- 1Department of Orthopedics, Beijing Jishuitan Hospital, Capital Medical University, Beijing, China
- 2Department of Joint Surgery, Beijing Jishuitan Guizhou Hospital, Guiyang, China
Objective: To compare the clinical outcomes of performing a closed tibial high osteotomy with an open osteotomy and the changes in posterior tibia slope and patellar height.
Methods: Methods were collected from three hundred and forty patients (440 knees) with high tibial osteotomy performed from January 2019 to January 2020. Forty patients (50 knees) had a lateral closed wedge tibial osteotomy (LCWHTO), and 300 patients (390 knees) had a medial open wedge tibial osteotomy (MOWHTO). The follow-up periods were 20.5 months and 19.9 months, respectively. At the final follow-up visit, both groups evaluated the Lysholm score and joint range of motion (ROM). Changes in preoperative and postoperative mechanical axis deviation (MAD), proximal medial tibial angle (MPTA), posterior tibial slope (PTS), and M-K index were compared between the two groups of patients.
Results: Lysholm scores were 79.6 ± 15.6 preoperatively and 96.0 ± 5.0 postoperatively in the LCWHTO group (p < 0.01); 83.7 ± 16.0 preoperatively and 94.3 ± 9.1 postoperatively in the MOWHTO group (p < 0.01). ROM was 136.0° ± 8.4° preoperatively and 133.2° ± 10.1° postoperatively in the LCWHTO group (p > 0.05); 136.5° ± 8.4° preoperatively and 135.7° ± 9.3° postoperatively in the MOWHTO group (p > 0.05). the MAD was (26.5 ± 4.1) mm preoperatively and 0.3 ± 2.9 mm postoperatively in the LCWHTO group (p < 0.01); 21.8 ± 6.5 mm preoperatively and −0.3 ± 2.6 mm postoperatively in the MOWHTO group (p < 0.01). The MPTA in the LCWHTO group was 75.3° ± 3.2° preoperatively and 89.5° ± 2.4° postoperatively (p < 0.01). 77.1° ± 3.0° preoperatively and 90.6° ± 2.7° postoperatively in the MOWHTO group (p < 0.01). M-K index was 0.78 ± 0.08 preoperatively and 0.79 ± 0.07 postoperatively in the LCWHTO group (p > 0.05). 0.78 ± 0.05 before and 0.75 ± 0.05 after surgery in the MOWHTO. 10.8° ± 3.0° PTS before and 8.1° ± 3.4° after surgery in the LCWHTO group (p < 0.05); 10.2° ± 3.1° preoperatively and 10.9° ± 4.0° postoperatively (p > 0.05).
Conclusions: LCWHTO decreases the PTS and has no effect on patellar height; MOWHTO does not affect the PTS but decreases patellar height. The patient should individualize the choice of the osteotomy.
Introduction
High tibia osteotomy (HTO) was the most successful and commonly used for treating medial compartment osteoarthritis of the knee with varus malalignment (1, 2). The basic concept of HTO was a correction of coronal malalignment, thereby shifting the weight-bearing load from the injured area to an uninjured area. The pressure in the medial compartment is decompressed, resulting in pain-relieving and delaying cartilage damage; even partial cartilage regeneration can be observed (3). In the past, lateral closed wedge HTO (LCWHTO) was the most widely used procedure; however, medial open wedge HTO (MOWHTO) was predominantly used recently owing to several advantages (4). The two types of osteotomy have their characteristics, with differences in the accuracy of lower extremity mechanical axis correction, postoperative effects on patellar height (PH), and posterior tibia slope (PTS). Changes in the PH and PTS may result in patellofemoral osteoarthritis and anterior cruciate ligament (ACL) injuries due to increased retro patellar cartilage pressure and higher anteroposterior translation, respectively. Previous studies have suggested that LCWHTO increases PH and decreases PTS, whereas MOWHTO decreases PH and PTS (5). However, most previous studies have a small sample size and inaccurate measuring methods (6, 7). This study aimed to compare the differences between these two methods by multi-center data through clinical evaluation and radiographic measurements.
