- Department of Otorhinolaryngology, Faculty of Medicine, Khon Kaen University, Khon Kaen, Thailand
Background: Cervicogenic dizziness is a clinical syndrome characterized by neck pain and dizziness. Recent evidence suggested that self-exercise could improve a patient's symptoms. The objective of this study was to evaluate the efficacy of self-exercise as an add-on therapy in patients with non-traumatic cervicogenic dizziness.
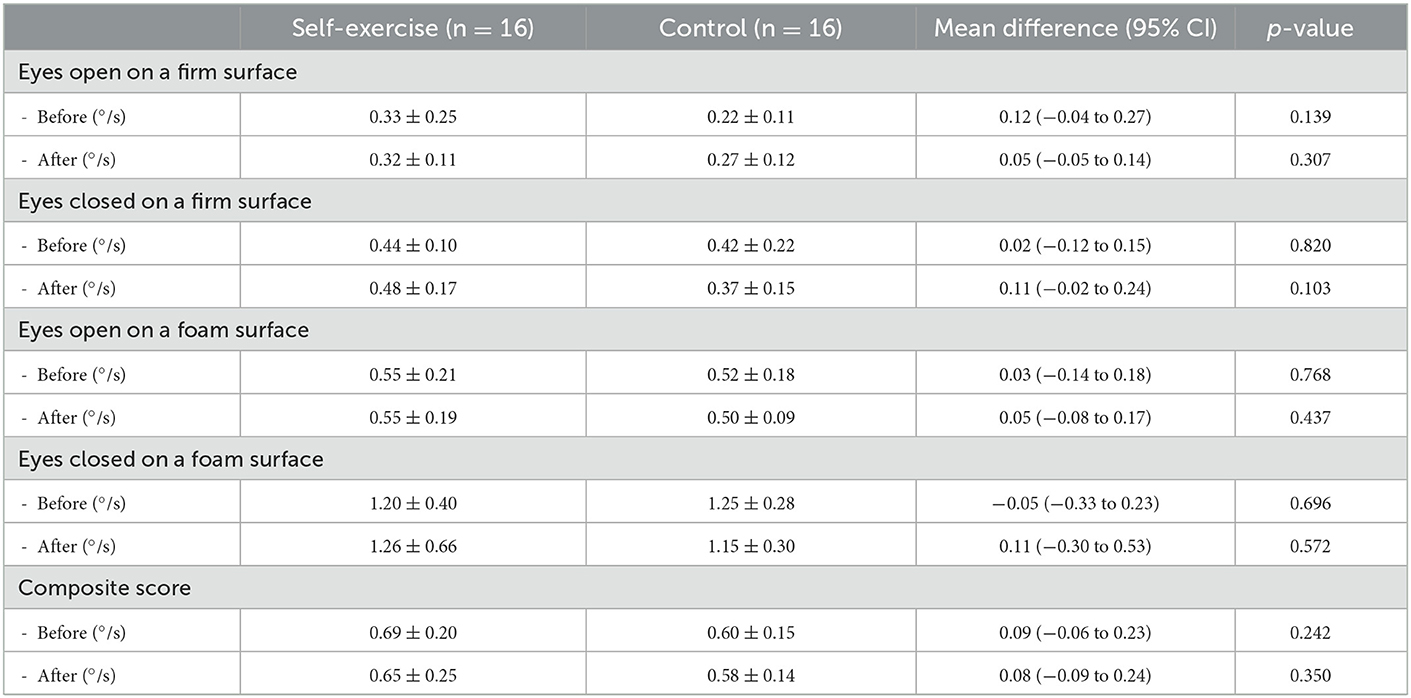
Methods: Patients with non-traumatic cervicogenic dizziness were randomly assigned to the self-exercise and control groups. The self-exercise group was instructed to perform muscle, mobilization, and oculomotor training at home while there was no specific training given to the control group. The neck pain, dizziness symptoms, and their impact on daily life were evaluated by the Dizziness Handicap Inventory (DHI) scale, the Neck Disability Index (NDI) scale, and the visual analog scale (VAS). The objective outcomes included the range of motion test of the neck and the posturography test. All outcomes were evaluated at 2 weeks after the initial treatment.
Results: A total of 32 patients participated in this study. The average age of the participants was 48 years. The DHI score of the self-exercise group after the treatment was significantly lower when compared to the control group [mean difference (MD) 25.92 points, 95% CI 4.21–47.63, p = 0.021]. The NDI score after treatment was also significantly lower in the self-exercise group (MD 6.16 points, 95% CI 0.42–11.88, p = 0.036). However, there was no statistical difference in the VAS score, the range of motion test, and the posturography test between the two groups (p > 0.05). No significant side effects were noted in either of the groups.
