- 1Advance Clinical and Translational Research, Division of Biology and Medicine, Brown University, Providence, RI, United States
- 2Department of Psychiatry and Human Behavior, Bradley Hospital, Riverside, RI, United States
- 3Department of Psychiatry and Human Behavior, Brown University, Providence, RI, United States
- 4Center for Biomedical Informatics, Brown University, Providence, RI, United States
- 5Progreso Latino, Central Falls, RI, United States
- 6Rhode Island Quality Institute, Providence, RI, United States
Introduction: Due to a combination of cultural, situational, social, and environmental factors, members of the Latine/Hispanic community experienced higher contagion and poorer outcomes amid the COVID-19 pandemic, and lower rates of testing and vaccination. Our aims were to use the frameworks of implementation science to identify barriers and facilitators impacting equitable access to COVID-19 testing and vaccination programs among Rhode Island's (RI's) Latine/Hispanic community.
Methods: Between February and June 2021, we implemented a community-centered approach, empowering Promatoras, trusted community health leaders, to conduct eight focus groups among RI's Latine/Hispanic community (n = 55). To gain the perspectives of health delivery experts, we conducted six one-on-one interviews with healthcare professionals serving this community. Recordings were translated into English as applicable, transcribed, and analyzed using directed content analysis and thematic analysis, guided by theories of implementation science.
Results: Latine/Hispanic community members made decisions about participation in testing and vaccination programs by considering factors primarily related to their communal, religious, interpersonal, and emotional contexts. The amount and sources of information they received, perceived accessibility of interventions, and their perceived agency (i.e., freedom to decide how/when/where to follow interventions) also shaped decisions. Many barriers identified by clinicians (e.g., structural determinants to access) were not discussed by Latine/Hispanic community members.
Discussion: Facilitators and barriers to test/vaccine implementation were shaped by local communal and individual factors, generally supporting previous arguments on implementation among Latine/Hispanic communities, and revealing the importance of context-specific examinations. In public health pandemic preparedness work, we encourage community-based participatory approaches to identify priorities/barriers and involvement of community leaders to build trust, frame messaging, and disseminate information.
1 Introduction
Since being declared a global pandemic in March 2020 (1), COVID-19 has caused the deaths of over 1.2 million U.S. citizens (2). Following larger healthcare trends in the U.S., race/ethnicity was among the strongest predictors of poor COVID-19 outcomes, evidenced by increased rates of infection, hospitalization, and mortality among Black, Indigenous, and People of Color (BIPOC) communities and those of Latine/Hispanic ethnicity (1–5). Recognizing these inequities, national research and health leaders have called for exploration of disparities relating to COVID-19 prevalence, outcomes, and care access among underserved populations, defined by the NIH as those who, because of biological, environmental, or systemic factors, were at heightened risk for COVID-19 complications or had limited access to necessary precautions (6).
Rhode Island (RI) is the second most densely populated and the most geographically compact state in the U.S., and it has a Latine/Hispanic population (16%) comparable to the national average (18.7%) (7, 8). It therefore provides a unique opportunity to examine factors contributing to COVID-19 disparities among Latine/Hispanic communities (7, 8). Reflecting national trends in racial and ethnic health disparities, inequities in COVID-19 outcomes were evident in RI as early as April 2020, when the Latine/Hispanic population accounted for 45% of the state's positive COVID-19 tests (8) and experienced higher rates of ICU admission and intubation (3). Latine/Hispanic diagnosis rates continued to be disproportionately higher through the completion of statewide data collection in March 2021 (2, 9).
The most effective public health interventions for preventing COVID-19 included social distancing and quarantining, mask-wearing, contact tracing, testing, and, upon development, vaccination (10, 11). Given the importance of these strategies, particularly among disproportionately-affected populations, previous research has focused on vaccine-related hesitancy and has identified lack of information, fear and mistrust, structural barriers, and doubts of efficacy as key barriers among (typically combined) Latine/Hispanic and African American populations (12–16). For example, one recent paper employing community-based research methods to examine the experiences of Latine/Hispanic, African American, and Native American individuals has identified the central role of communication techniques in addressing fear, mistrust, and context-specific barriers (16).
In the research that has been published specifically on the experience of Latine/Hispanic communities during the COVID-19 pandemic, many groups of scholars have focused on emotional well-being (17), or on the relationship between the pandemic and co-occurring experiences, such as cancer or pregnancy (18, 19). Likewise, few previous studies on COVID-19 outcome disparities and vaccine hesitancy have prioritized Latine/Hispanic community-member perceptions, often focusing on larger political, health (e.g., pregnancy), or psychological factors (13–15, 20, 21). Further, few studies have explored barriers and facilitators to COVID-19 prevention protocols more broadly (beyond vaccines; including distancing, tests, and masks), information crucial to crisis preparedness (13–15, 20, 21).
In prioritizing community-member voices, our main aims were to: (1) understand the experiences of information access, supply access, and emotional support among RI's Latine/Hispanic community throughout the COVID-19 pandemic and (2) identify barriers and facilitators to accessing and participating in related interventions. We supplemented this with the perspectives of clinical experts serving the Latine/Hispanic community to identify gaps in understanding and infrastructural factors. Considering together the emotional and access experiences of members of the Latine/Hispanic community, with the perspectives of local experts who worked directly with this community, we hope to identify exact informational and intervention junctures where misinformation and mistrust emerged in order that communication and action protocol for future pandemics might prevent these barriers to well-being. Our findings will facilitate called-for improvements in health crisis preparedness infrastructure, policy developments, and communication campaigns to support more equitable outcomes by both empowering agency and facilitating trust in the future (22).
2 Methods
2.1 Overview
The National Institute on Health's RADx-UP initiative includes research projects across the U.S. studying COVID-19 testing, vaccination, and outcomes among underserved populations (6). This RADx-UP study was part of a larger statewide tracking, exploratory, and implementation effort aiming to (1) leverage health information infrastructure to study COVID-19 test/vaccine access and uptake in RI, (2) identify barriers to uptake, and (3) identify opportunities to address these barriers via a community-based approach (47). This manuscript reports on the second of these aims. The Brown University Institutional Review Board approved all research procedures.
2.2 Procedure
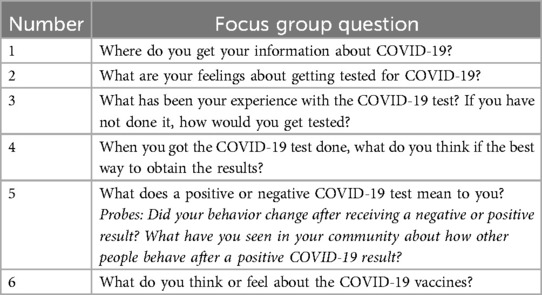
Using a community-centered model, researchers worked closely with Promotoras at Progreso Latino, RI's largest Latine/Hispanic-centered non-profit organization, who guided the development of focus group scripts and, using flyer-distribution, direct communication at events, and word-of mouth, recruited Latine/Hispanic community members. Promotoras (commonly referred to in English as Community Health Workers) are trusted community leaders who promote health, social justice, and equitable care in Spanish-speaking communities (23–25). Previous studies have shown Promotora-empowerment to be effective toward improving a range of health outcomes in Latine/Hispanic communities (23, 26, 27). Promotoras received comprehensive training, including formal CITI Program certification in human subjects research. Additionally, weekly meetings reinforced methodological rigor through debriefing focus groups, refining questions, and emphasizing ethical data collection practices. After being trained in facilitation, Promotoras conducted virtual focus groups (1–1.5 h long) between February and June 2021, to gather community-member perspectives on the COVID-19 pandemic generally and experiences of testing and vaccination specifically; see Table 1. Participants were deemed eligible based on RI residency, age (18+), and Latine/Hispanic identity. They provided informed consent through registration via the video conferencing platform and verbal agreement. Participants received compensation for their time, including financial compensation and the opportunity to ask questions of local health representatives. To minimize bias, focus groups were conducted in Spanish between community members and Promotoras. Research team members observed focus groups without participating and without visual presence.