Materials and methods
From January 2019 to January 2022, all patients undergoing HTO in Beijing Jishuitan Hospital, Guizhou provincial orthopedics hospital, Beijing Chaoyang emergency medical and rescue center, and Shenyang Jishuitan Hospital were enrolled in this retrospective study. This study obtained written informed consent from participants or their guardians and was approved by the Beijing Jishuitan Hospital Institutional Review Board for retrospective data analysis. The inclusion criteria were as follows: (1) patients with symptomatic genu varus, (2) patients in good condition for ligaments of the knee, and MRI was performed to check it if necessary, (3) active mobility is greater than 100° by physical examinations, (4) medial proximal tibia angle (MPTA) was less than 83°, (5) mechanical axis deviation (MAD) was greater than 8 mm. The Exclusion criteria included (1) lateral and patellofemoral compartments symptoms and (2) rheumatoid arthritis or inflammatory arthritis. All patients were fixed with TomoFix® plates (Johnson & Johnson, New Jersey, USA), LCWHTO with TomoFix® proximal tibial lateral anatomic locking plates, and MOWHTO with TomoFix® proximal tibial medial anatomic locking plate.
Surgical procedure
All patients were designed preoperatively using the Miniaci method (8). Intraspinal anesthesia was used, a tourniquet with a pressure of 300 mmHg was used during the procedure, a tourniquet was released to stop bleeding before closing the wound, and drainage was left at the osteotomy site. (1) LCWHTO: a curved oblique skin incision from 2 cm below the lateral joint line. Before tibial osteotomy, fibular midshaft osteotomy was performed at about 15 cm distal to the fibular head to decrease its tethering effect. A Kirschner pin was inserted parallel to the articular surface 2 cm below the joint line for tibial osteotomy. The calculated wedge length was marked; a second Kirschner pin was inserted toward the medial side. Osteotomy was performed to preserve the medial cortex under fluoroscopic guidance. A wedge-shaped bone was removed, leaving the medial cortex and periosteum intact. Using the creep phenomenon, a valgus force was gradually applied to close the osteotomy site. After the target mechanical axis was confirmed by fluoroscopy, the osteotomy site was fixed with a Tomofix plate. The fibular is drilled and tied with absorbable thread. (2) MOWHTO: a longitudinal skin incision was made in the medial aspect of the proximal tibia. The pes anserine was cut partially, and the superficial medial collateral ligament (MCL) was released. Distal to the joint line (3.5 cm) (9), 2 Kirschner pins were passed from the metaphyseal-diaphyseal junction in the direction of the hinge point between the tip and circumference line of the fibular head. Horizontal osteotomy was performed, leaving the lateral cortex intact. Afterward, an additional coronal osteotomy was performed almost parallel to the coronal plane and at an approximate angle of 110° with the horizontal osteotomy line. The osteotomy site was gradually opened to the calculated wedge length, and the target mechanical axis was confirmed by fluoroscopy. The osteotomy site was fixed with a Tomofix plate, and bone grafting was performed using calcium sulfate (CaSO4)/calcium phosphate (CaPO4) composite (PRO® DENSE Wright Medical Technology, Arlington, TN USA). The drainage was removed in 24 h, and partial weight-bearing was achieved under the protection of a double crutch in 48 h. Partial weight-bearing with crutches was allowed for six weeks. If the osteotomy was healing well, full weight-bearing was encouraged. They were reviewed at six weeks, 1-year, and 2-year postoperatively. Anteroposterior and lateral and lower limbs full-length films were taken.
Clinical and radiographic evaluation
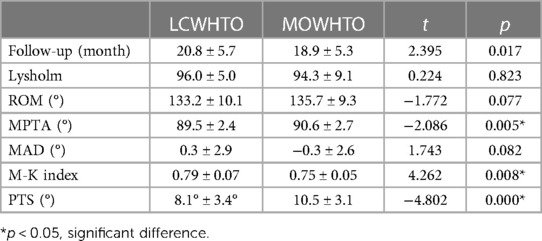
All patients' knee conditions were clinically evaluated preoperatively and at follow-up using the Lysholm score pre- and post-operative last follow-up. The evaluation included a ROM and Lysholm knee score (10). Independent of the surgical team, a rehabilitation doctor performed these measurements and was blinded to the radiographic findings. The radiographic examination used a digital fluoroscopy system (Sonial-vision Saline lI, Shimadzu, Japan). Pre- and post-operative lower extremity full-length radiographs of the patient's lower limbs and AP and lateral radiographs of the knee were taken (Figure 1). Changes in the patient's pre- and post-operative MPTA, MAD, and PTS were measured. The M-K index (Miura-Kawamura index) is estimated to estimate PH. The measurement method is shown in Figure 1.