Conclusion: Self-exercise is effective in reducing dizziness symptoms and its impact on daily life in patients with non-traumatic cervicogenic dizziness.
1. Introduction
Cervicogenic dizziness is a clinical syndrome characterized by neck pain and dizziness. It accounted for ~5% of all dizziness and vertigo encounters in our setting in a previous study (1, 2). In the retrospective chart review, non-traumatic cervicogenic dizziness was found in ENT clinics from 5.42 to 7.5% (3, 4). The prevalence of cervicogenic dizziness from a prospective multicenter study was 6.4% (5).
Cervicogenic dizziness is defined as dizziness from cervical spine disorders (6). The pathophysiology of this disease was from proprioceptive system abnormality (7, 8). Proprioceptive input from the neck helps in the coordination of eye, head, and body posture, as well as spatial orientation (7).
The treatment regimens for non-traumatic cervicogenic dizziness include muscle relaxants, analgesics, and antidizziness drugs. Physiotherapy and manual therapy are also recommended to improve cervical symptoms (7, 9, 10). However, physiotherapy and manual therapy were not effective to improve dizziness symptoms (11).
Self-exercise consists of strength, mobilization, and oculomotor training and has been proposed as an add-on therapy to address both cervical and dizziness symptoms. One promising study evaluated the effectiveness of self-exercise for non-traumatic cervicogenic dizziness in seven patients and found an improvement in the patient's dizziness symptoms and range of motion (12).
To the best of our knowledge, this is the first randomized controlled trial to evaluate the efficacy of self-exercise as an add-on therapy in patients with non-traumatic cervicogenic dizziness.
2. Methods
2.1. Study design and setting
This randomized controlled trial was conducted from October 2018 to December 2020 at Khon Kaen University, Faculty of Medicine, Department of Otorhinolaryngology, Thailand.
2.2. Randomization
The randomization list was computer-generated by a statistician based on the block randomization method with randomly selected block sizes of 2, 4, 6, and 8. The allocation assignment was sealed in opaque, sequentially numbered envelopes.
2.3. Participants
We included all patients aged 18 years or older who had non-traumatic cervicogenic dizziness. The exclusion criteria were as follows: (1) the presence of trauma or recent surgery to the head, face, neck, or chest; (2) patients diagnosed with central vertigo; (3) those diagnosed with vertigo of vestibular origin such as benign positional paroxysmal vertigo; (4) patients who cannot perform self-exercise such as cervical fracture, and (5) those with history of allergy to dimenhydrinate or ibuprofen.
2.4. Diagnosis of non-traumatic cervicogenic dizziness
The modified stepwise process for diagnosing non-traumatic cervicogenic dizziness according to Reiley et al. (13) was used in this study.
Step 1. Patient history: The patient should have a history of neck pathology and also experience dizziness that has a close temporal relationship with the onset of cervical spine symptoms.
Step 2. Triage: Patients with traumatic cervical spine injury were excluded. Cervical arterial dysfunction was excluded when the patient reported dizziness during the 10-s active cervical range of motion test. The central vestibular disorders were excluded by a neurological screen including an assessment of radicular symptoms, myotomes, dermatomes, deep-tendon reflexes, upper motor neuron signs, and cranial nerve function.
Step 3. Vestibular assessment: The tests were done to exclude vestibular dysfunctions including evaluation of nystagmus, skew, smooth pursuit, saccades, the Dix-Hallpike test, static and dynamic visual acuity, and the head thrust test. In addition, a videonystagmography test was conducted to examine and rule out vestibular and central motor dysfunctions.
Step 4. Detailed cervical spine evaluation: A manual spinal examination was used to identify the source of pain. Patients with non-traumatic cervicogenic dizziness commonly present with tight posterior neck muscles and tenderness of both posterior neck muscles and cervical facet joints.
2.5. Procedure
In the self-exercise group, the patients were instructed to perform the self-exercise at least 4 days per week and of 3 sets per day (12). The therapy includes the following factors (Figure 1):
1. Strength exercise
a. Flexion: Put one hand on the front of the head and apply force in the same direction against the hand for 5 s × 10 times.
b. Extension: Place the hands behind the head and perform opposing forces against the hands for 5 s × 10 times.
c. Rotation: Put one of the hands on the side of the forehead and apply force in the direction to make a turn to the left or right of the head for 5 s × 10 times.
d. Lateral flexion: Place the hand on the temporalis muscle and make the lateral flexion by isometric exercise, making opposing forces for 5 s × 10 times.
