- Department of Surgery, Banbuntane Houtokukai Hospital, Fujita Health University School of Medicine, Nagoya, Japan
Hepatocellular carcinoma (HCC) is the most common primary liver malignancy. The association of HCC with chronic liver disease (CLD) is well known and making treatment complex and challenging. The treatment of HCC must take into consideration, the severity of CLD, the stage of HCC, and the clinical condition of the patient. Liver resection (LR) is one of the most efficient treatments for patients with HCC. Better liver function assessment, increased understanding of segmental liver anatomy using more accurate imaging studies, and surgical technical progress are the important factors that have led to reduced mortality, with an expected 5 year survival of 38–61% depending on the stage of the disease. However, the procedure is applicable to <30% of all HCC patients, and 80% of the patients after LR recurred within 5 years. There are recent advances and prospects in LR for HCC in several aspects. Three-dimensional computed tomography imaging assisted preoperative surgical planning facilitates unconventional types of LR. Emerging evidences of laparoscopic hepatectomy and prospects for the use of newly developing chemotherapies as a combined therapy may lead to expanding indication of LR. LR and liver transplantation could be associated rather than considered separately with the current concepts of “bridging LR” and “salvage transplantation.”
Introduction
Hepatocellular carcinoma (HCC) is the sixth most common cancer and the most common primary liver malignancy (1). The association of HCC with chronic liver disease (CLD), due to viral infection, alcohol consumption, metabolic syndrome, etc., is well known and making treatment complex and challenging. The underlying liver parenchyma displays various histological changes, including steatosis, inflammation, and fibrosis to cirrhosis. These histological changes of the underlying parenchyma and the risk of multicentric carcinogenesis from chronically injured liver tissue limit the possibility of curative treatments, which include local ablation of small size and number tumors, liver resection (LR), and liver transplantation (LT) (2).
Liver resection is one of the most efficient treatments for HCC patients (3, 4). Considerable progress observed during the last 10 years in screening, treatment of the underlying liver disease, early radiological diagnosis, and surgical techniques has updated the indications for LR (2). Better liver function assessment, understanding of segmental liver anatomy using more accurate imaging studies, and surgical technical progress are the most important factors that have led to reduced mortality, with an expected 5-year survival of 38–61% depending on the stage of the disease (5). However, only <30% of patients with HCC are eligible for surgery (3, 4). Emerging evidences of laparoscopic hepatectomy and prospects for the use of newly developing chemotherapies as a combined therapy may lead to expanding indication of LR (6, 7).
In this review, we present recent advances in LR of HCC.
Current Concept of Liver Resection for Hepatocellular Carcinoma
The largest report of LR for HCC is from the Liver Cancer Study Group in Japan, which has reported 1-, 3-, 5-, and 10-year survival rates of 85, 64, 45, and 21%, respectively, in 6,785 cirrhotic patients treated by LR between 1988 and 1999 (8). Comparable results have been reported by other groups worldwide without differences between Western and Eastern countries. Survival rates as high as 60% at 5 years could have been achieved in Child-Pugh A patients with well-encapsulated tumors of ≤2 cm in diameter. Results from patients with good liver function and anatomical LR according to the architecture of the portal vein (although <10% of all patients) could be favorably compared with those from patients with LT.
There are several reports describing that anatomical LR for small solitary HCC achieve significantly better overall and disease-free survival than limited resections, without increasing the post-operative risk (9, 10). Intrahepatic metastasis of HCC along the portal vein and the presence of satellite nodules within 2 cm from the main nodule (11) are the basis of the concept for anatomical LR, complete removal of the tumor-bearing portal territory. Anatomical LR has the potential to remove undetected cancerous foci (portal vein metastases and satellite nodules) disseminated from the main tumor and is recommended in many reports if possible.
In patients with HCC, both tumor extension and severity of liver dysfunction influence the indication and extent of LR. When considering the treatment of HCC in patients with CLD, the degree of invasive surgical stress, especially to the impaired liver, should be considered in addition to the oncological therapeutic effects. Patients with severe CLD have various (overt and preliminary) symptoms, such as (1) deteriorations of protein synthesis and metabolism; (2) GI tract congestion, ascites, and pancytopenia due to portal hypertension and hypersplenism; and (3) susceptibility to infectious diseases and hepatopulmonary syndrome (hypoxemia) due to increased shunt vessels (12). Cirrhotic patients have high morbidity and mortality following anesthesia and surgery (13), and the risk of abdominal operations increases according to the preoperative Child-Pugh classification (14) of the patients (15). Major histological changes observed in patients with HCC include fibrosis ranging from mild (F1) to cirrhosis (F4). Latter stages of cirrhosis also have a lower rate of regeneration after LR, more frequent association with portal hypertension, and higher risk of tumor multiplicity/recurrence (16, 17). Steatosis and the inflammatory process also have a significant influence on the course after LR, even absence of extensive fibrosis. LR in diseased parenchyma presents operative risk due to altered texture of the liver parenchyma, impaired liver regeneration, and deteriorated liver function leading to coagulation defects, an increased risk of infection, etc. (18). There is a close relationship between the extent of resected liver volume and post-operative morbidity/mortality of LR in patients with CLD. The fact limits the indication of LR for large tumors or small but centrally located tumors (19). The most difficult point of LR in patients with HCC and CLD is that it should be curative with the resection of the tumor vascular territories and also preserve as much liver volume as possible to prevent post-operative liver failure.
Assessment and Modulation of Remnant Liver Function
Small remnant liver volume is associated with poor post-operative liver function and a high mortality/morbidity after LR (20). Although the safety limit for the remnant liver volume in patients with normal liver is approximately 30% of the total liver volume (TLV), it is generally thought that a remnant liver volume of 40–50% should be preserved after major LR in patients with CLD. The liver is characterized by its capacity to ensure apparent normal liver function with a reduced functional volume and its ability to regenerate. However, the ability to regeneration varies depending on factors such as fibrosis of remnant liver, portal flow, etc. Thus, adequate volume of future liver remnant (FLR) should be different in each individual patient. Although the aim of preoperative assessment of liver function is to prevent post-operative liver failure in each individual patient, the assessments for the post-operative functionality of a reduced-volume FLR and its capacity to regenerate is difficult. Because there are no valuable stress tests to assess the potential of liver function, preoperative assessment in patients with CLD involves joint interpretation of several biological, morphological, histological, and hemodynamic factors.
