- 1Department of gynecology, Ningbo Women and Children's Hospital, Ningbo, China
- 2Department of gynecology, Zhuji People’s Hospital of Zhejiang Province, Zhuji, China
Objective: To explore the efficacy, safety, and prognostic factors of intensity modulated radiation therapy (IMRT) and three dimensional conformal radiation therapy (3D-CRT) combined with intracavitary posterior radiotherapy for medium-term and advanced cervical cancer.
Methods: Retrospectively analyze the clinical data of 104 patients with medium-term and advanced cervical cancer who were treated in the radiotherapy department of our hospital from September 2015 to March 2017. According to the different radiotherapy techniques, they were divided into the IMRT combined with intracavitary posterior radiotherapy group (n = 52) and the 3D-CRT combined with intracavitary posterior radiotherapy group (n = 52). Observe and compare the short-term efficacy, occurrence of adverse reactions and overall survival rate of the two groups. The clinicopathological characteristics of the survival group and the death group were compared, and univariate analysis and multiple logistic regression models were used to analyze the relationship between the clinicopathological characteristics and the patient’s prognosis.
Results: The total effective rate of IMRT combined with intracavitary posterior radiotherapy group was 96.15%, which was higher than that of 3D-CRT combined with intracavitary posterior radiotherapy group (88.46%), but the difference was not statistically significant (p > 0.05). The incidence of digestive system injury, thrombocytopenia, and radiation proctitis in the IMRT combined intracavitary posterior radiotherapy group was lower than that of the 3D-CRT combined intracavitary posterior radiotherapy group, and the differences were statistically significant (p < 0.05). The prognosis and survival of the two groups of patients were similar, and the difference was not statistically significant (p > 0.05). Pathological classification, clinical stage, and lymph node metastasis are independent influencing factors of 3-year prognosis in patients with medium-term and advanced cervical cancer (p < 0.05).
Conclusion: IMRT combined with intracavitary posterior radiotherapy is equivalent to 3D-CRT combined with intracavitary posterior radiotherapy, but it can reduce the incidence of adverse reactions in patients with medium-term and advanced cervical cancer, and has higher safety. Pathological typing, clinical staging, Lymph node metastasis were independent factor affecting the prognosis of patients. In clinical treatment, IMRT combined with intracavitary posterior radiotherapy is more recommended as a treatment plan for patients with medium-term and advanced cervical cancer.
Introduction
Cervical cancer is one of the most common malignant tumors in women. Early stage cervical cancer is usually treated with surgery, while radiotherapy and chemotherapy are the main treatments in the medium-term and advanced stages (1). At present, external irradiation combined with intracavitary posterior radiotherapy and concurrent chemotherapy is the standard method for the treatment of medium-term and advanced cervical cancer. Traditional radiotherapy methods such as four-field box-type and front-to-back penetrating irradiation have been used earlier and are widely used, but their damage to the digestive tract, urinary tract and hematopoietic systems is relatively serious (2, 3). Intensity modulated radiation therapy (IMRT) and three dimensional conformal radiation therapy (3D-CRT) are new radiotherapy techniques, and there is no unified understanding on the specific effects of these two techniques. However, studies have confirmed that these two techniques can increase the irradiation dose of target area and effectively reduce the irradiation dose of surrounding normal tissues and organs, effectively control tumors and reduce damage to the body (4, 5). Whether IMRT and 3D-CRT can replace traditional radiotherapy in the treatment of medium-term and advanced cervical cancer is worth looking forward to. Therefore, in this study, IMRT combined with intracavitary radiotherapy was used to treat patients with medium-term and advanced cervical cancer, and compared with 3D-CRT combined with intracavitary posterior radiotherapy, in order to provide theoretical support for the efficient treatment of patients with medium-term and advanced cervical cancer. The specific research is shown as follows.
