- 1Department of Medical and Surgical Sciences, University of Catanzaro, Catanzaro, Italy
- 2Department of Health Sciences, University of Catanzaro, Catanzaro, Italy
- 3Biostat Research s.a.s, Borgomanero, Italy
Background: Pilonidal disease (PD) represents one of the most common proctological diseases in young adults. Although several approaches to treating PD have been described, there is still a lack of agreement on which is the best. The aim of this study was to evaluate the long-term efficacy of endoscopic pilonidal sinus treatment (EPSiT) at a tertiary care academic center.
Methods: Between June 2017 and January 2021, a total of 32 patients [12 women (37.5%) and 20 men (62.5%)] with a mean age of 29.22 ± 12.98 years were treated with EPSiT. Pre- and post-operative symptoms were assessed with a score of 0–5. Success was defined as the absence of any subjective symptoms, as well as by complete post-operative wound healing.
Results: Most of the patients had a midline external opening (17/32; 53.1%), with a mean number of external openings of 2.41 (1–4) ± 1.04. The median post-operative pain score was 0, and the mean follow-up period was 22 (4–42) ± 11.49 months. The time to wound healing was reduced in patients with one opening (28.14 ± 4.06 days) compared to patients with two or more openings (33.64 ± 7.3 days) (p = 0.067). The mean operative time was longer in patients who subsequently had a recurrence (41.75 ± 6.24 vs. 34.18 ± 6.24 min; p = 0.031). The overall success rate was 87.5% (28/32), and the mean time to recurrence was 3.25 (2–5) ± 1.26 months.
Conclusions: EPSiT represents a viable option for the treatment of PD. More evidence and a longer follow-up period are needed to validate the results.
Introduction
Pilonidal disease (PD) is one of the most common and debilitating proctological diseases, with an estimated incidence of 26 cases out of 100,000 (1) inhabitants and a higher frequency in young adult men aged between 15 and 30 years. In 1833, Herbert Mayo first described a sinus containing hair follicles in the sacrococcygeal area (2), but it was only in 1880 when Hodges used the term pilonidal, from the Latin “pilus,” meaning hair, and “nidus,” meaning nest (3). This differentiates the pathology from the presence of a single lesion.
Understanding the disease's pathophysiology was fundamental for the evolution of treatment. Indeed, it was initially assumed that the disease was of congenital origin (4); however, during the Second World War, its high frequency in soldiers refuted this origin theory due to the action of compression in the sacrococcygeal region and the consequent local trauma, leading to support for the theory that the disease instead had an acquired origin (5). In fact, according to Karydakis (6), hair penetration is the basis of the inflammatory process that leads to PD.
Although PD has been extensively researched and several techniques have been described, the lack of agreement on the best treatment approach, especially in complex conditions such as in the case of recurrent or acute PD, has led to the development of further innovations in the field.
The minimally invasive endoscopic treatment of PD was first described in 2013 by Meinero (7) and Milone (8), who, starting from the same concept, developed two techniques based on the use of a fistuloscope with an 8° angled eyepiece [i.e., endoscopic pilonidal sinus treatment (EPSiT)] and a hysteroscope with a 30° angled eyepiece [video-assisted ablation of pilonidal sinus (VAAPS)], respectively.
Over the years, the minimally invasive approach has demonstrated advantages such as the virtual absence of pain and complications, early return to work for patients, as treatment only results in an extremely small wound, and consequent patient satisfaction, which leads to willingness to repeat the treatment (9–11).
Furthermore, its success rate, even if lower than traditional techniques, remains considerably high (12). Therefore, the aim of the present study was to evaluate the long-term efficacy of EPSiT for pilonidal disease at a tertiary care academic center.
Materials and Methods
Study Design
This was a retrospective single-center study and is reported according to the Strengthening the Reporting of Observational Studies in Epidemiology (STROBE) statement for cohort studies (13).
Between June 2017 and January 2021, a total of 32 patients with pilonidal disease underwent EPSiT in our department.
Patient demographics, symptoms, previous surgeries, number and location of external openings, and operative details were prospectively recorded using our PC database.
A visual analog scale (VAS) score was used to assess post-operative pain (minimum score = 0; maximum score = 10).
