- 1Department of Plastic Surgery, Jinling Hospital, Nanjing Medical University, Nanjing, China
- 2Department of Plastic Surgery, Jinling Hospital, Southern Medical University, Nanjing, China
Background: Intramuscular venous malformations (IMVMs) can cause pain and contracture deformity, leading to dysfunction of limbs. Ethanol sclerotherapy is one of the main treatments for IMVMs. This study aims to evaluate the efficacy and the complications associated with intravascular ethanol sclerotherapy for IMVMs and to provide a comprehensive summary of clinical experiences for future reference.
Methods: A retrospective analysis was conducted on a cohort of 118 patients diagnosed with IMVMs who were treated with ethanol sclerotherapy in our center between 2006 and 2021. The plastic surgeons utilized a standardized collection pro forma to record the clinical data. Furthermore, a follow-up period ranging from 6 months to 5 years was implemented to assess the relief of symptoms, the change of lesion size, and the recovery of functional outcomes. In addition, an analysis of long-term complications was conducted.
Results: The clinical symptoms of the patients in this group included pain, swelling, and limited movement. On average, 5.61 mL (range 2–14 mL) of ethanol was used during the sclerotherapy procedure. The intraoperative and early postoperative complications were successfully relieved by means of timely intervention, as observed during the follow-up period. Based on the MRI results, the sizes of the lesions in 19% of the cases were significantly decreased, while a slight decrease was observed in 39% of the cases. During the follow-up period, it was found that only eight out of the 118 patients included in this study experienced long-term complications related to sclerotherapy.
Conclusions: Although ethanol sclerotherapy has proven to be an effective first-line treatment for IMVMs, it is associated with a variety of adverse reactions and short- and long-term complications. Surgeons are required to perform operations prudently and provide timely medical intervention for postoperative complications.
Introduction
As the most common congenital vascular anomalies, venous malformations (VMs) could occur in many tissues or organs, including the skin and muscles, with approximately 40% of cases occurring in skeletal muscles. At birth, patients with intramuscular venous malformations (IMVMs) typically exhibit few symptoms and indications. As the patients grow, or encounter trauma, puberty, pregnancy, or other factors, the lesion can progressively enlarge, resulting in worsening of symptoms, such as pain, swelling, and even motor limitation. Therefore, timely treatment is needed for IMVM patients to alleviate the symptoms and control the size of the lesions. At present, there are various therapies for the management of IMVMs, including conservative treatment, sclerotherapy, operations, laser treatment, and cryoablation, among which sclerotherapy is the most commonly used. There are also many kinds of sclerosants available. Ethanol is the most widely used sclerosant in our center due to its high efficacy and potent destructive properties. Meanwhile, some scholars expressed that future studies should be directed toward investigating the anatomic location and the depth of the malformations. Unfortunately, there is a lack of systematic research pertaining to the utilization of ethanol sclerotherapy for IMVM. In this study, a retrospective analysis was conducted to evaluate the therapeutic effectiveness and complications associated with ethanol sclerotherapy in IMVMs.
Methods
Study design and patients
This study was reviewed and approved by the Medical Ethics Committee of Jinling Hospital. The study complies with the Declaration of Helsinki. Informed consent for the treatment and the publication of images was obtained from all the patients. The participants included in this study were individuals diagnosed with IMVMs who were treated with ethanol sclerotherapy in our center between January 2006 and December 2021. The sample consisted of 77 female and 41 male patients, aged 4–59 years with an average age of 23.17.
The inclusion criteria are as follows: (1) patients diagnosed with IMVM by MRI; (2) patients with signs or symptoms; (3) patients who had undergone ethanol sclerotherapy; and (4) patients with pre- and post-treatment data, followed up for more than 6 months. The exclusion criteria are as follows: (1) digital subtraction angiography or MRI revealing arteriovenous malformations, capillary malformations, lymphatic malformations, or combined vascular malformations; (2) patients who received foam sclerotherapy, intralesional copper wire retention or surgical resection and other treatments; and (3) patients with incomplete clinical data.
