- 1Department of Forensic Medicine, School of Basic Medical Sciences, Gannan Medical University, Ganzhou, Jiangxi, China
- 2Key Laboratory of Prevention and Treatment of Cardiovascular and Cerebrovascular Disease of Ministry of Education, Gannan Medical University, Ganzhou, Jiangxi, China
- 3Key Laboratory of Forensic Pathology, Ministry of Public Security and Criminal Technology Center of Guangdong Province Public Security Bureau, Guangzhou, Guangdong, China
- 4Forensic Center of Gannan Medical University, Ganzhou, Jiangxi, China
Epilepsy is a common neurological disorder that is associated with increased morbidity and mortality. Sudden unexpected death in epilepsy (SUDEP) is one of the most common causes for epilepsy-related deaths and its characteristics remain largely unknown, particularly from a forensic autopsy perspective. The present study aimed to investigate the neurological, cardiac, and pulmonary findings for a total of 388 SUDEP decedents, encompassing three cases from our forensic center during 2011–2020 and 385 literature-reported autopsy cases. In the cases mentioned in this study, two of them presented with only mild cardiac abnormalities, such as focal myocarditis and mild coronary atherosclerosis of the left anterior coronary artery. The third one was negative of any pathological findings. After pooling together these SUDEP cases, we found that neurological changes (n = 218 cases, 56.2%) were the most common postmortem findings associated with SUDEP, with cerebral edema/congestion (n = 60 cases, 15.5%) and old traumatic brain injury (n = 58 cases, 14.9%) being the major findings. Interstitial fibrosis, myocyte disarray/hypertrophy, and mild coronary artery atherosclerosis were the most common findings related to primary cardiac pathology, documented in 49 (12.6%), 18 (4.6%), and 15 (3.9%) cases, respectively. Non-specific pulmonary edema was the major finding in the lungs. This is an autopsy-based study that reports the scenario of postmortem findings for SUDEP cases. Our study paves the way for understanding the pathogenesis of SUDEP and the interpretation of death.
1. Introduction
Sudden unexpected death in epilepsy (SUDEP) was defined as “sudden, unexpected, witnessed or un-witnessed, non-traumatic and non-drowning death in patients with epilepsy, with or without evidence for a seizure and excluding documented status epilepticus, in which postmortem examination does not reveal a toxicological or anatomic cause for death” (1). It is considered the main cause of death in patients with epilepsy and is the second most common neurological cause for potential years of life lost among all neurological diseases, second only to stroke (2, 3). The incidence rate of SUDEP was reported as 1.16 cases per 1,000 patients with epilepsy. SUDEP affected all age groups, but primarily young people with its incidence in the 20–45-year age group being 27 times higher than in control groups (4). Several risk factors have been identified, with generalized tonic–clonic seizures as the most important one. Other key risk factors include high seizure burden, lack of antiepileptic drug treatment, poly-therapy, intellectual disability, and prone position at the time of death (5).
In suspected SUDEP cases, a complete postmortem examination including both external and full internal examination, as well as toxicological analysis of antiepileptic drug (AED) levels should be made mandatory. Unfortunately, at postmortem investigation, a proportion of SUDEP cases were often unwitnessed and there was no information available on the victim's last moment of life and on the possible clues of seizures before death. Moreover, the majority of SUDEP cases were absent or at subtherapeutic levels of all AEDs (6). Owing to the limited evidence, it is often difficult to clarify whether epilepsy was the cause of death or not. Published case series did not suggest any definite pathological features or biomarkers for diagnosis of SUDEP (7). The most common mechanisms being studied are neuro-cardio-respiratory connections since ictal activity that arises in or spreads to the central autonomic network can disrupt functional connectivity of its network by inhibiting or activating autonomic areas, causing diverse autonomic manifestations, including cardiovascular and respiratory dysfunction, and brainstem damage (8, 9). There is also considerable evidence indicating that genetic factors may play a role. Cardiac genes associated with long QT syndrome, bradycardia, and sudden cardiac death can cause both epilepsy and arrhythmias or increase the risk of seizure-induced arrhythmias and have been linked to SUDEP (10, 11). Moreover, some AEDs may worsen patients' conditions, leading to other health complications including cardiovascular dysfunctions such as myocardial infarction, arrhythmias, and even cardiovascular death or SUDEP (12). All these studies provide a potential understanding of the mechanisms behind the SUDEP. However, the etiology and definite pathogenic mechanisms leading to SUDEP are still unknown.
The limited understanding of SUDEP pathogenesis is, at least in part, due to the scarce knowledge of postmortem findings for these cases. We present three cases of SUDEP individuals and summarized their epidemical and forensic characteristics. We also searched the literature on SUDEP that provided postmortem examination data, thereby summarizing common neurological, cardiac, or pulmonary pathologies with all these SUDEP cases, for the purpose of providing further insight into SUDEP from a forensic autopsy perspective.
2. Materials and methods
2.1. Study design
This is a retrospective and descriptive study with research interest in SUDEP cases undergoing a full autopsy examination. The study method was similar to those mentioned in previous studies (13, 14). We initially collected authentic SUDEP cases from our single center and then searched published literature to gather all relevant cases. We then described the neurological, cardiac, and pulmonary findings based on all the available SUDEP cases.