Pre- and post-operative symptoms after 3 months were assessed using a modified in-house questionnaire based on Meinero et al. (14), in which pain, body temperature, wound secretion, and removal frequency of the dressing were evaluated on a scale from 0 to 20. Each item was rated with a score of 0 to 5 (1 = mild; 2 = moderate; 3 = severe; 4–5 = extremely severe).
Post-operative complications were determined using the Clavien–Dindo classification (15).
Success was defined as the absence of any subjective symptoms, as well as by complete post-operative wound healing. Incomplete wound healing was defined as persistent wound swelling or discharge after 60 days post-operation.
Patients were clinically followed up at 2 and 4 weeks and 1, 3, 6, and 12 months after the procedure. Further follow-up visits were facilitated by telephone, and an eventual follow-up visit was organized according to the needs of the patient.
All the patients were admitted and discharged the day of the procedure, and antibiotic prophylaxis with cephalosporin was administered.
All procedures were performed with the patient in the prone position, with the hips slightly flexed and the buttocks retracted with adhesive tape, under local anesthesia, according to Meinero et al. (7).
We strongly suggest regular and periodic hair removal by shaving or depilatory cream, especially during the first two post-operative years.
Recurrence was defined as the reappearance of the symptoms or PD, as confirmed by both the scores and the findings during the follow-up visit.
Statistical Analysis
The results are reported as counts and percentages for categorical variables, as the means ± SDs (range) for continuous normally distributed variables, and as the median [interquartile range (IQR)] for ordinal categorical variables and for continuous non-normally distributed variables. The changes in in-house scores were analyzed with a Wilcoxon test for paired samples, because post-operative scores were not normally distributed. The correlation between categorical variables and disease recurrence was explored by crosstabulations with a chi-squared test, while differences in means were analyzed with an independent samples t-test. The freedom from recurrence was evaluated as the time elapsed from the procedure to the relapse of disease using Kaplan–Meier survival analysis. The results associated with a p-value <0.05 were considered statistically significant. Statistical data analysis was performed using IBM SPSS version 20.
Results
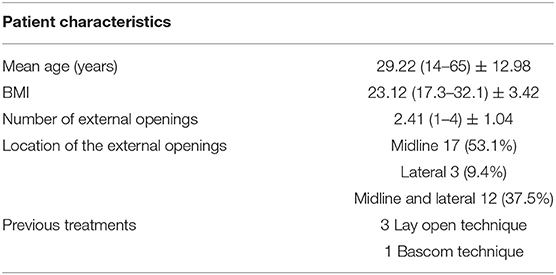
A total of 32 patients [12 women (37.5%) and 20 men (62.5%)] with a mean age of 29.22 ± 12.98 years were treated with EPSiT. Only four patients underwent previous surgery (three with the lay open technique and one with the Bascom technique) (Table 1).
Most of the patients had a midline external opening (17/32; 53.1%), with a mean number of openings of 2.41 (1–4) ± 1.04. The median post-operative pain score was 0 (IQR 0–0). Interestingly, nine patients reported a VAS of 0, 20 patients a VAS of 1, and only one and two patients reported a VAS of 2 and 3, respectively.
The mean follow-up period was 22 (4–42) ± 11.49 months, and no patient was lost at follow-up.
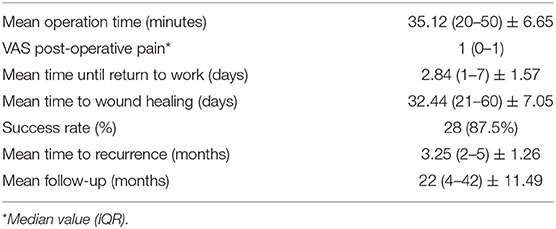
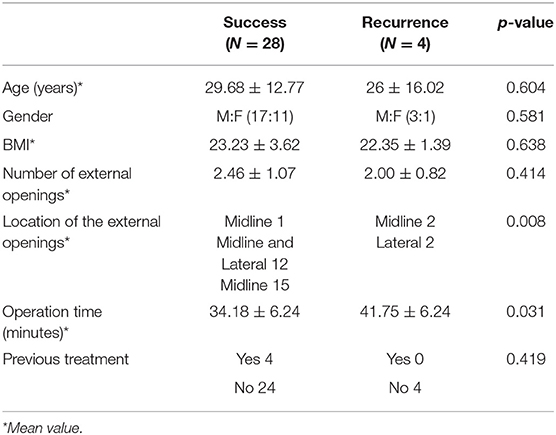
Neither intraoperative nor post-operative complications occurred. The operative results are detailed in Table 2.