Treatment
Following admission, all patients underwent routine examination to exclude surgery contraindications. General intravenous anesthesia or local infiltration anesthesia was administered according to the pain tolerance of the patients. Prior to the sclerotherapy procedure, all patients were administered 0.3 mg/kg of methylprednisolone intravenously to reduce the risk of complications such as cough and chest tightness. Based on the findings of the preoperative MRI and further imaging examinations, the lesion’s precise location was identified and subsequently accessed through percutaneous puncture using a 22-gauge scalp needle attached to a 10-mL syringe. The accuracy of needle positioning in the venous pouch was ascertained based on the venous blood reflux without obvious arterial pulsation through the needle. Some small lesions were punctured under ultrasound assistance. The treatment consisted of multifocal and repeated injections. The total amount of ethanol used in each treatment did not exceed 0.2 mL/kg. Throughout the injection process, vital signs and blood supply to the skin around the injection point were closely monitored. The treatment procedure was repeated after 2–3 months. Following the third treatment, an MRI scan was requested to evaluate the therapeutic effectiveness of the intervention and inform the determination of the subsequent treatment plan.
Outcome assessment and follow-up
The patients in this group were followed up for a period of 6 months to 5 years, with an average of 41 months. We followed up with patients at the outpatient clinic. Those who could not be followed up through personal visits at the clinic were evaluated by a validated phone questionnaire. The details of the follow-up included the therapeutic effects of absolute ethanol sclerotherapy on relieving clinical symptoms such as pain and swelling. To assess the outcome in a more scientific and objective manner, the degree of symptom relief was divided into three categories: improvement, no change, and deterioration.
At admission, all the patients underwent an MRI examination. For patients with several treatments, an MRI examination was performed after three consecutive treatment sessions. The patients who received fewer than three treatment sessions would be scheduled for an MRI examination prior to their last follow-up. The changes in the size of the lesion were evaluated by measuring the maximum diameter observed using MRI before and after treatment with the following categorization: (1) no significant changes if less than 10%; (2) moderate reduction between 10% and 50%; and (3) marked reduction if higher than 50%.
Complication analysis
After a sclerotherapy treatment, vital signs and blood supply to the skin around the injection point were closely monitored, and complications were recorded, such as blood supply disorder, ulceration, infection, nerve injury, superficial vein thrombosis, muscle contracture, and joint deformity.
Complications were categorized based on the timing of their occurrence: (1) intraoperative complications: complications that occurred immediately during the operation, including cough, chest tightness, and allergic reactions; (2) early postoperative complications: occurring within 1 month after sclerotherapy but could be cured by conservative treatment, including ulceration, infection, superficial vein embolization, and hematuria; (3) late postoperative complications: occurring beyond 1 month after sclerotherapy, including muscle contracture, joint deformity, and peripheral nerve injury.
Statistical analysis
Statistical analysis was performed using IBM's SPSS Statistics 25.0 for Windows. The measurement data conforming to the normal distribution were expressed as mean ± standard deviation (X ± SD), and a t-test was performed for comparisons between the two groups. Fisher's exact test was used for categorical data. Multiple groups were compared using the Kruskal–Wallis rank-sum test. A P-value < 0.05 was considered to indicate a statistically significant difference.
