- 1Legal Medicine Research Center, Legal Medicine Organization, Tehran, Iran
- 2Department of Gastroenterology and Hepatology, School of Medicine, Shahid Modarres Hospital, Shahid Beheshti University of Medical Sciences, Tehran, Iran
- 3Social Determinants of Health Research Center, Alborz University of Medical Sciences, Karaj, Iran
- 4Social Determinants of Health Research Center, Health Management and Safety Promotion Research Institute, Tabriz University of Medical Sciences, Tabriz, Iran
- 5Department of Criminal Law and Criminology, Islamic Azad University, Tehran, Iran
Background: Suicide is a public health issue and a main cause of mortality among adolescents and the youth worldwide, particularly in developing countries.
Objectives: The present research is a systematic review aiming to investigate the spatial, geographical, and demographic factors related to suicide among adolescents and the youth.
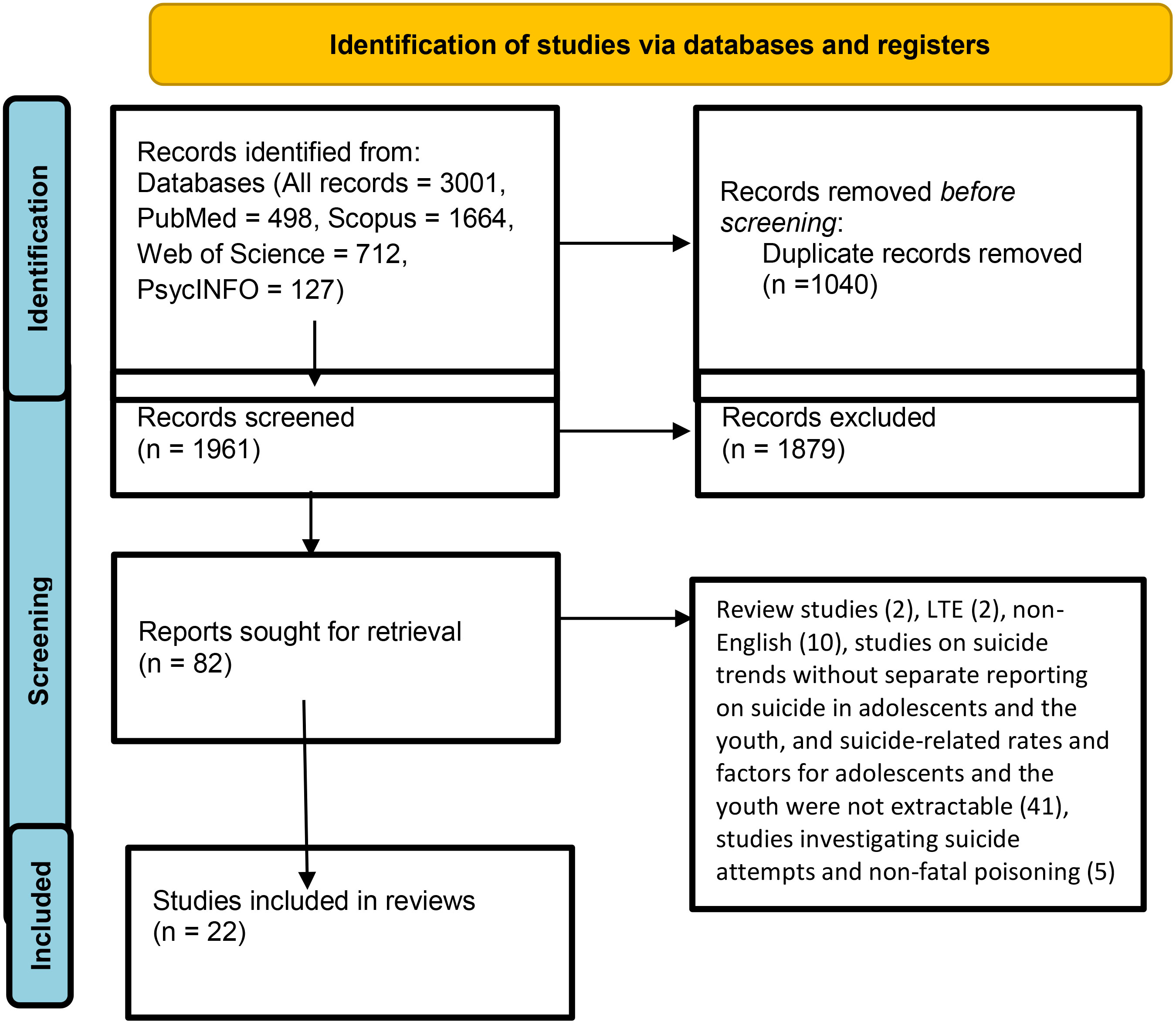
Methods: In this systematic review, two researchers examined PsycINFO, Web of Science, Scopus, and PubMed databases on December 7th, 2022 with no time limits from the beginning of publication until 2022 to identify the primary studies on spatial and geographic analysis on adolescent and youth suicides. Once duplicate studies were identified and removed, the titles and abstracts of studies were examined and irrelevant studies were also removed. Finally, 22 studies were reviewed based on the inclusion criteria.
Results: Our findings show that suicide rates are generally higher among men, residents of rural and less densely populated regions, coastal and mountainous regions, natives, 15-29 age group, less privileged populations with social fragmentation, unemployed, divorced or lonely people, those who live in single parent families, people with mental health issues, and those with low levels of education.
Conclusions: Stronger evidence supports the effects of geographic and demographic variables on youth and adolescent suicide rates as compared with spatial variables. These findings suggest that policy makers take spatial and demographic factors into consideration when health systems allocate resources for suicide prevention, and that national policymakers integrate demographic and geographic variables into health service programs.
Systematic Review Registration: https://www.crd.york.ac.uk/prospero/, identifier CRD42023430994.
Backgrounds
Suicide is defined as a death directly or indirectly caused by intentionally poisoning or injuring oneself (1). As a serious public health issue, suicide constitutes the cause of death of about 800,000 (1.4%) individuals per year in the world (2). Approximately 78% of suicide cases have been reported in low-income countries (3). The annual frequency of suicide in different countries ranges from below 1 per 100,000 deaths in Saudi Arabia and Belize to over 40 per 100,000 deaths in Lithuania and Guyana (4, 5). In 2016, the WHO estimated the annual mortality from suicide at 10.7 per 100,000 (6).
Suicide is a major cause of mortality among the youth and adolescents, especially in developing countries (7). In 2015, suicide was reported as the cause of death among 6% of adolescents (8, 9). After road accidents, suicide constitutes the second leading cause of death among individual aged 10-24 years (10, 11). Research suggests 1-10% of adolescents commit suicide at least once in their life given the social stigma of suicide and its misclassification (12–14), the suicide frequency is underestimated at 164,000 in individuals aged below 25 years (15, 16).
Pesticide poisoning, hanging and use of firearms globally constitute the cause of 30% of suicides. The means of suicide used by the victims largely depends on their accessibility to lethal objects (17, 18). Suicide exerts severe and long-lasting effects on the family and friends as suicide survivors. Research suggests positive relationships between degree of depression in the bereaved and their closeness with those committing suicide (19, 20). “Suicide and self-inflicted injuries” was the 14th and 18th (21) leading cause of disability-adjusted life years in 2013 and 2016, respectively (22).
Given the significant social and individual effects of suicide, acquiring awareness of its temporal and spatial patterns in different demographic groups by age, gender and ethnicity and identifying the causes of changes in these patterns are essential for designing effective suicide control and prevention plans. Identifying both risk factors and socio-geographical background is also integral to an effective suicide prevention strategy (23, 24).