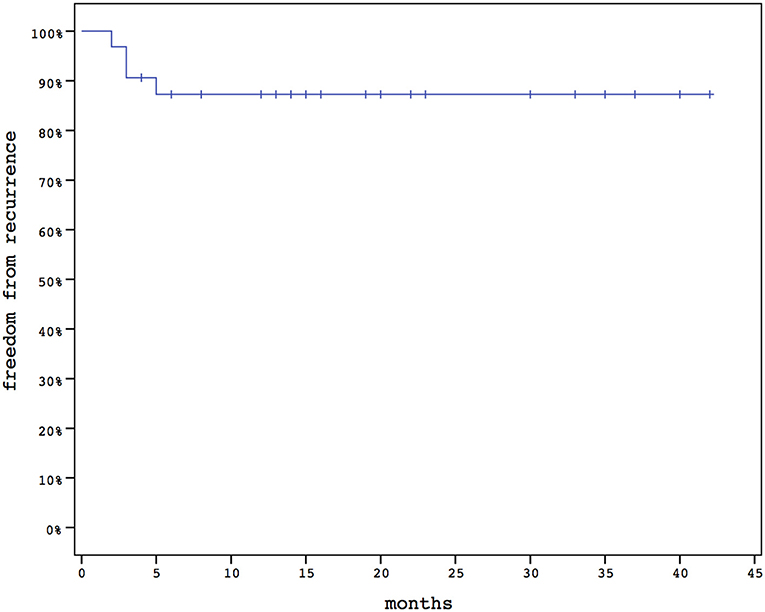
The overall success rate was 87.5% (28/32), and the mean time to recurrence was 3.25 (2–5) ± 1.26 (Figure 1). All the recurrences were successfully treated with the lay open technique.
Three patients who underwent follow-up at 12, 14, and 18 months after the procedure had partial reopening of wounds. Patients were treated conservatively with hydrogen peroxide and saline dressings and were given hair removal advice. They are currently disease-free.
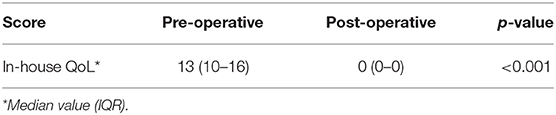
The in-house symptoms score significantly improved post-operatively, from a median pre-operative value of 13 (10–16) to 0 (0–0) (p <0.001; Table 3).
The mean operation time was 35.12 (20–50) ± 6.65 min. Interestingly, there was a statistically significant difference (p = 0.031) in mean operation time between successful (34.18 ± 6.24 min) and recurrence (41.75 ± 6.24) patients. No other differences between the two groups were found, except for the location of the openings (p = 0.008; Table 4).
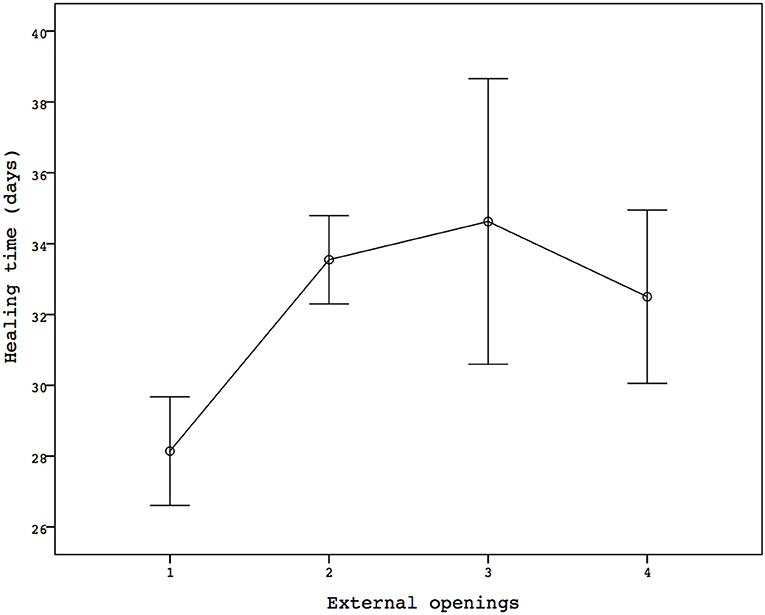
The mean time to wound healing was 32.44 (21–60) ± 7.05 days. The seven patients with only one opening had a mean healing time of 28.14 ± 4.06 days, while in the patients with two or more openings, 33.64 ± 7.3 days were needed to achieve a complete wound healing (p = 0.067; Figure 2). However, there was no linear correlation between the number of openings and wound healing (r = 0.212).
