- 1Dr. Rajesh Devassy’s Centre of Excellence in Gynecological Minimal Access Surgery and Oncology, Dubai London Clinic & Specialty Hospital, Dubai, United Arab Emirates
- 2Faculty of Mathematics and Computer Science, University of Bremen, Bremen, Germany
- 3Department of Obstetrics, Gynecology, Gynecologic Oncology and Senology, Bethesda Hospital Duisburg, Duisburg, Germany
- 4Clinic of Gynecology, Obstetrics and Gynecological Oncology, University Hospital for Gynecology, Pius-Hospital Oldenburg, Medical Campus University of Oldenburg, Oldenburg, Germany
Introduction: Pelvic organ prolapse is a common health issue that affects 30.8% of women. Laparoscopic sacrocolpopexy and colpopectopexy are two of the most common procedures to restore the pelvic anatomy. Mesh application on the other hand carries an increased complications risk over the short and long terms. The aim of this study is to provide a basis for meshless sacrocolpopexy and colpopectopexy.
Methods: This study is a retrospective cohort pilot study that analyzed the data of patients with a pelvic organ prolapse according to the pelvic organ prolapse quantification system and underwent the modified technique for sacrocolpopexy and colpopectopexy. Descriptive statistics were used to express the different variables.
Results: A total of 36 patients met the inclusion criteria and provided consent for the participation in this study. The majority of patients were postmenopausal. 22 out of 36 patients received a previous prolapse surgery. All patients presented with reducible vaginal lump. Dyspareunia and sexual dysfunction were the most commonly reported symptoms. The intraoperative complications rate was 0%. Only one patient had a postoperative persistent urinary retention that was managed medically.
Discussion: Sacrocolpopexy and colpopectopexy seems to be a safe alternative to the mesh-based pelvic surgeries with a very low rate of intraoperative complications and favorable follow up outcomes.
1. Introduction
Pelvic Organ Prolapse (POP) is the gradual descend of the pelvic structures from its normal anatomical positions to bulge into the vaginal cavity (1–3). This mainly occurs due to a progressive weakening in the pelvic ligaments with a subsequent loss of the apical support (4). The last is thought to predominantly cause anterior and middle compartment prolapse, but also could contribute to a lesser extent to the pathophysiology of the posterior prolapse (5). POP is a common condition affecting about 30.8% of women in the outpatient setting (6). Despite its wide prevalence, it only becomes symptomatic in 2%–3% of patients (7). The incidence of POP surgery peaks in the sixth decade of life, and ranges between 1.5–1.8 per 1,000 women (7, 8). However, with the increase in the living expectancy, it is expected that the number of women with POP and those seeking surgery for POP would increase within the next 20–40 years (9). Patients with symptomatic POP often complain from the sensation of a mass bulging into the vagina, urinary or fecal incontinence, and discomfort during sexual intercourse (10). The consequences of POP extend further to negatively affect the patient's body image and sexuality (11, 12).
Although POP was treated traditionally with hysterectomy (13), there are nowadays more than 40 surgical procedures to restore the normal pelvic anatomy (14). Nevertheless, hysterectomy is not among them anymore because the uterus itself is only a passive structure that has no effect on the prolapse occurrence (15, 16). Sacrocolpopexy was first described in 1957 as attaching the uterus to the sacrum to restore the normal vaginal axis (17). It is now considered the treatment of choice for POP (18, 19), despite the lack of a standardization for this procedure. Currently, laparoscopic sacrocolpopexy is heavily favored over the open approach owing to the comparable outcomes and decreased postoperative morbidity associated with the laparoscopic intervention (19). Another alternative for laparoscopic sacrocolpopexy is laparoscopic colpopectopexy, since it was proven to have comparable outcomes and less postoperative complications compared to sacrocolpopexy (20). One factor that increased the popularity of laparoscopic colpopexy approaches is the ban of transvaginal meshes for POP treatment in April 2019 by the Food and Drug Administration (FDA) due to safety concerns (21). Although the application of surgical meshes seems a safer alternative, a recent study demonstrated that the long-term complications rate of abdominal meshes is around 7%. Those may include pain, dyspareunia, mesh erosion, and small bowel ischemia in some severe cases (22). In light of these events, efforts are being made to eliminate the use of synthetic prostheses (23), or at least to promote the use of lightweight meshes in POP repair surgeries. Therefore, we aim by this paper to describe a modified technique for laparoscopic colpopexy with the use of a double-ended Mersilene suture for the purpose of utero-cervical suspension, and to report the preliminary data of patients who underwent this surgery.
