- 1Department of Neurosurgery, University of Tuebingen, Tuebingen, Germany
- 2Department of Anesthesiology and Intensive Care Medicine, University of Tuebingen, Tuebingen, Germany
- 3Department of Diagnostic and Interventional Neuroradiology, University of Tuebingen, Tuebingen, Germany
- 4Department of Thoracic and Cardiovascular Surgery, University of Tuebingen, Tuebingen, Germany
Background: Acute myocardial infarction (MI) frequently leads to consciousness disturbance following hemodynamic collapse. Therefore, MI can occur together with upper cervical spine trauma. Herein, we report the successful treatment of complex C1/C2 fractures in a patient with concomitant three-vessel coronary artery disease (CAD).
Case presentation: A 70-year-old patient presented in our emergency outpatient clinic after a hemodynamic collapse without neurological deficits or heart-related complaints. Computed tomography (CT) scan of the cervical spine revealed a dislocated odontoid fracture Anderson and D'Alonzo type II and an unstable Gehweiler type III injury (Jefferson's fracture). An intradiploic arachnoid cyst in the posterior wall of the posterior fossa was a coincident radiological finding. Furthermore, coronary angiography confirmed three-vessel CAD with high-grade coronary artery stenosis. Indication for upper cervical spine surgery and bypass surgery was given. An interdisciplinary team of neurosurgeons, cardiothoracic surgeons and anesthesiologists evaluated the patient's case to develop the most suitable therapy concept and alternative strategies. Finally, in first step, C1-C2 fusion was performed by Harms technique under general anesthesia with x-ray guidance, spinal neuronavigation, Doppler ultrasound and cardiopulmonary monitoring. Cardiothoracic surgeons were on standby. One month later bypass surgery was performed uneventfully. Follow-up CT scan of cervical spine revealed intraosseous screw positioning and beginning fusion of the fractures. The patient did not develop neurological deficits and recovered completely from both surgeries.
Conclusions: Treating complex C1/C2 fractures with concomitant severe CAD requiring treatment is challenging and carries a high risk of complications. To our knowledge, the literature does not provide any guidelines regarding therapy of this constellation. To receive upper cervical spine stability and to prevent both, spinal cord injury and cardiovascular complications, an individual approach is required. Interdisciplinary cooperation to determine optimal therapeutic algorithms is needed.
Introduction
Injuries to the cervical spine occur in 2%–4% of all patients on admission to the emergency room, but may be life-threatening if associated with spinal cord injury (SCI) (1). Between 19%–51% of spinal trauma cases involve injuries to the cervical spine (2), and approximately 30% affecting the atlantoaxial region, with the odontoid being the most common site of injury to the C2 vertebra (3–6). Typical causes of accidents are high-velocity impact in polytraumatized patients and increasingly low-energy trauma e.g., domestic collapses in the elderly due to hyperextension on head impact (7, 8). Identification of craniovertebral junction (CVJ) injury is difficult as patients often present with reduced level of consciousness. Related lesions are traumatic brain injury, additional fractures of the spine, the midface, the extremities (2, 9) and vertebral artery injury (10–12). Hence, immediate neuroradiological diagnostic is crucial, dictating patient management.
One of the most common reasons for emergency department admission remains chest pain caused by acute coronary syndrome. Myocardial infarction (MI) often manifests itself atypically e.g., dyspnea, cardiac arrhythmias, abdominal pain and autonomic dysregulation. The last is observed especially in women, the elderly and patients with diabetes mellitus or chronic renal insufficiency (13, 14). In addition, acute MI can lead to syncope, consciousness disturbance and cerebral dysfunction following hemodynamic collapse (15). Therefore, upper cervical spine trauma can occur together with MI (16). Treating complex CVJ-fractures with coronary artery disease (CAD) requiring treatment is challenging and carries a high risk of complications. To our knowledge, the literature does not provide any guidelines regarding the therapy of this constellation. Herein, we report the successful management of complex C1/C2 fractures in a patient with concomitant three-vessel CAD.
Case presentation
A 70-year-old male patient presented in our emergency outpatient clinic after a syncope, causing a bicycle accident. On admission, the patient had no neurological deficits or heart-related complaints. Identified cardiovascular risk factors were hypertension, obesity, smoking and diabetes mellitus. A computed tomography (CT) scan of the cervical spine revealed a displaced odontoid type II-C fracture (17, 18) and an unstable Gehweiler (19) type III injury (Jefferson's fracture) with a fracture of the anterior arch on the right, dual fractures of the posterior arch, and a fracture of the left lateral mass of C1 (Figure 1). A coincident finding was an intradiploic arachnoid cyst in the posterior wall of the posterior fossa (Figure 1). Other lesions included minor head trauma, a fracture of the T2 vertebral body, and rib fractures. CT angiography of cervical spine revealed no vascular injury and regular V3 segment of vertebral arteries (Figure 2). Furthermore, cardiac diagnostics revealed atrial fibrillation and non-ST-segment elevation MI. Coronary angiography confirmed a three-vessel CAD with high-grade stenosis not suitable for coronary stent insertion of left anterior descending artery, ramus circumflex, ramus diagonalis proximalis (RD1) and right coronary artery. Indication for upper cervical spine surgery and bypass surgery was given. The patient's case was evaluated by an interdisciplinary team of neurosurgeons, cardiothoracic surgeons and anesthesiologists to develop the most suitable therapeutic concept.