To supplement community-member responses, local health professionals who worked with the Latine/Hispanic community participated in virtual one-on-one semi-structured interviews, lasting 20–30 min, between March and May of 2021. Interviews were conducted by an experienced community practice facilitator and interviewees were all clinicians at local Federally Qualified Health Centers or Free Clinics serving high proportions (>50%) of Latine/Hispanic patients. Eligibility requirements included being clinically active and regular engagement with Latine/Hispanic patients. Interviewees provided verbal consent and were not compensated. The purpose of interviews was to gain clinician perspectives on key issues and experiences faced delivering tests/vaccines to the Latine/Hispanic community; see Table 2.
The leadership group and Promatoras, who conducted the focus groups and actively guided analysis discussions, determined data saturation collaboratively, rather than through a formal matrix. By later weeks, our weekly discussions, consistently revealed recurring themes across the focus groups, with little new information, indicating saturation in our understanding of participants’ experiences. Throughout the study, we addressed the trustworthiness criteria of credibility, dependability, confirmability, and transferability. To enhance credibility, we prioritized prolonged engagement and iterative discussions between researchers, Promatoras, and focus group transcripts, which ensured findings accurately reflected participant experiences. We defined dependability as consistent application of the research protocol and maintenance of data quality, and supported this through consistent weekly meetings, structured debriefings, and supervision of the Promotoras. We established confirmability hand-in-hand with saturation, by collaboratively identifying the consistency of themes across the focus groups, and we supported transferability by providing a rich context through detailed discussions of our study processes, enabling readers to assess the applicability of our findings to similar settings.
2.3 Data analysis
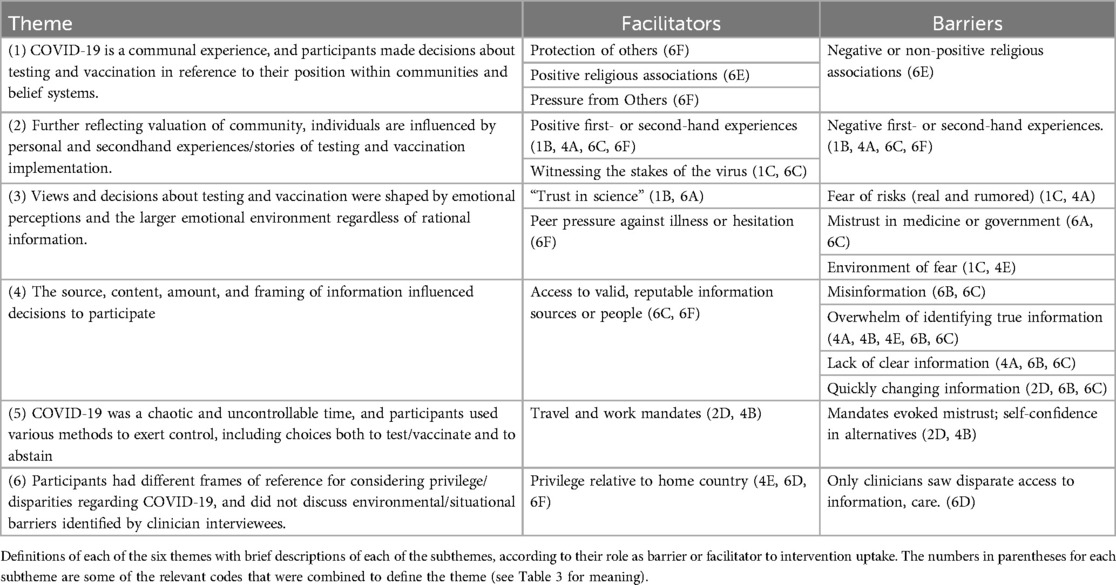
Focus group and interview data, recorded through the video conferencing platform, were transcribed and translated using a third-party secure professional translation service and analyzed in two phases. First, to identify barriers and facilitators to intervention uptake, we conducted a directed content analysis, with existing theory guiding (deductive) coding, and uncoded content prompting the development of inductive codes (28). The original Consolidated Framework for Implementation Research (CFIR) (24) domains and corresponding subconstructs informed our coding framework. The CFIR's five domains are: (1) intervention characteristics, (2) outer policy context, (3) inner context, (4) characteristics of individuals targeted in implementation, and (5) implementation process (29). Analysts individually coded each transcript using this framework and then, to maintain consistency and rigor, groups of 2–3 analysts cross-coded the transcripts. Because our priority in this work was to maintain a community-centered focus of analysis and empower the perspectives of the members of the Latine/Hispanic community and those who serve them, we held the CFIR categories loosely. In conversations among analysts and prioritizing the data, we redefined each of the categories so that they aligned with the main ideas articulated in CFIR texts, but were flexible and changed meaning to best accommodate the realities of the participants. Where there was tension between category definition and data, the data took priority, and we adjusted the definition, documenting changes in audit memos and a shared codebook (Table 3). The first author led the consensus process by which final coding decisions were made and entered coded data into the qualitative data management software NVivo (30).