2. Material and methods
2.1. Study design and setting
This is a single-centre retrospective observational study that included all patients who were admitted for surgical treatment of POP and received the modified Oxford surgical technique for colpopexy at the Dubai London Clinic and Specialty Hospital in Dubai, United Arab Emirates, between November 2017 and December 2021.
2.2. Ethical considerations and the patients consent
The study protocol was revised and approved by an independent institutional review board. All patients signed an informed consent for the participation in the study, collecting their medical data and analyzing it for research purposes. This research was conducted in accordance to the ethical standards of the declaration of Helsinki in 1946 and the guidelines of the Committee of Publication Ethics (COPE). This paper was written following the Reporting of studies Conducted using Observational Routinely-collected health Data (RECORD) statement, validated by the Enhancing the Quality and Transparency of Health Research (EQUATOR) network (www.equator-network.org).
2.3. Patient allocation and data collection
All included patients had a symptomatic Stage 2 prolapse or higher in any of the three compartments according to the Pelvic Organ Prolapse Quantification (POP-Q) system (24). The prolapse was diagnosed by gynecologic clinical examination and transvaginal ultrasound. Stress urinary incontinence was diagnosed clinically and confirmed through the urodynamic evaluation. Patients who were planning to conceive in the future, refused to receive the modified technique, refused to enroll in this study, had contraindication for general anesthesia, could not tolerate surgery due to chronic illnesses, or who were unwilling to present for at least one follow-up visit were excluded. The choice of sacrocolpopexy or colpopectopexy was done through a joint decision by the patients and the managing gynecologist after thorough clarification and explanation of both procedures. All surgeries were performed by the same surgeon. The patients were followed up postoperatively by re-evaluation during an outpatient visit each 3 months. Data regarding the patients age, symptoms, surgery type, concomitant surgical interventions, intra- and postoperative complications, follow up and recurrences were collected.
2.4. Surgical techniques description
2.4.1. Modified sacrocolpopexy technique
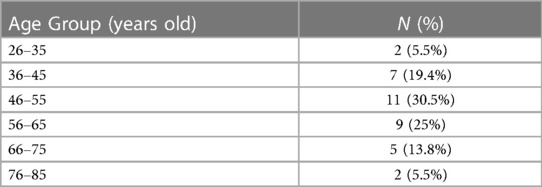
After standard patient positioning, abdominal insufflation, and classical laparoscopic ports insertion, the peritoneum over the sacral promontory was incised and the promontory was carefully dissected. The peritoneum was further opened until the retrocervical area was reached. The bladder fold was dissected to ensure an appropriate protection of the urinary bladder and the ureters. Upon completion of this step, the uterine cervix and the upper part of the vagina could be easily recognized. Afterwards, a double-ended Mersilene needle [RS21—5 mm Mersilene Tape White 1 STRIPX12″ (30 cm) BP-1 Double Armed, ©Ethicon US, LLC. 2022. Johnson & Johnson Health Care Systems Inc. 425 NJ-18, Piscataway, NJ 08854, United States] was introduced into the abdominal cavity. The Mersilene needle was inserted in the anterior left paracervical region (Figure 1A) and driven posteriorly (Figure 1B). The same procedure took place on the right side (Figure 1C). In order to avoid transvaginal suture, an assistant finger was always placed in the vagina to ensure subepithelial isolation. After appropriate tension adjustment to secure a proper suspension (Figure 1D), the suture was knotted and the knot was placed posterior to the uterine cervix (Figure 1E). The suture's ends were then fixed to the sacral promontory with permanent tackers (ProTack™) or polypropylene sutures (Figure 1F). The decision between using sutures or permanent tackers was done based on the surgeon's and patient's preference, and the cost covered by the insurance company; since tackers are much more expensive than sutures. Eventually, reperitonealization was done by continuous absorbable suture (Figure 1G).
