- 1Shaanxi Provincial People's Hospital, Xi'an, China
- 2Department of Gastroenterology, First Affiliated Hospital of Xinjiang Medical University, Urumqi, China
Background: Sedentary behavior is closely related to sleep disorders, and long-term lack of physical activity may disrupt circadian rhythms and increase the risk of sleep disorders; Excessive or insufficient sleep time may exacerbate health risks, therefore, analyzing the correlation between sedentary behavior, sleep duration, and sleep disorders.
Methods: Using the NHANES research project, multiple logistic regression analysis was conducted to investigate the relationship between sedentary behavior, sleep duration, and sleep disorders in adults. Restrictive cubic spline curves were used to further explore the dose–response relationship between sedentary behavior, sleep duration, and sleep disorders.
Results: In the entire study population, compared to the lowest quartile of Sedentary activity duration, the third quartile [OR = 1.441 (95% CI: 1.226–1.693), p < 0.05] and fourth quartile [OR = 1.480 (95% CI: 1.267–1.729), p < 0.05] had an increased risk of developing sleep disorders. Compared with adults who sleep for less than 6 h, those who sleep for 6 to less than 8 h [OR = 0.444 (95%CI: 0.395–0.499), p < 0.05], ≥8 h [OR = 0.370 (95%CI: 0.325–0.422), p < 0.05] the risk of developing sleep disorders decreases. Subgroup analysis found that sedentary behavior and sleep duration have a higher impact on sleep in men under 45 years old. There is a dose–response relationship between sedentary behavior, sleep duration, and the risk of sleep disorders. RCS analysis results show that prolonged sitting for more than 300 min significantly increases the risk of sleep disorders; when the sleep duration is less than 7 h or greater than 8 h, there is a significant increase in the risk of developing sleep disorders. Sensitivity analysis confirmed the robustness of the research results.
Conclusion: There is a significant non-linear relationship between sedentary time, sleep duration, and sleep disorders. It is recommended to limit sedentary time to 300 min per day and sleep duration to 7–8 h to reduce the risk of sleep disorders and improve sleep quality.
1 Introduction
Humans spend one-third of their lives sleeping, underscoring the critical role of sleep in overall health. Sleep quality directly impacts quality of life, mental health, and physiological wellbeing (1–7). Research has linked good sleep quality to cardiovascular health, metabolic function, immune system regulation, and cognitive performance (8–10). According to a 2023 World Health Organization (WHO) report, sleep disorders have become the second-largest global mental health issue, affecting approximately 45% of urban populations, with a global prevalence of 27%. Over the past 50 years, average sleep duration among adults has decreased by 1.5 h, and 30–45% of adults report insufficient sleep or poor sleep quality. In the United States alone, sleep disorders result in an annual productivity loss of $54 billion.
The widespread use of electronic devices and the rise of sedentary occupations have made prolonged sitting a common part of modern life. Studies indicate that 60% of jobs require extended periods of sitting, particularly in fields such as information technology, finance, and education. Occupational sedentary time has increased from an average of 3 h per day in 1950 to 8.2 h in 2020, with 30% of adults sitting for at least 6 h daily during weekdays and 37% on weekends (11).
The WHO’s 2020 Guidelines on Physical Activity and Sedentary Behavior define sedentary behavior as any waking activity with an energy expenditure ≤1.5 MET (metabolic equivalent), regardless of posture or duration (12). Common sedentary activities include working, studying, watching television, using computers, reading, writing, driving, and conversing. The WHO ranks sedentary behavior among the top 10 contributors to mortality and disease, associating it with cardiovascular diseases, obesity, diabetes, and other health issues (13–15). Globally, approximately 2 million deaths annually are attributed to sedentary behavior, which is now the fourth-leading risk factor for mortality. Systematic reviews and guidelines have summarized extensive evidence on the adverse health effects of prolonged sitting (16–25). A recent large-scale cohort study published in The Lancet (11) found that sitting for >6 h daily increases the risk of 12 non-communicable diseases, including migraines, rheumatoid arthritis, chronic obstructive pulmonary disease (COPD), chronic liver disease (CLD), diabetes, depression, chronic kidney disease (CKD), asthma, thyroid disorders, gout, diverticulosis, and ischemic heart disease (IHD) (26–31).
Sedentary behavior is closely linked to sleep disorders. Prolonged sitting reduces sleep drive, induces physical discomfort, disrupts metabolism and psychological states, shortens total sleep duration, and alters sleep architecture, thereby contributing to sleep disorders. Improving sedentary habits and increasing physical activity can enhance sleep quality and overall health. This study investigates the relationship between sedentary behavior, sleep duration, and sleep disorders to provide scientific evidence for public health interventions.
2 Methods
2.1 Data source and participants
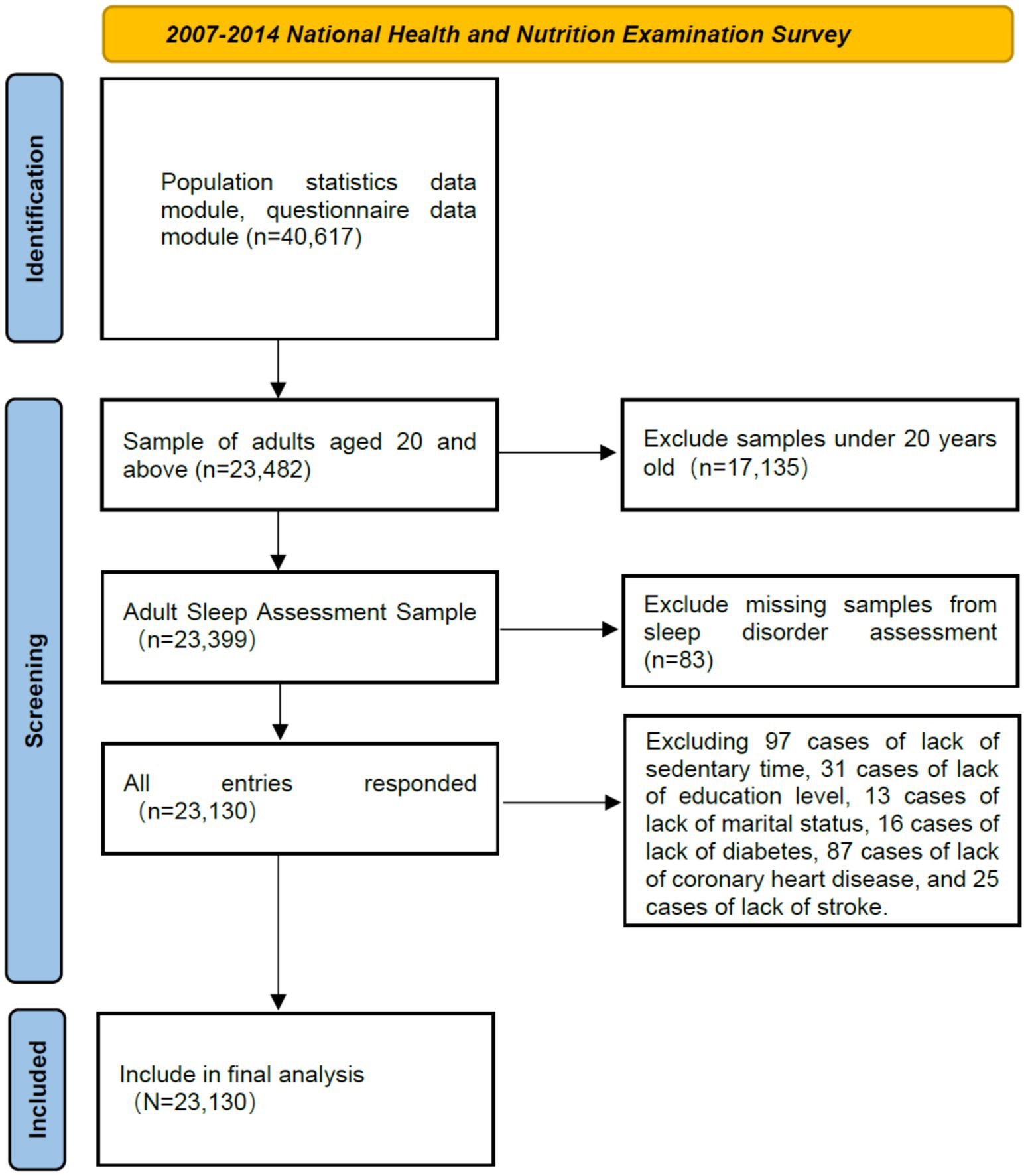
Data were obtained from the 2007–2014 National Health and Nutrition Examination Survey (NHANES), a biennial cross-sectional survey collecting demographic, socioeconomic, nutritional, and health information through interviews, physical examinations, and laboratory tests. NHANES is renowned for its high-quality data. We analyzed variables from the 2007–2014 surveys, including participants aged ≥20 years with complete data. The final sample comprised 23,130 eligible individuals (Figure 1).
