- 1Department of Orthopedics, Kaohsiung Veterans General Hospital, Kaohsiung, Taiwan
- 2Division of Nephrology, Department of Internal Medicine, Kaohsiung Veterans General Hospital, Kaohsiung, Taiwan
- 3Department of Medical Education and Research, Kaohsiung Veterans General Hospital, Kaohsiung, Taiwan
- 4Department of Pharmacy, School of Pharmacy, Kaohsiung Medical University, Kaohsiung, Taiwan
- 5Department of Occupational Therapy, Shu-Zen Junior College of Medicine and Management, Kaohsiung, Taiwan
- 6Department of Biomedical Engineering, I-Shou University, Kaohsiung, Taiwan
Background: Distal radius fractures are treated using open reduction and internal fixation and using general anesthesia (GA) or regional blocks. A new technique, wide-awake local anesthesia with no tourniquet (WALANT), allows this operation to be conducted in nonsedated patients without the use of tourniquets.
Objective: We analyzed whether WALANT yields better outcomes than GA in the treatment of patients with distal radius fractures.
Evidence Review: We searched the PubMed, Cochrane Library, Embase, and Scopus databases for cases of distal radius fractures treated using WALANT or GA. The outcomes of interest were duration of preparation for surgery, duration of surgery, blood loss, and length of postoperative hospitalization; visual analog scale (VAS), Mayo wrist score, and Quick Disabilities of the Arm, Shoulder and Hand (QuickDASH) questionnaire score on postoperative day 1; range of motion (ROM); time until bone union; and complication rate.
Findings: We systematically reviewed 4 studies with a total of 263 patients (128 with WALANT and 135 with GA). In comparison with GA, WALANT required less time for preparation for surgery, shorter postoperative hospitalization, and lower postoperative day 1 VAS scores; however, blood loss was greater. Functional outcomes (ROM, QuickDASH score, and Mayo wrist score), complication rates, and times until union did not differ considerably between the two methods.
Conclusion: The included studies demonstrated that durations of preparation for surgery and postoperative hospitalization were shorter and pain on postoperative day 1 was less severe with WALANT than with GA. Although blood loss in surgery was greater with WALANT, this technique is a novel and promising alternative to GA.
Highlights
A meta-analysis and systematic review compared wide-awake local anesthesia with no tourniquet (WALANT) versus general anesthesia (GA) in patients with a distal radius fracture.
WALANT is a promising alternative to GA for its reliable, cost-effective, and time-saving qualities, especially in older patients and those with various comorbidities.
Durations of preparation for surgery and postoperative hospitalization were shorter and pain on postoperative day 1 was less severe with WALANT than with GA.
Introduction
Distal radius fracture, a common upper-limb injury worldwide, has a bimodal age distribution pattern: It tends to occur in young adults with high-energy trauma and in older adults with osteoporosis (1). Open reduction and internal fixation provide immediate stability to support patients’ quick return to daily life and regular work. Such fixation with plates can be performed by administering regional blocks (e.g., Bier’s block and brachial plexus block) or general anesthesia (GA) to patients. With both types of anesthesia, a tourniquet can be used to control bleeding and provide a clear surgical field. However, administering regional blocks is technically demanding and requires special equipment, and GA can be dangerous in patients at high risk for complications (2).
A new method of administering anesthesia, wide-awake local anesthesia with no tourniquet (WALANT), was conceived by Lalonde et al. (3) The WALANT technique involves the local administration of lidocaine and epinephrine into the surgical field, thereby allowing to conduct the operation without using sedation or tourniquets (4). It is used mainly in numerous hand and wrist procedures such as trigger finger (5), carpal tunnel release (6), wrist arthroscopy for triangular fibrocartilage complex repair (7), radial forearm perforator flap (8), tendon repair or transfer (9, 10), and internal fixation or implant removal for metacarpal fractures (11).
In comparison with GA, WALANT can be performed in older patients and in those with various comorbidities. Intraoperative anesthetic monitoring is not required, and hand or wrist function can be assessed in real time with the cooperation of nonsedated patients (12). Furthermore, it precludes not only postoperative pain and swelling of soft tissues caused by the tourniquet (13) but also anesthetic care after surgery and complications such as nausea and vomiting caused by GA. Therefore, WALANT is more cost-effective because postoperative hospitalization is reduced (14) and the services of anesthesiologists and preoperative testing for sedation are not required (15).
Fixation of distal radius fractures necessitates a wide surgical field and complicated bony procedures. Therefore, our concern is whether WALANT is a feasible alternative to GA in surgical treatment. To compare the effectiveness of WALANT with that of GA in surgical treatment, we conducted a systematic review and meta-analysis. The outcomes of interest were duration of preparation for surgery, duration of surgery, blood loss, and duration of postoperative hospitalization; visual analog scale (VAS) score, Mayo wrist score, and Quick Disabilities of the Arm, Shoulder and Hand (QuickDASH) questionnaire score on postoperative day 1; range of motion (ROM), measured by wrist flexion and wrist extension; time until bone union; and complication rate.
Methods
Search Strategy
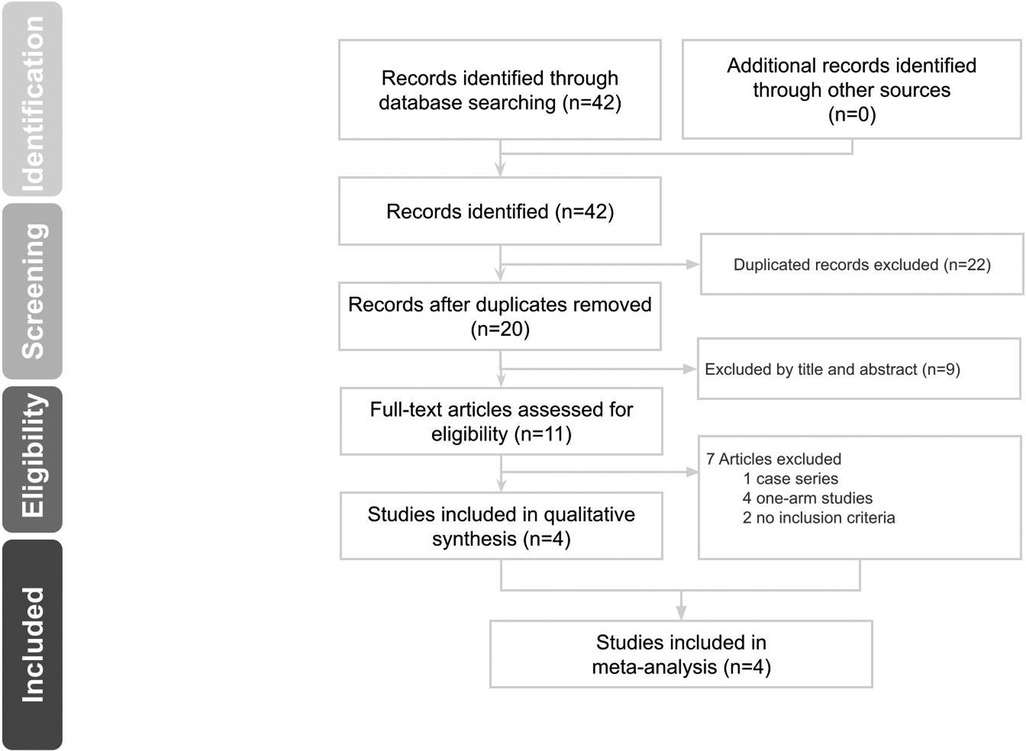
The study was conducted according to the Preferred Reporting Items for Systematic Review and Meta-Analysis guidelines. We searched the PubMed, the Cochrane Library, Embase, and Scopus databases for publications up to February 10, 2021, with the following search terms: “distal radius fracture,” “wide-awake local anesthesia no tourniquet,” and “WALANT” (search details are listed in the supplement). Randomized controlled trials (RCTs) and cohort studies were included, as were studies in which distal radius fractures were treated using a surgical intervention and WALANT or GA. Perioperative variables and clinical outcomes were included. Comments, letters, case reports, case series, editorials, proceedings, and personal communications were excluded. The search strategies are illustrated in the supplement. We also manually searched the reference lists of the relevant studies to retrieve additional studies. No language or date restriction was applied in this systematic search.