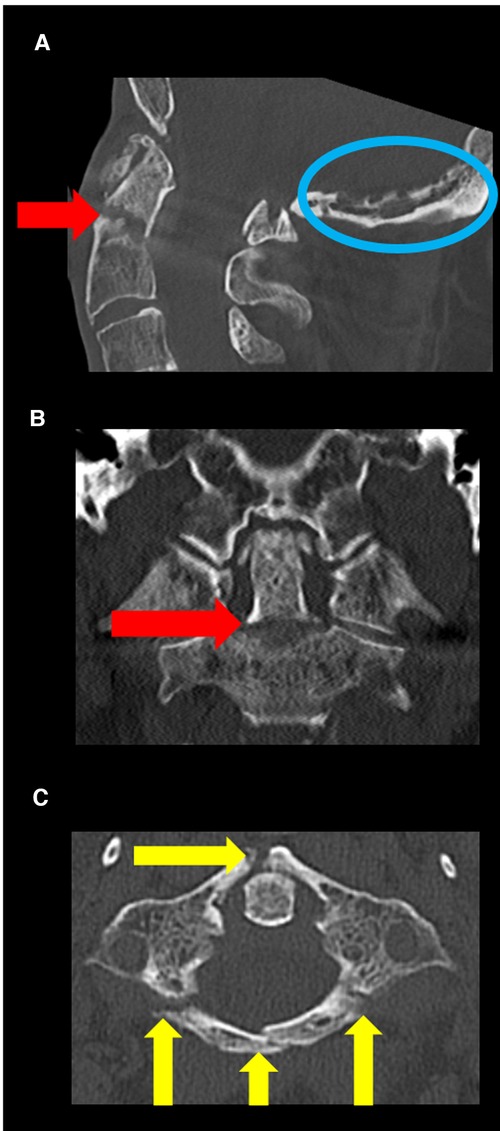
Figure 1. Preoperative CT scan (bone window) of craniocervical junction. (A) Sagittal CT revealed a dislocated odontoid type II-C fracture (red arrow) and an intradiploic arachnoid cyst in posterior wall of the posterior fossa (blue circle). (B) Coronal CT revealed no lateral dislocation of the fracture of the odontoid process (red arrow). (C) Axial CT scan revealed an unstable Jefferson's fracture (with fracture of the anterior arch on the right, dual fractures of the posterior arch and fracture of the left lateral mass of C1) (yellow arrows).

Figure 2. CT angiography of the brain-supplying vessels showing no vascular injury. (A) Axial CT scan revealed regular enhancement of internal carotid arteries and V3 segment of vertebral arteries. (B) Coronal CT scan revealed hypoplastic intradural segment of right vertebral artery.
The following three different strategies were discussed:
1. Conservative therapy of the upper cervical spine fractures and secondary bypass surgery after bone fusion.
2. Conservative therapy of the upper cervical spine fractures and simultaneous bypass surgery.
3. Fusion surgery of the upper cervical spine followed by bypass surgery.
The first concept has the advantage that no fusion surgery of the upper cervical spine needs to be performed if conservative treatment is successful. The disadvantage is that bone fusion might not occur, delaying bypass surgery.
The second option also has the advantage that no fusion surgery is required. During the intervention, bypass surgery could be performed using a Mayfield Headrest System to prevent SCI. Immobilization of the upper cervical spine in a neck brace or halo-fixation would not have been possible during surgery because of the necessary sternotomy. A neck brace or halo-fixation must be worn immediately after surgery. These orthoses might exert pressure on the sternotomy wound leading to delayed wound healing. The physical rehabilitation after coronary artery bypass surgery is also limited while wearing an orthosis. Furthermore, there is a residual risk of neurological impairment during surgery requiring intraoperative neuromonitoring (IOM).
The third option has the advantage that bypass surgery can be performed without any risk of SCI because of the dislocation of the fractures. However, there is a higher intraoperative risk of cardiac events during fusion surgery of the upper cervical spine and a myocardial infarction risk in the time between surgeries. Decision making depends mostly on the severity of MI and how near-term bypass surgery must be performed. Advanced anaesthesiological management is also required. In the present case, considering the patient's age and comorbidities, and due to the fact, that bypass surgery was not emergently indicated, a conservative therapy based on immobilization of the cervical spine in a neck brace was tried. In absence of fracture healing after 4 weeks, surgical approaches were again discussed. Aware of the risk of further dislocation and life-threatening SCI, neurosurgical intervention was performed first in interdisciplinary consent. The setup included general anesthesia, single-shot antibiotics and cardiopulmonary monitoring with resuscitation equipment. Cardiothoracic surgeons were on standby. Occipitocervical fusion was discussed, but not possible, due to the suboccipital intradiploic arachnoid cyst causing a cerebrospinal fluid (CSF) leak after exposure to the skull during surgery (Figure 1). This CSF-leak was closed by bone wax. Finally, the C1-C2 fusion was performed by Harms technique (20) with x-ray guidance, spinal neuronavigation (BrainLab AG, Feldkirchen, Germany) and Doppler ultrasound. Bilateral pedicle screws (Symphony, DePuy Synthes, Raynham, MA, USA) fixed the C2 vertebra, while bilateral mass screws (Symphony, DePuy Synthes, Raynham, MA, USA) were positioned in C1. The posterior atlas fragments were removed by laminectomy, and bone granulate was deposited.