Discussion
Minimally invasive approaches have completely revolutionized the treatment of PD. In fact, the reduction in discomfort and post-operative pain due to a smaller wound size and a fast return to work, facilitated by the use of local anesthesia, decreases the level of embarrassment experienced by patients, which is common in proctological diseases.
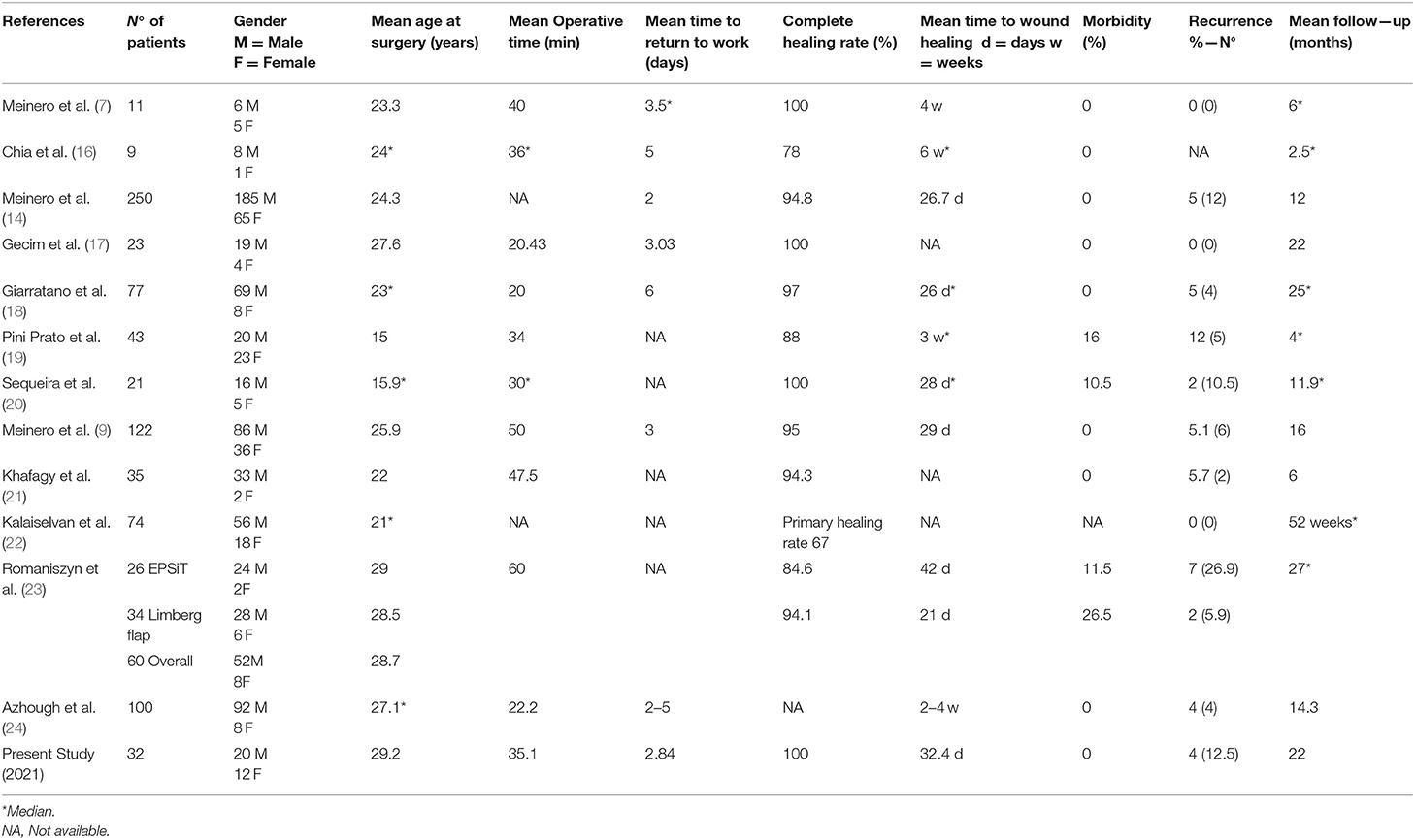
The results of the present study are consistent with those described in the current literature (Table 5) (7, 9, 14, 16–24).
