis. Because we do not have precise measures of the date of blast exposure, utilization of self-reported diagnoses afforded more efficiency in examining new-onset of these medical conditions as precise dates of exposure would be necessary to identify which diagnoses onset after the exposure. Although there are several limitations associated with self-report, self-reported diagnoses in the Millennium Cohort appear to have adequate agreement with official medical records (58). Additionally, by relying on self-reported rather than official diagnoses incorporated in the medical record, the present study was able to examine outcomes among those still currently serving in the military and veterans regardless of their utilization of the VA healthcare system or other insurance coverage, which is a notable addition to previous literature.
4.2. Future work
Despite these limitations, the current research suggests that there may be adverse health outcomes associated with overpressure exposure, including single HLB exposure, repeated HLB exposure, and repetitive LLB exposure. Although the current research articulates the association between these exposures and self-reported clinical diagnoses, it would also be worthwhile to examine whether service members and veterans also report subclinical symptoms, which may drive healthcare-seeking behavior. Additionally, future research can further investigate the medical conditions noted herein using more precise measures of overpressure exposure (e.g., impulse overpressure, distance from the blast, presence of personal protective equipment). Furthermore, additional research on the long-term implications associated with both single and repeated TBIs caused by both blast exposure and direct impact to the head are warranted.
4.3. Conclusions
Taken together, the findings herein suggest that overpressure exposure increases the likelihood of several self-reported diagnoses including PTSD, hearing loss, chronic fatigue syndrome, tinnitus, neuropathy-caused reduced sensation in the hands and feet, depression, vision loss, sinusitis, reflux, and anemia. Furthermore, the data reported herein provide additional support for the idea that the combination of HLB and LLB exposure may be associated with greater risk of migraines, PTSD, and impaired fecundity, and may adversely affect performance. These findings provide further evidence of the potential adverse consequences associated with overpressure exposure and underscore the necessity of public health surveillance initiatives for blast exposure and/or safety recommendations for training and operational environments.
Data availability statement
The datasets presented in this article are not readily available because of institutional regulations protecting service member survey responses, but may be available from the corresponding author on reasonable request following receipt of appropriate regulatory approvals. Requests to access the datasets should be directed to Millennium Cohort Study Principal Investigator, RG9ELk1pbGxlbm5pdW1Db2hvcnRQSUBoZWFsdGgubWls.
Ethics statement
The study protocol was approved by the Naval Health Research Center Institutional Review Board in compliance with all applicable Federal regulations governing the protection of human subjects. Research data were derived from an approved Naval Health Research Center Institutional Review Board protocol, number NHRC.2000.0007. The patients/participants provided their written informed consent to participate in this study.
Author contributions
JB, RR, and DT contributed to the conception of the study. JB, CK, RR, and DT contributed to the design of the study. JB and CK prepared the data for analysis. JB performed the statistical analyses and wrote the first draft of the manuscript. All authors contributed to manuscript revision, read, and approved the submitted version.
Funding
This research was supported by Military Operational Medicine Research Program, Defense Health Program, and Department of Veterans Affairs, under work unit no. 60002.
Acknowledgments
JB, RR, and DT are employees of the U.S. Government. This work was prepared as part of their official duties. Title 17, U.S.C. §105 provides that copyright protection under this title is not available for any work of the U.S. Government. Title 17, U.S.C. §101 defines a U.S. Government work as work prepared by a military service member or employee of the U.S. Government as part of that person's official duties.
Conflict of interest
JB and CK were employed by Leidos.
The remaining authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
Publisher's note
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
Author disclaimer
The views expressed in this article are those of the authors and do not necessarily reflect the official policy or position of the Department of the Navy, Department of Defense, nor the U.S. Government.