2. Mobilization exercise
a. Flexion: Try to touch the chest with the chin. Hold for 5 s × 10 times.
b. Extension: Slowly move the head backward and look upward. Hold for 5 s × 10 times.
c. Rotation: Turn the head to the right and left while making a stop in the middle of the range. Hold for 5 s × 10 times.
d. Lateral flexion: Tilt the head to the right and left making a stop in the middle of the range, keeping the shoulders down. Hold for 5 s × 10 times.
3. Oculomotor training
a. Flexion: Set a fixed point in front of the eyes by holding out the arm and looking at the thumb. Try to touch the chest with the chin while keeping the eyes on the thumb for 5 s × 10 times.
b. Extension: Set a fixed point in front of the eyes by holding out the arm and looking at the thumb. Slowly move the head backward and look upward while keeping the eyes on the thumb for 5 s × 10 times.
c. Rotation: Set a fixed point in front of the eyes by holding out the arm and looking at the thumb. Turn the head to the right and left making a stop in the middle of the range while keeping the eyes on the thumb for 5 s × 10 times.
d. Lateral flexion: Set a fixed point in front of the eyes by holding out the arm and looking at the thumb. Tilt the head to the right and the left, making a stop in the middle of the range, while keeping the eyes on the thumb for 5 s × 10 times.
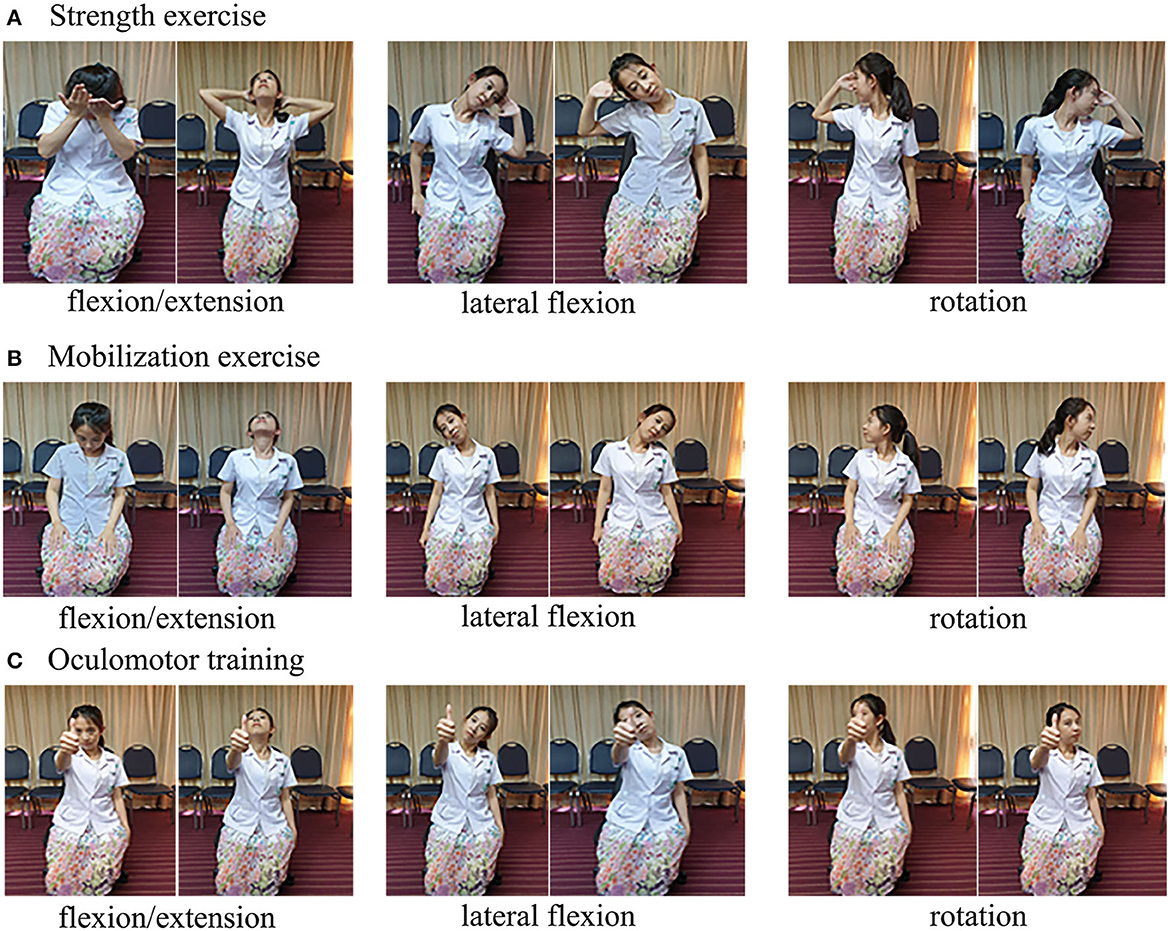
Figure 1. Self-exercise program. (A) Strength exercise. (B) Mobilization exercise. (C) Oculomotor training.
