- 1Curtin Medical School, Faculty of Health Sciences, Curtin University, Perth, WA, Australia
- 2Curtin School of Population Health, Faculty of Health Sciences, Curtin University, Perth, WA, Australia
- 3Department of Neurology, First Affiliated Hospital, Sun Yat-sen University, Guangzhou, China
Background: Significant associations exist between ambient temperature and stroke risk, but results in high cardiovascular risk populations are lacking. This systemic review summarised current evidence on ambient temperature and overall stroke risk in a high cardiovascular risk population.
Methods: We performed a systematic literature search across MEDLINE, Embase, PsycINFO, CINAHL, Web of Science, and GEOBASE, from inception to 3 July 2023, to identify all population-based studies. Eligible studies screened by independent reviewers recruited individuals aged 18 years and over, where minimum 80% of participants had a high cerebral vascular disease (CVD) risk profile. The primary outcomes are stroke morbidity and mortality, while the secondary outcomes are morbidity and mortality of ischaemic stroke (IS), intracranial cerebral haemorrhage (ICH), and subarachnoid haemorrhage (SH).
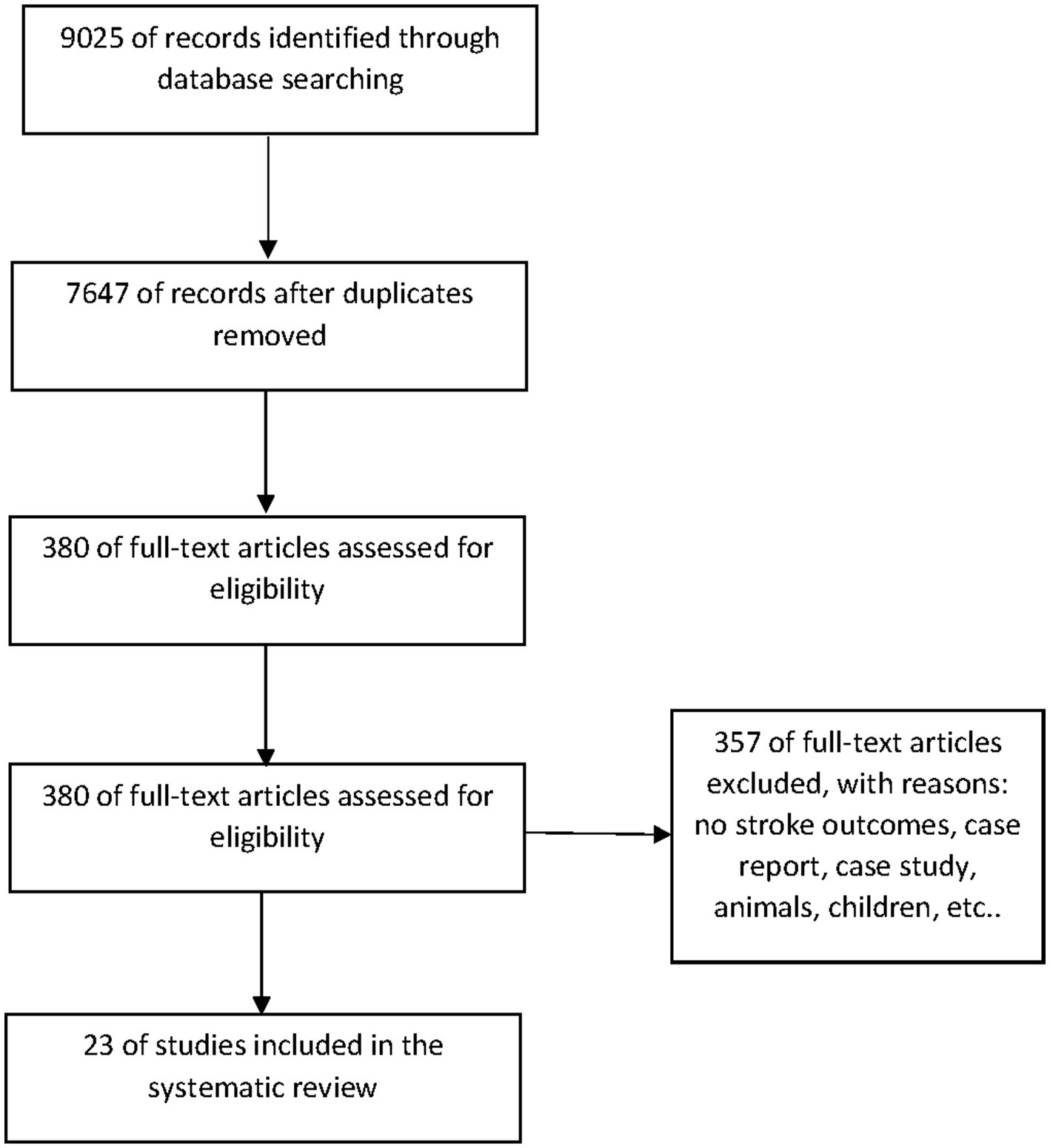
Results: The database searches identified 9,025 articles. After removing duplicates, 7,647 articles were screened in title and abstract to identify 380 articles for full-text screening. After the full-text screening of 380 articles by two independent reviewers, 23 articles were included in the review.
Conclusion: The evidence for an association between ambient temperature and stroke incidence is that lower temperatures were more likely to increase morbidity and mortality risk of both haemorrhagic and ischaemic stroke in older people. Conversely, higher ambient temperature is significantly associated with intracranial haemorrhage risk, but decreased risk with IS. Higher and lower ambient temperatures consistently increase stroke risks in patients with comorbidities of congestive heart failure and dyslipidaemia. This evidence implies the need to establish clinical guidelines for preventive intervention in patients with high stroke risks during extreme ambient temperatures.
Highlights
• Lower ambient temperatures are more likely to increase the morbidity and mortality risk of both ICH and IS in the elderly.
• Higher ambient temperatures are significantly associated with intracranial haemorrhage risk, but decreased risk of ischaemic stroke.
• Higher and lower ambient temperatures consistently increase stroke risks in patients with comorbidities of congestive heart failure and dyslipidaemia.
• Increased stroke risk was not observed, as compared to summer, in spring, autumn, or winter in stroke patients with comorbidities, including hypertension, diabetes, drinking, or smoking.
• Higher and lower ambient temperatures should be considered important influential factors when establishing clinical guidelines for preventive intervention in patients with high stroke risks.