2.2. Case collection
The cases were collected between January 2011 and December 2020 in the Forensic Center of the Gannan Medical University. Data for this study were taken from the completed postmortem reports, including details of sex, age at death, scene at death, circumstances surrounding the event, autopsy findings, and postmortem toxicological results. Cases were collected based on the following criteria: (1) decedents had a clear record of epilepsy or seizure disorder; (2) decedents experienced a sudden, unexpected, witnessed or unwitnessed, non-traumatic, and non-drowning death; and (3) absence of definite anatomic or toxicological cause of death after complete examination.
Death certificate for these patients was made without controversy by three independent pathologists. In case of multiple pathological changes, the severity of each pathological change and its contribution to the death were seriously evaluated and independently decided by three pathologists. In case of suspected SUDEP, a neuropathologist was routinely consulted. In case of inconsistent conclusion, the case was consulted with another external pathologist to reach the final decision.
Each case was anonymized to protect the patient's privacy. This study only extracted patients' information from archived records without using patients' specimens. The review of patients' medical and forensic records was approved by the Ethical Review Board at the School of Basic Medical Science, Gannan Medical University (Approval No.: 2022-178).
2.3. Literature search strategy and selection criteria
To collect the most matched literature, we used a two-step screen strategy, to systematically obtain publications reporting on cases of patients with epilepsy who died suddenly and unexpectedly and underwent autopsy. Initially, we used terms such as “Epilepsy” and “autopsy” or “SUDEP” and “autopsy” to detect all publications that studied the SUDEP cases from a forensic autopsy perspective. The search was limited to articles published in the English language. The restriction in publication date was set from January 1980 to September 2022.
After initial screening, candidate articles were further evaluated by title and abstract, and then by full-text reading. Studies that did not report postmortem findings were excluded. Reference lists of the retrieved studies were also checked for potential additional articles. Types of studies include retrospective study, case-control study, prospective study, survey, and case report, only if they provided macroscopic and microscopic results of the brain, the heart, and the lungs, as well as toxicological results including serum AED concentrations.
3. Result
3.1. Basic characteristics and autopsy findings of the three SUDEP cases
A review of the files from our forensic center yielded eight cases that had a clear medical history of epilepsy. Among these, three (three out of eight) cases were identified to have died from SUDEP, the other five cases died from explainable causes, such as accidental drowning (n = 1), suicide (n = 1), status epilepticus (n = 2), and rupture of the aortic dissection (n = 1). Of the three SUDEP cases aged 30.5 ± 7.3 years, two were men and one was a woman. The etiology of epilepsy is unclear for all three cases. Two individuals died at their residence, unwitnessed, found in bed or on the bedroom floor in a prone position. The third individual was witnessed to die during the daytime when watching TV. At autopsy, no significant toxicological or anatomical findings were revealed, except bite marks on the tongue and lips for two cases. Periorbital bruise was found in the third individual, indicating potential injury possibly caused by epileptic seizure prior to death. Two cases were presented with mild cardiac abnormalities, such as focal myocarditis and mild coronary atherosclerosis of the left anterior coronary artery. These two subjects also had detectable AEDs at the time of death, both in a sub-therapeutic range.
Basic characteristics and autopsy findings of the three cases categorized as SUDEP are summarized in Table 1.
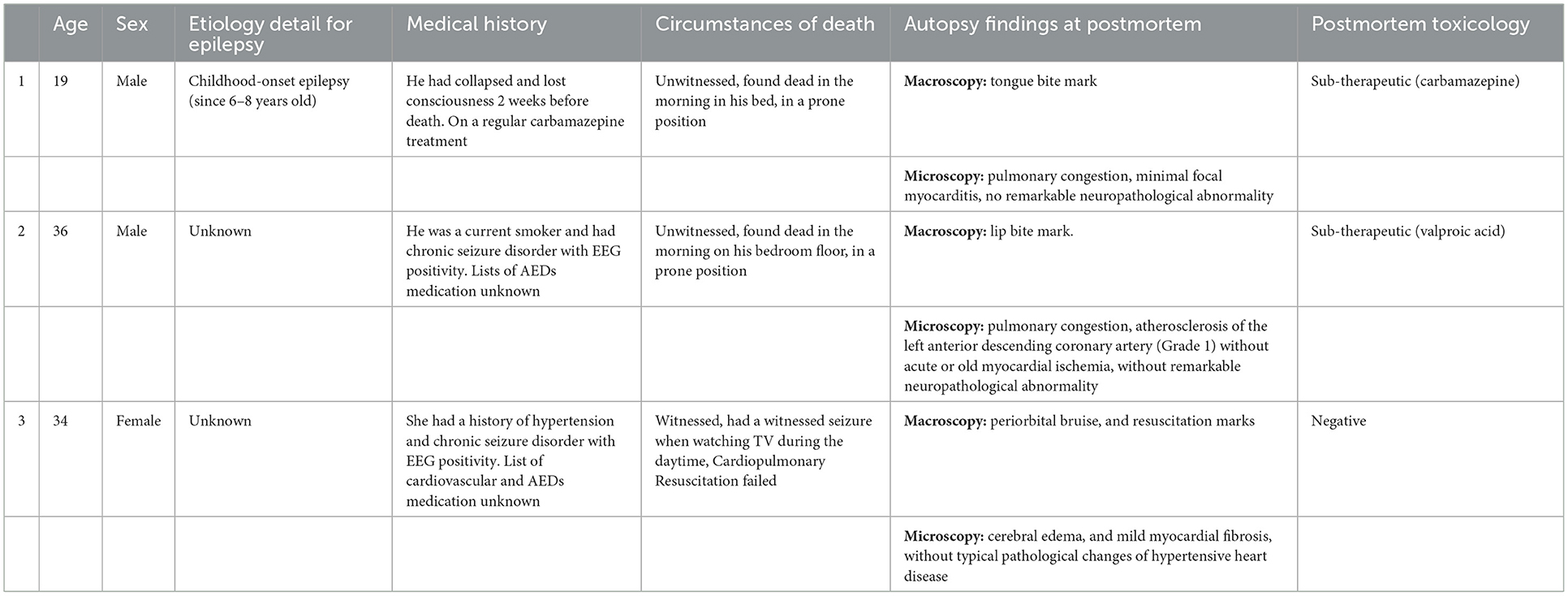
Table 1. Basic characteristics and autopsy findings of the three sudden unexpected deaths in epilepsy (SUDEP) cases.