The patient was monitored postoperatively in the intensive care unit (ICU) and later transferred to the neurosurgical ward in stable condition. Postoperative CT scan confirmed correct intraosseous screw positioning. Thromboprophylaxis (enoxaparin) was administered, while aspirin was paused pre- and postoperatively to prevent hemorrhage. Intravenous antibiotics (vancomycin, meropenem, clindamycin) were administered and a lumbar drain was placed. In the course, infection parameters decreased and wound healing was regular. The patient was discharged on day 12. Soft cervical collar was recommended for additional 4 weeks. One month later coronary artery bypass surgery (anastomosis of the left mammary artery to RD1 and the left radial artery to posterior interventricular ramus) was performed. Life-long medication with aspirin was resumed. Rivaroxaban was started due to intermittent atrial fibrillation. The patient was discharged to rehabilitation on day 7.
Follow-up
Three months' follow-up CT scan confirmed beginning fusion of the fractures (fusion of anterior arch of C1 and beginning fusion of odontoid process (Figure 3). The patient did not develop any neurological deficits and recovered completely from both surgeries.
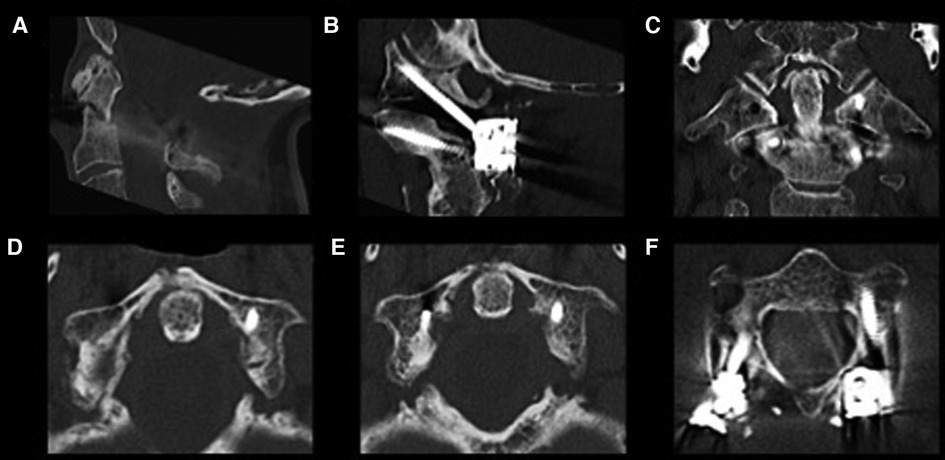
Figure 3. Follow-up sagittal (A,B), coronal (C) and axial (D–F) CT scan revealed proper intraosseous positioning of the screws, furthermore sufficient decompression of atlantoaxial region (A) and beginning fusion the odontoid process (C) and the anterior arch of C1 (D,E).
Discussion
Treating complex C1/C2 fractures with concomitant CAD requiring cardiac surgery is challenging. In addition to surgical indications, the patient's individual risk factors must be considered when determining the definitive therapy (1, 2, 6, 9, 21). Bypass surgery is the standard of care in three-vessel or left main CAD, resulting in lower rates of cardiac or cerebrovascular events compared with percutaneous coronary intervention (22). Preferably, surgery is performed after a stable interval of 2–3 days (14). Myocardial infarction is also a severe complication of noncardiothoracic surgery. For lumbar spine surgery, Harwin et al. (23) reported a significantly higher risk of postoperative MI in men, which increases with age. Furthermore, the incidence was higher in fusion surgeries than in nonfusion surgeries (23). Although systematic evidence is lacking, to best of our knowledge cases of postoperative MI have been described following upper cervical spine fusion (9, 24, 25). In high-risk constellations, it is advisable to provide cardiac and hemodynamic monitoring in the ICU. Decompression of cervical spine trauma at risk for secondary SCI is recommended at least within the first 24 h (21). Cardiovascular complications are a leading cause of death in cervical or high-thoracic (above T6) SCIs because of damage of supraspinal sympathetic nervous system control (26). Consecutive shift towards parasympathetic-dominated heart control leads to bradycardia, orthostatic hypotension, autonomic dysreflexia, and cardiac arrest (26). Hence, early management of cardiac arrhythmias and neurogenic shock is crucial to improve patient outcome.