There was no specific exercise instruction given to the control group. In the self-exercise group, all patients were instructed by the otolaryngologists until they were confident to practice the procedure at home.
2.6. Follow-up
The patients were followed up for 2 weeks.
2.7. Standard treatment procedure
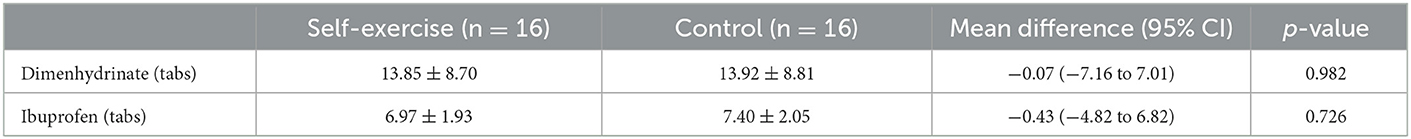
The patients were advised to take dimenhydrinate (50 mg) when they had severe vertigo every 8 h and to stop taking it when the symptoms improved. All patients have also been prescribed ibuprofen 400 mg every 8 h to reduce cervical pain and to stop taking it when the symptoms improved.
2.8. Outcomes
2.8.1. The Dizziness Handicap Inventory (DHI) questionnaire
The DHI questionnaire comprises 25 items to evaluate the self-perceived handicapping effects of dizziness symptoms. The patient was asked to answer each question as it pertains to dizziness or unsteadiness problems, specifically considering their condition during the last month. Questions were designed to incorporate the functional, physical, and emotional impacts on disability. Scores >10 points should be referred to balance specialists for further evaluation. The scores of 16–34, 36–52, and 54 points or more indicate mild, moderate, and severe handicaps (14). The DHI questionnaire has been validated as an assessment tool for non-traumatic cervicogenic dizziness (15).
2.8.2. Neck Disability Index (NDI) questionnaire
The NDI questionnaire is designed to measure neck-specific disability. The questionnaire has 10 items concerning pain and activities of daily living including personal care, lifting, reading, headaches, concentration, work status, driving, sleeping, and recreation. Each item is scored out of five (with the no disability response given a score of zero) with a total score of 50 for the questionnaire. Higher scores represent greater disability (16).
2.8.3. Visual analog scale (VAS) of neck pain
The VAS is a unidimensional measure of pain intensity, which has been widely used in diverse adult populations (17). The neck pain VAS is a continuous scale comprised of a horizontal line. The scale is anchored by “no pain” (score of 0) and “pain as bad as it could be” or “worst imaginable pain” (score of 10) (18).
2.8.4. Cervical range of motion
The full cervical active range of motion was defined as follows: a flexion range of more than 50°, an extension range of more than 60°, a lateral flexion range of more than 45°, and a rotation range of more than 80° (19, 20).
2.8.5. Posturography
Posturography was used to assess functional balance and relative contributions of visual, proprioceptive, and vestibular cues. Sensors within the platform footplate measure the force exerted by the feet when the patient's center of gravity is displaced (21).
We used the NeuroCom Balance Master, NeuroCom International, Inc., Oregon, USA to measure the sway velocity in this study. There was no standard normal value for the center of gravity sway velocity. However, from a study of 36 healthy subjects, the sway velocity when the eyes were open was 1.23° ± 0.14°/s (range 0.95–1.55) and when the eyes were closed was 2.15° ± 0.28°/s (range 1.70–2.85). The sway velocity will increase when changing the platform from a firm surface to a foam surface (22).
2.8.6. Adverse events
The adverse events observed include falling, neck injury, and allergy.
2.9. Statistical analysis
The sample size was calculated base on previous study (12). The DHI score of the non-traumatic cervicogenic dizziness patients before treatment was 20.85 ± 11.53 points, and the DHI score after the treatment was 11.14 ± 7.28 points. With a significance level of 0.05 and a power of 90%, the total number of patients required was determined to be 32 patients.
Statistical analyses were performed using the SPSS version 20 and Stata version 14. Data were described as either means (for the continuous variables) or frequencies and percentages (for the categorical variables). Significant differences between groups were determined using the Student's t-test or the Mann–Whitney U test for continuous variables. The chi-square test or the Fisher's exact test was used to determine whether there was a significant difference between the expected frequencies and the observed frequencies. For all tests, a p-value of < 0.05 was considered statistically significant.