3.2. Results of the literature search
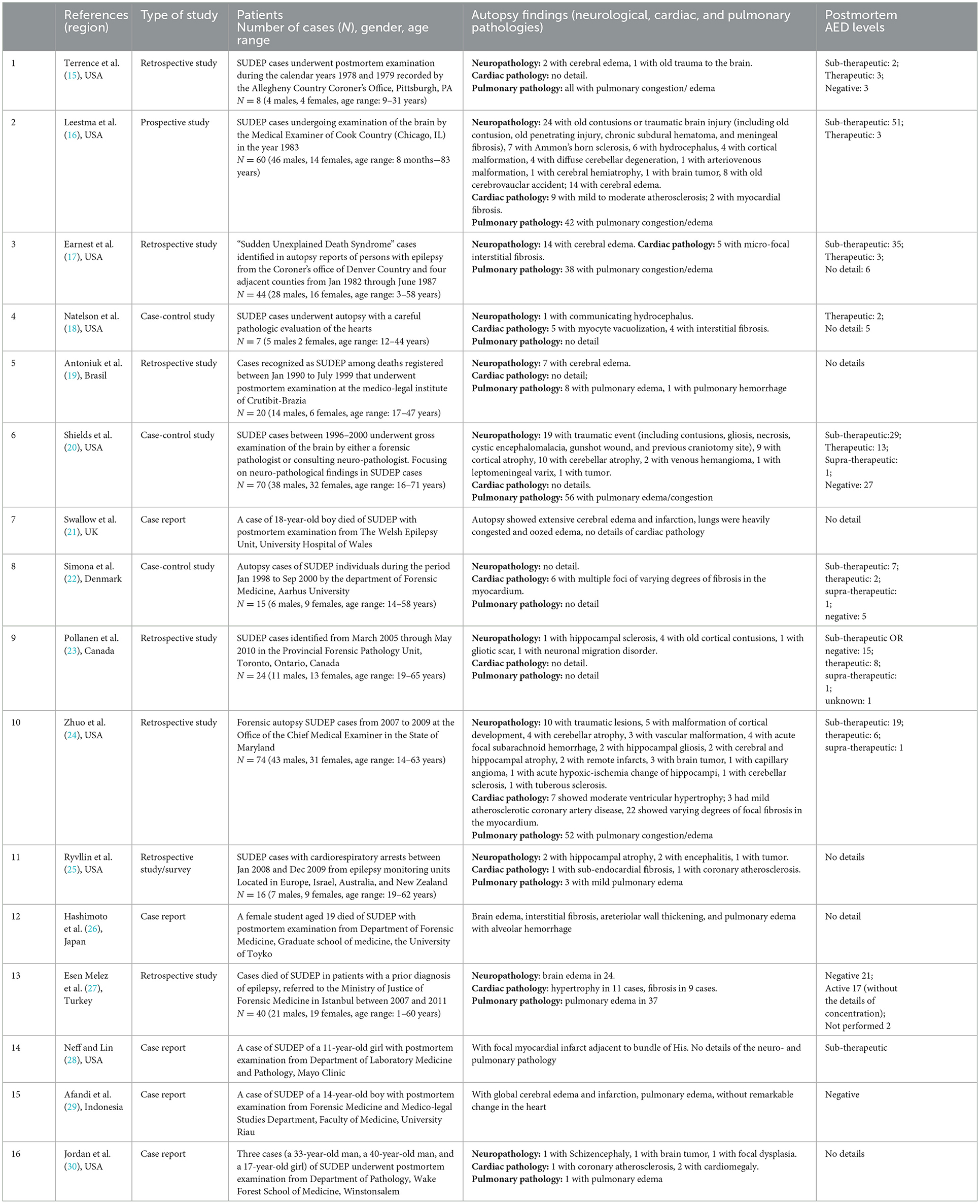
The described search strategy yielded 16 publications, including 7 retrospective studies, 3 case-control studies, 5 case reports, and 1 prospective study, claiming 385 SUDEP cases in total (15–30). These studies were mostly from the USA (9/16). Among the 385 SUDEP cases, the male-to-female ratio was 227:158, similar to the cases reported in this study. Cases from the published literature are concentrated in the age group of 10–40 years, with the age range from 8 months to 83 years. Information on these studies and their detailed findings are documented in Table 2.
3.3. Major neurological, cardiac, and pulmonary findings for the SUDEP cases
We then pooled our three cases with those publications, yielding a total of 388 cases (Table 3). After a full review of all these cases, we found that the cerebral edema/congestion and old traumatic injury were the most common symptoms of neurological pathology, accounting for 60 (15.5%) and 58 (14.4%) cases, respectively. Brain sclerosis, brain atrophy, cortical/vascular malformation, and old cerebrovascular infarction were the consequent changes, claiming 32 (8.3%), 14 (3.7%), 12 (3.1%), and 12 cases (3.1%), respectively. Intracranial tumors were found in 8 cases (2.1%). A total of 183 (47.2%) cases had none or unclarified neurological pathology.