One widely used method of biological assessment is the Child-Pugh classification (11), which was originally designed for predicting the prognosis of patients with portal hypertension undergoing shunting operations. Resection is contraindicated in grade C cirrhotic patients and restricted to very limited resection in grade B cirrhotic patients (21). However, even in grade A cirrhotic patients with apparently normal liver function, the risk of liver surgery is increased, necessitating the development of more sophisticated quantitative liver function tests. Among the various methods available, the indocyanine green (ICG) clearance rate represents the most common test for predicting mortality after hepatectomy (22, 23). The normal ICG value in healthy patients is approximately 10%, and cutoff values predictive of safe major hepatectomies range from 14 to 17% (24, 25). Minor resections can be performed for values up to 22% (26), limited hepatectomies for values up to 40% (19), and limited wedge laparoscopic resections, in the opinion of some researchers, can be tolerated for even higher values (27, 28). The model for end-stage liver disease (MELD) score was validated as an accurate predictor of survival among different populations of patients with advanced liver disease (29, 30). In the case of LR, the impact of the MELD score was studied only retrospectively in some series of cirrhotic patients, who had undergone LR for HCC. In two series of cirrhotic patients who underwent LR for HCC, the authors showed that a MELD score >8 was associated with a higher risk of mortality, morbidity, and impaired long-term survival (29, 30).
Preoperative portal vein embolization (PVE) was first introduced by Makuuchi et al. (28) and widely recognized as an effective method for preoperative volume modulation for small FLR. However, the degree of hypertrophy of the FLR after PVE is variable in patients with CLD (20, 31). It is generally accepted that the absence of early hypertrophy of a non-embolized liver following technically successful PVE is an indicator of low regenerative capacity that would contraindicate LR, and thus, the response represents a real dynamic stress test before major LR (32). It has been shown that sequential selective transarterial chemoembolization (TACE) before PVE increases the rate of hypertrophy (32, 33). In the event of inadequate FLR hypertrophy that precludes LR, this combined vascular obstruction of the tumor territory represents an efficient treatment of HCC. As other means of anticipating post-operative liver failure, there are several reports using the volumetry data from computed tomography (CT) for the evaluations of the FLR volume in the proportion of body weight, body surface area, and TLV (34, 35), the hypertrophy rate of the FLR/TLV ratio (36), etc.
Anatomical Resection and Imaging
The anatomical territory of HCC ranges from subsegment to lobe according to the size and location of the tumor. Anatomical resections of small solitary HCCs achieve significantly better overall and disease-free survival than do limited resections, without increasing the post-operative risk (9, 10). However, the benefit of segmental resection may only become apparent in tumors between 2 and 5 cm. For the tumors <2 cm in size, the risk of dissemination is considered to be negligible with equivalent efficacy of local ablative therapy; for the tumors more than 5 cm, majority of patients will already have macroscopic vascular invasion or satellite nodules that lead to a high incidence of recurrence (37). In the case of central tumors with undefined vascular territory, some authors have found lower recurrence rates and greater survival with 2-cm surgical margins compared with 1-cm margins (38), and other authors have found no difference between margins <1 or >1 cm (39, 40). The adequate margin of LR should also depend on the tumor type (with/without capsules, with/without invasion outside the capsule, etc.) and still under discussion. Three-dimensional CT-assisted preoperative surgical planning allows determination of resectability and changes in operative strategy (resection modifications/extensions/intrahepatic vascular reconstructions studying portal distribution, hepatic vein anatomy for adequate venous drainage, biliary distribution for avoiding biliary fistula) (41). This preoperative assessment seems particularly helpful in patients with unconventional resection planes and in those with central tumors. It allows complicated anatomical LR being adapted to more number of patients, such as subsegment anatomical LR for small tumor in highly injured liver and anatomical LR of combined territories for deep centrally located tumor on the border of territories.
Laparoscopic LR
Since the first successful report in 1992 (42), laparoscopic LR is thought to be a less invasive procedure than conventional open LR for the treatment of hepatic lesions (43). In a comprehensive meta-analysis study, laparoscopic LR was compared to open in 1,678 patients across 26 studies (44). While it is associated with longer operating times and no differences in oncological outcomes, it is advantageous in several aspects. Laparoscopic LR is associated with reduced blood loss, decreased portal clamp time, decreases in overall and liver-specific complications, and shorter post-operative hospital stays. Recent technological development of devices and accumulation of experiences have facilitated the expansion of the indication of the procedure (6, 45). Although common advantages of laparoscopic surgery, such as early recovery and discharge with smaller post-operative pain and earlier intake, have also been reported for laparoscopic hepatectomy (46), specific advantages and the indication of laparoscopic LR have yet to be well settled.
Even limited LR under open surgery for severe CLD patients often develops refractory ascites, which leads to fatal complications (47, 48). Laparoscopic LR may be particularly advantageous for those patients, given the potential for lower levels of parietal and hepatic injury and the preservation of venous and lymphatic collateral circulation, especially for the patients with multicentric/metachronous lesions occurring in chronically injured liver. The safety and feasibility of the laparoscopic approach and its short-term benefits for HCC patients with CLD have been demonstrated by several series. To date, several studies have investigated the major differences between laparoscopic LR and open LR (49–59). Favorable short-term results, including fewer incidences of ascites and liver failure, and shorter post-operative hospital stay correlates with the laparoscopic procedure. Tranchart et al. reported laparoscopic LR of HCC for selected patients resulted in better post-operative outcomes without long- and short-term oncologic consequences (60). Also in our experience (61), we reported the favorable perioperative course of the patients with severe CLD (Child B/C and ICG R15 of 40% or above) who underwent pure laparoscopic LR, which is comparable to that of the patients with mild/moderate CLD (Child A and ICG R15 of 10.1–27.4%). This study showed that laparoscopic LR has the advantage of minimal ascites (61) in addition to usual advantages of laparoscopic surgery, due to the preservation of venous and lymphatic collateral circulation, which leads to lower risk of disturbance in water and/or electrolyte balance and hypoproteinemia that could trigger fatal liver failure. This feature could be the most remarkable specific advantage for laparoscopic LR. Patients who undergo LR are exposed to three different types of stresses: (1) general, whole-body surgical stress, (2) reduced liver function due to resected liver volume, and (3) surgery-induced injury for liver parenchyma and environment around the liver caused by destruction of the collateral blood/lymphatic flow by laparotomy plus mobilization of the liver and parenchymal injury by compression of the liver. Reduction of the third mentioned stress by laparoscopic LR should lower the risk for HCC patients with severe CLD. Among these patients with severe CLD in our series, one underwent living-related LT 20 months after hepatectomy (28). The procedure could also be an advantageous option in bridging therapy to LT for certain HCC patients with severe CLD. Furthermore, our experience showed laparoscopic LR also results in improved vision and manipulation in a small operative field under several conditions, such as repeat hepatectomy with adhesions (28) and, also, some novel approach of LR [for example, caudal approach, not anterior approach, for oncologically appropriate posterior sectorectomy and right hepatectomy (62)] is also possible laparoscopically. These characteristics of laparoscopic LR may indicate that it is a superior method when compared to open LR under certain conditions and its application may lead to expanding indication of LR.