Spatial analysis can help investigate the geographic pattern of suicide (25), identify areas with greater risk of suicide, explore the potential relationship between local factors and suicide risk (26), and assess the rates across geographic units (27).
Multiple factors are associated with suicide as the outcome of complex interactions of individuals with family members and their community (28). Research suggests suicide relates to genetic, social and family factors (29) and psychological factors such as depression and anxiety (29–31) as well as adverse childhood experiences, neglect by parents (32), age, gender, sexual orientation, socioeconomic status (33, 34), academic achievement and absenteeism (35, 36), and substance abuse (2). Suicide protective factors also include having a large number of children, family support, coping skills and religiousness (37–39).
Despite the importance of these studies, their limitations include failure to explain suicide and its distribution in different locations. National and global initiatives based on early risk detection and management play a key role in saving lives and suicide prevention as a public health priority. As a suicide monitoring method, spatial and geographic analyses have been conducted to identify high suicide-risk areas (40). These analyses can assist policymakers in determining the causes of suicide, predicating local suicide patterns based on suicide-related data and developing suicide prevention strategies and appropriate interventions in high-risk regions. The present research was therefore conducted to systematically review the spatial and geographic analysis of suicide and its demographic factors in adolescents and the youth.
Methods
Study design
This systematic review was performed to investigate the spatial, geographic and demographic factors of suicide in adolescents and the youth based on the Preferred Reporting Items for Systematic Reviews and Meta-Analyses (PRISMA) (41), as a guideline for appropriate and accurate information sources. After formulating the research question, the search strategy was designed and the systematic review was conducted by screening for eligible articles. Afterwards, two researchers independently employed the Strengthening the Reporting of Observational studies in Epidemiology (STROBE) (42) to qualitatively evaluate the articles and extract data. A third person resolved potential conflicts in the interpretation of data. This systematic review has been registered on the International Prospective Register of Systematic Reviews (PROSPERO, Registration number: CRD42023430994).
Research question
The research question was formulated based on the population (P), exposure (E), comparator (C), and outcome of interest (O) in the review (PECO) for spatial and geographic analysis of completed suicide in teenagers and young adults (Studies and findings related to suicidal idea and suicidal thoughts, suicidal intention, unsuccessful attempts to commit suicide were excluded). PECO helps researchers create research questions (43). Three main dimensions of spatial, geographic, and demographic factors (E, exposure, interest), suicide (O, outcome based on the study interest) of adolescent and young boys and girls, and (P, population) were investigated by the researchers. Accordingly, what is the research question, and spatial, geographic, and demographic factors related to suicide in adolescents and the youth? It must be noted that the study was not context-specific (C).
Systematic search
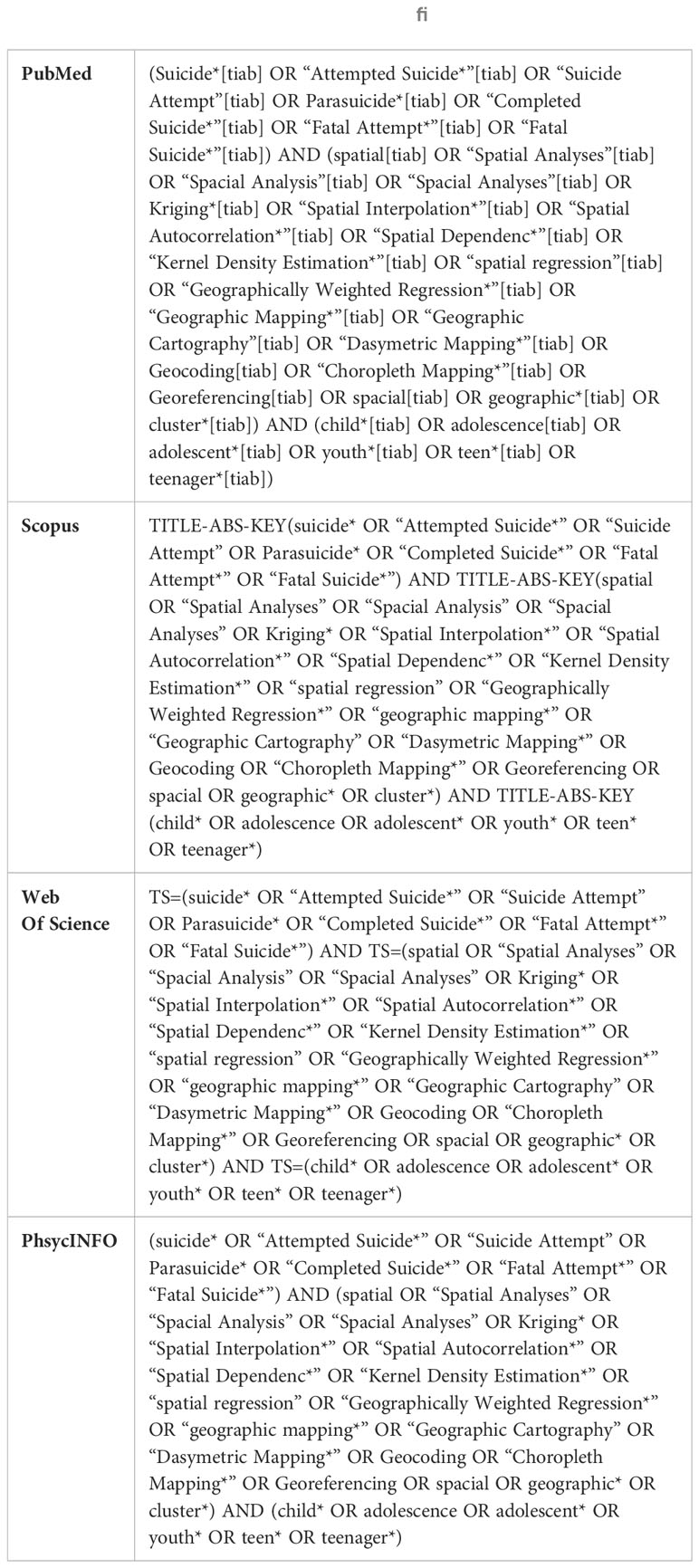
Table 1 presents the strategy of systematic search before identification and screening. The keyword search was enriched in the identification stage using synonyms and based on MeSH in PubMed, and was modified for other databases. Boolean operators were also used along with keywords. We retrieved 3001 articles in the systematic literature search conducted in PubMed, Scopus, Web of Science and PsycINFO on 7 December 2022. These four databases were selected due to their academic nature and accessibility in Iran. The retrieved data were entered into EndNote and 1040 duplicate articles were identified and eliminated.
Screening and inclusion and exclusion criteria
Two researchers separately assessed the titles and abstracts of 1961 studies for relevance. The search was run from database inception till December 7th, 2022 with no time limits with the inclusion criteria of being an original study in the English language, and focused on the spatial and geographic analysis of suicide in adolescents and the youth. Only studies on completed suicides were included. Studies and findings for suicidal ideation, suicide attempts, and failed suicides were excluded. Thus, qualitative studies, case reports, systematic reviews, meta-analyses, review studies, conference papers, book chapters, letters to editors, and intervention studies were excluded. Finally, 82 studies remained for full text evaluation.
Eligibility
Two of the authors independently evaluated the full texts of 82 studies, which resulted in the exclusion of 60 studies for reasons stated in Figure 1. The remaining studies were entered into the quality evaluation and data extraction process.
Quality assessment
The remaining articles were examined after the full-text reading stage and determining the eligibility in terms of the risk of bias assessment to ensure the quality of the studies (44). The quality of the studies was evaluated based on the STROBE checklist, and finally 22 articles were included for review in the present study. Quality assessment was performed by two people independently. The articles that scored between 11-16 were evaluated as appropriate and the articles that scored more than 16 were evaluated as good (45, 46). Each study was evaluated to check the potential risk of biases through the key areas of study design, sample size justification, target population, sampling strategy, sample selection, validity and reliability of measurement, methodological limitations, and discussion. Any differences between the two authors were resolved through discussion until an agreement was reached.
