- 1Department of Health Promotion, Care and Public Health Research Institute, Maastricht University, Maastricht, Netherlands
- 2Department of Medical Psychology, Amsterdam UMC, University of Amsterdam, Amsterdam, Netherlands
- 3Public Health Research Institute, Quality of Care/Personalized Medicine, Amsterdam, Netherlands
- 4Alzheimer Center Amsterdam, Department of Neurology, Amsterdam University Medical Center (UMC), Amsterdam, Netherlands
- 5Division of Clinical Geriatrics, Center for Alzheimer Research, Department of Neurobiology, Care Sciences and Society, Karolinska Institutet, Stockholm, Sweden
- 6Population Health Unit, Finnish Institute for Health and Welfare, Helsinki, Finland
- 7Alzheimer Europe, Senningerberg, Luxembourg
- 8Department of Applied Informatics, Institute of eHealth, FH Joanneum - University of Applied Sciences, Graz, Austria
- 9Theme Inflammation and Aging, Medical Unit Aging, Karolinska University Hospital, Stockholm, Sweden
- 10Institute of Public Health and Clinical Nutrition, University of Eastern Finland, Kuopio, Finland
- 11The Ageing Epidemiology Research Unit, School of Public Health, Imperial College London, London, United Kingdom
- 12Department of Caring Sciences, Faculty of Health and Occupational Studies, University of Gävle, Gävle, Sweden
Introduction: Social activities are important for health and act as a driver of cognitive reserve during aging. In this perspective paper, we describe challenges and outline future (research) endeavors to establish better operationalization of social activities in multidomain interventions to prevent dementia.
Body: We first address the lack of conceptual clarity, which makes it difficult to measure engagement in social activities. Second, drawing from our experience with the Finnish Geriatric Intervention Study to Prevent Cognitive Impairment and Disability (FINGER), we discuss social activities in multidomain dementia prevention interventions. Using qualitative data from the Multimodal Preventive Trial for Alzheimer’s Disease (MIND-ADmini), we reflect on participant experiences with social activities. Third, we address the potential and challenges of digital solutions in promoting social activities in interventions for dementia prevention. Finally, we share insights from a workshop on digital technology, where we consulted with individuals with and without cognitive impairment who have been involved in three European projects (i.e., EU-FINGERS, Multi-MeMo, and LETHE).
Discussion: Based on these insights, we advocate for research that strengthens and accelerates the integration of social activities into multidomain interventions for dementia prevention. We propose several ways to achieve this: (a) by conducting mixed methods research to formulate a broadly accepted definition and instructions to measure social activities; (b) by focusing on promoting engagement in social activities beyond the intervention setting; and (c) by exploring the needs and preferences of older adults towards digitally-supported interventions and co-design of new technologies that enrich in-person social activities.
Introduction
Discovering ways to prevent dementia or slow down the progression of underlying diseases such as Alzheimer’s disease (AD) has a high priority world-wide. According to the 2020 Lancet Commission, tackling 12 identified modifiable risk factors could potentially prevent around 40 percent of dementia cases globally. Social isolation is one of the risk factors that contributes 3.5% of the overall 39.7% of the population attributable fraction of dementia worldwide (1). Social isolation is characterized by an individual’s lack of meaningful interactions (2), and is related to other risk factors for dementia, such as depression (1). This indicates that social isolation and other risk factors can exacerbate each other, which stresses its importance. During the COVID-19 pandemic, social isolation has become more apparent, especially among older adults. This possibly results in negative cognitive health outcomes (3, 4), since social activities are hypothesized to contribute to cognitive reserve (5) and older adults who are socially active tend to experience less cognitive decline as they age (6–13). Yet, methodological issues, including a lack of robust cognitive assessment, reverse causation, and confounding factors, are suggested as alternative explanations for finding protective effects of social activities against dementia (13). In 2019, the World Health Organization (WHO) concluded that there is currently insufficient evidence to recommend social activity as a strategy to reduce dementia risk (14). More recently, Lenart-Bugla et al. (15) reviewed evidence from systematic reviews and conclude that social support and interactions seem to protect against cognitive decline, but the evidence is inconsistent. Among the challenges is that the etiology of late-life cognitive decline is complex and multifactorial, given the lifelong cumulative exposure to multiple risk and protective factors, which means there is a need to address several risk factors simultaneously (16). Protective factors, including physical, cognitive, and social factors, as well as education received during childhood and early adulthood, play an important role in preserving cognitive health (16). Due to insufficient evidence and the challenge of addressing multiple factors simultaneously, both research and evidence about the cognitive benefits of social activities is limited and scattered (14). Despite the lack of conclusive evidence, both the United Nations’ Decade of Healthy Ageing (2021-2030) (17), and the WHO have recently recognized social health as a priority for the upcoming years (i.e., 2024-2026) (18).
Many lifestyle behaviors, such as exercising or engaging in cognitive activities, can incorporate a social dimension. As a result, it is challenging to distinguish social activities from other activities (1). Additionally, social activities are often indirectly promoted through other activities, like group exercise sessions. In this perspective paper, we argue for a dedicated focus on promoting social activities within multidomain dementia prevention interventions. Therefore, we first address the complexity of defining ‘engagement in social activities’ which contributes to the ambiguity around the operationalization in measurements and interventions. Secondly, we reflect on social activities that are incorporated into existing multidomain interventions that offer a targeted prevention approach for older adults with risk factors for dementia. Drawing on our experience with the Finnish Geriatric Intervention Study to Prevent Cognitive Impairment and Disability (FINGER) (19–22) and the Multimodal Preventive Trial for AD (MIND-ADmini) (23), we explore how social activities are integrated into these interventions and experienced by participants. Thirdly, we explore the potential and challenges of using digital technology in the context of these multidomain interventions, especially for monitoring and promoting social activities. Finally, we share insights from a workshop on digital technology that was organized by Alzheimer Europe and allowed us to consult members of the public, including individuals living with cognitive impairment or dementia. In the discussion, we propose directions for the future to strengthen and accelerate the integration of social activities in research and interventions aimed at dementia prevention.