Because a meta-analysis does not involve human subjects, institutional review board review, ethical approval, and informed consent were not required.
Study Selection and Data Extraction
Studies were reviewed and selected by two independent reviewers. When study eligibility was uncertain, a third reviewer was consulted. The following information was extracted from the included studies: the name of the first author, year of publication, study design, sample size, participants’ ages, follow-up period, distal radius fracture classification, WALANT solutions, injection procedure, postoperative medication regimen, and surgical outcomes.
Quality Assessment
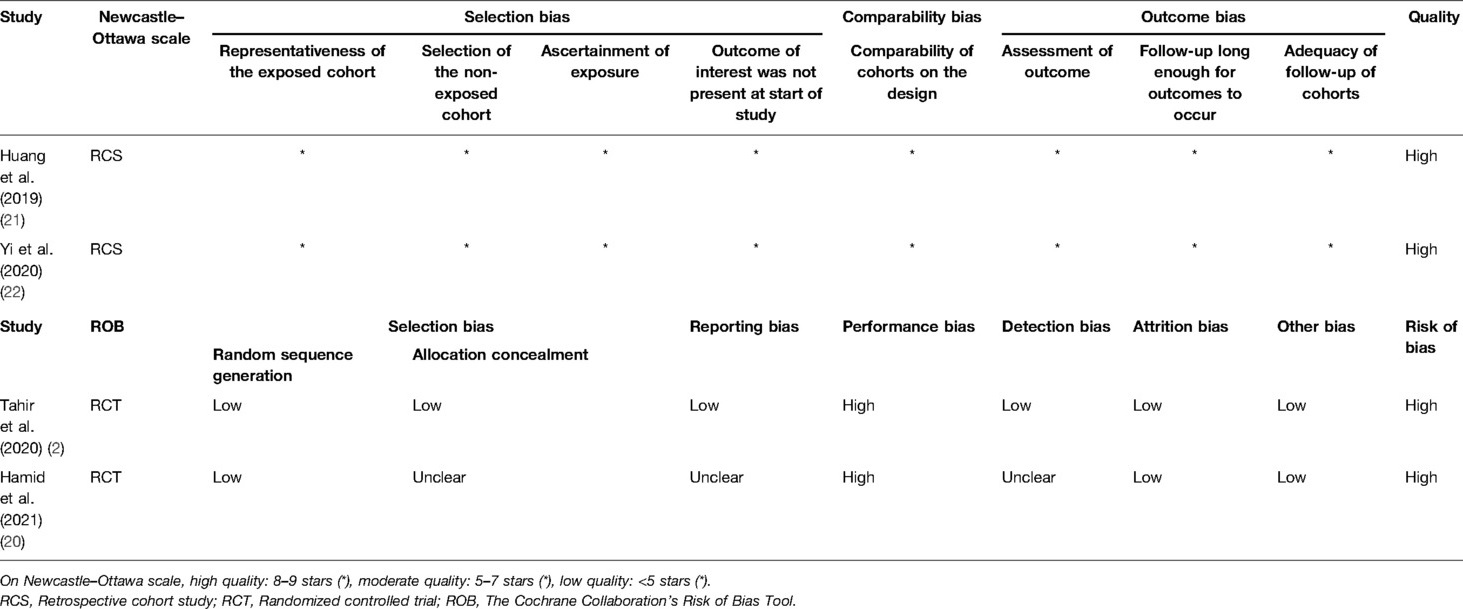
Two independent reviewers used the Newcastle–Ottawa Scale to assess the quality of the included retrospective cohort studies in terms of the selection bias (four items), comparability bias (one item), and outcome bias (three items). With the exception of one comparability item that was rated a maximum of two stars, each item was assigned one star at most if the quality of the study was high. The highest possible rating on the Newcastle–Ottawa Scale is 9 stars. A study with a score of 8 or 9 stars was recognized as high quality; 5–7 stars, as moderate or low quality; and fewer than 5 stars, as poor quality. After reviewers independently rated all studies, any disagreements were resolved through discussion.
RCTs were appraised by the Cochrane Collaboration’s Risk of Bias Tool (16) in the following six categories: (1) selection bias (use of random sequencing generation), (2) selection bias (use of allocation concealment), (3) detection bias (degree of “blinding” of outcome assessment), (4) performance bias (degree of “blinding” of participants and personnel), (5) attrition bias (presence of incomplete outcome data), and (6) reporting bias (as selective reporting). Each category was provided with one of three ratings: low, high, and unclear risk of bias. The overall risk of bias was considered low when all domains were rated as having a low risk of bias. It was considered unclear if at least one domain was considered to have an unclear risk of bias, but no domain was rated as having a high risk of bias; the overall risk of bias was otherwise considered high. After all studies were rated independently, any disagreements were resolved through discussion.
Outcome Measures
Outcomes of interest were perioperative variables and clinical outcomes such as duration of preparation for surgery, duration of surgery, blood loss, and length of postoperative hospitalization; VAS score, Mayo wrist score, and QuickDASH score on postoperative day 1; ROM, measured by wrist flexion and wrist extension; time to bone union; and complication rate.
Statistical Analysis
For the assessment of continuous data, we used mean differences (MDs) with corresponding 95% confidence intervals (CIs). For the assessment of dichotomous data, we used relative risk and 95% CIs. A p value of <0.05 was considered statistically significant. To assess the heterogeneity of the studies, we used Cochran’s Q test with the Ι2 statistic. The Ι2 values were defined as follows: 0%–24% heterogeneity was considered low; 25%–49% heterogeneity was considered moderate; 50%–74% heterogeneity was considered high; and 75%–100% heterogeneity was considered extremely high. Because the number of studies included in the meta-analysis was small, heterogeneity tests had low statistical power (17), and because we observed heterogeneity between studies, random-effects models were conservatively applied for the meta-analysis (18). In addition, the National Research Council recommended the use of random-effects approaches for meta-analyses and the exploration of sources of variation in study results (19). Pooled effects sizes were calculated, and a two-sided p value of <0.05 was considered to indicate statistical significance. We used the statistical software Comprehensive Meta-Analysis, version 3.0 (Biostat, Englewood, NJ, USA) to perform all analyses.