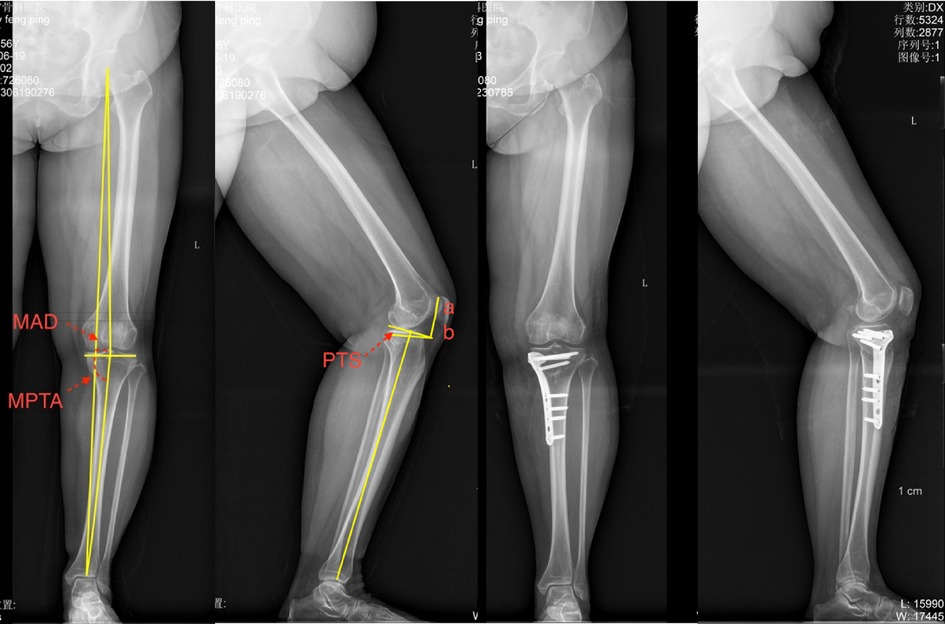
Figure 1. Preoperative and post-operative lower limb full-length, AP, and lateral films of the knee. MPTA: medial angle between the tangent line of the tibial plateau and the tibial mechanical axis in the coronal plane; MAD: distance from the center of the knee to the mechanical axis of the lower limb; PTS: angle between the vertical line of the tibial mechanical axis and the tangent line of the tibial plateau in the sagittal plane; M-K index: ratio of the distance from the lower edge of the patella to the tangent line of the femoral condyle to the length of the medial surface of the patella (a/b).
Statistical analysis
Two experienced orthopedic surgeons collected all radiographic parameters and repeatedly assessed them in a blinded fashion one week after the first measurement to reduce bias. The interclass correlation coefficients for the intra- and inter-observer agreements were calculated. Statistical evaluation was performed using SPSS 26.0 (IBM Corp., Armonk, NY, USA). The continuous data are presented as mean values ± standard deviation (SD). Differences between the groups were analyzed with the student-t test for continuous variables and the Pearson chi-square test for categorical variables. Differences were considered statistically significant at p < 0.05.
Results
From January 2019 to January 2022, 40 cases (50 knees) underwent LCWHTO, and 300 patients (390 knees) underwent MOWHTO were included. The two groups were compared, including gender, age, body mass index (BMI), preoperative range of motion (ROM), Lysholm score, M-K index, PTS, and other information. There was no statistically significant difference (P > 0.05). The MPTA and mechanical axis deviation (MAD) were compared between the LCWHTO and MOWHTO groups (P < 0.05) (Table 1).