Materials and Methods
General Information
A total of 104 patients with medium-term and advanced cervical cancer who were admitted to our hospital from September 2015 to March 2017 were selected. All patients met the diagnostic criteria for medium-term and advanced cervical cancer (6); Diagnosed by pathological and imaging examinations; tumor FIGO stage was IIB–IVA; Bian’s score was ≥70 points; expected survival >3 months; abnormal liver and kidney function and other organ diseases were excluded. According to the treatment method, the patients were divided into IMRT and 3D-CRT combined with intracavitary posterior radiotherapy groups, with 52 patients in each group. The age of IMRT combined with intracavitary posterior radiotherapy group was 32–77 years old, with an average age of (55.03 ± 7.14) years; 32 cases of IIB, 10 cases of IIIA, 9 cases of IIIB, and 1 case of IVA; 49 cases of squamous cell carcinoma and 3 cases of adenocarcinoma; 30 patients had tumor diameter ≥4 cm, and 22 patients had tumor diameter <4 cm. The age of 3D-CRT combined with intracavitary posterior radiotherapy group was 33–78 years old, with an average of (54.86 ± 7.25) years old; 34 cases of IIB, 9 cases of IIIA, 8 cases of IIIB, and 1 case of IVA; 50 cases of squamous cell carcinoma and 2 cases of adenocarcinoma; 29 patients had tumor diameter ≥4 cm, and 23 patients had tumor diameter <4 cm. There was no statistical difference in general clinical data such as age, FIGO stage, pathological classification and tumor diameter between the two groups (p > 0.05), which were comparable.
Research Methods
In terms of the IMRT combined with intracavitary posterior radiotherapy group: One day before localization, the patients underwent bowel preparation by oral administration of Meglumine. Before localization, the patients’ bladder was filled and the rectum was emptied. The joints were fixed with vacuum pad and thermoplastic film, and CT scan was performed. Clinical target volume (CTV): including the primary area of cervical tumor (parametrial triangle, cervix, vagina, etc.) and pelvic metastatic area (parametrium, paravaginal tissue, pelvic lymphatic area, etc.). Planned target volume (PTV): CTV was expanded by 5 mm in the S/I, A/P, and R/L directions, respectively. Gross tumor target volume (GTV): the cervical mass and lymph node metastases that have been diagnosed by imaging or definite diagnosis. Lymph node area delineation: The lymph node area and corresponding blood vessel area were delineated along the lymph node area and the corresponding blood vessel area in patients diagnosed with lymph node metastasis, followed by delineation of the para-aortic lymph nodes, anterior iliac, external iliac, internal iliac, common iliac and obturator foramen. The range was from the fifth lumbar vertebra to the obturator foramen. The PTV dose was 1.8 Gy/time, and the total dose was 48.60–50.40 Gy/27–28, 5 times a week. PTV adopted 7-field intensity-modulated irradiation, and was irradiated with an isodose curve of 95% of PTV, and the minimum and maximum doses of the target area were within the range of ±10% of the prescribed dose. After 25 times of external irradiation, the irradiation was stopped, intracavitary posterior radiotherapy was performed once a week, 6–7 Gy/time, with a total dose of 30–36 Gy/5–6 f. The radiation doses of the small intestine, rectum and bladder were V45 < 20%, V45 < 40% and V45 < 30%, respectively.
In terms of the 3D-CRT combined with intracavitary posterior radiotherapy group: the positioning and target delineation methods were the same as above. The target area was irradiated by four-field box type, 6MV-X-ray, 180–200 cGy/time, the total dose was 4,500–5,000 cGy. Conventional segmentation irradiation, 5 times a week. The method of intracavitary posterior radiotherapy was the same as above.
Observation indicators: The short-term efficacy and adverse reactions of the two groups of patients were recorded, analyzed and compared, and the adverse reactions included acute and chronic radiation injury. Acute and chronic radiation injuries were divided into grades I, II, III, and IV. The higher the grade, the more severe the adverse reaction. Acute radiation injury included digestive tract, blood, and urinary system injury; chronic radiation injury was mainly intestinal and urinary system injury, including radiation cystitis and proctitis. After radiotherapy, consolidation chemotherapy was performed according to the specific conditions of the patients. During hospitalization, the patients were regularly checked for blood routine every week. In the event of an acute chemoradiotherapy reaction, medical staff need to timely treat the symptoms according to the specific conditions of the patient.