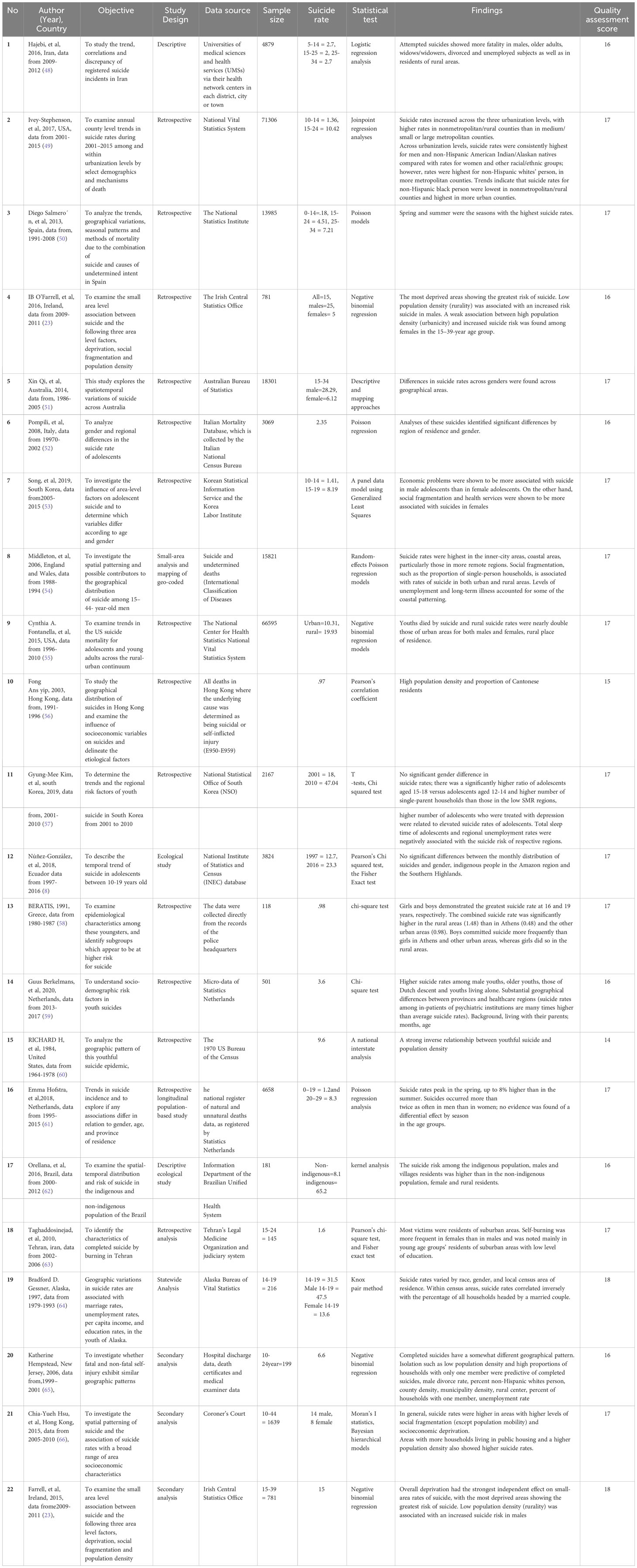
The two researchers independently extracted the following data from the studies: author’s name, publication date, country, study objective, study design, sample volume, statistical test, and findings. Disputes were resolved by talking and help from a third person. In the next stage, the researchers systematically merged the findings based on the use of words, text, and study findings to explain relationships between the extracted data (47). Discussions between the researchers about the relationship of similar data led to classification of the data into different categories. This technique was repeated until logical findings were formed for interpretation. Table 2 presents the results of the study review.
Data synthesis
Considering the method of systematic review for examining a spatial, geographic, and demographic analysis of factors associated with adolescent and youth suicide, a narrative synthesis was considered to be the most appropriate method of data analysis.
Results
Eight studies from Europe, seven from America, six from Asia, and one from Oceania were reviewed in the present study. No studies from Africa were retrieved in the review. The lowest suicide rate was reported at 0.97 per 100,000 in Hong Kong and the highest at 65.2 per 100,000 in Brazil. Most studies were longitudinal and retrospective. Regression and Poisson analyses were the most frequently used statistical tests in the studies. The largest sample size pertained to a study from the US with 71,306 people and the smallest sample size was 118 people in a study from Greece.
Age
Review of literature revealed lower suicide rates for the age group under 15 as compared with the age group 15-29 in most studies. As age increased in the 15-29 age group, suicide rates also increased (49, 54, 58, 60).
Gender
In most of the reviewed studies, men had higher suicide rates than women (8, 49–51, 54, 59, 60, 63, 65), but some studies reported higher death rates due to self-burning in women aged 15-24 (64), and completed suicide rates as higher in girls living in rural areas (8, 59). Also, despite the higher suicide rates for men, certain studies showed no difference between men and women (57), especially in the under-14 age bracket (53). In one study, however, suicide rates for men and women in rural areas were about twice as high as those for men and women in urban areas (55).
Depression
Higher suicide rates have been reported in regions with high numbers of patients with treated depression or under treatment for mental disorders (57).
Education level
Studies reported a significant relationship between low levels of education and self-burning (63). Only one study reported a significant relationship between high levels of education in mothers and higher suicide rates in adolescents and the youth (57).
Social isolation
Certain studies reported a low population density (60) with a high proportion of one-member and single-parent households as a suicide predictor (53, 54, 57, 65). One study showed lower suicide rates for people living in families than for those living alone (59).
Race and ethnicity
In two studies conducted in urban areas, minority people suffered higher suicide rates than other ethnic and racial groups (49, 65). However, the majority of studies showed higher suicide rates for natives of Alaska, Brazil, the Netherlands, Hong Kong, and Ecuador than non-natives, immigrants, and white individuals (8, 49, 56, 59, 62, 64).
Marital status
Some studies have confirmed the relationship between divorce and suicide [66]. Suicide rates also showed an inverse relationship with the percentage of households headed by married couples (65). Suicide rates were higher among widowed and divorced people than among married couples (64). Married women showed a higher rate of suicide and death by self-burning than married men (48).
Employment status
Several studies have confirmed the relationship between unemployment and suicide (48, 54, 65). Only one study showed a higher suicide rate in regions with low unemployment (57).
Deprivation and social fragmentation
Higher suicide rates were observed in underprivileged regions with social fragmentation (23, 66). Studies have shown higher suicide rates in men than in women in underprivileged regions (23).
Urban and rural area and the suburbs
The majority of studies reported higher suicide rates in regions classified as rural (23, 23, 48, 49, 54, 58, 62, 62, 65). Higher suicide rates were also reported in the suburbs relative to urban areas (49, 63). Other studies reported higher suicide rates in cities with psychiatric hospitals (59). Certain studies reported higher suicide rates for rural girls and urban boys (58). Other studies reported higher suicide rates for urban girls and rural boys (23). One study on the urban areas of the US reported a higher suicide rate among men and natives compared to women and non-natives (49).
Socioeconomic status
Higher suicide rates were observed in areas with a lower socioeconomic status (23, 66).
Highlands, mountainous, and coastal areas
A study in Ecuador reported a high suicide rate in the highlands and mountainous areas of the Amazon (8). A higher suicide rate was also observed in the Welsh and English coastal areas (54). Higher suicide rates were observed for the youths of northern Italy and Australia compared to other regions (51, 52).