The concept of engagement in social activities: definition and measurement
Social health includes the capacity to fulfill potential and obligations, maintaining independent despite medical conditions, and engagement in social activities (24). The term ‘social activity’ is however not defined in the Merriam-Webster Dictionary, nevertheless ‘activity’ is stated as a behavior or action while ‘social’ refers to pleasant companionship with friends or associates (25). This indicates that engagement in social activities concerns a behavior performed in the company of others. In literature, many related and overlapping terms are used interchangeably to describe engagement in social activities, such as social participation, social connectedness, social cohesion, social support, social network, social integration, and community involvement (26). Moreover, social isolation – as indicated by a lack of social contact – and loneliness – a sense of feeling alone – are concepts that are closely related to the engagement in social activities. Many of these distinct yet related concepts collectively impact the domain of social health, which can positively contribute to the preservation of cognitive abilities when aging (5). The operationalization of social health in research often overlooks this multidimensionality and is typically focused on the measurement of isolated aspects (27). Compared to social isolation and loneliness, the concept of engagement in social activities is particularly vaguely defined, with few validated questionnaires available for its assessment (28). Conceptual clarity is an inaugural step towards the development and validation of effective measurements (29, 30). Presently, the absence of a clear, broadly accepted definition poses challenges to operationalize an appropriate questionnaire to capture the engagement in social activities (31, 32).
In current research that explores risk factors for dementia, the operationalization of engagement in social activities often relies on questionnaires assessing frequency and duration of activities, such as going out, socializing, volunteering, and participation in clubs and communities (28). The engagement in social activities is complex to measure, as it should ideally mirror the diverse experiences of everyday life (31, 33). Various dimensions seem relevant (31), ranging from small and sporadic encounters with acquaintances (34) to in-depth emotional interactions with close relatives or friends (10). Potentially, measurements should evaluate the physical and subjective context of social engagements, rather than relying solely on frequency and duration (35). For instance, by assessing what activities are involved, who participates, where they take place, when they occur, and whether and why they are meaningful (33). Additionally, evaluations of expectations, perceived value, and satisfaction derived from activities would provide useful insights.
Across studies there is a considerable variety in which social activities are assessed (28). Additionally, engagement in social activities is frequently evaluated alongside the engagement in cognitive activities, such as reading, gaming, puzzling (36, 37). Typically, item scores are merged into a single composite score (38, 39), which overlooks the separate and distinct influence of social activities. Additionally, a high level of heterogeneity is observed across studies in terms of the thematic content of items, response scales utilized, and the recall periods specified (28). These inconsistencies make it difficult to compare findings across studies, which results in fragmented evidence about the protective effects of social activities on dementia risk. Comprehensive, validated measurements are urgently needed to align methods across trials and other research. This allows harmonization of data, which is needed to obtain a deeper understanding in the effects of social activities against dementia (14). This knowledge could result in more nuanced risk profiles, which help to tailor the content of future multidomain interventions to the individual.
Social activities in FINGER-model interventions for dementia prevention
Randomized controlled trials (RCTs) have provided promising evidence for the beneficial effects of multidomain interventions in older adults, to reduce the risk of cognitive decline (40). The FINGER-model interventions represent a form of targeted prevention directed at individuals on the at-risk continuum for dementia. This includes individuals with risk factors but without symptoms or brain damage, as well as those who are asymptomatic or early-symptomatic and have brain pathology (41). Regarding social activities, these multidomain interventions often include both individual and group activities (42), for instance group exercising and cognitive training (43). In the FINGER trial, the 2-year multidomain intervention included nutritional guidance, exercising, cognitive training, social activities, and management of metabolic and vascular risks, whereas a control group received general health advice. After two years, the multidomain intervention showed beneficial effects on cognition and quality of life as well as reduced risks of functional decline, cardiovascular accidents, and multimorbidity (22). In the FINGER trial, engagement in social activities between study participants was stimulated through group sessions regarding nutritional guidance, exercising, and psychoeducation about cognition and memory (23). Approximately 30% of the intervention participants self-reported an increase in cognitive and social activities. These participants exhibited slightly more improvement in their cognitive functioning (21). Moreover, 80% of the participants enjoyed meeting others involved in the intervention (44). This enjoyment may enhance intervention adherence, which is pivotal for the success of establishing lifestyle change.
The positive findings of the FINGER trial led to the World-Wide FINGERS (WW-FINGERS) global network of multidomain intervention trials for dementia risk reduction (45). Through this network over 60 countries are testing locally adapted versions in different cultural settings to evaluate feasibility and efficacy. These multidomain interventions target the whole spectrum of dementia risk, including persons with risk factors who are cognitively healthy, have mild cognitive impairment, or prodromal AD. One example is the MIND-ADmini RCT, that tested the feasibility of a FINGER-based multidomain intervention, alone or with medical food, in individuals with prodromal AD (23). Participants clearly perceived benefits from the social activities, including forming friendships, laughing about jokes, sharing personal stories, discussing experiences related to their diagnoses and daily life. These activities fostered a sense of mutual understanding, which was experienced as important by participants with cognitive symptoms.
“We are a good group of friends, or have become, I think, in every way. We have fun and laugh, and we each do our best in every possible way.”
“I also feel the companionship with those in the group, that have the same illness or whatever it is called. We talk openly about it, compare a bit with each other, and can laugh about it and get serious about it, and yes, it’s great that we’re a group with exactly the same thing.”
Participants experienced social support through collaborative activities. This was evident in actions such as offering encouraging cheers, waiting for each other after group sessions, and adapting the intensity of exercises to the group’s needs. The group setting also allowed to socialize during sessions, which participants perceived as a benefit compared to exercising alone as it created a sense of belonging. These meaningful, interpersonal dynamics were perceived as crucial for adherence and continuation of intervention participation.
“Yes, but if there’s something we do, it’s one thing at a time. I do or you do, we say, and the rest of us stand there watching and say, ‘Come on now, come on now, one more time,’ or something like that. That’s how it often goes.”
“We are a group, we know a lot about each other, we have coffee afterward, we support each other.”
Digital technologies to promote social activities in dementia prevention interventions
Digital technologies and tools, including wearables, sensors, and mobile phones, can improve the effectiveness and quality of healthcare, also in the domain of AD and dementia (46), for example by detecting and monitoring change in cognitive functioning. This could support timely identification of individuals in at-risk or in early-disease stages and improve the delivery of preventive interventions (47). For instance, digitally-supported interventions can be personalized and offer the flexibility to participate at convenient times and places, thereby making these interventions more accessible, even for participants in geographically isolated areas. Digital interventions also have the potential to be scalable, widely accessible, and relatively low in costs (48). This is particularly relevant given that the ageing population leads to an increase in healthcare demand and simultaneously results in a shrinking (healthcare) workforce (49, 50). The implementation of digital technologies offers opportunities to improve the delivery of preventive interventions. Digital tools can alleviate the workload on healthcare professionals, allowing them to dedicate more personal support to individuals who struggle with technology (51). It is crucial that technology does not seek to replace personal interactions, and that careful consideration is given to digital inequality to ensure that preventive interventions are accessible to those who need them most (1).