Adjuvant and/or Combined Therapy for LR
Recurrence after LR occurs in up to 80% of patients at 5 years (63). Two-year cutoff has been raised to distinguish between early and late recurrence. Two-thirds of the recurrence occurs within 2 years, which is considered as dissemination from the original tumor (64). The factors related to this recurrence are tumor size, microvascular invasion, satellite nodules, α-fetoprotein levels, and non-anatomical resection. Large portion of delayed recurrence may correspond to “de novo” tumors in the oncogenic CLD liver (65). Presence of cirrhosis (F4), hepatitis activity, and multinodularity are in the risk factors associated with delayed recurrence, besides vascular invasion, and moderate or poorly differentiated HCC (64).
Several strategies have been tested to prevent recurrence, such as preoperative chemoembolization (66), chemotherapy, internal radiation (67), adoptive immunotherapy (68), retinoids (69), or interferon. Three meta-analyses that favored the use of interferon have been published (70, 71), although there are few good-quality studies. Whether there is definite efficacy of the agent and, if there is, also whether the effect of interferon works on early recurrence as an anti-cancerous agent or on delayed recurrence through the control of CLD activity are still under discussion. The efficacy of sorafenib in advanced stages has encouraged evaluation of this agent at earlier phases of the disease, and the trials are ongoing. There is no proven neoadjuvant therapy that can decrease or delay the incidence of intrahepatic recurrence after LR (72). Despite the facts that TACE can downstage HCC, prospective trials have failed to show any significant benefit of this treatment before LR (73, 74). Although recurrence following LR is associated with a poor outcome in most cases, there is growing evidence that some patients with only intrahepatic recurrence will benefit from more aggressive approaches (75, 76). Multimodality therapy of recurrence, including TACE, percutaneous ablative therapy, and re-resection could result in prolonged survival, with an overall 5-year survival rate of 20% (75).
Vascular invasion of HCC, particularly portal and hepatic venous tumor thrombus (VTT), is one of the indicators of patient prognosis and development of tumor thrombi in a major branch of the veins is a frequent terminal feature of HCC. The prognosis of such patients is extremely poor, and survival is limited to a few months after diagnosis (77–79). For these advanced HCCs, conventional therapies like TACE and percutaneous ablative therapy are not indicated due to lack of efficacy and associated complications (80, 81). LT is a contra-indication for such cases (80). Several reports have mentioned the feasibility of LR for patients with VTT. However, the outcome is unsatisfactory with median survival of 6–12 months (77, 78, 81, 82), except for the cases with VTT located in the segmental or sectoral branches (83). Several approaches have been attempted to improve the surgical results, including combined radiotherapy and TACE to date with unsatisfactory results (84–87). There are recently emerging reports that the clinical efficiency of IFN-α plus transarterial 5-fluorouracil (5-FU) combination therapy for advanced HCC with VTT and intrahepatic metastasis (88–90) and also for resectable HCC as a post-operative adjuvant (91) and a multimodal treatment (7). The results show that this combination therapy with LR is a promising candidate for the treatment of such condition and other advanced cases. Now, several clinical trials for this combination therapy are ongoing. We also previously reported the efficacy of S-1 plus cisplatin combination therapy for the patients with advanced and/or recurrent primary liver carcinomas including HCC (92) and of TACE using degradable starch microspheres (DSM) in patients with liver tumors (93). This chemoembolization using DSM induces only short-term temporary vascular occlusion and chemotherapeutic agent retention on the site, which is applicable repeatedly in short interval with mild damage on the vessels and non-cancerous liver tissue (93). The potential candidates of adjuvant and/or combined therapy for LR should be tested for the future improvement of prognosis in recurrent and/or advanced patients.
Liver Resection and Liver Transplantation
Impairment of liver function and the risk of multicentric carcinogenesis from chronically injured liver tissue lead to consideration of LT as the ideal treatment for removal of existing tumors and injured/preneoplastic underlying liver. Furthermore, it also prevents the development of post-operative complications associated with portal hypertension and liver failure. LT is not limited by liver function, and in selected patients with limited tumors, survival is similar to LT for other indications (94, 95). However, it became evident that patients with extensive HCC had very poor outcomes, whereas most patients with small tumor load could be cured. Thus, there are discussions for the LT in patients with HCC about the matters, such as the selection of patients in the background of the organ shortage, control of tumors for patients on the waiting list (96).
On the waiting list for LT, HCC patients can experience tumor growth beyond the LT criteria and a high cumulative probability of drop-out from the waiting list. This probability has been reported to range between 7 and 11% at 6 months and to be approximately 38% at 12 months after enrollment by two reports at the late 1990s (97, 98).
Belghiti et al. have demonstrated that surgical resection before LT (“bridging LR”) does not increase the surgical risk nor impair survival (99) and stated that resection and transplantation could be associated rather than considered separately. They mentioned that resection could be used as a bridge to transplantation, especially for tumors located in the upper part of the right liver, which can be easily and completely removed through a transthoracic incision. Similarly, some superficial tumors that are not easily accessible by a percutaneous approach could be resected through a laparoscopic approach.
Several studies have confirmed that LT for recurrence after LR did not increase the operative risk and offered a chance of long-term survival when HCC recurrence was limited (99–101). Initial LR of HCC as primary therapy in patients, who otherwise could have been transplanted offers good quality of life and is less demanding than LT. Patients do not need long-term immunosuppression; in addition, grafts are saved for the community and can be transplanted to other patients with no alternative to LT (99, 100, 102). “Salvage transplantation” was first proposed by Majno et al. (103) for tumor recurrence or deterioration in liver function of the patients after LR as primary therapy. This concept seems to be applicable in a significant proportion of patients with long-term survival similar to that of patients who undergo primary LT (99–101). Also, histological analysis of specimens from LR, either in “bridging” or “salvage” setting, allows to show pejorative factors of the tumor, which lead to a valid selection of the subgroup of patients who could benefit from following LT.
