- 1Department of Biomedical Engineering, Shantou University, Shantou, China
- 2National Research Center for Rehabilitation Technical Aids, Ministry of Civil Affairs, Beijing, China
Telerehabilitation (TR) is a new model to provide rehabilitation services to stroke survivors. It is a promising approach to deliver mainstream interventions for movement, cognitive, speech and language, and other disorders. TR has two major components: information and communication technologies (ICTs) and stroke interventions. ICTs provide a platform on which interventions are delivered and subsequently result in stroke recovery. In this mini-review, we went over features of ICTs that facilitate TR, as well as stroke interventions that can be delivered via TR platforms. Then, we reviewed the effects of TR on various stroke disorders. In most studies, TR is a feasible and effective solution in delivering interventions to patients. It is not inferior to usual care and in-clinic therapy with matching dose and intensity. With new technologies, TR may result in better outcomes than usual care for some disorders. One the other hand, TR also have many limitations that could lead to worse outcomes than traditional rehabilitation. In the end, we discussed major concerns and possible solutions related to TR, and also discussed potential directions for TR development.
1. Introduction
Stroke is a leading cause of death and disability globally (1). The occurrence of stroke is increasing rapidly in terms of absolute numbers due to population aging (2). Worldwide in 2019, there are 143 million stroke survivors suffering from various symptoms such as hemiplegia, aphasia and depression, which greatly impair their independency and cause tremendous burden to patients, their family and the society (3, 4). Extensive studies demonstrated that proper rehabilitation programs can ease stroke symptoms, reduce long-term disability, and improve quality of life (5, 6). Patients should start rehabilitation as early as possible in order to prevent chronic damage to the brain (7), and continue to do so even after recovery is slower than before (8). Traditionally, rehabilitation services are provided by healthcare professionals in clinic settings. But this is difficult for patients living in remote areas, especially in low- and middle-income countries. They have no access to rehabilitation services or they have to take extra time and efforts to travel a long distance. In this situation, telerehabilitation (TR) can offer an alternative way to deliver services (9).
By using information and communication technologies (ICTs), TR is able to minimize the barrier of distance between patients and rehabilitation providers (10). The role of ICTs is to ensure traditional in-clinic rehabilitation services delivered remotely to patients as effectively as possible. TR is not a new subspeciality (9); instead, it covers all aspects of rehabilitation, including “evaluation, assessment, monitoring, prevention, intervention, supervision, education, consultation, and coaching (11).” There are a number of advantages to use TR for stroke patients. TR can save time and money, make the access to healthcare professionals easier, and provide extra training opportunities for interventions requiring higher dose. It also helped to decrease infection rates of certain diseases, and may provide emotional support to patients for being at home (12, 13).
In this mini-review, we will focus on two major components of TR: ICTs and stroke interventions, as well as outcomes of TR for various stroke conditions. ICTs serve as platforms on which interventions are delivered. Both of them are the keys to feasibility, effectiveness and safety of TR as well as to patients’ satisfaction and adherence. Previous reviews regarding stroke and TR are mainly focused on one aspect, such as upper limb rehabilitation or application of virtual reality (14, 15). So, we think it is necessary to provide an overall picture in order to summarize key factors in this topic. In the end, we also discussed existing issues and potential future development.
2. Information and communication technologies in telerehabilitation
ICTs are the foundation of TR, allowing stroke survivors to achieve optimal recovery outcomes by utilizing home-based therapies (16). There are a number of ICTs available, including text, audio, visual, mobile-based, computer-based, web-based, sensors and wireless devices (17). The major purpose of ICTs is to provide a platform for patients to receive rehabilitation services as if in clinical settings. The platform should be safe, user friendly and feasible to apply stroke interventions to all users with high tolerance for error (18). When possible, the platform should be easily modified to deliver personalized service. The considerations of building up a TR platform involve a variety of factors, such as effectiveness of intervention, customer support, cost, accessibility, usability and acceptability (19). For example, low-cost platform may be not effective enough but can be afforded by most people; while high-cost platform usually is more complicated with a higher learning curve resulting in less use.
Telephone is one of the earliest TR methods and still frequently used today. In a recent study by Cha et al. (20), nurse-initiated phone call interventions are able to increase physical activities of subacute patients after hospital discharge. Calls to discuss patients’ conditions may also increase their adherence to therapy and satisfaction with it (21). It is also used in goal setting programs for self-management of daily activities and stroke knowledge education (22). These results suggest that low-cost solutions, such as telephone and text, are still viable in plenty of situations.
Videoconferencing is an upgrade option of telephone service, providing both audio and visual communication between patients and healthcare professionals. Videoconferencing can be mobile-based or computer-based to support face-to-face information exchange. Li et al. (23). investigated feasibility, validity, and reliability of using videoconferencing for functional assessments of stroke patients after hospital discharge, and telephone service and home visit were used as controls. The functional status of patients was measured at the end of 2 weeks and 3 months. The authors found that patients offered videoconferencing and home visit have similar scores in functional status. Videoconferencing has higher validity and reliability than telephone based on measures from this study. Patients in videoconferencing group also showed high satisfaction and confidence. The results suggest that videoconferencing is a better solution than telephone.