Background
Stroke accounts for 6.5 million deaths each year and is the world’s second leading cause of mortality (1). Identification of modifiable risk factors for stroke is essential to mortality reduction. While risk factors, such as hypertension and diabetes, are well established, environmental risk factors for stroke remain to be investigated (1, 2). Acute stroke is not distributed randomly over time but depends on months/seasons of the year. Cold temperature was associated with an increased incidence of stroke morbidity and mortality (3–9) that may be attributable to the effect of cold temperature on increased blood pressure and serum cholesterol (10, 11). Hot temperature was associated with an increased risk of ischaemic stroke (IS) mortality but a decreased risk of intracerebral haemorrhage (ICH) mortality (12). A study by Salam et al. reported an increased incidence of IS relative to ICH during the summer months with higher solar radiation that cannot be explained by physiological measures suggestive of dehydration or hem-concentration (13). However, in a study by Cowperthwaite et al. (14), no significant association between weather and stroke incidence was recorded in the USA. A lack of evidence was reported in people with a high CVD risk profile, such as those with old age or CVD risk factors (e.g., a history of CVD, hypertension, and diabetes). Thus, in this systematic review, we aimed to investigate the association between extreme temperature and the relative risks of stroke morbidity and mortality in a high CVD risk population to inform the guidelines for the development of stroke preventive interventions.
Methods
Criteria for considering studies
Types of studies: All types of studies with a minimum 1-year duration to ensure all seasons were presented.
Types of participants: This review included individuals aged 18 years and over, where at least 80% of participants who had a high CVD risk profile, including the elderly who were 65 years or over, diabetes (defined as a previous diagnosis of type 1 or type 2 diabetes and/or current treatment with therapies to lower blood glucose levels), previous history of CVD (defined as myocardial infarction, angina pectoris, coronary bypass surgery, coronary angioplasty, stroke, transient ischaemic attack, carotid endarterectomy, surgery for peripheral vascular disease, intermittent claudication or renal failure determined as creatinine >1.5 times the upper limit of normal or chronic kidney diseases determined as eGFR<30 mL/min/1.73 m2), high blood pressure (defined as previous diagnosis of high blood pressure or on treatment with BP lowering drugs), and high blood lipid (defined as a previous diagnosis of high blood lipid or on treatment with lipid-lowering drugs).
Types of exposure: This review focused on ambient temperature, which is defined as the temperature of the surrounding air. As previous studies have shown the relatively same predictive ability of different temperature measures for health outcomes (15), we examined all available measurements of ambient temperature, such as daily or monthly mean, maximum or minimum temperatures, temperature change, or variation.
Type of outcome measures
Primary outcomes: Stroke morbidity and mortality.
Secondary outcomes: IS morbidity and mortality, ICH morbidity and mortality, subarachnoid haemorrhage (SH) morbidity and mortality.
Language: No restriction (English and non-English studies).
Publication type: Published and unpublished studies reported in peer-reviewed journals, reports, conference abstracts, and theses.
Search methods for identification of studies
We performed a similar search strategy developed by Wang et al. (16) in Ovid Medline, Ovid Embase, CINHL, Web of Science, and PsycINFO (Ovid). We combined the search terms relating to ‘ambient temperature’ and ‘stroke’ based on the strategy used by Wang et al. (16). We also searched reference lists of known previous systematic reviews and meta-analyses of the association between ambient temperature and stroke (17–19). Corresponding authors of relevant studies were contacted regarding any further published or unpublished study if needed.
Study selection
First, two independent reviewers screened a small sample of papers found in the search to revise any unclear or inappropriate inclusion criteria. In the full selection process, two reviewers independently scanned the results of the search and determined the eligibility of the studies. In the initial screening of titles and abstracts, the studies were included if they met the inclusion criteria or if they did not have enough information for exclusion. Rejected citations were recorded and classified as irrelevant studies. All potentially relevant articles were screened in full text for a final decision. If a study did not have sufficient information to assess eligibility, we attempted to contact the authors; the study was classified as a potentially relevant article and checked in sensitivity analyses if authors did reply after 1 month.
Data extraction and quality assessment
Data extraction forms and quality assessment forms were piloted on a small group of studies. Two reviewers independently performed data extraction and quality assessment in the prespecified form. If any disagreements were raised, the reviewers would discuss consensus or consult with the third reviewer. A report of corrections or amendments to the prespecified form would be recorded.
Quality assessment
The quality of the included studies was assessed following the Strengthening the Reporting of Observational Studies in Epidemiology (STROBE) statement (20). The quality criteria included setting, locations, and dates for the recruitment period; eligibility criteria, sources, and methods of selecting participants; consecutive or random participant sampling; the proportion of eligible participants (participant rate); the number of participants in each stage of the study or reasons for ineligibility; a description of the included participants; a description of ambient temperature measurement and stroke; and sources of funding acknowledgement. The bias was assessed as low risk (sufficient data were provided and fulfilled the criteria), partial risk (insufficient data were provided), or high risk (sufficient data were provided and did not fulfil the criteria). Publication bias was judged by observing the asymmetry of funnel plots; if they were asymmetric, contour-enhanced funnel plots were then analysed to examine whether publication bias alone caused the asymmetry (21).
Due to the substantial inconsistencies of the measurement for exposure (e.g., ambient temperature), we reviewed and summarised findings from included studies and did not process with a meta-analysis.
Ethics and dissemination
This systematic review analysed non-identifiable data; thus, a formal ethics approval is unlikely to be crucial.
Results
Result of searches
As presented in the flow chart (Figure 1), the database searches identified 9,025 articles. After removing duplicates, 7,647 articles were screened. A total of 380 articles were screened in full-text, with 65 potentially appropriate studies for full-text screening to be included in the systematic review. A total of 23 articles were included in the final systematic review. Most of the articles were excluded due to a lack of a high CVD risk cohort, stroke outcomes, exposure to ambient temperature, or unclear results.