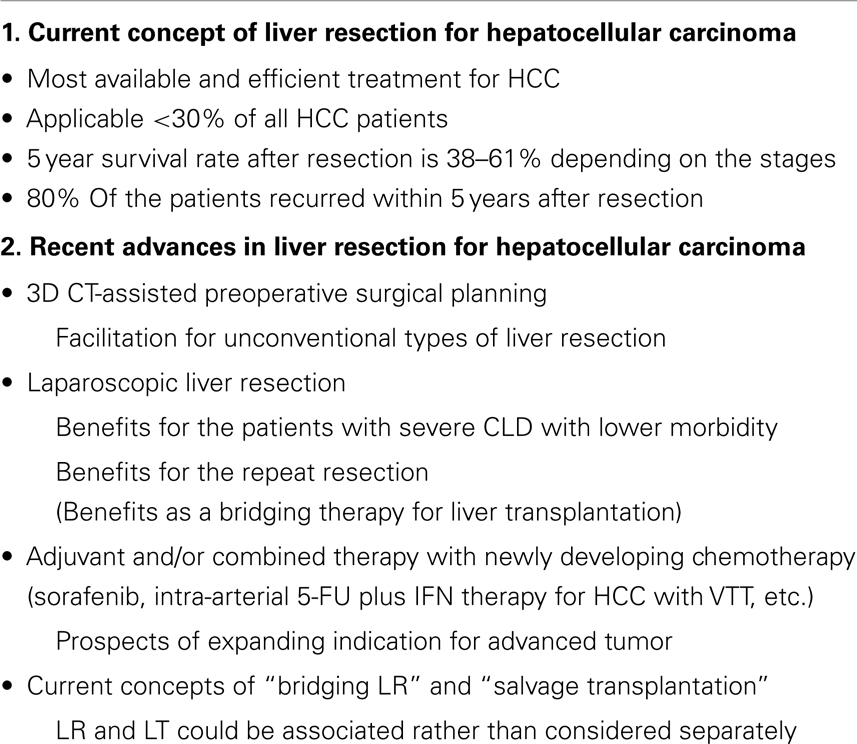
Conclusion (Table 1)
The association of HCC with CLD is making treatment complex and challenging. The treatment of HCC must take into consideration, the severity of CLD, the stage of HCC, and the clinical condition of the patient.
There are recent advances and prospects in LR for HCC in several aspects. Three-dimensional CT imaging assisted preoperative surgical planning facilitates unconventional types of LR. Emerging evidences of laparoscopic hepatectomy and prospects for the use of newly developing chemotherapies as a combined therapy may lead to expanding indication of LR.
Liver resection and LT could be associated rather than considered separately with the current concepts of “bridging LR” and “salvage transplantation.”
Author Contributions
Zenichi Morise wrote the manuscript; Norihiko Kawabe, Hirokazu Tomishige, Hidetoshi Nagata, Jin Kawase, Satoshi Arakawa, Rie Yoshida, and Masashi Isetani collected the data and assisted in writing of the manuscript.
Conflict of Interest Statement
We or our institution at any time did not receive any payment or services from a third party for any aspect of the submitted work. There is no financial relationship with entities that could be perceived to influence, or that give the appearance of potentially influencing, what we wrote in the submitted work. There are no patent and copyright, whether pending, issued, licensed, and/or receiving royalties relevant to the work. There is no other relationship or activity that readers could perceive to have influenced, or that give the appearance of potentially influencing, what we wrote in the submitted work.
References
1. Ferlay J, Shin HR, Bray F, Forman D, Mathers C, Parkin DM. Estimates of worldwide burden of cancer in 2008: GLOBOCAN 2008. Int J Cancer (2010) 127:2893–917. doi: 10.1002/ijc.25516
2. Rahbari NN, Mehrabi A, Mollberg NM, Muller SA, Koch M, Buchler MW, et al. Hepatocellular carcinoma: current management and perspectives for the future. Ann Surg (2011) 253:453–69. doi:10.1097/SLA.0b013e31820d944f
3. El-Serag HB, Marrero JA, Rudolph L, Reddy KR. Diagnosis and treatment of hepatocellular carcinoma. Gastroenterology (2008) 134:1752–63. doi:10.1053/j.gastro.2008.02.090
4. Forner A, Reig ME, de Lope CR, Bruix J. Current strategy for staging and treatment: the BCLC update and future prospects. Semin Liver Dis (2010) 30:61–74. doi:10.1055/s-0030-1247133
5. Torzilli G, Belghiti J, Kokudo N, Takayama T, Capussotti L, Nuzzo G, et al. A snapshot of the effective indications and results of surgery for hepatocellular carcinoma in tertiary referral centers: is it adherent to the EASL/AASLD recommendations?: an observational study of the HCC East-West study group. Ann Surg (2013) 257:929–37. doi:10.1097/SLA.0b013e31828329b8
6. World Consensus Conference on Laparoscopic Surgery. The international position on laparoscopic liver surgery: the Louisville statement, 2008. Ann Surg (2009) 250(5):825–30. doi:10.1097/SLA.0b013e3181b3b2d8
7. Nagano H, Miyamoto A, Wada H, Ota H, Marubashi S, Takeda Y, et al. Interferon-alpha and 5-fluorouracil combination therapy after palliative hepatic resection in patients with advanced hepatocellular carcinoma, portal venous tumor thrombus in the major trunk, and multiple nodules. Cancer (2007) 110(11):2493–501. doi:10.1002/cncr.23033
8. Ikai I, Itai Y, Okita K, Omata M, Kojiro M, Kobayashi K, et al. Report of the 15th follow-up survey of primary liver cancer. Hepatol Res (2004) 28:21–9. doi:10.1016/j.hepres.2003.08.002
9. Imamura H, Matsuyama Y, Miyagawa Y, Ishida K, Shimada R, Miyagawa S, et al. Prognostic significance of anatomical resection and des-gamma-carboxy prothrombin in patients with hepatocellular carcinoma. Br J Surg (1999) 86:1032–8. doi:10.1046/j.1365-2168.1999.01185.x
10. Wakai T, Shirai Y, Sakata J, Kaneko K, Cruz PV, Akazawa K, et al. Anatomic resection independently improves long-term survival in patients with T1-T2 hepatocellular carcinoma. Ann Surg Oncol (2007) 14:1356–65. doi:10.1245/s10434-006-9318-z
11. Roayaie S, Blume IN, Thung SN, Guido M, Fiel MI, Hiotis S, et al. A system of classifying microvascular invasion to predict outcome after resection in patients with hepatocellular carcinoma. Gastroenterology (2009) 137:850–5. doi:10.1053/j.gastro.2009.06.003
12. Hoeper MM, Krowka MJ, Strassburg CP. Portopulmonary hypertension and hepatopulmonary syndrome. Lancet (2004) 363(9419):1461–8. doi:10.1016/S0140-6736(04)16107-2
13. Ziser A, Plevak DJ, Wiesner RH, Rakela J, Offord KP, Brown DL. Morbidity and mortality in cirrhotic patients undergoing anesthesia and surgery. Anesthesiology (1999) 90(1):42–53. doi:10.1097/00000542-199901000-00008
14. Pugh RN, Murray-Lyon IM, Dawson JL, Pietroni MC, Williams R. Transection of the oesophagus for bleeding oesophageal varices. Br J Surg (1973) 60:646–9. doi:10.1002/bjs.1800600817
15. Mansour A, Watson W, Shayani V, Pickleman J. Abdominal operations in patients with cirrhosis: still a major surgical challenge. Surgery (1997) 122(4):730–5. doi:10.1016/S0039-6060(97)90080-5
16. Fuks D, Dokmak S, Paradis V, Diouf M, Durand F, Belghiti J. Benefit of initial resection of hepatocellular carcinoma followed by transplantation in case of recurrence: an intention-to-treat analysis. Hepatology (2012) 55:132–40. doi:10.1002/hep.24680
17. Poon RT, Fan ST, Lo CM, Liu CL, Wong J. Long-term survival and pattern of recurrence after resection of small hepatocellular carcinoma in patients with preserved liver function: implications for a strategy of salvage transplantation. Ann Surg (2002) 235:373–82. doi:10.1097/00000658-200203000-00009
18. Ishizawa T, Hasegawa K, Aoki T, Takahashi M, Inoue Y, Sano K, et al. Neither multiple tumors nor portal hypertension are surgical contraindications for hepatocellular carcinoma. Gastroenterology (2008) 134:1908–16. doi:10.1053/j.gastro.2008.02.091
19. Makuuchi M, Sano K. The surgical approach to HCC: our progress and results in Japan. Liver Transpl (2004) 10:S46–52. doi:10.1002/lt.20044
20. Farges O, Malassagne B, Flejou JF, Balzan S, Sauvanet A, Belghiti J. Risk of major liver resection in patients with underlying chronic liver disease: a reappraisal. Ann Surg (1999) 229:210–5. doi:10.1097/00000658-199902000-00008
21. Belghiti J, Regimbeau JM, Durand F, Kianmanesh AR, Dondero F, Terris B, et al. Resection of hepatocellular carcinoma: a European experience on 328 cases. Hepatogastroenterology (2002) 49:41–6.