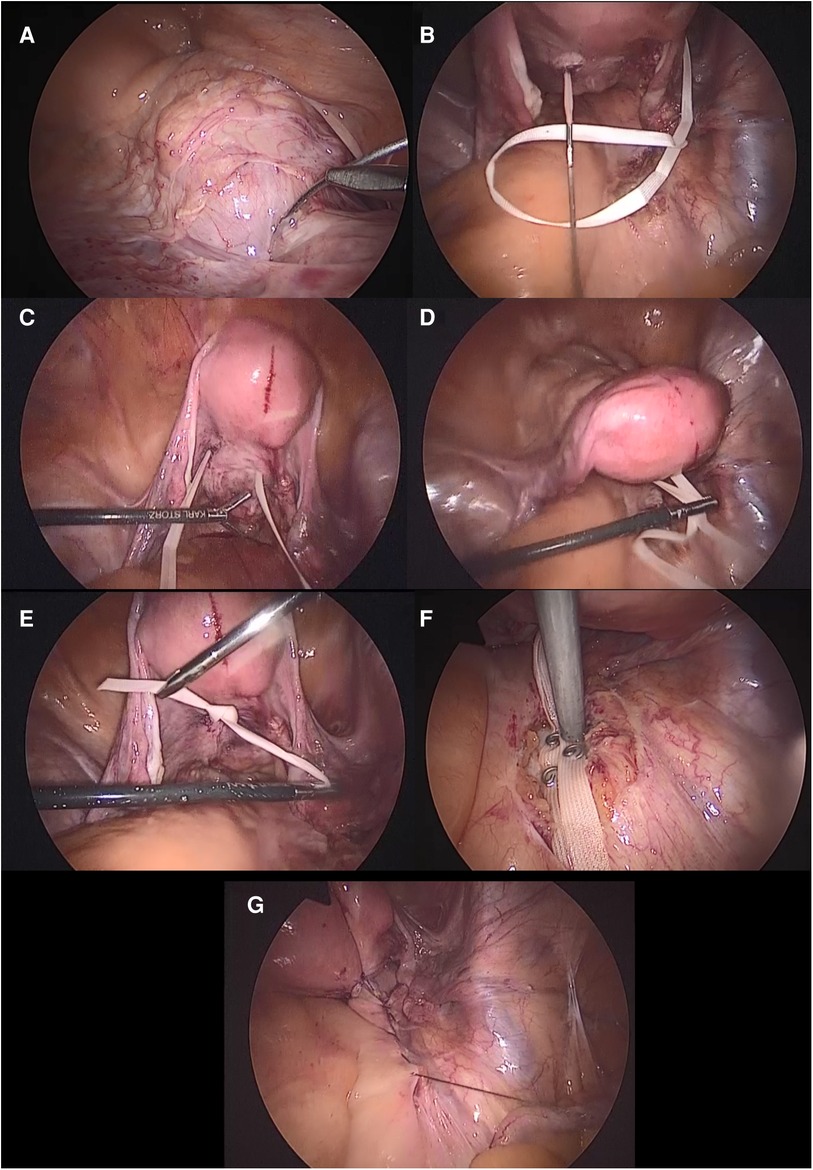
Figure 1. A graphical description of the surgical technique of the modified Mersilene-based sacrocolpopexy. (A) The Mersilene suture driven through the left region of the uterine cervix posteriorly. (B) The Mersilene suture pulled from the left posterior cervical region. (C) The same aforementioned steps repeated on the right side. (D) Tension adjustment to ensure a proper prolapse restoration. (E) The Mersilene suture knotted over the posterior surface of the uterine cervix. (F) The Mersilene suture fixed by permanent tackers on the sacral promontory or permanent polypropylene or polyester sutures. (G) Reperitonealization.
2.4.2. Modified colpopectopexy technique
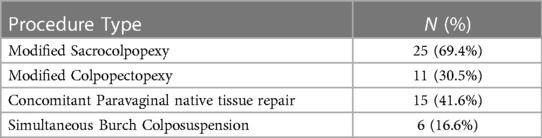
After standard patient positioning, abdominal insufflation, and classical laparoscopic ports insertion, the median umbilical ligament was incised and the dissection was carried out inferiorly until the pubic bone was reached. Thereafter, the dissection was extended laterally to identify Cooper's ligaments bilaterally. The vesico-vaginal space was carefully dissected afterwards to clearly identify the uterine cervix. The double-ended Mersilene needle was introduced into the abdominal cavity and driven transversally through the anterior paracervical fascia (Figure 2A). After intraoperative tension adjustment, the Mersilene suture was fixed to the left Cooper's ligament by a permanent suture (Figure 2B). The same was done on the right side. Eventually, reperitonealization over the suture took place.