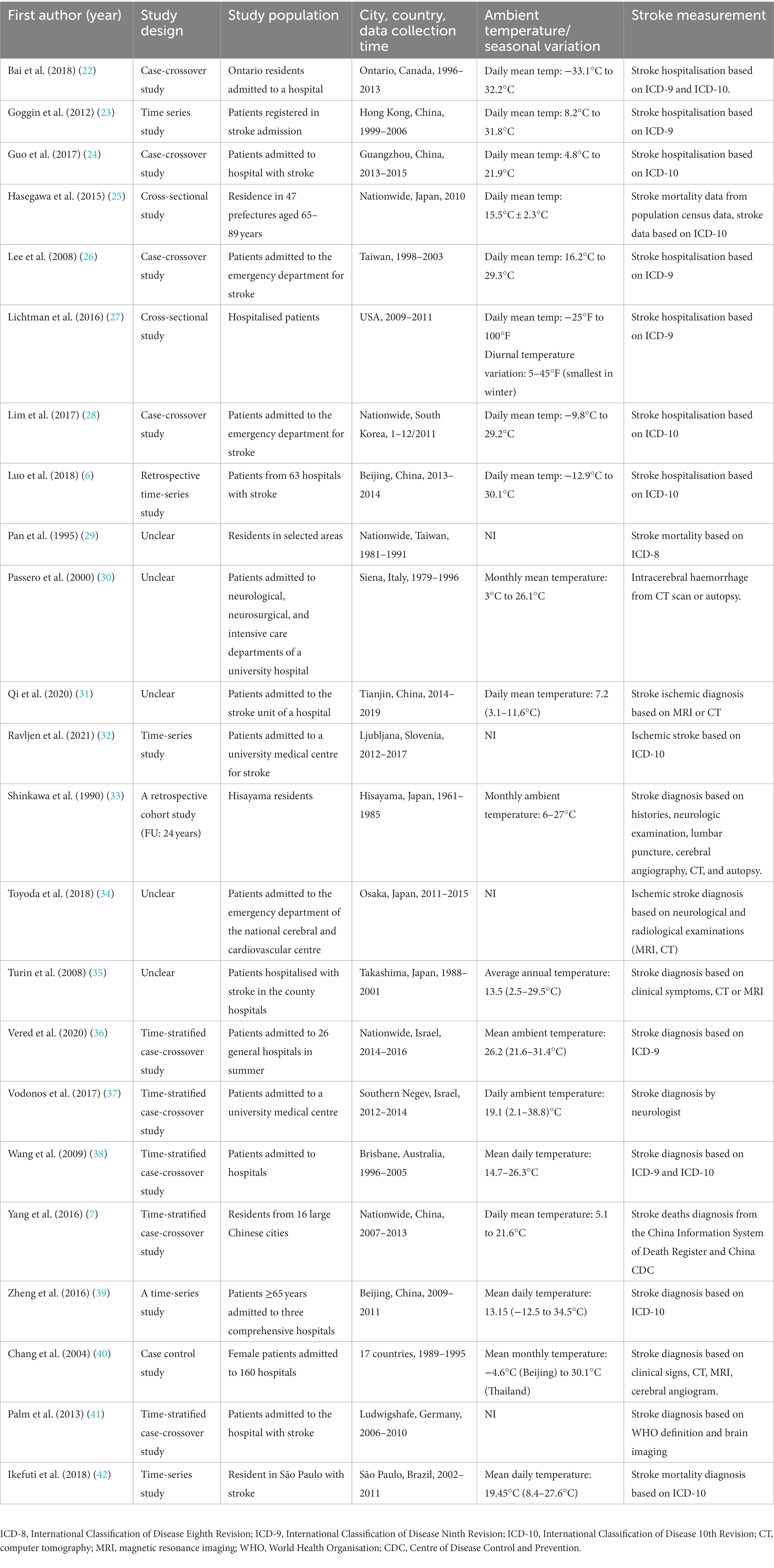
Characteristics of included studies
As presented in Table 1, most of the included studies were conducted in Asian countries, such as China and Japan, and were designed as time-series or time-stratified case–crossover study. However, a large number of studies did not sufficiently detail their study design, as mentioned in Table 1. More results were reported for the elderly group (>65 years) than those with CVD risk factors (e.g., hypertension, diabetes, and a history of CVD). Data on the high-risk population were substantially extracted from subgroup analyses, whereas two studies were restricted to the elderly. Diagnosis of stroke or stroke sub-type was based on the stratification of ICD-9th or 10th except for 10 studies (30, 31, 33–35, 40, 41, 43–45) that confirmed stroke by brain imaging, such as CT, MRI, or cerebral angiogram.
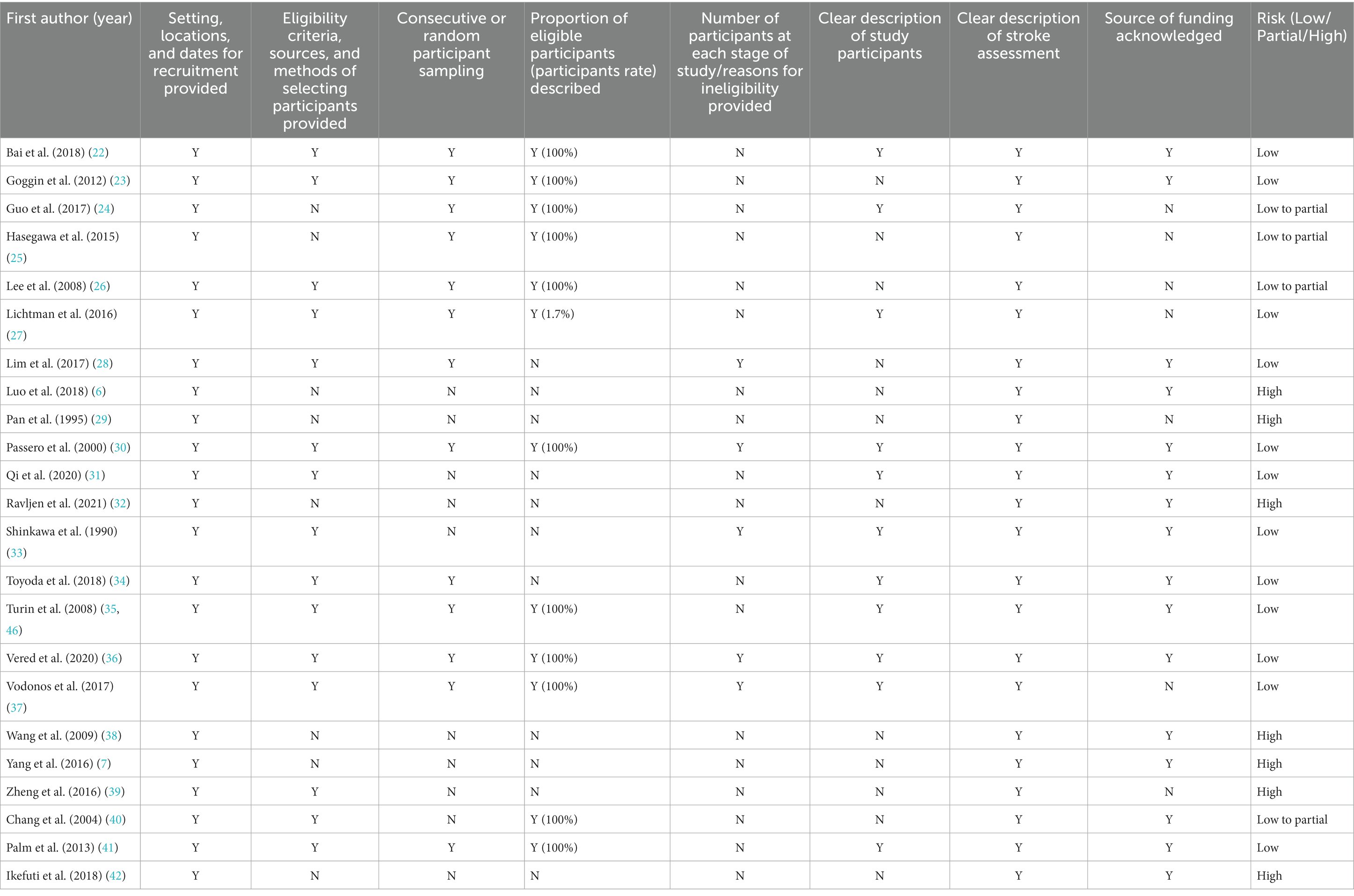
Risk of bias
Nine out of the 23 included studies were assessed as having a high risk of bias due to a lack of information on eligibility criteria, characteristics of study participants, and source of funding. All of the studies provided sufficient definitions for stroke assessment. Most of the studies utilised admission data or stroke registry data, so consecutive samples were recruited. More information is provided in Table 2. As studies reported results in different comparisons, we were unable to assess publication bias.