22. Torzilli G, Makuuchi M, Inoue K, Takayama T, Sakamoto Y, Sugawara Y, et al. No-mortality liver resection for hepatocellular carcinoma in cirrhotic and noncirrhotic patients: is there a way? A prospective analysis of our approach. Arch Surg (1999) 134:984–92. doi:10.1001/archsurg.134.9.984
23. Wakabayashi H, Ishimura K, Izuishi K, Karasawa Y, Maeta H. Evaluation of liver function for hepatic resection for hepatocellular carcinoma in the liver with damaged parenchyma. J Surg Res (2004) 116:248–52. doi:10.1016/j.jss.2003.09.015
24. Fan ST, Lai EC, Lo CM, Ng IO, Wong J. Hospital mortality of major hepatectomy for hepatocellular carcinoma associated with cirrhosis. Arch Surg (1995) 130:198–203. doi:10.1001/archsurg.1995.01430020088017
25. Lam CM, Fan ST, Lo CM, Wong J. Major hepatectomy for hepatocellular carcinoma in patients with an unsatisfactory indocyanine green clearance test. Br J Surg (1999) 86:1012–7. doi:10.1046/j.1365-2168.1999.01204.x
26. Fan ST. Liver functional reserve estimation: state of the art and relevance for local treatments: the Eastern perspective. J Hepatobiliary Pancreat Sci (2010) 17:380–4. doi:10.1007/s00534-009-0229-9
27. Belli G, Fantini C, Belli A, Limongelli P. Laparoscopic liver resection for hepatocellular carcinoma in cirrhosis: longterm outcomes. Dig Surg (2011) 28:134–40. doi:10.1159/000323824
28. Morise Z, Kawabe N, Kawase J, Tomishige H, Nagata H, Ohshima H, et al. Pure laparoscopic hepatectomy for hepatocellular carcinoma with chronic liver disease. World J Hepatol (2013) 5(9):487–95. doi:10.4254/wjh.v5.i9.487
29. Hsu KY, Chau GY, Lui WY, Tsay SH, King KL, Wu CW. Predicting morbidity and mortality after hepatic resection in patients with hepatocellular carcinoma: the role of model for end-stage liver disease score. World J Surg (2009) 33:2412–9. doi:10.1007/s00268-009-0202-4
30. Delis SG, Bakoyiannis A, Biliatis I, Athanassiou K, Tassopoulos N, Dervenis C. Model for end-stage liver disease (MELD) score, as a prognostic factor for post-operative morbidity and mortality in cirrhotic patients, undergoing hepatectomy for hepatocellular carcinoma. HPB (Oxford) (2009) 11:351–7. doi:10.1111/j.1477-2574.2009.00067.x
31. Yamakado K, Takeda K, Matsumura K, Nakatsuka A, Hirano T, Kato N, et al. Regeneration of the un-embolized liver parenchyma following portal vein embolization. J Hepatol (1997) 27:871–80. doi:10.1016/S0168-8278(97)80325-X
32. Ogata S, Belghiti J, Farges O, Varma D, Sibert A, Vilgrain V. Sequential arterial and portal vein embolizations before right hepatectomy in patients with cirrhosis and hepatocellular carcinoma. Br J Surg (2006) 93:1091–8. doi:10.1002/bjs.5341
33. Yoo H, Kim JH, Ko GY, Kim KW, Gwon DI, Lee SG, et al. Sequential transcatheter arterial chemoembolization and portal vein embolization versus portal vein embolization only before major hepatectomy for patients with hepatocellular carcinoma. Ann Surg Oncol (2011) 18:1251–7. doi:10.1245/s10434-010-1423-3
34. Truant S, Oberlin O, Sergent G, Lebuffe G, Gambiez L, Ernst O, et al. Remnant liver volume to body weight ratio > or =0.5%: a new cut-off to estimate postoperative risks after extended liver resection in noncirrhotic liver. J Am Coll Surg (2007) 204:22–33. doi:10.1016/j.jamcollsurg.2006.09.007
35. Chun YS, Ribero D, Abdalla EK, Madoff DC, Mortenson MM, Wei SH, et al. Comparison of two methods of future liver remnant volume measurement. J Gastrointest Surg (2008) 12:123–8. doi:10.1007/s11605-007-0323-8
36. Farges O, Belghiti J, Kianmanesh R, Regimbeau JM, Santoro R, Vilgrain V, et al. Portal vein embolization before right hepatectomy: prospective clinical trial. Ann Surg (2003) 237:208–17. doi:10.1097/00000658-200302000-00010
37. Ueno S, Kubo F, Sakoda M, Hiwatashi K, Tateno T, Mataki Y, et al. Efficacy of anatomic resection vs nonanatomic resection for small nodular hepatocellular carcinoma based on gross classification. J Hepatobiliary Pancreat Surg (2008) 15:493–500. doi:10.1007/s00534-007-1312-8
38. Shi M, Guo RP, Lin XJ, Zhang YQ, Chen MS, Zhang CQ, et al. Partial hepatectomy with wide versus narrow resection margin for solitary hepatocellular carcinoma: a prospective randomized trial. Ann Surg (2007) 245:36–43. doi:10.1097/01.sla.0000231758.07868.71
39. Arii S, Tanaka S, Mitsunori Y, Nakamura N, Kudo A, Noguchi N, et al. Surgical strategies for hepatocellular carcinoma with special reference to anatomical hepatic resection and intraoperative contrast-enhanced ultrasonography. Oncology (2010) 78(Suppl 1):125–30. doi:10.1159/000315240
40. Poon RT, Fan ST, Ng IO, Lo CM, Liu CL, Wong J. Different risk factors and prognosis for early and late intrahepatic recurrence after resection of hepatocellular carcinoma. Cancer (2000) 89:500–7. doi:10.1002/1097-0142(20000801)89:3<500::AID-CNCR4>3.0.CO;2-O
41. Radtke A, Sotiropoulos GC, Molmenti EP, Schroeder T, Peitgen HO, Frilling A, et al. Computer-assisted surgery planning for complex liver resections: when is it helpful? A single-center experience over an 8-year period. Ann Surg (2010) 252:876–83. doi:10.1097/SLA.0b013e3181fdd012