Neurosurgical concepts
Fortunately, occipitocervical fusion is rarely required since occipitoatlantal joint injury is seen in only 0,8%–1,1% of extreme trauma (5). In general, therapy for type I injuries and dislocated type II and type III injuries according to Anderson and Montesano (27) is conservative by closed repositioning and rigid immobilization for 6–12 weeks. In case of therapy failure or type III injury with ligamentous instability, C0–C2 fixation with modular occipital plate-rod construct is the strongest way to achieve fusion. On the other hand, the atlantoaxial joint is most prone to instability after cervical spine injury, with occipitocervical fusion reserved for the most complex (28). Atlas fractures account for 2%−13% of cervical spine injuries and occur through axial load (4, 5, 8, 28, 29). Ranging from 30% to 70% of prevalence, C1 fractures are associated with other cervical spine injuries with fractures of the odontoid process being the most significant (8, 28). Combined C1/C2 injuries have a higher rate of neurological deficits, morbidity and mortality. Non-operative management depends on C1-fracture type according to Gehweiler et al. (19): Isolated anterior (type I) and posterior (type II) arch, as well as lateral mass (type IV) and transverse process (type V) fractures are treated by immobilization in a neck brace for 6–12 weeks (8, 28). For type IV fractures with incongruence in the occipitocervical or atlantoaxial joints repositioning followed by halo-fixation for 6–12 weeks is recommended (5). Therapy of Jefferson's fractures (type III) varies depending on the condition of the transverse atlantal ligament (TAL). Conservative treatment by halo-fixation for 12 weeks is possible in stable type III-A fractures. Indication for posterior C1-C2 fusion is due to a large displacement, comminution and unstable Jefferson's fracture (type III-B), characterized by vertical atlantoaxial instability with partial or complete tearing of the TAL (6, 8, 28, 29). Imaging criteria for TAL likely to be disrupted are an overhang of the lateral masses of C1 > 6,9 mm beyond the lateral masses of C2 or enlargement of the anterior atlantodental interval > 3 mm (5, 8). Odontoid fractures account for 9%–15% of cervical spine fractures and are predominantly caused by hyperextension or hyperflexion trauma (8). According to Anderson and D'Alonzo (17), these are classified as type I-III fractures. In general, type I and most type III fractures are treated by external immobilization for 3–6 months (8). Type II fractures represent the most difficulty in management. Grauer et al. (18) proposed a subtype classification for decision-making: Non-displaced type II-A fractures can be treated conservative, while displacement and type II-B fractures require an anterior odontoid screw (8). Type II-C is defined as an unstable, displaced fracture extending from anterior-inferior to posterior-superior. Especially in geriatric patients (Age > 65 years), posterior C1-C2 fusion is the procedure of choice. Nonetheless, pseudarthrosis is seen in conservative therapy of type II odontoid fractures in geriatric patients (5, 6, 9). The literature (Table 1) offers various posterior C1-C2 fusion methods for atlantoaxial instability depending on patient's anatomy, comorbidities and concurrent injuries (8, 42). In general, Harms technique (20) using polyaxial screws is widely accepted as the standard of care (5, 28, 29). Special advantages, disadvantages and risks of different anterior and posterior fixation-techniques are summarized in Table 1. Common risks of all techniques are superficial and deep infections, malpositioning of screws, implant loosening and pseudoarthrosis. Moreover, Alhashash et al. (43) proposed a minimally invasive percutaneous procedure to achieve reduction in surgery time, blood loss and wound-healing disorder. Fusion rates have been reported as high as 100% after posterior atlantoaxial screw fixation (44). Nonetheless, reduced rotational capacity of the cervical spine remains a disadvantage.
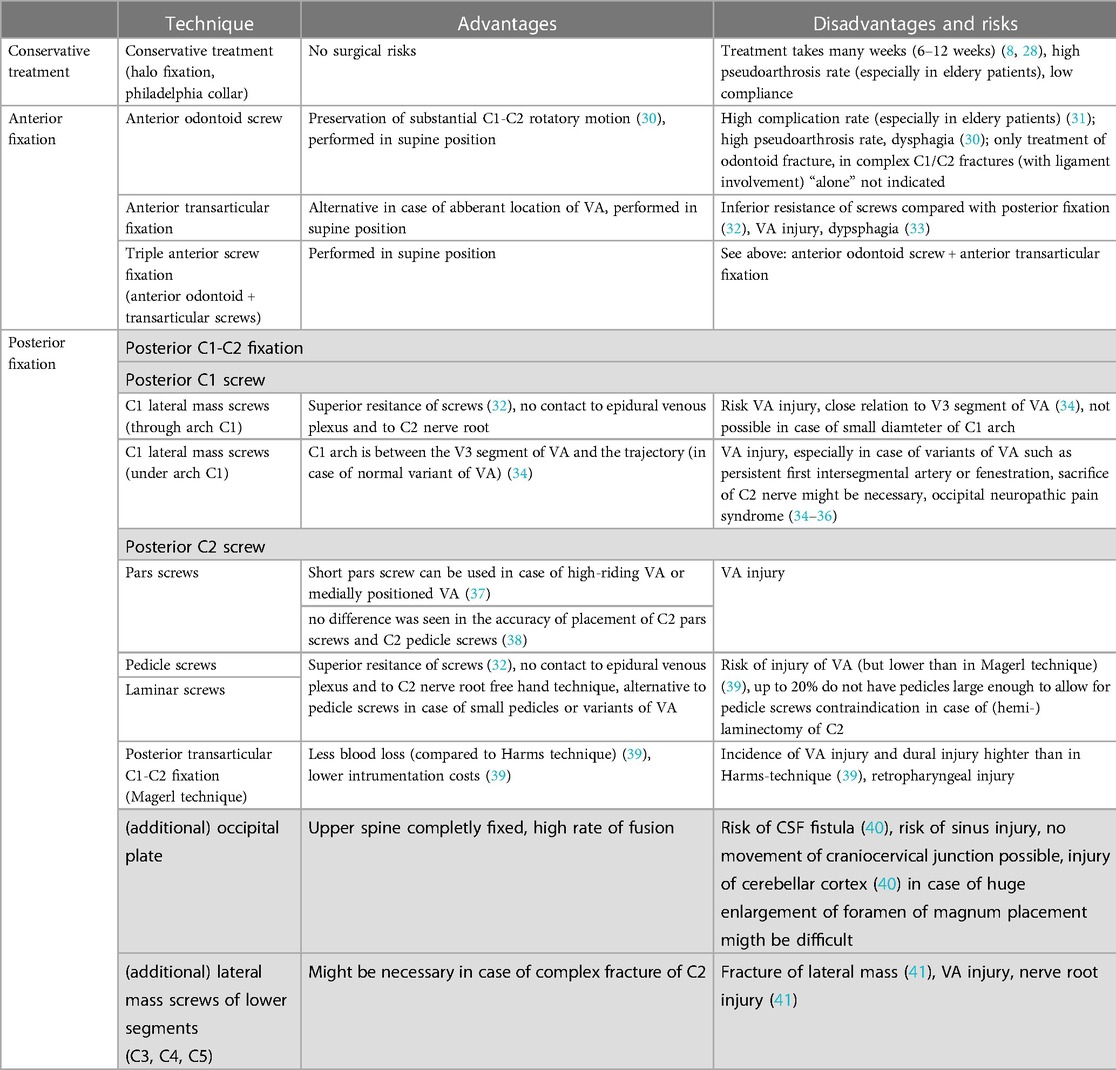
Table 1. Special advantages, disadvantages and risks of conservative treatment vs. different anterior and posterior fixation techniques for complex C1/C2 fractures.