3. Results
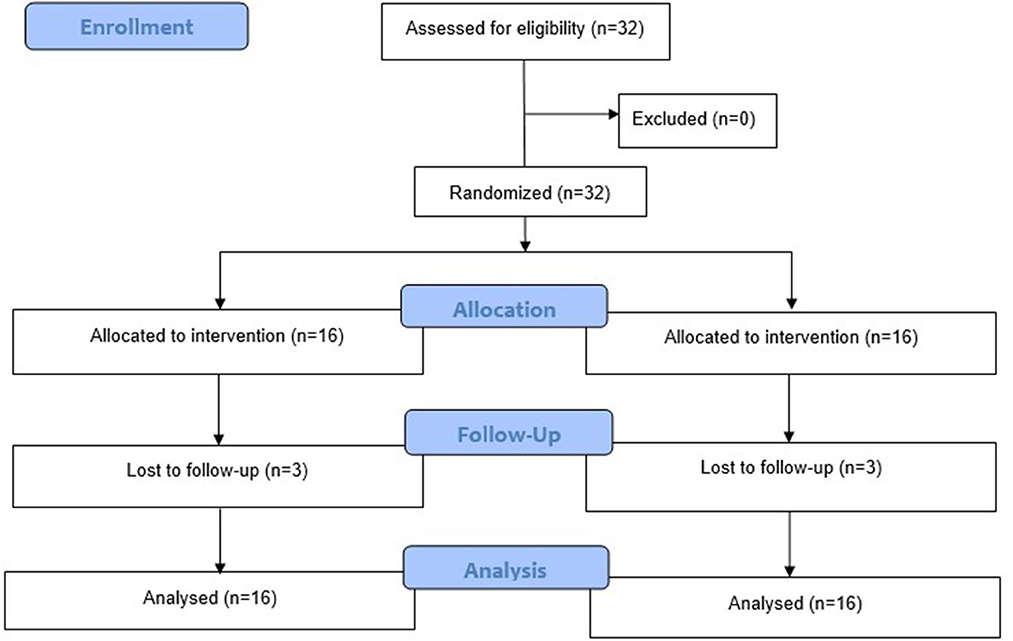
A total of 32 patients participated in this study, 16 of whom were allocated to the self-exercise group and 16 of whom were allocated to the control group. Three patients (18.75%) were lost to follow-up in both groups. The participant flow diagram is shown in Figure 2.
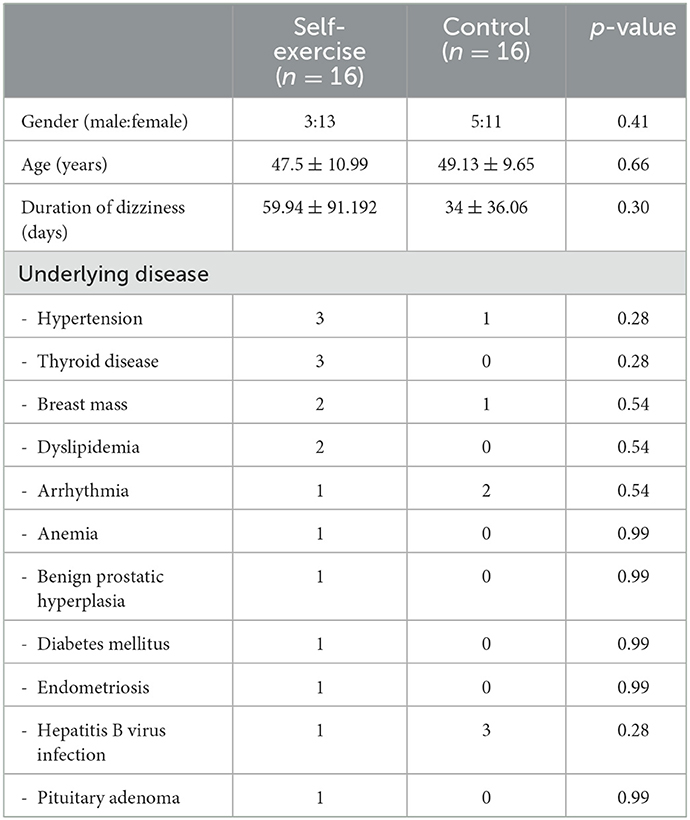
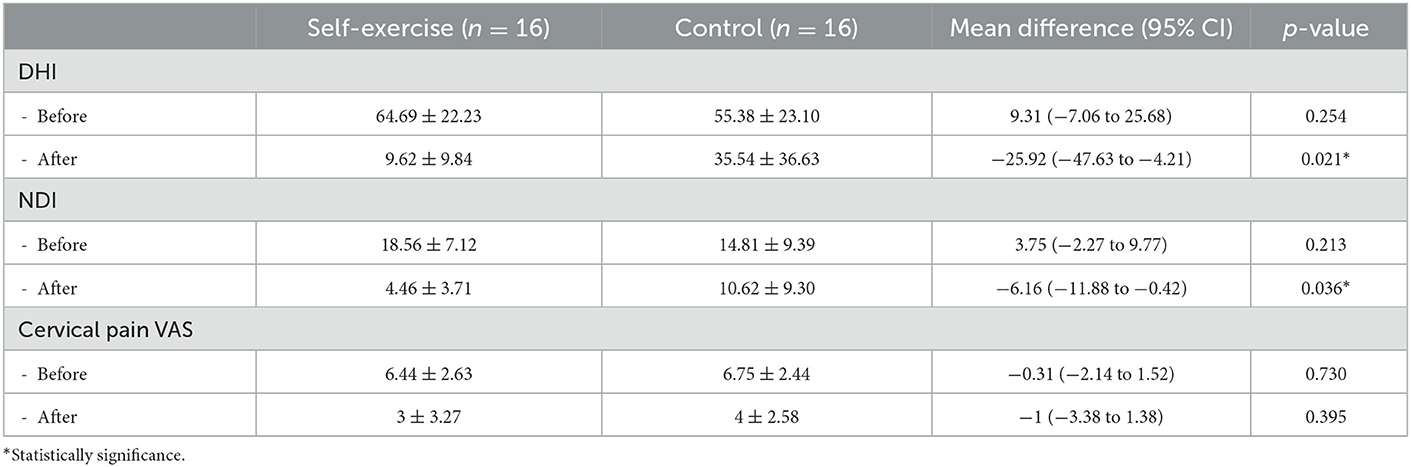
The average age of the participants was 48 years. Eight of the patients were men and 24 were women. There was no difference in sex, age, duration of vertigo, and underlying diseases (Table 1). At baseline, there was no difference in the DHI, the NDI, and the VAS of neck pain score between the groups (p > 0.05).
After treatment, the DHI score was significantly lower in the self-exercise group [mean difference (MD) 25.92, 95% CI 4.21 to 47.63; lower is better]. The neck disability index score was also significantly lower in the self-exercise group (MD 6.16, 95% CI 0.42 to 11.88; lower is better). However, there was no difference in cervical pain score (MD 1, 95% CI −1.38 to 3.38; lower is better) (Table 2).
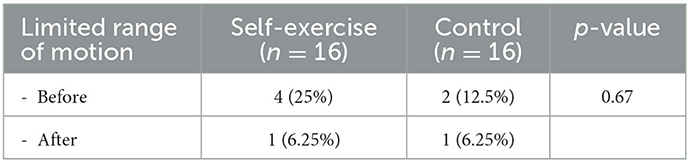
At baseline, four patients (25%) in the self-exercise group had a limited range of cervical motion and two patients (12.5%) in the control group had a limited range of cervical motion. After treatment, one patient (6.25%) in the self-exercise group had a limited range of cervical motion and one patient (6.25%) in the control group had a limited range of cervical motion. There was no statistically significant difference between the groups (Table 3).
The mean sway velocity was decreased in both groups (lower is better). However, there was no significant difference between the groups (MD 0.08°/s, 95% CI −0.09 to 0.24, p = 0.35) (Table 4).