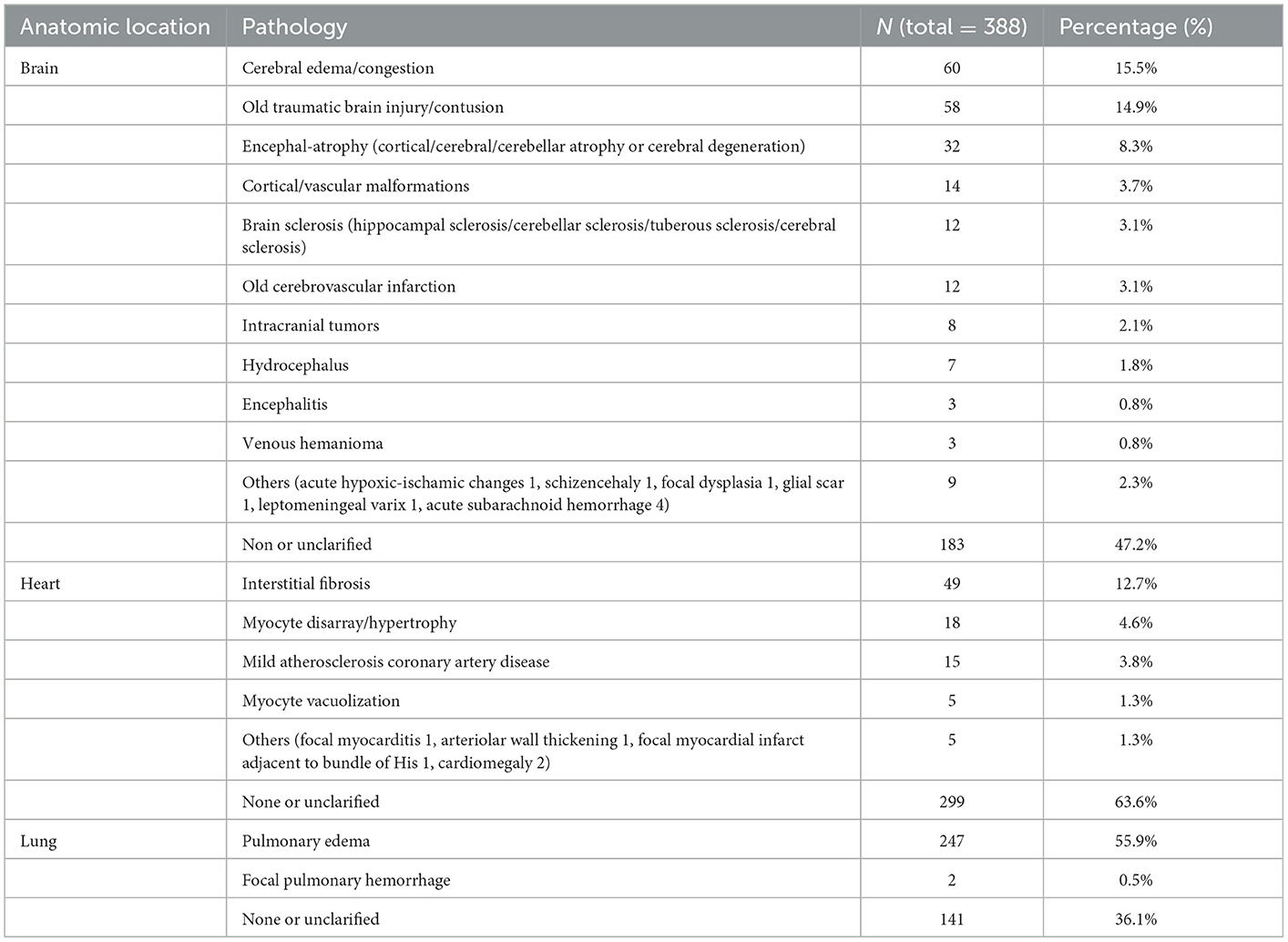
Table 3. Major autopsy findings at the brain, the heart, and the lungs for sudden unexpected death in epilepsy (SUDEP) cases.
Interstitial fibrosis, myocyte disarray/hypertrophy, and mild atherosclerotic coronary artery disease were the most common symptoms of cardiac pathology, documented in 49 (12.7%), 18 (4.6%), and 15 cases (3.8%), respectively. Myocyte vacuolization was documented in 5 cases (1.3%). Other findings presented in five cases (1.3%) included focal myocarditis in one case, arteriolar wall thickening in one case, focal myocardial infarct adjacent to the bundle of His in one case, and cardiomegaly in two cases. A total of 299 (63.6%) cases had none or unclarified cardiac pathology.
Though it is non-specific to SUDEP and probably a result of any death, pulmonary congestion/edema comprised the most common finding of pulmonary pathology, documented in 247 cases (55.9%). Focal intra-alveolar hemorrhage was documented in two cases (0.5%). A total of 141 cases (36.1%) had none or unclarified pulmonary pathology.