References
1. Belding JN, Englert RM, Fitzmaurice S, Jackson JR, Koenig HG, Hunter MA, et al. Potential health and performance effects of high-level and low-level blast: a scoping review of two decades of research. Front Neurol. (2021) 12:628782. doi: 10.3389/fneur.2021.628782
2. Wolf SJ, Bebarta VS, Bonnett CJ, Pons PT, Cantrill SV. Blast injuries. Lancet. (2009) 374:405–15. doi: 10.1016/S0140-6736(09)60257-9
3. Cernak I, Noble-Haeusslein LJ. Traumatic brain injury: an overview of pathobiology with emphasis on military populations. J Cerebral Blood Flow Metabol. (2009) 30:255–66. doi: 10.1038/jcbfm.2009.203
4. Belding JN, Egnoto M, Englert RM, Fitzmaurice S, Thomsen CJ. Getting on the same page: consolidating terminology to facilitate cross-disciplinary health-related blast research. Front Neurol. (2021) 12:1011. doi: 10.3389/fneur.2021.695496
5. DoD Blast Injury Research Coordinating Office. FY20 Report to the Executive Agent: Prevention, Mitigation, and Treatment of Blast Injuries. Fort Detrick, MD: U.S. Army Medical Research & Development Command (2020).
6. Owens BD, Kragh JF, Wenke JC, Macaitis J, Wade CE, Holcomb JB. Combat wounds in operation iraqi freedom and operation enduring freedom. J Trauma Acute Care Surgery. (2008) 64:1011. doi: 10.1097/TA.0b013e318163b875
7. Galarneau MR, Woodruff SI, Dye JL, Mohrle CR, Wade AL. Traumatic brain injury during Operation Iraqi Freedom: findings from the United States Navy–Marine Corps Combat Trauma Registry. J Neurosurgery. (2008) 108:950–7. doi: 10.3171/JNS/2008/108/5/0950
8. Magnuson J, Leonessa F, Ling GSF. Neuropathology of explosive blast traumatic brain injury. Curr Neurol Neurosci Rep. (2012) 12:570–9. doi: 10.1007/s11910-012-0303-6
9. Hoge CW, McGurk D, Thomas JL, Cox AL, Engel CC, Castro CA. Mild traumatic brain injury in U.S. Soldiers Returning from Iraq New England. J Med. (2008) 358:453–63. doi: 10.1056/NEJMoa072972
10. Clark ME, Walker RL, Gironda RJ, Scholten JD. Comparison of pain and emotional symptoms in soldiers with polytrauma: unique aspects of blast exposure. Pain Med. (2009) 10:447–55. doi: 10.1111/j.1526-4637.2009.00590.x
11. Belanger HG, Bowling F, Yao EF. Low-level blast exposure in humans a systematic review of acute and chronic effects. J Spec Oper Med. (2020) 20:87–93. doi: 10.55460/3AC6-AX9I
12. Simmons MM, Engel CC, Hoch E, Orr P, Anderson B, Azhar GS. Neurological Effects of Repeated Exposure to Military Occupational Levels of Blast: A Review of Scientific Literature. Santa Monica, CA: RAND Corporation (2020). doi: 10.7249/RR2350
13. Belding JN, Englert R, Bonkowski J, Thomsen CJ. Occupational risk of low-level blast exposure and TBI-related medical diagnoses: a population-based epidemiological investigation (2005–2015). Int J Environ Res Public Health. (2021) 18:12925. doi: 10.3390/ijerph182412925
14. Belding JN, Fitzmaurice S, Englert RM, Koenig HG, Thomsen CJ, Olaghere da. Silva U. Self-reported concussion symptomology during deployment: differences as a function of injury mechanism and low-level blast exposure. J Neurotrauma. (2020) 37:2219–26. doi: 10.1089/neu.2020.6997
15. Belding JN, Fitzmaurice S, Englert RM, Lee I, Kowitz B, Highfill-McRoy RM, et al. Blast exposure and risk of recurrent occupational overpressure exposure predict deployment TBIs. Mil Med. (2020) 185:e538–e44. doi: 10.1093/milmed/usz289
16. Belding JN, Khokhar B, Englert RM, Fitzmaurice S, Thomsen CJ. The persistence of blast- vs. impact-induced concussion symptomology following deployment. J Head Trauma Rehabilitat. (2021) 36:E397–E405. doi: 10.1097/HTR.0000000000000715
17. Carr W, Kelley AL, Toolin CF, Weber NS. Association of MOS-based blast exposure with medical outcomes. Front Neurol. (2020) 11:619. doi: 10.3389/fneur.2020.00619
