- 1ICVNS - CMC Bizet, Paris, France
- 2CIMOP - CMC Bizet, Paris, France
Background: In the event of syringomyelia communicating with the fourth ventricle, a fourth ventricle to cervical subarachnoid space shunting could be proposed.
Case Report: In this review article, we describe the case of a 40-year-old woman who had a previously implanted fourth ventricle to spinal subarachnoid space shunt for the treatment of syringomyelia in the context of Chiari syndrome. The catheter migrated intradurally to the lumbosacral space, but in the absence of neurological repercussions, we decided to leave it in place.
Conclusions: To the best of our knowledge, this is the first case described in the literature review of a catheter migration in the subarachnoid space from occipitocervical to lumbosacral level.
Introduction
Syringomyelia is frequently associated with Chiari syndrome (1, 2). When syrinx cavities communicate with the fourth ventricle, a fourth ventricle to spinal subarachnoid space shunting could be proposed with good clinical results (3, 4). Neurological complications reported with this surgical technique are mainly related to the misplacement of the shunt (5, 6), but the migration of the catheter itself has never been described. In this review article, we report for the first time a case of migration of a subarachnoid catheter from the craniocervical level into the lumbosacral intradural space. We also propose a review of the literature concerning the complications and, in particular, the migration of the different types of shunts used at present.
Case Report
This is the case of a 40-year-old woman who was referred to our institution for the assessment of a complex pathology. She was operated three times for Chiari syndrome between 2010 and 2012. During the second intervention in 2011, a ventriculoperitoneal shunt was placed for neurological deterioration secondary to hydrocephalus. During the last intervention, a fourth ventricle to spinal subarachnoid space shunt with a 15 cm catheter was placed for the progression of syringomyelia associated with a fourth ventricle entrapment. The patient presented significant sequelae including right-side hemiparesis, permanent dizziness, and diffuse chronic pain. In the course of the assessment of recent abdominal pain, the patient benefited from an abdominal CT (Figure 1). The CT showed no intra-abdominal complications. However, the presence of an intradural catheter at the L2-S1 level measuring around 15 cm in length and 2.5 mm in diameter was noted. When looking back to a spine MRI taken in 2018 carried out to investigate mechanical low back pain, the presence of the catheter was hard to identify even for experienced radiologists, as its intensity on T1-weighted and T2-weighted images were similar to that of the cauda equina nerve roots. We concluded that this catheter must have migrated intradurally since it was put in place in 2012. To date, this is the first time such migration of the fourth ventricle to spinal subarachnoid space shunt is described in the literature review. Its presence is not responsible for pain or neurological symptoms as it is well-confirmed clinically and on the electromyogram. The ventriculoperitoneal shunt seemed to be functional, and no fourth ventricle entrapment was found (Figure 2). No residual syringomyelia was detected on the spine MRI. Hence, we found no indication to place a new shunt nor to remove the migrated one.
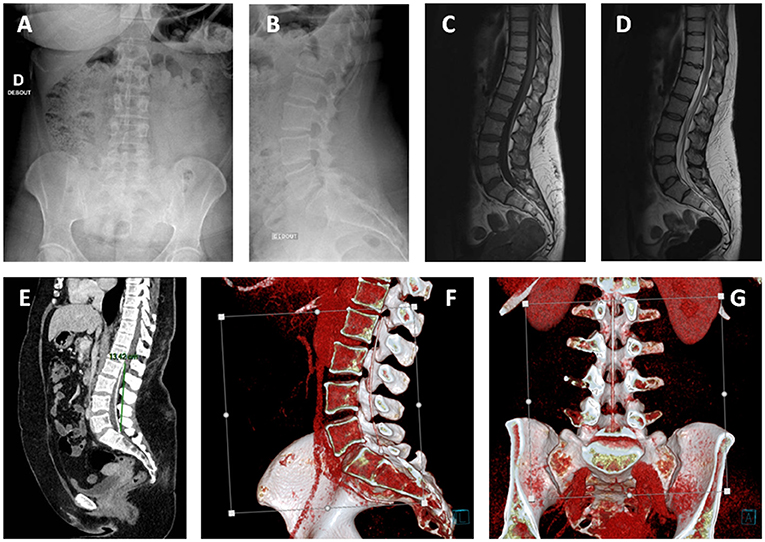
Figure 1. Lumbar x-rays: anteroposterior (A) and lateral views (B), MRI sagittal view, respectively, T1 (C), and T2 (D) sequences. The presence of the catheter was hard to identify even for experienced radiologists, as its intensity on T1-weighted and T2-weighted images was similar to that of the cauda equina nerve roots. (E) Lumbar CT scanner sagittal view showing the initially placed fourth ventricle to cervical subarachnoid space shunt located at L2-S1 level measuring around 15 cm in length and 2.5 mm in diameter. (F,G) Three-dimensional (3D) reconstructions. There is no local compression of neurological elements.