4. Discussion
Sudden unexpected death in epilepsy was considered the leading cause of death in patients with epilepsy. By the common definition, the patients die suddenly with no anatomical or toxicological cause of death found, namely the negative postmortem examination. Diagnosis of SUDEP remains a difficult task for forensic pathologists (7, 31). Nevertheless, there is often a spectrum of pathological abnormalities among SUDEP individuals, including neuro- and cardiopulmonary pathological changes. To uncover such pathological changes, the present study pooled cases from our forensic center with literature-reported SUDEP cases and studied the neurological, cardiac, and pulmonary findings from a forensic autopsy perspective. The investigation yielded a total of 388 cases. All the SUDEP cases died at an early age (mostly 10–40 years), with the male-to-female ratio as 229:159. Neurological changes were the most common postmortem findings associated with SUDEP. Interstitial fibrosis, myocyte hypertrophy, and mild coronary artery atherosclerosis were the most common symptoms of primary cardiac pathology, and non-specific pulmonary edema/congestion was the major pulmonary finding.
The common neuropathological findings include mild degrees of cerebral edema or congestion, traumatic brain lesions, hippocampal sclerosis, vascular malformations, low-grade neoplasms, cerebellar atrophy, and cortical malformations (32, 33). The range of pathologies encompasses those commonly encountered in surgical epilepsy series, but no significant difference was shown in the frequency of neuropathological findings between the SUDEP cases and living patients with epilepsy (34). From a histological point of view, the most common finding was related to acute hypoxic neuronal changes, that is, eosinophilic neuronal changes, occurring in 55% of the SUDEP cases, most often in the hippocampus and also sometimes in the cortical and subcortical regions. Epilepsy-related acute hypoxic neuropathology in the brainstem may also contribute to the progression of epilepsy and eventually lead to brainstem dysfunction and cause SUDEP. These acute changes were more frequent when a seizure occurred 24 h before death, the body was in a prone position, or brain swelling was present (32–35). It is worth noting that, although many lesions may be identified, either grossly or microscopically, some epilepsy-related pathologies required specific immunohistochemistry to confirm the diagnosis (32, 33). In addition, published data suggested that neuropathology was very heterogeneous. The diverse neurological findings and heterogeneous data may reflect the non-standard method for conducting a brain examination across forensic institutes. It is thus important to highlight a standardized, widely occupied protocol for brain examination in suspected cases of SUDEP. The Royal College of Pathologists of United Kingdom (UK) issued guidelines in 2006 on autopsy practice in epilepsy death, suggesting that pathologists should have information on epilepsy, including seizure control, treatments, and the circumstantial evidence surrounding the death; a neuropathologist should be involved in the interpretation of brain pathology; and a case should be made for whole brain fixation and examination. A higher detection of intracerebral pathology was noted by examination of the whole fixed brain and examination of all essential regions microscopically compared with other methods (35). These guidelines are useful in forensic practice and may be recommended to be applied across different institutes to execute a uniform brain examination protocol.
Pulmonary pathology in SUDEP mainly consists of pulmonary edema/congestion and less often focal pulmonary hemorrhage. The two cases showing focal pulmonary hemorrhage may reflect asphyxia right before death due to SUDEP. Edema and pulmonary congestion are common autopsy findings of various cardiogenic or neurogenic deaths, including SUDEP (36). Confounding factors, such as postmortem interval, resuscitation with chest compression, and intravenous fluid administration as well as premorbid cardiopulmonary disease, may potentially contribute to the development of pulmonary edema (37). Therefore, pulmonary edema was a non-specific finding and may be of little association with SUDEP.
At the cardiac level, interstitial fibrosis, myocyte disarray/hypertrophy, myocyte vacuolization, and mild atherosclerotic coronary artery disease were mostly described in the literature. The increased frequency of cardiac findings in SUDEP may relate to the effects of seizures or psychotropic medications on the cardiac tissue (12, 38). Some studies argued that the presence and severity of cardiac pathology are not higher among SUDEP cases compared to age- and sex-matched controls who died from sudden cardiac death or trauma or to patients with epilepsy who died from causes other than SUDEP (39). From the forensic perspective, unremarkable coronary artery atherosclerosis, focal myocardial inflammatory infiltrates, isolated myocyte disarray, and idiopathic cardiac fibrosis were occasionally encountered by forensic pathologists, especially in case of sudden unexplained death. These changes, the so-called non-diagnostic autopsy findings, were insufficient to meet diagnostic criteria for known pathologies and insufficient to accord as causes for sudden death (40, 41). Although these subtle cardiac pathological findings could not prove the cause of death, a routine systemic histological examination of the myocardium, even in those who appear to be SUDEP cases, is warranted to monitor the significance of these unexpected findings. Furthermore, as regards the cardiac pathology among patients with epilepsy or SUDEP individuals, there is a need to obtain more information about the cardiorespiratory function in patients with epilepsy, which may contribute to better interpretation, and possibly, prevent SUDEP through interventions such as cardioprotective drugs and effective respiratory therapy.
Another important finding of the present study pertains to the varied postmortem levels of AEDs, ranging from the supra-therapeutic level to zero, mostly at sub-therapeutic concentration or being negative. Out of the 388 cases, 218 cases (56.2%) were at sub-therapeutic or negative levels of AEDs. Low levels of AEDs in postmortem blood have been proposed as a strong predictor of SUDEP, for low AED levels reflecting an inadequate dosage or non-compliance before death (42). However, some studies argued that detecting sub-therapeutic AED levels at autopsy has limited value in determining the cause of death, due to uncertainties in the correlation of postmortem whole blood levels with antemortem serum levels and the definition of a therapeutic level (43). In a recently published study comparing 13 SUDEP cases with 18 non-SUDEP forensic autopsy cases, the authors also found no significant difference between the two groups of cases with regard to the use of AEDs when considering postmortem toxicological results (44). Though the connection between sub-therapeutic or absent AEDs and the occurrence of SUDEP remains to be debated, the adjuvant use of antipsychotic drugs serving as an underlying mechanism of SUDEP received widespread attention. Psychiatric comorbidity is common in patients with epilepsy, and antipsychotic drugs may be prescribed more commonly among patients with epilepsy than in the general population (45). Antipsychotics could induce cardiac side effects, including heart rate changes, blood pressure alterations, and more severe and fatal issues, such as QTc prolongation, congestive heart failure, and even sudden unexpected death (46) via directly binding to cardiac CB1R (47) or disturbing spliceosome signaling (48). Therefore, it is necessary to evaluate the safety and efficiency of antipsychotic medications among patients with epilepsy, and their potential contribution toward SUDEP.