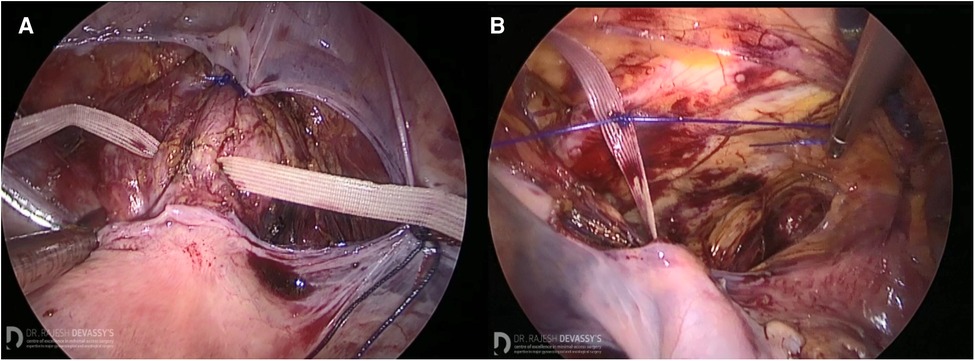
Figure 2. A graphical description of the surgical technique of the modified Mersilene-based colpopectopexy. (A) The Mersilene suture driven through the anterior paracervical fascia. (B) The Mersilene suture fixed to Cooper's ligament on the left side.
2.5. Statistical analysis
All data were analyzed by descriptive statistics. Continuous variables were expressed by ranges. Categorical variables were expressed by frequencies and percentages. The statistical analysis was performed using Statistical Package for Social Science (SPSS) software, version 25.0 (SPSS, Chicago, IL).
3. Results
A total of 36 patients met the inclusion criteria and provided consent to participate in this study. About one third of the sample (30.5%) fell in the age range 46–55 years. 16 out of 36 patients (44.4%) were postmenopausal. Table 1 demonstrates the patients’ distribution among different age groups. In our series, 10 patients (27.7%) had a previous repair of rectocele, 8 patients (22.2%) had a previous repair of cystocele and 3 patients (8.3%) had prior colposuspension with mesh. There were only 14 patients (38.8%) who did not have a previous POP surgery. 3 patients (8.3%) with prior mesh colposuspension had recurrence. It occurred after 2 years in 1 patient following childbirth, and after 7 and 10 years in the remaining two patients. Upon clinical examination, all patients had a reducible vaginal lump. Urinary incontinence was observed in 34.15% of cases. Sexual dysfunction was reported by two thirds of the patients (60.61%) and dyspareunia was reported by 41.84% of them.
The modified sacrocolpopexy was performed in 25 patients (69.4%) and the modified colpopectopexy was performed in 11 patients (30.5%). Treatment of cystocele and rectocele using native tissue repair by polypropylene sutures were performed laparoscopically in all cases, besides the modified sacrocolpopexy and colpopectopexy. Table 2 demonstrates the performed procedures. No intraoperative complications were reported, in terms of bowel or bladder injury. Only one patient had a postoperative persistent urinary retention. She was treated with intermittent catheterization for 2 weeks and bladder tonics for a period of 3 months. Thereafter, the bladder shrinkage was reduced and the compartmentalization had disappeared. Erosion or infection were not reported postoperatively by any patient. The mean follow-up time was 3 years, and ranged between 7 months and 5 years.
4. Discussion
In this study, we have provided evidence that using a Mersilene suture could be a safe alternative to synthetic meshes in the laparoscopic management of pelvic organ prolapse. The intraoperative complications rate was 0% and only one patient reported urinary retention postoperatively (2.7%). This condition was successfully treated medically. It is noteworthy that major postoperative complications such as erosion, infection, and pelvic pain were not reported by any patient. This is thought to further justify our hypothesis that the presented modified techniques are an alternative to mesh-based sacrocolpopexy and colpopectopexy. Although it is too early to draw conclusions, our sample indicates that these procedures could be helpful for patients with recurrent POP, since the majority of the sample had a previous prolapse surgery. Despite the promising results, it should be noted that this technique could be a feasible but not an easy-to-learn alternative to the traditional approaches. This is mainly attributed to the fact that the dissection of the promontory, pararectal and bladder regions are still needed. Therefore, the same inherent risks of sacrocolpopexy and colpopectopexy should be accounted for. Another drawback of this technique could be the large size of the Mersilene suture, which may hardens its introduction to the abdominal cavity. However, we believe that attaching the Mersilene suture to the cervical and pre-cervical regions is easier and more straightforward than the fixation of traditional meshes to the cervix and upper part of the vagina. On this basis, it is reasonable to postulate that the learning curve of this technique would be higher than the traditional ones. Nevertheless, high suturing skills and precise anatomical knowledge are definitely required for a safe surgery. Of note, a previous study has demonstrated that a surgeon needs to perform 60 laparoscopic sacrocolpopexy to ensure good outcomes and minimal complications rates (25).