2.2 Study variables and definitions
• Sleep disorders: Defined as physician-diagnosed sleep disorders, recorded as “yes” or “no” in NHANES.
• Sedentary duration: Categorized into quartiles: Q1 (<180 min), Q2 (180–<300 min), Q3 (300–<480 min), Q4 (≥480 min).
• Sleep duration: Grouped as <6 h, 6–<8 h, and ≥8 h.
• Covariates: Demographic (age, sex, education level, marital status) and health-related (coronary heart disease, stroke, diabetes).
2.3 Statistical analysis
Perform statistical analysis using R version 4.3.0. Classify the data as n (%) and use chi square test for inter group comparison. Use binary logistic regression to analyze the relationship between sedentary behavior, sleep duration, and sleep disorders. Model 1 did not adjust for any variables; Model 2 has been adjusted based on significant differences in social and demographic characteristics; Model 3 has been adjusted based on demographic characteristics and chronic diseases. Perform subgroup analysis by age and gender to explore differences between subgroups. Use restricted cubic spline (RCS) to analyze the dose–response relationship between sedentary behavior, sleep duration, and sleep disorders. The results are expressed as the odds ratio (OR) of the 95% confidence interval (CI), and when p < 0.05, the difference is considered statistically significant.
3 Results
3.1 Baseline characteristics
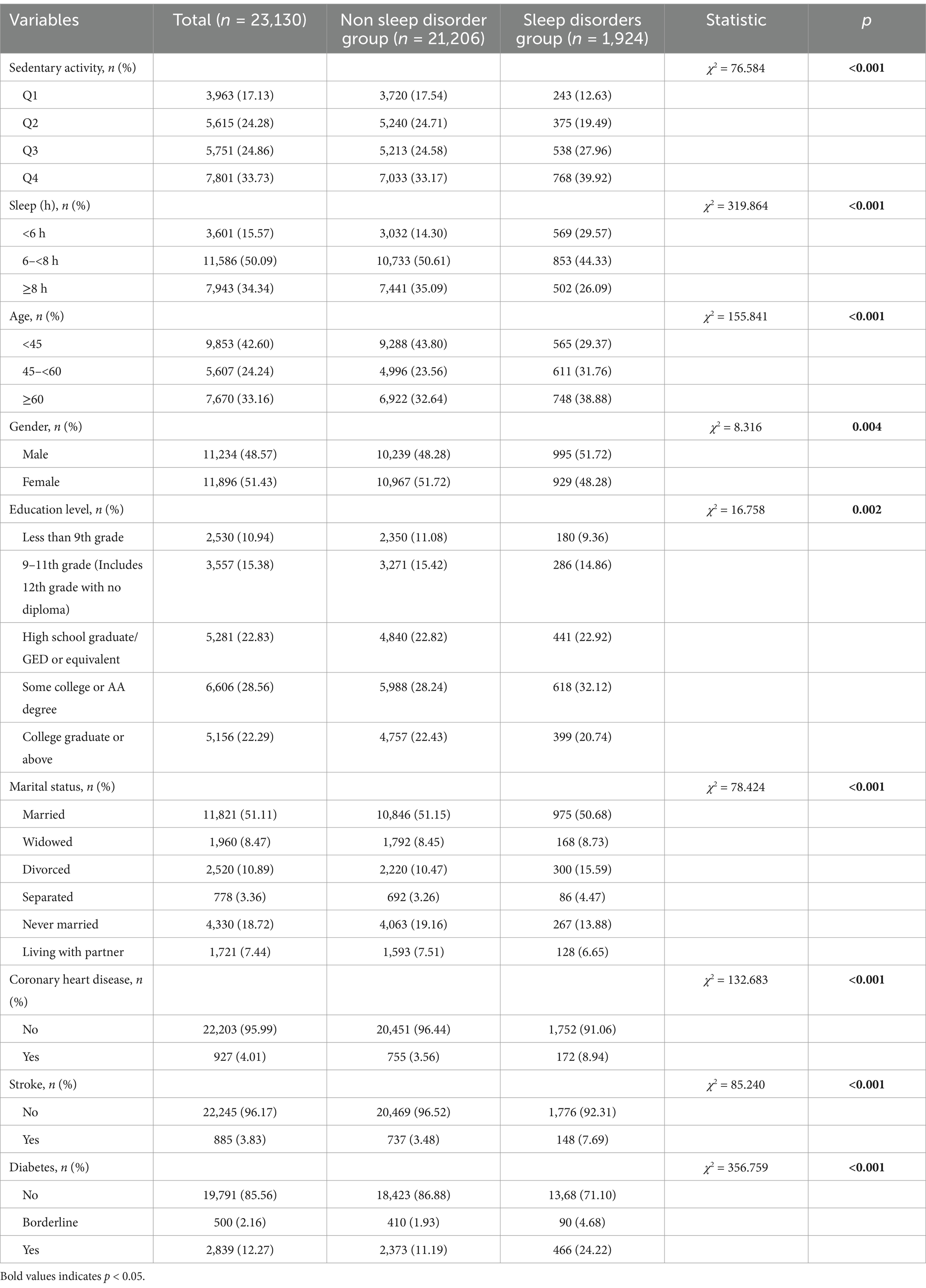
The study included 23,130 adults (mean age: 49.49 ± 17.80 years; 48.57% male, 51.43% female). Significant differences (p < 0.05) were observed between groups with and without sleep disorders in sedentary duration, sleep duration, age, sex, education level, marital status, and chronic conditions (Table 1).
3.2 Multivariate logistic regression
The first logistic regression model only included Sedentary activity or Sleep duration. The results showed that the third quartile of Sedentary activity duration [OR = 1.580 (95% CI: 1.350–1.849), p < 0.05] and the fourth quartile [OR = 1.672 (95% CI: 1.439–1.942), p < 0.05] had an increased risk of developing sleep disorders in adults relative to the first quartile. Adults with sleep duration of 6–<8 h [OR = 0.423 (95% CI: 0.378–0.474), p < 0.05] and ≥8 h [OR = 0.359 (95% CI: 0.317–0.408), p < 0.05] have a lower risk of developing sleep disorders compared to those with sleep duration of <6 h.
The second logistic regression model adjusted for variables with significant differences in demographic characteristics (age, gender, education level, marital status), and the results showed that the third and fourth percentiles of sedentary activity duration [OR = 1.528 (95% CI: 1.302–1.794), p < 0.05], and the fourth quartile [OR = 1.616 (95% CI: 1.385–1.885), p < 0.05] had an increased risk of sleep disorders compared to the first quartile of adults. Adults with sleep duration of 6–<8 h [OR = 0.432 (95% CI: 0.385–0.485), p < 0.05] and ≥8 h [OR = 0.368 (95% CI: 0.324–0.419), p < 0.05] have a lower risk of developing sleep disorders compared to those with sleep duration of <6 h.