Results
Patient characteristics
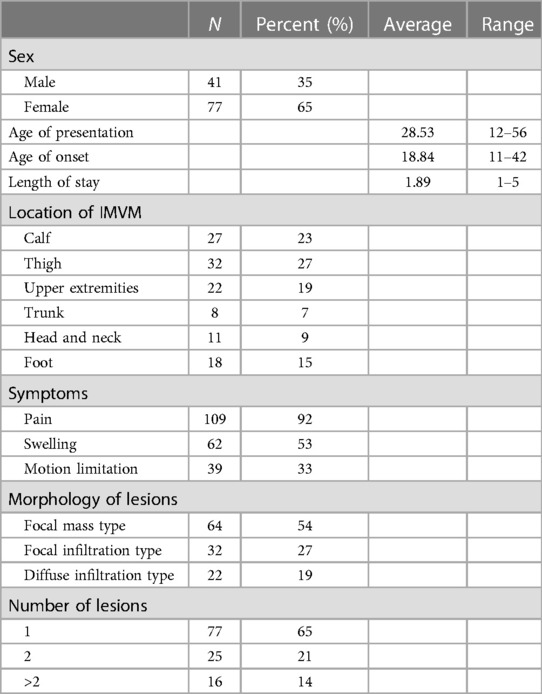
A total of 118 patients with IMVM were enrolled in this study. IMVM lesions can be located all over the body, such as in the lower leg (n = 27), thigh (n = 32), upper limb (n = 22), trunk (n = 8), face (n = 11), and foot (n = 18). Meanwhile, 90 patients experienced pain, with 19 patients exhibiting symptoms of persistent pain, 39 patients reporting limited movement, and 62 patients presenting with swelling. The relevant demographic data, lesion location, symptoms, and imaging findings are shown in Table 1.
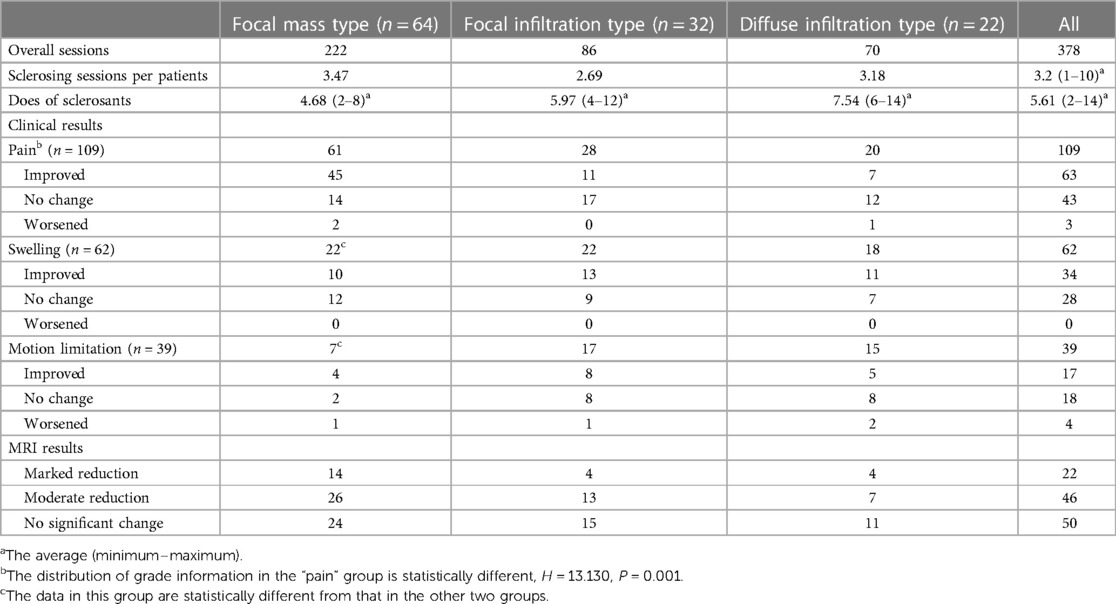
All patients were routinely examined using MRI at the first admission to evaluate the range and location of the lesions. Based on the imaging findings, IMVM was categorized into three types: (1) Focal mass type (n = 64): the lesions were localized with well-defined margins. (2) Focal infiltration type (n = 32): the lesions were diffused in one muscle. (3) Diffuse infiltration type (n = 22): the lesions were extensive in more than one muscle with margins ill-defined.