C1-C2 fusion: risks and rescue techniques
As mentioned, x-ray guidance, spinal neuronavigation and Doppler ultrasound may be helpful to achieve safer screw insertion. Regarding vascular complications of fusion techniques, the rate of VAI after C1-C2 fusion was found to be 2% per patient and 1% per screw inserted in a systematic review by Ghaith et al. (45) Currier et al. (46) investigated the potential risk of injury to internal carotid artery (ICA) during screw placement into C1. The ICA was found to be at moderate risk on at least one side in 46% of cases and at high risk in 12% of cases (46). The course of these brain-supplying vessels to the atlas, the axis and in the lateral region to the facet joints may differ individually. Therefore, appropriate trajectory should be carefully assessed on CT angiography to reduce injury risk during screw positioning.
Furthermore, ganglionectomy of the C2 nerve root should be avoided, even if the sectioning is generally safe. Superior and inferior mobilization of the C2 nerve root can assist in appropriate exposure for screw insertion and placement of the implants (42).
Ryken et al. (35) concluded that class III medical evidence exists for a variety of treatment options of combined fractures of the atlas and axis in adults, and reviewed different concepts for their management, which included conservative management, posterior C1-C2 fixation, anterior odontoid screw fixation, occipitocervical fusion and posterior transarticular fixation of C1-C2. Furthermore, the anterior transarticular fixation for C1-C2 fractures had been described (also in some cases with additional screw fixation of odontoid process, so called ‘triple anterior screw fixation’) (47–51). Agrillo et Mastronardi (48) described this technique in a case of a 92-year-old man with posterior arch fracture of the atlas, associated with a type II odontoid fracture. The advantage of this procedure is that it can be performed in supine position. For Jefferson’s fracture together with odontoid type II-C fracture Guiot et Fessler (52) described one case which they treated by ‘triple anterior screw fixation’.
However, in case of Jefferson’s fracture a shift of the fragments of C1 might be possible using this stabilization technique. Levine et Edwards (49) mentioned that this technique is fraught “with great surgical risks and are not easily accomplished”. In our opinion in case of fracture of C1 and C2 with three-vessel CAD with high-grade coronary artery stenosis this option should also be discussed in future.
Nontraumatic intradiploic arachnoid cyst
Weinand et al. (53) first introduced the term intradiploic arachnoid cyst. Nontraumatic intradiploic cysts (the only extradural manifestation of intracranial arachnoid cysts) expand the diploic space through a small congenital dural defect due to CSF-pulsation while the outer table of the skull is intact. In general, it is a coincident radiological finding in asymptomatic patients without trauma history. Nonetheless, cases with symptoms such as headache, dizziness, and local pain have been reported in the literature (54–57). CT scan reveals solitary or multiple, intradiploic, CSF-density, symmetrical well-demarcated lytic lesions with focal cortical erosions (53, 57). Differential diagnoses include epidermoid/dermoid cyst, hemangioma, intraosseus meningioma, eosinophilic granuloma, plasmacytoma, osteogenic sarcoma and metastasis (53, 55–57). Intradiploic arachnoid cysts are primary documented in the occipital bone (53–56), whereas our patient presented one in the suboccipital bone. This cyst localization made occipitocervical fusion impossible. The surgical treatment consists of the excision of the pedicle by craniectomy and repair of dural and skull defects. However, given the benign nature of the lesion, we strongly recommend radiological follow-up for small cysts in asymptomatic patients.
Conclusion
Complex C1/C2 fractures with concomitant severe CAD remain challenging and require an individual approach to receive upper cervical spine stability and to prevent both, SCI and cardiovascular complications. If the injuries are unstable and bypass surgery is not immediately necessary, surgical intervention is indicated. Therefore, interdisciplinary cooperation is essential to determine optimal therapeutic algorithms.
Data availability statement
The original contributions presented in the study are included in the article, further inquiries can be directed to the corresponding author.
Ethics statement
Written informed consent was obtained from the individual(s) for the publication of any potentially identifiable images or data included in this article.
Author contributions
All authors listed have made substantial, direct, and intellectual contribution to the work and approved it for publications. MED: wrote the article, performed analyses, figure design; HM: performed analyses and critical revision; AÖ: performed analyses and critical revision; MT: performed analyses and critical revision; MR: performed analyses and critical revision, SDA: performed analyses, critical revision, figure design. All authors contributed to the article and approved the submitted version.