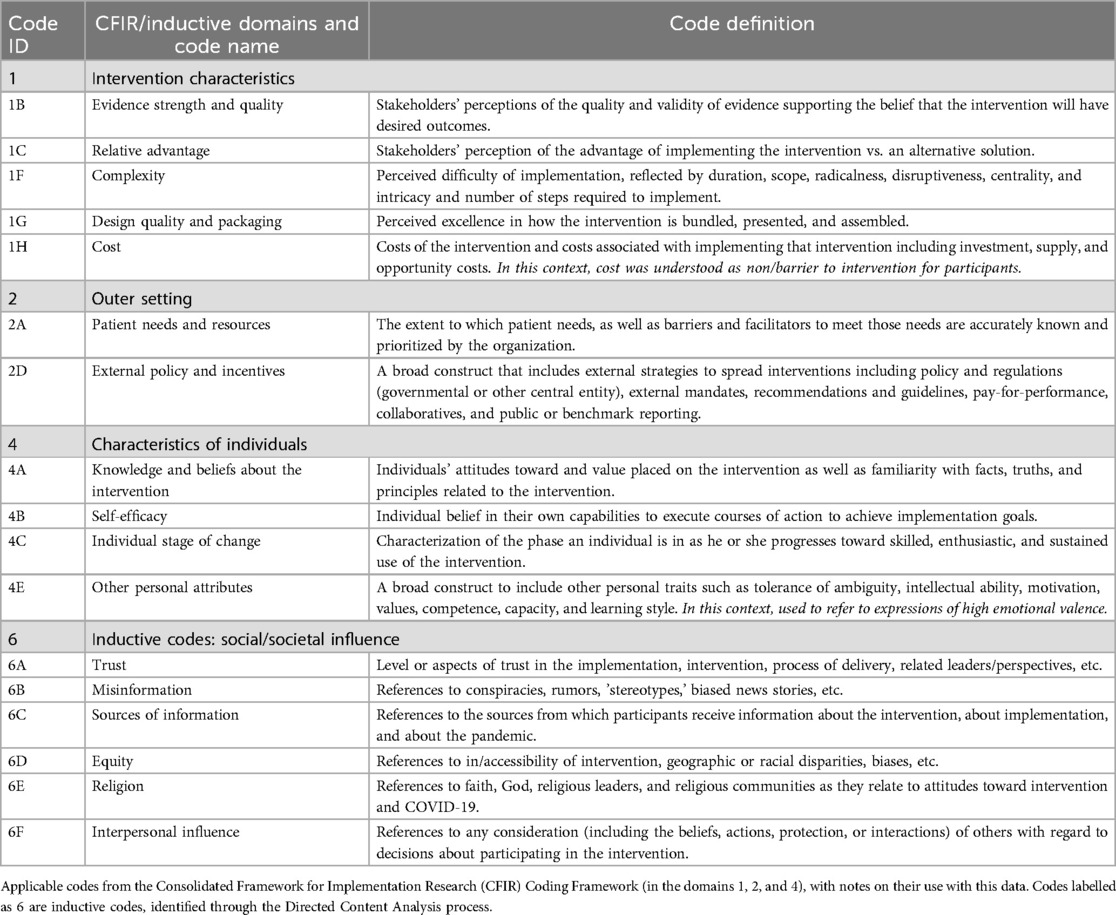
Table 3. Consolidated framework for implementation research (CFIR) selected codes and inductive codes.
The second phase of analysis was thematic (31), examining the coded data for patterns within and across codes towards the development of overarching themes that describe key implementation trends. With guidance and review from a secondary analyst (fifth author), the primary analyst reviewed, defined, and named the themes, and selected illustrative participant quotations (31).
3 Results
Eight focus groups were conducted among groups of 3–12 Latine/Hispanic individuals, with a total of 55 participants, 30 females and 25 males. Six supplemental interviews were conducted among female and male practitioners at local clinics.
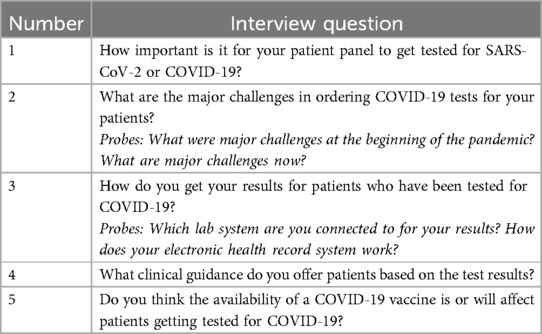
In the directed content analysis phase, we identified as applicable to the data 11 codes from CFIR subconstructs in three domains: (1) Intervention Characteristics (test and vaccine), (2) Outer Setting (environmental and policy determinants, RI), and (4) Characteristics of Individuals (Latine/Hispanic community-members). Because of our community-centered methods, we inductively generated six codes related to social influences; see Table 3. In the thematic analysis phase, we generated six themes, which are described below, with exemplar quotes in text. The definitions and relevant codes for all themes and subthemes are in Table 4. To protect participant identity, all quotes are de-identified; community member quotes are marked as [CM] and healthcare workers as [HCW].
On the whole, participants expressed a range of views regarding COVID-19 testing and vaccination, from trust and enthusiastic participation to mistrust and refusal to participate. Many variables influenced these decisions, including information sources, perceived ease of access, and personal, religious, and communal factors. Clinician interview data largely supported the views expressed in focus groups. Notable contrasts existed in perceptions of risks, barriers, and knowledge access.
3.1 COVID-19 is a communal experience, and participants made decisions about testing and vaccination in reference to their position within communities and belief systems
3.1.1 Facilitators
Many participants viewed intervention uptake as advantageous—and worth discomfort, fear, or other risks—because it helped to protect both themselves and their family/community members, particularly those that, because of age or underlying factors, were at heightened risk of harm. Some participants spoke to the inherently communal nature and high stakes of contagion, encouraging others to participate (i.e., towards “herd immunity”) or saying that they had participated in the intervention in response to others.
“Let us remember that there are elderly people, much older people who do not have the strength or the capacity that we have. Therefore, we have to take the test and keep our distance as soon as [inaudible] we find out we are positive. Why? Because of others.” [CM]
Further, when religious beliefs/leaders encouraged the intervention directly or indirectly (e.g., intervention is from God, or is okay because it does not keep us from God's wishes), participants were more likely to partake in masking, distancing, or vaccination.
“I am 100% positive and I think it was a great opportunity that first God gave us, and then the scientists.” [CM]
3.1.2 Barriers
When participants’ religious beliefs/leaders directly dissuaded them from participation or when participants decided to prioritize faith in God over intervention participation (i.e., faith would keep them healthy), they were less likely to participate in the intervention.
“So many people say, ‘I am not going to get vaccinated, because if I get vaccinated, I am doing something to favor the devil.'” [CM]
3.2 Further reflecting valuation of community, individuals are influenced by personal and secondhand experiences/stories of testing and vaccination implementation
3.2.1 Facilitators
Almost all participants described personal/secondhand experiences as crucial to their decision-making regarding testing/vaccination. When participants or their community-members had positive experiences (e.g., test results affirming symptom experiences or vaccine providing immunity), they gave both rational and emotional articulations of trust.
“My mother is 90 years old and a month ago my brother got the coronavirus, but my mother has already been vaccinated and they are both alive.. I believe very much in the vaccine and I recommend people who don't believe in it to get vaccinated.” [CM]
Some participants described participating in the intervention with fear, or despite having heard negative stories from others.
“The expectation of what side effect it is going to have on you. Many people would say to you, ‘It put me in bed for four days.’ Another would tell you, ‘It didn't do anything to me.’ ‘I had a lot of pain in my arm.'” [CM]
After stating these fears, many participants shared that they had had a positive personal experience. This in turn led to future participation. Further, some described being motivated to participate in the intervention upon witnessing the severe illnesses of others, realizing the stakes of implementation through others’ experiences.
3.2.2 Barriers
When participants were exposed to first- or second-hand experiences that were negative (e.g., of pain/discomfort, incorrect test results, or vaccine inefficacy), they were dissuaded from initial or repeated participation in the intervention on account of mistrust or fear.
“I had 14 days in isolation in the attic of the house, with all the symptoms that came with it, very strong, very difficult, but the test came back negative. It is somewhat frustrating and disconcerting… I'm definitely 100% sure that I got it. However, the tests came back negative.” [CM]
3.3 Views and decisions about testing and vaccination were shaped by emotional perceptions and the larger emotional environment regardless of rational information
3.3.1 Facilitators
Some participants articulated full trust in “science” or belief that the intervention would result in the desired outcome. These occurred most frequently without any further explanation.