Mobile-based, computer-based and web-based ICTs are usually integrated into interventions in the form of games, virtual reality (VR) and other trainings. They can deliver user training data to healthcare professionals for evaluation (17). They also can be combined with videoconferencing for better outcomes. Wearable sensors are used to collect patients’ data in order to monitor their status including falls, heart rate, blood pressure, respiratory rate and blood oxygen levels (24). In a study by Asano et al. (25), 61 patients performed rehabilitation training though tablet-based TR system followed by a review through videoconferencing. Sensers were used to obtain their physiological signals to find adverse effects from TR for safety reason. Nasrabadi et al. (26) developed an activity recognition system based on inertial measurement units (IMU) for TR. The system can be used to track body motion during movement-based therapies in order to detect wrong actions and to assess training effectiveness. Accelerometer, gyroscope and electromyograph (EMG) sensors are also frequently used to track body motion and muscle activities. Furthermore, artificial intelligence (AI) approach was increasingly used in stroke rehabilitation. For example, machine learning methods were adopted as a promising support tool for clinicians to predict functional recovery of stroke patients (27). Major technologies used in TR were summarized in Figure 1.
3. Interventions and related technologies in telerehabilitation
According to a highly cited review article, interventions for stroke recovery were divided into four types. They are training interventions, technological interventions, pharmacological interventions and neuromodulation interventions (28). Among them, pharmacological interventions are not directly associated to TR. Thus, we will consider only the other three types of interventions below.
Both training interventions and technological interventions are related to physical activity and exercise. The former is in the form of strength or/and task-oriented trainings, while the latter consists of serious gaming, VR and robotics. These interventions are not mutually exclusive. Instead, they can be combined together to achieve optimal outcomes for stroke recovery. For example, Lee et al. (29) studied the role of a smart glove in upper limb function recovery. Participants were asked to perform task-oriented actions in a VR environment. The control group takes usual care plus recreational activities. As a result, the intervention group demonstrated better outcomes for all measures. Hao et al. (15) reviewed effects of VR-based TR systems including totally 260 stroke patients. The VR-TR group showed similar outcomes to in-person rehabilitation group in terms of upper limb and balance functions. Rozevink et al. (30) studied the effects of an upper limb robot-assisted serious game therapy in a TR setting. Their system significantly improved motor function of patients with high satisfaction and adherence.
Neuromodulation interventions include electrical stimulation and magnetic stimulation for the purpose to enhance neural pathways of different human body systems (24). Electrical stimulation (ES) is a popular and well-established intervention for stroke therapy, and it can be broken down into several subcategories, such as functional electrical stimulation (FES) for peripheral nerve system and transcranial direct current stimulation (tDCS) for central nerve system (31, 32). The effectiveness of ES for stroke recovery has been extensively studied with positive results (33, 34). But these interventions require sufficient knowledge and experience in order to operate ES devices properly. Additionally, there are also safety concerns. As a result, there are very few studies combining ES and TR for stroke recovery. Hermann et al. (35) examined the efficacy of FES treatment for post-stroke arm disorder, while Ko et al. (36) reported the use of home-based tDCS for cognitive training. Their data suggest that using ES in TR is promising. On the hand, transcranial magnetic stimulation (TMS) has been widely used to treat various stroke conditions (37, 38). But it has not been used in TR in our literature search, possibly because TMS device is very expensive and complex. The use of neuromodulation interventions in TR is just starting to receive attention, and further studies are needed to examine their outcomes.
4. Effects of telerehabilitation on post-stroke functional impairments
4.1. Movement disorders
Majority stroke survivors suffer from movement disorders (39), and rehabilitation practices are the key to help patients to regain their lost abilities (28). In a random clinical trial (RCT), 124 patients with arm motor disorders were equally divided into two groups – TR group and in-clinic therapy group. All patient received thirty six 72-min sessions of identical interventions in the form of daily functional games, exercise videos, and stroke education. The results demonstrated that both groups have significant gains in arm functionality based on Fugl-Meyer (FM) scores with high satisfaction, and there is no significant difference between the two groups. But in-clinic therapy group showed better adherence compared to TR group (40). In a similar study, the authors found that early TR after stroke is suitable for intensive arm motor trainings with excellent feasibility, safety and efficacy (41). Stzurm et al. (42) developed a computer game-assisted TR platform to improve compliance and accessibility of rehabilitation programs for individuals. They found that the TR service resulted significant improvement of patients’ hand-arm functions which were evaluated by Wolf Motor Function Test and a customized computer-based system. Additionally, robotic rehabilitation for motor recovery via TR service substantially improved the upper limb function of patients with high satisfaction (43, 44).
For lower limb related disorders, Held et al. (45) developed an autonomous TR system for balance and gait recovery. During a 12-week period, patients play exercise games in a VR environment for 40 min per session. Their results suggest the TR system is safe, feasible and able to provide intensive therapy at home for lower limb trainings. Lin et al. (46) recruited 24 chronic stroke patients who were asked to perform a 50-min balance training session, and three times each week. The authors found that TR increased balance abilities of patients in terms of Berg Balance Scale, and there is no difference in training effect and satisfaction between TR group and conventional therapy group. In another study, patients reported high acceptability and satisfaction of a serious game-based TR system for ankle movements (47).