There was no difference in the number of standard treatment medication tablets used by the patients between the groups (Table 5). There were no major complications such as cervical spine injury or accidental falling, or allergy in both groups.
4. Discussions
The perception of head rotation was from three afference systems including vestibular, proprioceptive, and visual receptors. Therefore, the abnormalities of these systems can induce a distorted sensation of head motion. The neck contains the neural system (afferent/efferent), the cardiovascular structures (carotid body and vertebral artery), and the cervico-proprioceptive system (cervical muscle and spine). Disorders of these systems can cause vertigo and dizziness (7, 23).
The treatment of non-traumatic cervicogenic dizziness with medications, such as NSAIDs and antihistamines, can reduce neck pain and vertigo symptoms. Physiotherapy and manual therapy were also proven to improve the range of motion (10, 24). However, they were not effective in improving dizziness symptoms (11).
We proposed that self-exercise consists of strength, mobilization, and oculomotor training as an add-on therapy that can help to relieve dizziness symptoms by improving balance and motor control.
In this study, we found that the dizziness handicap inventory score was significantly lower in the self-exercise group [mean difference (MD) 25.92, 95% CI 4.21 to 47.63; lower is better]. The neck disability index score was also significantly lower in the self-exercise group (MD 6.16, 95% CI 0.42 to 11.88; lower is better). However, there was no difference in cervical pain score (MD 1, 95% CI −1.38 to 3.38; lower is better) and mean sway velocity (MD 0.08°/s, 95% CI −0.09 to 0.24, p = 0.35).
The results from this study were consistent with those of Minguez-Zuazo et al. who examined the effectiveness of self-exercise in seven patients (12). They found an improvement in the range of motion, the dizziness handicap inventory score, and the neck disability index score.