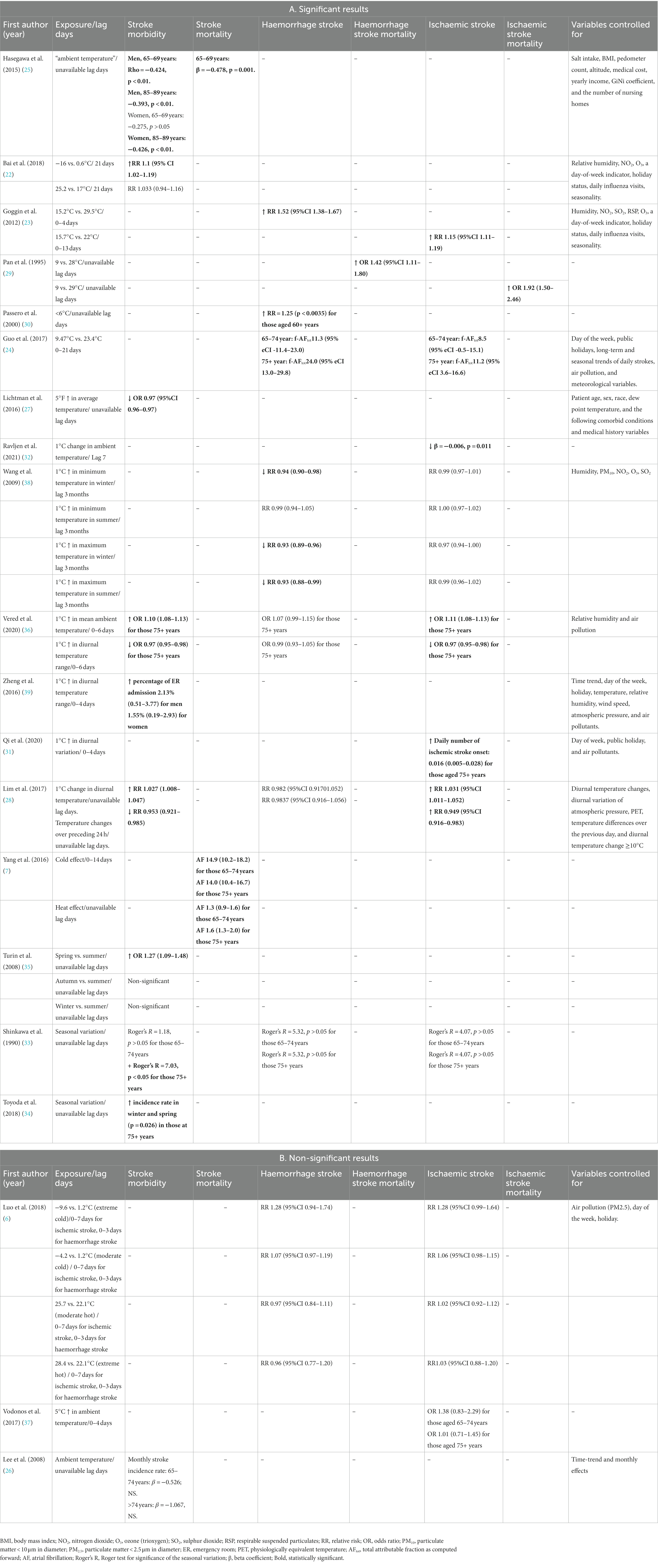
Association between ambient temperature and stroke in the elderly
As shown in Table 3A, most of the included studies showed a significant association between ambient temperature or seasonal pattern and stroke in the elderly, except for the studies by Luo et al. (6) (Table 3B), Vodonos et al. (37) (Table 3B), and Lee et al. (26) (Table 3B). Exposure to cold or lower temperature was more likely to increase the morbidity and mortality risk of stroke and stroke sub-type by a magnitude of 10–50% (22, 23, 29, 30) (Table 3A). An increase in mean ambient temperature was associated with a decreased risk of morbidity of general stroke and haemorrhagic stroke by a magnitude of 1–7% (27, 38). Studies by Zheng et al. (39) (Table 3A), Qi et al. (31) (Table 3A), and Lim et al. (28) (Table 3A) showed a positive association between a 1°C increase in diurnal temperature range and the risk of general stroke and ischaemic stroke morbidity that varied from 1.5 to 3.1%. In contrast to these observations, Vered et al. (36) (Table 3A) reported that a 1°C increase in a diurnal temperature range was associated with a reduced risk of general stroke and stroke sub-type morbidity by 1–3% and a 1°C increase in mean ambient temperature was associated with an increased risk of general stroke and stroke sub-type morbidity by a magnitude of 7–10%.