18. Military Leadership Diversity Commission. National Guard and Reserve Manpower. Arlington, VA (2010).
19. Carr W, Polejaeva E, Grome A, Crandall B, LaValle C, Eonta SE, et al. Relation of repeated low-level blast exposure with symptomology similar to concussion. J Head Trauma Rehabilitat. (2015) 30:47–55. doi: 10.1097/HTR.0000000000000064
20. Carr W, Stone JR, Walilko T, Young LA, Snook TL, Paggi ME, et al. Repeated low-level blast exposure: a descriptive human subjects study. Mil Med. (2016) 181:28–39. doi: 10.7205/MILMED-D-15-00137
21. Bryden DW, Tilghman JI, Hinds SR. Blast-related traumatic brain injury: current concepts and research considerations. J Exp Neurosci. (2019) 13:1179069519872213. doi: 10.1177/1179069519872213
22. Reid MW, Miller KJ, Lange RT, Cooper DB, Tate DF, Bailie J, et al. A multisite study of the relationships between blast exposures and symptom reporting in a post-deployment active duty military population with mild traumatic brain injury. J Neurotrauma. (2014) 31:1899–906. doi: 10.1089/neu.2014.3455
23. DePalma RG, Hoffman SW. Combat blast related traumatic brain injury (TBI): decade of recognition; promise of progress. Behav Brain Res. (2018) 340:102–5. doi: 10.1016/j.bbr.2016.08.036
24. Belding JN, Castañeda SF, Jacobson IG, LeardMann CA, Porter B, Powell TM, et al. The millennium cohort study: the first 20 years of research dedicated to understanding the long-term health of US service members and veterans. Ann Epidemiol. (2022) 67:61–72. doi: 10.1016/j.annepidem.2021.12.002
25. Chesbrough KB, Ryan MAK, Amoroso P, Boyko EJ, Gackstetter GD, Hooper TI, et al. The millennium cohort study: a 21-year prospective cohort study of 140,000 military personnel. Mil Med. (2002) 167:483–8. doi: 10.1093/milmed/167.6.483
26. Ryan MAK, Smith TC, Smith B, Amoroso P, Boyko EJ, Gray GC, et al. Millennium Cohort: enrollment begins a 21-year contribution to understanding the impact of military service. J Clin Epidemiol. (2007) 60:181–91. doi: 10.1016/j.jclinepi.2006.05.009
27. Smith B Smith TC Gray GC Ryan MAK for the Millennium Cohort Study T. When epidemiology meets the internet: web-based surveys in the millennium cohort study. Am J Epidemiol. (2007) 166:1345–54. doi: 10.1093/aje/kwm212
28. Belding JN, Jackson JR, Englert RM, Fitzmaurice S, Koenig HG, Thomsen CJ, et al. Blast Exposure, Traumatic Brain Injury, and Self-Reported Symptomology Among Active Duty Enlisted Marines: An examination of Post-Deployment Health Assessment Records, 2005–2012. Defense Technical Information Center: Naval Health Research Center (2020).