Results
Search Results
We identified 42 potentially eligible studies in the initial search (Figure 1). We excluded 22 duplicates and 9 irrelevant studies by reviewing titles and abstracts. The remaining 11 studies underwent full-text review, and 7 were excluded because they were case series or one-arm studies or had different inclusion criteria. Four studies (2, 20–22) were thus included in the systematic review.
Study Characteristics
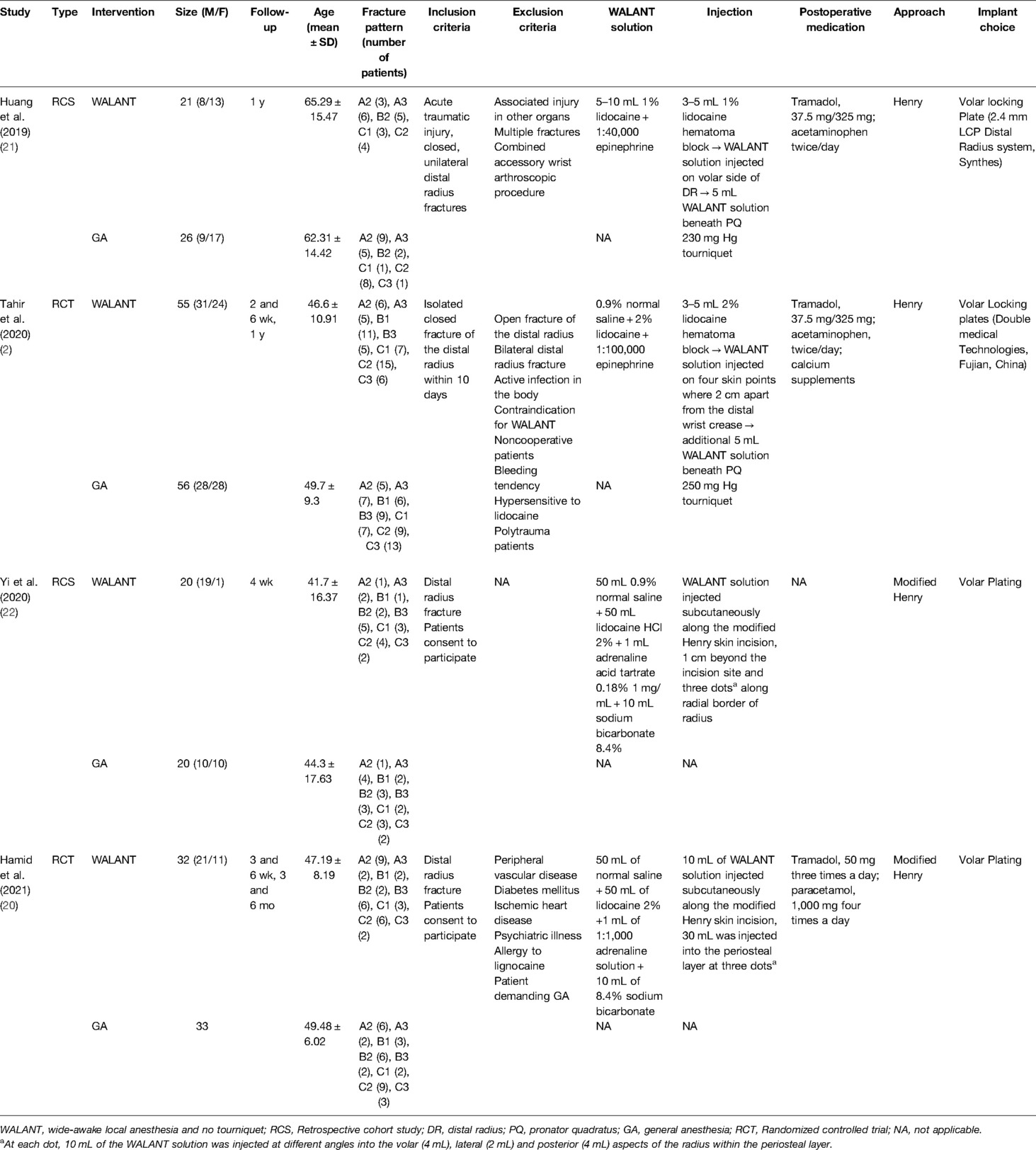
Table 1 summarizes the main demographics of these four studies. Huang et al. (21) and Yi et al. (22) conducted retrospective cohort studies, and Tahir et al. (2) and Hamid et al. (20) conducted RCTs. The total number of patients in these studies was 263; 128 underwent surgery with WALANT, and 135 with GA. The Arbeitsgemeinschaft für Osteosynthesefragen (AO)/Orthopedic Trauma Association (OTA) classification varied across studies; with C2 fractures being the most common (22.1%), followed by A2 fractures (15.2%). The mean ages of patients among the studies ranged from 41 to 65 years. The lengths of follow-up ranged from 4 weeks to 1 year.
