- Department of Orthopaedic Surgery, Yichun People's Hospital, Yichun, China
Background: Extraosseous Ewing's sarcoma/primary neuroectodermal tumor (EES/PNET) is a rare, malignant, small round blue cell tumor, which usually involves the larynx, kidneys, and esophagus. The most common metastatic sites are lung and bone. The incidence of epidural EES/PNET was 0.9%, and a detailed search of the PubMed literature found only 7 case reports of epidural ESS/PNET at the cervicothoracic junction in children.
Case description: We report a case of epidural ESS/PNET at the cervicothoracic junction in a child with chest and back pain as the first symptom, which worsened after half a year and developed incomplete paralysis of both lower extremities and urinary incontinence. She underwent emergency surgery, chemotherapy and radiotherapy, and died of lung metastases 8 months after surgery.
Conclusion: Primary epidural tumors are mostly benign, such as spinal meningiomas and neuromas. Contrary to what has been previously thought, we report a case of malignant epidural EES/PNET at the cervicothoracic junction without bone destruction; The rarity of epidural EES/PNET at the cervicothoracic junction in children has led to a lack of data, particularly on prognostic factors and recurrence patterns. Due to the difficulty of early diagnosis and high mortality, spine surgeons must explore and increase their awareness of this disease.
Introduction
Ewing sarcoma (ES) and primitive neuroectodermal tumors (PNET) are collectively referred to as ES/PNET because they share the same genetic and histological features (1). ES/PNET are highly malignant small round cell tumors with multidirectional differentiation potential and can be classified as intraosseous and extraosseous depending on their origin in bone or soft tissue (2). Extraosseous Ewing's sarcoma (EES)/PNET is an extremely rare primary malignant tumor with rapid progression and poor prognosis (3). EES/PNET has been reported mainly in the chest wall, lower extremities and paravertebral regions, followed by the upper extremities, hip and pelvis, and rarely in the epidural space, especially at the cervicothoracic junction (4, 5).
To date, the involvement of the epidural space in the cervicothoracic junction is rarely described in the literature, and there are only a few cases reported worldwide. The rarity of epidural EES/PNET at the cervicothoracic junction in children has led to a lack of data, particularly on prognostic factors and recurrence patterns. We report a rare case of cervicothoracic junction EES/PNET in a 12-year-old boy. Surgical resection was performed with postoperative radiotherapy and chemotherapy. The entire clinical diagnosis and treatment process is reported, and our case is compared with other previously reported cases.
Case report
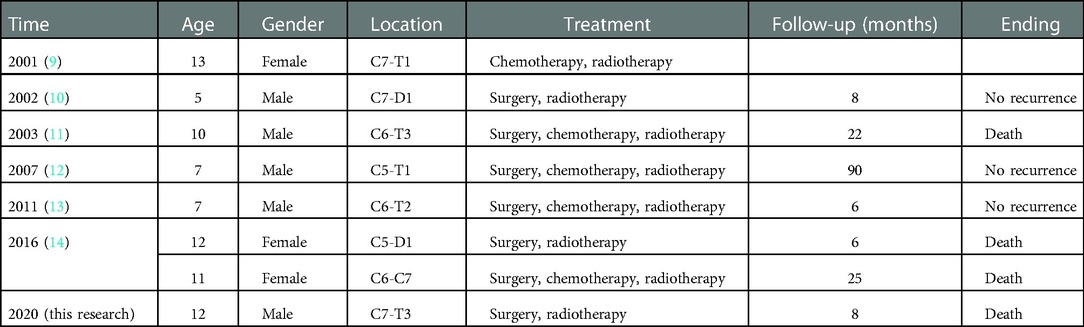
A 12-year-old boy who appeared to be healthy developed chest and back pain. His symptoms improved after treatment with nonsteroidal anti-inflammatory drugs (NSAIDs) at a local hospital. however, his condition, gradually worsened within 6 months. One day ago, he was transferred to our hospital for sudden incomplete paralysis of both lower limbs, and urinary incontinence. He had no history of any trauma or cerebrovascular accident. On examination, he was conscious with normal higher mental functions. Motor system examination showed that the strength of the upper limbs was MRC grade 5/5, and the strength of the lower limbs was only MRC grade 1/5. The tone of the muscles of the upper limbs was normal, but the tone of the muscles of the lower limbs was decreased. The skin sensation below the T3 plane was decreased. The deep tendon reflexes of the patella and Achilles tendon were impaired, and the Babinski sign was positive on both sides. The JOA score was 8 points. Preoperative transverse and sagittal CT showed no bone destruction in the cervicothoracic junction, and CT of the lungs showed no significant abnormalities. MRI showed a long soft tissue mass at the cervicothoracic junction (C7-T3) with the spinal cord compressed and shifted to the right. It was isointense on T1W and hyperintense on T2W images. MRI showed that the tumor in the cervicothoracic spinal canal was approximately 8 mm × 15 mm × 63 mm (Figure 1).