“I have been tested several times, I am like a fanatic, because I look for the safety of not infecting others” [CM]
A few participants also described emotional environments of judgement against those who were ill or not testing/vaccinating, encouraging participation.
“At work there is also that panic, if someone sneezes they already have COVID, I have seen at work how two women grabbed each other by the hair because one of them sneezed.” [CM]
3.3.2 Barriers
One of the most significant barriers to testing/vaccination was fear, with participants arguing that participation was not worth the risks involved. Many mentioned both real (e.g., side effects, discomfort, speedy production) and rumored (e.g., death or sterility) risks, and a few described mistrust in the medical institution/government.
“It is practically an invasion of one's nose to try to prove that one has or does not have it.” [CM]
Clinician interviewees affirmed this trend, mentioning hesitancy as a consistent barrier to intervention.
“I think that we're still fighting the hesitancy, right?” [HCW]
Participants described additional contributing emotional factors including the larger panic surrounding COVID-19.
“We were all, in one way or another, in a panic because it created a panic. The panic was so great that people were killing each other for toilet paper. People were going to the supermarkets and there was fighting over toilet paper, something astonishing, something unbelievable.” [CM]
For some, fear prevented intervention participation.
“The stereotypes and everything that people say, that it is going to turn you into a zombie, that it is going to give you I don't know what, that it is going to give you I don't know how many consequences.” [CM]
For others, the impetus to overcome fear facilitated participation, in that participants, observing the chaos around them or experiencing great fear of infection themselves, saw the intervention as their main source of hope and participated accordingly.
3.4 The source, content, amount, and framing of information influenced decisions to participate
3.4.1 Facilitators
When participants had access to valid information about COVID-19 (e.g., contagion rates) and about the function and efficacy of tests/vaccines, most consistently via medical or governmental sources, they were more likely to participate in the intervention.
“I receive the information every day since the pandemic started, wherever we go, there is always information about COVID, through social networks, the same way you find out about it through the news, through television, you find out at every moment.” [CM]
Clinician interviewees affirmed this, saying that community members had access to reputable sources of information.
“I think, in terms of what’s being communicated at the state level as far as what procedures to do is pretty clear, and I think people have a pretty good understanding at this point, but always checking in back with us with anything regarding symptoms or what to expect for their health going forward.” [HCW]
3.4.2 Barriers
The most common source of information, by far, was news or social media. Participants described accessing both misinformation, rumors, or other untrue dissuading information and helpful/truthful information from these sources. Many also described the overwhelm resulting from media excess and the difficulty parsing truth from misinformation, preventing trust and participation.
“Unfortunately people take a lot from what other people say and not from authorized sources. That is why so many conspiracy theories have been created, that this is from the devil, that the vaccine, that this is the new world order.” [CM]
Moreover, many clinician interviewees identified access to detailed and comprehensible information as a key barrier, and a few described efforts to provide information to community-members.
“Even, let’s say, they live with family members, I don't think they really understood what quarantine meant, and that meant being in a separate room from everyone else, making sure you're cleaning after yourself.” [HCW]
Despite these efforts (suggesting possible inefficacy or communication barriers), most focus group participants described feeling unsupported by medical professionals/sources, not having enough information, or lacking access to suitable evidence for the intervention’s efficacy. For example, only one of the 55 participants articulated an understanding of the process by which the vaccine works.
“I took care of myself a little bit, but they never told me what I should do. They did not give me any medication, they did not tell me what I should take, what I should not take. I have been really worried about it and I will not forget the way they acted about it, because if so many people are dying, how is it that they did not pay a little attention.” [CM]
Further, because of the real inefficacy, speed, and risks of interventions, information access was a barrier when these disadvantages were taken as more salient than advantages.
“I'm skeptical about the process of the vaccine, the record time in which the vaccine was made, it definitely makes one worry about, why so fast if the tests that have been done are not that many, and it hasn't lasted long enough to know what the long term effects are.” [CM]
3.5 COVID-19 was a chaotic and uncontrollable time, and participants used various methods to exert control, including choices both to test/vaccinate and to abstain
3.5.1 Facilitators
Many participants described participating in the intervention on account of travel-based or medical policies mandating it.
“About the vaccine, actually, they told me to get it. They told me, ‘Get it, because you're going to need it like an ID or something. Then to go out or to go into a mall, etcetera. That’s going to be like your social security, this whole residency thing, something like that, the paper they give you when you get vaccinated.’ What I think about the vaccine is that–I've always been afraid to get the vaccine.” [CM]
3.5.2 Barriers
Even as these policies/mandates facilitated participation, some viewed this as a violation of agency and, for this reason, expressed mistrust of the intervention and medical institutions, preventing further participation.
“The one I was given was Johnson’s, I was not given a choice, I have heard that Moderna’s and the others are better than Johnson’s, why is Johnson’s a single dose?” [CM]
Additionally, even as many participants articulated confidence in their abilities to prevent COVID-19, these actions took varying forms, from intervention participation, to medical practices excluding the interventions (e.g., hand-washing or isolation), to religious action and faith.
“What I did do was to take good care of myself. I took a lot of vitamin C and ate a lot of yellow fruits, which is what prevents diseases. The truth is that I have not taken the test throughout the year. I can't say what COVID is, what the test is, nothing like that. I have had no need for any of it.” [CM]
Participants also exerted control in choosing information sources—including medical, social/media, and religious.
3.6 Participants had different frames of reference for considering privilege/disparities regarding COVID-19, and did not discuss environmental/situational barriers identified by clinician interviewees
3.6.1 Facilitators
Participants saw themselves as privileged by free/affordable and straightforward access to the intervention and supportive community-members, particularly compared to the costliness or inaccessibility experienced by residents of their home-countries—for some, this relative privilege encouraged participation in the intervention.
“We have a great opportunity here, because in my country, in Colombia, they are not even doing the tests, and if they do, they are very expensive.” [CM]
“It would be great if everyone could have access to the vaccine, like we have here in the United States and not like in our countries where we see that people are dying more and more every day. It is a shame to see that many people here are refusing to get the vaccine, when in our countries people are begging for the vaccine to arrive” [CM]
3.6.2 Barriers
Clinician interviewees saw the Latine/Hispanic community as experiencing significant disparities in resource access, insurance-related barriers, and lack of information, education, and understanding.
“I will say that as far as patients that do come in, that have difficulties with health insurance, it becomes a little challenging, especially when you try and navigate how can we, A, get them tested, and then B, address their health insurance concerns. That makes things a little complex.” [HCW]
“Our population was hit not only the hardest in Rhode Island but actually in the world. It ranked pretty high in terms of positivity rate. There’s a lot of factors that go into that. I'd say the most basic one is the fact that we're a densely populated area, and we are very underserved where we serve a very underserved population, that’s not a secret.” [HCW]
Clinician interviewees also described the elevated risk of COVID-19 contagion faced by the Latine/Hispanic population due to cohousing norms (increasing risk of contagion and making isolation difficult), financial pressures to continue in-person work, lack of transportation/clinical access.
“I think [testing/vaccination is] incredibly important, especially considering people’s dwellings, the amount of contact that people have with each other. A lot of higher level cultural things like religion and people’s affinity for gathering for spiritual purposes, it’s a really big part of our community and our culture. I think, the more testing for our community, the better.” [HCW]
“No matter what you said, they're like, ‘Well, I've got to put food on the tables, got to go to work.’” [HCW]
Notably, no participants mentioned these barriers.