There were no statistically significant differences observed in the levels of pain experienced by patients in each group. However, there was a statistically significant difference in swellings of patients not only between focal mass type and focal infiltration type (P = 0.001) but also between focal mass type and diffuse infiltration type (P ≈ 0.000), while there was no statistically significant difference observed between focal infiltration type and diffuse infiltration type (P > 0.05). The difference in motion limitation was statistically significant between not only focal mass type and focal infiltration type (P ≈ 0.000) but also focal mass type diffuse infiltration type (P = 0.000). Still, there was no statistically significant difference between focal infiltration type and diffuse infiltration type (P > 0.05).
Sclerotherapy treatment
The cohort of 118 patients underwent a total of 378 treatment sessions (1–10 times per patient), with an average of 3.20 sessions per patient. In each session, 2–16 mL of absolute ethanol was injected, with an average of 5.61 mL and a maximum dosage of 0.2 mL/kg per patient.
Outcome assessment and follow-up
The follow-up data of 118 patients are shown in Table 2. Among the 118 patients, 109 experienced pain, of which 63 (58%) cases had improved after ethanol sclerotherapy. A total of 62 patients were complicated with swelling, of which 34 (55%) cases had improved. A total of 39 patients experienced motion limitation, of which 17 (44%) cases had improved. Among them, there was a statistically significant difference in the improvement of pain among the three groups (H = 13.130, P = 0.001). In addition, there was a statistically significant difference in the swelling of patients not only between focal mass type and focal infiltration type (P = 0.015) but also between focal mass type and diffuse infiltration type (P = 0.009). Under MRI examinations, the lesions of 22 patients (19%) showed a remarkable reduction in size, as the typical cases shown in Figures 1–3. The lesions of 46 patients (39%) showed a moderate reduction in size, while that of 50 patients (42%) showed no significant change.
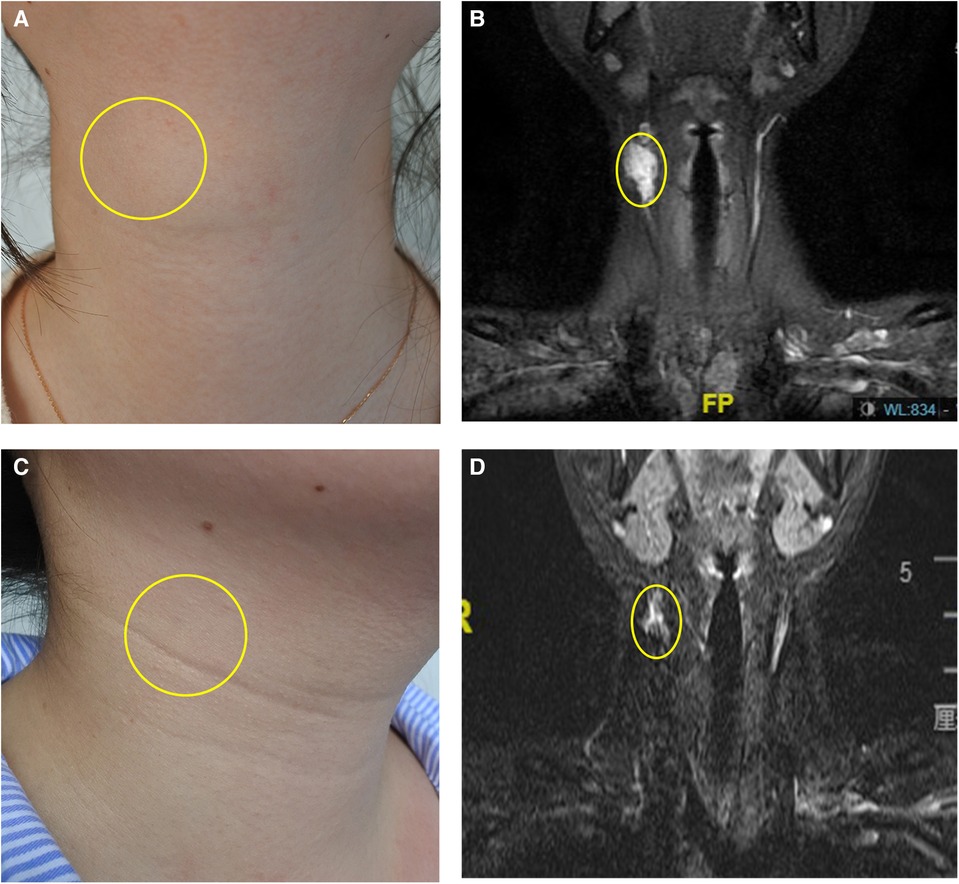
Figure 1. Focal mass type IMVM in the right neck. (A) The appearance before treatment. (B) The MRI before treatment. (C) The appearance after two times of treatment. (D) The MRI after treatment. The yellow ellipse indicated the lesion. The copyrights of the figure were held by corresponding author.