Early dementia lifestyle-based preventive interventions predominantly relied on trained professionals to deliver the intervention, and social interaction was stimulated by bringing participants together (40). The recent generation of trials often adopt a fully-digital or digitally-supported design, such as studies on the Healthy Aging Through Internet Counselling in the Elderly (HATICE) (52, 53), Maintain Your Brain (54), MyCoach (55), or APPLE Tree (56). Although digital interventions enable participants to access the intervention from their own home, which could stimulate adoption and adherence, it seems counter intuitive when stimulating social activities. Still, there are behavioral change methods that transfer well to the digital context, which may be useful to stimulate social activity, including psychoeducation, modelling, and social support (57–59). For instance, in APPLE Tree online video-call ‘tea breaks’ are organized to enhance social support (56). The weak tie network theory posits that such digital interactions, which involves weaker social interactions, can be beneficial for socially stigmatized conditions like dementia (60).
The two-year multinational LETHE RCT, which is a novel study within WW-FINGERS, is an example of a digitally-supported multidomain intervention for dementia risk reduction (61, 62). In LETHE, digital tools are used to complement the in-person activities to streamline the intervention delivery, personalize recommendations, and collect digital biomarkers through a smartwatch and smartphone application. In LETHE, the feasibility of using digital tools to measure social activity is explored, since these tools allow for unobtrusive monitoring of lifestyle behavior patterns, such as step counting and sleep tracking. This approach not only helps to personalize the intervention but also generates a context-rich longitudinal dataset. While tracking certain behaviors with technology is relatively straightforward, monitoring social activities is challenging. Although digital biomarkers exist for social activity, it is uncertain how accurately they reflect social interaction. These include the time spent outdoors, number of social contacts, calendar entries, social network size, social media usage, and exchanged text messages (46). Additionally, it is crucial to acknowledge that the use of these digital biomarkers raise privacy concerns, necessitating careful reflection of whether the data collected justifies the methods used.
A workshop on digital technologies to promote social activities
The use of digital technology in multidomain interventions for dementia prevention seems promising, but the success critically depends on the alignment of technology with the needs and preferences of the people who need to use them (63). Therefore, in the multinational EU-FINGERS, Multi-MeMo, and LETHE projects, public involvement is achieved by including members of the public (i.e., with and without cognitive impairment) through project Advisory Boards (64–66). These three Advisory Boards include 10 males and 10 females from Finland (n = 4), Sweden (n = 4), Luxembourg (n = 1), United Kingdom (n = 2), Netherlands (n = 2), Spain (n = 1), Hungary (n = 2), Austria (n = 2), Italy (n = 2). The boards include individuals at risk (n = 7), with cognitive complaints (n = 9), with dementia (n = 2), and caregivers (n = 2). Their ages range from 45 to 70 years, with most in their 60s.
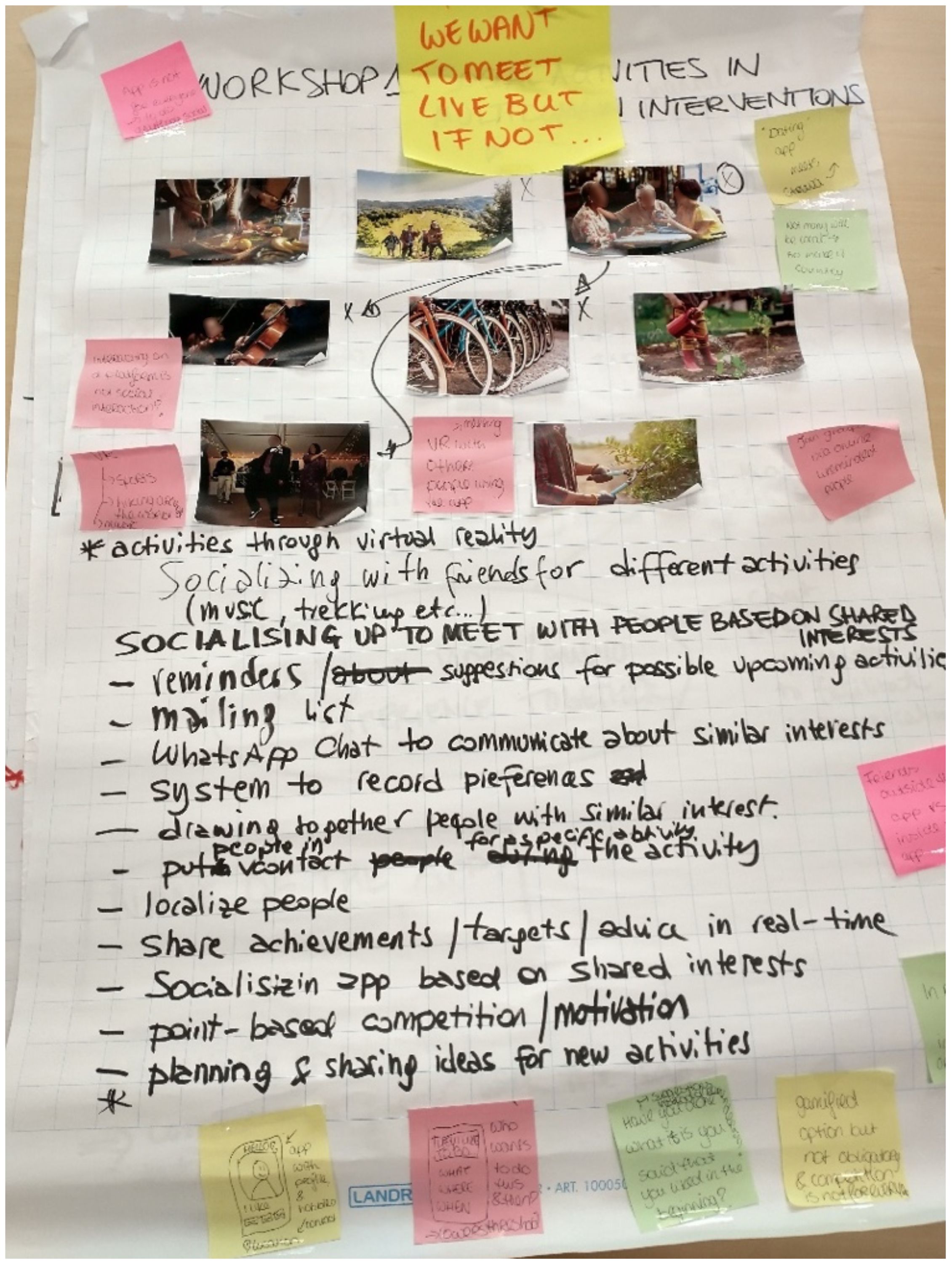
In November 2023, Alzheimer Europe hosted a face-to-face workshop attended by 17 members of these Advisory Boards, where they brainstormed in four smaller subgroups about the use of digital tools to stimulate social activities (see Figure 1 for a snippet of the output). Based on their written input and our fieldnotes, we synthesized four take away messages relevant for the future development of technology-supported multidomain dementia prevention interventions and social activities. First, according to members of the Advisory Boards social activities do not occur in isolation. They highlighted that most social activities intersect with other lifestyle domains and should be stimulated simultaneously. For example, through group exercising, playing board games, or cooking. Second, they strongly preferred meeting in person and mentioned that digital technology could help to connect with others who have similar interests. They envisioned digital technology could link participants who share hobbies, to organize and plan activities together, to inform others about community-based activities, or to share lifestyle progress with others. Third, members from the Advisory Boards recommended to rely on already existing and relatively simple digital tools, such as (private) WhatsApp groups, Facebook pages, or other social media and message-based services. They also brainstormed about more advanced applications such as a dating app to meet participants with shared interests and hobbies, as well as social interaction established by means of virtual reality. Lastly, they raised their concerns regarding safety, privacy, and trustworthiness. For instance, by stressing the importance of preventing that participants share too much personal details and to ensure that others cannot take advantage of the information shared.
Discussion
