- 1Orthopaedic Medical Center, Second Hospital of Jilin University, Changchun, China
- 2Operating Room, Second Hospital of Jilin University, Changchun, China
Background: Calcific tendonitis rarely occurs in the fingers, and it is easily misdiagnosed. Herein we describe the case of a patient with multiple calcific lesions within the flexor digitorum superficialis and the extensor digitorum tendons of the distal interphalangeal joints of the right index finger, and the surgical treatment of those lesions.
Case presentation: The patient was a 66-year-old man who reported pain and swelling in his right index finger for one year. He was diagnosed with chronic calcific tendonitis based on his symptoms and radiology images. He was successfully treated surgically, and histopathological examination confirmed the diagnosis. After one month, the patient had healed well, and there was no recurrence.
Conclusions: This is the first report of a patient suffering from chronic calcific tendonitis in a finger who failed conservative treatment and was successfully treated with surgery. The outcome demonstrates that surgical debridement can yield a good outcome in patients with chronic calcific tendonitis.
Introduction
Calcific tendinitis is an acute idiopathic inflammatory disease that involves pain, tenderness, and edema (1). It mainly occurs in joints or tendons, and most commonly occurs in shoulder joints. It only occurs in the hands in approximately 2.4% of cases (2). Calcific tendinitis in the fingers has rarely been reported. Due to its low incidence and atypical clinical manifestations, calcific tendonitis in the fingers is usually misdiagnosed as flexor sheath infection, tenosynovitis, septic arthritis, fracture, cellulitis, or gout (3–5). Such misdiagnoses have resulted in unnecessary antibiotic treatment and surgery. Conservative treatment is usually administered for calcified tendinitis, including splinting and non-steroidal anti-inflammatory medications (6). The effects of conservative treatment can be insufficient however, and the condition is prone to relapse. When conservative treatment is ineffective, or the symptoms persist, surgery can be considered (5, 6).
Herein we describe a case of chronic calcified tendinitis in the distal interphalangeal (DIP) joint of the right index finger. The calcifications were located in both the flexor digitorum superficialis (FDS) and the extensor digitorum tendons of the right index DIP joint. Surgery was performed, and complete finger photography, x-rays, and histopathological examinations were conducted before and after surgery.
This report is intended to provide orthopedic surgeons with a better understanding of calcific tendinitis, particularly with respect to surgical outcomes and specific treatment concerns. The patient provided informed written consent for the publication of the report, including all images, and the Jilin University Second Hospital Institutional Review Board approved the publication of the report.
Case presentation
A 66-year-old man presented with pain and swelling of the right index finger. He reported that he had had it for one year, which had progressively worsened during the previous week. There was no history of trauma, fever, injury, or similar episodes of pain. The results of serological examinations were normal. Physical examination revealed slight swelling, redness, and tenderness on the back of the right index DIP joint, and noticeable swelling, paleness, and tenderness on the palm side (Figure 1). The patient was initially diagnosed with chronic tendon sheath infection, but there were no typical Kanavel symptoms, such as tenderness along the flexor sheath, fusiform swelling, or pain on passive extension or with the finger held in partial flexion (7). x-rays of the right index finger depicted soft tissue swelling at the DIP joint (Figure 2). Collectively these results suggested calcific tendonitis in the FDS and extensor digitorum tendons of the DIP joint.