42. Gagner M, Rheault M, Dubuc J. Laparoscopic partial hepatectomy for liver tumor. Surg Endosc (1992) 6:97–8.
43. Kaneko H, Tsuchiya M, Otsuka Y, Yajima S, Minagawa T, Watanabe M, et al. Laparoscopic hepatectomy for hepatocellular carcinoma in cirrhotic patients. J Hepatobiliary Pancreat Surg (2009) 16(4):433–8. doi:10.1007/s00534-009-0123-5
44. Mirnezami R, Mirnezami AH, Chandrakumaran K, Abu Hilal M, Pearce NW, Primrose JN, et al. Short- and long-term outcomes after laparoscopic and open hepatic resection: systematic review and meta-analysis. HPB (Oxford) (2011) 13(5):295–308. doi:10.1111/j.1477-2574.2011.00295.x
45. Tsuchiya M, Otsuka Y, Tamura A, Nitta H, Sasaki A, Wakabayashi G, et al. Status of endoscopic liver surgery in Japan: a questionnaire survey conducted by the Japanese endoscopic liver surgery study group. J Hepatobiliary Pancreat Surg (2009) 16(4):405–9. doi:10.1007/s00534-009-0119-1
46. Viganò L, Tayar C, Laurent A, Cherqui D. Laparoscopic liver resection: a systematic review. J Hepatobiliary Pancreat Surg (2009) 16(4):410–21. doi:10.1007/s00534-009-0120-8
47. Belghiti J, Hiramatsu K, Benoist S, Massault P, Sauvanet A, Farges O. Seven hundred forty-seven hepatectomies in the 1990s: an update to evaluate the actual risk of liver resection. J Am Coll Surg (2000) 191(1):38. doi:10.1016/S1072-7515(00)00261-1
48. Lai EC, Fan ST, Lo CM, Chu KM, Liu CL, Wong J. Hepatic resection for hepatocellular carcinoma. An audit of 343 patients. Ann Surg (1995) 221(3):291–8. doi:10.1097/00000658-199503000-00012
49. Morise Z. Pure laparoscopic hepatectomy for HCC patients. In: Lau WY, editor. Hepatocellular Carcinoma – Clinical Research. Zagreb: InTech (2012). p. 183–96.
50. Chen HY, Juan CC, Ker CG. Laparoscopic liver surgery for patients with hepatocellular carcinoma. Ann Surg Oncol (2008) 15(3):800–6. doi:10.1245/s10434-007-9749-1
51. Dagher I, Lainas P, Carloni A, Caillard C, Champault A, Smadja C, et al. Laparoscopic liver resection for hepatocellular carcinoma. Surg Endosc (2008) 22(2):372–8. doi:10.1007/s00464-007-9487-2
52. Kaneko H, Takagi S, Otsuka Y, Tsuchiya M, Tamura A, Katagiri T, et al. Laparoscopic liver resection of hepatocellular carcinoma. Am J Surg (2005) 189(2):190–4. doi:10.1016/j.amjsurg.2004.09.010
53. Cherqui D, Laurent A, Tayar C, Chang S, Van Nhieu JT, Loriau J, et al. Laparoscopic liver resection for peripheral hepatocellular carcinoma in patients with chronic liver disease: midterm results and perspectives. Ann Surg (2006) 243(4):499–506. doi:10.1097/01.sla.0000206017.29651.99
54. Shimada M, Hashizume M, Maehara S, Tsujita E, Rikimaru T, Yamashita Y, et al. Laparoscopic hepatectomy for hepatocellular carcinoma. Surg Endosc (2001) 15(6):541–4. doi:10.1007/s004640080099
55. Sarpel U, Hefti MM, Wisnievsky JP, Roayaie S, Schwartz ME, Labow DM. Outcome for patients treated with laparoscopic versus open resection of hepatocellular carcinoma: case-matched analysis. Ann Surg Oncol (2009) 16:1572–7. doi:10.1245/s10434-009-0414-8
56. Hu BS, Chen K, Tan HM, Ding XM, Tan JW. Comparison of laparoscopic vs open liver lobectomy (segmentectomy) for hepatocellular carcinoma. World J Gastroenterol (2011) 17:4725–8. doi:10.3748/wjg.v17.i42.4725
57. Ker CG, Chen JS, Kuo KK, Chuang SC, Wang SJ, Chang WC, et al. Liver surgery for hepatocellular carcinoma: laparoscopic versus open approach. Int J Hepatol (2011) 2011:596792. doi:10.4061/2011/596792
58. Endo Y, Ohta M, Sasaki A, Kai S, Eguchi H, Iwaki K, et al. A comparative study of the long-term outcomes after laparoscopy-assisted and open left lateral hepatectomy for hepatocellular carcinoma. Surg Laparosc Endosc Percutan Tech (2009) 19:e171–4. doi:10.1097/SLE.0b013e3181bc4091
59. Nguyen KT, Marsh JW, Tsung A, Steel JJ, Gamblin TC, Geller DA. Comparative benefits of laparoscopic vs open hepatic resection: a critical appraisal. Arch Surg (2011) 146:348–56. doi:10.1001/archsurg.2010.248
60. Tranchart H, Di Giuro G, Lainas P, Roudie J, Agostini H, Franco D, et al. Laparoscopic resection for hepatocellular carcinoma: a matched-pair comparative study. Surg Endosc (2010) 24(5):1170–6. doi:10.1007/s00464-009-0745-3
61. Morise Z, Sugioka A, Kawabe N, Umemoto S, Nagata H, Ohshima H, et al. Pure laparoscopic hepatectomy for hepatocellular carcinoma patients with severe liver cirrhosis. Asian J Endosc Surg (2011) 4(3):143–6. doi:10.1111/j.1758-5910.2011.00081.x