The connection between engagement in social activities and cognitive health is promising for preventive endeavors (67–69). Currently, social activities in our, and many other, multidomain dementia prevention studies are mainly stimulated through group sessions (22, 70). However, there is room for improvement, by promoting engagement in social activities that occur beyond the intervention setting, and adopting appropriate behavior change strategies and digital tools. To accommodate this, we present directions for the future.
a) The considerable heterogeneity in measuring engagement in social activities poses challenges for cross-study comparison and results in fragmented insights into protective effects of these activities against dementia (28). Although diversity in assessment can be beneficial for epistemic diversity and scientific progress (30), the current practice of measuring engagement in social activities lacks clear and standardized criteria. The heterogeneity in measurements, and particularly the limited transparency about it, undermines the validity of findings and the quality of research in this area (28, 71). Partly, this seems is attributed to the lack of conceptual clarity, which leaves too much freedom for the measurement of social activities (29). This can be addressed by explicitly defining concepts and formulating assessment instructions aligned with these definitions (30). Research is underway to develop a broadly accepted definition and appropriate measurement instructions to assess engagement in social activities (28, 72). This research is guided by frameworks for developing conceptual definitions (29, 73) and includes mixed methods research to triangulate literature through an integrative review, expert opinion using think-aloud sessions, and the perspectives of older adults through conducting interviews.
b) Multidomain preventive interventions should prioritize stimulating engagement in community-based activities and everyday interpersonal interactions. Our qualitative findings reveal that the inclusion of social activities support the forming new, meaningful groups that provide social opportunities that provide social support. Beyond creating these new “within-trial” social connections through group sessions, it seems promising to also encourage social involvement in local clubs, communities, and strengthening ties with relatives and friends (10, 40). This requires a well-thought, systematically planned, and theoretically-sound intervention approach including behavior change methods targeting relevant determinants to promote engagement in social activities (74, 75). For instance, through verbal persuasion about the benefits, role modelling, guided practice or by mobilizing social support (76). To select appropriate behavior change methods, more research is needed to obtain a deeper understanding of the psychological determinants that drive engagement in social activities. The use of behavior change theories, such as the Social Cognitive Theory (77), may provide useful insights into how personal and environmental factors influence the adherence to preventive interventions. This would guide the embodiment of behavior change methods to support long lasting engagement in a wide range of social activities that extend beyond the trial duration. The large network of WW-FINGERS provides a unique opportunity to further explore the incorporation of new interventions to promote social activities. For instance, the 2-year multidomain AGELESS trial in Malaysia already experiments with recreational activities offered by local community centers (78).
c) Digital technologies present innovative opportunities for monitoring and stimulating social activities in multidomain interventions for dementia prevention (46). WW-FINGERS RCTs, like LETHE (61), incorporate qualitative interviews to explore and evaluate the needs and preferences of older adults towards digitally-supported multidomain interventions. Other WW-FINGERS RCTs have also used digital technology (55, 79), which allows to further explore the benefits in terms of intervention delivery, monitoring adherence, and efficacy. The effectiveness of digital technology depends on the alignment with older adults’ needs and preferences to ensure usability, feasibility, and acceptability. Therefore, co-design should be employed to carefully develop new technologies that aim to enrich in-person social activities for older adults, rather than replacing real-world interactions. If researchers work in partnership with older adults, it empowers both parties (80) to ensure that the technological solutions created are based on needs and preferences (81).
In conclusion, social health and engagement in social activities should be further incorporated within multidomain interventions for preventing cognitive decline and dementia. Stimulating social activities could benefit cognitive health directly and also increase adherence to interventions to generate long-lasting effects. In this perspective paper, we identified key challenges and proposed directions for future research including: (a) conducting mixed methods research to formulate a broadly accepted definition and instructions to measure social activities; (b) focusing on the promotion of engagement in social activities that occur outside the intervention setting; and (c) by exploring the needs and preferences of older adults towards digitally-supported interventions using co-design to develop new technologies that enrich in-person social activities. These research endeavors could contribute to, and accelerate, the improved integration of social activities in multidomain dementia prevention interventions.
Data availability statement
The raw data supporting the conclusions of this article will be made available by the authors, without undue reservation.