Although the DHI was significantly improved, we found no difference in the center of gravity sway velocity. This lack of difference can be explained by the fact that, since the postural stability was not impaired before treatment, the improvement could only be small.
The strength of this study is the relatively large sample size when compared to other non-traumatic cervicogenic dizziness trials. To the best of our knowledge, this is the first randomized controlled trial to evaluate the efficacy of self-exercise as an add-on therapy for non-traumatic cervicogenic dizziness. The results of this study can be applied to help improve the quality of life of the patients.
In this study, we used the common assessment tools for dizziness, such as DHI, NDI, VAS, and posturography. There was a possibility to use an emerging tool to assess cervicogenic dizziness such as the Jenaer Standing Stability Score (25) or the Horizontal Plane Target Platform (26) in the future study.
The limitation of this study were a short follow-up period and the high use of rescue medication in both groups of patients, especially the usage of dimenhydrinate, which may affect the results. The recruitment period of this study was 2 years due to this condition being quite rare. We suggest that future studies should conduct as multicenter studies.
There was also a common limitation of this study and other cervicogenic dizziness trials due to a lack of standard diagnostic criteria for cervicogenic dizziness. We used the modified stepwise process to accurately rule in and rule out competing diagnoses (13). We propose that a cross-professional consensus on the diagnosis criteria of cervicogenic dizziness is needed.
Conclusion
Self-exercise for non-traumatic cervicogenic dizziness is effective in reducing the dizziness symptom and its impact on daily life.
Data availability statement
The original contributions presented in the study are included in the article/supplementary material, further inquiries can be directed to the corresponding author.
Ethics statement
The studies involving human participants were reviewed and approved by Khon Kaen University Ethics Committee in Human Research (approval ID: HE611337). The patients/participants provided their written informed consent to participate in this study. Written informed consent was obtained from the individual(s) for the publication of any potentially identifiable images or data included in this article.
Author contributions
PP contributed to study design, data acquisition, analysis and interpretation of results, statistical analysis, drafting of the manuscript, critical manuscript revision, and final approval. NT contributed to study design, data acquisition, statistical analysis, manuscript editing, and final approval. SS and KY contributed to study design, manuscript editing, and final approval. All authors contributed to the article and approved the submitted version.
Funding
This study received internal funding from the Faculty of Medicine, Khon Kaen University (grant number: AS65201).
Acknowledgments
The authors would like to thank the staff and nurses at Srinagarind Hospital for their excellent care of the patients and The Khon Kaen Ear, Hearing, and Balance Research Group for their support.
Conflict of interest
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
Publisher's note
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
References
1. Piromchai P, Laohasiriwong S, Saesiew P, Teeramaswanitch W, Reechaipichitkul W. Ear, nose, throat, and craniofacial disease screening in primary school: Khon Kaen University 2017 initiative. J Med Assoc Thai. (2018) 101:77.
2. Piromchai P, Saeseow P, Reechaipichitkul W, Kasemsiri P, Chayaopas N. Prevalence of ear, nose, and throat diseases in the elderly: Khon Kaen University's community service from 2017 to 2018. J Med Assoc Thai. (2019) 102:128.
3. Polaczkiewicz L, Olszewski J. Analyze causes and results of vng examinations in patients with vertigo and balance disorders in the private ENT practice. Otolaryngol Pol. (2019) 74:23–30. doi: 10.5604/01.3001.0013.4374
4. Ardic FN, Topuz B, Kara CO. Impact of multiple etiology on dizziness handicap. Otol Neurotol. (2006) 27:676–80. doi: 10.1097/01.mao.0000226292.49789.c9
5. Luscher M, Theilgaard S, Edholm B. Prevalence and characteristics of diagnostic groups amongst 1034 patients seen in ent practices for dizziness. J Laryngol Otol. (2014) 128:128–33. doi: 10.1017/S0022215114000188
6. Grieve GP, Boyling JD, Jull GA. Grieve's Modern Manual Therapy: The Vertebral Column. 3rd ed. Edinburgh: Churchill Livingstone (2004).