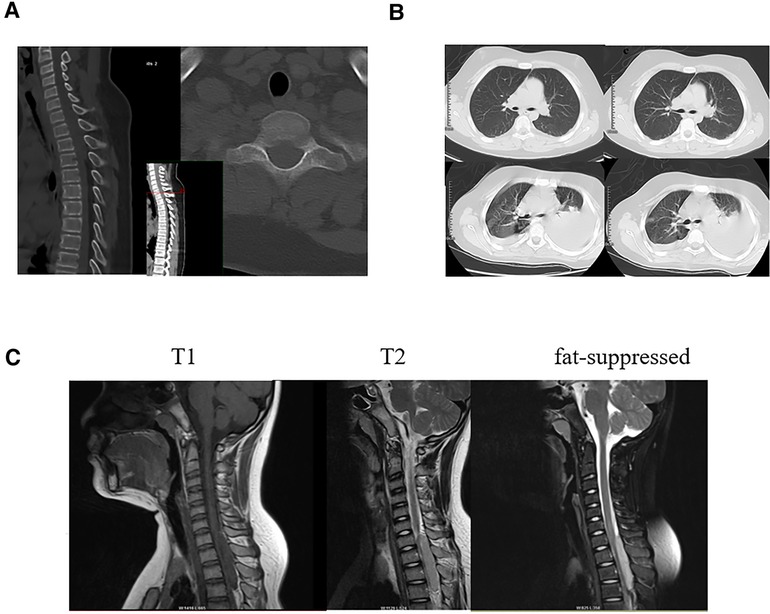
Figure 1. (A) Preoperative transverse and sagittal CT showed no bone destruction in the cervicothoracic junction. (B) Preoperative lung CT showed no obvious signs of tumor metastasis,Six months after the operation, lung CT showed multiple nodules in both lungs, and metastasis was considered. (C) T1-weighted, T2-weighted, and fat-suppressed sagittal MRI showed a long tubular mass in the spinal canal at the cervicothoracic junction, with a size of about 8 mm × 15 mm × 63 mm, and no abnormal signal vertebral body and appendage morphology.
Due to the sudden onset of symptoms of bilateral lower limb incomplete paralysis, preoperative biopsy and chemotherapy were not performed. After ruling out contraindications to surgery, an emergency C7-T3 laminectomy was performed. Pedicle screws were placed on both sides of C7 and T3, the right side of T1 and the left side of T2 to fix the unstable cervical spine.C7 and T3, the right side of T1 and the left side of T2 to fix the unstable cervical spine (Figure 2). Intraoperatively, a flesh-like tumor with soft texture and rich blood supply was found in the epidural space. It filled the entire vertebral cavity of C7-T3 and extruded the dura mater to the ventral side. The tumor was completely separated out and excised along the envelope under microscopic manipulation, the dura mater was intact and pulsatile, and the lesion was biopsied (Figure 2). Immunohistochemistry showed positivity for Ki67, strong positivity for Vimentin, Cyclin D1, and CD99, and negativity for CD56, EMA, CKpan, Desmin, LCA, CD34, NKX2.2 and Syn. The histopathological report showed malignant small round blue tumors, which is consistent with Ewing's sarcoma/PNET (Figure 3). The patient's family decided not to perform next-generation sequencing (NGS) due to the high cost of the test.