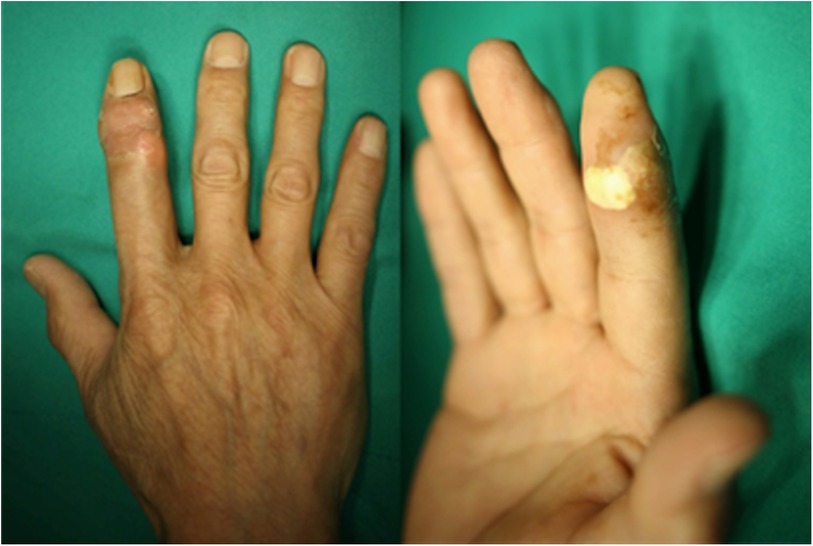
Figure 1. The right index finger with slight swelling and redness on the back of the right index distal interphalangeal joint, and obvious swelling and paleness on the palm side in the distal interphalangeal joint.

Figure 2. Preoperative x-ray of the right index finger depicting soft tissue swelling at the distal interphalangeal joint.
Due to the long period of disease and severe clinical manifestations, surgical treatment was recommended to the patient. He opted to take the surgery, and the operation was performed under local anesthesia. The patient was placed in a supine position with his right hand on the operating table. After a temporary rubber ring tourniquet was placed behind the metacarpophalangeal (MCP) joint, a zigzag incision was made on the back of the DIP joint. The ulnar side was then incised to the level of the FDS tendon of the index finger, and small calcifications were detected (Figure 3). A 1 cm × 1 cm calcification was detected via radial exploration of the extensor digitorum tendon on the palm of the finger. All of the calcifications were removed without tendon damage. The resected tissue was sent for histological examination.
Hematoxylin-eosin staining of histological sections of the resected tissue revealed calcium hydroxyapatite deposition with necrosis of surrounding tissue (Figure 4), confirming the diagnosis of calcific tendinitis. Postoperative x-rays did not depict any residual calcification. One month after surgery, the pain and swelling had completely disappeared (Figures 5, 6).
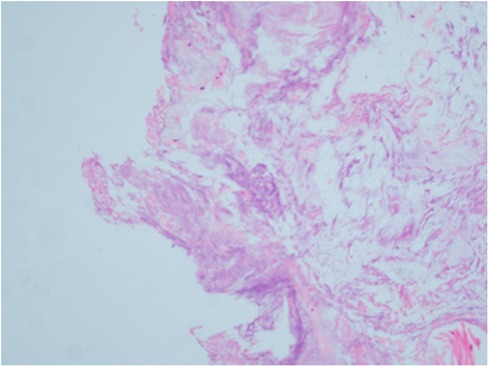
Figure 4. Postoperative histopathological examination revealed calcium hydroxyapatite deposition with necrosis of surrounding tissue.
Discussion and conclusions
Calcific tendinitis is caused by hydroxyapatite crystals or carbonate apatite, but its precise etiology is unknown (1). Some scholars believe that it is caused by localized tissue hypoxia or trauma (8, 9), and that hypoxia of the tendon is an inductive event. Poor blood perfusion caused by mechanical or metabolic problems causes the tendon to be converted into fibrocartilage, and chondrocytes mediate calcium salt deposition. The main factors influencing calcific tendinitis are female sex, trauma to the tendon causing local hypoxia (including repetitive trauma), autoimmune diseases such as rheumatoid arthritis, and metabolic conditions including diabetes (5, 10).