TR also plays an important role in the recovery of activities of daily living (ADL) after stroke, which is a key indicator of one’s functional status. In a systematic review, the authors conclude that there is no significant difference between TR intervention group and in-person physical therapy group, as well as usual care group (10). These studies suggest that TR is a feasible and effective way to improve motor functions of stroke patients, and its effects are not inferior to traditional therapies. But augmented TR training may be not effective in improving physical function compared with usual care (48).
4.2. Cognitive disorders
Post-stroke cognitive disorders may result in tremendous reduction in quality of life and independence on ADL, and they can also lead to poor adherence to treatments (49). In a study by Faria et al. (50), 36 chronic stroke patients were recruited, and divided into two groups – adaptive VR-based TR group and paper-and-pencil-based control group with task generator. Both groups performed equivalent cognitive trainings for 12 sessions over 1 month. The results showed that the TR group had significant improvement in cognitive functions compared to control group. In another study, VR-based cognitive TR also resulted better outcomes than traditional rehabilitation for stroke patients in terms of global cognitive level, attentive, memory and linguistic skills (51). Additionally, Lawson et al. demonstrated feasibility of TR in cognitive trainings as well as its non-inferiority compared with their previous in-person rehabilitation trainings (52). Bernini et al. (53, 54) also showed TR is not inferior to in-person rehabilitation with satisfiable user experience for general cognitive disorders. Overall, TR system is feasible for cognitive trainings, and has similar or better performance compared to traditional cognitive training methods.
4.3. Speech and language disorders
Aphasia has an occurrence rate of 30% in hospitalized stroke patients. It often leads to social isolation and low mood, and was rated as one of the worst diseases that has negative impact on quality of life (55). Meltzer et al. evaluated the effectiveness of TR for communication disorders by conducting identical treatments with 44 patients for TR group and in-person group. After 10-week treatment, all patients had significant improvement on evaluated indices, and the gain is similar for both groups. Their findings suggest that TR is highly effective for communication disorders (56). In another study, Maresca et al. conducted a RCT consisting of 30 patients with aphasia, who were assigned to either control group trained with a conventional treatment or experimental group trained with tablet-based TR platform. After 6-month treatment, the experimental group demonstrated significant improvement in all evaluations expect writing, and performed much better than control group (57). Similarly, a web-based application demonstrated TR is effective way for aphasia training (58). Ora et al. also conducted a RCT consisting of a TR group and a control group with 31 patients for each. Both of them received usual care, but TR group also received additional 5-h training per week. As a result, there is no significant difference between the two groups for assessed indicis after 4 weeks (59). In a another study by the same authors, TR were shown to be a feasible and acceptable way for aphasia training (60). A review suggests intensity of therapy is the key for aphasia trainings (61), thus TR may serve as a complementary intervention for better outcomes.
4.4. Other disorders
Approximately 50% of stroke patients have swallowing disorders, and TR composed of motion and muscle exercises can effectively improve swallow functions with high patient satisfaction (62). Wearable EMG sensors can monitor swallowing activities and subsequently detect dysphagia in remote settings (63). TR is also used to reduce post-stroke depression, and telephone intervention demonstrated similar effects in reducing depression to usual care or in-person intervention (64).
5. Discussion
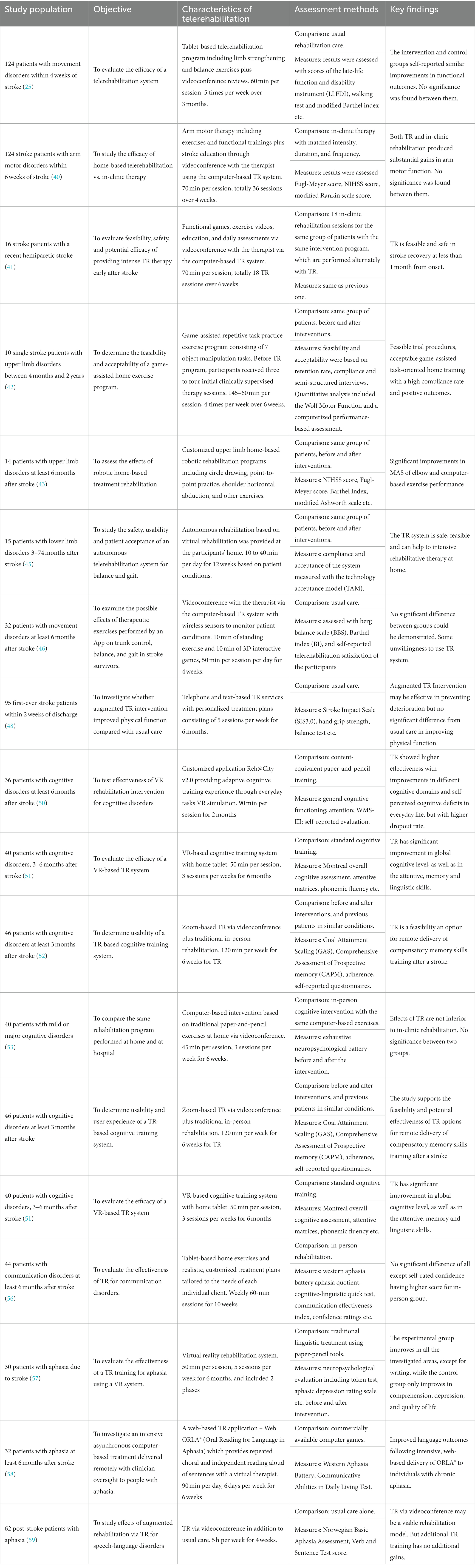
As shown in Table 1, TR demonstrated considerable feasibility and effectiveness for stroke recovery. It is not inferior to usual care and in-clinic therapy with matched intensity, duration, and frequency. It also has a high satisfaction rate among stroke patients. But TR is probably not suitable for every patient because of technical barriers and various personal reasons. TR treatments have a higher dropout rate than traditional rehabilitation programs because some patients, especially those with cognitive disorders, have difficulties in completing the training session remotely (50). Additionally, without healthcare professionals standing aside, many patients have less confidence and motivation to conduct interventions, which subsequently results in low adherence and poorer clinical outcomes. Furthermore, some interventions requiring large, expensive or dangerous devices may be not suitable for home settings. There are also some concerns in interpreting TR outcomes. First, inclusion and exclusion criteria for participants are not perfect due to limited availability of patients (40). Second, cohort studies lack control groups, which may lead to wrong conclusions (42). Third, satisfaction and other self-reported data are not subjective (41). On the other hand, a recent survey research regarding telemedicine showed that majority physicians and patients still prefer in-person care, because they do not trust the quality of TR. Lack of physical exam and intervention accuracy were cited as key reasons (65). The results also suggest that self-reported satisfaction rate from patients may be questionable.