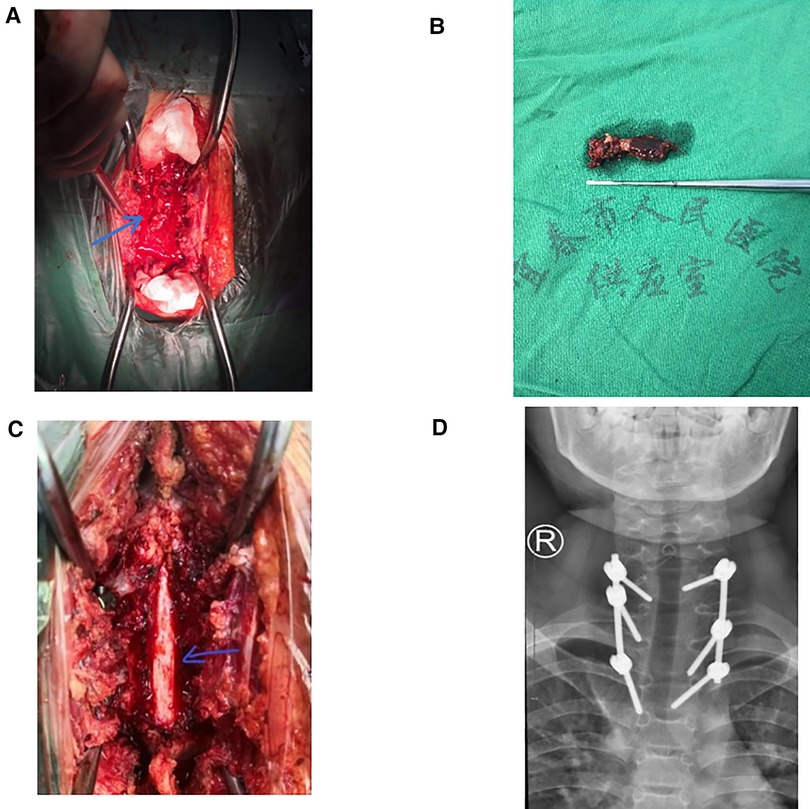
Figure 2. (A) Severe dural sac compression before surgery, (B) intraoperative excision of the tumor, about 5 cm long, (C) the dural sac was entire and pulsating after tumor resection, (D) postoperative radiographs showed accurate pedicle screw placement.
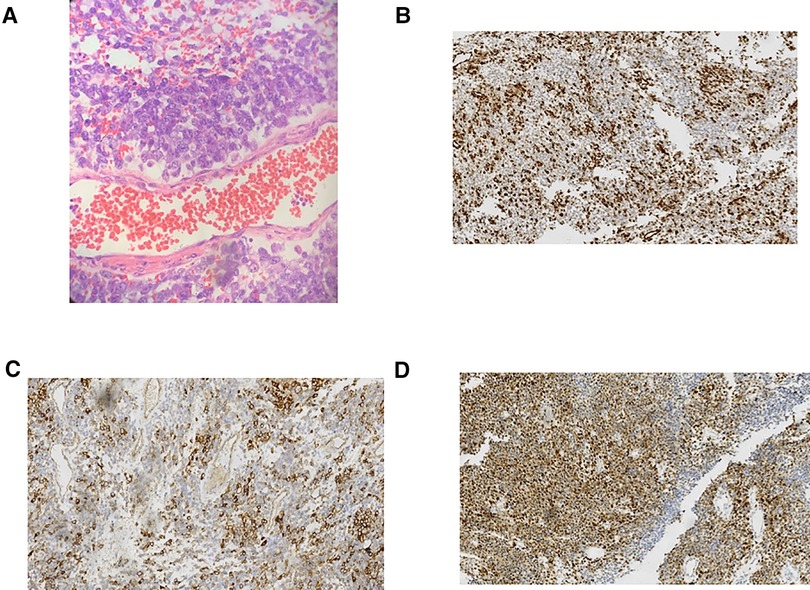
Figure 3. (A) Pathological examination microscope showed small round blue cells (HE staining, ×200). (B–D) Immunohistochemical staining showed that vimentin (B), CD99 (C) and Cyclin D1 (D) were strongly positive in small round blue cells (×100).