7. Li Y, Peng B. Pathogenesis, diagnosis, and treatment of cervical vertigo. Pain Physician. (2015) 18:E583–95. doi: 10.36076/ppj.2015/18/E583
8. Brandt T, Bronstein AM. Cervical vertigo. J Neurol Neurosurg Psychiatry. (2001) 71:8–12. doi: 10.1136/jnnp.71.1.8
9. Karlberg M, Magnusson M, Malmstrom EM, Melander A, Moritz U. Postural and symptomatic improvement after physiotherapy in patients with dizziness of suspected cervical origin. Arch Phys Med Rehabil. (1996) 77:874–82. doi: 10.1016/S0003-9993(96)90273-7
10. Reid SA, Rivett DA. Manual therapy treatment of cervicogenic dizziness: a systematic review. Man Ther. (2005) 10:4–13. doi: 10.1016/j.math.2004.03.006
11. Reid SA, Callister R, Katekar MG, Rivett DA. Effects of cervical spine manual therapy on range of motion, head repositioning, and balance in participants with cervicogenic dizziness: a randomized controlled trial. Arch Phys Med Rehabil. (2014) 95:1603–12. doi: 10.1016/j.apmr.2014.04.009
12. Minguez-Zuazo A, Grande-Alonso M, Saiz BM, La Touche R, Lara SL. Therapeutic patient education and exercise therapy in patients with cervicogenic dizziness: a prospective case series clinical study. J Exerc Rehabil. (2016) 12:216–25. doi: 10.12965/jer.1632564.282
13. Reiley AS, Vickory FM, Funderburg SE, Cesario RA, Clendaniel RA. How to diagnose cervicogenic dizziness. Arch Physiother. (2017) 7:12. doi: 10.1186/s40945-017-0040-x
14. Jacobson GP, Newman CW. The Development of the dizziness handicap inventory. Arch Otolaryngol Head Neck Surg. (1990) 116:424–7. doi: 10.1001/archotol.1990.01870040046011
15. Reid SA, Callister R, Katekar MG, Treleaven JM. Utility of a brief assessment tool developed from the dizziness handicap inventory to screen for cervicogenic dizziness: a case control study. Musculoskelet Sci Pract. (2017) 30:42–8. doi: 10.1016/j.msksp.2017.03.008
16. Vernon H, Mior S. The neck disability index: a study of reliability and validity. J Manipulative Physiol Ther. (1991) 14:409–15. doi: 10.1037/t35122-000
17. McCormack HM, Horne DJ, Sheather S. Clinical applications of visual analogue scales: a critical review. Psychol Med. (1988) 18:1007–19. doi: 10.1017/S0033291700009934
19. Niewiadomski C, Bianco RJ, Afquir S, Evin M, Arnoux PJ. Experimental assessment of cervical ranges of motion and compensatory strategies. Chiropr Man Therap. (2019) 27:9. doi: 10.1186/s12998-018-0223-x
20. Swartz EE, Floyd RT, Cendoma M. Cervical spine functional anatomy and the biomechanics of injury due to compressive loading. J Athl Train. (2005) 40:155–61.
21. Valente LM. Assessment techniques for vestibular evaluation in pediatric patients. Otolaryngol Clin North Am. (2011) 44:273–90, vii. doi: 10.1016/j.otc.2011.01.002
22. Woods J. The effect of balance training in healthy subjects as assessed by the neurocom balance master. Phys Ther Schol Projects. (2000) 486.
23. Wrisley DM, Sparto PJ, Whitney SL, Furman JM. Cervicogenic dizziness: a review of diagnosis and treatment. J Orthop Sports Phys Ther. (2000) 30:755–66. doi: 10.2519/jospt.2000.30.12.755
24. Reid SA, Rivett DA, Katekar MG, Callister R. Comparison of mulligan sustained natural apophyseal glides and maitland mobilizations for treatment of cervicogenic dizziness: a randomized controlled trial. Phys Ther. (2014) 94:466–76. doi: 10.2522/ptj.20120483
25. Buder A, Derlien S, Loudovici-Krug D, Best N. Validating the balance of semi-professional dancers by use of the jenaer-standing-stability-score (Jess-Score). Phys Med Rehabil Kurortmedizin. (2021) 32:146–50. doi: 10.1055/a-1590-8116
Keywords: exercise, vertigo, peripheral vertigo, self-exercise, dizziness
Citation: Piromchai P, Toumjaidee N, Srirompotong S and Yimtae K (2023) The efficacy of self-exercise in a patient with cervicogenic dizziness: A randomized controlled trial. Front. Neurol. 14:1121101. doi: 10.3389/fneur.2023.1121101
Received: 11 December 2022; Accepted: 24 January 2023;
Published: 14 February 2023.
Edited by:
Hubertus Axer, Jena University Hospital, GermanyReviewed by:
Norman Best, University Hospital Jena, GermanyFazil Necdet Ardiç, Pamukkale University, Turkey
Copyright © 2023 Piromchai, Toumjaidee, Srirompotong and Yimtae. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Patorn Piromchai,  cGF0b3JuQGtrdS5hYy50aA==
cGF0b3JuQGtrdS5hYy50aA==
 Patorn Piromchai
Patorn Piromchai Nattaporn Toumjaidee
Nattaporn Toumjaidee