Efficacy evaluation: The changes in tumor size were observed by CT or MRI, and graded according to the WHO efficacy evaluation criteria. including disease progression (PD): the product of the largest vertical diameter and the largest diameter of the lesion (the product of the two diameters) increased by more than 25% compared with that before radiotherapy, and time continued more than 30 days; stable disease (SD): the two-dimensional product of the lesion decreased by less than 50% or increased by less than 25% compared with that before radiotherapy, and lasted for more than 30 days; partial remission (PR): the two-dimensional product of the lesion decreased by at least 50% compared with that before radiotherapy, duration of more than 30 days; complete remission (CR): the lesions completely disappeared, the duration of more than 30 days. Total effective rate = (PR + CR) / total number of cases × 100%.
Follow-up: Patients were regularly followed up every 3 months by outpatient or telephone, all patients were followed up for 3 years. The follow-up contents included patient survival time and adverse reactions. Survival time was calculated from the time of diagnosis to the date of death or the end of follow-up.
Statistical Methods
SPSS 22.0 software was used for processing. The measurement data conforming to normal distribution were expressed as mean ± standard deviation, and t test was used for comparison. Count data were expressed as (%), and χ2 test was used for comparison. Survival curves were drawn by using the Kaplan-Meier method. The test level was α = 0.05, and p < 0.05 was considered statistically significant.
Results
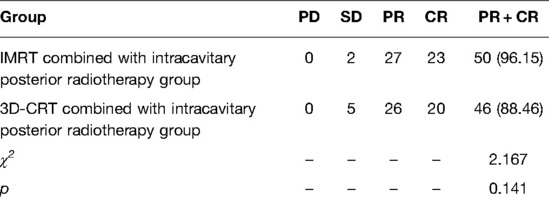
Comparison of Short-Term Curative Effect between Two Groups of Patients
The results showed that the total effective rate of IMRT combined with intracavitary posterior radiotherapy group was 96.15%, which was higher than that of 3D-CRT combined with intracavitary posterior radiotherapy group (88.46%), but the difference was not statistically significant (p > 0.05), as shown in Table 1.
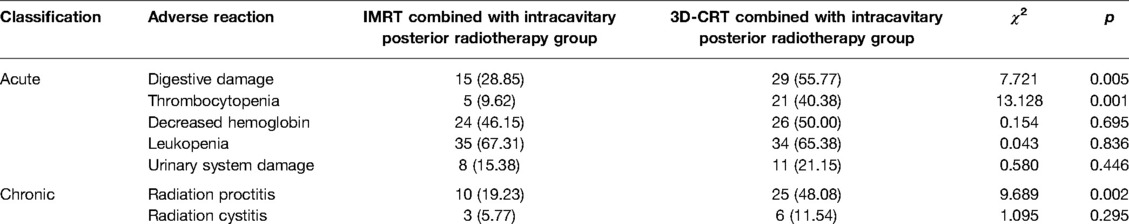
Comparison of Adverse Reactions of the Two Groups of Patients
The results showed that the incidence of digestive system injury, thrombocytopenia, and radiation proctitis in the IMRT combined with intracavitary posterior radiotherapy group were 28.85%, 9.62%, and 19.23%, respectively, which were lower than those in the 3D-CRT combined with intracavitary posterior radiotherapy group (55.77%, 40.38%, 48.08%), the differences were statistically significant (p < 0.05). There was no significant difference in the incidence of hemoglobin reduction, leukopenia, urinary system injury and radiation cystitis between the two groups (p > 0.05), as shown in Table 2.