Our study has several limitations. First, due to a lack of information on individual race, we were unable to determine whether neurological, cardiac, and pulmonary pathologies have racial differences or not. Second, due to technical limitations, we failed to obtain sufficient information on patients' medical records, such as the clinical type of seizure. Collaborative studies involving both clinical physicians and forensic pathologists would be more helpful in illustrating the characteristics of SUDEP.
5. Conclusion
In all, we systemically analyzed the neurological, cardiac, and pulmonary pathology for SUDEP using cases from both our forensic center and literature resources. Neuropathology was the most common change for such cases. While all these changes do not explain the cause of death, our study might pave the way for understanding the pathogenesis of SUDEP and the interpretation of death. The present study also highlighted the standard examination of the vital organs in circumstances of such cases.
Data availability statement
The original contributions presented in the study are included in the article/supplementary material, further inquiries can be directed to the corresponding author.
Ethics statement
The studies involving human participants were reviewed and approved by Ethical Review Board at the School of Basic Medical Science, Gannan Medical University. The patients/participants provided their written informed consent to participate in this study. Written informed consent was obtained from the individual(s) for the publication of any potentially identifiable images or data included in this article.
Author contributions
FY and YC were involved in the conception and design of the study and wrote the original draft. FZ, YY, and LZ were involved in the forensic data collection, literature search, and data analysis. All authors have read and agreed to the published version of the manuscript.
Funding
This study received funding from the open project of the Key Laboratory of Forensic Pathology, Ministry of Public Security (No. GAFYBL201903), the Science and Technology Project of Jiangxi Provincial Department of Education (No. GJJ160979), the Research Project of Gannan Medical University (No. XN201924), and the open project of the Key Laboratory of Prevention and Treatment of Cardiovascular and Cerebrovascular Diseases of Ministry of Education, Gannan Medical University (No. XN201810).
Conflict of interest
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
Publisher's note
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
References
1. Nashef L, So EL, Ryvlin P, Tomson T. Unifying the definitions of sudden unexpected death in epilepsy. Epilepsia. (2012) 53:227. doi: 10.1111/j.1528-1167.2011.03358.x
2. Thurman DJ, Hesdorffer DC, French JA. Sudden unexpected death in epilepsy: assessing the public health burden. Epilepsia. (2014) 55:1479–85. doi: 10.1111/epi.12666
3. Harden C, Tomson T, Gloss D, Buchhalter J, Cross JH, Donner E, et al. Practice guideline summary: sudden unexpected death in epilepsy incidence rates and risk factors: report of the guideline development, dissemination, and implementation subcommittee of the American Academy of Neurology and the American Epilepsy Society. Neurology. (2017) 88:1674–80. doi: 10.1212/WNL.0000000000003685
4. Devinsky O, Hesdorffer DC, Thurman DJ, Lhatoo S, Richerson G. Sudden unexpected death in epilepsy: epidemiology, mechanisms, and prevention. Lancet Neurol. (2016) 15:1075–88. doi: 10.1016/S1474-4422(16)30158-2
5. DeGiorgio CM, Curtis A, Hertling D, Moseley BD. Sudden unexpected death in epilepsy: risk factors, biomarkers, and prevention. Acta Neurol Scand. (2019) 139:220–30. doi: 10.1111/ane.13049
6. Thom M, Boldrini M, Bundock E, Sheppard MN, Devinsky O. Review: the past, present and future challenges in epilepsy-related and sudden deaths and biobanking. Neuropathol Appl Neurobiol. (2018) 44:32–55. doi: 10.1111/nan.12453
7. Barranco R, Caputo F, Molinelli A, Ventura F. Review on post-mortem diagnosis in suspected SUDEP: currently still a difficult task for forensic pathologists. J Forensic Leg Med. (2020) 70:101920. doi: 10.1016/j.jflm.2020.101920
8. Manolis TA, Manolis AA, Melita H, Manolis AS. Sudden unexpected death in epilepsy: the neuro-cardio-respiratory connection. Seizure. (2019) 64:65–73. doi: 10.1016/j.seizure.2018.12.007