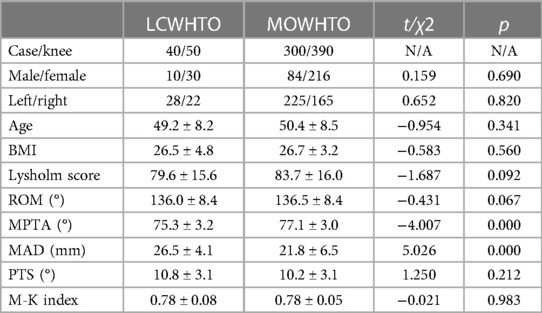
Table 1. Demographics characteristics, preoperative clinical evaluation, and radiographic measurement of LCWHTO and MOWHT.
The Lysholm score for LCWHTO was improved from 79.6 ± 15.6 to 96.0 ± 5.0 (p = 0.000); the Lysholm score for MOWHTO improved from 83.6 ± 16.0 preoperatively to 94.3 ± 9.1 postoperatively (p = 0.000). The postoperative improvement over preoperative was statistically significant in both groups. 133.2° ± 10.1° of ROM after LCWHTO and 135.7° ± 9.3° of ROM after MOWHTO, with no statistically significant difference between the two groups compared to preoperative ROM. There were no infections, vascular nerve complications, or postoperative complications such as non-union of the bone in either group. A comparison of the parameters between the two groups is shown in Table 2.
The postoperative MAD was (0.3 ± 2.9) mm in the LCWHTO group and (−0.3 ± 2.6) mm in the MOWHTO group. Both two groups were a statistically significant difference compared with that of the preoperative, respectively. The postoperative MPTA was 89.5° ± 2.4° in the LCWHTO group and 90.6° ± 5.0° in the MOWHTO group. The postoperative M-K index in the LCWHTO group was 0.75 ± 0.05. The postoperative PTS in the LCWHTO group was 0.79 ± 0.07, with a statistically significant decrease compared with that of the preoperative; the postoperative PTS in the MOWHTO group was 10.9° ± 4.0°, with no difference compared with the preoperative. The detail of comparisons preoperative and postoperative between the two groups are shown in Table 3.
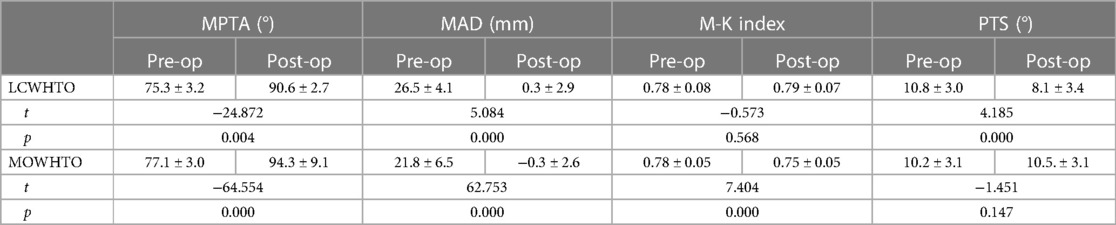
Table 3. Comparison of preoperative and postoperative radiographic evaluation between the two groups.
Discussion
Coventry started performing LCWHTO in 1965. The advantages of LCWHTO were good initial stability, no need for bone grafting, and a lower rate of non-union. The disadvantages are the need for a concomitant fibular osteotomy or superior tibiofibular joint separation and the potential for an axial offset of the proximal tibia after the osteotomy, which complicated total knee replacement if it was needed. The risk of common peroneal nerve injury is high (incidence of 1% to 2.8%). In recent years, MOWHTO has become more popular due to innovations in internal fixation materials, fixation techniques, and a wider choice of materials for bone grafting (11). The advantages of MOWHTO were that the procedure was easy to control and more accurate, with no need for a fibular osteotomy, has a low risk of common peroneal nerve injury, does not shorten the length of the lower limb, and less soft tissue stripping. The disadvantages are that bone grafting may be necessary, and there is a relatively high risk of delayed or non-healing of the bone. There may also be an increased PTS, decreased patellar height, and increased patellofemoral joint cavity pressure. MOW and LCW techniques allow for high return rates to work and sport. Ekhtiari illustrated return to sport and work rates of 87% and 85%, respectively (12). In the present study, there was no difference in the postoperative Lysholm score and ROM between the two groups at a mean follow-up of 20.5 months and 19.9 months, and both showed significant improvement compared to the preoperative period. Thus, MOWHTO and LCWHTO were essential techniques to consider candidates with genu vara who wish to return to sports, especially those involving impact loading. The most common alternative to HTO is medial unicompartmental knee arthroplasty, which has been show in some studies to be equally effective in restoring patients' activity levels (13, 14). However, unlike unicompartmental knee arthroplasty, HTO allows a faster return to impact work and sporting activities at a higher rate (15).