The main aim of our modification is promoting native tissue repair and taking a step forward towards a “meshless” pelvic reconstructive surgery. Mesh-based POP surgeries are widely implicated with favorable outcomes, but the short- and long-term mesh-related complications could be the major drawback and a safety concern regarding the use of these prosthetic materials. A recent analysis demonstrated that the complications rate of heavy meshes is 18.8%, which is significantly higher than that of lightweight meshes (2.1%) (22). It is reasonable to consider the use of lightweight meshes instead of the heavier ones, especially when knowing that the recurrence rates were comparable between the two products. However, it should be noted that those complications are serious and worth consideration, especially the ureteric mesh erosion (22). In a different series reporting on the mesh-related complications after the uphold procedure, the erosion and pelvic pain rates were 4% and 5% respectively (26). Another long-term follow up study demonstrated that the 24-month urinary retention rate related to mesh inlay was 2.5% and vaginal adhesions occurred in 1.2% (27). Hospitalization due to mesh-related complications occurred in 7.1% of the followed patients (27). It is already established that some risk factors increase further the risk of vaginal mesh erosion, such as smoking and performing a concomitant total hysterectomy (28). In spite of the protective advantage of supracervical hysterectomy against mesh erosion (29), this procedure could not be always indicated. Therefore, it is quite obvious that the application of abdominal meshes carries inherent risks due to the prosthetic nature of these grafts.
Laparoscopic sacrocolpopexy remains the golden standard for POP surgery (30), as it was reported to carry favorable results in terms of restoring the anterior and middle compartments (31). In their study, Campagna et al. reported that patients undergoing high uterosacral ligament suspension are at 6 times higher risk of prolapse recurrence compared to those who had laparoscopic sacrocolpopexy (8). Similarly, Maher et al. (14) found that vaginal suspension carries an increased risk of subjective failure in comparison with sacrocolpopexy. On the other hand, one randomized controlled trial has demonstrated that both laparoscopic sacrocolpopexy and colpopectopexy carry the same postoperative outcomes in terms of anterior, apical, and posterior objective failure rates (20, 32). It is noteworthy that de novo constipation was significantly more reported by patients receiving sacrocolpopexy (20). In another randomized controlled trial comparing sacrocolpopexy to sacrospinous hysteropexy, Van IJsselmuiden et al. (33) found comparable composite success, anatomical and surgical failure rates between the two groups. However, patients who had sacrocolpopexy reported significantly more fecal incontinence compared to the other study group. Bothersome over-active bladder symptoms were also more frequent among patient receiving sacrocolpopexy (33). Those urinary and fecal complications are thought to result from the presacral and pararectal dissection and a subsequent injury to the hypogastric nerves (34, 35). However, it is not clear whether the mesh-associated fibrosis could contribute to those dysfunctions.
Another feasible approach could be the uterosacral ligaments suspension. Some reports showed promising results of this technique when applied laparoscopically or by vaginal natural transluminal endoscopic surgery (36–38).
Moreover, some authors reported the use of the semitendinosus tendon for uterine suspension in sacrocolpopexy and colpopectopexy. This approach sheds light on the use of autologous materials in POP surgery but it is not studied sufficiently yet (39).
Our study has many limitations that should be accounted for. The sample size is small and the follow up period differed among patients. We did not include a control arm to test the differences between the modified and original procedures. In addition, this study was conducted in a tertiary care centre, which makes our sample prone to selection bias. Additionally, some important variables like the timing of surgery, blood loss, and postoperative pain are missing due to the retrospective design of this study. All surgical procedures were performed by the same surgeon. Although it is believed that this would improve the internal validity of this research, it limits its generalizability by making the outcomes and complications rate questionable when this technique is performed by less experienced surgeons, like residents or general gynecologists. On the other hand, the main strength of this research is introducing a new use of the Mersilene suture and highlighting the potential positive outcomes of replacing synthetic meshes with it. Finally, we need to emphasize the fact that this is a pilot study and it is early to draw conclusions about the effectiveness of this technique or recommend standardizing it instead of the current practices. Although our results are promising, future research should consider the differences in operation times, short and long term outcomes and complication rates between the traditional mesh-based surgeries and the Mersilene modified approaches through larger cohort studies and clinical trials.
5. Conclusions
The modified technique of sacrocolpopexy and colpopectopexy using a Mersilene suture seems to be a safe alternative to mesh-based pelvic prolapse surgeries. Intraoperative complications were absent and the follow up outcomes were favorable. Future research should investigate the safety, efficacy and the learning curve associated with this modified approach.