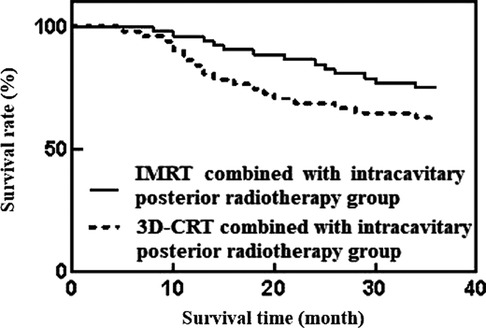
Comparison of Prognosis and Survival between the Two Groups of Patients
The results showed that during the 3-year follow-up, the total number of deaths was 32 cases. Among them, the mortality rate of IMRT combined with intracavitary posterior radiotherapy was 25.00% (13/52) lower than that of 3D-CRT combined with intracavitary posterior radiotherapy group, which was 36.54% (19/52), and the median survival time of both groups was 36 months. The difference was not statistically significant (p > 0.05), as shown in Figure 1.
Analysis of Prognostic Factors of Patients with Medium-Term and Advanced Cervical Cancer
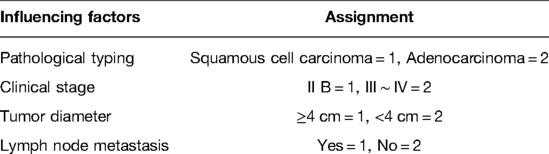
The results showed that there were significant differences in case type, clinical stage, tumor diameter, and lymph node metastasis between the survival group and the death group (p < 0.05). There was no statistically significant difference in age (p > 0.05) as shown in Table 3.
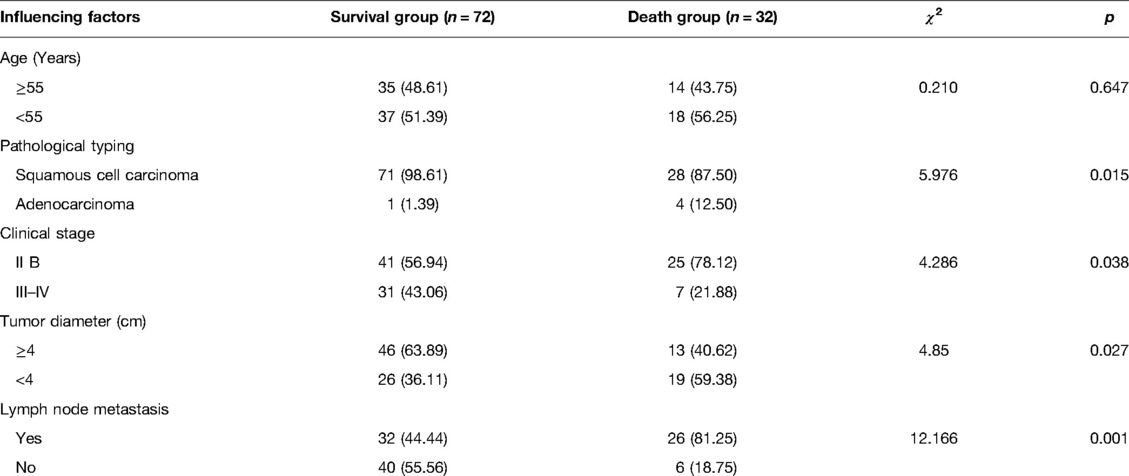
Table 3. Analysis of prognostic factors of patients with medium-term and advanced cervical cancer (n, %).
Multivariate Analysis of Prognosis of Patients with Medium-Term and Advanced Cervical Cancer
Logistic regression analysis showed that pathological type, clinical stage and lymph node metastasis were independent influencing factors of 3-year prognosis of patients with medium-term and advanced cervical cancer (p < 0.05), while tumor diameter had no significant effect on 3-year prognosis of patients (p > 0.05), as shown in Tables 4 and 5.
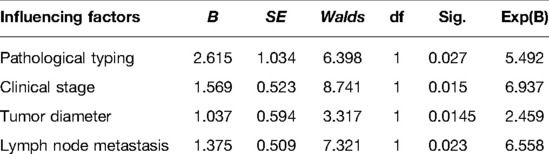
Table 5. Multivariate analysis of prognosis of patients with medium-term and advanced cervical cancer.