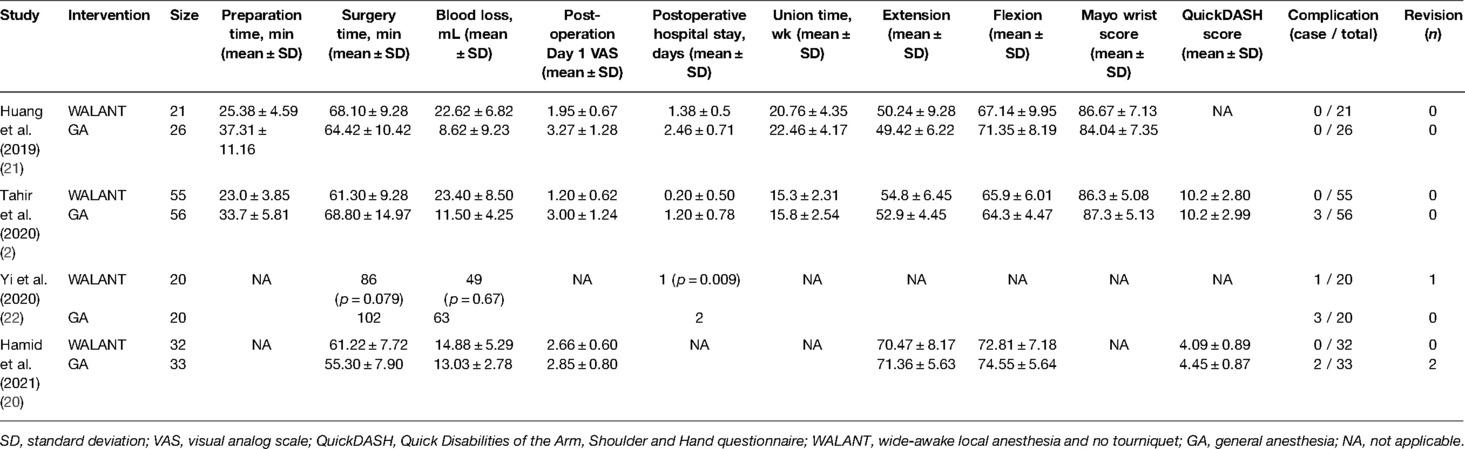
Summary of Outcomes
Table 2 lists the outcomes of interest in each study. Preparation time for surgery was considerably shorter with WALANT than with GA in the studies conducted by Tahir et al. (2) and Huang et al. (21); duration of surgery was considerably longer with WALANT in Hamid et al.’s study (20) but substantially shorter in Tahir et al.’s study (2) Blood loss was considerably greater with WALANT in the studies conducted by Tahir et al. (2) and Huang et al. (21) Duration of hospitalization was substantially shorter after surgery with WALANT in the studies conducted by Tahir et al. (2), Huang et al. (21), and Yi et al. (22) VAS scores were considerably lower 1 day after surgery with WALANT in the studies conducted by Tahir et al. (2) and Huang et al. (21); the QuickDASH score was substantially lower (which indicates better functional outcome) after surgery with WALANT in Hamid et al.’s study (20); in all these studies, Mayo wrist scores, wrist flexion, wrist extension, time to bone union, and complication rates did not differ between patients who underwent surgery using WALANT and surgery using GA. The total complication rate was 0.8% after surgery using WALANT (1 of 128 patients) and 5.9% after surgery using GA (8 of 135 patients). The proportions of patients requiring revision surgery were 0.8% after initial surgery with WALANT (1 of 128 patients) and 1.5% after surgery with GA (2 of 135 patients).
Meta-Analysis
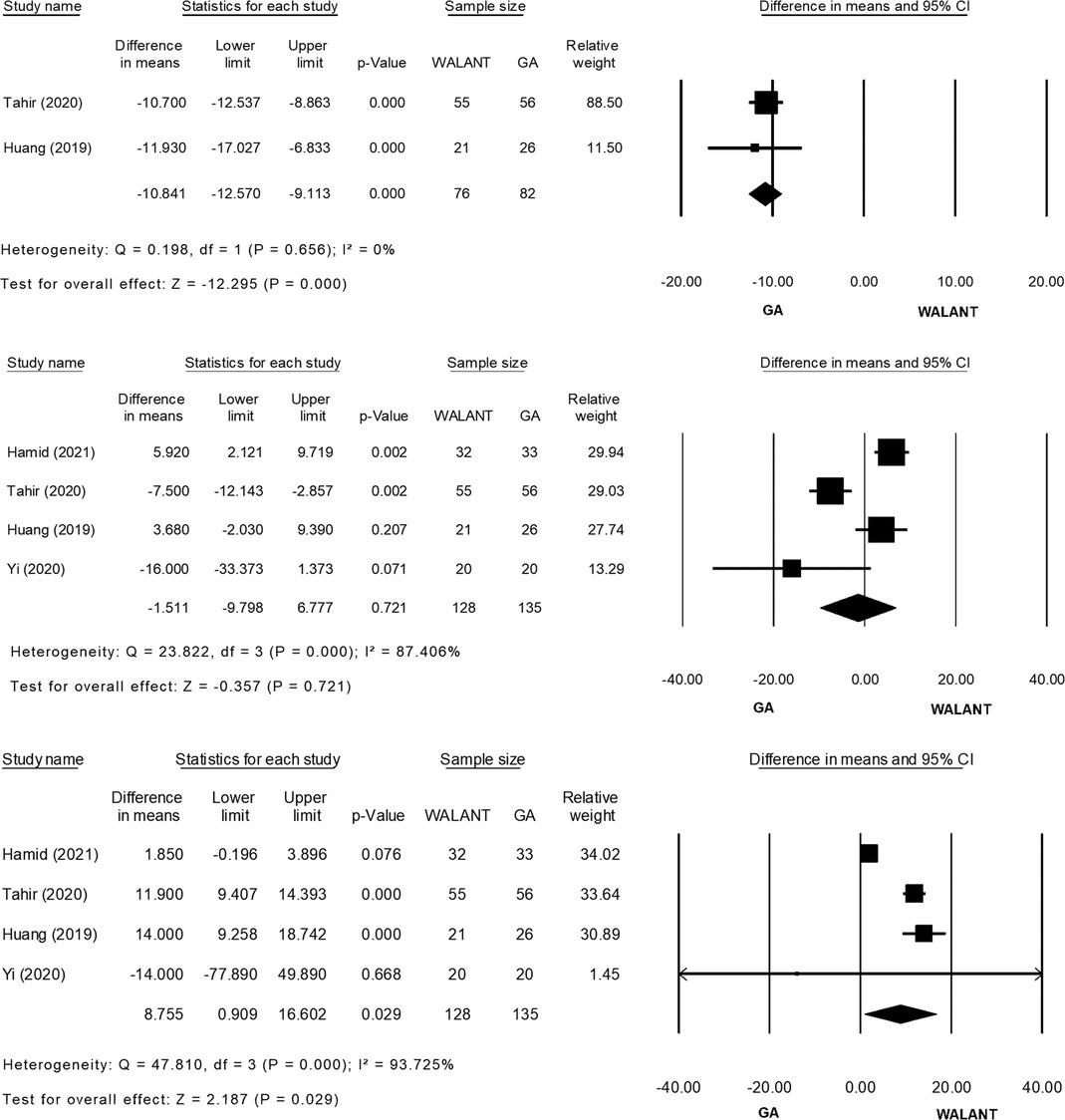
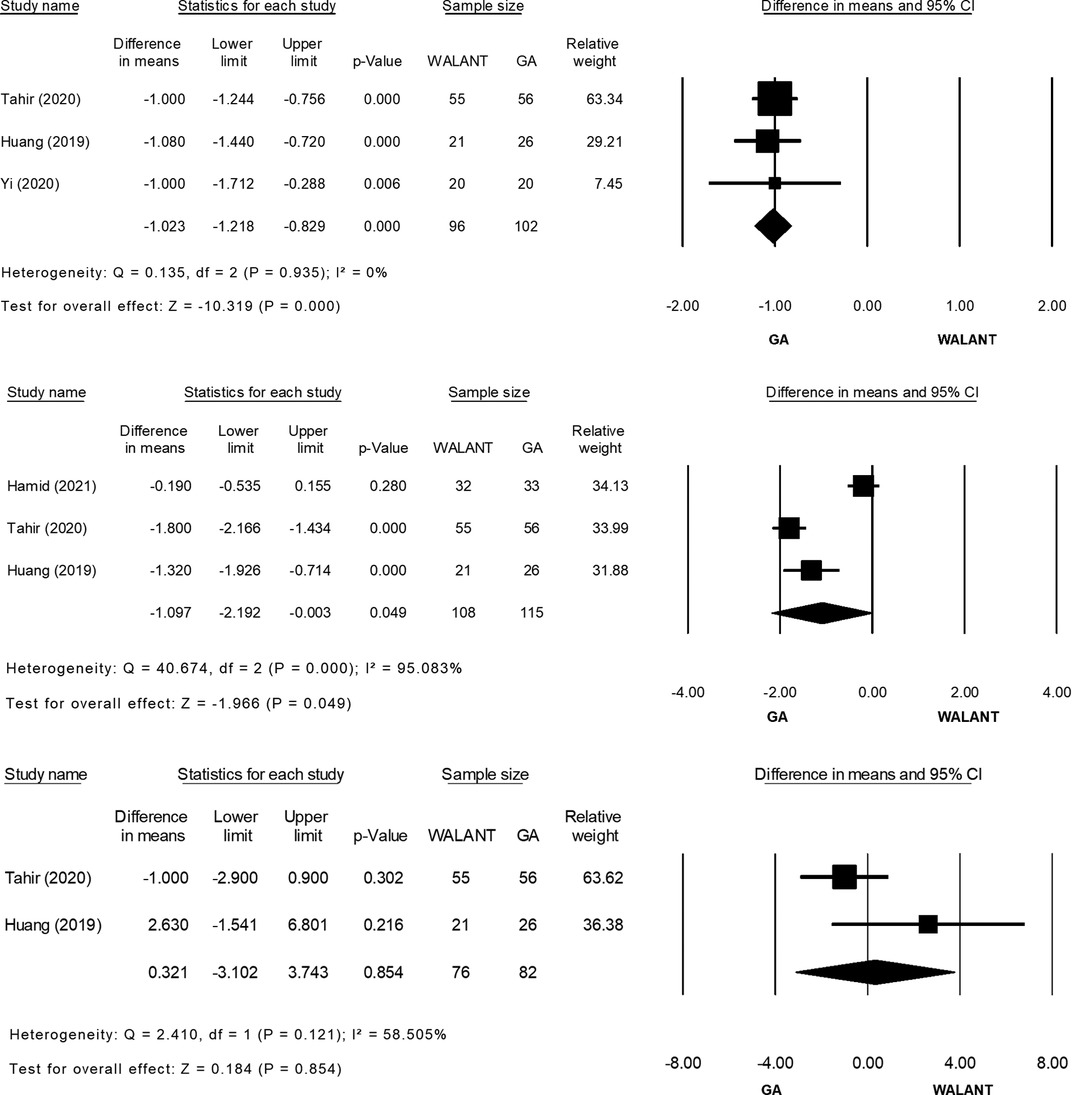
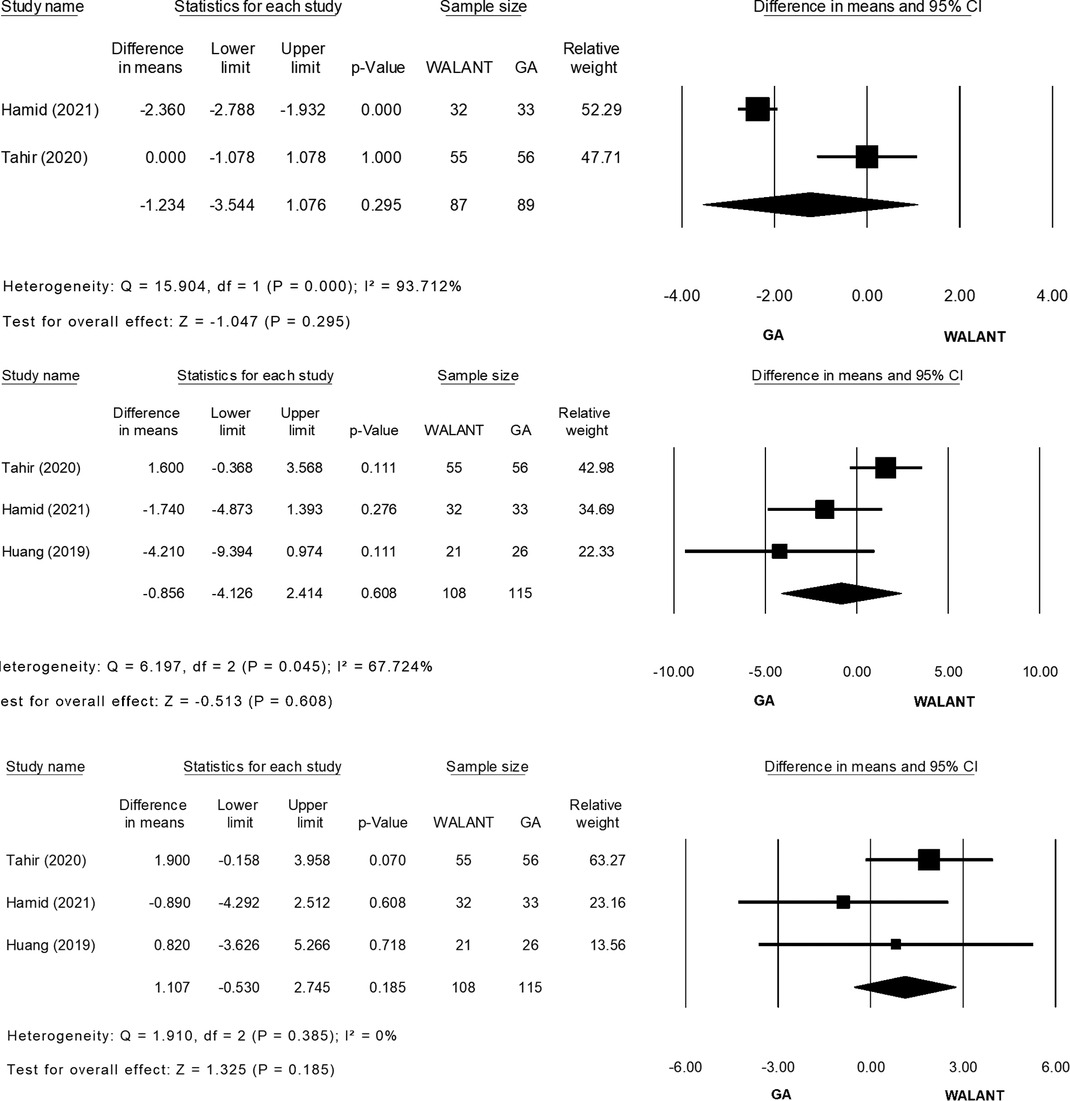
All studies were included in the meta-analysis and evaluated for differences in the outcomes of interest (Figure 2). Preparation for surgery using WALANT was significantly shorter than that for surgery using GA (MD = −10.841; 95% CI, −12.570 to −9.113; p = 0.000), with no heterogeneity observed in these two studies (2, 20) (Ι2 = 0%; χ2 = 0.198; p = 0.656; Figure 2A). Duration of surgery did not differ significantly between the two techniques (MD = −1.511; 95% CI, −9.798 to 6.777; p = 0.721), and extreme heterogeneity was found among the four studies (Ι2 = 87.40%; χ2 = 23.822; p = 0.000; Figure 2B). Blood loss was significantly greater during surgery using WALANT than during surgery using GA (MD = 8.755; 95% CI, 0.909–16.602; p = 0.029), and extreme heterogeneity was noted among the four studies (Ι2 = 93.725%; χ2 = 47.810; p = 0.000; Figure 2C). Hospitalization was significantly shorter after surgery using WALANT than after surgery using GA (MD = −1.023; 95% CI, −1.218 to −0.829; p = 0.000), and no heterogeneity was noted among three studies (2,21,22) (Ι2 = 0%; χ2 = 0.135; p = 0.935; Figure 2D). VAS scores were significantly lower the day after surgery using WALANT (MD = −1.097; 95% CI, −2.192 to −0.003; p = 0.049), and extreme heterogeneity was observed among three