The main clinical manifestations of calcific tendinitis include acute erythema, swelling of the lesion, and limited activity (1). Rather than the calcification itself, most symptoms of calcific tendinitis result from the destruction of surrounding soft tissues caused by the calcified foci, which leads to non-specific inflammatory reactions (10). Therefore, the clinical symptoms of calcific tendinitis are not typical. Results of serological examinations are usually normal, including serum calcium, phosphorous, alkaline phosphate, and uric acid levels (11, 12). Occasionally the white blood cell count and the erythrocyte sedimentation rate are elevated. Accordingly, a serological examination can be useful for distinguishing calcific tendinitis from tendon sheath infection and gout, but not from a fracture (6). As in the present case, radiology imaging depictions of calcific tendinitis can be relatively mild, and this can be used to distinguish calcific tendinitis from a fracture (13–15). It is these inconspicuous clinical examination features that can render the diagnosis of calcific tendinitis difficult.
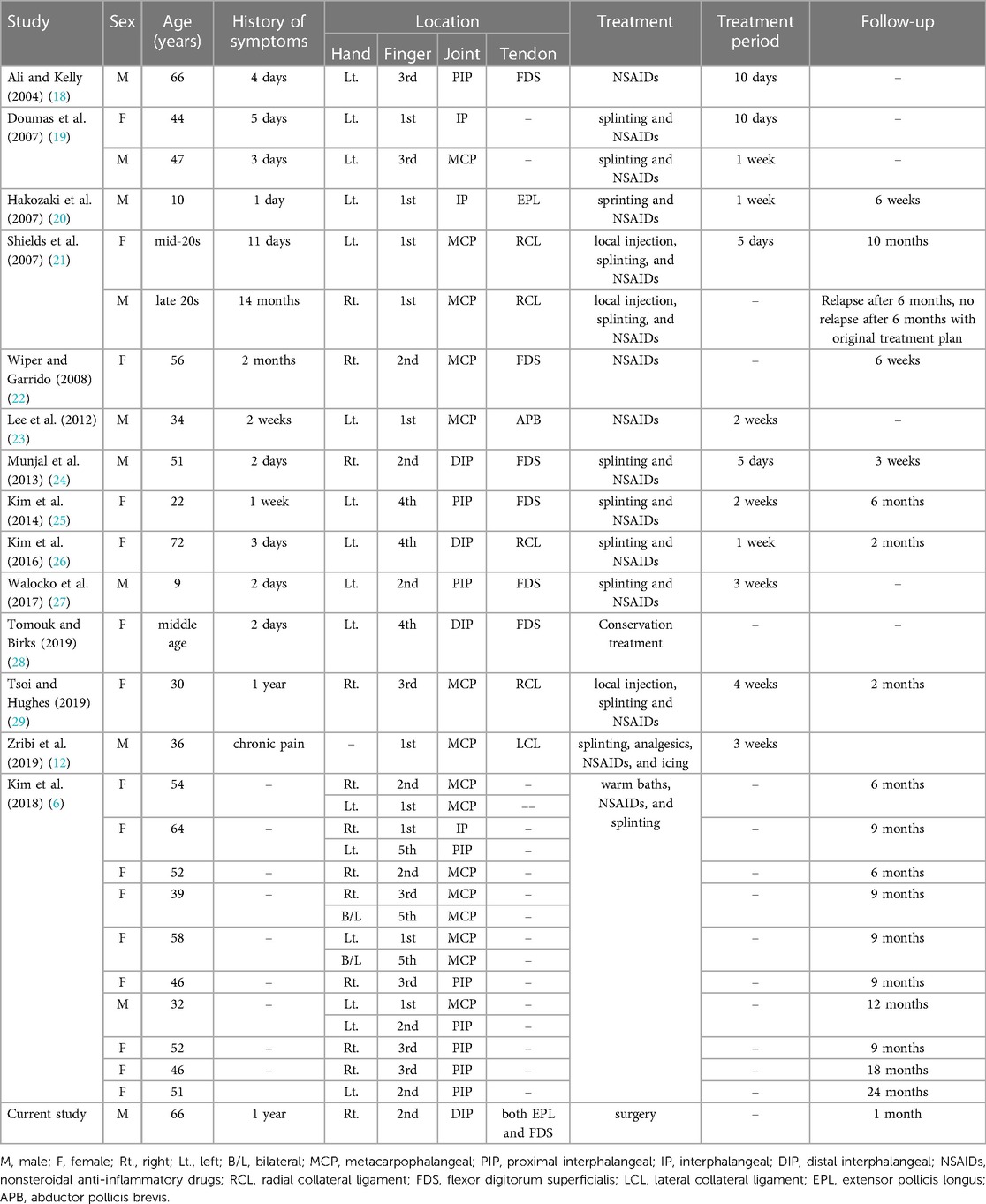
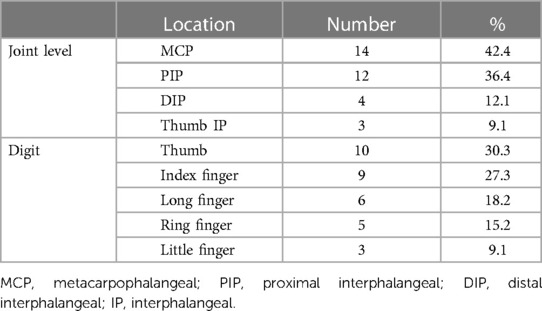
Calcific tendinitis most commonly occurs in the shoulder joint, followed by the knees and hips, and it rarely occurs in the hands or wrists. In the hands, the most common location is the carpal tunnel (16). The most common location of calcific tendinitis occurring in the finger is the MCP joint, followed by the proximal interphalangeal joint, and the least common is the DIP joint (17). To our knowledge, a total of 26 cases of calcific tendinitis in the fingers have previously been reported (Table 1). The most common joint involved has been the MCP, and the most common digit involved has been the thumb (Table 2).
Calcific tendinitis is a self-limiting disease, but both conservative treatment and surgical treatment have been successfully utilized (5, 30). Conventional treatment methods involve immobilization in conjunction with aspirin or non-steroidal anti-inflammatory medications, with the aim of reducing pain and relieving symptoms. These measures can be tried for at least six months before considering surgical treatment, particularly in cases involving a finger (6). Surgical intervention is more suitable in patients with severe symptoms and, or a long period of disease, or after the failure of conservative treatment (31).