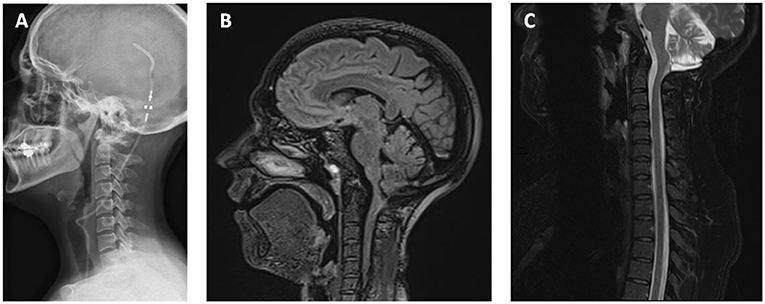
Figure 2. (A) Lateral x-ray showing the ventriculoperitoneal shunt. (B) No hydrocephaly and dilatation of fourth ventricles on MRI sagittal view T1 sequence. The syrinx has completely regressed (C) on MRI sagittal view T2 sequence.
Discussion
In this review article, we describe the case of a 40-year-old woman with a history of syringomyelia in a context of Chiari syndrome (1), who had a previously implanted fourth ventricle to cervical subarachnoid space shunt that migrated to the subdural lumbosacral level. Because of the absence of syringomyelia and ventricular dilation, as well as the absence of neurological repercussions, we decided to leave the catheter in place.
Several types of shunts can be used in the treatment of syringomyelia, namely, fourth ventricle to cervical subdural, syringo-subarachnoid, syringo-peritoneal, syringo-pleural, lumboperitoneal, and ventricular shunts. Each of these techniques has its well-known advantages and complications. Among the complications, catheter migration remains extremely rare. However, to be safe and effective, it is recommended to perform such techniques selectively by an experienced neurosurgeon.
In 1995, Lee et al. reported five complications on 12 patients treated by fourth-ventricular shunting for symptomatic posterior fossa cysts of the Dandy-Walker malformation and trapped the fourth ventricle: Three patients developed new cranial nerve dysfunction caused by direct injury to the floor of the fourth ventricle, one patient suffered an intracystic hemorrhage and acute shunt malfunction, and one patient had the catheter tip in the brainstem on postoperative studies without new neurological deficit (5). These complications were mainly related to the misplacement of the catheter, and even if the techniques have evolved, options include, nowadays, the following: open fenestration through a suboccipital craniotomy, fourth-ventricular shunting, and minimally invasive procedures including endoscopic stenting and fenestration. These techniques are associated with complications in 42% of cases (6–10).
Trapped fourth ventricle with or without syringomyelia is a rare condition, and there is still no consensus on its management strategy. However, in this context of migration of the fourth ventricle to subarachnoid space shunt, the ventriculoperitoneal shunt previously implanted might have in itself induced the long-term resolution of the syringomyelia. This would, therefore, suggest the limited impact of the fourth ventricle to subarachnoid space shunting. Such a view is also shared by a growing portion of the adult and pediatric neurosurgical community (11).