Postoperative motor system examination showed that the strength of the right lower limbs was MRC grade 3/5, and the strength of the left lower limbs was MRC grade 1/5. The JOA score was11 points. After discussion with the oncologist two weeks after the surgery, it was decided to give him chemoradiotherapy. First-line palliative chemotherapy with vincristine (VCR), doxorubicin (DOX), and cyclophosphamide (CPA) was initiated in June 2019. We planned 1.5 mg/m2 of VCR per week, 30 mg/m2 of DOX per day and 1.2 mg/m2 of CPA per day. After two cycles we implemented ifosfamide and etoposide as alternative treatment. We planned 1,800 mg/m2 of ifosfamide per day and 100 mg/m2 of etoposide per day for five days. Pulmonary metastases occurred after 6 months of follow-up with no local recurrence (Figure 1). Motor system examination showed MRC grade 3/5 strength in the right lower extremity and MRC grade 2/5 strength in the left lower extremity. The treatment group discussed the treatment plan with the patient's family, the patient's family decided not to pursue additional treatment, and he died 8 months after surgery. The course of the disease diagnosis and treatment is shown in the timeline.
Timeline: NSAIDs: Nonsteroidal anti-inflammatory drugs
Discussion
EES is a rare, malignant, small round blue cell tumor of undifferentiated mesenchymal origin, originating from the neural crest of the central and sympathetic nervous systems. It was first reported by Tefft et al. in 1969. Both PNET and Ewing's sarcoma (ES) have the same small round blue cells and similar molecular relationships. In most literature reports, researchers describe these entities together as EES/PNET (6). EES/PNET has been reported in various sites, such as the larynx, kidneys, and esophagus. The presence of EES/PNET in the extradural area is very rare, with an incidence of 0.9% (7). Pediatric spinal epidural EES/PNET is a very rare tumor. There have been less than 50 cases reported thus far. The most common site was the lumbar spine. Cervical and thoracic spines are rare sites, and males are most commonly affected (8). A detailed search of the literature in PubMed revealed only 8 cases of epidural ESS/PNET in the cervicothoracic junction in children, and the ratio of males to females was 1.67 : 1 as previously reported (Table 1).
In general, the intradural and extramedullary EES/PNET will not extend into the adjacent vertebrae and tends to infiltrate the paravertebral muscle tissue or neural foramina (6). This can potentially cause nerve damage, resulting in loss of sensory or motor function of the arms and legs (paraplegia or quadriplegia). Pain and muscle weakness corresponding to the tumor location are the most common clinical features of EES/PNET (15, 16). Our patient had only chest pain before incomplete paralysis of both lower extremities, and the failure to receive timely and accurate treatment was considered to be a factor in the poor prognosis of the patient.
The differential diagnosis of EES/PNETs in children includes Hodgkin’s disease, neuroblastoma, rhabdomyosarcoma, and Wilms’ tumor (17). Early diagnosis of EES/PNETs was mainly based on MRI, but it was considered difficult to distinguish EES/PNET from other tumors originating in the spinal cord based on depending upon the MRI signal intensity alone (13, 18). On MRI, EES/PNET was usually isointense to the muscles on T1W and hyperintense on T2W images, with enhancement on postcontrast scans. The histopathological biopsy features of EES/PNET consist of uniform small round blue cells, but they often need to be distinguished from other small round cell malignancies, which can easily be misdiagnosed as lymphoma (19). These small round blue cells often show immunohistochemical positivity for CD99, vimentin, and cyclin D1, as in our case report.