29. Ling G, Bandak F, Armonda R, Grant G, Ecklund J. Explosive blast neurotrauma. J Neurotrauma. (2009) 26:815–25. doi: 10.1089/neu.2007.0484
30. Wilk JE, Thomas JL, McGurk DM, Riviere LA, Castro CA, Hoge CW. Mild traumatic brain injury (concussion) during combat: lack of association of blast mechanism with persistent postconcussive symptoms. J Head Trauma Rehabilitat. (2010) 25:9–14. doi: 10.1097/HTR.0b013e3181bd090f
31. Tsao JW, Stentz LA, Rouhanian M, Howard RS, Perry BN, Haran FJ, et al. Effect of concussion and blast exposure on symptoms after military deployment. Neurology. (2017) 89:2010. doi: 10.1212/WNL.0000000000004616
32. Patil VK, Andre JR, Crisan E, Smith BM, Evans CT, Steiner ML, et al. Prevalence and treatment of headaches in veterans with mild traumatic brain injury headache. J Head Face Pain. (2011) 51:1112–21. doi: 10.1111/j.1526-4610.2011.01946.x
33. Modica CM, Johnson BR, Zalewski C, King K, Brewer C, King JE, et al. Hearing loss and irritability reporting without vestibular differences in explosive breaching professionals. Front Neurol. (2020) 11:588377. doi: 10.3389/fneur.2020.588377
34. Reichenbach T. Hearing Damage Through Blast. In: Bull AMJ, Clasper J, Mahoney PF. Blast Injury Science and Engineering: A Guide for Clinicians and Researchers. Cham: Springer International Publishing (2016). p. 307–14. doi: 10.1007/978-3-319-21867-0_30
35. Karch SJ, Capo-Aponte JE, McIlwain DS, Lo M, Krishnamurti S, Staton RN, et al. Hearing loss and tinnitus in military personnel with deployment-related mild traumatic brain injury. US Army Med Dep J. (2016) 52–63.
36. Hudak SJ. Genitourinary Injuries. In: Callaway DW, Burstein JL. Operational and Medical Management of Explosive and Blast Incidents. Berlin: Springer (2020). p. 465–73. doi: 10.1007/978-3-030-40655-4_33
37. Sherrie L. Wilcox, Ashley Schuyler, Hassan AM. Genitourniary Trauma in the Military: Impact, Prevention, and Recommendations. Los Angeles, CA: USC School of Social Work (2015).
38. Moye LS, Pradhan AA. From blast to bench: A translational mini-review of posttraumatic headache. J Neurosci Res. (2017) 95:1347–54. doi: 10.1002/jnr.24001
39. Theeler BJ, Erickson JC. Posttraumatic headache in military personnel and veterans of the iraq and afghanistan conflicts. Curr Treat Options Neurol. (2012) 14:36–49. doi: 10.1007/s11940-011-0157-2
40. Elder GA, Stone JR, Ahlers ST. Effects of low-level blast exposure on the nervous system: is there really a controversy? Front Neurol. (2014) 5:269. doi: 10.3389/fneur.2014.00269
41. Elder GA, Dorr NP, De Gasperi R, Gama Sosa MA, Shaughness MC, Maudlin-Jeronimo E, et al. Blast exposure induces post-traumatic stress disorder-related traits in a rat model of mild traumatic brain injury. J Neurotrauma. (2012) 29:2564–75. doi: 10.1089/neu.2012.2510
42. Verfaellie M, Lee LO, Lafleche G, Spiro A. Self-reported sleep disturbance mediates the relationship between PTSD and cognitive outcome in blast-exposed OEF/OIF veterans. J Head Trauma Rehabil. (2016) 31:309–19. doi: 10.1097/HTR.0000000000000197
43. Perez-Garcia G, Gama Sosa MA, De Gasperi R, Lashof-Sullivan M, Maudlin-Jeronimo E, Stone JR, et al. Exposure to a predator scent induces chronic behavioral changes in rats previously exposed to low-level blast: implications for the relationship of blast-related TBI to PTSD. Front Neurol. (2016) 7:176. doi: 10.3389/fneur.2016.00176
44. Perez-Garcia G, Gama Sosa MA, De Gasperi R, Lashof-Sullivan M, Maudlin-Jeronimo E, Stone JR, et al. Chronic post-traumatic stress disorder-related traits in a rat model of low-level blast exposure. Behav Brain Res. (2018) 340:117–25. doi: 10.1016/j.bbr.2016.09.061