9. Costagliola G, Orsini A, Coll M, Brugada R, Parisi P, Striano P. The brain-heart interaction in epilepsy: implications for diagnosis, therapy, and SUDEP prevention. Ann Clin Transl Neurol. (2021) 8:1557–68. doi: 10.1002/acn3.51382
10. Fialho GL, Wolf P, Walz R, Lin K. SUDEP—more attention to the heart? A narrative review on molecular autopsy in epilepsy. Seizure. (2021) 87:103–6. doi: 10.1016/j.seizure.2021.03.010
11. Sahly AN, Shevell M, Sadleir LG, Myers KA SUDEP risk and autonomic dysfunction in genetic epilepsies. Auton Neurosci. (2022) 237:102907. doi: 10.1016/j.autneu.2021.102907
12. Olesen JB, Abildstrom SZ, Erdal J, Gislason GH, Weeke P, Andersson C, et al. Effects of epilepsy and selected antiepileptic drugs on risk of myocardial infarction, stroke, and death in patients with or without previous stroke: a nationwide cohort study. Pharmacoepidemiol Drug Saf. (2011) 20:964–71. doi: 10.1002/pds.2186
13. Chen Y, Zhang F, Yan Y, Wang S, Zhang L, Yan F. Sudden cardiac death in schizophrenia during hospitalization: an autopsy-based study. Front Psychiatry. (2022) 13:933025. doi: 10.3389/fpsyt.2022.933025
14. Sun D, Li L, Zhang X, Blanchard TG, Fowler DR, Li L. Causes of sudden unexpected death in schizophrenia patients: a forensic autopsy population study. Am J Forensic Med Pathol. (2019) 40:312–7. doi: 10.1097/PAF.0000000000000512
15. Terrence CF, Rao GR, Perper JA. Neurogenic pulmonary edema in unexpected, unexplained death of epileptic patients. Ann Neurol. (1981) 9:458–64. doi: 10.1002/ana.410090508
16. Leestma JE, Walczak T, Hughes JR, Kalelkar MB, Teas SS. A prospective study on sudden unexpected death in epilepsy. Ann Neurol. (1989) 26:195–203. doi: 10.1002/ana.410260203
17. Earnest MP, Thomas GE, Eden RA, Hossack KF. The sudden unexplained death syndrome in epilepsy: demographic, clinical, and postmortem features. Epilepsia. (1992) 33:310–6. doi: 10.1111/j.1528-1157.1992.tb02321.x
18. Natelson BH, Suarez RV, Terrence CF, Turizo R. Patients with epilepsy who die suddenly have cardiac disease. Arch Neurol. (1998) 55:857–60. doi: 10.1001/archneur.55.6.857
19. Antoniuk SA, Oliva LV, Bruck I, Malucelli M, Yabumoto S, Castellano JL. Sudden unexpected, unexplained death in epilepsy autopsied patients. Arq Neuropsiquiatr. (2001) 59:40–5. doi: 10.1590/S0004-282X2001000100009
20. Shields LB, Hunsaker DM, Hunsaker JC 3rd, Parker JC Jr. Sudden unexpected death in epilepsy: neuropathologic findings. Am J Forensic Med Pathol. (2002) 23:307–14. doi: 10.1097/00000433-200212000-00001
21. Swallow RA, Hillier CE, Smith PE. Sudden unexplained death in epilepsy (SUDEP) following previous seizure-related pulmonary oedema: case report and review of possible preventative treatment. Seizure. (2002) 11:446–8. doi: 10.1053/seiz.2002.0683
22. Simona PCT, Dalager-Pedersen S, Baandrup U, Dam M, Vesterby-Charles A. Sudden unexpected death in epilepsy: is death by seizures a cardiac disease? Am J Forensic Med Pathol. (2005) 26:99–105. doi: 10.1097/01.paf.0000159993.01962.c5
23. Pollanen MS, Kodikara S. Sudden unexpected death in epilepsy: a retrospective analysis of 24 adult cases. Forensic Sci Med Pathol. (2012) 8:13–8. doi: 10.1007/s12024-011-9263-4
24. Zhuo L, Zhang Y, Zielke HR, Levine B, Zhang X, Chang L, et al. Sudden unexpected death in epilepsy: evaluation of forensic autopsy cases. Forensic Sci Int. (2012) 223:171–5. doi: 10.1016/j.forsciint.2012.08.024
25. Ryvlin P, Nashef L, Lhatoo SD, Bateman LM, Bird J, Bleasel A, et al. Incidence and mechanisms of cardiorespiratory arrests in epilepsy monitoring units (MORTEMUS): a retrospective study. Lancet Neurol. (2013) 12:966–77. doi: 10.1016/S1474-4422(13)70214-X
26. Hashimoto M, Nakajima M, Kuroda R, Yamaguchi R, Maeda H, Nagai H, et al. Sudden unexpected death in a patient with epilepsy presenting with high N-terminal probrain natriuretic peptide level, cardiac lesions, and pulmonary edema. Int J Cardiol. (2014) 172:e265–7. doi: 10.1016/j.ijcard.2013.12.069
27. Esen Melez I, Arslan MN, Melez DO, Sanli AN, Koc S. Sudden unexpected death in epilepsy: a retrospective autopsy study of 112 epileptic patients. Noro Psikiyatr Ars. (2017) 54:225–33. doi: 10.5152/npa.2016.14863
28. Neff JL, Lin PT. An unexpected finding in SUDEP involving a child: focal myocardial infarct adjacent to bundle of his. J Forensic Sci. (2017) 62:1662–4. doi: 10.1111/1556-4029.13454
30. Jordan RD, Coscia M, Lantz P, Harrison W. Sudden unexpected death in epilepsy: a report of three commonly encountered anatomic findings in the forensic setting with recommendations for best practices. Am J Forensic Med Pathol. (2022) 43:259–62. doi: 10.1097/PAF.0000000000000773