Compared to the first study published by Meinero et al. (7), the length of the follow-up treatment period has increased and the success rate of the technique has remained consistently high. Only Giarratano et al. (18) and Romaniszyn et al. (23) had a more extensive follow-up than ours. Interestingly, in the latter, the authors reported the highest failure rate described so far, i.e., 42.3%, and superiority of the Limberg flap (Table 5). However, the study concerned cases of complicated PD, where 50% of patients had three or more external openings or recurrent disease.
In our study, 14 patients (44%) had three or more external openings, and we agree with Romaniszyn et al. that the procedure has greater complexity in this scenario. In fact, even if there was no correlation between recurrence and the risk factors assessed such as age, BMI, and gender, the wound healing rate in patients with multiple openings was prolonged (p = 0.067). Unfortunately, the small number of patients included did not allow statistical significance to be reached.
We found a significantly longer operating time (41.75 vs. 34.18 min) in patients with recurrences (Table 4). This is probably due to the difficulty in finding all sinus tracks and highlights the complexity of that specific situation. Moreover, we did not report any recurrence when the external openings were placed simultaneously in the midline and lateral positions. Two out of the three patients with lateral localization and one out of the 15 with midline localization had a relapse (p = 0.008). Although statistically significant, in the present study, we did not have enough cases to be able to prove its validity. Certainly, we would expect a recurrence in patients with multiple PD localizations.
Recently, Strong et al. (25) stressed the importance of discussion with the patient in the surgical decision-making process, especially in terms of expectations. We agree that patient understanding of the procedures, as well as of the outcomes and complications, is mandatory.
Four patients (12.5%) experienced a recurrence of the disease and underwent a lay open technique.
Treatment decisions were discussed and shared with the patients, who, in this case, expressed their preference for a treatment that could guarantee a greater success rate, even if paying the price of having post-operative pain and a larger wound. Conversely, three patients treated with EPSiT had previously undergone the lay open technique and, after discussing the limitations and advantages, they opted for the minimally invasive procedure, which turned out to be successful.
The symptom score had a post-operative median value of 0 with a statistically significant difference compared to the pre-operative period. It is worth noting that the scores of the patients with recurrence also decreased, which highlights how failure in minimally invasive treatment can still lead to a decline in the disease's.
The three patients who had a wound reopen about 1 year after surgery underwent dressing with complete hair removal. For this reason, we recommend laser hair depilation in order to reduce the likelihood of recurrence (26).
Furthermore, there are two other significant concepts. First, reoperation in a patient who has previously received EPSiT is certainly less complicated than a flap, where extensive mobilization is necessary. Second, failure and re-EPSiT are more easily accepted by the patient, considering the low burden caused by the technique.
In this context, Meinero et al. (9) reported a complete wound healing rate in 116 out of 122 patients with recurrent PD. Most of the patients had undergone one previous procedure (89; 72.9%), while 26 (21.3%) and 7 (5.7%) had undergone two and three previous procedures, respectively.
These results were consistent with those described by Manigrasso et al. (27).
The minimally invasive endoscopic treatment of pilonidal disease represents one of the greatest technological innovations for proctological diseases. Magnification has facilitated a decrease in the rate of unrecognized sinus tracks with complete removal of the hair, as well as a consequent decrease in recurrences.
However, more evidence is needed to verify the results. In fact, so far, there has only been one randomized trial, published by Milone et al. (28), to compare minimally invasive treatment (VAAPS) with the Bascom cleft lift procedure, demonstrating superiority in terms of early return to work and pain control.
Our study has some limitations. This was a retrospective single-center study with a small sample size and no control group. However, the length of the follow-up and the complete statistical analysis without the loss of any patient represent the greatest strengths.
Data Availability Statement
The raw data supporting the conclusions of this article will be made available by the authors, without undue reservation.
Ethics Statement
Ethical review and approval was not required for the study on human participants in accordance with the local legislation and institutional requirements. Written informed consent to participate in this study was provided by the participants' legal guardian/next of kin. Ethical review and approval was not required for the animal study because it concerns standard clinical practice.