To address above-mentioned issues, technological advances are the key. Intelligent devices requiring less efforts from patients can overcome technical barriers in usability. VR and haptic devices can be used to create an environment mimicking clinic setting to increase confidence and motivation of patients (66, 67). Additionally, many devices for stroke interventions can be redesigned to adapt TR platforms. For example, FES and tDCS devices have already been used for neuromodulation in TR (68), but the number of studies is very limited mainly for safety reasons. With additions of remote control and extensive safety mechanisms, ES devices have potential to be used in TR more frequently. To address the lack of physical exam and accuracy in TR, wearable sensors can be used to acquire a variety of parameters of patients and to monitor their health conditions and activities (69, 70). Thus, healthcare professionals can detect adverse effects during TR and make better intervention plans.
With further development of technologies, fully digitalized TR system may be possible. TR-based interventions, which combine serious games, immersive VR, rehabilitation robots and various sensors, have possibility to achieve better outcomes. Patients’ data can be collected with sensors and analyzed though machine learning approach. Traditional measures for evaluating intervention outcomes, such as Berg balance scale, can be performed automatically with proper devices (71, 72). Besides technology aspects, new TR models should also be considered. Community health workers and caregivers have received much attention (73, 74), but their roles in TR were not fully explored. They can serve as a bridge between healthcare professionals and patients to overcome certain communication-related issues and technical barriers. Overall speaking, TR is still in its developing stage, and further studies are needed to provide evidence for optimal use of TR.
Author contributions
YX and QW wrote and finalized the manuscript. JX and BZ provided support in reference searching. All authors contributed to the article and approved the submitted version.
Funding
The research was supported by Research Startup Funding of Shantou University #NTF21014 to YX.
Conflict of interest
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
Publisher’s note
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
Supplementary material
The Supplementary material for this article can be found online at: https://www.frontiersin.org/articles/10.3389/fneur.2023.1234003/full#supplementary-material
References
1. Owolabi, MO, Thrift, AG, Mahal, A, Ishida, M, Martins, S, Johnson, WD, et al. Primary stroke prevention worldwide: translating evidence into action. Lancet Public Health. (2022) 7:e74–85. doi: 10.1016/S2468-2667(21)00230-9
2. Feigin, VL, Norrving, B, and Mensah, GA. Global burden of stroke. Circ Res. (2017) 120:439–48. doi: 10.1161/CIRCRESAHA.116.308413
4. GBD 2019 Stroke Collaborators. Global, regional, and national burden of stroke and its risk factors, 1990-2019: a systematic analysis for the global burden of disease study 2019. Lancet Neurol. (2021) 20:795–820. doi: 10.1016/S1474-4422(21)00252-0
5. Pollock, A, Baer, G, Campbell, P, Choo, PL, Forster, A, Morris, J, et al. Physical rehabilitation approaches for the recovery of function and mobility following stroke. Cochrane Database Syst Rev. (2014) 2014:Cd001920. doi: 10.1002/14651858.CD001920.pub3
6. Kuriakose, D, and Xiao, ZC. Pathophysiology and treatment of stroke: present status and future perspectives. Int J Mol Sci. (2020) 21:7609. doi: 10.3390/ijms21207609
7. Ostrowska, PM, Śliwiński, M, Studnicki, R, and Hansdorfer-Korzon, R. Telerehabilitation of post-stroke patients as a therapeutic solution in the era of the Covid-19 pandemic. Healthcare. (2021) 9:654. doi: 10.3390/healthcare9060654
8. Boyd, LA, Hayward, KS, Ward, NS, Stinear, CM, Rosso, C, Fisher, RJ, et al. Biomarkers of stroke recovery: consensus-based core recommendations from the stroke recovery and rehabilitation roundtable. Int J Stroke. (2017) 12:480–93. doi: 10.1177/1747493017714176
9. Winters, JM. Telerehabilitation research: emerging opportunities. Annu Rev Biomed Eng. (2002) 4:287–320. doi: 10.1146/annurev.bioeng.4.112801.121923
10. Laver, KE, Adey-Wakeling, Z, Crotty, M, Lannin, NA, George, S, and Sherrington, C. Telerehabilitation services for stroke. Cochrane Database Syst Rev. (2020) 1:Cd010255. doi: 10.1002/14651858.CD010255.pub3
11. Shem, K, Irgens, I, and Alexander, M. Chapter 2—getting started: mechanisms of telerehabilitation In: M Alexander, editor. Telerehabilitation. New Delhi: Elsevier (2022). 5–20.