The third logistic regression model adjusted for all significant differences in demographic characteristics (age, gender, education level, marital status) and chronic diseases (Coronary heart disease, stroke, diabetes). The results showed that the third and fourth percentiles of sedentary activity duration [OR = 1.441 (95% CI: 1.226–1.693), p < 0.05] and the fourth quartile [OR = 1.480 (95% CI: 1.267–1.729), p < 0.05] had an increased risk of developing sleep disorders in adults relative to the first quartile. Sleep duration 6–<8 h [OR = 0.444 (95%CI: 0.395–0.499), p < 0.05], ≥8 h [OR = 0.370 (95%CI: 0.325–0.422), p < 0.05] the risk of sleep disorders decreases in adults with a relative duration of less than 6 h.
In binary logistic regression analysis, confounding variables may be associated with sedentary behavior, sleep duration, and the onset of sleep disorders, which may lead to biased results. Therefore, this study will construct three logistic regression models to evaluate the robustness of the results by sequentially excluding these confounding factors. Sensitivity analysis confirms that the relationship between sedentary behavior, sleep duration, and sleep disorders remains close (Table 2).
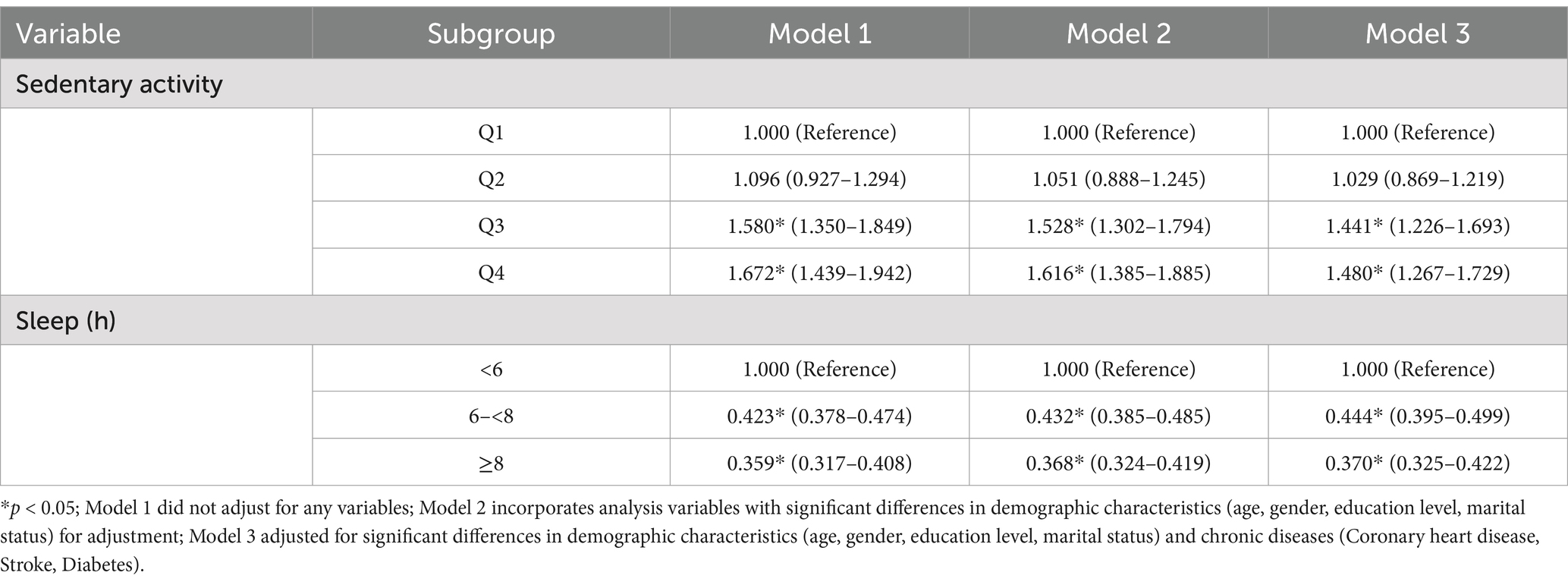
Table 2. Multivariate logistic regression analysis of sedentary behavior, sleep duration, and sleep disorders.
Further subgroup analysis of the association between sedentary behavior, sleep duration, and sleep disorders (Table 3). The results of the third logistic regression model showed that compared with the first quartile of Sedentary activity duration in age subgroups <45 years old, 45–<60 years old, and ≥60 years old, fourth quartiles increased the risk of sleep disorders (all OR > 1, all p < 0.05) The risk of sleep disorders is higher in the fourth quartile of sedentary behavior among the 45 year old population.
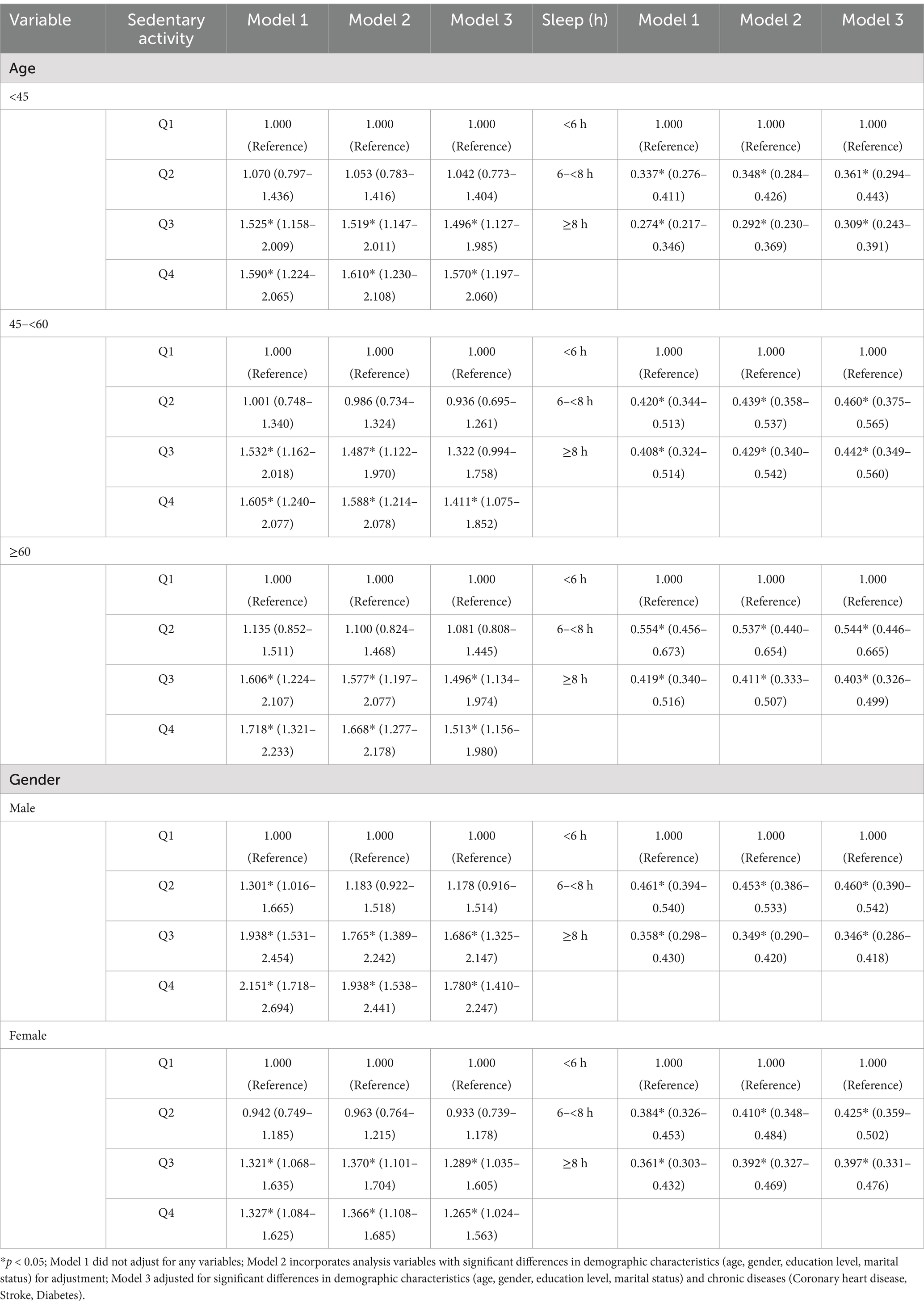
Table 3. Logistic regression table of the relationship between sedentary behavior, sleep duration, and sleep disorders in subgroups.