45. Zuckerman A, Ram O, Ifergane G, Matar MA, Sagi R, Ostfeld I, et al. Controlled low-pressure blast-wave exposure causes distinct behavioral and morphological responses modelling mild traumatic brain injury, post-traumatic stress disorder, and comorbid mild traumatic brain injury–post-traumatic stress disorder. J Neurotrauma. (2016) 34:145–64. doi: 10.1089/neu.2015.4310
46. Theodoroff SM, Lewis MS, Folmer RL, Henry JA, Carlson KF. Hearing impairment and tinnitus: prevalence, risk factors, and outcomes in US service members and veterans deployed to the Iraq and Afghanistan Wars. Epidemiol Rev. (2015) 37:71–85. doi: 10.1093/epirev/mxu005
47. Gent TC, Bassetti CLA, Adamantidis AR. Sleep-wake control and the thalamus. Curr Opin Neurobiol. (2018) 52:188–97. doi: 10.1016/j.conb.2018.08.002
48. Coulon P, Budde T, Pape H-C. The sleep relay—the role of the thalamus in central and decentral sleep regulation. Pflügers Archiv Eur J Physiol. (2012) 463:53–71. doi: 10.1007/s00424-011-1014-6
49. Bryan CJ, Jennings KW, Jobes DA, Bradley JC. Understanding and preventing military suicide. Arch Suicide Res. (2012) 16:95–110. doi: 10.1080/13811118.2012.667321
50. McKeon AB, Stocker RPJ, Germain A. Traumatic brain injury and sleep disturbances in combat-exposed service members and veterans: where to go next? NeuroRehabilitat. (2019) 45:163–85. doi: 10.3233/NRE-192804
51. Troxel WM, Shih RA, Pedersen ER, Geyer L, Fisher MP, Griffin BA, et al. Sleep in the military: promoting healthy sleep among U.S. servicemembers. Rand Health Q. (2015) 5:19.
52. Good CH, Brager AJ, Capaldi VF, Mysliwiec V. Sleep in the United States military. Neuropsychopharmacology. (2020) 45:176–91. doi: 10.1038/s41386-019-0431-7
53. Pruitt LD, Smolenski DJ, Bush NE, Tucker J, Issa F, Hoyt TV, et al. Suicide in the military: understanding rates and risk factors across the United States' armed forces. Military Med. (2019) 184:432–7. doi: 10.1093/milmed/usy296
54. Lyon J. New data on suicide risk among military veterans. JAMA. (2017) 318:1531. doi: 10.1001/jama.2017.15982
55. Ramchand R. Suicide Prevention for U.S. Veterans: The Need for Data-Driven Solutions. Santa Monica, CA: RAND Corporation (2021).
56. Stoltzfus JC. Logistic regression: a brief primer. Acad Emergency Med. (2011) 18:1099–104. doi: 10.1111/j.1553-2712.2011.01185.x
57. Best H, Wolf C. Logistic regression. The SAGE handbook of regression analysis and causal inference (2003). p. 153–72. doi: 10.4135/9781446288146.n8
Keywords: blast, overpressure, high-level blast, low-level blast, diagnosis, military, occupational health
Citation: Belding JN, Kolaja CA, Rull RP and Trone DW (2023) Single and repeated high-level blast, low-level blast, and new-onset self-reported health conditions in the U.S. Millennium Cohort Study: An exploratory investigation. Front. Neurol. 14:1110717. doi: 10.3389/fneur.2023.1110717
Received: 29 November 2022; Accepted: 13 February 2023;
Published: 21 March 2023.
Edited by:
James Radford Stone, University of Virginia, United StatesReviewed by:
Gregory Elder, Icahn School of Medicine at Mount Sinai, United StatesMichael Joseph Egnoto, Walter Reed Army Institute of Research, United States
Copyright © 2023 Belding, Kolaja, Rull and Trone. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Jennifer N. Belding, amVubmlmZXIubi5iZWxkaW5nLmNpdkBoZWFsdGgubWls
 Jennifer N. Belding
Jennifer N. Belding Claire A. Kolaja1,2
Claire A. Kolaja1,2