Population density and housing
Areas with a larger number of families living in more populated public housing (66) had higher suicide rates (23, 53, 56, 66). Some studies also report higher suicide rates in low density populations (54, 60), or lower risk of suicide in high density populations (23).
Seasons of the year
Some studies reported that suicide rates were higher in the spring (50, 61) and summer (50). Other studies, however, showed no relationship between suicide and days and seasons of the year (8, 59, 63).
Miscellaneous
One study showed a relationship between the poverty rate, GDP per capita, employment rate, foreign married women’s rate, crime rate, number of psychiatrists, and social welfare costs, with suicide rates in 15-19-year-old adolescents (53).
Discussion
A classical study by Durkheim found geographical and temporal variations effective in mortality from suicide and community effective in the tendency of individuals to commit suicide. This study found suicide frequency in a population to reflect its geographical and socioeconomic features, and suicide risk factors at a community level not to simply constitute the sum of individual risk factors. The limitations of the studies conducted on individual risk factors were also highlighted in this study in terms of investigating the fundamental causes and preventive measures of suicide (67). The present research aimed at exploring the spatial, geographical and demographic factors related to suicide in adolescents and the youth. Numerous studies on spatial and temporal variations in suicide reported mortality from suicide as a function of geographical location (19, 40). In contrast, Fowler and Caley reported insignificant differences in the frequency and risk of suicide in 1.3 million individuals in England and Wales among different populations and geographical locations. They explained their findings by the scarcity of suicide as an outcome and found collecting data on suicide to rarely lead to discovering local groups and targeted interventions (68).
The present systematic review showed a higher suicide frequency for the age group of 15-29 years old than that for the age group of below 15 years. Similarly, numerous studies suggest the growing suicide frequency at the age of below 29 years than in other age groups (69, 70). Research indicates positive relationships between age and suicide frequency such that 6% of suicides were reported in adolescents aged below fifteen, 34% in those aged 15-19 and 60% in the 20-24 age group (55). These findings are a global alarm to urgently adopt appropriate preventive measures. Research also relates the higher risk of suicide at lower ages to receiving decreased support, poor religious activities, living alone or in single-parent families, alcohol abuse, unemployment and facing new stressful responsibilities such as financially or vocationally supporting oneself or one’s family (69, 71–73).
In line with literature, the present systematic review found increased suicide frequencies in males than those in females of the adolescent and young age group (74, 75), which can be explained by the heavier burden of economic loads carried by men (66). Gender-based social expectations of men, their higher exposure to risk and their lower tendency to seek help during depression or on the verge of suicidal behaviors can be attributed to an emphasis on their commitment to be strong, independent and capable (8, 76). The present review rarely observed a higher suicide frequency in women than that in men; e.g. the higher suicide rate in Iranian women was attributed to their cultural background and means of suicide (63).
The present research observed a higher suicide frequency in the patients with psychological disorders, including depression. Previous studies also reported more suicidal ideation and attempts in adolescents with depression or living in areas with high suicide rates. These adolescents felt a lack of access to medical services in their neighborhood (77, 78). Promoting access to health services thus appears essential for evaluating health and preventing suicide in adolescents (57). Depression might have lowered the tendency to receive psychological services. It is therefore recommended that preventive services be actively provided for patients with depression, especially in high-risk areas.
The present research found negative relationships between education levels and suicide frequency. Low levels of literacy have also been found to relate to suicide rates in literature (79). The lower suicide frequency in educated individuals can be explained by their higher perception of the damage caused by suicide (80).
The present study found the total suicide frequency to be higher in native, racial and ethnic groups. Similarly, a higher suicide frequency was reported in the native Taiwanese (81). Research explains this finding by easy access to pesticides, especially in rural areas (81); nevertheless, the small proportion of minority populations should be included in the analysis of ethnic and racial data. The data should also be cautiously interpreted due to failure to report suicides (65).
The present research observed positive relationships between social isolation and suicide frequency. Similarly, previous studies suggest shrinking peer-to-peer networks and social isolation can increase suicide rates (74). Research also demonstrates higher suicide rates in areas with more single-parent families (81). Studies on differences in suicide rates between rural and urban areas have found environmental factors such as transition from an agricultural economy, decline in population, marital instability and growing rates of living in isolation to increase social fragmentation.
In line with the present study, research suggests positive associations between divorce and suicide rates (75, 79, 82). The risk of suicide was also found to increase in singles and divorced individuals (83). Marriage can exert its protective effects through improving socio-emotional stability and conformity to social norms. The significant and positive relationship observed between divorce and suicide, even in high-income strata, reflects the effects of social welfare on suicide (75, 84). Marriage at young ages can increase suicide frequency in women by increasing their family and social stresses (63). According to Durkheim, divorce rates, number of children, indicators of social integrity, and family ties play a key role in suicide rates. In fact, the higher the divorce rate and the fewer the children, the weaker the social integrity of the family and thus the higher the suicide rate (85).
The present findings showed relationships between suicide and unemployment. A review of the studies mostly conducted in Western countries showed that unemployment is a socioeconomic factor associated with suicide rates (83, 86). Despite the reported negative relationships of the socioeconomic status and unemployment with suicide (75, 86), these relationships have not been confirmed in the youth (57, 87). These findings appear rational given that individuals aged below 18 are not employed or allowed to be employed in most countries. Certain studies also observed no significant relationships between unemployment and suicide rates (79).
According to Durkheim, increased suicide caused by weakened social norms can be associated with rapid economic and demographic changes. Social displacement caused by population and economic expansion and contraction can create an environment for suicide in the absence of social workforce that serves to reduce suicidal tendencies. In line with this argument by Durkheim, the present and previous research suggests social solidarity constitutes a major predictor of cross-sectional and temporal changes in suicide rates (75). Research also suggests positive relationships between socioeconomic deprivation and suicide (75, 86). Furthermore, socioeconomic growth has been found to prevent or reduce suicide (88).
This study observed the positive relationships of deprivation and social disintegration with suicide in the youth and adolescents (89). Some studies have found deprivation more effective than social disintegration in suicide, whereas certain researchers reported social disintegration as the dominant factor (54, 83); nevertheless, these two variables were also found not to affect suicide elsewhere (90).
The present study found a higher suicide rate in adolescents and the youth living in rural areas and on the outskirts than in those living in urban areas; nevertheless some studies reported higher suicide frequencies in urban areas (91, 92). According to previous studies, the risk and frequency of suicide is higher in rural than in urban areas (74, 75, 81, 93) This finding can be explained by higher development, better socioeconomic status and access to psychiatric services in urban areas as compared to villages (55, 94). The limited economic infrastructure and jobs coupled with high unemployment, low education levels and economic deprivation in rural areas can adversely affect mental health. Climatic conditions, social isolation, lack of intimate friends and jobs and more firearms can be associated with higher suicide rates in rural areas (55, 94). Research suggests a spatial inequality in suicide rates between rural and urban residents (91, 92).
According to previous studies, the risk factors of suicide include social isolation, stigma of psychological disorders, easy access to poisonous pesticides, economic problems and concentration of ethnic minority groups (81, 95). In line with the present research, previous studies demonstrated a higher suicide frequency in rural than urban men (94). The higher prevalence of mortality in urban areas can be explained by the extent of deprivation, low socioeconomic status and large ethnic population in the neighborhood where suicide occurs (92, 96).
This study found higher suicide rates in areas with a low population density and coastal and mountainous regions. Similarly, research suggests negative relationships between population density and suicide rates (81). In low-density population areas, individuals at risk may receive inadequate outpatient care and treatment for psychological disorders and drug abuse compared to the services provided in urban areas. The residents of low density population areas also tend to keep and use firearms, and some studies revealed relationships between higher suicide rates and using firearms (65).