Ethics statement
The studies involving humans were approved by Regional Ethical Review Board (Regionala Etikprövningsnämnden) in Stockholm, Sweden (Registration number: 2016/2605-31/1). The studies were conducted in accordance with the local legislation and institutional requirements. The participants provided their written informed consent to participate in this study.
Author contributions
JB: Conceptualization, Data curation, Formal analysis, Funding acquisition, Investigation, Methodology, Project administration, Resources, Software, Supervision, Validation, Visualization, Writing – original draft, Writing – review & editing. LV: Conceptualization, Data curation, Formal analysis, Funding acquisition, Investigation, Methodology, Project administration, Resources, Software, Supervision, Validation, Visualization, Writing – original draft, Writing – review & editing. AA: Formal analysis, Investigation, Writing – original draft, Writing – review & editing, Conceptualization. AR: Writing – original draft, Writing – review & editing. AD: Writing – original draft, Writing – review & editing. SH: Writing – original draft, Writing – review & editing. RC: Conceptualization, Writing – original draft, Writing – review & editing. FM: Writing – original draft, Writing – review & editing. MK: Conceptualization, Writing – original draft, Writing – review & editing. CT: Conceptualization, Data curation, Formal analysis, Funding acquisition, Investigation, Methodology, Project administration, Resources, Software, Supervision, Validation, Visualization, Writing – original draft, Writing – review & editing.
Funding
The author(s) declare financial support was received for the research, authorship, and/or publication of this article. This work is supported by various funding sources, including through the LETHE project that is supported by the European Union’s Horizon 2020 research and innovation program (grant number 101017405), and by Joint Program of Neurodegenerative Disorders -JPND (MIND-AD, EU-FINGERS and Multi-MeMo projects). AE received funding for the EU-FINGERS and Multi-MeMo Advisory Boards from the Luxembourg National Research Fund (FNR) under the aegis of the EU Joint Programme – Neurodegenerative Disease Research (JPND). Furthermore, JB received funding from the Netherlands Organization for Health Research and Development (grant number 105110022310004) and LV is supported by an InterAct grant from Alzheimer Nederland (grant number WE.08-2022-10). Additionally, CT, FM, and MK are supported by a FORTE grant (grant number 2023-01125), and CT and MK are funded by the Region Stockholm through an ALF grant. MK is also funded by region Stockholm NSV, Stockholms Sjukhem and the Jubilee Program, Stockholms Sjukhem. Additionally, MK, CT, and FM are supported by Alzheimerfonden, Center for Innovative Medicine (CIMED) at Karolinska Institutet South Campus and Hjärnfonden. CT is funded by Demensfonden.
Acknowledgments
We would like express appreciation to the participants of the MIND-ADmini study for their valuable contribution to our research. Additionally, we would like to acknowledge the support of members of the public who take part in the Advisory Boards of the EU-FINGERS, Multi-MeMo, and LETHE projects. Their involvement has been crucial in guiding our research efforts and enhancing the relevance of our work.
Conflict of interest
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
Publisher’s note
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
References
1. Livingston G, Huntley J, Sommerlad A, Ames D, Ballard C, Banerjee S, et al. Dementia prevention, intervention, and care: 2020 report of the Lancet Commission. Lancet. (2020) 396:413–46. doi: 10.1016/S0140-6736(20)30367-6
2. Rosenau C, Köhler S, Soons LM, Anstey KJ, Brayne C, Brodaty H, et al. Umbrella review and Delphi study on modifiable factors for dementia risk reduction. Alzheimers Dement. (2024) 20:2223–39. doi: 10.1002/alz.13577
3. Lehtisalo J, Palmer K, Mangialasche F, Solomon A, Kivipelto M, Ngandu T. Changes in lifestyle, behaviors, and risk factors for cognitive impairment in older persons during the first wave of the coronavirus disease 2019 pandemic in Finland: results from the FINGER study. Front Psychiatry. (2021) 12:624125. doi: 10.3389/fpsyt.2021.624125
4. Waterink L, Bakker ED, Visser LN, Mangialasche F, Kivipelto M, Deckers K, et al. Changes in brain-health related modifiable risk factors in older adults after one year of COVID-19-restrictions. Front Psychiatry. (2022) 13:877460. doi: 10.3389/fpsyt.2022.877460
5. Vernooij-Dassen M, Verspoor E, Samtani S, Sachdev PS, Ikram MA, Vernooij MW, et al. Recognition of social health: A conceptual framework in the context of dementia research. Front Psychiatry. (2022) 13:1052009. doi: 10.3389/fpsyt.2022.1052009
6. Kendig H, McDonald P, Piggott J. Population ageing and Australia's future. Australia: ANU Press (2016). doi: 10.22459/PAAF.11.2016
7. Sachdev PS. Social health, social reserve and dementia. Curr Opin Psychiatry. (2022) 35:111–7. doi: 10.1097/YCO.0000000000000779
8. Paiva AF, Cunha C, Voss G, Matos AD. The interrelationship between social connectedness and social engagement and its relation with cognition: a study using SHARE data. Ageing Soc. (2021) 43:1735–53. doi: 10.1017/S0144686X2100129X
9. Douglas H, Georgiou A, Westbrook J. Social participation as an indicator of successful aging: an overview of concepts and their associations with health. Aust Health Rev. (2017) 41:455–62. doi: 10.1071/AH16038
10. Kelly ME, Duff H, Kelly S, McHugh Power JE, Brennan S, Lawlor BA, et al. The impact of social activities, social networks, social support and social relationships on the cognitive functioning of healthy older adults: a systematic review. Syst Rev. (2017) 6:259. doi: 10.1186/s13643-017-0632-2
11. Bourassa KJ, Memel M, Woolverton C, Sbarra DA. Social participation predicts cognitive functioning in aging adults over time: comparisons with physical health, depression, and physical activity. Aging Ment Health. (2017) 21:133–46. doi: 10.1080/13607863.2015.1081152
12. Duffner LA, DeJong N, Jansen JF, Backes W, de Vugt M, Deckers K, et al. Associations between social health factors, cognitive activity and neurostructural markers for brain health–A systematic literature review and meta-analysis. Ageing Res Rev. (2023) 89:1–18. doi: 10.1016/j.arr.2023.101986
13. James BD, Wilson RS, Barnes LL, Bennett DA. Late-life social activity and cognitive decline in old age. J Int Neuropsychol Soc. (2011) 17:998–1005. doi: 10.1017/S1355617711000531
14. World Health Organization. Risk reduction of cognitive decline and dementia: WHO guidelines. Geneva: WHO (2019).
15. Lenart-Bugla M, Łuc M, Pawłowski M, Szcześniak D, Seifert I, Wiegelmann H, et al. What do we know about social and non-social factors influencing the pathway from cognitive health to dementia? A systematic review of reviews. Brain Sci. (2022) 12:1–20. doi: 10.3390/brainsci12091214
16. Kivipelto M, Mangialasche F, Ngandu T. Lifestyle interventions to prevent cognitive impairment, dementia and Alzheimer disease. Nat Rev Neurol. (2018) 14:653–66. doi: 10.1038/s41582-018-0070-3
17. United Nations. The united nations decade of healthy ageing (2021-2030) (2021). Available at: https://www.un.org/en/UN-system/ageing.