Recent studies have shown that OWHTO has several advantages over CWHTO, including higher accuracy of correction, better survival at ten years, a more comprehensive range of motion, less soft-tissue dissection, and more reserve of the proximal tibiofibular joint (16). However, OWHTO also increases the PTS and limb length and decreases the PH (17) Change in PTS was a risk factor for rupture of the ACL and PCL (18, 19). Therefore HTO should avoid PTS changes as possible. This study showed a difference in the preoperative MAD (p = 0.013) and MPTA (p = 0.000) between the two groups, with LCWHTO being more severe than the MOWHTO varus groups. This suggests that surgeons prefer LCWHTO in more severe cases. Matsuda compared the PTS between the varus of the knee (9.9°) and the normal knee (10.7°), and there was no difference between the two groups. Our study, therefore, suggested that the change in PTS after surgery was independent of the extent of genu varus.
Most previous studies have concluded that LCWHTO would decrease PTS and MOWHTO would increase PTS (20). A meta-analysis by Nha (21) summarised previous studies and concluded that LCWHTO decreased PTS and MOWHTO increased PTS. The increase in tibial posterior slope is attributed to the perpendicular orientation of the lateral tibial cortex, incomplete osteotomy of the posterolateral cortex, and incomplete release of posterior soft tissue (22). There are many methods to measure PTS, the tibial proximal anatomical axis (TPAA) is not affected by the patient's gender, age, or weight and is the most constant (23), so this study used TPPA for PTS measurements. In this study, the LCWHTO group had a statistically significant decrease in PTS postoperatively compared with preoperatively (p = 0.011). In contrast, there was no statistically significant difference in the change in PTS in the MOWHT group preoperatively and postoperatively (p = 0.194). This is different from many previous reports in the literature. The statement suggests that by paying attention to the operating points during the procedure, MOWHTO can prevent an increase in PTS. This indicates that careful management of the surgical technique and proper positioning of the components can help avoid undesired changes in the posterior tilt during the procedure.
The change in PTS was associated with several reasons. At first, the proximal tibia was like a triangular column, anteriorly narrow and posteriorly wide. So the osteotomy plane was angled with the coronal plane. The bottom edge of the wedge-shaped bone block resected in LCWHTO was located anterolaterally rather than laterally to the tibia, resulting in more anterior bone removal than posterior and decreased PTS, whereas, in MOWHTO, the osteotomy gap was located anteromedially to the tibia, with more spreading anteriorly than posterior, which increases PTS This increases PTS. Secondly, the origin of the superficial MCL on the tibial side was on the posteromedial side of the proximal tibia. For MOWHTO spreading, more posterior resistance resulted in a narrower spreading gap than anteriorly (24). Thirdly, for MOWHTO, the anteromedial tibia was exposed much better than the posteromedial tibia due to the anteromedial incision and simple anteromedial anatomy. Tomofix plate can easily be placed anteriorly.LaPrade's study showed that PTS increased by 4.3° when the plate was placed anteriorly and by only 1° when the plate was placed posteriorly (25). Therefore, we have several key points to avoid increased PTS when performing MOWHTO. At first, care should be taken to place the spreader as far posteriorly as possible so that the posterior spreading gap can be slightly more than the anterior gap, with a slightly trapezoidal gap to counteract error caused by the angle between the osteotomy plane and the coronal plane. The pes anserine and the superficial MCL should be adequately released. Otherwise, the gap would be wide anteriorly and narrow posteriorly, increasing the PTS.