Data availability statement
The raw data supporting the conclusions of this article will be made available by the authors, without undue reservation.
Ethics statement
The studies involving human participants were reviewed and approved by The Ethical Committee of the Dubai London Clinic and Specialty Hospital, Dubai, United Arab Emirates. The patients/participants provided their written informed consent to participate in this study.
Author contributions
RD, Conceptualization and Methodology; AN, Formal Analysis and Writing—Original Draft Preparation; HK, Methodology and Writing—Review and Editing. RW, Supervision and Writing—Review & Editing. All authors meaningfully contributed to the article and approved the submitted version.
Conflict of interest
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
Publisher's note
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
References
1. American college of obstetricians and gynecologists and the American urogynecologic society. Pelvic organ prolapse. Female Pelvic Med Reconstr Surg. (2019) 25(6):397–408. doi: 10.1097/SPV.000000000000079431663890
2. Haylen BT, Maher CF, Barber MD, Camargo S, Dandolu V, Digesu A, et al. An International Urogynecological Association (IUGA)/International Continence Society (ICS) joint report on the terminology for female Pelvic Organ Prolapse (POP). Neurourol Urodyn. (2016) 35(2):137–68. doi: 10.1002/nau.2292226749391
3. Campagna G, Vacca L, Panico G, Rumolo V, Caramazza D, Lombisani A, et al. Laparoscopic sacral hysteropexy versus laparoscopic sacral colpopexy plus supracervical hysterectomy in patients with pelvic organ prolapse. Int Urogynecol J. (2022) 33(2):359–68. doi: 10.1007/s00192-021-04865-034132865
4. Madsen AM, Raker C, Sung VW. Trends in hysteropexy and apical support for uterovaginal prolapse in the United States from 2002 to 2012. Female Pelvic Med Reconstr Surg. (2017) 23(6):365–71. doi: 10.1097/SPV.000000000000042628723720
5. Kieserman-Shmokler C, Swenson CW, Chen L, Desmond LM, Ashton-Miller JA, DeLancey JO. From molecular to macro: the key role of the apical ligaments in uterovaginal support. Am J Obstet Gynecol. (2020) 222(5):427–36. doi: 10.1016/j.ajog.2019.10.00631639371
6. Samuelsson EC, Victor FT, Tibblin G, Svärdsudd KF. Signs of genital prolapse in a Swedish population of women 20 to 59 years of age and possible related factors. Am J Obstet Gynecol. (1999) 180:299–305. doi: 10.1016/s0002-9378(99)70203-69988790
7. Barber MD, Maher C. Epidemiology and outcome assessment of pelvic organ prolapse. Int Urogynecol J. (2013) 24(11):1783–90. doi: 10.1007/s00192-013-2169-924142054
8. Campagna G, Vacca L, Panico G, Vizzielli G, Caramazza D, Zaccoletti R, et al. Laparoscopic high uterosacral ligament suspension vs. laparoscopic sacral colpopexy for pelvic organ prolapse: a case-control study. Front Med. (2022) 4(9):853694. doi: 10.3389/fmed.2022.853694
9. Dieter AA, Wilkins MF, Wu JM. Epidemiological trends and future care needs for pelvic floor disorders. Curr Opin Obstet Gynecol. (2015) 27(5):380–4. doi: 10.1097/GCO.000000000000020026308198
10. Manonai J, Mouritsen L, Palma P, Contreras-Ortiz O, Korte JE, Swift S. The inter-system association between the simplified pelvic organ prolapse quantification system (S-POP) and the standard pelvic organ prolapse quantification system (POPQ) in describing pelvic organ prolapse. Int Urogynecol J. (2011) 22(3):347–52. doi: 10.1007/s00192-010-1286-y20936258
11. Lowder JL, Ghetti C, Nikolajski C, Oliphant SS, Zyczynski HM. Body image perceptions in women with pelvic organ prolapse: a qualitative study. Am J Obstet Gynecol. (2011) 204(5):441.e1-5. doi: 10.1016/j.ajog.2010.12.02421292234