18. World Health Organisation. WHO commission on social connection (2023). Available at: https://www.who.int/groups/commission-on-social-connection.
19. Lehtisalo J, Rusanen M, Solomon A, Antikainen R, Laatikainen T, Peltonen M, et al. Effect of a multi-domain lifestyle intervention on cardiovascular risk in older people: the FINGER trial. Eur Heart J. (2022) 43:2054–61. doi: 10.1093/eurheartj/ehab922
20. Neuvonen E, Lehtisalo J, Solomon A, Antikainen R, Havulinna S, Hänninen T, et al. Psychosocial determinants for adherence to a healthy lifestyle and intervention participation in the FINGER trial: an exploratory analysis of a randomised clinical trial. Aging Clin Exp Res. (2022) 34:1793–805. doi: 10.1007/s40520-022-02088-x
21. Ngandu T, Lehtisalo J, Korkki S, Solomon A, Coley N, Antikainen R, et al. The effect of adherence on cognition in a multidomain lifestyle intervention (FINGER). Alzheimers Dement. (2022) 18:1325–34. doi: 10.1002/alz.12492
22. Ngandu T, Lehtisalo J, Solomon A, Levälahti E, Ahtiluoto S, Antikainen R, et al. A 2 year multidomain intervention of diet, exercise, cognitive training, and vascular risk monitoring versus control to prevent cognitive decline in at-risk elderly people (FINGER): a randomised controlled trial. Lancet. (9984) 2015:2255–63:385. doi: 10.1016/S0140-6736(15)60461-5
23. Sindi S, Thunborg C, Rosenberg A, Andersen P, Andrieu S, Broersen LM, et al. Multimodal preventive trial for Alzheimer’s disease: MIND-ADmini pilot trial study design and progress. J Prev Alzheimers Dis. (2022) 9:30–9. doi: 10.14283/jpad.2022.4
24. Huber M, Knottnerus JA, Green L, Van Der Horst H, Jadad AR, Kromhout D, et al. How should we define health? BMJ. (2011) 343:d4163. doi: 10.1136/bmj.d4163
25. Merriam-webster.com dictionary, in merriam-webster. Springfield: Encyclopaedia Britannica company (2024).
26. Macinko J, Starfield B. The utility of social capital in research on health determinants. Milbank Q. (2001) 79:387–427. doi: 10.1111/1468-0009.00213
27. Wiegelmann H, Lenart-Bugla M, Vernooij-Dassen M, Verspoor E, Seifert I, Szcześniak D, et al. (conference proceeding) How to measure social health in the context of cognitive decline and dementia-A systematic review on instruments. Int Psychogeriatrics. (2023) 35:15–6. doi: 10.1017/S1041610223001722
28. Bruinsma J, Roodbeen R, Menting GGA, Deckers K, Hendriks S, Crutzen R. A scoping review on operationalizing cognitive and social activities in research on dementia risk reduction. [Preprint]. (2024). doi: 10.31234/osf.io/q3u9a
29. Podsakoff PM, MacKenzie SB, Podsakoff NP. Recommendations for creating better concept definitions in the organizational, behavioral, and social sciences. Organ Res Methods. (2016) 19:159–203. doi: 10.1177/1094428115624965
30. Peters G-JY, Crutzen R. Knowing what we’re talking about: facilitating decentralized, unequivocal publication of and reference to psychological construct definitions and instructions. Meta-Psychology. (2024) 8:1–27. doi: 10.15626/MP.2024
31. Levasseur M, Richard L, Gauvin L, Raymond É. Inventory and analysis of definitions of social participation found in the aging literature: proposed taxonomy of social activities. Soc Sci Med. (2010) 71:2141–9. doi: 10.1016/j.socscimed.2010.09.041
32. Dehi Aroogh M, Mohammadi F, Shahboulaghi F. Social participation of older adults: A concept analysis. Int J Community Based Nurs Midwifery. (2020) 8:55–72. doi: 10.30476/IJCBNM.2019.82222.1055
33. Levasseur M, Lussier-Therrien M, Biron ML, Raymond É, Castonguay J, Naud D, et al. Scoping study of definitions of social participation: update and co-construction of an interdisciplinary consensual definition. Age Ageing. (2022) 51:1–13. doi: 10.1093/ageing/afab215
34. Moreton J, Kelly CS, Sandstrom G,M. Social support from weak ties: Insight from the literature on minimal social interactions. Soc Pers Psychol Compass. (2023) 17:1–12. doi: 10.1111/spc3.12729
35. Maier H, Klumb PL. Social participation and survival at older ages: is the effect driven by activity content or context? Eur J Ageing. (2005) 2:31–9. doi: 10.1007/s10433-005-0018-5
36. Cheng F, Ju Y, Chen X, Jia H. The regulatory roles of socio-economic status, social and intellectual activity in the relationship between alcohol consumption and cognitive decline trajectory in middle-aged and elderly Chinese: A prospective cohort study. Int J Geriatr Psychiatry. (2023) 38:e5877. doi: 10.1002/gps.5877
37. Zhang N, Chen F, Wang C, Yan P. Incidence of cognitive impairment after hypothetical interventions on depression, nighttime sleep duration, and leisure activity engagement among older Chinese adults: An application of the parametric g-formula. Front Public Health. (2023) 11:1088833. doi: 10.3389/fpubh.2023.1088833
38. Casaletto KB, Rentería MA, Pa J, Tom SE, Harrati A, Armstrong NM, et al. Late-life physical and cognitive activities independently contribute to brain and cognitive resilience. J Alzheimers Dis. (2020) 74:363–76. doi: 10.3233/JAD-191114
39. Lim S, Yoo E, Hong I, Park JH. Age-specific findings on lifestyle and trajectories of cognitive function from the Korean Longitudinal Study of Aging. Epidemiol Health. (2023) 45:e2023098. doi: 10.4178/epih.e2023098
40. Solomon A, Stephen R, Altomare D, Carrera E, Frisoni GB, Kulmala J, et al. Multidomain interventions: state-of-the-art and future directions for protocols to implement precision dementia risk reduction. A user manual for Brain Health Services-part 4 of 6. Alzheimers Res Ther. (2021) 13:171. doi: 10.1186/s13195-021-00875-8
41. Mangialasche F, Ngandu T, Kivipelto M. Cognitive impairment – risk factors and prevention. In: Oxford textbook of geriatric medicine, 3. Oxford: Oxford University Press (2017).