The present study observed no regular patterns of suicide; nevertheless, previous studies reported the highest suicide frequency in the spring, early summer and fall (61, 97, 98). Certain researchers have also confirmed the relationship between season and suicide in young age groups (99, 100). It appears that seasonal patterns constitute a popular factor in suicide risk and seasonal variations in mortality from suicide can help identify factors affecting or preventing suicide.
Limitations
Inappropriate age classifications in previous studies prevented a favorable comparison and meta-analysis in some cases. The limitations of primary studies, such as the possibility of inaccurate recording of suicide statistics in some years or underreporting could have also affected the results of this study. Alongside these limitations, however, the present study also has strongpoints including that, to our knowledge, this is the first study on the systematic evaluation of spatial, geographic, and other factors related to suicide in adolescents and the youth; and its findings can serve as a guide for qualitative and quantitative research which may identify potential preventive interventions.
Policy making implications
Developing training courses and implementing suicide prevention strategies in schools with the help of local leaders, influencers and peers; developing suicide prevention strategies in villages and low-density areas; reducing access to firearms in villages; allocating funds to geographical areas with a high prevalence of suicide among the native people; increasing access to mental health services, especially for men, individuals of 15-29 years, people living in rural areas and suburbs; socio-economic development (policies to reduce divorce, increase the level of education, reduce unemployment), and informing psychologists and social workers about spatial and geographic factors related to suicide in teenagers and young adults.
Conclusions
Geographic and demographic variables were found more effective than spatial variables on suicide in the youth and adolescents. Mortality from suicide was higher in men, residents of rural and low population density areas, natives, 15-29 age group, individuals suffering deprivation, social disintegration and unemployment, divorced individuals and singles, single-parent families, patients with psychological disorders and individuals with low education levels. These findings suggest that policy makers take spatial and demographic factors into consideration when health systems allocate resources for suicide prevention, and that national policymakers integrate demographic and geographic variables into health service programs. Finally, future intervention studies should seriously address the role of the variables in this study in reducing the prevalence of suicide in teenagers and young adults.
Data availability statement
All data generated or analyzed during this study are included in this published article, and the datasets used and/or analyzed during the current study available from the corresponding author on reasonable request.
Author contributions
MG: Conceptualization, Writing – review & editing. RT: Conceptualization, Methodology, Writing – review & editing. ZM: Conceptualization, Methodology, Writing – review & editing. SK: Conceptualization, Methodology, Project administration, Writing – original draft. MF: Conceptualization, Writing – review & editing. MM: Data curation, Writing – review & editing. SAM: Conceptualization, Methodology, Writing – review & editing. SSM: Investigation, Supervision, Writing – review & editing. SA: Conceptualization, Writing – review & editing. RK: Investigation, Writing – review & editing. ND: Conceptualization, Methodology, Writing – original draft.
Funding
The author(s) declare that no financial support was received for the research, authorship, and/or publication of this article.
Acknowledgments
The authors would like to express many thanks for Forensic medicine specialist, Legal medicine Research center, Legal medicine organization, Tehran, Iran for giving us the opportunity to carry out this study.
Conflict of interest
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
Publisher’s note
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
References
1. Ortiz-Prado E, Simbaña K, Gómez L, Henriquez-Trujillo AR, Cornejo-Leon F, Vasconez E, et al. The disease burden of suicide in Ecuador, a 15 years’ geodemographic cross-sectional study (2001–2015). BMC Psychiatry (2017) 17(1):1–11. doi: 10.1186/s12888-017-1502-0
2. O’Beaglaoich C, McCutcheon J, Conway PF, Hanafin J, Morrison TG. Adolescent suicide ideation, depression and self-esteem: relationships to a new measure of gender role conflict. Front Psychol (2020) 111. doi: 10.3389/fpsyg.2020.00111
3. Bachmann S. Epidemiology of suicide and the psychiatric perspective. Int J Environ Res Public Health (2018) 15(7):1425. doi: 10.3390/ijerph15071425
4. Värnik P. Suicide in the world. Int J Environ Res Public Health (2012) 9(3):760–71. doi: 10.3390/ijerph9030760
5. Organization WH. Preventing suicide: A global imperative. Geneva: World Health Organization (2014).
6. Qu G, Shu L, Zhang J, Wu Y, Ma S, Han T, et al. Suicide ideation, suicide plan, and suicide attempt among left-behind children and adolescents: A systematic review and meta-analysis. Suicide Life-Threatening Behavior (2021) 51(3):515–27. doi: 10.1111/sltb.12731
7. Shain B, Braverman PK, Adelman WP, Alderman EM, Breuner CC, Levine DA, et al. Suicide and suicide attempts in adolescents. Pediatrics (2016) 138(1). doi: 10.1542/peds.2016-1420
8. Núñez-González S, Lara-Vinueza AG, Gault C, Delgado-Ron JA. Trends and spatial patterns of suicide among adolescent in Ecuador, 1997-2016. Clin Pract Epidemiol Ment Health: CP EMH (2018) 14:283. doi: 10.2174/1745017901814010283
9. McKinnon B, Gariépy G, Sentenac M, Elgar FJ. Adolescent suicidal behaviours in 32 low-and middle-income countries. Bull World Health Organization (2016) 94(5):340. doi: 10.2471/BLT.15.163295
10. Patton GC, Coffey C, Sawyer SM, Viner RM, Haller DM, Bose K, et al. Global patterns of mortality in young people: a systematic analysis of population health data. Lancet (2009) 374(9693):881–92. doi: 10.1016/S0140-6736(09)60741-8
11. Query W-bIS. Reporting system (WISQARS). In: Centers for Disease Control and Prevention, vol. 2019. National Center for Injury Prevention and Control (2019).