At present, neoadjuvant radiotherapy and chemotherapy combined with en bloc resection is the gold standard for treating limb Ewing's sarcoma (20). However, when the intradural and extramedullary EES/ PNET compress the spinal cord, radiotherapy and chemotherapy may cause damage to the spinal cord nerves, and immediate decompression surgery may be necessary (21). In our case, the patient needed emergency decompression due to sudden numbness and weakness of both lower limbs. Then C7-T3 laminectomy was performed as an emergency operation. Moreover, en bloc resection is the standard procedure for EES/PNET, but in practice, most epidural EES/PNET cases are partially excised to preserve the nerve and await a definitive pathological diagnosis. The most common metastatic sites of EES/PNET are the lung and bone. In our case, after the complete removal of tumor tissue, the dura was intact and pulsatile. Postoperative radiotherapy and chemotherapy. Lung metastasis occurred after 6 months of follow-up, with no local recurrence, and died 8 months after surgery.
EES/PNET in the epidural space of the cervicothoracic junction is a malignant tumor with rapid progression and poor prognosis. We found, through the literature review, that a total of 7 children (including the case in this study) were followed up, and the case fatality rate was 57% (4/7) (Table 1). Factors involved in prognosis include tumor location, tumor volume, tumor resection rate, treatment response, time of onset, and presence of metastasis. The cause of death may be associated with an onset of symptoms 6 months prior to diagnosis and, a large tumor that, is located in the epidural space of the cervicothoracic junction. Incomplete surgical tumor resection may also be a reason for the high recurrence rate and low survival rate of patients (5, 22). In our case, since PET-CT was not performed, the patient may have had bone metastases in other parts of the body at the first admission. This may be the main reason for the occurrence of late lung metastases. Another reason may be the increased risk of secondary cancers, mainly treatment-induced acute myeloid leukemia (t-AML) or radiation-induced sarcomas, and breast and thyroid cancers, in pediatric EES/PNET patients after treatment (23). The lack of NGS technology to further clarify the pathological classification of Ewing's sarcoma may also contribute to the poor prognosis of patients.
Conclusion
Primary epidural tumors are mostly benign, such as spinal meningiomas and neuromas. Contrary to what has been previously thought, we report a case of malignant epidural EES/PNET at the cervicothoracic junction without bone destruction. Preoperative PET-CT scanning is important to determine whether the tumor has metastasized to other organs and to assess the patient's survival prognosis.
Data availability statement
The original contributions presented in the study are included in the article/Supplementary Material, further inquiries can be directed to the corresponding author.
Ethics statement
The studies involving human participants were reviewed and approved by Studies involving human participants were reviewed and approved by the Institutional Review Board of Yichun People’s Hospital (no. 2022220). Written informed consent to participate in this study was provided by the participants' legal guardian/next of kin. Written informed consent was obtained from the individual(s), and minor(s)' legal guardian/next of kin, for the publication of any potentially identifiable images or data included in this article.
Author contributions
J-ML and G-HZ, conceptualization and writing-original draft preparation; W-HX, Z-YH and X-JY, writing-review and editing; XG, methodology and validation; Z-YH and GL, investigation and resources; X-RG, supervision; S-SC, project administration. All authors contributed to the article and approved the submitted version.
Conflict of interest
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
Publisher's note
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
References
1. Hu X, Huang Q, Wang J, Li D, Wang P, Cai J. Case report: primary intracranial EWs/PNET in adults: clinical experience and literature review. Front Oncol. (2022) 12:1035800. doi: 10.3389/fonc.2022.1035800
2. Kampman WA, Kros JM, Jong THRD, Lequin MH. Primitive neuroectodermal tumours (PNETs) located in the spinal canal; the relevance, of classification as central or peripheral PNET. J. Neurooncol. (2006) 77(1):65–72.