Author Contributions
GG substantial contributions to the conception and design of the work, acquisition, analysis, interpretation of data for the work, drafting the work and revising it critically for important intellectual content, final approval of the version to be published, agreement to be accountable for all aspects of the work in ensuring that questions related to the accuracy, and integrity of any part of the work are appro-priately investigated and resolved. GD and EN substantial contributions to the conception and design of the work, acquisition, analysis, and interpretation of data for the work, agreement to be accountable for all aspects of the work in ensuring that questions related to the accuracy, and integrity of any part of the work are appropriately inves-tigated and resolved. AC, SF, and FF substantial contributions to the acquisition of data for the work and final approval of the version to be published. GS drafting the work and revising it critically for important intellectual content and final approval of the version to be published. All authors contributed to the article and approved the submitted version.
Conflict of Interest
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
Publisher's Note
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
References
1. Loganathan A, Zadeh RA, Hartley J. Pilonidal disease: time to reevaluate a Common Pain in the Rear! Dis Colon Rectum. (2012) 55:491–3. doi: 10.1097/DCR.0b013e31823fe06c
3. Hodges RM. Pilonidal sinüs. Boston Med Surg J. (1880) 103:485–6. doi: 10.1056/NEJM188011181032101
4. Gage M. Pilonidal sinuses: an explanation of its embryologic development. Arch Surg. (1935) 31:175–89. doi: 10.1001/archsurg.1935.01180140003001
6. Karydakis GE. Easy and successful treatment of pilonidal sinus after explanation of its causative process. Aust N Z J Surg. (1992) 62:385–9. doi: 10.1111/j.1445-2197.1992.tb07208.x
7. Meinero P, Mori L, Gasloli G. Endoscopic pilonidal sinus treatment (E.P.Si.T.). Tech Coloproctol. (2014) 18:389–92. doi: 10.1007/s10151-013-1016-9
8. Milone M, Musella M, Di Spiezio Sardo A, Bifulco G, Salvatore G, Sosa Fernandez LM, et al. Video-assisted ablation of pilonidal sinus: a new minimally invasive treatment–a pilot study. Surgery. (2014) 155:562–6. doi: 10.1016/j.surg.2013.08.021
9. Meinero P, La Torre M, Lisi G, Stazi A, Carbone A, Regusci L, et al. Endoscopic pilonidal sinus treatment (EPSiT) in recurrent pilonidal disease: a prospective international multicenter study. Int J Colorectal Dis. (2019) 34:741–6. doi: 10.1007/s00384-019-03256-8
10. Milone M, Basso L, Manigrasso M, Pietroletti R, Bondurri A, La Torre M, et al. Consensus statement of the Italian society of colorectal surgery (SICCR): management and treatment of pilonidal disease. Tech Coloproctol. (2021). doi: 10.1007/s10151-021-02487-8
11. Milone M, Velotti N, Manigrasso M, Vertaldi S, Di Lauro K, De Simone G, et al. Long-term results of a randomized clinical trial comparing endoscopic versus conventional treatment of pilonidal sinus. Int J Surg. (2020) 74:81–5. doi: 10.1016/j.ijsu.2019.12.033
12. Tien T, Athem R, Arulampalam T. Outcomes of endoscopic pilonidal sinus treatment (EPSiT): a systematic review. Tech Coloproctol. (2018) 22:325–31. doi: 10.1007/s10151-018-1803-4
13. Vandenbroucke JP, von Elm E, Altman DG, Gøtzsche PC, Mulrow CD, Pocock SJ, et al. Strengthening the reporting of observational studies in epidemiology (STROBE): explanation and elaboration. Int J Surg. (2014) 12:1500–24. doi: 10.1016/j.ijsu.2014.07.014
14. Meinero P, Stazi A, Carbone A, Fasolini F, Regusci L, La Torre M. Endoscopic pilonidal sinus treatment: a prospective multicentre trial. Colorectal Dis. (2016) 18:O164–70. doi: 10.1111/codi.13322