12. Digital Technologies, Web and Social Media Study Group of the Italian Society of NeurologyIodice, F, Romoli, M, Giometto, B, Clerico, M, Tedeschi, G, et al. Stroke and digital technology: a wake-up call from COVID-19 pandemic. Neurol Sci. (2021) 42:805–9. doi: 10.1007/s10072-020-04993-3
13. Prvu Bettger, J, and Resnik, LJ. Telerehabilitation in the age of COVID-19: an opportunity for learning health system research. Phys Ther. (2020) 100:1913–6. doi: 10.1093/ptj/pzaa151
14. Moulaei, K, Sheikhtaheri, A, Nezhad, MS, Haghdoost, AA, Gheysari, M, and Bahaadinbeigy, K. Telerehabilitation for upper limb disabilities: a scoping review on functions, outcomes, and evaluation methods. Arch Public Health. (2022) 80:196. doi: 10.1186/s13690-022-00952-w
15. Hao, J, Pu, Y, Chen, Z, and Siu, KC. Effects of virtual reality-based telerehabilitation for stroke patients: a systematic review and meta-analysis of randomized controlled trials. J Stroke Cerebrovasc Dis. (2023) 32:106960. doi: 10.1016/j.jstrokecerebrovasdis.2022.106960
16. Neibling, BA, Jackson, SM, Hayward, KS, and Barker, RN. Perseverance with technology-facilitated home-based upper limb practice after stroke: a systematic mixed studies review. J Neuroeng Rehabil. (2021) 18:43. doi: 10.1186/s12984-021-00819-1
17. Edwards, D, Williams, J, Carrier, J, and Davies, J. Technologies used to facilitate remote rehabilitation of adults with deconditioning, musculoskeletal conditions, stroke, or traumatic brain injury: an umbrella review. JBI Evid Synth. (2022) 20:1927–68. doi: 10.11124/JBIES-21-00241
18. Krishnan, G. Telerehabilitation: an overview. Telehealth Med Today. (2021) 6:285. doi: 10.30953/tmt.v6.285
19. Nikolaev, VA, and Nikolaev, AA. Recent trends in telerehabilitation of stroke patients: a narrative review. NeuroRehabilitation. (2022) 51:1–22. doi: 10.3233/NRE-210330
20. Cha, S, Chang, WK, Cho, HM, Jung, YS, Kang, M, Paik, NJ, et al. The effect of a telephone-based intervention on physical activity after stroke. PLoS One. (2022) 17:e0276316. doi: 10.1371/journal.pone.0276316
21. Rochette, A, Korner-Bitensky, N, Bishop, D, Teasell, R, White, CL, Bravo, G, et al. The YOU CALL-WE CALL randomized clinical trial: impact of a multimodal support intervention after a mild stroke. Circ Cardiovasc Qual Outcomes. (2013) 6:674–9. doi: 10.1161/CIRCOUTCOMES.113.000375
22. Wan, LH, Zhang, XP, Mo, MM, Xiong, XN, Ou, CL, You, LM, et al. Effectiveness of goal-setting telephone follow-up on health Behaviors of patients with ischemic stroke: a randomized controlled trial. J Stroke Cerebrovasc Dis. (2016) 25:2259–70. doi: 10.1016/j.jstrokecerebrovasdis.2016.05.010
23. Li, L, Huang, J, Wu, J, Jiang, C, Chen, S, Xie, G, et al. A Mobile health app for the collection of functional outcomes after inpatient stroke rehabilitation: pilot randomized controlled trial. JMIR Mhealth Uhealth. (2020) 8:e17219. doi: 10.2196/17219
24. Eng, JJ, and Pastva, AM. Advances in remote monitoring for stroke recovery. Stroke. (2022) 53:2658–61. doi: 10.1161/STROKEAHA.122.038885
25. Asano, M, Tai, BC, Yeo, FYT, Yen, SC, Tay, A, Ng, YS, et al. Home-based tele-rehabilitation presents comparable positive impact on self-reported functional outcomes as usual care: the Singapore tele-technology aided rehabilitation in stroke (STARS) randomised controlled trial. J Telemed Telecare. (2021) 27:231–8. doi: 10.1177/1357633X19868905
26. Nasrabadi, AM, Eslaminia, AR, Bakhshayesh, PR, Ejtehadi, M, Alibiglou, L, and Behzadipour, S. A new scheme for the development of IMU-based activity recognition systems for telerehabilitation. Med Eng Phys. (2022) 108:103876. doi: 10.1016/j.medengphy.2022.103876
27. Campagnini, S, Arienti, C, Patrini, M, Liuzzi, P, Mannini, A, and Carrozza, MC. Machine learning methods for functional recovery prediction and prognosis in post-stroke rehabilitation: a systematic review. J Neuroeng Rehabil. (2022) 19:54. doi: 10.1186/s12984-022-01032-4
28. Stinear, CM, Lang, CE, Zeiler, S, and Byblow, WD. Advances and challenges in stroke rehabilitation. Lancet Neurol. (2020) 19:348–60. doi: 10.1016/S1474-4422(19)30415-6