62. Tomishige H, Morise Z, Kawabe N, Nagata H, Ohshima H, Kawase J, et al. Caudal approach to pure laparoscopic posterior sectionectomy under the laparoscopy-specific view. World J Gastrointest Surg (2013) 5(6):173–7. doi:10.4240/wjgs.v5.i6.173
63. Torzilli G, Belghiti J, Kokudo N, Takayama T, Capussotti L, Nuzzo G, et al. A snapshot of the effective indications and results of surgery for hepatocellular carcinoma in tertiary referral centers: is it adherent to the EASL/AASLD recommendations?: an observational study of the HCC East-West study group. Ann Surg (2013) 257:929–37. doi:10.1097/SLA.0b013e31828329b8
64. Imamura H, Matsuyama Y, Tanaka E, Ohkubo T, Hasegawa K, Miyagawa S, et al. Risk factors contributing to early and late phase intrahepatic recurrence of hepatocellular carcinoma after hepatectomy. J Hepatol (2003) 38:200–7. doi:10.1016/S0168-8278(02)00360-4
65. Hoshida Y, Villanueva A, Kobayashi M, Peix J, Chiang DY, Camargo A, et al. Gene expression in fixed tissues and outcome in hepatocellular carcinoma. N Engl J Med (2008) 359:1995–2004. doi:10.1056/NEJMoa0804525
66. Zhou WP, Lai EC, Li AJ, Fu SY, Zhou JP, Pan ZY, et al. A prospective, randomized, controlled trial of preoperative transarterial chemoembolization for resectable large hepatocellular carcinoma. Ann Surg (2009) 249:195–202. doi:10.1097/SLA.0b013e3181961c16
67. Lau WY, Leung TW, Ho SK, Chan M, Machin D, Lau J, et al. Adjuvant intra-arterial iodine-131-labelled lipiodol for resectable hepatocellular carcinoma: a prospective randomised trial. Lancet (1999) 353:797–801. doi:10.1016/S0140-6736(98)06475-7
68. Takayama T, Sekine T, Makuuchi M, Yamasaki S, Kosuge T, Yamamoto J, et al. Adoptive immunotherapy to lower postsurgical recurrence rates of hepatocellular carcinoma: a randomised trial. Lancet (2000) 356:802–7. doi:10.1016/S0140-6736(00)02654-4
69. Muto Y, Moriwaki H, Ninomiya M, Adachi S, Saito A, Takasaki KT, et al. Prevention of second primary tumors by an acyclic retinoid, polyprenoic acid, in patients with hepatocellular carcinoma. Hepatoma Prevention Study Group. N Engl J Med (1996) 334:1561–7. doi:10.1056/NEJM199606133342402
70. Breitenstein S, Dimitroulis D, Petrowsky H, Puhan MA, Mullhaupt B, Clavien PA. Systematic review and meta-analysis of interferon after curative treatment of hepatocellular carcinoma in patients with viral hepatitis. Br J Surg (2009) 96:975–81. doi:10.1002/bjs.6731
71. Shen YC, Hsu C, Chen LT, Cheng CC, Hu FC, Cheng AL. Adjuvant interferon therapy after curative therapy for hepatocellular carcinoma (HCC): a meta-regression approach. J Hepatol (2010) 52:889–94. doi:10.1016/j.jhep.2009.12.041
73. Luo YQ, Wang Y, Chen H, Wu MC. Influence of preoperative transcatheter arterial chemoembolization on liver resection in patients with resectable hepatocellular carcinoma. Hepatobiliary Pancreat Dis Int (2002) 1: 523–6.
74. Schwartz JD, Schwartz M, Mandeli J, Sung M. Neoadjuvant and adjuvant therapy for resectable hepatocellular carcinoma: review of the randomised clinical trials. Lancet Oncol (2002) 3:593–603. doi:10.1016/S1470-2045(02)00873-2
75. Poon RT, Fan ST, O’Suilleabhain CB, Wong J. Aggressive management of patients with extrahepatic and intrahepatic recurrences of hepatocellular carcinoma by combined resection and locoregional therapy. J Am Coll Surg (2002) 195:311–8. doi:10.1016/S1072-7515(02)01226-7
76. Minagawa M, Makuuchi M, Takayama T, Kokudo N. Selection criteria for repeat hepatectomy in patients with recurrent hepatocellular carcinoma. Ann Surg (2003) 238:703–10. doi:10.1097/01.sla.0000094549.11754.e6
77. Asahara T, Itamoto T, Katayama K, Nakahara H, Hino H, Yano M, et al. Hepatic resection with tumor thrombectomy for hepatocellular carcinoma with tumor thrombi in the major vasculature. Hepatogastroenterology (1999) 46:1862–9.
78. Ohkubo T, Yamamoto J, Sugawara Y, Shimada K, Yamasaki S, Makuuchi M, et al. Surgical results for hepatocellular carcinoma with macroscopic portal vein thrombosis. J Am Coll Surg (2000) 191:657–60. doi:10.1016/S1072-7515(00)00740-7
79. Lee HS, Kim JS, Choi IJ, Chung JW, Park JH, Kim CY. The safety and efficacy of transcatheter arterial chemoembolization in the treatment of patients with hepatocellular carcinoma and main portal vein obstruction: a prospective controlled study. Cancer (1997) 79:2087–94.