Secondly, when placing the internal fixation, the plate should be placed as far posteriorly as possible on the medial side of the tibia rather than on the anteromedial of the proximal tibia (26). Application of the plate in a more posterior position not only avoid changes to PTS but also provides greater stability (26). Thirdly, after intraoperative fluoroscopic examination of the coronal mechanical axis, it was essential to determine the PTS on fluoroscopy before fixation. The greater the extent of correction, the more care must be taken. Otherwise, the greater the effect on the PTS. Schubert also emphasized the necessity for a small anteroposterior gap in his study of MOWHTO, where the postoperative PTS increased by only 0.07°, a statistically insignificant increase compared with the preoperative (27). The increase in PTS in MOWHTO was also shown to be avoidable in our study.
Previous studies have suggested that MOWHTO decreases PH and LCWHTO increases PH. Insall-Salvati, Blackburn-Peel, and Caton-Deschamps parameters PH were commonly used to measure patellar height. However, HTO changes the proximal tibial anatomy, and using femoral anatomical landmarks as a reference would be more accurate. Hence the M-K index was used for measurement in this study (28). This study showed no statistically significant change in PH after LCWHTO compared with preoperatively (p = 0.726). There was a statistically significant difference in PH after MOWHTO compared with preoperatively (p = 0.000). The absence of an increase in PH in the LCWHTO group was probably due to the osteotomy position being far from the joint line, which was through the lower part of the tibial tuberosity, leaving the patellar tendon origin intact and minimizing the effect on the knee extension device. Miura concluded that a change of less than 10% in the patellofemoral position would have no impact on the function of the knee extension device. In this study, the M-K index in the MOWHTO group decreased by 3% postoperatively compared with the preoperative and had little effect on clinical function.
Conclusion
LCWHTO and MOWHTO were effective procedures for unloading the medial compartment of the knee joint. Satisfactory clinical results were obtained with both LCWHTO and MOWHTO.MOWHTO avoids an increase in PTS by improving surgical procedures. MOWHTO should be avoided in patients with preoperative patellar baja to prevent further aggravation of the patellar baja. LCOHTO may decrease the PTS and should be chosen cautiously in cases with a minor preoperative PTS.
Data availability statement
The original contributions presented in the study are included in the article/Supplementary Material, further inquiries can be directed to the corresponding authors.
Ethics statement
The studies involving human participants were reviewed and approved by Beijing Jishuitan Hospital Institutional Review Board. Written informed consent to participate in this study was provided by the participants’ legal guardian/next of kin. Written informed consent was obtained from the individual(s), and minor(s)' legal guardian/next of kin, for the publication of any potentially identifiable images or data included in this article.
Author contributions
SJ and XJ conceptualized the study; SJ, YG, JZ, and FP collected and analyzed the data; SJ, YZ, and XJ interpreted the results; SJ wrote the paper; all authors discussed the results and revised the manuscript. All authors contributed to the article and approved the submitted version.
Funding
This study was supported financially by Wujieping Medical Foundation of China (320.6750.2121-20-4) and Beijing Jishuitan Hospital (XKGG 202208 to JI), and Science and Technology Fund project of Guizhou Provincial Health Commission (2024GZWJKJXM0801). The funding body had no role in the study design, data collection, analyses, interpretation, or manuscript writing.
Conflict of interest
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
Publisher's note
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
Abbreviations
MOWHTO, medial open wedge high tibial osteotomy; LCOHTO, lateral closed wedge high tibial osteotomy; MAD, mechanical axis deviation; MPTA, proximal medial tibial angle; PTS, posterior tibial slope; PH, patellar height; ACL, anterior cruciate ligament; M-K index, Miura-Kawamura index.