Syringomyelia associated with spinal arachnoiditis or arachnoid adhesions can be treated by adhesiolysis using a conventional microscopic approach or an endoscopic technique in order to place a spinal cysto-subarachnoid shunt (12).
A thorough neuroradiological workup is the best way to ensure the least number of perioperative and postoperative complications and maximal chances of satisfactory long-term clinical improvement in Chiari syndrome (13). When there is persistence, recurrence, or progression of the syrinx after a foramen magnum decompression (30% of the patients), syringomyelia can be treated with a syringo-subarachnoid shunt (14). However, rare neurological complications have been reported (15).
Complications of migration of lumboperitoneal shunt are frequent (16, 17). General complications are similar to ventriculoperitoneal shunt, i.e., abdominal pseudocyst, distal catheter migration, inguinal hernia, catheter disconnection, infection, and intestinal obstruction (18).
Conclusions
To our knowledge, this is the first described case of catheter migration from the fourth ventricle to the lumbar subarachnoid space in the context of Chiari syndrome associated with syringomyelia. Because of the absence of radiological and neurological repercussions, we decided to leave the catheter in place.
Data Availability Statement
The original contributions presented in the study are included in the article/supplementary material, further inquiries can be directed to the corresponding author/s.
Ethics Statement
Ethical review and approval was not required for the study on human participants in accordance with the local legislation and institutional requirements. The patients/participants provided their written informed consent to participate in this study.
Author Contributions
NS: investigation, writing—original draft, and visualization. JF: writing—review and editing and visualization. BT and ST: writing—review and editing. GNAL: supervision and writing—review and editing. All authors contributed to the article and approved the submitted version.
Conflict of Interest
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
Acknowledgments
We are grateful to coauthors for the rereading of the article.
References
1. Di Rocco C. Should we stop using the term “malformation” for Chiari type I? Childs Nerv Syst. (2019) 35:1649–50. doi: 10.1007/s00381-019-04311-z
2. Hidalgo JA, Tork CA, Varacallo M. Arnold Chiari Malformation. Treasure Island, FL: StatPearls Publishing (2020).
3. Fukushima T, Yoshinaga S, Matsuda T, Tomonaga M, Takahashi S, Oita J, et al. [Syringomyelia, its pathogenesis and surgical treatment based on 4 cases' experience]. No Shinkei Geka. (1986) 14:909–16.
4. Davidoff CL, Liu S, Wong JHY, Koustais S, Rogers JM, Stoodley MA. Treatment of Syringomyelia in patients with arachnoiditis at the craniocervical junction. World Neurosurg. (2017) 107:565–73. doi: 10.1016/j.wneu.2017.08.064
5. Lee M, Leahu D, Weiner HL, Abbott R, Wisoff JH, Epstein FJ. Complications of fourth-ventricular shunts. Pediatr Neurosurg. (1995) 22:309–313; discussion 314. doi: 10.1159/000120921
6. Dollo C, Kanner A, Siomin V, Ben-Sira L, Sivan J, Constantini S. Outlet fenestration for isolated fourth ventricle with and without an internal shunt. Childs Nerv Syst. (2001) 17:483–6. doi: 10.1007/s003810100444