12. Kokkevi A, Rotsika V, Arapaki A, Richardson C. Adolescents’ self-reported suicide attempts, self-harm thoughts and their correlates across 17 European countries. J Child Psychol Psychiatry (2012) 53(4):381–9. doi: 10.1111/j.1469-7610.2011.02457.x
13. Moran P, Coffey C, Romaniuk H, Olsson C, Borschmann R, Carlin JB, et al. The natural history of self-harm from adolescence to young adulthood: a population-based cohort study. Lancet (2012) 379(9812):236–43. doi: 10.1016/S0140-6736(11)61141-0
14. Nock MK, Green JG, Hwang I, McLaughlin KA, Sampson NA, Zaslavsky AM, et al. Prevalence, correlates, and treatment of lifetime suicidal behavior among adolescents: results from the National Comorbidity Survey Replication Adolescent Supplement. JAMA Psychiatry (2013) 70(3):300–10. doi: 10.1001/2013.jamapsychiatry.55
15. Gosney H, Hawton K. Inquest verdicts: youth suicides lost. Psychiatr Bulletin (2007) 31(6):203–5. doi: 10.1192/pb.bp.105.007773
16. Harris IM, Beese S, Moore D. Predicting repeated self-harm or suicide in adolescents and young adults using risk assessment scales/tools: a systematic review protocol. Systematic Rev (2019) 8:1–6. doi: 10.1186/s13643-019-1007-7
17. Page A, Liu S, Gunnell D, Astell-Burt T, Feng X, Wang L, et al. Suicide by pesticide poisoning remains a priority for suicide prevention in China: analysis of national mortality trends 2006–2013. J Affect Disord (2017) 208:418–23. doi: 10.1016/j.jad.2016.10.047
18. Barber CW, Miller MJ. Reducing a suicidal person’s access to lethal means of suicide: a research agenda. Am J Prev Med (2014) 47(3):S264–S72. doi: 10.1016/j.amepre.2014.05.028
19. Ngui AN, Apparicio P, Moltchanova E, Vasiliadis H-M. Spatial analysis of suicide mortality in Québec: spatial clustering and area factor correlates. Psychiatry Res (2014) 220(1-2):20–30. doi: 10.1016/j.psychres.2014.07.033
20. Zhang J, Tong HQ, Zhou L. The effect of bereavement due to suicide on survivors' depression: a study of Chinese samples. Omega-Journal Death Dying (2005) 51(3):217–27. doi: 10.2190/496B-Q1WQ-K9TJ-518E
21. Abubakar I, Tillmann T, Banerjee A. Global, regional, and national age-sex specific all-cause and cause-specific mortality for 240 causes of death, 1990-2013: a systematic analysis for the Global Burden of Disease Study 2013. Lancet (2015) 385(9963):117–71. doi: 10.1016/S0140-6736(14)61682-2
22. Murray CJ, Vos T, Lozano R, Naghavi M, Flaxman AD, Michaud C, et al. Disability-adjusted life years (DALYs) for 291 diseases and injuries in 21 regions, 1990–2010: a systematic analysis for the Global Burden of Disease Study 2010. Lancet (2012) 380(9859):2197–223. doi: 10.1016/S0140-6736(12)61689-4
23. O’Farrell IB, Corcoran P, Perry IJ. The area level association between suicide, deprivation, social fragmentation and population density in the Republic of Ireland: a national study. Soc Psychiatry Psychiatr Epidemiol (2016) 51(6):839–47. doi: 10.1007/s00127-016-1205-8
24. Crawford MJ, Kuforiji B, Ghosh P. The impact of social context on socio-demographic risk factors for suicide: a synthesis of data from case–control studies. J Epidemiol Community Health (2010) 64(6):530–4. doi: 10.1136/jech.2008.084145
25. Yoshioka E, Hanley SJ, Sato Y, Saijo Y. Geography of suicide in Japan: spatial patterning and rural–urban differences. Soc Psychiatry Psychiatr Epidemiol (2021) 56:731–46. doi: 10.1007/s00127-020-01978-7
26. Rostami M, Jalilian A, Mahdavi SA, Bagheri N. Spatial heterogeneity in gender and age of fatal suicide in Iran. J Res Health Sci (2022) 22(1):e00541. doi: 10.34172/jrhs.2022.76
27. Johnson C, Hahn C. Spatial clustering of suicide and associated community characteristics, idaho, 2010–2014. In: Population Health, Place, and Space: Spatial Perspectives in Chronic Disease Research and Practice. doi: 10.5888/pcd16.180429
28. Kwon H, Hong HJ, Kweon Y-S. Classification of adolescent suicide based on student suicide reports. J Korean Acad Child Adolesc Psychiatry (2020) 31(4):169. doi: 10.5765/jkacap.200030
29. Cluver L, Orkin M, Boyes ME, Sherr L. Child and adolescent suicide attempts, suicidal behavior, and adverse childhood experiences in South Africa: a prospective study. J Adolesc Health (2015) 57(1):52–9. doi: 10.1016/j.jadohealth.2015.03.001
30. Soto-Sanz V, Castellví P, Piqueras JA, Rodríguez-Marín J, Rodríguez-Jiménez T, Miranda-Mendizábal A, et al. Internalizing and externalizing symptoms and suicidal behaviour in young people: A systematic review and meta-analysis of longitudinal studies. Acta Psychiatrica Scandinavica (2019) 140(1):5–19. doi: 10.1111/acps.13036
31. Forouzesh M, Barzegar A, Mahdavi SA, Ghadipasha M, Mousavi SS, Kordrostami R, et al. The rate of suicide and its reasons in children under the age of 18 years. Int J Med Toxicol Forensic Med (2022) 12(2):35084. doi: 10.32598/ijmtfm.v12i2.35084
32. Ports KA, Merrick MT, Stone DM, Wilkins NJ, Reed J, Ebin J, et al. Adverse childhood experiences and suicide risk: Toward comprehensive prevention. Am J Prev Med (2017) 53(3):400–3. doi: 10.1016/j.amepre.2017.03.015
33. Miranda-Mendizabal A, Castellví P, Parés-Badell O, Alayo I, Almenara J, Alonso I, et al. Gender differences in suicidal behavior in adolescents and young adults: systematic review and meta-analysis of longitudinal studies. Int J Public Health (2019) 64(2):265–83. doi: 10.1007/s00038-018-1196-1
34. Di Giacomo E, Krausz M, Colmegna F, Aspesi F, Clerici M. Estimating the risk of attempted suicide among sexual minority youths: a systematic review and meta-analysis. JAMA pediatrics (2018) 172(12):1145–52. doi: 10.1001/jamapediatrics.2018.2731
35. Epstein S, Roberts E, Sedgwick R, Polling C, Finning K, Ford T, et al. School absenteeism as a risk factor for self-harm and suicidal ideation in children and adolescents: a systematic review and meta-analysis. Eur Child Adolesc Psychiatry (2020) 29(9):1175–94. doi: 10.1007/s00787-019-01327-3
36. Orozco R, Benjet C, Borges G, Moneta Arce MF, Fregoso Ito D, Fleiz C, et al. Association between attempted suicide and academic performance indicators among middle and high school students in Mexico: results from a national survey. Child Adolesc Psychiatry Ment Health (2018) 12(1):1–10. doi: 10.1186/s13034-018-0215-6
37. Balint L, Dome P, Daroczi G, Gonda X, Rihmer Z. Investigation of the marked and long-standing spatial inhomogeneity of the Hungarian suicide rate: A spatial regression approach. J Affect Disord (2014) 155:180–5. doi: 10.1016/j.jad.2013.10.047
38. Wasserman D, Rihmer Z, Rujescu D, Sarchiapone M, Sokolowski M, Titelman D, et al. The European Psychiatric Association (EPA) guidance on suicide treatment and prevention. Eur Psychiatry (2012) 27(2):129–41. doi: 10.1016/j.eurpsy.2011.06.003
39. Gearing RE, Lizardi D. Religion and suicide. J religion Health (2009) 48(3):332–41. doi: 10.1007/s10943-008-9181-2
40. Qi X, Hu W, Page A, Tong S. Spatial clusters of suicide in Australia. BMC Psychiatry (2012) 12(1):1–11. doi: 10.1186/1471-244X-12-86
41. Page MJ, McKenzie JE, Bossuyt PM, Boutron I, Hoffmann TC, Mulrow CD, et al. The PRISMA 2020 statement: an updated guideline for reporting systematic reviews. Systematic Rev (2021) 10(1):1–11. doi: 10.1136/bmj.n71
42. Cuschieri S. The STROBE guidelines. Saudi J anaesthesia (2019) 13(Suppl 1):S31. doi: 10.4103/sja.SJA_543_18
43. Lockwood C, Munn Z, Porritt K. Qualitative research synthesis: methodological guidance for systematic reviewers utilizing meta-aggregation. JBI Evidence Implementation (2015) 13(3):179–87. doi: 10.1097/XEB.0000000000000062
44. Higgins JP, Thomas J, Chandler J, Cumpston M, Li T, Page MJ, et al. Cochrane handbook for systematic reviews of interventions. Cavendish Square, London, W1G 0AN, United Kingdom: John Wiley & Sons (2019).