Adults aged <45, 45–<60, and ≥60 years who sleep for 6–<8 h [all OR<1, all p < 0.05] and ≥8 h [all OR < 1, all p < 0.05] have a lower risk of developing sleep disorders compared to adults aged <6 h The risk of sleep disorders is higher in the fourth quartile of sedentary behavior among the 45 year old population 6–<8 h, The risk of sleep disorders decreases even more after 8 h.
In the gender subgroups of males and females, compared with those with Sedentary activity duration in the first quartile, both the third and fourth quartiles increased the risk of sleep disorders (all OR > 1, all p < 0.05). Men with sedentary behavior have a higher risk of sleep disorders in the third and fourth quartiles.
Among males and females, adults with sleep duration of 6–<8 h [OR < 1, p < 0.05] and ≥8 h [OR < 1, p < 0.05] have a lower risk of developing sleep disorders compared to adults with sleep duration less than 6 h. Sensitivity analysis within subgroups confirmed that the relationship between sedentary behavior, sleep duration, and sleep disorders remains close.
3.3 Restrictive cubic spline curves of sedentary behavior, sleep duration, and sleep disorders
The dose–response relationship between sedentary time and sleep disorders showed a non-linear curve (Poverall < 0.001, Pnonlinear = 0.001) (Figure 2C). As sedentary time increased, the risk of sleep disorders showed an increasing trend, and at 300 min, the risk of sleep disorders significantly increased. In RCS analysis, confounding variables may affect the dose–response relationship between sedentary time and the onset of sleep disorders. The study will evaluate the robustness of the results by sequentially excluding these confounding factors. Sensitivity analysis confirms that the relationship between sedentary time and sleep disorders remains close (Figures 2A, B).
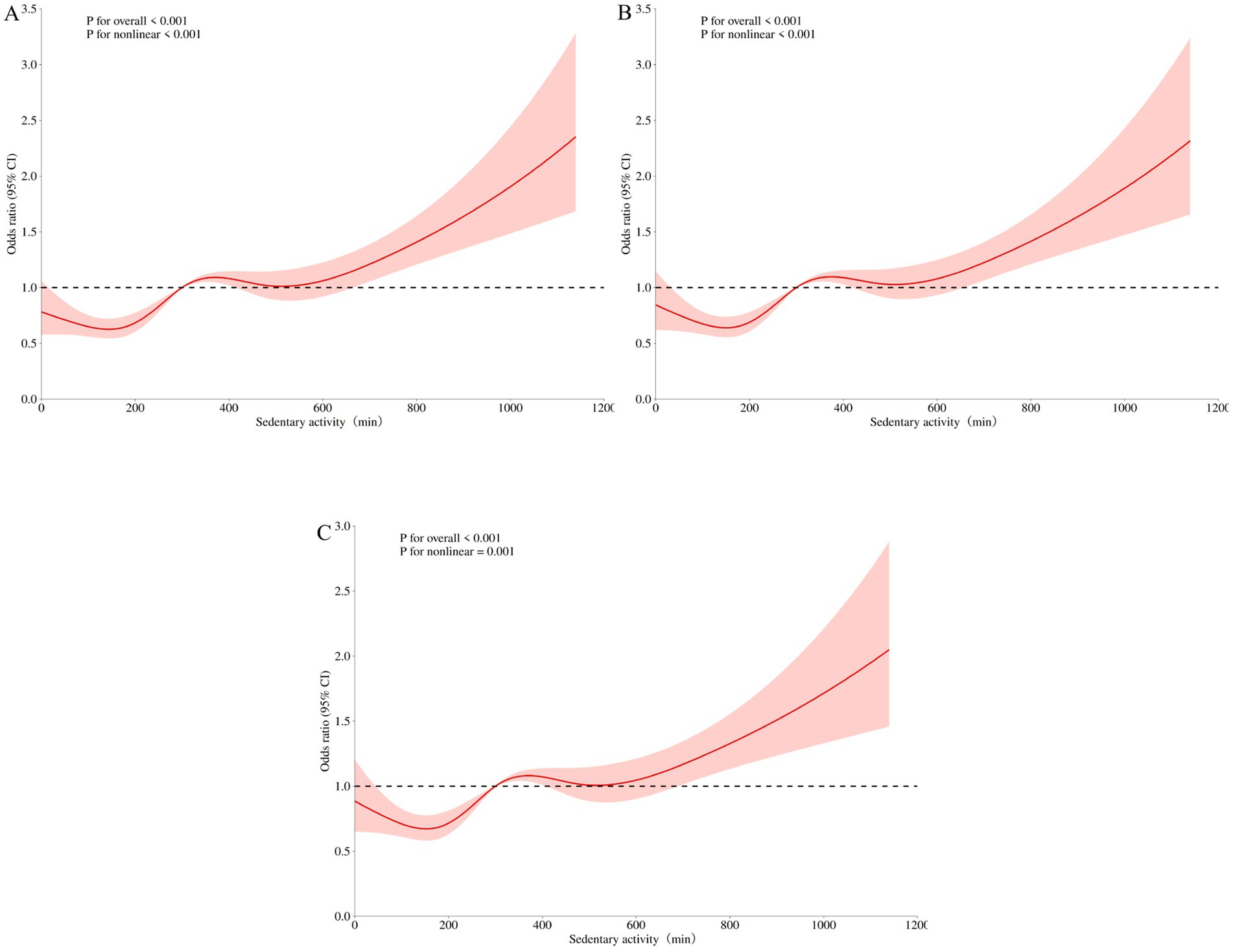
Figure 2. Restricted cubic spline curve of sedentary time and sleep disorders. (A) RCS 1 did not adjust for any variables; (B) RCS 2 incorporates analysis variables with significant differences in demographic characteristics (age, gender, education level, marital status) for adjustment; (C) RCS 3 adjusted for significant differences in demographic characteristics (age, gender, education level, marital status) and chronic diseases (Coronary heart disease, Stroke, Diabetes).
The dose–response relationship between sleep duration and sleep disorders showed a non-linear curve (Poverall < 0.001, Pnonlinear < 0.001) (Figure 3C). As sleep duration increased, the risk of developing sleep disorders gradually decreased, and at 7 h, the risk of developing sleep disorders was significantly reduced. It reaches its lowest point around 8 h and shows an upward trend after 8 h. In RCS analysis, confounding variables may affect the dose–response relationship between sleep duration and the onset of sleep disorders. The study will evaluate the robustness of the results by sequentially excluding these confounding factors. Sensitivity analysis confirms that the relationship between sleep duration and sleep disorders remains close (Figures 3A, B).