References
1. Jeong SH, Samuel LT, Acuña AJ, Kamath AF. Patient-specific high tibial osteotomy for varus malalignment: 3D-printed plating technique and review of the literature. Eur J Orthop Surg Traumatol. (2022) 32(5):845–55. doi: 10.1007/s00590-021-03043-8
2. Franceschi F, Longo UG, Ruzzini L, Marinozzi A, Maffulli N, Denaro V. Simultaneous arthroscopic implantation of autologous chondrocytes and high tibial osteotomy for tibial chondral defects in the varus knee. Knee. (2008) 15(4):309–13. doi: 10.1016/j.knee.2008.04.007
3. Liu X, Chen Z, Gao Y, Zhang J, Jin Z. High tibial osteotomy: review of techniques and biomechanics. J Healthc Eng. (2019) 2019:8363128. doi: 10.1155/2019/8363128
4. Murray R, Winkler PW, Shaikh HS, Musahl V. High tibial osteotomy for varus deformity of the knee. J Am Acad Orthop Surg Glob Res Rev. (2021) 5(7):e21.00141. doi: 10.5435/JAAOSGlobal-D-21-00141
5. Ducat A, Sariali E, Lebel B, Mertl P, Hernigou P, Flecher X, et al. Posterior tibial slope changes after opening- and closing-wedge high tibial osteotomy: a comparative prospective multicenter study. Orthop Traumatol Surg Res. (2012) 98(1):68–74. doi: 10.1016/j.otsr.2011.08.013
6. Cotic M, Vogt S, Hinterwimmer S, Feucht MJ, Slotta-Huspenina J, Schuster T, et al. A matched-pair comparison of two different locking plates for valgus-producing medial open-wedge high tibial osteotomy: peek-carbon composite plate versus titanium plate. Knee Surg Sports Traumatol Arthrosc. (2015) 23(7):2032–40. doi: 10.1007/s00167-014-2914-8
7. Cerciello S, Vasso M, Maffulli N, Neyret P, Corona K, Panni AS. Total knee arthroplasty after high tibial osteotomy. Orthopedics. (2014) 37(3):191–8. doi: 10.3928/01477447-20140225-08
8. Miniaci A, Ballmer FT, Ballmer PM, Jakob RP. Proximal tibial osteotomy. A new fixation device. Clin Orthop Relat Res. (1989246):250–9.2766613
9. Mederake M, Eleftherakis G, Schüll D, Springer F, Maffulli N, Migliorini F, et al. The gap height in open wedge high tibial osteotomy is not affected by the starting point of the osteotomy. BMC Musculoskelet Disord. (2023) 24(1):373. doi: 10.1186/12891-023-06478-8
10. Lysholm J, Gillquist J. Evaluation of knee ligament surgery results with special emphasis on use of a scoring scale. Am J Sports Med. (1982) 10(3):150–4. doi: 10.1177/036354658201000306
11. Niemeyer P, Stohr A, Kohne M, Hochrein A. Medial opening wedge high tibial osteotomy. Oper Orthop Traumatol. (2017) 29(4):294–305. doi: 10.1007/s00064-017-0509-5
12. Ekhtiari S, Haldane CE, de Sa D, Simunovic N, Musahl V, Ayeni OR. Return to work and sport following high tibial osteotomy: a systematic review. J Bone Joint Surg Am. (2016) 98(18):1568–77. doi: 10.2106/JBJS.16.00036
13. Belsey J, Yasen SK, Jobson S, Faulkner J, Wilson AJ. Return to physical activity after high tibial osteotomy or unicompartmental knee arthroplasty: a systematic review and pooling data analysis. Am J Sports Med. (2021) 49(5):1372–80. doi: 10.1177/0363546520948861
14. Ji S, Huang Y, Zhou Y, Wang C, Wang X, Ma C, et al. Pre-operative predictive factors of residual varus on the mechanical axis after Oxford unicompartmental knee arthroplasty. Front Surg. (2022) 9:1054351. doi: 10.3389/fsurg.2022.1054351
15. Jacquet C, Gulagaci F, Schmidt A, Pendse A, Parratte S, Argenson JN, et al. Opening wedge high tibial osteotomy allows better outcomes than unicompartmental knee arthroplasty in patients expecting to return to impact sports. Knee Surg Sports Traumatol Arthrosc. (2020) 28(12):3849–57. doi: 10.1007/s00167-020-05857-1