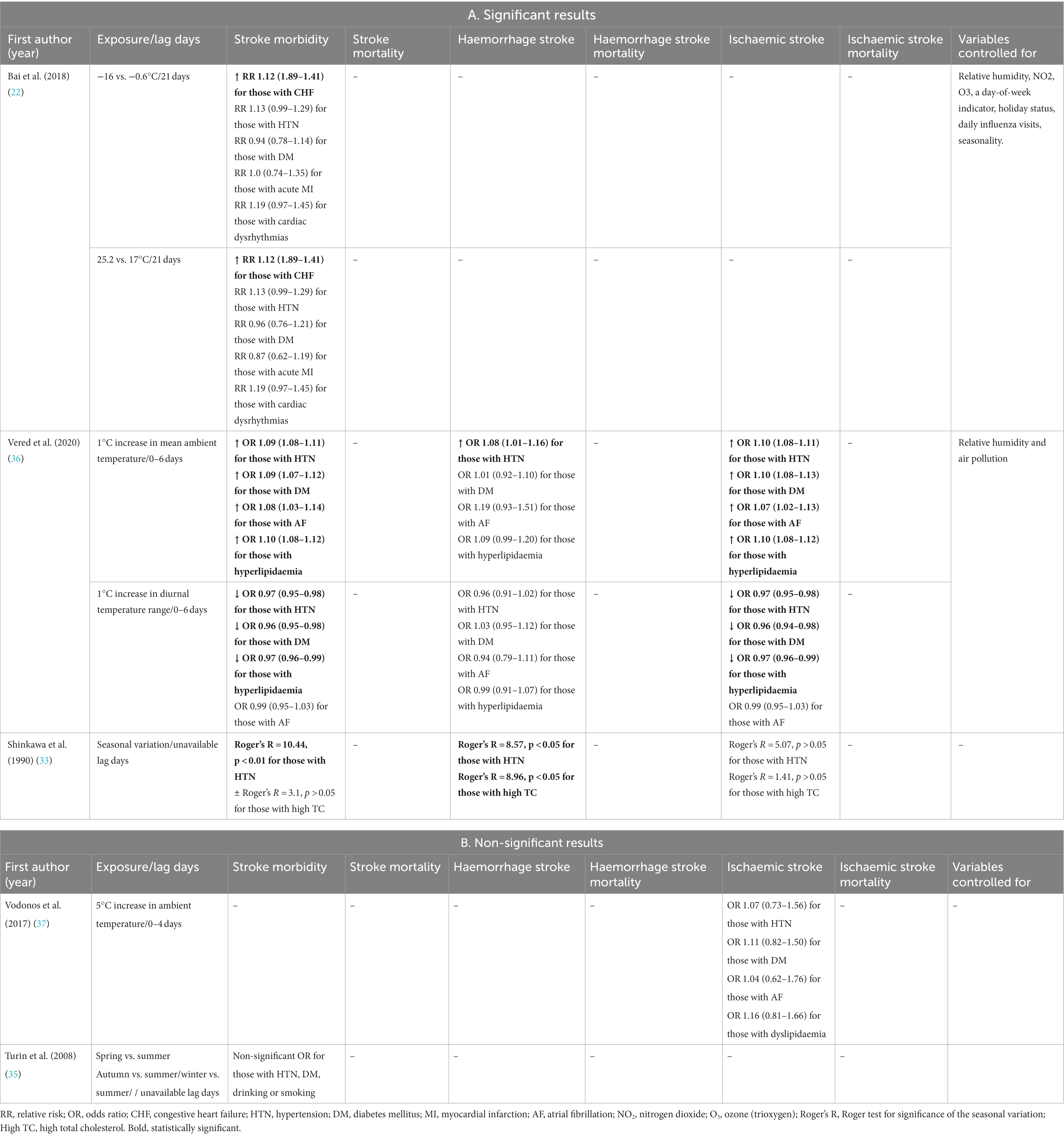
Association between ambient temperature and stroke in patients with comorbidities
As shown in Table 4, Vered et al. (36) reported a significant association between a 1°C increase in mean ambient temperature and general stroke and ischemic stroke in subgroups with hypertension, diabetes, atrial fibrillation, or hyperlipidaemia, whereas Vodonos et al. (Table 4 non-significant results) (37) and Bai et al. (22) did not show any significant effect of exposure to a 5°C increase in ambient temperature or hot effect on stroke or stroke sub-type in this population. However, Bai et al. (22) observed a significant effect of exposure to both cold (−16°C vs. −0.6°C) and hot temperatures (25.2°C vs. 17°C) on the increased risk of general stroke in those with congestive heart failure, with a RR of 1.12 (95%CI 1.89–1.41). Shinkawa et al. (33) reported a seasonal pattern of general stroke in patients with hypertension and ischemic stroke in patients with high total cholesterol. In the study (33), by Turin et al. (Table 4 non-significant results), as compared to summer, no significant difference in the risk of general stroke was recorded in spring, autumn, or winter in patients with hypertension, diabetes, drinking, or smoking.
Discussion
In this systemic review, a consistent observation in the elderly indicated that lower temperature was more likely to increase the morbidity and mortality risk of both haemorrhagic and ischaemic strokes in a temperature-dependent manner with a magnitude of 10–50%. Increased ambient temperature was associated with decreased stroke morbidity, especially haemorrhagic stroke, in a temperature-dependent manner with a magnitude of 1–7%. An increase in the diurnal temperature range was associated with an elevated risk of stroke, in particular, ischemic stroke morbidity, which varied from 1.5 to 3.1%. However, another study gave the opposite finding: raised diurnal temperature range variation was associated with reduced stroke, especially ischaemic stroke, while raised mean ambient temperature was associated with an increased risk of general stroke, in particular, ischaemic stroke by a magnitude of 7–10%.
The mechanisms for the impact of ambient temperature, including low and high temperatures on stroke risks, morbidity, and mortality, have attracted much literature discussion. Vasoconstriction is postulated to divert blood flow to central organs (brain, heart, and kidneys) in response to a lower ambient temperature, consequently increasing systemic vascular resistance and leading to high blood pressure, which is a known risk factor for stroke (47, 48). It is well established that mean blood pressure tends to be higher in the colder months, and cold exposure can further worsen hypertension in predisposed individuals (49). This exacerbated hypertension may reflect increasing systemic vascular resistance and oxygen demand and ineffective cold adaptation due to autonomic neuropathy in hypertensive patients (50). Another mechanistic explanation indicated that peripheral vasoconstriction may lead to cerebral vasculature congestion, which theoretically could increase the risk of haemorrhage (51). Dehydration is thought to be the potential mechanism for the high ambient temperature associated with increased ischaemic stroke risks, which was demonstrated in a study that dehydration in hospitalised stroke patients is associated with severe stroke morbidity and increased mortality (52).
In reviewing the association between ambient temperature and stroke patients with comorbidity, there were contrasting reported stroke risks. The ischemic stroke patients with comorbidities of hypertension, diabetes, atrial fibrillation, or hyperlipidaemia reported a significant association at a 1°C increase versus an insignificant association at a 5°C increase in mean ambient temperature. However, increased stroke risk was observed with exposure to both low and high ambient temperatures in congestive heart failure patients, as well as exposure to seasonal patterns in patients with hypertension, ischemic stroke, and hypercholesterolemia. In contrast, increased stroke risk was not observed, as compared to summer, spring, autumn, or winter, in stroke patients with comorbidities including hypertension, diabetes, drinking, or smoking.