Funding
We acknowledge support by Deutsche Forschungsgemeinschaft and Open Access Publishing Fund of the University of Tübingen.
Conflict of interest
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
Publisher's note
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
References
1. Varma A, Hill EG, Nicholas J, Selassie A. Predictors of early mortality after traumatic spinal cord injury: a population-based study. Spine. (2010) 35(7):778–83. doi: 10.1097/BRS.0b013e3181ba1359
2. Hasler RM, Exadaktylos AK, Bouamra O, Bennecker LM, Clancy M, Sieber R, et al. Epidemiology and predictors of cervical spine injury in adult major trauma patients: a multicenter cohort study. Journal of Trauma and Acute Care Surgery. (2012) 72(4):975–981. doi: 10.1097/TA.0b013e31823f5e8e
3. Goldberg W, Mueller C, Panacek E, Tigges S, Hoffman JR, Mower WR. Distribution and patterns of blunt traumatic cervical spine injury. Ann Emerg Med. (2001) 38(1):17–21. doi: 10.1067/mem.2001.116150
4. Riascos R, Bonfante E, Cotes C, Guirguis M, Hakimelahi R, West C. Imaging of atlanto-occipital and atlantoaxial traumatic injuries: what the radiologist needs to know. RadioGraphics. (2015) 35(7):2121–34. doi: 10.1148/rg.2015150035
5. Scholz M, Kandziora F, Hildebrand F, Kobbe P. Verletzungen der oberen halswirbelsäule: update zu diagnostik und management. Unfallchirurg. (2017) 120(8):683–700. doi: 10.1007/s00113-017-0380-8
6. Charles YP, Ntilikina Y, Blondel B, Fuentes S, Allia J, Bronsard N, et al. Mortality, complication, and fusion rates of patients with odontoid fracture: the impact of age and comorbidities in 204 cases. Arch Orthop Trauma Surg. (2019) 139(1):43–51. doi: 10.1007/s00402-018-3050-6
7. Stiell IG, Wells GA, Vandemheen KL, Clement CM, Lesiuk H, De Maio VJ, et al. The Canadian C-spine rule for radiography in alert and stable trauma patients. JAMA. (2001) 286(15):1841. doi: 10.1001/jama.286.15.1841
8. Kalantar SB. Fractures of the C1 and C2 vertebrae. Semin Spine Surg. (2013) 25(1):23–35. doi: 10.1053/j.semss.2012.07.002
9. Ryang YM, Török E, Janssen I, Reinke A, Buchmann N, Gempt J, et al. Early morbidity and mortality in 50 very elderly patients after posterior atlantoaxial fusion for traumatic odontoid fractures. World Neurosurg. (2016) 87:381–391. doi: 10.1016/j.wneu.2015.12.026
10. Inamasu J, Guiot BH. Vertebral artery injury after blunt cervical trauma: an update. Surg Neurol. (2006) 65(3):238–45. doi: 10.1016/j.surneu.2005.06.043
11. Cothren CC, Moore EE, Ray CE, Johnson JL, Moore JB, Burch JM. Cervical spine fracture patterns mandating screening to rule out blunt cerebrovascular injury. Surgery. (2007) 141(1):76–82. doi: 10.1016/j.surg.2006.04.005
12. Fassett DR, Dailey AT, Vaccaro AR. Vertebral artery injuries associated with cervical spine injuries: a review of the literature. J Spinal Disord Tech. (2008) 21(4):252–8. doi: 10.1097/BSD.0b013e3180cab162
13. Post F, Münzel T. Das akute koronarsyndrom: eine in der praxis unscharf gehandhabte diagnose. Internist. (2010) 51(8):953–62. doi: 10.1007/s00108-009-2536-2
14. Rupprecht HJ, Geeren M, Geeren M, Weilemann S, Schuster HP. Akutes koronarsyndrom ohne ST-hebung (NSTE-ACS). Herz. (2019) 44(1):10–5. doi: 10.1007/s00059-018-4776-1
15. Kumagai N, Dohi K, Tanigawa T, Ito M. Haemodynamic collapse in a patient with acute inferior myocardial infarction and concomitant traumatic acute spinal cord injury. Case Rep. (2013) 2013(nov22 1):bcr2013201544-bcr2013201544. doi: 10.1136/bcr-2013-201544
16. Bowers CA, Jost GF, Dailey AT. An odontoid fracture causing apnea, cardiac instability, and quadriplegia. Case Rep Crit Care. (2012) 2012:1–2. doi: 10.1155/2012/821565
17. Anderson LD, D'alonzo RT. Fractures of the odontoid process of the axis. J Bone Jt Surg. (1974) 56(8):1663–74. doi: 10.2106/00004623-197456080-00017
18. Grauer JN, Shafi B, Hilibrand AS, Harrop JS, Kwon BK, Beiner JM, et al. Proposal of a modified, treatment-oriented classification of odontoid fractures. The Spine Journal. (2005) 5(2):123–129. doi: 10.1016/j.spinee.2004.09.014