16. Kim JH, Kim HJ, Lee DH. Survival of opening versus closing wedge high tibial osteotomy: a meta-analysis. Sci Rep. (2017) 7(1):7296. doi: 10.1038/s41598-017-07856-8
17. Sun H, Zhou L, Li F, Duan J. Comparison between closing-wedge and opening-wedge high tibial osteotomy in patients with medial knee osteoarthritis: a systematic review and meta-analysis. J Knee Surg. (2017) 30(2):158–65. doi: 10.1055/s-0036-1584189
18. Song GY, Zhang H, Zhang J, Liu X, Xue Z, Qian Y, et al. Greater static anterior tibial subluxation of the lateral compartment after an acute anterior cruciate ligament injury is associated with an increased posterior tibial slope. Am J Sports Med. (2018) 46(7):1617–23. doi: 10.1177/0363546518760580
19. Webb JM, Salmon LJ, Leclerc E, Pinczewski LA, Roe JP. Posterior tibial slope and further anterior cruciate ligament injuries in the anterior cruciate ligament-reconstructed patient. Am J Sports Med. (2013) 41(12):2800–4. doi: 10.1177/0363546513503288
20. Ogawa H, Matsumoto K, Ogawa T, Takeuchi K, Akiyama H. Effect of wedge insertion angle on posterior tibial slope in medial opening wedge high tibial osteotomy. Orthop J Sports Med. (2016) 4(2):2325967116630748. doi: 10.1177/2325967116630748
21. Nha KW, Kim HJ, Ahn HS, Lee DH. Change in posterior tibial slope after open-wedge and closed-wedge high tibial osteotomy: a meta-analysis. Am J Sports Med. (2016) 44(11):3006–13. doi: 10.1177/0363546515626172
22. Jones GG, Jaere M, Clarke S, Cobb J. 3D Printing and high tibial osteotomy. EFORT Open Rev. (2018) 3(5):254–9. doi: 10.1302/2058-5241.3.170075
23. Bisicchia S, Scordo GM, Prins J, Tudisco C. Do ethnicity and gender influence posterior tibial slope? J Orthop Traumatol. (2017) 18(4):319–24. doi: 10.1007/s10195-017-0443-1
24. Turgut A, Kayali C, Agus H. Radiological analysis of closed-wedge high tibial osteotomy. Eklem Hastalik Cerrahisi. (2012) 23(2):82–7.22765486
25. LaPrade RF, Oro FB, Ziegler CG, Wijdicks CA, Walsh MP. Patellar height and tibial slope after opening-wedge proximal tibial osteotomy: a prospective study. Am J Sports Med. (2010) 38(1):160–70. doi: 10.1177/0363546509342701
26. Martinez de Albornoz P, Leyes M, Forriol F, Del Buono A, Maffulli N. Opening wedge high tibial osteotomy: plate position and biomechanics of the medial tibial plateau. Knee Surg Sports Traumatol Arthrosc. (2014) 22(11):2641–7. doi: 10.1007/s00167-013-2517-9
27. Schubert I, Ferner F, Dickschas J. The effect of open-wedge and closed-wedge high tibial osteotomies on the tibial posterior slope-a study of two hundred seventy-nine cases. Int Orthop. (2020) 44(6):1077–82. doi: 10.1007/s00264-020-04499-9
Keywords: high tibial osteotomy (HTO), open, closed, posterior tibial slope (PTS), patellar height (PH)
Citation: Ji S, Gao Y, Zhang J, Pan F, Zhu K, Jiang X and Zhou Y (2023) High tibial lateral closing wedge and opening wedge valgus osteotomy produce different effects on posterior tibial slope and patellar height. Front. Surg. 10:1219614. doi: 10.3389/fsurg.2023.1219614
Received: 9 May 2023; Accepted: 19 July 2023;
Published: 12 September 2023.
Edited by:
Vassilios S. Nikolaou, National and Kapodistrian University of Athens, GreeceReviewed by:
Matteo Innocenti, University of Florence, ItalyStefano Marco Paolo Rossi, Fondazione Poliambulanza Istituto Ospedaliero, Italy
© 2023 Ji, Gao, Zhang, Pan, Zhu, Jiang and Zhou. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Songjie Ji amlzb25namllQGdtYWlsLmNvbQ== Yixin Zhou b3J0aG95aW54aW5AeWFob28uY29t
 Songjie Ji
Songjie Ji Yuan Gao2
Yuan Gao2