4 Discussion
Our research explored facilitators and barriers to the access and use of COVID-19 mitigation interventions among RI's Latine/Hispanic community, and moves beyond previous studies in two important ways. First, in working toward health equity, we centered Latine/Hispanic community-member perspectives in analytic prioritization, use of qualitative methods, and empowerment of Promotoras for design, recruitment, and moderation. This specificity to one minoritized community [rather than combining multiple BIPOC communities, for example (13–16)], allowed for more clear and specific trends, the leadership of Promotoras fostered participant comfort and honesty, and the analysis extended the possibilities of implementation science frameworks by combining inductive with deductive methods. Second, in seeking a broader understanding of facilitators and barriers to crisis intervention generally, we analyzed discussion of vaccines alongside tests, masking, and distancing. We argue that these decisions at the core of the study make it particularly applicable to the development of equitable health crisis preparedness protocol.
Overall, we found that members of the Latine/Hispanic community made decisions about intervention participation in a deeply contextualized way, shaped by beliefs and duties associated with their larger community and by first- and second-hand experiences/influences. We also found that Latine/Hispanic community members made decisions in reference to their emotional instincts and within fear- and mis/trust-laden environments, that some experienced an excess of (conflicting) information and a dearth of medical information, and that many viewed decisions on test/vaccine participation as an opportunity to exert agency within these environments. Finally, we found that Latine/Hispanic community members’ decisions about test/vaccine uptake were influenced by perceived ease of access, and that they did not identify the structural barriers that clinicians named as significant.
Our findings support studies positing that key factors preventing vaccine uptake among Latine/Hispanic and African American communities include fear and mistrust related to incorrect, inconsistent, and lacking information (13, 16, 32, 33). Some scholars have argued that COVID-19 was intertwined with an “infodemic,” marked by excessive, rapidly changing, and conflicting information released surrounding disease outbreak (34, 35), and others have identified the lack of clear information as a direct cause of isolation and uncertainty among Latine/Hispanic, as well as among other, populations (31). These authors propose access to correct information was a facilitator of vaccine uptake or precautionary behaviors, and lacking or incorrect information were barriers (13, 16, 32, 34); our conclusions generally support this claim. One of these studies has argued for the power of anecdotal, personal, examples as an important evidence base for vaccine trust in the general public (33). Our findings on the significance of positive interpersonal influence as a facilitator to intervention uptake supports these findings in the Latine/Hispanic context. However, in our sample, knowledge about true risks of tests/vaccines, or negative interpersonal influence, was a barrier for some, suggesting that medical information must be communicated intentionally, particularly with communities less prone to trust (13, 14). Future health crisis preparedness plans should take into account the complexities of infodemics, the power of interpersonal influence, and their particularly significant impact on Latine/Hispanic communities.
Our findings also establish a deeper understanding of the contexts in which Latine/Hispanic community members received and interpreted information, which we argue are key to their decision-making. Previous studies acknowledge religious, trusted community spaces/leaders, and the experiences of others as important for communicating information and establishing trust (13, 14, 16, 32). Our findings support these claims, and we add consideration of duties to protect and interpersonal relationships. Relatedly, previous explorations of vaccine hesitancy among BIPOC communities have claimed that much mistrust stems from historical exertions of injustice and violence (13, 14, 16, 23). In combining study of multiple minoritized/BIPOC communities in the U.S., studies have generalized these historically-rooted traumas/mistrusts to the Latine/Hispanic community (16). Our results differ from this assumption: while multiple participants in this study voiced doubts in the intervention, and a few mistrust in “science,” in line with previous studies (16), none discussed these histories. We note this not to minimize attention to these histories or claim they have no impact on the Latine/Hispanic community, but to highlight the importance of implementation strategies shaped according to community-specific barriers. Our conclusions suggest that, in contrast with African American, Native American, and combined/generalized communities previously surveyed (13–16), Latine/Hispanic participants in RI experienced fear primarily associated with community environments and social/media information, establishing the importance strengthening community-specific trust and communication networks.
This insight, among others, illustrates the methodological contributions of the study. Even as we used an implementation science framework to structure analysis of the themes, we centered these community-based methods by changing and adding to the framework. This application of both inductive and deductive methods expands the possibilities in implementation science work, allowing local knowledge to lead insights, and eventually implementation, even beyond that typically allowed by the frameworks. For example, we found factors, including interpersonal influence, religious affiliation, and a sense of trust, which the CFIR does not take into account (29), to be central to understanding Rhode Island's Latine/Hispanic community's experience and perspectives. Future implementation science studies, particularly among underserved or minoritized populations, might benefit from similar combinations of deductive and community-centered, inductive, methods.
Using participatory, community engagement methods may also increase future implementation success. Involving interested parties as key members of the research team from the beginning of a project may lead to their involvement as communication and dissemination partners during implementation phases, creating trust with communities in the process (36). Involving community participation on a research team also allows for the co-production of knowledge and solutions which inform implementation strategies to increase the uptake of evidence-based interventions in community settings (37). Just as we included Promotoras as part of our team, future implementation science efforts also need to include trusted members of the community in the research effort, providing a bridge between the research team and implementation efforts in the community.
However, participatory methods often require an inductive approach, as theory-driven methods (e.g., CFIR) may not be well understood by community members on the team. These inductive and theory-driven approaches may complement each other if they are used in a two-step fashion, as our team did with the current study. We first identified the lived experiences of barriers and facilitators to COVID-19 testing and vaccination from community members and health care workers. Through this, we redefined the specific CFIR categories, and added new context-specific categories, to align with these lived experiences. We applied this new framework deductively. In this way, our project used community-driven knowledge to inform future implementation strategies that come from CFIR, a method which informs the selection of implementation strategies for future implementation efforts (38).
Further, many participants mentioned receiving a COVID-19 test or vaccine on account of mandates for travel, medical visits, or work. While previous studies have noted that requirements increase test/vaccine uptake, and thus are crucial to population safety (10), some members of our sample spoke to the importance of granting agency, particularly toward establishing trust. This extension to previous research provides additional evidence for the importance of inductive, community-based prioritizations beyond the deductive, implementation-science-based methods, as it illustrates the complex relationship between trust, experience, and perceptions of agency, beyond those that the CFIR considers (29). This is especially important among communities with lower trust in medical institutions/interventions, and should be taken into account in framing equity-oriented communication in future health emergencies, as we discuss below.
Our final theme described important discrepancies between the Latine/Hispanic community members and local clinicians, not thoroughly discussed in the literature. Notably, members of the Latine/Hispanic community—in contrast to the clinicians serving them—did not describe lack of access to tests/vaccines and did not comment on social and environmental determinants of COVID-19 outcome. Scholars have established that a key source of emotional burden among Latine/Hispanic individuals during COVID-19 was concern about family members living abroad (7), and others have highlighted the significant stress of immigration status and familial vulnerability as significant beyond pandemic-fears (17). Our arguments expand these claims by proposing that, relative to these concerns, perceptions of privilege (particularly among those farther from borderlands or less directly impacted by immigration threats 17) motivated testing/vaccination. Additionally, participants perceived a lack of communication from medical professions, discordant with clinician attempts to educate. Noting these discrepancies and the prevalence of public health research shaped within positions of power, as opposed to the community-centered perspectives we strive for here, we urge further study into the perceptions of privilege, priorities, and barriers among Latine/Hispanic communities to establish stronger collaboration models in addressing inequalities.