29. Lee, HS, Lim, JH, Jeon, BH, and Song, CS. Non-immersive virtual reality rehabilitation applied to a task-oriented approach for stroke patients: a randomized controlled trial. Restor Neurol Neurosci. (2020) 38:165–72. doi: 10.3233/RNN-190975
30. Rozevink, SG, van der Sluis, CK, Garzo, A, Keller, T, and Hijmans, JM. HoMEcare aRm rehabiLItatioN (MERLIN): telerehabilitation using an unactuated device based on serious games improves the upper limb function in chronic stroke. J Neuroeng Rehabil. (2021) 18:48. doi: 10.1186/s12984-021-00841-3
31. Cheung, VCK, Niu, CM, Li, S, Xie, Q, and Lan, N. A novel FES strategy for poststroke rehabilitation based on the natural organization of neuromuscular control. IEEE Rev Biomed Eng. (2019) 12:154–67. doi: 10.1109/RBME.2018.2874132
32. Veldema, J, and Gharabaghi, A. Non-invasive brain stimulation for improving gait, balance, and lower limbs motor function in stroke. J Neuroeng Rehabil. (2022) 19:84. doi: 10.1186/s12984-022-01062-y
33. Lee, JH, Baker, LL, Johnson, RE, and Tilson, JK. Effectiveness of neuromuscular electrical stimulation for management of shoulder subluxation post-stroke: a systematic review with meta-analysis. Clin Rehabil. (2017) 31:1431–44. doi: 10.1177/0269215517700696
34. Andreopoulou, G, Busselli, G, Street, T, Bulley, C, Safari, R, van der Linden, ML, et al. Is functional electrical stimulation effective in improving walking in adults with lower limb impairment due to an upper motor neuron lesion? An umbrella review. Artif Organs. (2023). doi: 10.1111/aor.14563
35. Hermann, VH, Herzog, M, Jordan, R, Hofherr, M, Levine, P, and Page, SJ. Telerehabilitation and electrical stimulation: an occupation-based, client-centered stroke intervention. Am J Occup Ther. (2010) 64:73–81. doi: 10.5014/ajot.64.1.73
36. Ko, MH, Yoon, JY, Jo, YJ, Son, MN, Kim, DS, Kim, GW, et al. Home-based transcranial direct current stimulation to enhance cognition in stroke: randomized controlled trial. Stroke. (2022) 53:2992–3001. doi: 10.1161/STROKEAHA.121.037629
37. Kim, WS, Kwon, BS, Seo, HG, Park, J, and Paik, NJ. Low-frequency repetitive transcranial magnetic stimulation over Contralesional motor cortex for motor recovery in subacute ischemic stroke: a randomized sham-controlled trial. Neurorehabil Neural Repair. (2020) 34:856–67. doi: 10.1177/1545968320948610
38. Xi, X, Wang, H, Han, L, Ding, M, Li, J, Qiao, C, et al. Meta-analysis of repetitive transcranial magnetic stimulation combined with task-oriented training on upper limb function in stroke patients with hemiplegia. Medicine. (2023) 102:e33771. doi: 10.1097/MD.0000000000033771
39. Kim, J, Thayabaranathan, T, Donnan, GA, Howard, G, Howard, VJ, Rothwell, PM, et al. Global stroke statistics 2019. Int J Stroke. (2020) 15:819–38. doi: 10.1177/1747493020909545
40. Cramer, SC, Dodakian, L, le, V, See, J, Augsburger, R, McKenzie, A, et al. Efficacy of home-based telerehabilitation vs in-clinic therapy for adults after stroke: a randomized clinical trial. JAMA Neurol. (2019) 76:1079–87. doi: 10.1001/jamaneurol.2019.1604
41. Edwards, D, Kumar, S, Brinkman, L, Ferreira, IC, Esquenazi, A, Nguyen, T, et al. Telerehabilitation initiated early in post-stroke recovery: a feasibility study. Neurorehabil Neural Repair. (2023) 37:131–41. doi: 10.1177/15459683231159660
42. Szturm, T, Imran, Z, Pooyania, S, Kanitkar, A, and Mahana, B. Evaluation of a game based tele rehabilitation platform for in-home therapy of hand-arm function post stroke: feasibility study. PM R. (2021) 13:45–54. doi: 10.1002/pmrj.12354
43. Bressi, F, Campagnola, B, Cricenti, L, Santacaterina, F, Miccinilli, S, di Pino, G, et al. Upper limb home-based robotic rehabilitation in chronic stroke patients: a pilot study. Front Neurorobot. (2023) 17:1130770. doi: 10.3389/fnbot.2023.1130770
44. Hu, J, Zou, J, Wan, Y, Yao, Q, Dong, P, Li, G, et al. Rehabilitation of motor function after stroke: a bibliometric analysis of global research from 2004 to 2022. Front Aging Neurosci. (2022) 14:1024163. doi: 10.3389/fnagi.2022.1024163