studies (2, 21, 22) (Ι2 = 95.083%; χ2 = 40.674; p = 0.000; Figure 2E). No significant differences between the two techniques were found for the following outcomes of interest: Mayo wrist scores (MD = 0.321; 95% CI, −3.102 to 3.743; p = 0.854), for which heterogeneity between two studies (2, 21) was high (Ι2 = 58.505%; χ2 = 2.410; p = 0.121; Figure 2F); QuickDASH scores (MD = −1.234; 95% CI, −3.544 to 1.076; p = 0.295), for which heterogeneity between two studies (2, 21) was extremely high (Ι2 = 93.71; χ2 = 15.904; p = 0.000; Figure 2G); wrist flexion (MD = −0.856; 95% CI, −4.126 to 2.414; p = 0.608), for which heterogeneity among three studies (2, 21, 22) was high (Ι2 = 67.724%; χ2 = 6.197; p = 0.045; Figure 2H); wrist extension (MD = 1.107; 95% CI, −0.530 to 2.745; p = 0.185), for which no heterogeneity was found among three studies (2, 21, 22) (Ι2 = 0%; χ2 = 1.910; p = 0.385; Figure 2I); time until bone union (MD = −0.644; 95% CI, −1.492 to 0.203; p = 0.136), for which no heterogeneity was found between two studies (2, 22) (Ι2 = 0%; χ2 = 0.814; p = 0.367; Figure 2J); and complication rates (relative risk = 0.294; 95% CI, 0.072–1.204; p = 0.089), for which no heterogeneity was found among four studies (2, 21, 22) (Ι2 = 0%; χ2 = 0.822; p = 0.844; Figure 2K).

Figure 2. (A) Forest plot of Preparation time for surgery (minute) comparing WALANT with GA. (B) Forest plot of Surgery time (minute) comparing WALANT with GA. (C) Forest plot of Blood loss (mL) comparing WALANT with GA. (D) Forest plot of Postoperative Hospital stays comparing WALANT with GA. (E) Forest plot of Post-operation day 1 visual analog scale (VAS) comparing WALANT with GA. (F) Forest plot of Mayo Wrist score comparing WALANT with GA. (G) Forest plot of Quick DASH score comparing WALANT with GA. (H) Forest plot of Wrist Flexion (degree) comparing WALANT with GA. (I) Forest plot of Wrist Extension (degree) comparing WALANT with GA. (J) Forest plot of Union time (week) comparing WALANT with GA. (K) Forest plot of Complication rate comparing WALANT with GA.
Quality Assessment
The Newcastle–Ottawa Scale was used to evaluate the quality of the studies by Huang et al. (21) and Yi et al. (22) (Table 3), and the Cochrane Collaboration’s Risk of Bias Tool was used to evaluate bias in the studies conducted by Tahir et al. (2) and Hamid et al. (20) The studies conducted by Huang et al. (21) and Yi et al. (22) were considered to have superior quality. The risk of bias in the studies conducted by Tahir et al. (2) and Hamid et al. (20) was considered high caused by performance bias (“blinding” of participants and personnel in both studies).
Discussion