4.1 Limitations
In sharing these results, we describe only a portion of RI's Latine/Hispanic community. While we hope that the richness of these findings will be helpful in developing more equitable health crisis preparedness plans more broadly, we do not claim these results to be generalizable (27). Further, our data collection methods brought limitations insofar as, outside of focus groups, but as for their time, participants were given the opportunity to ask questions of state health leaders. This might have created pressure influencing participants’ sharing. To mitigate impact, these leaders, when applicable, left before the focus group began, and Promotoras repeatedly emphasized confidentiality and welcomed all opinions. Open expressions of disagreement or mistrust of interventions suggests that these measures were, at least in part, successful, but we acknowledge that other participants may have not shared as freely as hoped because of research team presence. We also recognize that trends particular to COVID-19 tests or vaccines may have been missed because we analyzed discussion of both interventions together, preventing intervention-specific implementation recommendations.
Furthermore, we did not collect racial information, using only Latine/Hispanic ethnic identity to reflect the population prioritized by RIPIN; this neglects differences among possible variations in racial self-identification. Prioritizing the safety and comfort of participants, we also did not collect citizenship information. This prevented examination of insurance- and other status-related fears and barriers to the intervention, previously identified as key determinants of COVID-19 outcome and care access (7, 13, 39, 40). While we believe this was the correct approach for our study, it limits the scope of our conclusions, as citizenship status may be an unrecognized mediating factor (39, 40).
5 Conclusions
Adjusting implementation science methods of analysis to center the voices of RI's Latine/Hispanic community, we have discussed key barriers and facilitators to test/vaccine implementation. Taken together, our findings contribute both to COVID-19-specific considerations, and to the broader implementation of public health interventions in the Latine/Hispanic community, by exploring the wide range of interpersonal, belief-based, and global contexts within which community members make personal health decisions. Even as our Latine/Hispanic specific findings differ in important ways from a published community-based participatory study among minoritized populations, our results emphatically support their conclusion that cultural and environmental contexts are central to understanding medical beliefs and decisions (16). These authors have argued for the implementation of further participatory leadership, empowering members of the local community in leadership and decisions even in non-crisis moments (16). This includes establishing communication methods according to community norms and needs (16, 33, 41, 42). Beyond the pandemic, researchers have implemented community-based methods in public health interventions among the Latine/Hispanic community, holding public events to ascertain local needs and opinions on advance care planning (41), or delivering cancer education to be more effective and efficiently disseminated (42). In line with our findings, such interventions have identified the importance of local representatives, both in disseminating scientific information among the community and in communicating community needs and beliefs to health leaders (41, 42).
Given the degree to which members of the Latine/Hispanic community made COVID-19 decisions according to their local community and environment, we urge future pandemic researchers to employ community-based methods to both develop and disseminate knowledge/tools most effectively. We urge community-led research and relationship-development to build trust, address barriers, and decrease the inequity of health outcomes in future crises. Based on these conclusions, we identify the relevance of this study via three key actions to guide development of more equitable public health crisis preparedness plans, preventing disproportionate impact on Latine/Hispanic communities (1, 3–5).
5.1 Empower the values, perceptions, and priorities of the community members
Learn about the local community. Before future health crises, intentional research relationships should be established to identify community leaders, communication networks, and perceptions of health priorities, privileges, and challenges. Toward this end, we recommend methods such as community-based participatory research (CBPR), which implements intentional collaboration with community members for all steps of study development and application, increasing perceived relevance and actual efficacy of hypothetical interventions before beginning intervention design (16, 43, 44). Local public health leaders should identify key informants, community health workers, and other members of underserved communities and establish permanent lines of communication in times of calm (16). This will allow scholars and leaders to, first, gain an understanding of when, why, and how community members make health decisions. The deeper understanding of priorities, definitions of health, and avenues of information access will empower effective understanding before any intervention development begins (5.2).
5.2 Collaborate to maximize influence within trusted communication networks
Implement context-based intervention strategies. It is important that we accept the realities of the local community's perceptions of needs and reliable information sources. For example, among RI's Latine/Hispanic community, interpersonal agents and community members played a more significant role in decisions to participate in interventions than that of officials, scientific results, or mandates. Recognizing this, and noting the success of Promotora involvement in increasing both test-rates and psychological health during COVID-19 (16, 17, 45), we posit that including Promotoras as CBPR team members or design and implementation leaders might enable researchers to effectively address barriers of trust and information access by leading intervention design, communicating priorities, and disseminating information. We therefore urge public health policy and action leaders to prioritize collaboration with Promotoras in the development and implementation of interventions on the local health infrastructure. This might include the development of ongoing working groups or the appointment of key community members to local positions, and will allow local and health leaders to, together, develop both community-based plans for future crises and structures of bidirectional knowledge-production for non-crisis, ongoing, healthcare needs (16, 31).
5.3 Frame communication about interventions honestly and empower individual choice
Previous research has suggested that communication about the vaccine be clear, comprehensible, and emphasize findings on efficacy and safety, both through large-scale results and through anecdotal evidence (32–34, 46). We add that the likelihood of possible risks should be honestly communicated, and framed within the larger benefits. In addition to being developed according to knowledge about the local context (5.1) and in partnership with local leaders (5.2), policies related to interventions should protect the agency of individuals, particularly from historically underrepresented groups. We believe that full and direct communication and decision-making power, particularly within CBPR-developed and Promotora-led communication networks, will decrease fear and grant agency to community members, fostering trust through choice rather than mandate.
According to our findings, and those of community-based public health initiatives (16, 32–34), we believe that establishing ongoing bidirectional structures for both learning about local communities and providing them education, and then empowering all members to make decisions according to their own beliefs, might empower communities of trust, protecting the well-being of underserved communities during and even beyond crisis situations.
Data availability statement
Anonymized transcripts (or excerpts) generated and analyzed for this study may be provided upon request to the corresponding author.
Ethics statement
The studies involving humans were approved by Brown University Institutional Review Board. The studies were conducted in accordance with the local legislation and institutional requirements. The participants provided their written informed consent to participate in this study.
Author contributions
DGS: Formal analysis, Methodology, Writing – original draft. YD-V: Conceptualization, Writing – review & editing. EC: Conceptualization, Writing – review & editing. MB: Conceptualization, Data curation, Writing – review & editing. ARE: Conceptualization, Methodology, Writing – review & editing. INS: Conceptualization, Funding acquisition, Methodology, Project administration, Writing – review & editing.
Funding
The author(s) declare that financial support was received for the research and/or publication of this article. This project was supported by Institutional Development Award Number U54GM115677 from the National Institute of General Medical Sciences of the National Institutes of Health, which funds Advance Clinical and Translational Research (Advance-CTR).
Acknowledgments
We would like to thank the individuals who assisted with data collection, participant recruitment, and transcript coding: Nicholas Jones, PhD; Katherine Brown, MSN, RN; Alexandra Howe, BA; Mary Kathryn Cancilliere, PhD; Crosby Modrowski, PhD; Margaret Maris, MPH; Maria Correa; Marylu Gonzales; Rosa Sierra, BA; Philip Chan, MD, MS; and Amy Nunn, MS, ScD. We would also like to thank the 55 members of the local Latine/Hispanic community who shared their time and thoughts with us, and the clinical experts who worked to support them through the pandemic.