Discussion
The incidence of cervical cancer is increasing year by year, and the patients tend to be younger. Therefore, it is particularly important to reduce the mortality rate of cervical cancer and control the development of cervical cancer (7). External beam radiation combined with intracavitary radiotherapy and concurrent chemotherapy in the treatment of medium-term and advanced cervical cancer can prevent tumor metastasis and local recurrence. The scope of external irradiation not only includes the uterus, paracyngeal tissues, cervix and vagina, but also needs to cover the pelvic lymphatic drainage area (8, 9). Traditional external irradiation techniques are relatively backward, and the incidence of various complications has increased, which has been gradually replaced by IMRT, 3D-CRT and other new radiotherapy technologies (10).
3D-CRT is based on the reconstruction of three-dimensional image of human body structure, and can accurately distinguish normal tissue and tumor tissue. The radiation dose of the rectum, bladder and other organs at risk can be reduced by adjusting the radiation direction and changing the radiation dose (11). IMRT is an in vitro three-dimensional irradiation method developed through improved 3D-CRT technology. By adjusting the output dose, the radiation shape in all three-dimensional directions can be kept consistent with the target area, and the radiation dose of organs at risk and normal tissues around the target area can be reduced. so as to effectively treat and control tumors (12). Compared with 3D-CRT technology, IMRT technology can better adapt to irregularly shaped tumors, and at the same time, by controlling the dose intensity, a high-dose target area can be concentrated in the target area (13). IMRT can reduce the acute myelosuppression and other reactions caused by concurrent chemotherapy, which can reduce the harm to surrounding tissues and reduce the occurrence of various complications.
IMRT and 3D-CRT are widely used in cancer treatment. Guillemin et al. (14) used IMRT and 3D-CRT in the treatment of non-small cell lung cancer and found that IMRT can more effectively reduce the radiation dose to the surrounding organs at risk of patients. In cervical cancer, Contreras’ team (15) found that IMRT can reduce the amount of rectal and bladder tissue around the tumor, ensure the coverage of tumor tissue, and alleviate complications caused by radiotherapy. This study found that the total effective rate of IMRT combined with intracavitary posterior radiotherapy was higher than that of 3D-CRT combined with intracavitary posterior radiotherapy, but the difference was not statistically significant. There was no significant difference in the overall survival rate and median survival time between the two groups. The results showed that the treatment efficacy of the two regimens were equivalent. However, the incidences of gastrointestinal tract injury, thrombocytopenia and subsequent radiation proctitis in the IMRT combined with intracavitary posterior radiotherapy group were significantly lower than those in the 3D-CRT combined with intracavitary posterior radiotherapy group. This suggested that when all conditions of intracavitary posterior radiotherapy were the same, IMRT can relieve gastrointestinal and hematological injury, with higher safety.
The results of this study showed that pathological type, clinical stage and lymph node metastasis were independent prognostic factors for patients with medium-term and advanced cervical cancer. Among them, patients with squamous cell carcinoma, late clinical stage, and lymph node metastasis have higher mortality rates. This may be related to the fact that the cancer cells of squamous cell carcinoma patients have invaded into the muscle layer, the distance from the radiation source is far, patients with advanced staging have increased tumor uncontrollability, and patients with lymph node metastasis have wider tumor distribution (16, 17). Yüksel et al. (18), Ramlov et al. (19) found that case typing, tumor size, lymph node metastasis, etc. are all risk factors for the prognosis of patients with medium-term and advanced cervical cancer. However, this study showed that tumor size was not a prognostic factor for patients with medium-term and advanced cervical cancer, which was partially deviated from previous studies. This may be related to the small sample size and short follow-up time in this study. It is necessary to expand the sample size and extend the follow-up time in the future to improve the credibility of the research results.
In conclusion, IMRT combined with intracavitary posterior radiotherapy has the same curative effect as 3D-CRT combined with intracavitary posterior radiotherapy, but it can reduce the incidence of adverse reactions of patients with medium-term and advanced cervical cancer and has higher safety. Pathological type, clinical stage, and lymph node metastasis are independent factors affecting the prognosis of patients. In clinical treatment, IMRT combined with intracavitary posterior radiotherapy is more recommended as the treatment plan for patients with medium-term and advanced cervical cancer.