19. Gehweiler JA, Osborne RL, Becker RF. The radiology of vertebral trauma. Philadelphia: Saunders (1980).
20. Harms J, Melcher RP. Posterior C1–C2 fusion with polyaxial screw and rod fixation. Spine. (2001) 26(22):2467–71. doi: 10.1097/00007632-200111150-00014
21. Fehlings MG, Tetreault LA, Wilson JR, Aarabi B, Anderson P, Arnold PM, et al. A clinical practice guideline for the management of patients with acute spinal cord injury and central cord syndrome: recommendations on the timing (≤24 hours vs. >24 hours) of decompressive surgery. Global Spine Journal. (2017) 7(3_suppl):195S–202S. doi: 10.1177/2192568217706367
22. Serruys PW, Morice MC, Kappetein AP, Colombo A, Holmes DR, Mack MJ, et al. Percutaneous coronary intervention vs. coronary-artery bypass grafting for severe coronary artery disease. N Engl J Med. (2009) 360(10):961–972. doi: 10.1056/NEJMoa0804626
23. Harwin B, Formanek B, Spoonamore M, Robertson D, Buser Z, Wang JC. The incidence of myocardial infarction after lumbar spine surgery. Eur Spine J. (2019) 28(9):2070–6. doi: 10.1007/s00586-019-06072-4
24. Platzer P, Thalhammer G, Oberleitner G, Schuster R, Vécsei V, Gaebler C. Surgical treatment of Dens fractures in elderly patients. J Bone Jt Surg. (2007) 89(8):1716–22. doi: 10.2106/JBJS.F.00968
25. Wu MT, Chang WC, Hu TL, Shen CC. Modified Halifax interlaminar clamp with shaped autograft secured with polydioxanone(PDS) improves C1-C2 fusion. J Med Sci. (2011) 31(1):37–40. doi: 10.6136/JMS.2011.31(1).037
26. Furlan JC, Fehlings MG. Cardiovascular complications after acute spinal cord injury: pathophysiology, diagnosis, and management. FOC. (2008) 25(5):E13. doi: 10.3171/FOC.2008.25.11.E13
27. Anderson PA, Montesano PX. Morphology and treatment of occipital condyle fractures. Spine. (1988) 13(7):731–6. doi: 10.1097/00007632-198807000-00004
28. Kandziora F, Chapman JR, Vaccaro AR, Schroeder GD, Scholz M. Atlas fractures and atlas osteosynthesis: a comprehensive narrative review. J Orthop Trauma. (2017) 31(4):S81–9. doi: 10.1097/BOT.0000000000000942
29. Lleu M, Charles YP, Blondel B, Baressi L, Nicot B, Challier V, et al. C1 fracture: analysis of consolidation and complications rates in a prospective multicenter series. Orthopaedics & Traumatology: Surgery & Research. (2018) 104(7):1049–1054. doi: 10.1016/j.otsr.2018.06.014
30. Lee T-K, Han M-S, Lee S-K, Moon BJ, Lee J-K. Outcomes of patients undergoing anterior screw fixation for odontoid fracture and analysis of the predictive factors for surgical failure. Neurospine. (2020) 17:603–9. doi: 10.14245/ns.2040362.181
31. Andersson S, Olerud C, Rodrigues M. Odontoid fractures: high complication rate associated with anterior screw fixation in the elderly. Eur Spine J. (2000) 9:56–9. doi: 10.1007/s005860050009
32. Gembruch O, Ahmadipour Y, Lemonas E, Müller O. The anterior transarticular fixation of C1/C2 in the elderly with Dens fractures. Int J Spine Surg. (2020) 14:162–9. doi: 10.14444/7031
33. Mourad MA, Ottenbacher A, Rizk AR. Modified anterior transarticular C1/2 fixation for odontoid fractures: an approach with high complication rate in geriatric population. Surg Neurol Int. (2022) 13:457. doi: 10.25259/SNI_707_2022
34. Haas P, Hauser T-K, Kandilaris K, Schenk S, Tatagiba M, Adib SD. Posterolateral epidural supra-C2-root approach (PESCA) for biopsy of lesions of the odontoid process in same sitting after occipitocervical fixation and decompression-perioperative management and how to avoid vertebral artery injury. Neurosurg Rev. (2021) 44(5):2947–56. doi: 10.1007/s10143-020-01468-z
35. Hu Y, Kepler CK, Albert TJ, Yuan Z, Ma W, Gu Y, et al. Accuracy and complications associated with the freehand C-1 lateral mass screw fixation technique: a radiographic and clinical assessment: clinical article. SPI. (2013) 18:372–7. doi: 10.3171/2013.1.SPINE12724
36. Huang D, Hao D, Li G, Guo H, Zhang Y, He B. C 2 nerve dysfunction associated with C 1 lateral mass screw fixation: c 2 nerve dysfunction after C 1 fixation. Orthop Surg. (2014) 6:269–73. doi: 10.1111/os.12136
37. Eshra MA. C2 pars/pedicle screws in management of craniocervical and upper cervical instability. Asian Spine J. (2014) 8:156–60. doi: 10.4184/asj.2014.8.2.156
38. Azimi P, Yazdanian T, Benzel EC, Aghaei HN, Azhari S, Sadeghi S, et al. Accuracy and safety of C2 pedicle or pars screw placement: a systematic review and meta-analysis. J Orthop Surg Res. (2020) 15:272. doi: 10.1186/s13018-020-01798-0
39. Dunn RN, Stander H. Atlanto-axial fusion: magerl transarticular vs. Harms instrumentation techniques. SA Orthopaedic J. (2014) 13(2):31–4.