Conflict of interest
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
Publisher's note
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
References
1. McWilliams C, Bothwell L, Yousey-Hindes K, Hadley JL. Trends in disparities in COVID hospitalizations among community-dwelling residents of two counties in Connecticut, before and after vaccine introduction, March 2020–September 2021. Influenza Other Respir Viruses. (2023) 17:1–9. doi: 10.1111/irv.13082
2. Centers for Disease Control and Prevention. COVID Data Tracker. Atlanta, GA: U.S. Department of Health and Human Services, CDC (2025). Available online at: https://covid.cdc.gov/covid-data-tracker/#datatracker-home (Accessed May 16, 2025).
3. Gil RM, Touzard-Romo F, Sanchez MC, Pandita A, Kalligeros M, Mylona EK, et al. Characteristics and outcomes of Hispanic/Latinx patients with coronavirus disease 19 (COVID-19) requiring hospitalization in Rhode Island: a retrospective cohort study. Ann Epidemiol. (2021) 58:64–8. doi: 10.1016/j.annepidem.2021.03.003
4. Carethers JM. Insights into disparities observed with COVID-19. J Intern Med. (2021) 289:463–73. doi: 10.1111/joim.13199
5. Hadler J, Edmundson A, Luc C, Yousey-Hindes K. Race/ethnic disparities in COVID-19 hospitalizations stronger than socioeconomic ones during stay safe, stay home, New Haven and middlesex counties, March 1–May 8, 2020. Connecticut Epidemiol. (2020) 40(4):13–6.
6. National Institute for Health. RADX® Underserved Populations (RADx-UP). Bethesda, MD: National Institute for Health (2021). Available online at: https://www.nih.gov/research-training/medical-research-initiatives/radx/radx-programs#radx-underserved-populations-radx-up (Accessed May 16, 2025).
7. Pineros-Leano M, Perez-Flores NJ, Damian K, Rodrigues K, Ortiz G, Simonovich SD. Mental health disparities in latinx immigrant communities residing in the United States during COVID-19: implications for policy and practice. Front Public Health. (2022) 10:1000233. doi: 10.3389/fpubh.2022.1000233
8. Fitzpatrick E. Latino Leaders Alarmed by Report that 45 Percent of Rhode Islanders with Coronavirus are Latino. Boston, MA: Boston Globe (2020). Available online at: https://www.bostonglobe.com/2020/04/17/metro/latino-leaders-alarmed-by-report-that-45-rhode-islanders-with-covid-19-are-latino/ (Accessed June 15, 2023).
9. Weng CH, Saal A, McGuire DC, Chan PA. Persistently high SARS-CoV-2 positivity rate and incidence for Hispanic/Latinos during state reopening in an urban setting: a retrospective cohort study. Epidemiol Infect. (2021) 149(e25):1–4. doi: 10.1017/S0950268821000133
10. Ayouni I, Maatoug J, Dhouib W, Zammit N, Ben Fredi S, Ghammam R, et al. Effective public health measures to mitigate the spread of COVID-19: a systematic review. BMC Public Health. (2021) 21:1015. doi: 10.1186/s12889-021-11111-1
11. Mercadante AR, Law AV. Will they, or won’t they? Examining patients’ vaccine intention for flu and COVID-19 using the health belief model. Res Soc Admin Pharm. (2021) 17:1596–605. doi: 10.1016/j.sapharm.2020.12.012
12. Ruiz JB, Bell RA. Predictors of intention to vaccinate against COVID-19: results of a nationwide survey. Vaccine. (2021) 39:1080–6. doi: 10.1016/j.vaccine.2021.01.010
13. Bateman LB, Hall AG, Anderson WA, Cherrington AL, Helova A, Judd S, et al. Exploring COVID-19 vaccine hesitancy among stakeholders in African American and latinx communities in the deep south through the Lens of the health belief model. Qual Res. (2022) 36(2):288–95. doi: 10.1177/08901171211045038
14. Balasuriya L, Santilli A, Morone J, Ainooson J, Roy B, Njoku A, et al. COVID-19 vaccine acceptance and access among black and latinx communities. JAMA Network Open. (2021) 4(10):e2128575. doi: 10.1001/jamanetworkopen.2021.28575
15. Jimenez ME, Rivera-Nunez Z, Crabtree BF, Hill D, Pellerano MB, Devance D, et al. Black and latinx community perspectives on COVID-19 mitigation behaviors, testing, and vaccines. JAMA Netw Open. (2021) 4(7):e2117074. doi: 10.1001/jamanetworkopen.2021.17074
16. Haboush-Deloye A, Marquez E, Dunne R, Pharr JR. Using community-based participatory research to understand the experiences of African American, native American, and latinx people during a pandemic. Prev Chronic Dis. (2023) 20(12):220152. doi: 10.5888/pcd20.220152
17. Wagner KM, Chatham AA, Prado K, Walsdorf AA, Villatoro AP, Garcia D, et al. Emotional wellbeing and coping among latinx young adults in the time of COVID-19. J Community Psychol. (2022) 51(3):1217–32. doi: 10.1002/jcop.22983
18. Parker RS, Le J, Doan A, Aguayo-Hiraldo P, Pannaraj PS, Rushing T, et al. COVID-19 outcomes in children, adolescents, and young adults with cancer. Cancer Epidemiol. (2022) 151(11):1913–24. doi: 10.1002/ijc.34202
19. Daily C, Gresh A, Hamilton ER, Marea CX. Adapting group prenatal care for telehealth: a COVID-era innovation to address barriers to care for latinx clients. J Midwifery Womens Health. (2024) 69(6):945–51. doi: 10.1111/jmwh.13701
20. Goldenberg RL, Naqvi S, Saleem S, Koso-Thomas M, McClure EM. COVID-19 Vaccination rates and vaccine hesitancy in pregnant women in seven low- and middle-income countries through May 2023: an observational study from the global network. BJOG. (2024) 132(3):387–8. doi: 10.1111/1471-0528.17977
21. Lalot F, Abrams D, Heering MS, Babaian J. Distrustful complacency and the COVID-19 vaccine: how concern and political trust interact to affect vaccine hesitancy. J Polit Psychol. (2023) 44(5):983–1011. doi: 10.1111/pops.12871
22. Jha A. Preparing the United States for the next pandemic. Ann Intern Med. (2023) 176(9):1277–8. doi: 10.7326/M23-1894
23. Matthew RA, Orpinas P, Calva A, Bermudez MJ, Darbisi C. Lazos hispanos: promising strategies and lessons learned in the development of a multisystem, community-based promotoras program. J Prim Prev. (2020) 41(3):229–43. doi: 10.1007/s10935-020-00587-z
24. Centers for Disease Control and Prevention. Promotores de Salud/Community Health Workers. Atlanta, GA: CDC (2019). Available online at: https://www.cdc.gov/minorityhealth/promotores/index.html (Accessed July 07, 2023).