Data Availability Statement
The original contributions presented in the study are included in the article/Supplementary Material, further inquiries can be directed to the corresponding author/s.
Ethics Statement
The studies involving human participants were reviewed and approved by This study was approved by the ethics committee of our hospital. The patients/participants provided their written informed consent to participate in this study.
Author Contributions
The first author is KY, he is responsible for the writing, research design, data analysis of the article. LZ is responsible for the guidance of the entire research. All authors contributed to the article and approved the submitted version.
Conflict of Interest
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest
Publisher's Note
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
References
1. Williamson CW, Liu HC, Mayadev J, Mell LK. Advances in external beam radiation therapy and brachytherapy for cervical cancer. Clin Oncol (R Coll Radiol). (2021) 33:567–78. doi: 10.1016/j.clon.2021.06.012
2. Lee J, Lin JB, Chang CL, Sun FJ, Wu MH, Jan YT, et al. Impact of para-aortic recurrence risk-guided intensity-modulated radiotherapy in locally advanced cervical cancer with positive pelvic lymph nodes. Gynecol Oncol. (2018) 148:291–8. doi: 10.1016/j.ygyno.2017.12.003
3. Ping Q, Zeng J, Sun P, Qu P, Jiang S, Hu Y. Efficacy of preoperative brachytherapy for controlling vaginal bleeding in early-stage cervical cancer: a retrospective study. Transl Cancer Res. (2021) 10:3259–67. doi: 10.21037/tcr-21-467
4. Yang H, Feng C, Cai BN, Yang J, Liu HX, Ma L. Comparison of three-dimensional conformal radiation therapy, intensity-modulated radiation therapy, and volumetric-modulated arc therapy in the treatment of cervical esophageal carcinoma. Dis Esophagus. (2017) 30:1–8. doi: 10.1111/dote.12497
5. Arul Ponni TR, Avinash HU, Nirmala S, Janaki MG, Kirthi Koushik AS. Optimal technique of radiotherapy for carcinoma cervix in developing countries: dosimetric and logistic comparison. J Cancer Res Ther. (2018) 14:1207–13. doi: 10.4103/jcrt.JCRT_454_17
6. Massad LS, Einstein MH, Huh WK, Katki HA, Kinney WK, Schiffman M, et al. 2012 updated consensus guidelines for the management of abnormal cervical cancer screening tests and cancer precursors. Obstet Gynecol. (2013) 121:829–46. doi: 10.1097/AOG.0b013e3182883a34
7. Aghili M, Andalib B, Karimi Moghaddam Z, Maddah Safaie A, Amoozgar Hashemi F, Mousavi Darzikolaie N. Concurrent chemo- radiobrachytherapy with cisplatin and medium dose rate intra- cavitary brachytherapy for locally advanced uterine cervical cancer. Asian Pac J Cancer Prev. (2018) 19:2745–50. doi: 10.22034/APJCP.2018.19.10.2745
8. Yu H, Zhang L, Li D, Liu N, Yin Y, Zhang L, et al. Postoperative adjuvant chemotherapy combined with intracavitary brachytherapy achieved the equivalent survival compared with concurrent chemoradiotherapy in cervical cancer patients with intermediate-risk. Jpn J Clin Oncol. (2019) 49:714–8. doi: 10.1093/jjco/hyz057
9. Xiang J, Liu F, Wang B, Chen L, Liu W, Tan S. A literature review on maillard reaction based on milk proteins and carbohydrates in food and pharmaceutical products: advantages, disadvantages, and avoidance strategies. Foods. (2021) 10:1998. doi: 10.3390/foods10091998