31. Ellis SP Jr, Szabo CA. Sudden unexpected death in epilepsy: incidence, risk factors, and proposed mechanisms. Am J Forensic Med Pathol. (2018) 39:98–102. doi: 10.1097/PAF.0000000000000394
32. Blumcke I, Spreafico R, Haaker G, Coras R, Kobow K, Bien CG, et al. Histopathological findings in brain tissue obtained during epilepsy surgery. N Engl J Med. (2017) 377:1648–56. doi: 10.1056/NEJMoa1703784
33. Blumcke I, Aronica E, Miyata H, Sarnat HB, Thom M, Roessler K, et al. International recommendation for a comprehensive neuropathologic workup of epilepsy surgery brain tissue: a consensus task force report from the ILAE commission on diagnostic methods. Epilepsia. (2016) 57:348–58. doi: 10.1111/epi.13319
34. Leitner DF, Faustin A, Verducci C, Friedman D, William C, Devore S, et al. Neuropathology in the North American sudden unexpected death in epilepsy registry. Brain Commun. (2021) 3:fcab192. doi: 10.1093/braincomms/fcab192
35. Thom M, Michalak Z, Wright G, Dawson T, Hilton D, Joshi A, et al. Audit of practice in sudden unexpected death in epilepsy (SUDEP) post mortems and neuropathological findings. Neuropathol Appl Neurobiol. (2016) 42:463–76. doi: 10.1111/nan.12265
36. Rose S, Wu S, Jiang A, Kim J, Tao JX. Neurogenic pulmonary edema: an etiological factor for SUDEP? Epilepsy Behav. (2015) 52:76. doi: 10.1016/j.yebeh.2015.08.010
37. Nascimento FA, Tseng ZH, Palmiere C, Maleszewski JJ, Shiomi T, McCrillis A, et al. Pulmonary and cardiac pathology in sudden unexpected death in epilepsy (SUDEP). Epilepsy Behav. (2017) 73:119–25. doi: 10.1016/j.yebeh.2017.05.013
38. Jaychandran R, Chaitanya G, Satishchandra P, Bharath RD, Thennarasu K, Sinha S. Monitoring peri-ictal changes in heart rate variability, oxygen saturation and blood pressure in epilepsy monitoring unit. Epilepsy Res. (2016) 125:10–8. doi: 10.1016/j.eplepsyres.2016.05.013
39. Devinsky O, Kim A, Friedman D, Bedigian A, Moffatt E, Tseng ZH. Incidence of cardiac fibrosis in SUDEP and control cases. Neurology. (2018) 91:e55–61. doi: 10.1212/WNL.0000000000005740
40. Raju H, Parsons S, Thompson TN, Morgan N, Zentner D, Trainer AH, et al. Insights into sudden cardiac death: exploring the potential relevance of non-diagnostic autopsy findings. Eur Heart J. (2019) 40:831–8. doi: 10.1093/eurheartj/ehy654
41. Papadakis M, Raju H, Behr ER, De Noronha SV, Spath N, Kouloubinis A, et al. Sudden cardiac death with autopsy findings of uncertain significance: potential for erroneous interpretation. Circ Arrhythm Electrophysiol. (2013) 6:588–96. doi: 10.1161/CIRCEP.113.000111
42. Lund A, Gormsen H. The role of antiepileptics in sudden death in epilepsy. Acta Neurol Scand. (1985) 72:444–6. doi: 10.1111/j.1600-0404.1985.tb00898.x
43. Lathers CM, Koehler SA, Wecht CH, Schraeder PL. Forensic antiepileptic drug levels in autopsy cases of epilepsy. Epilepsy Behav. (2011) 22:778–85. doi: 10.1016/j.yebeh.2011.10.011
44. Zhang X, Zhang J, Wang J, Zou D, Li Z. Analysis of forensic autopsy cases associated with epilepsy: comparison between sudden unexpected death in epilepsy (SUDEP) and not SUDEP groups. Front Neurol. (2022) 13:1077624. doi: 10.3389/fneur.2022.1077624
45. Natalia G, Jakub S, Wieslaw J. Antipsychotic drugs in epilepsy. Neurol Neurochir Pol. (2019) 53:408–12. doi: 10.5603/PJNNS.a2019.0052
46. Li X, Tang X, Li L. Antipsychotics cardiotoxicity: what's known and what's next. World J Psychiatry. (2021)11:736–753. doi: 10.5498/wjp.v11.i10.736
47. Li L, Gao P, Tang X, Liu Z, Cao M, Luo R, et al.CB1R-stabilized NLR3 inflammasome drives antipsychotic cardiotoxicity. Signal Transduct Target Ther. (2022) 7:190. doi: 10.1038/s41392-022-01018-7
Keywords: epilepsy, SUDEP, autopsy, cause of death, forensic pathology
Citation: Yan F, Zhang F, Yan Y, Zhang L and Chen Y (2023) Sudden unexpected death in epilepsy: Investigation of autopsy-based studies. Front. Neurol. 14:1126652. doi: 10.3389/fneur.2023.1126652
Received: 18 December 2022; Accepted: 23 January 2023;
Published: 16 February 2023.
Edited by:
Beixu Li, Shanghai University of Political Science and Law, ChinaCopyright © 2023 Yan, Zhang, Yan, Zhang and Chen. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Fengping Yan,  dG9tamlhbmd4aUAxNjMuY29t; Yuanyuan Chen,
dG9tamlhbmd4aUAxNjMuY29t; Yuanyuan Chen,  Y2hlbl95dWFueXVhbjIwMDhAMTYzLmNvbQ==
Y2hlbl95dWFueXVhbjIwMDhAMTYzLmNvbQ==
 Fengping Yan
Fengping Yan Fu Zhang
Fu Zhang Yanan Yan1,2
Yanan Yan1,2