25. Cherrington A, Ayala GX, Elder JP, Arredondo EM, Fouad M, Scarinci I. Recognizing the diverse roles of community health workers in the elimination of health disparities: from paid staff to volunteers. Ethn Dis. (2010) 20(2):189–94.20503902
26. Heisler M, Kaselitz E, Rana GK, Piette JD. Diabetes prevention interventions in Latin American countries: a scoping review. Curr Diab Rep. (2016) 16(9):80. doi: 10.1007/s11892-016-0778-7
27. Ferdinand KC, Patterson KP, Taylor C, Fergus IV, Nasser SA, Ferdinand DP. Community-based approaches to prevention and management of hypertension and cardiovascular disease. J Clin Hypertens. (2012) 14(5):336–43. doi: 10.1111/j.1751-7176.2012.00622.x
28. Hsieh HF, Shannon SE. Three approaches to qualitative content analysis. Qual Health Res. (2005) 15(9):1277–88. doi: 10.1177/1049732305276687
29. Damschroder LJ, Reardon CM, Opra Widerquist MA, Lowery J. The updated consolidated framework for implementation research based on user feedback. Implement Sci. (2022) 17:75. doi: 10.1186/s13012-022-01245-0
30. NVivo. Burlington, MA: QSR International Pty Ltd (2022). Available online at: https://www.qsrinternational.com/nvivo-qualitative-data-analysis-software/home (Accessed February 04, 2023).
31. Braun V, Clarke V. Using thematic analysis in psychology. Qual Res Psychol. (2006) 3(2):77–101. doi: 10.1191/1478088706qp063oa
32. Martinez LS, Sharma N, John J, Battaglia TA, Linas BP, Clark CR, et al. Long COVID impacts: the voices and views of diverse black and latinx residents in Massachusetts. BMC Public Health. (2024) 42:2265. doi: 10.1186/s12889-024-19567-7
33. Nusbaum NJ. The COVID vaccine hesitancy epidemic. J Community Health. (2024) 49:377–8. doi: 10.1007/s10900-024-01350-9
34. Braun V, Clarke V. Chapter Twelve: Quality Criteria and Techniques for Qualitative Research. in: Successful Qualitative Research: A Practical Guide for Beginners. 1st Eds London, UK: SAGE Publications Ltd (2013).
35. Solomon DH, Bucala R, Kaplan MJ, Nigrovic PA. The “infodemic” of COVID-19. Arthritis Rheumatol. (2020) 72(11):1806–8. doi: 10.1002/art.41468
36. Elwy AR, Maguire EM, Kim B, West GS. Involving stakeholders as communication partners in research dissemination efforts. J Gen Intern Med. (2022) 37(Suppl 1):123–7. doi: 10.1007/s11606-021-07127-3
37. Ramanadhan S, Davis MM, Armstrong R, Baquero B, Ko LK, Leng JC, et al. Participatory implementation science to increase the impact of evidence-based cancer prevention and control. Cancer Causes Control. (2018) 29(3):363–9. doi: 10.1007/s10552-018-1008-1
38. Waltz TJ, Powell BJ, Fernández ME, Abadie B, Damschroder LJ. Choosing implementation strategies to address contextual barriers: diversity in recommendations and future directions. Implement Sci. (2019) 14(1):42. doi: 10.1186/s13012-019-0892-4
39. Cadenas GA, Cerezo A, Carlos Chavez FL, Capielo Rosario C, Torres L, Suro B, et al. The citizenship shield: mediated and moderated links between immigration status, discrimination, food insecurity, and negative health outcomes for latinx immigrants during the COVID-19 pandemic. J Community Psychol. (2023) 51:2355–71. doi: 10.1002/jcop.22831
40. Valdez CR, Walsdorf AA, Wagner KM, Salgado de Snyder NV, Garcia D, Villatoro AP. The intersection of immigration policy impacts and COVID-19 for latinx young adults. Am J Community Psychol. (2022) 70:420–32. doi: 10.1002/ajcp.12617
41. Nuori S, Tan CH, Rangel M, Wertz M, Sanchez A, Alvarado A, et al. “Advocating for what we need”: a CBPR approach to advance care planning in the latinx older adult community. J Am Geriatr Soc. (2023) 71:2601–14. doi: 10.1111/jgs.18236
42. Rodriguez NM, Casanova F, Pages G, Claure L, Pedreira M, Touchton M, et al. Community-based participatory design of a community-health worker breast cancer training intervention for South Florida latinx farmworkers. PLoS One. (2020) 15(10):e0240827. doi: 10.1371/journal.pone.0240827
43. De las Nueces D, Hacker K, DiGirolamo A, LeRoi SH. A systematic review of community-based participatory research to enhance clinical trials in racial and ethnic minority groups. Health Serv Res. (2012) 47(3 Pt 2):1363–86. doi: 10.1111/j.1475-6773.2012.01386.x
44. Molassiotis A, Xie YJ, Leung AYM, Ho GWK, Li Y, Leung PHM, et al. A community-based participatory research approach to developing and testing social and behavioural interventions to reduce the spread of SARS-CoV-2: a protocol for the ‘COPAR for COVID’ programme of research with five interconnected studies in the Hong Kong context. Int J Environ Res Public Health. (2022) 19(20):13392. doi: 10.3390/ijerph192013392
45. De Anda S, Budd EL, Halvorson S, Mauricio AM, McWhirter EH, Cioffi CC, et al. Effects of a health education intervention for COVID-19 prevention in latinx communities: a cluster-randomized controlled trial. Am J Public Health. (2022) 112(S9):S923–7. doi: 10.2105/AJPH.2022.307129
46. Dell’Imperio SG, Aboul-Hassan D, Batchelor R, Chambers-Peeple K, Clauw DJ, DeJonckcheere M, et al. Vaccine perceptions among black adults with long COVID. Ethn Health. (2023) 28(6):853–73. doi: 10.1080/13557858.2023.2191914
47. Rhode Island Quality Institute. About: Mission and Vision. Providence, RI: Rhode Island Quality Institute (2021). Available online at: https://riqi.org/about/ (Accessed May 20, 2025).
Keywords: COVID-19, Latine/Hispanic, implementation science, health disparities, health behaviors, qualitative methods
Citation: Smith DG, Duarte-Velez Y, Chen ES, Bueno M, Elwy AR and Sarkar IN (2025) Barriers and facilitators to COVID-19 testing and vaccination: a qualitative focus group study among Rhode Island’s Latine/Hispanic community. Front. Health Serv. 5:1473375. doi: 10.3389/frhs.2025.1473375
Received: 30 July 2024; Accepted: 14 July 2025;
Published: 29 July 2025.
Edited by:
Nick Sevdalis, National University of Singapore, SingaporeReviewed by:
Shafayat Sultan, University of Dhaka, BangladeshShefaly Shorey, National University of Singapore, Singapore
Copyright: © 2025 Smith, Duarte-Velez, Chen, Bueno, Elwy and Sarkar. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Indra Neil Sarkar, bmVpbF9zYXJrYXJAYnJvd24uZWR1
 D. Grace Smith
D. Grace Smith Yovanska Duarte-Velez
Yovanska Duarte-Velez Elizabeth S. Chen
Elizabeth S. Chen Mario Bueno5
Mario Bueno5 A. Rani Elwy
A. Rani Elwy Indra Neil Sarkar
Indra Neil Sarkar