3. Yasuda T, Suzuki K, Kanamori M, Hori T, Huang D, Bridge JA, et al. Extraskeletal Ewing's sarcoma of the thoracic epidural space: case report and review of the literature. Oncol Rep. (2011) 26: 711–5.
4. Ikhwan SM, Kenneth VK, Seoparjoo A, Zin AA. Primary extraskeletal Ewing's sarcoma/primitive neuroectodermal tumour of breast. BMJ Case Rep. (2013) 2013:bcr2013009584. doi: 10.1136/bcr-2013-009584
5. Kobayashi S, Takahashi J, Sakashita K, Fukushima M, Kato H. Ewing sarcoma of the thoracic epidural space in a young child. Eur Spine J. (2013) 22(3):373–9. doi: 10.1007/s00586-012-2481-y
6. Kutty Raja K, Anilkumar P, Sunilkumar Balakrishnan S, Krishna GB, Korde P, Jain SK. Ewing sarcoma of the cervical epidural space presenting with tetraplegia: case report and review of literature. World Neurosurg. (2017) 107:1046.e9–1046.e15. doi: 10.1016/j.wneu.2017.07.182
7. Klimo P, Codd PJ, Grier H, Goumnerova LC. Primary pediatric intraspinal sarcomas. J Neurosurg Pediatr. (2009) 4(3):222–9. doi: 10.3171/2009.3.PEDS08272
8. Mark B, Cheddhi T, Joshua F, Modrek AS, Bayin NS, Snuderl M, et al. Adult primary spinal epidural extraosseous Ewing's sarcoma: a case report and review of the literature. Case Rep Neurol Med. (2016) 2016:1–8. doi: 10.1155/2016/1217428
9. Izycka-Swieszewska E, Stefanowicz J, Debiec-Rychter M, Rzepko R, Borowska-Lehman J. Peripheral primitive neuroectodermal tumor within the spinal epidural space. Neuropathology. (2001) 21(3):218–21. doi: 10.1046/j.1440-1789.2001.00387.x
10. Virani MJ, Jain S. Primary intraspinal primitive neuroectodermal tumor (PNET): a rare occurrence. Neurol India. (2002) 50:75–80. PMID: 11960157
11. Harimaya K, Oda Y, Matsuda S, Tanaka K, Chuman H, Iwamoto Y. Primitive neuroectodermal tumor and extraskeletal Ewing sarcoma arising primarily around the spinal column. Spine. (2003) 28(19):E408–12. doi: 10.1097/01.BRS.0000085099.47800.DF
12. Erkutlu I, Buyukhatipoglu H, Alptekin M, Ozsarac C, Buyukbese I, Gok A. Primary spinal epidural extraosseous Ewing’s sarcoma mimicking a spinal abscess. Pediatr Hematol Oncol. (2007) 24(7):537–42. doi: 10.1080/08880010701534163
13. Duan XH, Ban XH, Bo L, Zhong XM, Guo RM, Zhang F, et al. Intraspinal primitive neuroectodermal tumor: imaging findings in six cases. Eur J Radiol. (2011) 80(2):426–31. doi: 10.1016/j.ejrad.2010.06.005
14. Qi W, Deng X, Liu T, Hou Y, Yang C, Wu L, et al. Comparison of primary spinal central and peripheral primitive neuroectodermal tumors in clinical and imaging characteristics and long-term outcome. World Neurosurg. (2016) 88:359–69. doi: 10.1016/j.wneu.2015.12.033
15. Kogawa M, Asazuma T, Iso K, Koike Y, Domoto H, Aida S, et al. Primary cervical spinal epidural extra-osseous Ewing's sarcoma. Acta Neurochir. (2004) 146(9):1051–3; discussion 1053. doi: 10.1007/s00701-004-0294-4
16. Bailey M, Mccabe M, Pal P, Agushi E, Karabatsou K. Cervical epidural extra-osseous Ewing sarcoma mimicking an epidural abscess. Br J Neurosurg. (2016) 30(1):113–4. doi: 10.3109/02688697.2015.1071337
17. Dome JS, Perlman E, Ritchey ML, Kalapurakal JA, Grundy P. Principles and practice of pediatric oncology. 5th ed. New York: Lippincott Williams and Wilkins (2006).