45. Held, JP, Ferrer, B, Mainetti, R, Steblin, A, Hertler, B, Moreno-Conde, A, et al. Autonomous rehabilitation at stroke patients home for balance and gait: safety, usability and compliance of a virtual reality system. Eur J Phys Rehabil Med. (2018) 54:545–53. doi: 10.23736/S1973-9087.17.04802-X
46. Lin, KH, Chen, CH, Chen, YY, Huang, WT, Lai, JS, Yu, SM, et al. Bidirectional and multi-user telerehabilitation system: clinical effect on balance, functional activity, and satisfaction in patients with chronic stroke living in long-term care facilities. Sensors. (2014) 14:12451–66. doi: 10.3390/s140712451
47. Lim, H, Marjanovic, N, Luciano, C, and Madhavan, S. Feasibility and acceptability of game-based cortical priming and functional lower limb training in a remotely supervised home setting for chronic stroke: a case series. Front Rehabil Sci. (2022) 3:775496. doi: 10.3389/fresc.2022.775496
48. Saywell, NL, Vandal, AC, Mudge, S, Hale, L, Brown, P, Feigin, V, et al. Telerehabilitation after stroke using readily available technology: a randomized controlled trial. Neurorehabil Neural Repair. (2021) 35:88–97. doi: 10.1177/1545968320971765
49. Cumming, TB, Marshall, RS, and Lazar, RM. Stroke, cognitive deficits, and rehabilitation: still an incomplete picture. Int J Stroke. (2013) 8:38–45. doi: 10.1111/j.1747-4949.2012.00972.x
50. Faria, AL, Pinho, MS, and Bermúdez i Badia, S. A comparison of two personalization and adaptive cognitive rehabilitation approaches: a randomized controlled trial with chronic stroke patients. J Neuroeng Rehabil. (2020) 17:78. doi: 10.1186/s12984-020-00691-5
51. Torrisi, M, Maresca, G, de Cola, MC, Cannavò, A, Sciarrone, F, Silvestri, G, et al. Using telerehabilitation to improve cognitive function in post-stroke survivors: is this the time for the continuity of care? Int J Rehabil Res. (2019) 42:344–51. doi: 10.1097/MRR.0000000000000369
52. Lawson, DW, Stolwyk, RJ, Ponsford, JL, McKenzie, DP, Downing, MG, and Wong, D. Telehealth delivery of memory rehabilitation following stroke. J Int Neuropsychol Soc. (2020) 26:58–71. doi: 10.1017/S1355617719000651
53. Bernini, S, Panzarasa, S, Sinforiani, E, Quaglini, S, Cappa, SF, Cerami, C, et al. HomeCoRe for telerehabilitation in mild or major neurocognitive disorders: a study protocol for a randomized controlled trial. Front Neurol. (2021) 12:752830. doi: 10.3389/fneur.2021.752830
54. Bernini, S, Panzarasa, S, Quaglini, S, Costa, A, Picascia, M, Cappa, SF, et al. HomeCoRe system for telerehabilitation in individuals at risk of dementia: a usability and user experience study. Front Med. (2023) 10:1129914. doi: 10.3389/fmed.2023.1129914
55. Doogan, C, Dignam, J, Copland, D, and Leff, A. Aphasia recovery: when, how and who to treat? Curr Neurol Neurosci Rep. (2018) 18:90. doi: 10.1007/s11910-018-0891-x
56. Meltzer, JA, Baird, AJ, Steele, RD, and Harvey, SJ. Computer-based treatment of poststroke language disorders: a non-inferiority study of telerehabilitation compared to in-person service delivery. Aphasiology. (2018) 32:290–311. doi: 10.1080/02687038.2017.1355440
57. Maresca, G, Maggio, MG, Latella, D, Cannavò, A, de Cola, MC, Portaro, S, et al. Toward improving poststroke aphasia: a pilot study on the growing use of telerehabilitation for the continuity of care. J Stroke Cerebrovasc Dis. (2019) 28:104303. doi: 10.1016/j.jstrokecerebrovasdis.2019.104303
58. Cherney, LR, Lee, JB, Kim, KYA, and van Vuuren, S. Web-based Oral Reading for language in aphasia (web ORLA(®)): a pilot randomized control trial. Clin Rehabil. (2021) 35:976–87. doi: 10.1177/0269215520988475
59. Øra, HP, Kirmess, M, Brady, MC, Partee, I, Hognestad, RB, Johannessen, BB, et al. The effect of augmented speech-language therapy delivered by telerehabilitation on poststroke aphasia-a pilot randomized controlled trial. Clin Rehabil. (2020) 34:369–81. doi: 10.1177/0269215519896616
60. Øra, HP, Kirmess, M, Brady, MC, Sørli, H, and Becker, F. Technical features, feasibility, and acceptability of augmented telerehabilitation in post-stroke aphasia-experiences from a randomized controlled trial. Front Neurol. (2020) 11:671. doi: 10.3389/fneur.2020.00671