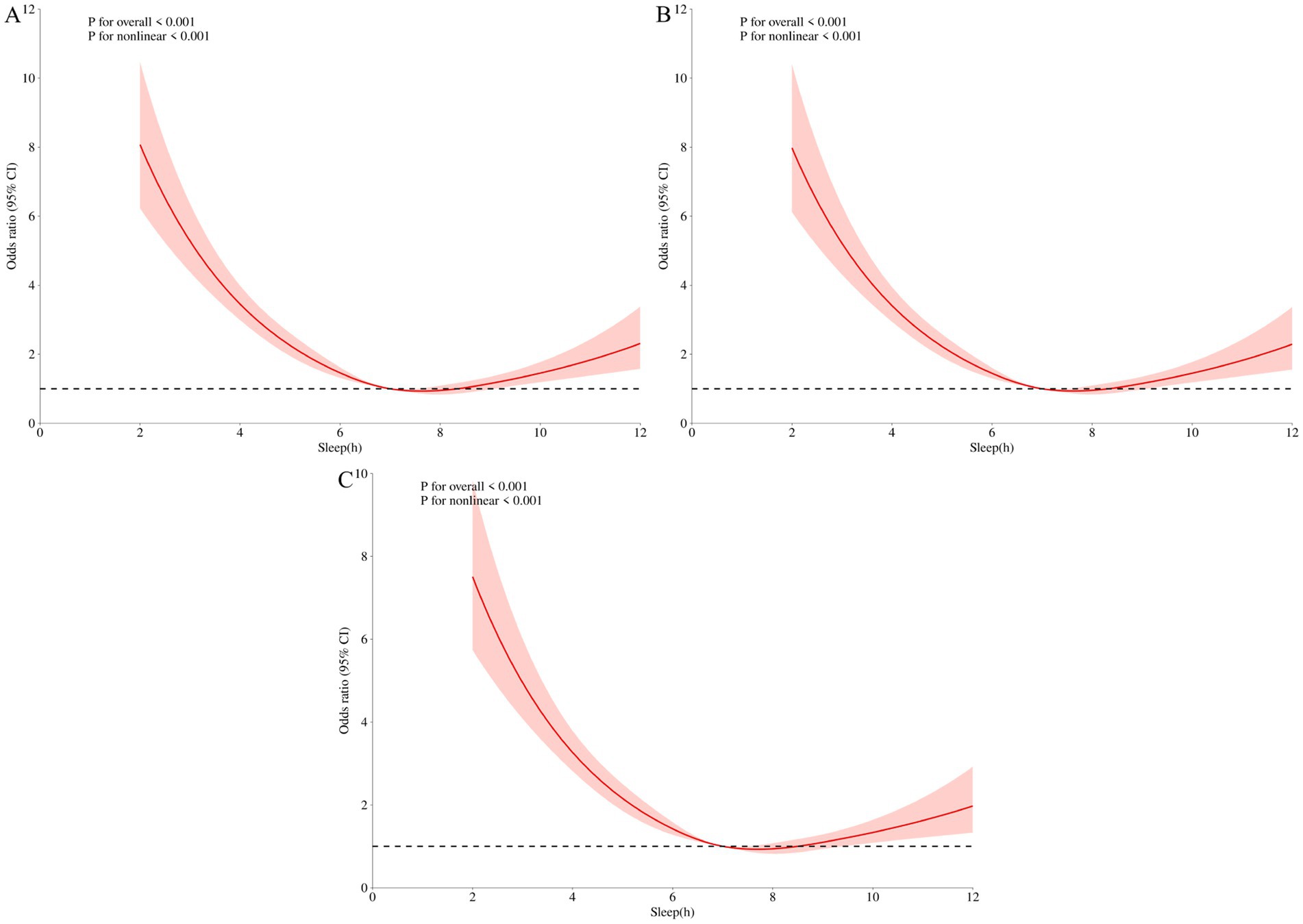
Figure 3. Sleep duration and sleep disorder restrictive cubic spline curve. (A) RCS 1 did not adjust for any variables; (B) RCS 2 incorporates analysis variables with significant differences in demographic characteristics (age, gender, education level, marital status) for adjustment; (C) RCS 3 adjusted for significant differences in demographic characteristics (age, gender, education level, marital status) and chronic diseases (Coronary heart disease, Stroke, Diabetes).
4 Discussion
Good sleep quality plays an important role in physical health. Effective sleep duration not only ensures the normal needs of the body, but also accelerates the recovery of physical and mental strength (32–36). Sleep disorders can lead to disrupted sleep patterns and disrupted regular daily activities, resulting in decreased mental energy and vitality, increased fatigue and sleep disorders (37, 38). They may also impair cognitive function (35, 36) and affect physical and mental health (39–41).
The NHANES questionnaire survey is a commonly used research method that collects a large amount of data to analyze people’s work habits, lifestyle, and sleep conditions, providing rich data support for research (42). This study conducted empirical analysis based on NHANES data, and the results showed a significant correlation between sedentary time, sleep duration, and sleep disorders, which is consistent with the findings of Heiland et al. (43–47). There is a non-linear dose–response relationship between sedentary time and sleep disorders. The risk of sleep disorders in adults increases with time after sedentary time reaches 300 min, which is consistent with the findings of Koohsari et al. (48–51). The reasons why prolonged sitting increases the risk of sleep disorders involve multiple physiological, psychological, and behavioral mechanisms. From a physiological mechanism analysis: Prolonged sitting leads to a decrease in bodily functions, especially affecting metabolism and blood circulation, all of which directly affect sleep quality. Sitting still for a long time can also reduce cerebral blood flow and affect areas related to sleep wake regulation, such as the hypothalamus and brainstem. Metabolic slowdown may also induce insulin resistance and obesity, indirectly exacerbating the risk of sleep apnea. Secondly, prolonged sitting is accompanied by stress reactions and disrupted cortisol secretion, leading to shallow sleep and early awakening. Prolonged sitting can also promote the release of pro-inflammatory cytokines such as IL-6 and TNF-α, and chronic low-grade inflammation is associated with fragmented sleep and reduced deep sleep. From the perspective of biological clock and neural regulation mechanisms, prolonged mental stress associated with prolonged sitting can activate the sympathetic nervous system, inhibit the relaxation state dominated by the parasympathetic nervous system at night, and manifest as difficulty falling asleep and sleep maintenance disorders (52). From the perspective of psychological and behavioral mechanisms, prolonged sitting is often associated with high-intensity work and long screen time. Continuous psychological stress can lead to excessive sympathetic nervous system stimulation, causing insomnia or sleep maintenance disorders (53, 54). Sedentary sitting leads to insufficient exercise, which directly affects sleep. Exercise improves sleep by increasing the accumulation of adenosine and regulating serotonin levels. Sedentary individuals lack pathways for exercise regulation. Sedentary individuals are more likely to continue sitting at night (such as using their phones or watching TV), delaying bedtime and disrupting their sleep rhythm. From the perspective of physical discomfort: Fixed posture leads to continuous compression of the cervical and lumbar vertebrae, muscle stiffness or soreness directly interfering with falling asleep. Sedentary sitting may also cause shoulder and neck strain, increasing the frequency of turning over or adjusting posture during sleep. Sedentary sitting can also lead to reduced venous reflux in the lower limbs, causing restless leg syndrome or nighttime leg cramps, disrupting sleep continuity. From the perspective of the interaction between society and the environment, prolonged sitting reduces exposure to natural light, weakens the adaptability of the biological clock to external light, and leads to abnormal secretion of melatonin and disrupted sleep wake cycles (55, 56). Lack of exercise and social interaction may increase the risk of depression, which is a common comorbidity of sleep disorders. Sleep disorders lead to daytime sleepiness and lack of energy, further reducing activity willingness and exacerbating the interaction between sedentary time and sleep problems (57). In addition, prolonged sitting is often associated with unhealthy eating habits, such as high calorie and high-fat food intake, which may also affect sleep. From a psychological perspective, prolonged periods of static living reduce physical activity, which may affect an individual’s mental health status, such as increasing the risk of anxiety and depression, which are direct causes of sleep disorders (58–60).