7. Udayakumaran S, Biyani N, Rosenbaum DP, Ben-Sira L, Constantini S, Beni-Adani L. Posterior fossa craniotomy for trapped fourth ventricle in shunt-treated hydrocephalic children: long-term outcome. J Neurosurg Pediatr. (2011) 7:52–63. doi: 10.3171/2010.10.PEDS10139
8. Yadav YR, Parihar V. The endoscopic trans-fourth ventricle aqueductoplasty and stent placement for the treatment of trapped fourth ventricle; stent blockage complications under estimated? Neurol India. (2012) 60:455. doi: 10.4103/0028-3886.100743
9. Say I, Dodson V, Tomycz L, Mazzola C. Endoscopic fourth ventriculostomy: suboccipital transaqueductal approach for fenestration of isolated fourth ventricle: case report and technical note. World Neurosurg. (2019) 129:440–4. doi: 10.1016/j.wneu.2019.06.010
10. Tyagi G, Singh P, Bhat DI, Shukla D, Pruthi N, Devi BI. Trapped fourth ventricle-treatment options and the role of open posterior fenestration in the surgical management. Acta Neurochir. (2020) 162:2441–9. doi: 10.1007/s00701-020-04352-3
11. Singhal A, Cheong A, Steinbok P. International survey on the management of Chiari 1 malformation and syringomyelia: evolving worldwide opinions. Childs Nerv Syst. (2018) 34:1177–82. doi: 10.1007/s00381-018-3741-x
12. Tan DCH, Vaughan KA, Koeck H. Endoscopic-assisted spinal arachnoiditis adhesiolysis and placement of a spinal cysto-subarachnoid shunt. World Neurosurg. (2019) 131:43–6. doi: 10.1016/j.wneu.2019.07.160
13. D'Arco F, Ganau M. Which neuroimaging techniques are really needed in Chiari I? A short guide for radiologists and clinicians. Childs Nerv Syst. (2019) 35:1801–8. doi: 10.1007/s00381-019-04210-3
14. Soleman J, Roth J, Bartoli A, Rosenthal D, Korn A, Constantini S. Syringo-subarachnoid shunt for the treatment of persistent syringomyelia following decompression for chiari type I malformation: surgical results. World Neurosurg. (2017) 108:836–43. doi: 10.1016/j.wneu.2017.08.002
15. Levi V, Franzini A, Di Cristofori A, Bertani G, Pluderi M. Subacute posttraumatic ascending myelopathy (SPAM): a potential complication of subarachnoid shunt for syringomyelia? J Spinal Cord Med. (2020) 43:714–8. doi: 10.1080/10790268.2018.1512735
16. Kanai M, Kawano K, Uehara S. Upward migration of the L-P shunt catheter into the cranial base. Osaka City Med J. (1999) 45:123–7.
17. Yoshida S, Masunaga S, Hayase M, Oda Y. Migration of the shunt tube after lumboperitoneal shunt–two case reports. Neurol Med Chir. (2000) 40:594–6. doi: 10.2176/nmc.40.594
Keywords: cranio-cervical junction, syringomyelia, trapped fourth ventricle, trapped fourth ventricle with syrinx, fourth ventricle to spinal subarachnoid space shunt, catheter migration, Chiari syndrome
Citation: Serratrice N, Faddoul J, Tarabay B, Taifour S and Abi Lahoud GN (2021) Case Report: A Rare Case of Fourth Ventricle to Spinal Subarachnoid Space Shunt Migration: Surgical Pearl and Literature Review. Front. Surg. 8:696457. doi: 10.3389/fsurg.2021.696457
Received: 16 April 2021; Accepted: 14 June 2021;
Published: 08 July 2021.
Edited by:
Michael Sughrue, University of New South Wales, AustraliaReviewed by:
Mario Ganau, University of Toronto, CanadaFahd Derkaoui Hassani, Cheikh Zaid International University Hospital, Morocco
Copyright © 2021 Serratrice, Faddoul, Tarabay, Taifour and Abi Lahoud. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Nicolas Serratrice, bi5zZXJyYXRyaWNlQGNsaW5pcXVlLWJpemV0LmNvbQ==; bmljby5zZXJyYXRyaWNlQG9yYW5nZS5mcg==
 Nicolas Serratrice
Nicolas Serratrice Joe Faddoul
Joe Faddoul Bilal Tarabay1
Bilal Tarabay1 Georges Naïm Abi Lahoud
Georges Naïm Abi Lahoud