10. Mohanty SK, Chopra S, Mudaliar A, Kannan S, Mahantshetty U, Engineer R, et al. A comparative analysis of quality of life after postoperative intensity-modulated radiotherapy or three-dimensional conformal radiotherapy for cervical cancer. Indian J Cancer. (2018) 55:327–35. doi: 10.4103/ijc.IJC_453_17
11. Dracham CB, Mahajan R, Rai B, Elangovan A, Bhattacharya T, Ghoshal S. Toxicity and clinical outcomes with definitive three-dimensional conformal radiotherapy (3DCRT) and concurrent cisplatin chemotherapy in locally advanced cervical carcinoma. Jpn J Clin Oncol. (2019) 49:146–52. doi: 10.1093/jjco/hyy164
12. Shang H, Pu Y, Wang W, Dai Z, Jin F. Evaluation of plan quality and robustness of IMPT and helical IMRT for cervical cancer. Radiat Oncol. (2020) 15:34. doi: 10.1186/s13014-020-1483-x.32054496
13. Lin Y, Chen K, Lu Z, Zhao L, Tao Y, Ouyang Y, et al. Intensity-modulated radiation therapy for definitive treatment of cervical cancer: a meta-analysis. Radiat Oncol. (2018) 13:177. doi: 10.1186/s13014-018-1126-7
14. Guillemin F, Berger L, Lapeyre M, Bellière-Calandry A. Dosimetric and toxicity comparison of IMRT and 3D-CRT of non-small cell lung cancer. Cancer Radiother. (2021) 25:747–54. French. doi: 10.1016/j.canrad.2021.03.001
15. Contreras J, Srivastava A, Chundury A, Schwarz JK, Markovina S, Thaker PH, et al. Long-term outcomes of intensity-modulated radiation therapy (IMRT) and high dose rate brachytherapy as adjuvant therapy after radical hysterectomy for cervical cancer. Int J Gynecol Cancer. (2020) 30:1157–61. doi: 10.1136/ijgc-2020-001412
16. Xu XH, Chen YC, Xu YL, Feng ZL, Liu QY, Guo X, et al. Garcinone E blocks autophagy through lysosomal functional destruction in ovarian cancer cells. World J Tradit Chin Med. (2021) 7:209–16. doi: 10.4103/wjtcm.wjtcm_83_20
17. Aslan K, Haberal A, Akıllı H, Meydanli MM, Ayhan A. Prognostic value of the number of the metastatic lymph nodes in locally early-stage cervical cancer: squamous cell carcinoma versus non-squamous cell carcinoma. Arch Gynecol Obstet. (2021) 304:1279–89. doi: 10.1007/s00404-021-06030-w
18. Yüksel D, Karataş Şahin E, Ünsal M, Çakır C, Kılıç Ç, Kimyon Cömert G, et al. The prognostic factors in 384 patients with FIGO 2014 stage IB cervical cancer: what is the role of tumor size on prognosis? Eur J Obstet Gynecol Reprod Biol. (2021) 266:126–32. doi: 10.1016/j.ejogrb.2021.09.028
Keywords: medium-term and advanced cervical cancer, intensity modulated radiation therapy, three-dimensional conformal radiotherapy, efficacy, prognosis
Citation: Yu K and Zhou L (2022) Intensity-Modulated Radiotherapy and Three-Dimensional Conformal Radiotherapy Combined with Intracavitary Posterior Radiotherapy for the Treatment of Medium-Term and Advanced Cervical Cancer: Efficacy, Safety and Prognostic Factors. Front. Surg. 9:906117. doi: 10.3389/fsurg.2022.906117
Received: 28 March 2022; Accepted: 20 April 2022;
Published: 23 May 2022.
Edited by:
Songwen Tan, Central South University, ChinaReviewed by:
Li Genlin, The First Affiliated Hospital, University of South China, ChinaLihong Chen, The First Affiliated Hospital of Fujian Medical University, China
Copyright © 2022 Yu and Zhou. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Liping Zhou ZXRlcm5hbHpscEAxNjMuY29t
Specialty section: This article was submitted to Visceral Surgery, a section of the journal Frontiers in Surgery
 Kewen Yu1
Kewen Yu1 Liping Zhou
Liping Zhou