The mechanism of the contrasted report of significant association in terms of ischaemic stroke risks with comorbidity (hypertension, diabetes, atrial fibrillation, or hyperlipidaemia) at different mean ambient temperatures remains to be established. The apparent observation with 1°C and 5°C increases in mean ambient temperature showed an equivalent baseline mean ambient temperature, and the 1°C increase still made it into the temperature range of below 130C41 in contrast to the 5°C increase in the temperature range of well above 130C34 (17–19°C), which is a normal range ambient temperature having minimal impacts on stroke risks. The underlying pathology of low and high ambient temperatures increasing the risk of stroke in patients with congestive heart failure included two aspects: (1) low ambient temperature may be mediated by peripheral vasoconstriction and cerebral vasculature congestion (51) due to congestive heart failure; (2) high ambient temperature may be mediated by peripheral vasodilatation, intravascular hypovolemia, and reduced cerebral perfusion due to congestive heart failure. The mechanism of seasonal change having a minimal impact on increasing stroke risk in patients with hypertension, diabetes, drinking, or smoking may be due to a relatively normal ambient temperature (35).
The final discussion point lies in the most recent evidence (53) evaluating the impact of ambient temperature and altitude exposure on stroke burden in a Chinese cohort. This research used data from the National Stroke High-Risk Population Screening System 2020 and assessed the overall prevalence, incidence, and mortality rate of stroke in China by obtaining the annual mean ambient temperature, diurnal temperature range, and altitude for each city. To observe stroke burden through quantifying the three risk elements, including incidence, prevalence, and mortality, the outcome of this research (53) demonstrated a negative linear relationship between mean ambient temperature and stroke risk (incidence and prevalence) as well as a negative association between mean ambient temperature and stroke mortality. A non-linear relationship with decreased risk in both high and low diurnal temperature ranges is observed for stroke burden. Overall, this research outcome (53) is in concert with our systematic review research findings in terms of examining the association between ambient temperature and stroke risk in high-risk populations.
Limitations
There are three major limitations to this review. First, we have assessed the quality of the included articles but have been unable to incorporate quality scores into the analysis because of the overall poor reporting of results. Second, some of the included studies had small sample sizes, and results were not adjusted for confounders such as air conditioning and heating systems, together with the direct effect of the weather on behaviours, including alcohol intake and activity level, which are crucial confounding factors that are virtually impossible to adjust for in retrospective analyses. Third, we were not able to pool results for the majority of studies due to a lack of crude data and/or inconsistent presentation of data.
Conclusion
The convincing evidence for an association between ambient temperature and the incidence of stroke lies in the fact that lower temperature was more likely to increase the morbidity and mortality risk of both haemorrhagic and ischaemic stroke in the elderly. In contrast, higher ambient temperature is significantly associated with intracranial haemorrhage risk but decreases risk with ischaemic stroke. Higher and lower ambient temperatures consistently increase stroke risks in patients with comorbidities of congestive heart failure and dyslipidaemia. This evidence implies the need to establish clinical guidelines for preventive intervention in patients with high stroke risks at higher and lower ambient temperatures. Ultimately, further research is needed to explore the relationship between temperature and stroke in different geographical locations, with different assessment tools, such as MRI scans, and with respect to stroke subtypes, including ischaemic and haemorrhagic stroke.
Data availability statement
All research data are available on reasonable request from the corresponding author.
Author contributions
ND: Data curation, Formal analysis, Investigation, Methodology, Software, Validation, Visualization, Writing – original draft, Writing – review & editing. CH: Data curation, Formal analysis, Investigation, Methodology, Software, Validation, Visualization, Writing – review & editing. EF: Data curation, Investigation, Methodology, Software, Validation, Visualization, Writing – original draft, Writing – review & editing. JZ: Conceptualization, Supervision, Validation, Visualization, Writing – review & editing. HH: Conceptualization, Supervision, Validation, Visualization, Writing – review & editing. CR: Conceptualization, Resources, Supervision, Validation, Visualization, Writing – review & editing. DX: Conceptualization, Investigation, Methodology, Project administration, Resources, Supervision, Validation, Visualization, Writing – original draft, Writing – review & editing.
Funding
The author(s) declare that no financial support was received for the research, authorship, and/or publication of this article.
Acknowledgments
The authors thank the staff at the Curtin School of Population Health and Curtin Medical School, Faculty of Health Sciences, Curtin University. The authors thank Ruxun Huang for providing the expertise and advice to initiate the review and extend their condolences to Ruxun Huang’s family for his passing at the initiation of the review.
Conflict of interest
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
Publisher’s note
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
References