As age increases, the duration and quality of nighttime sleep decrease, which is consistent with previous research results (61–63). Further age subgroup analysis revealed that the fourth quartile of sedentary behavior in the middle-aged (<45) population has a higher risk of sleep disorders. In the middle-aged stage, excessive anxiety and tension may occur due to work competition, family responsibilities, etc., leading to difficulty falling asleep or maintaining sleep (64). Women approaching menopause (around 45 years old) may experience fluctuations in sex hormone levels, causing autonomic nervous system disorders and sleep problems (65). Gender subgroup analysis found that there are differences in the impact of sedentary time on sleep disorders between males and females. Males are more likely to experience sleep disorders, which may be related to physiological factors such as hormone levels and circadian rhythms, as well as psychological factors such as social roles and stress. The gradual decrease of testosterone in middle-aged men may cause metabolic disorders and autonomic nervous system disorders, indirectly leading to difficulty falling asleep or fragmented sleep. Men generally bear the burden of family economic support and social competition pressure, and long-term anxiety and tension can easily lead to chronic insomnia. Men are less likely to actively release negative emotions, and the accumulation of psychological stress may transform into somatic symptoms (such as insomnia). Excessive drinking, smoking, caffeine dependence, and other behaviors in men directly affect the excitability of the nervous system and disrupt sleep rhythms.
This study has certain limitations: firstly, it used cross-sectional surveys from 2007 to 2014, which cannot confirm the causal relationship between sedentary time, sleep duration, and sleep disorders; Secondly, sleep disorders are not only influenced by lifestyle habits, but also by factors such as living environment, social environment, family relationships, and economic level. Looking forward to future research continuing to focus on the relationship between sedentary time and sleep disorders, particularly investigating sleep fragmentation, sleep interruption time, sleep rhythms, and exploring more effective interventions to improve this issue.
5 Conclusion
In summary, there is a clear non-linear relationship between sedentary time, sleep duration, and sleep disorders. Therefore, it is recommended to limit sedentary time to 300 min per day, and to get up and move for 5–10 min every hour to engage in simple stretching or walking exercises to promote blood circulation and reduce health risks caused by prolonged sitting. It is recommended to engage in at least 30 min of moderate intensity or 15 min of high-intensity physical activity per day to improve sleep quality, and a recommended sleep duration of 7–8 h to reduce the risk of sleep disorders.
Data availability statement
The raw data supporting the conclusions of this article will be made available by the authors without undue reservation.
Ethics statement
Ethical review and approval was not required for the study on human participants in accordance with the local legislation and institutional requirements. Written informed consent from the patients or patients legal guardian/next of kin was not required to participate in this study in accordance with the national legislation and the institutional requirements.
Author contributions
KJ: Writing – original draft, Writing – review & editing. NL: Data curation, Formal analysis, Methodology, Resources, Supervision, Validation, Visualization, Conceptualization, Investigation, Software, Writing – original draft, Writing – review & editing. RW: Conceptualization, Data curation, Formal analysis, Funding acquisition, Investigation, Methodology, Project administration, Resources, Software, Supervision, Validation, Visualization, Writing – original draft, Writing – review & editing. XS: Data curation, Formal analysis, Funding acquisition, Methodology, Project administration, Resources, Supervision, Validation, Visualization, Conceptualization, Investigation, Software, Writing – original draft, Writing – review & editing.
Funding
The author(s) declare that no financial support was received for the research and/or publication of this article.
Acknowledgments
Thank you to all participants of NHANES for their support and contributions.
Conflict of interest
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
Publisher’s note
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
References
1. Zhou, Q, Guo, C, Yang, X, and He, N. Dose-response association of total sedentary behaviour and television watching with risk of depression in adults: a systematic review and meta-analysis. J Affect Disord. (2023) 324:652–9. doi: 10.1016/j.jad.2022.12.098
2. Matricciani, L, Bin, YS, Lallukka, T, Kronholm, E, Wake, M, Paquet, C, et al. Rethinking the sleep-health link. Sleep Health. (2018) 4:339–48. doi: 10.1016/j.sleh.2018.05.004
3. Baranwal, N, Yu, PK, and Siegel, NS. Sleep physiology, pathophysiology, and sleep hygiene. Prog Cardiovasc Dis. (2023) 77:59–69. doi: 10.1016/j.pcad.2023.02.005
4. Seweryn, P, Orzeszek, SM, Waliszewska-Prosół, M, Jenča, A, Osiewicz, M, Paradowska-Stolarz, A, et al. Relationship between pain severity, satisfaction with life and the quality of sleep in polish adults with temporomandibular disorders. Dent Med Probl. (2023) 60:609–17. doi: 10.17219/dmp/171894
5. Seweryn, P, Waliszewska-Prosol, M, Straburzynski, M, Smardz, J, Orzeszek, S, Bombala, W, et al. Prevalence of central sensitization and somatization in adults with temporomandibular disorders-a prospective observational study. J Oral Facial Pain Headache. (2024) 38:33–44. doi: 10.22514/jofph.2024.037
6. Chattrattrai, T, Thymi, M, Su, N, and Lobbezoo, F. Changes in self-reported sleep and awake bruxism in relation to the management of temporomandibular disorders ("care as usual") in a specialty clinic population. Dent Med Probl. (2024) 61:697–704. doi: 10.17219/dmp/193125
7. Chattrattrai, T, Aarab, G, Su, N, Blanken, TF, Mitrirattanakul, S, and Lobbezoo, F. The association of self-reported awake bruxism and sleep bruxism with temporomandibular pain and dysfunction in adult patients with temporomandibular disorders. Clin Oral Investig. (2023) 27:7501–11. doi: 10.1007/s00784-023-05338-y
8. Grandner, MA, and Fernandez, FX. The translational neuroscience of sleep: a contextual framework. Science. (2021) 374:568–73. doi: 10.1126/science.abj8188
9. Shi, L, Chen, SJ, Ma, MY, Bao, YP, Han, Y, Wang, YM, et al. Sleep disturbances increase the risk of dementia: a systematic review and meta-analysis. Sleep Med Rev. (2018) 40:4–16. doi: 10.1016/j.smrv.2017.06.010
10. Kwok, CS, Kontopantelis, E, Kuligowski, G, Gray, M, Muhyaldeen, A, Gale, CP, et al. Self-reported sleep duration and quality and cardiovascular disease and mortality: a dose-response meta-analysis. J Am Heart Assoc. (2018) 7:e008552. doi: 10.1161/jaha.118.008552
11. Cao, Z, Xu, C, Zhang, P, and Wang, Y. Associations of sedentary time and physical activity with adverse health conditions: outcome-wide analyses using isotemporal substitution model. Eclinicalmedicine. (2022) 48:101424. doi: 10.1016/j.eclinm.2022.101424