80. Mazzaferro V, Regalia E, Doci R, Andreola S, Pulvirenti A, Bozzetti F, et al. Liver transplantation for the treatment of small hepatocellular carcinomas in patients with cirrhosis. N Engl J Med (1996) 334:693–700. doi:10.1056/NEJM199603143341104
81. Poon RT, Fan ST, Ng IO, Wong J. Prognosis after hepatic resection for stage IVA hepatocellular carcinoma: a need for reclassification. Ann Surg (2003) 237:376–83. doi:10.1097/01.SLA.0000055224.68432.80
82. Ikai I, Yamaoka Y, Yamamoto Y, Ozaki N, Sakai Y, Satoh S, et al. Surgical intervention for patients with stage IV-A hepatocellular carcinoma without lymph node metastasis proposal as a standard therapy. Ann Surg (1998) 227:433–9. doi:10.1097/00000658-199803000-00016
83. Shi J, Lai EC, Li N, Guo WX, Xue J, Lau WY, et al. Surgical treatment for hepatocellular carcinoma with portal vein tumor thrombus. Ann Surg Oncol (2010) 17:2073–80. doi:10.1245/s10434-010-0940-4
84. Tazawa J, Maeda M, Sakai Y, Yamane M, Ohbayashi H, Kakinuma S, et al. Radiation therapy in combination with transcatheter arterial chemoembolization for hepatocellular carcinoma with extensive portal vein involvement. J Gastroenterol Hepatol (2001) 16:660–5. doi:10.1046/j.1440-1746.2001.02496.x
85. Ishikura S, Ogino T, Furuse J, Satake M, Baba S, Kawashima M, et al. Radiotherapy after transcatheter arterial chemoembolization for patients with hepatocellular carcinoma and portal vein tumor thrombus. Am J Clin Oncol (2002) 25:189–93. doi:10.1097/00000421-200204000-00019
86. Minagawa M, Makuuchi M, Takayama T, Ohtomo K. Selection criteria for hepatectomy in patients with hepatocellular carcinoma and portal vein tumor thrombus. Ann Surg (2001) 233:379–84. doi:10.1097/00000658-200103000-00012
87. Peng BG, He Q, Li JP, Zhou F. Adjuvant transcatheter arterial chemoembolization improves efficacy of hepatectomy for patients with hepatocellular carcinoma and portal vein tumor thrombus. Am J Surg (2009) 198:313–8. doi:10.1016/j.amjsurg.2008.09.026
88. Sakon M, Nagano H, Dono K, Nakamori S, Umeshita K, Yamada A, et al. Combined intraarterial 5-fluorouracil and subcutaneous interferon-α therapy for advanced hepatocellular carcinoma with tumor thrombi in the major portal branches. Cancer (2002) 94:435–42. doi:10.1002/cncr.10246
89. Ota H, Nagano H, Sakon M, Eguchi H, Kondo M, Yamamoto T, et al. Treatment of hepatocellular carcinoma with major portal vein thrombosis by combined therapy with subcutaneous interferon-alpha and intra-arterial 5-fluorouracil; role of type 1 interferon receptor expression. Br J Cancer (2005) 93:57–64. doi:10.1038/sj.bjc.6602742
90. Nagano H, Wada H, Kobayashi S, Marubashi S, Eguchi H, Tanemura M, et al. Long-term outcome of combined interferon-α and 5-fluorouracil treatment for advanced hepatocellular carcinoma with major portal vein thrombosis. Oncology (2011) 80(1–2):63–9. doi:10.1159/000328281
91. Nagano H, Sakon M, Eguchi H, Kondo M, Yamamoto T, Ota H, et al. Hepatic resection followed by IFN-alpha and 5-FU for advanced hepatocellular carcinoma with tumor thrombus in the major portal branch. Hepatogastroenterology (2007) 54:172–9.
92. Morise Z, Sugioka A, Fujita J, Hoshimoto S, Kato T, Ikeda M. S-1 plus cisplatin combination therapy for the patients with primary liver carcinomas. Hepatogastroenterology (2007) 54:2315–8.
93. Morise Z, Sugioka A, Kato R, Fujita J, Hoshimoto S, Kato T. Transarterial chemoembolization with degradable starch microspheres, irinotecan, and mitomycin-C in patients with liver metastases. J Gastrointest Surg (2006) 10(2):249–58. doi:10.1016/j.gassur.2005.08.004
94. Llovet JM, Burroughs A, Bruix J. Hepatocellular carcinoma. Lancet (2003) 362:1907–17. doi:10.1016/S0140-6736(03)14964-1
95. Bruix J, Sherman M; Practice Guidelines Committee, American Association for the Study of Liver Diseases. Management of hepatocellular carcinoma. Hepatology (2005) 42:1208–36. doi:10.1002/hep.20933
96. Bruix J, Sherman M; American Association for the Study of Liver Diseases. Management of hepatocellular carcinoma: an update. Hepatology (2011) 53:1020–2. doi:10.1002/hep.24199
97. Llovet JM, Fuster J, Bruix J. Intention-to-treat analysis of surgical treatment for early hepatocellular carcinoma: resection versus transplantation. Hepatology (1999) 30:1434–40. doi:10.1002/hep.510300629
98. Yao FY, Bass NM, Nikolai B, Davern TJ, Kerlan R, Wu V, et al. Liver transplantation for hepatocellular carcinoma: analysis of survival according to the intention-to-treat principle and dropout from the waiting list. Liver Transpl (2002) 8:873–83. doi:10.1053/jlts.2002.34923
99. Belghiti J, Cortes A, Abdalla EK, Régimbeau JM, Prakash K, Durand F, et al. Resection prior to liver transplantation for hepatocellular carcinoma. Ann Surg (2003) 238:885–92. doi:10.1097/01.sla.0000098621.74851.65
100. Cherqui D, Laurent A, Mocellin N, Tayar C, Luciani A, Van Nhieu JT, et al. Liver resection for transplantable hepatocellular carcinoma: long-term survival and role of secondary liver transplantation. Ann Surg (2009) 250:738–46. doi:10.1097/SLA.0b013e3181bd582b
101. Del Gaudio M, Ercolani G, Ravaioli M, Cescon M, Lauro A, Vivarelli M, et al. Liver transplantation for recurrent hepatocellular carcinoma on cirrhosis after liver resection: University of Bologna experience. Am J Transplant (2008) 8:1177–85. doi:10.1111/j.1600-6143.2008.02229.x
102. Cucchetti A, Vitale A, Gaudio MD, Pinna AD. Harm and benefits of primary liver resection and salvage transplantation for hepatocellular carcinoma. Am J Transplant (2010) 10:619–27. doi:10.1111/j.1600-6143.2009.02984.x
103. Majno PE, Sarasin FP, Mentha G, Hadengue A. Primary liver resection and salvage transplantation or primary liver transplantation in patients with single, small hepatocellular carcinoma and preserved liver function: an outcome-oriented decision analysis. Hepatology (2000) 31:899–906. doi:10.1053/he.2000.5763
Keywords: hepatocellular carcinoma, liver resection, laparoscopic hepatectomy, chemotherapy, 3-dimensional computed tomography
Citation: Morise Z, Kawabe N, Tomishige H, Nagata H, Kawase J, Arakawa S, Yoshida R and Isetani M (2014) Recent advances in liver resection for hepatocellular carcinoma. Front. Surg. 1:21. doi: 10.3389/fsurg.2014.00021
Received: 05 March 2014; Accepted: 03 June 2014;
Published online: 16 June 2014.
Edited by:
Vincenzo Neri, University of Foggia, ItalyReviewed by:
Jose M. Ramia, Regional Public Health System of Castilla-La Mancha, SpainKun-Ming Chan, Chang Gung Memorial Hospital at Linkou, Taiwan
Copyright: © 2014 Morise, Kawabe, Tomishige, Nagata, Kawase, Arakawa, Yoshida and Isetani. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) or licensor are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Zenichi Morise, Department of Surgery, Banbuntane Houtokukai Hospital, Fujita Health University School of Medicine, 3-6-10 Otobashi Nakagawa-ku, Nagoya, Aichi 454-8509, Japan e-mail:em1vcmlzZUBmdWppdGEtaHUuYWMuanA=
 Zenichi Morise
Zenichi Morise Norihiko Kawabe
Norihiko Kawabe