1. Virani, SS, Alonso, A, Aparicio, HJ, Benjamin, EJ, Bittencourt, MS, Callaway, CW, et al. Heart disease and stroke statistics—2021 update: a report from the American Heart Association. Circulation. (2021) 143:e254–743. doi: 10.1161/CIR.0000000000000950
2. Grysiewicz, RA, Thomas, K, and Pandey, DK. Epidemiology of ischemic and hemorrhagic stroke: incidence, prevalence, mortality, and risk factors. Neurol Clin. (2008) 26:871–95. doi: 10.1016/j.ncl.2008.07.003
3. Chen, J-h, Jiang, H, Wu, L, Liao, X, Lu, Y, Tao, X-Q, et al. Association of ischemic and hemorrhagic strokes hospital admission with extreme temperature in Nanchang, China—a case-crossover study. J Clin Neurosci. (2017) 43:89–93. doi: 10.1016/j.jocn.2017.04.044
4. Gill, RS, Hambridge, HL, Schneider, EB, Hanff, T, Tamargo, RJ, and Nyquist, P. Falling temperature and colder weather are associated with an increased risk of aneurysmal subarachnoid hemorrhage. World Neurosurg. (2013) 79:136–42. doi: 10.1016/j.wneu.2012.06.020
5. Han, J, Liu, S, Zhang, J, Zhou, L, Fang, Q, Zhang, J, et al. The impact of temperature extremes on mortality: a time-series study in Jinan, China. BMJ Open. (2017) 7:e014741. doi: 10.1136/bmjopen-2016-014741
6. Luo, Y, Li, H, Huang, F, van Halm-Lutterodt, N, Qin Xu,, Wang, A, et al. The cold effect of ambient temperature on ischemic and hemorrhagic stroke hospital admissions: a large database study in Beijing, China between years 2013 and 2014—utilizing a distributed lag non-linear analysis. Environ Pollut. (2018) 232:90–6. doi: 10.1016/j.envpol.2017.09.021
7. Yang, J, Yin, P, Zhou, M, Ou, CQ, Li, M, Li, J, et al. The burden of stroke mortality attributable to cold and hot ambient temperatures: epidemiological evidence from China. Environ Int. (2016) 92-93:232–8. doi: 10.1016/j.envint.2016.04.001
8. Zeka, A, Browne, S, McAvoy, H, and Goodman, P. The association of cold weather and all-cause and cause-specific mortality in the island of Ireland between 1984 and 2007. Environ Health. (2014) 13:1–9. doi: 10.1186/1476-069X-13-104
9. Zheng, D, Arima, H, Sato, S, Gasparrini, A, Heeley, E, Delcourt, C, et al. Low ambient temperature and intracerebral hemorrhage: the INTERACT2 study. PLoS One. (2016) 11:e0149040. doi: 10.1371/journal.pone.0149040
10. Hong, Y-C, Kim, H, Oh, S-Y, Lim, Y-H, Kim, S-Y, Yoon, H-J, et al. Association of cold ambient temperature and cardiovascular markers. Sci Total Environ. (2012) 435:74–9. doi: 10.1016/j.scitotenv.2012.02.070
11. Keatinge, W, Coleshaw, S, Cotter, F, Mattock, M, Murphy, M, and Chelliah, R. Increases in platelet and red cell counts, blood viscosity, and arterial pressure during mild surface cooling: factors in mortality from coronary and cerebral thrombosis in winter. Br Med J. (1984) 289:1405–8. doi: 10.1136/bmj.289.6456.1405
12. Lim, Y-H, Kim, H, and Hong, Y-C. Variation in mortality of ischemic and hemorrhagic strokes in relation to high temperature. Int J Biometeorol. (2013) 57:145–53. doi: 10.1007/s00484-012-0542-x
13. Salam, A, Kamran, S, Bibi, R, Korashy, HM, Parray, A, Mannai, AA, et al. Meteorological factors and seasonal stroke rates: a four-year comprehensive study. J Stroke Cerebrovasc Dis. (2019) 28:2324–31. doi: 10.1016/j.jstrokecerebrovasdis.2019.05.032
14. Cowperthwaite, MC, and Burnett, MG. An analysis of admissions from 155 United States hospitals to determine the influence of weather on stroke incidence. J Clin Neurosci. (2011) 18:618–23. doi: 10.1016/j.jocn.2010.08.035
15. Conlon, KC, Rajkovich, NB, White-Newsome, JL, Larsen, L, and O’Neill, MS. Preventing cold-related morbidity and mortality in a changing climate. Maturitas. (2011) 69:197–202. doi: 10.1016/j.maturitas.2011.04.004
16. Wang, X, Cao, Y, Hong, D, Zheng, D, Richtering, S, Sandset, E, et al. Ambient temperature and stroke occurrence: a systematic review and meta-analysis. Int J Environ Res Public Health. (2016) 13:698. doi: 10.3390/ijerph13070698
17. Lavados, PM, Olavarría, VV, and Hoffmeister, L. Ambient temperature and stroke risk: evidence supporting a short-term effect at a population level from acute environmental exposures. Stroke. (2018) 49:255–61. doi: 10.1161/STROKEAHA.117.017838
18. Lian, H, Ruan, Y, Liang, R, Liu, X, and Fan, Z. Short-term effect of ambient temperature and the risk of stroke: a systematic review and meta-analysis. Int J Environ Res Public Health. (2015) 12:9068–88. doi: 10.3390/ijerph120809068
19. Zorrilla-Vaca, A, Healy, RJ, and Silva-Medina, MM. Revealing the association between cerebrovascular accidents and ambient temperature: a meta-analysis. Int J Biometeorol. (2017) 61:821–32. doi: 10.1007/s00484-016-1260-6
20. Von Elm, E, Altman, DG, Egger, M, Pocock, SJ, Gøtzsche, PC, and Vandenbroucke, JP. The strengthening the reporting of observational studies in epidemiology (STROBE) statement: guidelines for reporting observational studies. Ann Intern Med. (2007) 147:573–7. doi: 10.7326/0003-4819-147-8-200710160-00010
21. Sterne, JA, and Harbord, RM. Funnel plots in meta-analysis. Stata J. (2004) 4:127–41. doi: 10.1177/1536867X0400400204
22. Bai, L, Li, Q, Wang, J, Lavigne, E, Gasparrini, A, Copes, R, et al. Increased coronary heart disease and stroke hospitalisations from ambient temperatures in Ontario. Heart. (2018) 104:673–9. doi: 10.1136/heartjnl-2017-311821
23. Goggins, WB, Woo, J, Ho, S, Chan, EY, and Chau, PH. Weather, season, and daily stroke admissions in Hong Kong. Int J Biometeorol. (2012) 56:865–72. doi: 10.1007/s00484-011-0491-9
24. Guo, P, Zheng, M, Wang, Y, Feng, W, Wu, J, Deng, C, et al. Effects of ambient temperature on stroke hospital admissions: results from a time-series analysis of 104,432 strokes in Guangzhou, China. Sci Total Environ. (2017) 580:307–15. doi: 10.1016/j.scitotenv.2016.11.093
25. Hasegawa, T, and Fujikawa, M. Environmental factors determine the cerebrovascular disease (CVD) in the Japanese adults. Int Med J. (2015) 22:492–5.