40. Macki M, Hamilton T, Pawloski J, Chang V. Occipital fixation techniques and complications. J Spine Surg. (2020) 6:145–55. doi: 10.21037/jss.2019.12.01
41. Katonis P, Papadakis SA, Galanakos S, Paskou D, Bano A, Sapkas G, et al. Lateral mass screw complications: analysis of 1662 screws. J Spinal Disord Tech. (2011) 24:415–20. doi: 10.1097/BSD.0b013e3182024c06
42. Goel A. Craniovertebral junction instability: a review of facts about facets. Asian Spine J. (2015) 9(4):636. doi: 10.4184/asj.2015.9.4.636
43. Alhashash M, Shousha M, Gendy H, Barakat AS, Boehm H. Percutaneous posterior transarticular atlantoaxial fixation for the treatment of odontoid fractures in the elderly: a prospective study. Spine. (2018) 43(11):761–6. doi: 10.1097/BRS.0000000000002417
44. Dickman CA, Sonntag VKH. Posterior C1-C2 transarticular screw fixation for atlantoaxial arthrodesis. Neurosurgery. (1998) 43(2):275–80. doi: 10.1097/00006123-199808000-00056
45. Ghaith AK, Yolcu YU, Alvi MA, Bhandarkar AR, Sebastian AS, Freedman BA, et al. Rate and characteristics of vertebral artery injury following C1-C2 posterior cervical fusion: a systematic review and meta-analysis. World Neurosurgery. (2021) 148:118–126. doi: 10.1016/j.wneu.2020.12.165
46. Currier BL, Maus TP, Eck JC, Larson DR, Yaszemski MJ. Relationship of the internal carotid artery to the anterior aspect of the C1 vertebra: implications for C1–C2 transarticular and C1 lateral mass fixation. Spine. (2008) 33(6):635–9. doi: 10.1097/BRS.0b013e318166e083
47. Ryken TC, Hadley MN, Aarabi B, Dhall SS, Gelb DE, Hurlbert RJ, et al. Management of acute combination fractures of the atlas and axis in adults. Neurosurgery. (2013) 72(Suppl 2):151–8. doi: 10.1227/NEU.0b013e318276ee55
48. Agrillo U, Mastronardi L. Acute combination fracture of atlas and axis: “triple” anterior screw fixation in a 92-year-old man: technical note. Surg Neurol. (2006) 65:58–62. doi: 10.1016/j.surneu.2005.04.043
49. Levine AM, Edwards CC. Treatment of injuries in the C1-C2 Complex. Orthopedic Clin North Am. (1986) 17:31–44. doi: 10.1016/S0030-5898(20)30416-8
50. Dean Q, Jiefu S, Jie W, Yunxing S. Minimally invasive technique of triple anterior screw fixation for an acute combination atlas-axis fracture: case report and literature review. Spinal Cord. (2010) 48:174–7. doi: 10.1038/sc.2009.108
51. Ben Aïcha K, Laporte C, Akrout W, Atallah A, Kassab G, Jégou D. Surgical management of a combined fracture of the odontoid process with an atlas posterior arch disruption: a review of four cases. Orthop Traumatol Surg Res. (2009) 95:224–8. doi: 10.1016/j.otsr.2008.11.004
52. Guiot B, Fessler RG. Complex atlantoaxial fractures. J Neurosurg. (1999) 91:139–43. doi: 10.3171/spi.1999.91.2.0139
53. Weinand ME, Rengachary SS, McGregor DH, Watanabe I. Intradiploic arachnoid cysts: report of two cases. J Neurosurg. (1989) 70(6):954–8. doi: 10.3171/jns.1989.70.6.0954
54. Hasegawa H, Bitoh S, Koshino K, Obashi J, Iwaisako K, Fukushima Y. Nontraumatic intradiploic arachnoid cysts report of five cases. Neurol Med Chir (Tokyo). (1992) 32(12):887–90. doi: 10.2176/nmc.32.887
55. Iplikcioglu AC, Dinc C, Bikmaz K, Bek S, Gokduman CA, Cosar M. Non-traumatic intradiploic arachnoid cyst. Acta Neurochir (Wien). (2006) 148(6):659–62. doi: 10.1007/s00701-006-0746-0
56. Sharma R, Gupta P, Mahajan M, Sharma P, Gupta A, Khurana A. Giant nontraumatic intradiploic arachnoid cyst in a young male. Radiol Bras. (2016) 49(5):337–9. doi: 10.1590/0100-3984.2013.0022
Keywords: Jefferson's fracture, odontoid fracture, coronary artery disease, intradiploic arachnoid cyst, interdisciplinary
Citation: Di Francesco ME, Magunia H, Örgel A, Tatagiba M, Radwan M and Adib SD (2023) Case report: Interdisciplinary treatment of complex C1/C2 fractures in a patient with concomitant three-vessel coronary artery disease requiring bypass surgery. Front. Surg. 10:1123947. doi: 10.3389/fsurg.2023.1123947
Received: 14 December 2022; Accepted: 25 April 2023;
Published: 16 May 2023.
Edited by:
Carlos A. Bagley, University of Texas Southwestern Medical Center, United StatesReviewed by:
Luca Ricciardi, Sapienza University of Rome, ItalyBarbara Cappelletto, Ospedale Santa Maria della Misericordia di Udine, Italy
© 2023 Di Francesco, Magunia, Örgel, Tatagiba, Radwan and Adib. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: S. D. Adib c2FzYW5fYWRpYjIwMDJAeWFob28uZGU=
 M. E. Di Francesco1
M. E. Di Francesco1 H. Magunia
H. Magunia M. Tatagiba
M. Tatagiba S. D. Adib
S. D. Adib