45. Vandenbroucke JP, Von Elm E, Altman DG, Gøtzsche PC, Mulrow CD, Pocock SJ, et al. Strengthening the reporting of observational studies in epidemiology (STROBE): explanation and elaboration. Gaceta sanitaria (2009) 23(2):158–. doi: 10.1016/j.gaceta.2008.12.001
46. Von Elm E, Altman DG, Egger M, Pocock SJ, Gøtzsche PC, Vandenbroucke JP. The Strengthening the Reporting of Observational Studies in Epidemiology (STROBE) statement: guidelines for reporting observational studies. Bull World Health Organization (2007) 85:867–72. doi: 10.2471/BLT.07.045120
47. Braun V, Clarke V. Using thematic analysis in psychology. Qual Res Psychol (2006) 3(2):77–101. doi: 10.1191/1478088706qp063oa
48. Hajebi A, Ahmadzad-Asl M, Davoudi F, Ghayyomi R. Trend of suicide in Iran during 2009 to 2012: Epidemiological evidences from national suicide registration. Iranian J Psychiatry Behav Sci (2016) 10(4). doi: 10.17795/ijpbs-4398
49. Ivey-Stephenson AZ, Crosby AE, Jack SP, Haileyesus T, Kresnow-Sedacca M-j. Suicide trends among and within urbanization levels by sex, race/ethnicity, age group, and mechanism of death—United States, 2001–2015. MMWR Surveillance Summaries (2017) 66(18):1. doi: 10.15585/mmwr.ss6618a1
50. Salmerón D, Cirera L, Ballesta M, Navarro-Mateu F. Time trends and geographical variations in mortality due to suicide and causes of undetermined intent in Spain, 1991–2008. J Public Health (2013) 35(2):237–45. doi: 10.1093/pubmed/fds103
51. Qi X, Hu W, Page A, Tong S. Dynamic pattern of suicide in Australia, 1986–2005: a descriptive-analytic study. BMJ Open (2014) 4(7):e005311. doi: 10.1136/bmjopen-2014-005311
52. Pompili M, Masocco M, Vichi M, Lester D, Innamorati M, Tatarelli R, et al. Suicide among Italian adolescents: 1970–2002. Eur Child Adolesc Psychiatry (2009) 18(9):525–33. doi: 10.1007/s00787-009-0007-x
53. Song J, Park S, Lee K, Hong HJ. Influence of area-level characteristics on the suicide rate in Korean adolescents. Psychiatry Invest (2019) 16(11):800. doi: 10.30773/pi.2019.0025
54. Middleton N, Sterne JA, Gunnell D. The geography of despair among 15–44-year-old men in England and Wales: putting suicide on the map. J Epidemiol Community Health (2006) 60(12):1040–7. doi: 10.1136/jech.2005.045302
55. Fontanella CA, Hiance-Steelesmith DL, Phillips GS, Bridge JA, Lester N, Sweeney HA, et al. Widening rural-urban disparities in youth suicides, United States, 1996-2010. JAMA pediatrics (2015) 169(5):466–73. doi: 10.1001/jamapediatrics.2014.3561
56. Fong DY, Yip PS. Economic and environmental factorsin Hong Kong suicides. Arch suicide Res (2003) 7(2):123–33. doi: 10.1080/13811110301582
57. Kim G-M, Kim J-M, Kyung Hyun M, Mi Choi S, Woo J-M. Comparison of the risk factors of Korean adolescent suicide residing in high suicidal regions versus those in low suicidal regions. Psychiatria Danubina (2019) 31(4):397–404. doi: 10.24869/psyd.2019.397
58. Beratis S. Suicide among adolescents in Greece. Br J Psychiatry (1991) 159(4):515–9. doi: 10.1192/bjp.159.4.515
59. Berkelmans G, van der Mei R, Bhulai S, Merelle S, Gilissen R. Demographic risk factors for suicide among youths in the Netherlands. Int J Environ Res Public Health (2020) 17(4):1182. doi: 10.3390/ijerph17041182
60. Seiden RH. Death in the West—A regional analysis of the youthful suicide rate. Western J Med (1984) 140(6):969.
61. Hofstra E, Elfeddali I, Bakker M, De Jong JJ, Van Nieuwenhuizen C, van der Feltz-Cornelis CM. Springtime peaks and Christmas troughs: a national longitudinal population-based study into suicide incidence time trends in the Netherlands. Front Psychiatry (2018) 9:45. doi: 10.3389/fpsyt.2018.00045
62. Orellana JD, Balieiro AA, Fonseca FR, Basta PC, Souza ML. Spatial-temporal trends and risk of suicide in Central Brazil: an ecological study contrasting indigenous and non-indigenous populations. Braz J Psychiatry (2016) 38:222–30. doi: 10.1590/1516-4446-2015-1720
63. Taghaddosinejad F, Sheikhazadi A, Behnoush B, Reshadati J, Anary SHS. A survey of suicide by burning in tehran, Iran. Acta Med Iranica (2010) 48(4):266–72.
64. Gessner BD. Temporal trends and geographic patterns of teen suicide in Alaska, 1979–1993. Suicide Life-Threatening Behavior (1997) 27(3):264–73. doi: 10.1111/j.1943-278X.1997.tb00408.x
65. Hempstead K. The geography of self-injury: spatial patterns in attempted and completed suicide. Soc Sci Med (2006) 62(12):3186–96. doi: 10.1016/j.socscimed.2005.11.038
66. Hsu CY, Chang SS, Lee EST, Yip PSF. "Geography of suicide in Hong Kong: Spatial patterning, and socioeconomic correlates and inequalities". Soc Sci Med (2015) 130:190–203. doi: 10.1016/j.socscimed.2015.02.019
67. Durkheim E. Suicide: A study in sociology. Routledge (2005). Available at: https://www.routledge.com/Suicide-A-Study-in-Sociology/Durkheim/p/book/9780415278317.
68. Caley M, Fowler T. Suicide prevention: Is more demographic information the answer? J Public Health (2009) 31(1):95–7. doi: 10.1093/pubmed/fdn101
69. Santos A, Guimarães LML, Carvalho Y, Viana L, Alves GL, Lima ACR, et al. Spatial analysis and temporal trends of suicide mortality in Sergipe, Brazil, 2000-2015. Trends Psychiatry psychother (2018) 40:269–76. doi: 10.1590/2237-6089-2017-0028
70. Brzozowski FS, Soares GB, Benedet J, Boing AF, Peres MA. Suicide time trends in Brazil from 1980 to 2005. Cadernos saúde pública (2010) 26:1293–302. doi: 10.1590/S0102-311X2010000700008
71. Meneghel SN, Victora CG, Faria NMX, Carvalho L, Falk JW. Características epidemiológicas do suicídio no Rio Grande do Sul. Rev Saúde Pública (2004) 38:804–10. doi: 10.1590/S0034-89102004000600008
72. Gunnell D, Middleton N, Whitley E, Dorling D, Frankel S. Why are suicide rates rising in young men but falling in the elderly?—a time-series analysis of trends in England and Wales 1950–1998. Soc Sci Med (2003) 57(4):595–611. doi: 10.1016/S0277-9536(02)00408-2
73. Nazari SSH, Mansori K, Kangavari HN, Shojaei A, Arsang-Jang S. Spatio-temporal distribution of suicide risk in Iran: a Bayesian hierarchical analysis of repeated cross-sectional data. J Prev Med Public Health (2022) 55(2):164. doi: 10.3961/jpmph.21.385
74. Chan CH, Caine ED, You S, Yip PSF. Changes in South Korean urbanicity and suicide rates, 1992 to 2012. BMJ Open (2015) 5(12):e009451. doi: 10.1136/bmjopen-2015-009451
75. Phillips JA. Factors associated with temporal and spatial patterns in suicide rates across US states, 1976–2000. Demography (2013) 50(2):591–614. doi: 10.1007/s13524-012-0176-y
76. Mascayano F, Irrazabal M, Emilia WD, Shah B, Vaner SJ, Sapag JC, et al. Suicide in Latin America: a growing public health issue. Rev Fac Cien Med Univ Nac Cordoba (2015) 72(4):295–303.