26. Lee, HC, Hu, CJ, Chen, CS, and Lin, HC. Seasonal variation in ischemic stroke incidence and association with climate: a six-year population-based study. Chronobiol Int. (2008) 25:938–49. doi: 10.1080/07420520802551469
27. Lichtman, JH, Leifheit-Limson, EC, Jones, SB, Wang, Y, and Goldstein, LB. Average temperature, diurnal temperature variation, and stroke hospitalizations. J Stroke Cerebrovasc Dis. (2016) 25:1489–94. doi: 10.1016/j.jstrokecerebrovasdis.2016.02.037
28. Lim, JS, Kwon, HM, Kim, SE, Lee, J, Lee, YS, and Yoon, BW. Effects of temperature and pressure on acute stroke incidence assessed using a Korean Nationwide insurance database. J Stroke. (2017) 19:295–303. doi: 10.5853/jos.2017.00045
29. Pan, WH, Li, LA, and Tsai, MJ. Temperature extremes and mortality from coronary heart-disease and cerebral infarction in elderly Chinese. Lancet. (1995) 345:353–5. doi: 10.1016/S0140-6736(95)90341-0
30. Passero, S, Reale, F, Ciacci, G, and Zei, E. Differing temporal patterns of onset in subgroups of patients with intracerebral hemorrhage. Stroke. (2000) 31:1538–44. doi: 10.1161/01.STR.31.7.1538
31. Qi, XM, Wang, ZY, Xia, XS, Xue, J, Gu, Y, Han, S, et al. Potential impacts of meteorological variables on acute lschemic stroke onset. Risk Manag Healthc Policy. (2020) 13:615–21. doi: 10.2147/RMHP.S253559
32. Ravljen, M, Bajrovic, F, and Vavpotic, D. A time series analysis of the relationship between ambient temperature and ischaemic stroke in the Ljubljana area: immediate, delayed and cumulative effects. BMC Neurol. (2021) 21:23. doi: 10.1186/s12883-021-02044-8
33. Shinkawa, A, Ueda, K, Hasuo, Y, Kiyohara, Y, and Fujishima, M. Seasonal-variation in stroke incidence in Hisayama, Japan. Stroke. (1990) 21:1262–7. doi: 10.1161/01.STR.21.9.1262
34. Toyoda, K, Koga, M, Yamagami, H, Yokota, C, Sato, S, Inoue, M, et al. Seasonal variations in neurological severity and outcomes of ischemic stroke—5-year single-center observational study—. Circ J. (2018) 82:1443–50. doi: 10.1253/circj.CJ-17-1310
35. Turin, TC, Kita, Y, Murakami, Y, Rumana, N, Sugihara, H, Morita, Y, et al. Higher stroke incidence in the spring season regardless of conventional risk factors - Takashima stroke registry, Japan, 1988-2001. Stroke. (2008) 39:745–52. doi: 10.1161/STROKEAHA.107.495929
36. Vered, S, Paz, S, Negev, M, Tanne, D, Zucker, I, and Weinstein, G. High ambient temperature in summer and risk of stroke or transient ischemic attack: a national study in Israel. Environ Res. (2020) 187:109678. doi: 10.1016/j.envres.2020.109678
37. Vodonos, A, Novack, V, Horev, A, Abu Salameh, I, Lotan, Y, and Ifergane, G. Do gender and season modify the triggering effect of ambient temperature on ischemic stroke? Womens Health Issues. (2017) 27:245–51. doi: 10.1016/j.whi.2016.11.002
38. Wang, XY, Barnett, AG, Hu, WB, and Tong, SL. Temperature variation and emergency hospital admissions for stroke in Brisbane, Australia, 1996-2005. Int J Biometeorol. (2009) 53:535–41. doi: 10.1007/s00484-009-0241-4
39. Zheng, S, Wang, MZ, Li, B, Wang, S, He, S, Yin, L, et al. Gender, age and season as modifiers of the effects of diurnal temperature range on emergency room admissions for cause-specific cardiovascular disease among the elderly in Beijing. Int J Environ Res Public Health. (2016) 13:447. doi: 10.3390/ijerph13050447
40. Chang, CL, Shipley, M, Marmot, M, and Poulter, N. Lower ambient temperature was associated with an increased risk of hospitalization for stroke and acute myocardial infarction in young women. J Clin Epidemiol. (2004) 57:749–57. doi: 10.1016/j.jclinepi.2003.10.016
41. Palm, F, Dos Santos, M, Urbanek, C, Greulich, M, Zimmer, K, Safer, A, et al. Stroke seasonality associations with subtype, etiology and laboratory results in the Ludwigshafen stroke study (LuSSt). Eur J Epidemiol. (2013) 28:373–81. doi: 10.1007/s10654-013-9772-4
42. Ikefuti, PV, Barrozo, LV, and Braga, ALF. Mean air temperature as a risk factor for stroke mortality in São Paulo, Brazil. Int J Biometeorol. (2018) 62:1535–42. doi: 10.1007/s00484-018-1554-y
43. Fodor, DM, Fodor, M, and Perju-Dumbrava, L. Seasonal variation of stroke occurrence: a hospital based-study. Balneo Res J. (2018) 9:82–7. doi: 10.12680/balneo.2018.178
44. Oyoshi, T, Nakayama, M, and Kuratsu, J. Relationship between aneurysmal subarachnoid hemorrhage and climatic conditions in the subtropical region, Amami-Oshima, in Japan. Neurol Med Chir (Tokyo). (1999) 39:585–91; discussion 590-581. doi: 10.2176/nmc.39.585
45. Ranganai, E, and Matizirofa, L. An analysis of recent stroke cases in South Africa: trend, seasonality and predictors. S Afr Med J. (2020) 110:92–9. doi: 10.7196/SAMJ.2020.v110i2.013891
46. Turin, TC, Kita, Y, Rumana, N, Murakami, Y, Ichikawa, M, Sugihara, H, et al. Stroke case fatality shows seasonal variation regardless of risk factor status in a Japanese population: 15-year results from the Takashima stroke registry. Neuroepidemiology. (2009) 32:53–60. doi: 10.1159/000170907
47. Woodhouse, PR, Khaw, K-T, and Plummer, M. Seasonal variation of blood pressure and its relationship to ambient temperature in an elderly population. J Hypertens. (1993) 11:1267–74.
48. Ishigami, A, Hajat, S, Kovats, RS, Bisanti, L, Rognoni, M, Russo, A, et al. An ecological time-series study of heat-related mortality in three European cities. Environ Health. (2008) 7:5. doi: 10.1186/1476-069X-7-5
49. Cheng, X, and Su, H. Effects of climatic temperature stress on cardiovascular diseases. Eur J Intern Med. (2010) 21:164–7. doi: 10.1016/j.ejim.2010.03.001
50. Abboud, FM, Harwani, SC, and Chapleau, MW. Autonomic neural regulation of the immune system: implications for hypertension and cardiovascular disease. Hypertension. (2012) 59:755–62. doi: 10.1161/HYPERTENSIONAHA.111.186833
51. McArthur, K, Dawson, J, and Walters, M. What is it with the weather and stroke? Expert Rev Neurother. (2010) 10:243–9. doi: 10.1586/ern.09.154
52. Rowat, A, Graham, C, and Dennis, M. Dehydration in hospital-admitted stroke patients detection, frequency, and association. Stroke. (2012) 43:857–9. doi: 10.1161/STROKEAHA.111.640821
Keywords: ambient temperature, high cardiovascular risk population, stroke risk, stroke morbidity, stroke mortality, ischaemic stroke, haemorrhagic stroke
Citation: Danh N, Ho C, Ford E, Zhang J, Hong H, Reid C and Xu D (2024) Association between ambient temperature and stroke risk in high-risk populations: a systematic review. Front. Neurol. 14:1323224. doi: 10.3389/fneur.2023.1323224
Edited by:
Wen-Jun Tu, Capital Medical University, ChinaReviewed by:
Yair Zlotnik, Soroka Medical Center, IsraelRyo Itabashi, Iwate Medical University, Japan
Copyright © 2024 Danh, Ho, Ford, Zhang, Hong, Reid and Xu. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Dan Xu, ZGFuaWVsLnh1QGN1cnRpbi5lZHUuYXU=
†These authors share first authorship
 Nathan Danh1†
Nathan Danh1† Chau Ho
Chau Ho Jian Zhang
Jian Zhang Hua Hong
Hua Hong Dan Xu
Dan Xu