12. Jelovsek JE, Barber MD. Women seeking treatment for advanced pelvic organ prolapse have decreased body image and quality of life. Am J Obstet Gynecol. (2006) 194(5):1455–61. doi: 10.1016/j.ajog.2006.01.06016647928
13. Gopinath D, Yong C, Harding-Forrester S, McIntyre F, McKenzie D, Carey M. Laparoscopic and robot-assisted suture versus mesh hysteropexy: a retrospective comparison. Int Urogynecol J. (2023) 34(1):105–13. doi: 10.1007/s00192-022-05283-635881174
14. Maher C, Feiner B, Baessler K, Christmann-Schmid C, Haya N, Brown J. Surgery for women with apical vaginal prolapse. Cochrane Database Syst Rev. (2016) 10(10):CD012376. doi: 10.1002/14651858.CD01237627696355
15. Gutman R, Maher C. Uterine-preserving POP surgery. Int Urogynecol J. (2013) 24(11):1803–13. doi: 10.1007/s00192-013-2171-224142056
16. DeLancey JO. Anatomic aspects of vaginal eversion after hysterectomy. Am J Obstet Gynecol. (1992) 166(6 Pt 1):1717–24; discussion 1724-8. doi: 10.1016/0002-9378(92)91562-o1615980
17. Arthure HG, Savage D. Uterine prolapse and prolapse of the vaginal vault treated by sacral hysteropexy. J Obstet Gynaecol Br Emp. (1957) 64(3):355–60. doi: 10.1111/j.1471-0528.1957.tb02652.x13449656
18. Anger JT, Mueller ER, Tarnay C, Smith B, Stroupe K, Rosenman A, et al. Robotic compared with laparoscopic sacrocolpopexy: a randomized controlled trial. Obstet Gynecol. (2014) 123(1):5–12. doi: 10.1097/AOG.000000000000000624463657
19. McDermott CD, Hale DS. Abdominal, laparoscopic, and robotic surgery for pelvic organ prolapse. Obstet Gynecol Clin North Am. (2009) 36(3):585–614. doi: 10.1016/j.ogc.2009.09.00419932417
20. Noé KG, Schiermeier S, Alkatout I, Anapolski M. Laparoscopic pectopexy: a prospective, randomized, comparative clinical trial of standard laparoscopic sacral colpocervicopexy with the new laparoscopic pectopexy-postoperative results and intermediate-term follow-up in a pilot study. J Endourol. (2015) 29(2):210–5. doi: 10.1089/end.2014.0413
21. Shoureshi PS, Lee W, Kobashi KC, Sajadi KP. Media coverage of the 2019 United States food and drug administration ordered withdrawal of vaginal mesh products for pelvic organ prolapse. Int Urogynecol J. (2021) 32(2):375–9. doi: 10.1007/s00192-020-04401-632601782
22. Page AS, Cattani L, Pacquée S, Claerhout F, Callewaert G, Housmans S, et al. Long-term data on graft-related complications after sacrocolpopexy with lightweight compared with heavier-weight mesh. Obstet Gynecol. (2023) 141(1):189–98. doi: 10.1097/AOG.000000000000502136701619
23. Aleksandrov A, Meshulam M, Rabischong B, Botchorishvili R. Laparoscopic TOT-like burch colposuspension: back to the future? J Minim Invasive Gynecol. (2021) 28(1):24–5. doi: 10.1016/j.jmig.2020.04.01832339752
24. Persu C, Chapple CR, Cauni V, Gutue S, Geavlete P. Pelvic organ prolapse quantification system (POP-Q)—a new era in pelvic prolapse staging. J Med Life. (2011) 4(1):75–81.21505577
25. Claerhout F, Roovers JP, Lewi P, Verguts J, De Ridder D, Deprest J. Implementation of laparoscopic sacrocolpopexy–a single centre’s experience. Int Urogynecol J Pelvic Floor Dysfunct. (2009) 20(9):1119–25. doi: 10.1007/s00192-009-0914-x19479177
26. Munch A, Greisen S, Axelsen SM, Bek KM, Glavind-Kristensen M. Treatment of apical vaginal prolapse with minimal mesh repair (uphold): patient-reported long-term outcomes and mesh-related complications. Acta Obstet Gynecol Scand. (2022) 101(6):589–96. doi: 10.1111/aogs.1432235150002
27. Reid FM, Elders A, Breeman S, Freeman RM; PROSPECT study group. How common are complications following polypropylene mesh, biological xenograft and native tissue surgery for pelvic organ prolapse? A secondary analysis from the PROSPECT trial. BJOG. (2021) 128(13):2180–9. doi: 10.1111/1471-0528.16897