77. Koenig J, Oelkers-Ax R, Parzer P, Haffner J, Brunner R, Resch F, et al. The association of self-injurious behaviour and suicide attempts with recurrent idiopathic pain in adolescents: evidence from a population-based study. Child Adolesc Psychiatry Ment Health (2015) 9(1):1–9. doi: 10.1186/s13034-015-0069-0
78. Husky MM, Olfson M, J-p He, MK N, Swanson SA, Merikangas KR. Twelve-month suicidal symptoms and use of services among adolescents: results from the National Comorbidity Survey. Psychiatr services (2012) 63(10):989–96. doi: 10.1176/appi.ps.201200058
79. Haghparast-Bidgoli H, Rinaldi G, Shahnavazi H, Bouraghi H, Kiadaliri AA. Socio-demographic and economics factors associated with suicide mortality in Iran, 2001–2010: application of a decomposition model. Int J equity Health (2018) 17(1):1–7. doi: 10.1186/s12939-018-0794-0
80. Marusic A, Khan M, Farmer A. Can the interaction of poverty and literacy explain some variability of suicide rates in Europe? Eur J Psychiatry (2002) 16(2):103–7.
81. Chang S-S, Sterne JA, Wheeler BW, Lu T-H, Lin J-J, Gunnell D. Geography of suicide in Taiwan: spatial patterning and socioeconomic correlates. Health place (2011) 17(2):641–50. doi: 10.1016/j.healthplace.2011.01.003
82. Nazarzadeh M, Bidel Z, Ayubi E, Asadollahi K, Carson KV, Sayehmiri K. Determination of the social related factors of suicide in Iran: a systematic review and meta-analysis. BMC Public Health (2013) 13(1):1–9. doi: 10.1186/1471-2458-13-4
83. Middleton N, Whitley E, Frankel S, Dorling D, Sterne J, Gunnell D. Suicide risk in small areas in England and Wales, 1991–1993. Soc Psychiatry Psychiatr Epidemiol (2004) 39(1):45–52. doi: 10.1007/s00127-004-0707-y
84. Barth A, Sögner L, Gnambs T, Kundi M, Reiner A, Winker R. Socioeconomic factors and suicide: an analysis of 18 industrialized countries for the years 1983 through 2007. J Occup Environ Med (2011) 53(3):313–7. doi: 10.1097/JOM.0b013e31820d161c
86. Rehkopf DH, Buka SL. The association between suicide and the socio-economic characteristics of geographical areas: a systematic review. psychol Med (2006) 36(2):145–57. doi: 10.1017/S003329170500588X
87. Cheong K-S, Choi M-H, Cho B-M, Yoon T-H, Kim C-H, Kim Y-M, et al. Suicide rate differences by sex, age, and urbanicity, and related regional factors in Korea. J Prev Med Public Health (2012) 45(2):70. doi: 10.3961/jpmph.2012.45.2.70
88. Cai ZY, Chen MN, Ye PP, Yip PSF. Socio-economic determinants of suicide rates in transforming China: A spatial-temporal analysis from 1990 to 2015. Lancet Regional Health-Western Pacific (2022) 19. doi: 10.1016/j.lanwpc.2021.100341
89. Hawton K, Harriss L, Hodder K, Simkin S, Gunnell D. The influence of the economic and social environment on deliberate self-harm and suicide: an ecological and person-based study. psychol Med (2001) 31(5):827–36. doi: 10.1017/S0033291701003993
90. O'Reilly D, Rosato M, Connolly S, Cardwell C. Area factors and suicide: 5-year follow-up of the Northern Ireland population. Br J Psychiatry (2008) 192(2):106–11. doi: 10.1192/bjp.bp.107.040360
91. Pearce J, Barnett R, Jones I. Have urban/rural inequalities in suicide in New Zealand grown during the period 1980–2001? Soc Sci Med (2007) 65(8):1807–19. doi: 10.1016/j.socscimed.2007.05.044
92. Middleton N, Sterne JA, Gunnell DJ. An atlas of suicide mortality: England and Wales, 1988–1994. Health place (2008) 14(3):492–506. doi: 10.1016/j.healthplace.2007.09.007
93. Kim M-H, Jung-Choi K, Jun H-J, Kawachi I. Socioeconomic inequalities in suicidal ideation, parasuicides, and completed suicides in South Korea. Soc Sci Med (2010) 70(8):1254–61. doi: 10.1016/j.socscimed.2010.01.004
94. Middleton N, Gunnell D, Frankel S, Whitley E, Dorling D. Urban-rural differences in suicide trends in young adults: England and Wales, 1981-1998. Soc Sci Med (2003) 57(7):1183–94. doi: 10.1016/S0277-9536(02)00496-3
95. Hirsch JK. A review of the literature on rural suicide: risk and protective factors, incidence, and prevention. Crisis: J Crisis Intervention Suicide Prev (2006) 27(4):189. doi: 10.1027/0227-5910.27.4.189
96. Qin P. Suicide risk in relation to level of urbanicity—a population-based linkage study. Int J Epidemiol (2005) 34(4):846–52. doi: 10.1093/ije/dyi085
97. Pajić V, Orešković S. An exploratory analysis of fifteen years suicide trends using population-level data from Croatian committed suicides registry. Front Public Health (2022) 10. doi: 10.3389/fpubh.2022.857284
98. Beauchamp GA, Ho ML, Yin S. Variation in suicide occurrence by day and during major American holidays. J Emergency Med (2014) 46(6):776–81. doi: 10.1016/j.jemermed.2013.09.023
99. Erazo N, Baumert J, Ladwig K-H. Sex-specific time patterns of suicidal acts on the German railway system. Anal 4003 cases J Affect Disord (2004) 83(1):1–9. doi: 10.1016/j.jad.2004.04.012
Keywords: spatial analysis, geography, suicide, adolescents, youth, systematic review
Citation: Ghadipasha M, Talaie R, Mahmoodi Z, Karimi SE, Forouzesh M, Morsalpour M, Mahdavi SA, Mousavi SS, Ashrafiesfahani S, Kordrostami R and Dadashzadehasl N (2024) Spatial, geographic, and demographic factors associated with adolescent and youth suicide: a systematic review study. Front. Psychiatry 15:1261621. doi: 10.3389/fpsyt.2024.1261621
Received: 19 July 2023; Accepted: 26 January 2024;
Published: 09 February 2024.
Edited by:
Tushar Singh, Banaras Hindu University, IndiaReviewed by:
Pillaveetil Sathyadas Indu, Government Medical College, IndiaMohsen Khosravi, Zahedan University of Medical Sciences, Iran
Rikinkumar S. Patel, Duke University, United States
Copyright © 2024 Ghadipasha, Talaie, Mahmoodi, Karimi, Forouzesh, Morsalpour, Mahdavi, Mousavi, Ashrafiesfahani, Kordrostami and Dadashzadehasl. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Nahid Dadashzadehasl, nah.dadasl@gmail.com
†ORCID: Masoud Ghadipasha, orcid.org/0000-0002-7459-0985
Ramin Talaie, orcid.org/0000-0002-1914-0893
Zohreh Mahmoodi, orcid.org/0000-0002-7868-6941
Salah Eddin Karimi, orcid.org/0000-0002-1542-0214
Mehdi Forouzesh, orcid.org/0000-0001-9773-5473
Masoud Morsalpour, orcid.org/0009-0006-1962-9265
Seyed Amirhosein Mahdavi, orcid.org/0000-0001-6057-0302
Seyed Shahram Mousavi, orcid.org/0009-0000-2141-6740
Shayesteh Ashrafiesfahani, orcid.org/0000-0002-6919-5155
Roya Kordrostami, orcid.org/0000-0002-6654-2078
Nahid Dadashzadehasl, orcid.org/0000-0002-3497-4028
 Masoud Ghadipasha1†
Masoud Ghadipasha1† Zohreh Mahmoodi
Zohreh Mahmoodi Salah Eddin Karimi
Salah Eddin Karimi Nahid Dadashzadehasl
Nahid Dadashzadehasl