12. Tremblay, MS, Aubert, S, Barnes, JD, Saunders, TJ, Carson, V, Latimer-Cheung, AE, et al. Sedentary behavior research network (SBRN) - terminology consensus project process and outcome. Int J Behav Nutr Phys Act. (2017) 14:75. doi: 10.1186/s12966-017-0525-8
13. Ekelund, U, Brown, WJ, Steene-Johannessen, J, Fagerland, MW, Owen, N, Powell, KE, et al. Do the associations of sedentary behaviour with cardiovascular disease mortality and cancer mortality differ by physical activity level? A systematic review and harmonised meta-analysis of data from 850 060 participants. Br J Sports Med. (2019) 53:886–94. doi: 10.1136/bjsports-2017-098963
14. Patterson, R, mcnamara, E, Tainio, M, de Sá, TH, Smith, AD, Sharp, SJ, et al. Sedentary behaviour and risk of all-cause, cardiovascular and cancer mortality, and incident type 2 diabetes: a systematic review and dose response meta-analysis. Eur J Epidemiol. (2018) 33:811–29. doi: 10.1007/s10654-018-0380-1
15. Ford, ES, and Caspersen, CJ. Sedentary behaviour and cardiovascular disease: a review of prospective studies. Int J Epidemiol. (2012) 41:1338–53. doi: 10.1093/ije/dys078
16. Ross, R, Chaput, JP, Giangregorio, LM, Janssen, I, Saunders, TJ, Kho, ME, et al. Canadian 24-hour movement guidelines for adults aged 18-64 years and adults aged 65 years or older: an integration of physical activity, sedentary behaviour, and sleep. Appl Physiol Nutr Metab. (2020) 45:S57–S102. doi: 10.1139/apnm-2020-0467
17. Saunders, TJ, mcisaac, T, Douillette, K, Gaulton, N, Hunter, S, Rhodes, RE, et al. Sedentary behaviour and health in adults: an overview of systematic reviews. Appl Physiol Nutr Metab. (2020) 45:S197–s217. doi: 10.1139/apnm-2020-0272
18. Bull, FC, Al-Ansari, SS, Biddle, S, Borodulin, K, Buman, MP, Cardon, G, et al. World health organization 2020 guidelines on physical activity and sedentary behaviour. Br J Sports Med. (2020) 54:1451–62. doi: 10.1136/bjsports-2020-102955
19. Chaput, JP, Willumsen, J, Bull, F, Chou, R, Ekelund, U, Firth, J, et al. 2020 WHO guidelines on physical activity and sedentary behaviour for children and adolescents aged 5-17 years: summary of the evidence. Int J Behav Nutr Phys Act. (2020) 17:141. doi: 10.1186/s12966-020-01037-z
20. Dempsey, PC, Friedenreich, CM, Leitzmann, MF, Buman, MP, Lambert, E, Willumsen, J, et al. Global public health guidelines on physical activity and sedentary behavior for people living with chronic conditions: a call to action. J Phys Act Health. (2021) 18:76–85. doi: 10.1123/jpah.2020-0525
21. Dipietro, L, Al-Ansari, SS, Biddle, SJH, Borodulin, K, Bull, FC, Buman, MP, et al. Advancing the global physical activity agenda: recommendations for future research by the 2020 WHO physical activity and sedentary behavior guidelines development group. Int J Behav Nutr Phys Act. (2020) 17:143. doi: 10.1186/s12966-020-01042-2
22. Dempsey, PC, Biddle, SJH, Buman, MP, Chastin, S, Ekelund, U, Friedenreich, CM, et al. New global guidelines on sedentary behaviour and health for adults: broadening the behavioural targets. Int J Behav Nutr Phys Act. (2020) 17:151. doi: 10.1186/s12966-020-01044-0
23. Katzmarzyk, PT, Powell, KE, Jakicic, JM, Troiano, RP, Piercy, K, and Tennant, B. Sedentary behavior and health: update from the 2018 physical activity guidelines advisory committee. Med Sci Sports Exerc. (2019) 51:1227–41. doi: 10.1249/mss.0000000000001935
24. Zhao, R, Bu, W, Chen, Y, and Chen, X. The dose-response associations of sedentary time with chronic diseases and the risk for all-cause mortality affected by different health status: a systematic review and meta-analysis. J Nutr Health Aging. (2020) 24:63–70. doi: 10.1007/s12603-019-1298-3
25. Young, DR, Hivert, MF, Alhassan, S, Camhi, SM, Ferguson, JF, Katzmarzyk, PT, et al. Sedentary behavior and cardiovascular morbidity and mortality: a science advisory from the American Heart Association. Circulation. (2016) 134:e262–79. doi: 10.1161/cir.0000000000000440
26. Cheng, J, Huang, Y, Ren, Z, Xu, P, Tan, J, Huang, B, et al. Compositional isotemporal substitution analysis of physical activity, sedentary behaviour and cardiometabolic biomarkers in US adults: a nationally representative study. Eur J Sport Sci. (2023) 23:2119–28. doi: 10.1080/17461391.2023.2177198
27. Hansen, BH, Anderssen, SA, Andersen, LB, Hildebrand, M, Kolle, E, Steene-Johannessen, J, et al. Cross-sectional associations of reallocating time between sedentary and active behaviours on cardiometabolic risk factors in young people: an international children's accelerometry database (ICAD) analysis. Sports Med. (2018) 48:2401–12. doi: 10.1007/s40279-018-0909-1
28. Silva, RR, Galvão, LL, Martins, GS, Meneguci, J, Virtuoso-Júnior, JS, Santos, DAT, et al. Reallocation of time spent on sedentary behavior by time spent on physical activity reduces dynapenia in older adults: a prospective cohort study. Sao Paulo Med J. (2022) 141:2022188. doi: 10.1590/1516-3180.2022.0188.R2.20092022
29. Meneguci, J, Galvão, LL, Tribess, S, Meneguci, CAG, and Virtuoso Júnior, JS. Isotemporal substitution analysis of time between sleep, sedentary behavior, and physical activity on depressive symptoms in older adults: a cross-sectional study. Sao Paulo Med J. (2024) 142:e2023144. doi: 10.1590/1516-3180.2023.0144.R2.04122023
30. Wei, J, Xie, L, Song, S, Wang, T, and Li, C. Isotemporal substitution modeling on sedentary behaviors and physical activity with depressive symptoms among older adults in the U.S.: the national health and nutrition examination survey, 2007-2016. J Affect Disord. (2019) 257:257–62. doi: 10.1016/j.jad.2019.07.036
31. Kracht, CL, Katzmarzyk, PT, Champagne, CM, Broyles, ST, Hsia, DS, Newton, RL Jr, et al. Association between sleep, sedentary time, physical activity, and adiposity in adolescents: a prospective observational study. Med Sci Sports Exerc. (2023) 55:110–8. doi: 10.1249/mss.0000000000003018
32. Hayley, AC, Williams, LJ, Venugopal, K, Kennedy, GA, Berk, M, and Pasco, JA. The relationships between insomnia, sleep apnoea and depression: findings from the American national health and nutrition examination survey, 2005-2008. Aust N Z J Psychiatry. (2015) 49:156–70. doi: 10.1177/0004867414546700
33. Dalmases, M, Benítez, I, Sapiña-Beltran, E, Garcia-Codina, O, Medina-Bustos, A, Escarrabill, J, et al. Impact of sleep health on self-perceived health status. Sci Rep. (2019) 9:7284. doi: 10.1038/s41598-019-43873-5
34. Nie, Q, Shen, Y, Luo, M, Sheng, Z, Zhou, R, Li, G, et al. Analysis of sleep for the American population: result from NHANES database. J Affect Disord. (2024) 347:134–43. doi: 10.1016/j.jad.2023.11.082
35. German, C, Makarem, N, Fanning, J, Redline, S, Elfassy, T, mcclain, A, et al. Sleep, sedentary behavior, physical activity, and cardiovascular health: MESA. Med Sci Sports Exerc. (2021) 53:724–31. doi: 10.1249/mss.0000000000002534
36. Manifield, J, Chaudhry, Y, Singh, SJ, Ward, TJC, Whelan, ME, and Orme, MW. Changes in physical activity, sedentary behaviour and sleep following pulmonary rehabilitation: a systematic review and network meta-analysis. Eur Respir Rev. (2024) 33:230225. doi: 10.1183/16000617.0225-2023
37. Pan, CW, Cong, X, Zhou, HJ, Li, J, Sun, HP, Xu, Y, et al. Self-reported sleep quality, duration, and health-related quality of life in older Chinese: evidence from a rural town in Suzhou, China. J Clin Sleep Med. (2017) 13:967–74. doi: 10.5664/jcsm.6696