All the patients in the recently reported cases have opted for conservative treatment (6, 13, 18–20, 22–29). The characteristics of these patients included common clinical symptoms and mild medical histories. During the treatment follow-up periods, only one patient exhibited a recurrence of calcified deposits within 18 months (21). Calcium deposits on the hands are highly misdiagnosed not only because of their similar symptomology to more common conditions, but also because clinicians are unfamiliar with the disease process. The differential diagnosis is broad and includes infections, fractures, metabolic disorders, degenerative and autoimmune diseases (17, 27). Due to the severe symptoms in the present case, however, as well as the long disease course and the associated substantial effects on quality of life, the adequacy of conservative treatment could not be predicted. It is also notable that the operation is simple and easy, they can yield curative effects rapidly. Therefore, surgery was recommended to the patient in the current case.
In conclusion, this is the first case report of a patient suffering from multiple chronic calcific tendonitis lesions in the finger who failed conservative treatment and was successfully treated with surgery. The present case demonstrates that surgical repair can yield a good outcome in patients with chronic calcific tendonitis. Orthopedic surgeons should consider the possibility of calcified tendinitis when they encounter patients with hand swelling and pain. Although some calcific tendinitis patients can be cured via conservative treatment, we recommend surgical intervention in patients with severe symptoms. It is critical for surgeons to evaluate the disease status of patients with calcific tendinitis in a finger comprehensively and develop the most suitable treatment plan.
Data availability statement
The raw data supporting the conclusions of this article will be made available by the authors, without undue reservation.
Ethics statement
The studies involving human participants were reviewed and approved by Ethics Committee of the Second Hospital of Jilin University. The patients/participants provided their written informed consent to participate in this study.
Author contributions
DG, JY, XL contributed to the design and implementation of the research, to the analysis of the results and to the writing of the manuscript. All authors contributed to the article and approved the submitted version.