28. Cundiff GW, Varner E, Visco AG, Zyczynski HM, Nager CW, Norton PA, et al. Risk factors for mesh/suture erosion following sacral colpopexy. Am J Obstet Gynecol. (2008) 199(6):688.e1-5. doi: 10.1016/j.ajog.2008.07.02918976976
29. Dallas K, Taich L, Kuhlmann P, Rogo-Gupta L, Eilber K, Anger JT, et al. Supracervical hysterectomy is protective against mesh complications after minimally invasive abdominal sacrocolpopexy: a population-based cohort study of 12,189 patients. J Urol. (2022) 207(3):669–76. doi: 10.1097/JU.000000000000226234694142
30. Costantini E, Brubaker L, Cervigni M, Matthews CA, O'Reilly BA, Rizk D, et al. Sacrocolpopexy for pelvic organ prolapse: evidence-based review and recommendations. Eur J Obstet Gynecol Reprod Biol. (2016) 205:60–5. doi: 10.1016/j.ejogrb.2016.07.50327566224
31. Morciano A, Ercoli A, Caliandro D, Campagna G, Panico G, Giaquinto A, et al. Laparoscopic posterior vaginal plication plus sacral colpopexy for severe posterior vaginal prolapse: a randomized clinical trial. Neurourol Urodyn. (2023) 42(1):98–105. doi: 10.1002/nau.2505236135387
32. Larouche M, Belzile E, Geoffrion R. Surgical management of symptomatic apical pelvic organ prolapse: a systematic review and meta-analysis. Obstet Gynecol. (2021) 137(6):1061–73. doi: 10.1097/AOG.000000000000439333957652
33. van IJsselmuiden MN, van Oudheusden A, Veen J, van de Pol G, Vollebregt A, Radder CM, et al. Hysteropexy in the treatment of uterine prolapse stage 2 or higher: laparoscopic sacrohysteropexy versus sacrospinous hysteropexy-a multicentre randomised controlled trial (LAVA trial). BJOG. (2020) 127(10):1284–93. doi: 10.1111/1471-0528.1624232267624
34. Christmann-Schmid C, Koerting I, Ruess E, Faehnle I, Krebs J. Functional outcome after laparoscopic nerve-sparing sacrocolpopexy: a prospective cohort study. Acta Obstet Gynecol Scand. (2018) 97(6):744–50. doi: 10.1111/aogs.1333729495121
35. Nygaard IE, McCreery R, Brubaker L, Connolly A, Cundiff G, Weber AM, et al. Abdominal sacrocolpopexy: a comprehensive review. Obstet Gynecol. (2004) 104(4):805–23. doi: 10.1097/01.AOG.0000139514.90897.0715458906
36. Restaino S, Ronsini C, Finelli A, Santarelli A, Scambia G, Fanfani F. Laparoscopic approach for shull repair of pelvic floor defects. J Minim Invasive Gynecol. (2018) 25(6):954. doi: 10.1016/j.jmig.2017.12.01629289624
37. Scollo P, Pecorino B, Ferrara M, Mereu L. Uterosacral ligament suspension sec shull by vaginal natural transluminal endoscopic surgery (vNOTES). J Obstet Gynaecol Can. (2022) 44(6):703. doi: 10.1016/j.jogc.2022.02.12635276427
38. Spelzini F, Frigerio M, Manodoro S, Interdonato ML, Cesana MC, Verri D, et al. Modified McCall culdoplasty versus shull suspension in pelvic prolapse primary repair: a retrospective study. Int Urogynecol J. (2017) 28(1):65–71. doi: 10.1007/s00192-016-3016-627048368
Keywords: pelvic organ prolapse, sacrocolpopexy, pectopexy, mersilene, mesh, uterine suspension
Citation: Devassy R, Naem A, Krentel H and De Wilde RL (2023) Modified Oxford technique of colpopexy for the treatment of uterine and vaginal vault prolapse: a retrospective pilot cohort study. Front. Surg. 10:1222950. doi: 10.3389/fsurg.2023.1222950
Received: 15 May 2023; Accepted: 21 June 2023;
Published: 30 June 2023.
Edited by:
Stefano Cianci, University of Messina, ItalyReviewed by:
Carlo Ronsini, Università degli Studi della Campania "Luigi Vanvitelli", ItalyGiovanni Buzzaccarini, Vita-Salute San Raffaele University, Italy
Alin Constantin, Albertinen Hospital Hamburg, Germany
© 2023 Devassy, Naem, Krentel and De Wilde. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Antoine Naem YW50b2luZS5uYWVtQGdtYWlsLmNvbQ==
Abbreviations POP, Pelvic Organ Prolapse; FDA, Food and Drug Administration; POP-Q, Pelvic Organ Prolapse Quantification.
 Rajesh Devassy1
Rajesh Devassy1 Antoine Naem
Antoine Naem Harald Krentel
Harald Krentel