For a long time, epinephrine was considered the leading cause of severe complications, such as gangrene or necrosis, following hand or wrist surgeries. However, Lalonde et al. showed that epinephrine injections produced no digital tissue loss or skin necrosis in 3,110 consecutive patients (3). Because epinephrine was proven safe, McKee et al. (23, 24) proposed waiting approximately 30 min after administering the injection to maximize hemostasis before making an incision. The widely accepted maximal dose of lidocaine that is believed to be safe for upper extremity surgery is 7 mg/kg (25). The addition of epinephrine prolongs the duration of action of lidocaine from 30–60 min to 120–360 min (26). The acidity of the solution (pH: 4.2) is likely to cause pain to the patient during injection; therefore, buffering the WALANT solution (1% lidocaine with 1:100,000 epinephrine) with 8.4% sodium bicarbonate at a ratio of 1:20 to reach the physiologic pH of 7.4 was recommended (27, 28). According to a Cochrane review (29), patients favor buffered lidocaine over unbuffered lidocaine.
WALANT appears to be a safe, cost-effective, and time-efficient technique. Compared with GA, the primary advantages of WALANT are that (1) because a tourniquet is not required, postoperative discomfort, muscle necrosis, and nerve injury can be avoided. (2) Deep sedation is not essential; thus, recovery is faster, fewer side effects such as nausea and vomiting occur, and the anesthesia risk in older patients with multiple comorbidities is lower. (3) Patients do not need to fast overnight, which minimizes the risk of glycemic change in patients with diabetes before surgery. (4) Preoperative testing—such as blood tests, chest radiographs, electrocardiography, and medical clearance—and the services of an anesthesiologist and postoperative anesthetic care are not required, which thereby saves time and decreases costs (30). However, WALANT application was restricted in case of patients with needle phobia, peripheral vascular diseases or active infection, bleeding tendency, abnormal clotting profile, and hypersensitivity to lidocaine (2).
A mean saving of USD 1320 in health care costs, including anesthesia cost, preoperative cost, and postoperative cost, was noted in an American study in which the cost of WALANT was compared with that of GA in surgery for carpal tunnel syndrome (31). Furthermore, despite the MDs in annual household incomes between the United States and Pakistan, Tahir et al. demonstrated that WALANT costs less in hospital spending (USD 202.10; p < 0.001) compared with GA in terms of repairs of distal radius fracture in both countries (2). In contrast, Caggiano et al. (32) showed that the choice of anesthesia considerably affected total nonsurgical time, room turnover time, in-room presurgical time, and in-room postsurgical time; for instance, local anesthesia reduced the total nonsurgical time by 40% in comparison with GA. In the repair of distal radius fractures, WALANT, a safe, cost-effective, and time-efficient technique, resulted in better patient satisfaction (p < 0.001) compared with GA (2).