18. Kennedy JG, Eustace S, Caulfield R, Fennelly DJ, Hurson B, O'Rourke KS. Extraskeletal Ewing's sarcoma: a case report and review of the literature. Spine. (2000) 25(15):1996–9. doi: 10.1097/00007632-200008010-00022
19. Folpe AL, Goldblum JR, Rubin BP, Shehata BM, Liu W, Dei Tos AP. Morphologic and immunophenotypic diversity in Ewing family tumors: a study of 66 genetically confirmed cases. Am J Surg Pathol. (2005) 29(8):1025–33. doi: 10.1097/01.pas.0000167056.13614.62
20. Saeedinia S, Nouri M, Alimohammadi M, Morad H, Amirjamshidi A. Primary spinal extradural Ewing's sarcoma (primitive neuroectodermal tumor): reportof a case and meta-analysis of the reported cases inthe literature. Surg Neurol Int. (2012) 3:55. doi: 10.4103/2152-7806.96154
21. Indelicato DJ, Keole SR, Shahlaee AH, Morris CG, Gibbs CP Jr, Scarborough MT, et al. Spinal and paraspinal Ewing tumors. Int J Radiat Oncol Biol Phys. (2009) 76(5):1463–71. doi: 10.1016/j.ijrobp.2009.03.042
22. Bacci G, Ferrari S, Bertoni F, Rimondini S, Longhi A, Bacchini P, et al. Prognostic factors in nonmetastatic Ewing's sarcoma of bone treated with adjuvant chemotherapy: analysis of 359 patients at the istituto ortopedico rizzoli. J Clin Oncol. (2000) 18(1):4–11. doi: 10.1200/JCO.2000.18.1.4
23. Bacci G, Longhi A, Barbieri E, Ferrari S, Mercuri M, Briccoli A, et al. Second malignancy in 597 patients with Ewing sarcoma of bone treated at a single institution with adjuvant and neoadjuvant chemotherapy between 1972 and 1999. J Pediatr Hematol Oncol. (2005) 27(10):517–20. doi: 10.1097/01.mph.0000183270.28785.33
Keywords: extraosseous Ewing's sarcoma/primitive neuroectodermal tumor, children, cervicothoracic junction, case report, paralysis
Citation: Zhang G-H, Lin J-M, He Z-Y, Yuan X-J, Li G, Gan X-R, Xu W-H and Cao S-S (2023) A case of giant Ewing's sarcoma (EES)/primitive neuroectodermal tumor (PNET) of the cervicothoracic junction in children with incomplete paralysis of both lower limbs: Case report and literature review. Front. Surg. 9:1066304. doi: 10.3389/fsurg.2022.1066304
Received: 10 October 2022; Accepted: 5 December 2022;
Published: 6 January 2023.
Edited by:
Yang Lv, Peking University Third Hospital, ChinaReviewed by:
Zhuo Ran Sun, Peking University Third Hospital, ChinaShan Gao, Peking University Third Hospital, China
Yang Sun, Peking University, China
© 2023 Zhang, Lin, He, Yuan, Li, Gan, Xu and Cao. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Sheng-Sheng Cao MTU5NzUwNDc5MEBxcS5jb20=
†These authors have contributed equally to this work
Specialty Section: This article was submitted to Orthopedic Surgery, a section of the journal Frontiers in Surgery
 Gong-Heng Zhang†
Gong-Heng Zhang† Jun-Ming Lin
Jun-Ming Lin Zhen-Yu He
Zhen-Yu He