38. Peng, A, Ji, S, Lai, W, Hu, D, Wang, M, Zhao, X, et al. The bidirectional relationship between sleep disturbance and anxiety: sleep disturbance is a stronger predictor of anxiety. Sleep Med. (2024) 121:63–8. doi: 10.1016/j.sleep.2024.06.022
39. Asplund, CA. The importance of sleep for health and athletic performance. Sports Health. (2024) 16:499–500. doi: 10.1177/19417381241257952
40. Jiang, J, Li, Y, Mao, Z, Wang, F, Huo, W, Liu, R, et al. Abnormal night sleep duration and poor sleep quality are independently and combinedly associated with elevated depressive symptoms in Chinese rural adults: Henan rural cohort. Sleep Med. (2020) 70:71–8. doi: 10.1016/j.sleep.2019.10.022
41. Yin, J, Jin, X, Shan, Z, Li, S, Huang, H, Li, P, et al. Relationship of sleep duration with all-cause mortality and cardiovascular events: a systematic review and dose-response meta-analysis of prospective cohort studies. J Am Heart Assoc. (2017) 6:e005947. doi: 10.1161/jaha.117.005947
42. Cheng, TD, Ferderber, C, Kinder, B, and Wei, YJ. Trends in dietary vitamin a intake among US adults by race and ethnicity, 2003-2018. JAMA. (2023) 329:1026–9. doi: 10.1001/jama.2023.0636
43. Heiland, EG, Ekblom, Ö, Bojsen-Møller, E, Larisch, LM, Blom, V, and Ekblom, MM. Bi-directional, day-to-day associations between objectively-measured physical activity, sedentary behavior, and sleep among office workers. Int J Environ Res Public Health. (2021) 18:7999. doi: 10.3390/ijerph18157999
44. Kim, Y, Wijndaele, K, Sharp, SJ, Strain, T, Pearce, M, White, T, et al. Specific physical activities, sedentary behaviours and sleep as long-term predictors of accelerometer-measured physical activity in 91,648 adults: a prospective cohort study. Int J Behav Nutr Phys Act. (2019) 16:41. doi: 10.1186/s12966-019-0802-9
45. Hofman, A, Voortman, T, Ikram, MA, and Luik, AI. Time spent in physical activity, sedentary behavior, and sleep: associations with self-rated sleep quality in middle-aged and older adults. Sleep Health. (2022) 8:701–4. doi: 10.1016/j.sleh.2022.06.009
46. Vancampfort, D, Stubbs, B, Firth, J, Hagemann, N, Myin-Germeys, I, Rintala, A, et al. Sedentary behaviour and sleep problems among 42,489 community-dwelling adults in six low- and middle-income countries. J Sleep Res. (2018) 27:e12714. doi: 10.1111/jsr.12714
47. Huang, WC, Chang, SH, Hsueh, MC, and Liao, Y. Relationship of sleep regularity with device-based sedentary behavior time and physical activity time in working adults. Sleep Health. (2023) 9:86–92. doi: 10.1016/j.sleh.2022.10.002
48. Koohsari, MJ, Yasunaga, A, mccormack, GR, Shibata, A, Ishii, K, Liao, Y, et al. Sedentary behaviour and sleep quality. Sci Rep. (2023) 13:1180. doi: 10.1038/s41598-023-27882-z
49. Liangruenrom, N, Dumuid, D, and Pedisic, Z. Physical activity, sedentary behaviour, and sleep in the Thai population: a compositional data analysis including 135,824 participants from two national time-use surveys. PLoS One. (2023) 18:e0280957. doi: 10.1371/journal.pone.0280957
50. Jeong, SH, Jang, BN, Kim, SH, Kim, GR, Park, EC, and Jang, SI. Association between sedentary time and sleep quality based on the Pittsburgh sleep quality index among South Korean adults. BMC Public Health. (2021) 21:2290. doi: 10.1186/s12889-021-12388-y
51. Jayamaha, AR, Jones, AV, Katagira, W, Girase, B, Yusuf, ZK, Pina, I, et al. Systematic review of physical activity, sedentary behaviour and sleep among adults living with chronic respiratory disease in low- and middle-income countries. Int J Chron Obstruct Pulmon Dis. (2022) 17:821–54. doi: 10.2147/copd.S345034
52. Greenlund, IM, and Carter, JR. Sympathetic neural responses to sleep disorders and insufficiencies. Am J Physiol Heart Circ Physiol. (2022) 322:H337–h349. doi: 10.1152/ajpheart.00590.2021
53. Yang, Y, Shin, JC, Li, D, and An, R. Sedentary behavior and sleep problems: a systematic review and meta-analysis. Int J Behav Med. (2017) 24:481–92. doi: 10.1007/s12529-016-9609-0
54. Li, D, and Li, X. Independent and combined associations between physical activity and sedentary time with sleep quality among Chinese college students. Int J Environ Res Public Health. (2022) 19:6697. doi: 10.3390/ijerph19116697
55. Xie, Z, Chen, F, Li, WA, Geng, X, Li, C, Meng, X, et al. A review of sleep disorders and melatonin. Neurol Res. (2017) 39:559–65. doi: 10.1080/01616412.2017.1315864
56. Cajochen, C, Kräuchi, K, and Wirz-Justice, A. Role of melatonin in the regulation of human circadian rhythms and sleep. J Neuroendocrinol. (2003) 15:432–7. doi: 10.1046/j.1365-2826.2003.00989.x
57. Bloomberg, M, Brocklebank, L, Hamer, M, and Steptoe, A. Joint associations of physical activity and sleep duration with cognitive ageing: longitudinal analysis of an English cohort study. Lancet Healthy Longev. (2023) 4:e345–53. doi: 10.1016/s2666-7568(23)00083-1
58. Zhang, X, Mao, F, Wu, L, Zhang, G, Huang, Y, Chen, Q, et al. Associations of physical activity, sedentary behavior and sleep duration with anxiety symptoms during pregnancy: an isotemporal substitution model. J Affect Disord. (2022) 300:137–44. doi: 10.1016/j.jad.2021.12.102
59. Vancampfort, D, Van Damme, T, Stubbs, B, Smith, L, Firth, J, Hallgren, M, et al. Sedentary behavior and anxiety-induced sleep disturbance among 181,093 adolescents from 67 countries: a global perspective. Sleep Med. (2019) 58:19–26. doi: 10.1016/j.sleep.2019.01.048
60. Luo, Y, Li, Y, Xie, J, Duan, Y, Gan, G, Zhou, Y, et al. Symptoms of depression are related to sedentary behavior and sleep duration in elderly individuals: a cross-sectional study of 49,317 older Chinese adults. J Affect Disord. (2022) 308:407–12. doi: 10.1016/j.jad.2022.04.102
61. Zitser, J, Allen, IE, Falgàs, N, Le, MM, Neylan, TC, Kramer, JH, et al. Pittsburgh sleep quality index (PSQI) responses are modulated by total sleep time and wake after sleep onset in healthy older adults. PLoS One. (2022) 17:e0270095. doi: 10.1371/journal.pone.0270095
62. Feinsilver, SH, and Hernandez, AB. Sleep in the elderly: unanswered questions. Clin Geriatr Med. (2017) 33:579–96. doi: 10.1016/j.cger.2017.06.009
63. Feinsilver, SH. Normal and abnormal sleep in the elderly. Clin Geriatr Med. (2021) 37:377–86. doi: 10.1016/j.cger.2021.04.001
64. Farnsworth, JL, Kim, Y, and Kang, M. Sleep disorders, physical activity, and sedentary behavior among U.S. adults: national health and nutrition examination survey. J Phys Act Health. (2015) 12:1567–75. doi: 10.1123/jpah.2014-0251
Keywords: sedentary behavior, sleep duration, sleep disorders, RCS, subgroup analysis
Citation: Ju K, Liu N, Wu R and Shi X (2025) The relationship between sedentary behavior, sleep duration, and sleep disorders: analysis of the 2007–2014 National Health and Nutrition Examination Survey. Front. Neurol. 16:1488443. doi: 10.3389/fneur.2025.1488443
Edited by:
Qing-Wei Chen, South China Normal University, ChinaReviewed by:
Anna Paradowska-Stolarz, Wroclaw Medical University, PolandDuy-Thai Nguyen, Ministry of Health, Vietnam
Yinghua He, FR Acupuncture & Chinese Medicine Clinic, United States
Xuexing Luo, Macau University of Science and Technology, Macao SAR, China
Copyright © 2025 Ju, Liu, Wu and Shi. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Xiujiang Shi, ODY1NTY0MzU1QHFxLmNvbQ==
†These authors share first authorship
 Keke Ju
Keke Ju Na Liu2†
Na Liu2† Ruikai Wu
Ruikai Wu