In this quantitative, comparative meta-analysis of four studies (two retrospective cohort studies and two RCTs) with a total of 263 patients, C2 and A2 were the most common types of distal radius fractures according to the AO/OTA classification. With WALANT, preparation for surgery and postoperative hospitalization were shorter and VAS scores on postoperative day 1 were lower, but blood loss was greater in comparison with GA. For conventional GA, an anesthesiologist and nursing staff must be available, in addition to information about the patient’s medical history and vital sign monitoring equipment, before and after anesthesia induction, and the patient needs to be intubated. WALANT does not require the abovementioned staff and procedures, and surgical preparation time can thus be substantially shortened. Because a tourniquet is not used, the pain in the upper arm is reduced, and the painful swelling and ecchymosis caused by the immediate venous return after release of the tourniquet can be avoided. When pain decreases and the effects of deep sedation, including nausea, vomiting, and dizziness, do not occur, hospitalization is considerably shortened. However, no significant differences were found between the two techniques in terms of the functional outcome (ROM, QuickDASH score, and Mayo wrist score), complication rate, and time to bone union. The total complication rates were lower after surgery using WALANT (0.8%) than after surgery using GA (5.9%), and the proportions of patients requiring revision surgery using WALANT (0.8%) were lower than those using GA (1.5%).
Complications with GA occurred in three patients in the study by Yi et al. (20), who experienced nausea and vomiting for 1 day; in one patient with attrition injury and two patients with mild wound inflammation in the study by Tahir et al. (2); and in one patient with screw penetration of the wrist joint and another with distal radioulnar joint dissociation (both of whom underwent subsequent revision surgery) in the study by Hamid et al. (20). Conversely, complications with WALANT—a reduction in radial inclination and an increase in dorsal tilt, treated using revision surgery with K-wire augmentation—were noted in one patient in the study by Yi et al.. The definitive functional outcome and complication rate after surgery should depend on the severity of the fracture in terms of whether it involves the joint surface, the appropriate selection and placement of an implant, and the reduction and surgical technique. In addition to disparate surgery-related problems, different postoperative rehabilitation protocols and medications may have contributed to the discrepancies in functional outcomes among the studies. Therefore, the present study of these two different anesthesia approaches revealed only differences in immediate recovery and pain after surgery but not in different functional outcomes and complication rates.
This study had several limitations. First, the follow-up periods in most studies varied and were no more than 1 year; several outcomes and complications may have emerged during a more extended follow-up period. Second, these four studies with small sample sizes (two nonrandomized controlled studies and two randomized controlled studies with an overall high risk of bias) may have been affected by various biases and a low statistical power. Third, the high heterogeneity among studies that was observed for some outcomes may be attributable to different covariates. Incongruous distribution among different types of distal radius fractures and different WALANT solution formulas presumably resulted in heterogeneity in surgery duration and blood loss among studies. Last, despite the apparently lower complication rate using WALANT compared with GA, some of the complications that necessitated secondary revisions were associated with technical problems rather than problems associated with anesthesia. The misattribution of these complications might cause misclassification bias. There are still some distinctions in the anesthesia methods used in these included articles. Moreover, different epinephrine and xylocaine concentrations were administered. Further research is essential for further investigation and objective observations of factors such as oozing status, difficulty of reduction, patients’ pain perceptions, and variation in vital signs during surgery.
In summary, this systemic review and meta-analysis demonstrated that WALANT, in comparison with GA, shortened the time required for the preparation of surgery, shortened postoperative hospitalization, and resulted in less pain 1 day after distal radius fracture fixation; however, blood loss was greater with WALANT, which is a drawback. According to some studies (2, 21), even if blood loss is greater without the use of a tourniquet, it is still minimal and does not affect the operation. Otherwise, the final functional outcome and complication rates did differ considerably between the two different anesthetic approaches. Although this study showed that WALANT is a favorable alternative to GA in terms of reliability, cost-effectiveness, and time saved, each patient should be treated on a case-by-case basis because both treatments have benefits and drawbacks.
Data Availability Statement
The original contributions presented in the study are included in the article/Supplementary Material, further inquiries can be directed to the corresponding author/s.
Author Contributions
Study conception and design: C-YC; Acquisition of data: T-YT; Analysis and interpretation of data: T-YT, C-YH, P-CL, C-YC; Writing (original draft preparation): T-YT; Writing (review and editing): C-YH, P-CL, C-YC; Guarantor: C-YC. All authors contributed to the article and approved the submitted version.
Acknowledgments
We thank all the authors of the studies included in our meta-analysis and meta-analysis discussion group of Kaohsiung Veterans General Hospital. Special thanks to Hamid et al. and Universiti Kebangsaan Malaysia, Kuala Lumpur, MYS.
Conflict of Interest
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
Publisher's Note
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
References
1. Nellans KW, Kowalski E, Chung KC. The epidemiology of distal radius fractures. Hand Clin. (2012) 28(2):113–25. doi: 10.1016/j.hcl.2012.02.001
2. Tahir M, Chaudhry EA, Zaffar Z, Anwar K, Mamoon MAH, Ahmad M, et al. Fixation of distal radius fractures using wide-awake local anaesthesia with no tourniquet (WALANT) technique. Bone Joint Res. (2020) 9(7):429–39. doi: 10.1302/2046-3758.97.BJR-2019-0315.R1
3. Lalonde D, Bell M, Benoit P, Sparkes G, Denkler K, Chang P. A multicenter prospective study of 3,110 consecutive scases of elective epinephrine use in the fingers and hand: the dalhousie project clinical phase. J Hand Surg. (2005) 30(5):1061–7. doi: 10.1016/j.jhsa.2005.05.006