15. Dindo D, Demartines N, Clavien PA. Classification of surgical complications: a new proposal with evaluation in a cohort of 6336 patients and results of a survey. Ann Surg. (2004) 240:205–13. doi: 10.1097/01.sla.0000133083.54934.ae
16. Chia CL, Tay VW, Mantoo SK. Endoscopic pilonidal sinus treatment in the Asian population. Surg Laparosc Endosc Percutan Tech. (2015) 25:e95–7. doi: 10.1097/SLE.0000000000000131
17. Gecim IE, Goktug UU, Celasin H. Endoscopic pilonidal sinus treatment combined with crystalized phenol application may prevent recurrence. Dis Colon Rectum. (2017) 60:405–7. doi: 10.1097/DCR.0000000000000778
18. Giarratano G, Toscana C, Shalaby M, Buonomo O, Petrella G, Sileri P. Endoscopic pilonidal sinus treatment: long-term results of a prospective series. JSLS. (2017) 21:e2017.00043. doi: 10.4293/JSLS.2017.00043
19. Pini Prato A, Mazzola C, Mattioli G, Escolino M, Esposito C, D'Alessio A, et al. Preliminary report on endoscopic pilonidal sinus treatment in children: results of a multicentric series. Pediatr Surg Int. (2018) 34:687–92. doi: 10.1007/s00383-018-4262-0
20. Sequeira JB, Coelho A, Marinho AS, Bonet B, Carvalho F, Moreira-Pinto J. Endoscopic pilonidal sinus treatment versus total excision with primary closure for sacrococcygeal pilonidal sinus disease in the pediatric population. J Pediatr Surg. (2018) 53:2003–7. doi: 10.1016/j.jpedsurg.2018.02.094
21. Khafagy A, Al Haddad E, AlSabah S. The endoscopic treatment of pilonidal sinus disease: a short-term case-series study. Ann Saudi Med. (2019) 39:192–6. doi: 10.5144/0256-4947.2019.192
22. Kalaiselvan R, Liyanage A, Rajaganeshan R. Short-term outcomes of endoscopic pilonidal sinus treatment. Ann R Coll Surg Engl. (2020) 102:94–7. doi: 10.1308/rcsann.2019.0097
23. Romaniszyn M, Swirta JS, Walega PJ. Long-term results of endoscopic pilonidal sinus treatment vs. Limberg flap for treatment of difficult cases of complicated pilonidal disease: a prospective, nonrandomized study. Colorectal Dis. (2020) 22:319–24. doi: 10.1111/codi.14857
24. Azhough R, Azari Y, Taher S, Jalali P. Endoscopic pilonidal sinus treatment: a minimally invasive surgical technique. Asian J Endosc Surg. (2021) 14:458–63. doi: 10.1111/ases.12893
25. Strong E, Callaghan T, Beal E, Moffatt C, Wickramasekera N, Brown S, et al. Patient decision-making and regret in pilonidal sinus surgery: a mixed-methods study. Colorectal Dis. (2021) 23:1487–98. doi: 10.1111/codi.15606
26. Halleran DR, Onwuka AJ, Lawrence AE, Fischer BC, Deans KJ, Minneci PC. Laser hair depilation in the treatment of pilonidal disease: a systematic review. Surg Infect (Larchmt). (2018) 19:566–72. doi: 10.1089/sur.2018.099
27. Manigrasso M, Velotti N, Sosa Fernandez LM, Vertaldi S, Maione F, Gennarelli N, et al. Endoscopic Approach to Recurrent Pilonidal Sinus: A Retrospective Analysis. J Laparoendosc Adv Surg Tech A. (2021) 31:1–5. doi: 10.1089/lap.2020.0252
Keywords: endoscopic pilonidal sinus treatment, minimally invasive treatment, pilonidal disease, pilonidal recurrence, academic center
Citation: Gallo G, Carpino A, De Paola G, Fulginiti S, Novelli E, Ferrari F and Sammarco G (2021) Endoscopic Pilonidal Sinus Treatment: A Tertiary Care Academic Center Experience. Front. Surg. 8:723050. doi: 10.3389/fsurg.2021.723050
Received: 09 June 2021; Accepted: 08 July 2021;
Published: 09 August 2021.
Edited by:
Marco Milone, Federico II University Hospital, ItalyReviewed by:
Lorenzo Mori, Ospedale di Lavagna, ItalyGianluca Rompianesi, University of Naples Federico II, Italy
Copyright © 2021 Gallo, Carpino, De Paola, Fulginiti, Novelli, Ferrari and Sammarco. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Gaetano Gallo, Z2FsbG9nQHVuaWN6Lml0 orcid.org/0000-0003-1066-4671
†These authors have contributed equally to this work
 Gaetano Gallo1*
Gaetano Gallo1* Gilda De Paola
Gilda De Paola Giuseppe Sammarco
Giuseppe Sammarco