Funding
This work was funded by the Special Foundation for Science and Technology Innovation of Jilin Province (No. 20200201566JC). The funders had no role in the decision to publish the report, or the preparation of the manuscript.
Conflict of interest
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
Publisher's note
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
Abbreviations
DIP, distal interphalangeal; FDS, flexor digitorum superficialis; MCP, metacarpophalangeal.
References
1. Uhthoff HK, Sarkar K, Maynard JA. Calcifying tendinitis: a new concept of its pathogenesis. Clin Orthop Relat Res. (1976) 118:164.
2. Sandstrom C. Peritendintis calcarea. A common disease of middle life: its diagnosis, pathology and treatment. AJR. (1938) 40:1.
3. Thompson GR, Ting YM, Riggs GA, Fenn ME, Denning RM. Calcific tendinitis and soft-tissue calcification resembling gout. JAMA. (1968) 203:464. doi: 10.1001/jama.1968.03140070020005
4. Selby CL. Acute calcific tendinitis of the hand: an infrequently recognized and frequently misdiagnosed form of periarthritis. Arthritis Rheum. (1984) 27:337. doi: 10.1002/art.1780270314
5. Beckmann NM. Calcium apatite deposition disease: diagnosis and treatment. Radiol Res Pract. (2016) 2016:4801474. doi: 10.1155/2016/4801474
6. Kim J, Bae KJ, Lee DW, Lee YH, Gong HS, Baek GH. Effective period of conservative treatment in patients with acute calcific periarthritis of the hand. J Orthop Surg Res. (2018) 13:287. doi: 10.1186/s13018-018-0997-5
7. Kennedy CD, Huang JI, Hanel DP. In brief: Kanavel’s signs and pyogenic flexor tenosynovitis. Clin Orthop Relat Res. (2016) 474:280. doi: 10.1007/s11999-015-4367-x
8. Moyer R, Bush D, Harrington T. Acute calcific tendinitis of the hand and wrist: a report of 12 cases and a review of the literature. J Rheumatol. (1989) 16:198.2664164
9. Dilley D, Tonkin M. Acute calcific tendinitis in the hand and wrist. J Hand Surg Br. (1991) 16:215. doi: 10.1016/0266-7681(91)90181-M
10. Oliva F, Via AG, Maffulli N. Physiopathology of intratendinous calcific deposition. BMC Med. (2012) 10:95. doi: 10.1186/1741-7015-10-95
11. Flemming DJ, Murphey MD, Shekitka KM, Temple HT, Jelinek JJ, Kransdorf MJ. Osseous involvement in calcific tendinitis: a retrospective review of 50 cases. AJR Am J Roentgenol. (2003) 181:965. doi: 10.2214/ajr.181.4.1810965
12. Zribi W, Jmal MM, Abid A, Jemaa BM, Krid N, Zribi M, et al. Apatite calcific periarthritis of the radial collateral ligament of the thumb: a case report and review of the literature. Case Reports Plast Surg Hand Surg. (2019) 6:92. doi: 10.1080/23320885.2019.1654871
13. Siegal DS, Wu JS, Newman JS, del Cura JL, Hochman MG. Calcific tendinitis: a pictorial review. Can Assoc Radiol J. (2009) 60:263. doi: 10.1016/j.carj.2009.06.008
14. Izadpanah K, Jaeger M, Maier D, Sudkamp NP, Ogon P. Preoperative planning of calcium deposit removal in calcifying tendinitis of the rotator cuff—possible contribution of computed tomography, ultrasound and conventional x-ray. BMC Musculoskelet Disord. (2014) 15:385. doi: 10.1186/1471-2474-15-385
15. McAuliffe JA. Tendon disorders of the hand and wrist. J Hand Surg Am. (2010) 35:846. doi: 10.1016/j.jhsa.2010.03.001
16. McRae B, Nusem L. A rare case of acute carpal tunnel syndrome secondary to calcific tendinitis: a case report. Open Orthop J. (2019) 13:198. doi: 10.2174/1874325001913010198