4. Pires Neto PJ, Moreira LA, Las Casas PP. Is it safe to use local anesthesia with adrenaline in hand surgery? WALANT technique. Rev Bras Ortop. (2017) 52(4):383–9. doi: 10.1016/j.rbo.2017.05.002
5. Codding JL, Bhat SB, Ilyas AM. An economic analysis of MAC versus WALANT: a trigger finger release surgery case study. Hand (New York, NY). (2017) 12(4):348–51. doi: 10.1177/1558944716669693
6. Gunasagaran J, Sean ES, Shivdas S, Amir S, Ahmad TS. Perceived comfort during minor hand surgeries with wide awake local anaesthesia no tourniquet (WALANT) versus local anaesthesia (LA)/tourniquet. J Orthop Surg (Hong Kong). (2017) 25(3):2309499017739499. doi: 10.1177/2309499017739499
7. Hagert E, Lalonde DH. Wide-awake wrist arthroscopy and open TFCC repair. J Wrist Surg. (2012) 1(1):55–60. doi: 10.1055/s-0032-1312045
8. Prasetyono TO. Tourniquet-Free hand surgery using the one-per-mil tumescent technique. Arch Plast Surg. (2013) 40(2):129–33. doi: 10.5999/aps.2013.40.2.129
9. Lalonde D, Martin A. Epinephrine in local anesthesia in finger and hand surgery: the case for wide-awake anesthesia. J Am Acad Orthop Surg. (2013) 21(8):443–7. doi: 10.5435/JAAOS-21-08-443
10. Nakanishi Y, Omokawa S, Kobata Y, Shimizu T, Kira T, Onishi T, et al. Ultrasound-guided selective sensory nerve block for wide-awake forearm tendon reconstruction. Plast Reconstr Surg Glob open. (2015) 3(5):e392. doi: 10.1097/GOX.0000000000000365
11. Xing SG, Tang JB. Surgical treatment, hardware removal, and the wide-awake approach for metacarpal fractures. Clin Plast Surg. (2014) 41(3):463–80. doi: 10.1016/j.cps.2014.03.005
12. Teo I, Lam W, Muthayya P, Steele K, Alexander S, Miller G. Patients’ perspective of wide-awake hand surgery–100 consecutive cases. J Hand Surg Eur Vol. (2013) 38(9):992–9. doi: 10.1177/1753193412475241
13. Al Youha S, Lalonde DH. Update/Review: changing of use of local anesthesia in the hand. Plast Reconstr Surg Glob open. (2014) 2(5):e150. doi: 10.1097/GOX.0000000000000095
14. Bismil M, Bismil Q, Harding D, Harris P, Lamyman E, Sansby L. Transition to total one-stop wide-awake hand surgery service-audit: a retrospective review. JRSM Short Rep. (2012) 3(4):23. doi: 10.1258/shorts.2012.012019
15. Lalonde D, Martin A. Tumescent local anesthesia for hand surgery: improved results, cost effectiveness, and wide-awake patient satisfaction. Arch Plast Surg. (2014) 41(4):312–6. doi: 10.5999/aps.2014.41.4.312
16. Higgins JPT, Altman DG, Gøtzsche PC, Jüni P, Moher D, Oxman AD, et al. The Cochrane Collaboration’s tool for assessing risk of bias in randomised trials. BMJ. (2011) 343:d5928. doi: 10.1136/bmj.d5928
17. Hardy RJ, Thompson SG. Detecting and describing heterogeneity in meta-analysis. Stat Med. (1998) 17(8):841–56. doi: 10.1002/(SICI)1097-0258(19980430)17:8<841::AID-SIM781>3.0.CO;2-D
18. Takkouche B, Cadarso-Suárez C, Spiegelman D. Evaluation of old and new tests of heterogeneity in epidemiologic meta-analysis. Am J Epidemiol. (1999) 150(2):206–15. doi: 10.1093/oxfordjournals.aje.a009981
19. Combining Information. Statistical issues and opportunities for research. Washington, DC: The National Academies Press (1992).
20. Abd Hamid MH, Abdullah S, Ahmad AA, Narin Singh PSG, Soh EZF, Liu CY, et al. A randomized controlled trial comparing wide-awake local anesthesia with no tourniquet (WALANT) to general anesthesia in plating of distal radius fractures with pain and anxiety level perception. Cureus. (2021) 13(1):e12876. doi: 10.7759/cureus.12876
21. Huang YC, Chen CY, Lin KC, Yang SW, Tarng YW, Chang WN. Comparison of wide-awake local anesthesia no tourniquet with general anesthesia with tourniquet for volar plating of distal radius fracture. Orthopedics. (2019) 42(1):e93–8. doi: 10.3928/01477447-20181206-01
22. Yi LM, Ahmad AA, Ruslan SR, Abdullah S, Ahmad AR. Plating distal radius fractures using wide-awake local anesthesia no tourniquet (WALANT) versus general anesthesia: a cohort study. J Hand Surg Glob Online. (2020) 2(6):331–8. doi: 10.1016/j.jhsg.2020.09.003
23. McKee DE, Lalonde DH, Thoma A, Glennie DL, Hayward JE. Optimal time delay between epinephrine injection and incision to minimize bleeding. Plast Reconstr Surg. (2013) 131(4):811–4. doi: 10.1097/PRS.0b013e3182818ced
24. McKee DE, Lalonde DH, Thoma A, Dickson L. Achieving the optimal epinephrine effect in wide awake hand surgery using local anesthesia without a tourniquet. Hand (New York, NY). (2015) 10(4):613–5. doi: 10.1007/s11552-015-9759-6
25. Lalonde DH, Wong A. Dosage of local anesthesia in wide awake hand surgery. J Hand Surg. (2013) 38(10):2025–8. doi: 10.1016/j.jhsa.2013.07.017
26. Higgins A, Lalonde DH, Bell M, McKee D, Lalonde JF. Avoiding flexor tendon repair rupture with intraoperative total active movement examination. Plast Reconstr Surg. (2010) 126(3):941–5. doi: 10.1097/PRS.0b013e3181e60489
27. Lee HJ, Cho YJ, Gong HS, Rhee SH, Park HS, Baek GH. The effect of buffered lidocaine in local anesthesia: a prospective, randomized, double-blind study. J Hand Surg. (2013) 38(5):971–5. doi: 10.1016/j.jhsa.2013.02.016
28. Strazar AR, Leynes PG, Lalonde DH. Minimizing the pain of local anesthesia injection. Plast Reconstr Surg. (2013) 132(3):675–84. doi: 10.1097/PRS.0b013e31829ad1e2
29. Cepeda MS, Tzortzopoulou A, Thackrey M, Hudcova J, Arora Gandhi P, Schumann R. Adjusting the pH of lidocaine for reducing pain on injection. Cochrane Database Syst Rev. (2010) (12):Cd006581. doi: 10.1002/14651858.CD006581.pub2
30. Steiner MM, Calandruccio JH. Use of wide-awake local anesthesia no tourniquet in hand and wrist surgery. Orthop Clin North Am. (2018) 49(1):63–8. doi: 10.1016/j.ocl.2017.08.008
31. Alter TH, Warrender WJ, Liss FE, Ilyas AM. A cost analysis of carpal tunnel release surgery performed wide awake versus under sedation. Plast Reconstr Surg. (2018) 142(6):1532–8. doi: 10.1097/PRS.0000000000004983
Keywords: wide-awake local anesthesia no tourniquet, WALANT, general anesthesia, GA, distal radius, fracture, fixation
Citation: Tu T, Hsu C, Lin P and Chen C (2022) Wide-Awake Local Anesthesia With no Tourniquet Versus General Anesthesia for the Plating of Distal Radius Fracture: A Systematic Review and Meta-Analysis. Front. Surg. 9:922135. doi: 10.3389/fsurg.2022.922135
Received: 17 April 2022; Accepted: 6 June 2022;
Published: 27 June 2022.
Edited by:
Paphon Sa-ngasoongsong, Mahidol University, ThailandReviewed by:
David Joshua Mayich, Vitalité Health Network, CanadaTulyapruek Tawonsawatruk, Mahidol University, Thailand
Copyright © 2022 Tu, Hsu, Lin and Chen. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Chun-Yu Chen aWVyZ3kyMDAwQGdtYWlsLmNvbQ==
Specialty section: This article was submitted to Orthopedic Surgery, a section of the journal Frontiers in Surgery
 Ting-Yu Tu
Ting-Yu Tu Chih-Yang Hsu2
Chih-Yang Hsu2 Chun-Yu Chen
Chun-Yu Chen