61. Brady, MC, Kelly, H, Godwin, J, Enderby, P, and Campbell, P, Cochrane Stroke Group. Speech and language therapy for aphasia following stroke. Cochrane Database Syst Rev. (2016) 2016:Cd000425. doi: 10.1002/14651858.CD000425.pub4
62. Hota, S, Inamoto, Y, Oguchi, K, Kondo, T, Otaka, E, Mukaino, M, et al. Outcomes of dysphagia following stroke: factors influencing Oral intake at 6 months after onset. J Stroke Cerebrovasc Dis. (2021) 30:105971. doi: 10.1016/j.jstrokecerebrovasdis.2021.105971
63. Kantarcigil, C, Kim, MK, Chang, T, Craig, BA, Smith, A, Lee, CH, et al. Validation of a novel wearable electromyography patch for monitoring submental muscle activity during swallowing: a randomized crossover trial. J Speech Lang Hear Res. (2020) 63:3293–310. doi: 10.1044/2020_JSLHR-20-00171
64. Kirkness, CJ, Cain, KC, Becker, KJ, Tirschwell, DL, Buzaitis, AM, Weisman, PL, et al. Randomized trial of telephone versus in-person delivery of a brief psychosocial intervention in post-stroke depression. BMC Res Notes. (2017) 10:500. doi: 10.1186/s13104-017-2819-y
65. SteelFisher, GK, McMurtry, CL, Caporello, H, Lubell, KM, Koonin, LM, Neri, AJ, et al. Video telemedicine experiences in COVID-19 were positive, but physicians and patients prefer in-person care for the future. Health Aff. (2023) 42:575–84. doi: 10.1377/hlthaff.2022.01027
66. Liu, Y, Guo, S, Yang, Z, Hirata, H, and Tamiya, T. A home-based tele-rehabilitation system with enhanced therapist-patient remote interaction: a feasibility study. IEEE J Biomed Health Inform. (2022) 26:4176–86. doi: 10.1109/JBHI.2022.3176276
67. Berton, A, Longo, UG, Candela, V, Fioravanti, S, Giannone, L, Arcangeli, V, et al. Virtual reality, augmented reality, gamification, and telerehabilitation: psychological impact on Orthopedic Patients' rehabilitation. J Clin Med. (2020) 9:2567. doi: 10.3390/jcm9082567
68. Chung, J, Kim, CT, Lee, J, Lee, E, Jung, KI, Yoo, WK, et al. Factors affecting participation in telerehabilitation using transcranial direct current stimulation for patients with poststroke paralysis in South Korea. Telemed J E Health. (2023). doi: 10.1089/tmj.2022.0452
69. Malik, AN, Tariq, H, Afridi, A, and Rathore, FA. Technological advancements in stroke rehabilitation. J Pak Med Assoc. (2022) 72:1672–4. doi: 10.47391/JPMA.22-90
70. Langerak, AJ, Regterschot, GRH, Selles, RW, Meskers, CGM, Evers, M, Ribbers, GM, et al. Requirements for home-based upper extremity rehabilitation using wearable motion sensors for stroke patients: a user-centred approach. Disabil Rehabil Assist Technol. (2023):1–13. doi: 10.1080/17483107.2023.2183993
71. Dubois, A, Mouthon, A, Sivagnanaselvam, RS, and Bresciani, JP. Fast and automatic assessment of fall risk by coupling machine learning algorithms with a depth camera to monitor simple balance tasks. J Neuroeng Rehabil. (2019) 16:71. doi: 10.1186/s12984-019-0532-x
72. Lin, BS, Zhang, Z, Peng, CW, Lin, CC, Lin, CH, and Lin, BS. Automatic assessment system based on IMUs and machine learning for predicting berg balance scale. IEEE Sensors J. (2022) 22:19919–30. doi: 10.1109/JSEN.2022.3200986
73. Bhattacharjya, S, Lenker, J, and Ghosh, R. Assessing the usefulness of an mHealth strategy to support implementation of multi-faceted adaptive feeding interventions by community-based rehabilitation workers. Assist Technol. (2023) 35:228–34. doi: 10.1080/10400435.2022.2028936
Keywords: telerehabilitation, telehealth, stroke, information and communication technologies, rehabilitation
Citation: Xing Y, Xiao J, Zeng B and Wang Q (2023) ICTs and interventions in telerehabilitation and their effects on stroke recovery. Front. Neurol. 14:1234003. doi: 10.3389/fneur.2023.1234003
Edited by:
Won-Seok Kim, Seoul National University Bundang Hospital, Republic of KoreaReviewed by:
Muhammad Hafiz Hanafi, Universiti Sains Malaysia Health Campus, MalaysiaCopyright © 2023 Xing, Xiao, Zeng and Wang. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Yanghui Xing, eWh4aW5nQHN0dS5lZHUuY24=; Qiang Wang, d2FuZ3FpYW5nQG5yY3J0YS5jbg==
 Yanghui Xing
Yanghui Xing Jianxin Xiao1
Jianxin Xiao1 Buhui Zeng
Buhui Zeng