42. Zhou Z, Wang P, Fang Y. Social engagement and its change are associated with dementia risk among chinese older adults: A longitudinal study. Sci Rep. (2018) 8:1551. doi: 10.1038/s41598-017-17879-w
43. Hikichi H, Kondo K, Takeda T, Kawachi I. Social interaction and cognitive decline: Results of a 7-year community intervention. Alzheimers Dement. (2017) 3:23–32. doi: 10.1016/j.trci.2016.11.003
44. Kulmala J, Ngandu T, Kivipelto M. Prevention matters: time for global action and effective implementation. J Alzheimers Dis. (2018) 64:S191–8. doi: 10.3233/JAD-179919
45. Kivipelto M, Mangialasche F, Snyder HM, Allegri R, Andrieu S, Arai H, et al. World-Wide FINGERS Network: A global approach to risk reduction and prevention of dementia. Alzheimers Dement. (2020) 16:1078–94. doi: 10.1002/alz.12123
46. Kourtis LC, Regele OB, Wright JM, Jones GB. Digital biomarkers for Alzheimer's disease: the mobile/ wearable devices opportunity. NPJ Digit Med. (2019) 2:1–9. doi: 10.1038/s41746-019-0084-2
47. Gold M, Amatniek J, Carrillo MC, Cedarbaum JM, Hendrix JA, Miller BB, et al. Digital technologies as biomarkers, clinical outcomes assessment, and recruitment tools in Alzheimer's disease clinical trials. Alzheimer's Dementia: Trans Res Clin Interventions. (2018) 4:234–42. doi: 10.1016/j.trci.2018.04.003
48. Gentili A, Failla G, Melnyk A, Puleo V, Tanna GLD, Ricciardi W, et al. The cost-effectiveness of digital health interventions: A systematic review of the literature. Front Public Health. (2022) 10:787135. doi: 10.3389/fpubh.2022.787135
49. 2021 Alzheimer's disease facts and figures. Alzheimers Dement. (2021) 17:327–406. doi: 10.1002/alz.12328
50. Beard JR, Bloom DE. Towards a comprehensive public health response to population ageing. Lancet. (9968) 2015:658–61:385. doi: 10.1016/S0140-6736(14)61461-6
51. Kaye J, Aisen P, Amariglio R, Au R, Ballard C, Carrillo M, et al. Using digital tools to advance Alzheimer’s drug trials during a pandemic: the EU/US CTAD task force. J Prev Alzheimers Dis. (2021) 8:513–9. doi: 10.14283/jpad.2021.36
52. Barbera M, Mangialasche F, Jongstra S, Guillemon J, Ngandu T, Beishuizen C, et al. Designing an internet-based multidomain intervention for the prevention of cardiovascular disease and cognitive impairment in older adults: the HATICE trial. J Alzheimers Dis. (2018) 62:649–63. doi: 10.3233/JAD-170858
53. Richard E, van Charante EPM, Hoevenaar-Blom MP, Coley N, Barbera M, Van Der Groep A, et al. Healthy ageing through internet counselling in the elderly (HATICE): a multinational, randomised controlled trial. Lancet Digit Health. (2019) 1:e424–34. doi: 10.1016/S2589-7500(19)30153-0
54. Heffernan M, Andrews G, Fiatarone Singh MA, Valenzuela M, Anstey KJ, Maeder AJ, et al. Maintain your brain: protocol of a 3-year randomized controlled trial of a personalized multi-modal digital health intervention to prevent cognitive decline among community dwelling 55 to 77 year olds. J Alzheimers Dis. (2019) 70:S221–37. doi: 10.3233/JAD-180572
55. Amos JG, Zheng L, Eramudugolla R, Parekh D, Huque MH, Delbaere K, et al. MyCOACH (COnnected Advice for Cognitive Health): a digitally delivered multidomain intervention for cognitive decline and risk of dementia in adults with mild cognitive impairment or subjective cognitive decline-study protocol for a randomised controlled trial. BMJ Open. (2023) 13:e075015. doi: 10.1136/bmjopen-2023-075015
56. Poppe M, Duffy L, Marchant NL, Barber JA, Hunter R, Bass N, et al. The APPLE Tree programme: Active Prevention in People at risk of dementia through Lifestyle, bEhaviour change and Technology to build REsiliEnce—randomised controlled trial. Trials. (2022) 23:596. doi: 10.1186/s13063-022-06557-6
57. Rigabert A, Motrico E, Moreno-Peral P, Resurrección DM, Conejo-Cerón S, Cuijpers P, et al. Effectiveness of online psychological and psychoeducational interventions to prevent depression: Systematic review and meta-analysis of randomized controlled trials. Clin Psychol Rev. (2020) 82:101931. doi: 10.1016/j.cpr.2020.101931
58. Mair JL, Salamanca-Sanabria A, Augsburger M, Frese BF, Abend S, Jakob R, et al. Effective behavior change techniques in digital health interventions for the prevention or management of noncommunicable diseases: an umbrella review. Ann Behav Med. (2023) 57:817–35. doi: 10.1093/abm/kaad041
59. Namkoong K, Nah S, Record RA, Van Stee SK. Communication, reasoning, and planned behaviors: unveiling the effect of interactive communication in an anti-smoking social media campaign. Health Commun. (2017) 32:41–50. doi: 10.1080/10410236.2015.1099501
60. Wright KB, Bell SB, Wright KB, Bell SB. Health-related support groups on the internet: linking empirical findings to social support and computer-mediated communication theory. J Health Psychol. (2003) 8:39–54. doi: 10.1177/1359105303008001429
61. Digitally Supported Lifestyle Programme to Promote Brain Health Among Older Adults (LETHE). Identifier NCT05565170. US national library of medicine (2023). Available at: https://clinicaltrials.gov/study/NCT05565170?term=NCT05565170&rank=1.