17. Kim JK, Park ES. Acute calcium deposits in the hand and wrist; comparison of acute calcium peritendinitis and acute calcium periarthritis. J Hand Surg Eur. (2014) 39:436. doi: 10.1177/1753193413478393
18. Ali SN, Kelly JL. Acute calcific tendinitis of the finger—a case report. Hand Surg. (2004) 9:105. doi: 10.1142/S0218810404001954
19. Doumas C, Vazirani RM, Clifford PD, Owens P. Acute calcific periarthritis of the hand and wrist: a series and review of the literature. Emerg Radiol. (2007) 14:199. doi: 10.1007/s10140-007-0626-9
20. Hakozaki M, Iwabuchi M, Konno S, Kikuchi S. Acute calcific tendinitis of the thumb in a child: a case report. Clin Rheumatol. (2007) 26:841. doi: 10.1007/s10067-006-0384-1
21. Shields JS, Chhabra AB, Pannunzio ME. Acute calcific tendinitis of the hand: 2 case reports involving the abductor pollicis brevis. Am J Orthop. (2007) 36:605.18075609
22. Wiper JD, Garrido A. Acute calcific tendinitis. N Engl J Med. (2008) 359:2477. doi: 10.1056/NEJMicm063524
23. Lee HO, Lee YH, Mun SH, Kang UR, Lee CK, Suh KJ. Calcific tendinitis of the hand and foot: a report of four cases. J Korean Soc Magn Reson Med. (2012) 16:177. doi: 10.13104/jksmrm.2012.16.2.177
24. Munjal A, Munjal P, Mahajan A. Diagnostic dilemma: acute calcific tendinitis of flexor digitorum profundus. Hand. (2013) 8:352. doi: 10.1007/s11552-013-9514-9
25. Kim YS, Lee HM, Kim JP. Acute calcific tendinitis of the flexor digitorum superficialis of the finger: a case report. Open J Orthop. (2014) 04:45. doi: 10.4236/ojo.2014.43008
26. Kim JH, Lee JH, Park JU, Kwon ST. Acute calcific tendinitis in the distal interphalangeal joint. Arch Plast Surg. (2016) 43:301. doi: 10.5999/aps.2016.43.3.301
27. Walocko FM, Sando IC, Haase SC, Kozlow JH. Acute calcific tendinitis of the index finger in a child. Hand. (2017) 12:NP84. doi: 10.1177/1558944716675146
28. Tomouk T, Birks M. An endoscopist with a painful finger. Br Med J. (2019) 365:l1485. doi: 10.1136/bmj.l1485
29. Tsoi K, Hughes R. An unusual case of steroid responsive idiopathic ectopic calcification. Oxf Med Case Rep. (2019) 2019:466–8. doi: 10.1093/omcr/omz108
30. ElShewy MT. Calcific tendinitis of the rotator cuff. World J Orthop. (2016) 7:55. doi: 10.5312/wjo.v7.i1.55
Keywords: calcific tendonitis, distal interphalangeal joint, finger, surgical treatment, case report
Citation: Guo D, Yang J and Liu X (2023) Surgical management of chronic calcific deposit resembling tendon sheath infection in the index finger: A rare case report and literature review. Front. Surg. 10:1119612. doi: 10.3389/fsurg.2023.1119612
Received: 9 December 2022; Accepted: 24 March 2023;
Published: 19 April 2023.
Edited by:
Jaimo Ahn, University of Michigan, United StatesReviewed by:
Lei Zhang, Southwest Medical University, ChinaJason Wink, University of Pennsylvania, United States
Guangming Han, Southern Medical University, China
© 2023 Guo, Yang and Liu. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Xiaoning Liu bGl1eHk5OUBqbHUuIGVkdS5jbg==
†These authors have contributed equally to this work
Specialty Section: This article was submitted to Orthopedic Surgery, a section of the journal Frontiers in Surgery
 Deming Guo
Deming Guo Jingjing Yang2,†
Jingjing Yang2,† Xiaoning Liu
Xiaoning Liu