62. Hanke S, Mangialasche F, Bödenler M, Neumayer B, Ngandu T, Mecocci P, et al. AI-based predictive modelling of the onset and progression of dementia. Smart Cities. (2022) 5:700–14. doi: 10.3390/smartcities5020036
63. Yardley L, Morrison L, Bradbury K, Muller I. The person-based approach to intervention development: application to digital health-related behavior change interventions. J Med Internet Res. (2015) 17:e30. doi: 10.2196/jmir.4055
64. LETHE. Public involvement. Available at: https://www.lethe-project.eu/public-involvement/.
65. EU-FINGERS. The advisory board. Available at: https://eufingers.com/for-general-public/patient-and-public-involvement/the-advisory-board/.
66. Multi-MeMo. About the advisory board. Available at: https://www.multi-memo.eu/public-involvement/about-the-advisory-board/.
67. Pitkala KH, Routasalo P, Kautiainen H, Sintonen H, Tilvis RS. Effects of socially stimulating group intervention on lonely, older people's cognition: a randomized, controlled trial. Am J Geriatr Psychiatry. (2011) 19:654–63. doi: 10.1097/JGP.0b013e3181f7d8b0
68. Mortimer JA, Ding D, Borenstein AR, DeCarli C, Guo Q, Wu Y, et al. Changes in brain volume and cognition in a randomized trial of exercise and social interaction in a community-based sample of non-demented Chinese elders. J Alzheimers Dis. (2012) 30:757–66. doi: 10.3233/JAD-2012-120079
69. Duan Y, Lu L, Chen J, Wu C, Liang J, Zheng Y, et al. Psychosocial interventions for Alzheimer's disease cognitive symptoms: a Bayesian network meta-analysis. BMC Geriatr. (2018) 18:175. doi: 10.1186/s12877-018-0864-6
70. Akenine U, Thunborg C, Kivipelto M, Fallahpour M. Experiences of participation in a multimodal preventive trial MIND-ADMINI among persons with prodromal Alzheimer’s disease: A qualitative study. J Multidiscip Healthc. (2021) 15:219–34. doi: 10.2147/JMDH.S345607
71. Flake JK, Fried EI. Measurement schmeasurement: Questionable measurement practices and how to avoid them. Adv Methods Pract Psychol Sci. (2020) 3:456–65. doi: 10.1177/2515245920952393
72. Menting GGA, Bruinsma J, Crutzen R. Preserving cognitive abilities during aging and dementia risk reduction: conceptualization, measurement, and promotion of cognitive and social activities. Open Science Framework. (2024). doi: 10.17605/OSF.IO/EABX9
73. Walker LO, Avant KC. Strategies for theory construction in nursing. New York: Upper Saddle River (2019).
74. Bartholomew Eldredge LK, Markham CM, Ruiter RA, Fernández ME, Kok G, Parcel GS. Planning health promotion programs: an intervention mapping approach. San Francisco: John Wiley & Sons (2016).
75. Kok G, Gottlieb NH, Peters GJY, Mullen PD, Parcel GS, Ruiter RA, et al. A taxonomy of behaviour change methods: an Intervention Mapping approach. Health Psychol Rev. (2016) 10:297–312. doi: 10.1080/17437199.2015.1077155
76. Carey RN, Connell LE, Johnston M, Rothman AJ, De Bruin M, Kelly MP, et al. Behavior change techniques and their mechanisms of action: A synthesis of links described in published intervention literature. Ann Behav Med. (2019) 53:693–707. doi: 10.1093/abm/kay078
77. Bandura A. Health promotion from the perspective of social cognitive theory. In: Understanding and Changing Health Behaviour. New York: Psychol Press (2013).
78. Ponvel P, Shahar S, Singh DKA, Ludin AFM, Rajikan R, Rajab NF, et al. Multidomain intervention for reversal of cognitive frailty, towards a personalized approach (AGELESS trial): study design. J Alzheimers Dis. (2021) 82:673–87. doi: 10.3233/JAD-201607
79. Rohr S, Arai H, Mangialasche F, Matsumoto N, Peltonen M, Raman R, et al. Impact of the COVID-19 pandemic on statistical design and analysis plans for multidomain intervention clinical trials: Experience from World-Wide FINGERS. Alzheimers Dement (N Y). (2021) 7:e12143. doi: 10.1002/trc2.12143
80. Darley A, Carroll A. Conducting co-design with older people in a digital setting: methodological reflections and recommendations. Int J Integr Care. (2022) 22:18. doi: 10.5334/ijic.6546
Keywords: social activities, prevention, cognitive decline, dementia, multidomain intervention
Citation: Bruinsma J, Visser LNC, Abaci A, Rosenberg A, Diaz A, Hanke S, Crutzen R, Mangialasche F, Kivipelto M and Thunborg C (2024) Social activities in multidomain dementia prevention interventions: insights from practice and a blueprint for the future. Front. Psychiatry 15:1386688. doi: 10.3389/fpsyt.2024.1386688
Received: 15 February 2024; Accepted: 01 May 2024;
Published: 20 May 2024.
Edited by:
Myrra Vernooij-Dassen, Radboud University Medical Centre, NetherlandsReviewed by:
Manuel Gonçalves Pereira, Universidade Nova de Lisboa, PortugalCopyright © 2024 Bruinsma, Visser, Abaci, Rosenberg, Diaz, Hanke, Crutzen, Mangialasche, Kivipelto and Thunborg. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Charlotta Thunborg, charlotta.thunborg@ki.se
†These authors share first authorship
 Jeroen Bruinsma
Jeroen Bruinsma Leonie N. C. Visser2,3,4,5†
Leonie N. C. Visser2,3,4,5† Ana Diaz
Ana Diaz Sten Hanke
Sten Hanke Rik Crutzen
Rik Crutzen Francesca Mangialasche
Francesca Mangialasche Miia Kivipelto
Miia Kivipelto Charlotta Thunborg
Charlotta Thunborg