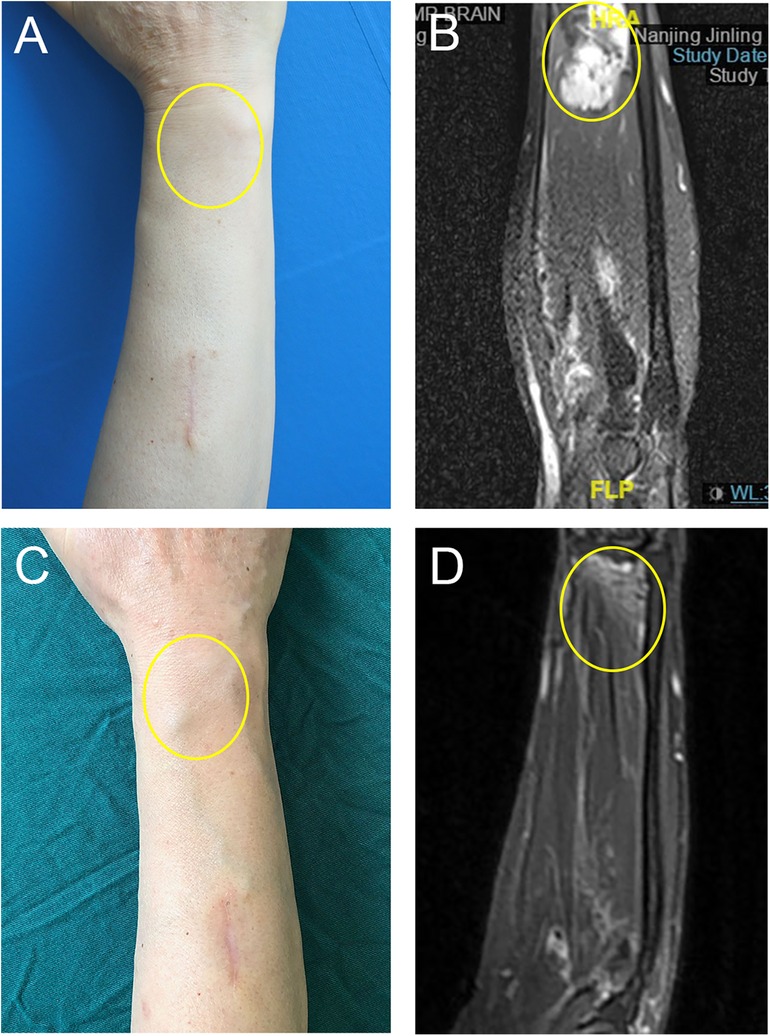
Figure 2. Focal mass type IMVM in the right upper extremity. (A) The appearance before treatment. (B) The MRI before treatment. (C) The appearance after three times of treatment. (D) The MRI after treatment. The yellow ellipse indicated the lesion. The copyrights of the figures were held by corresponding author.
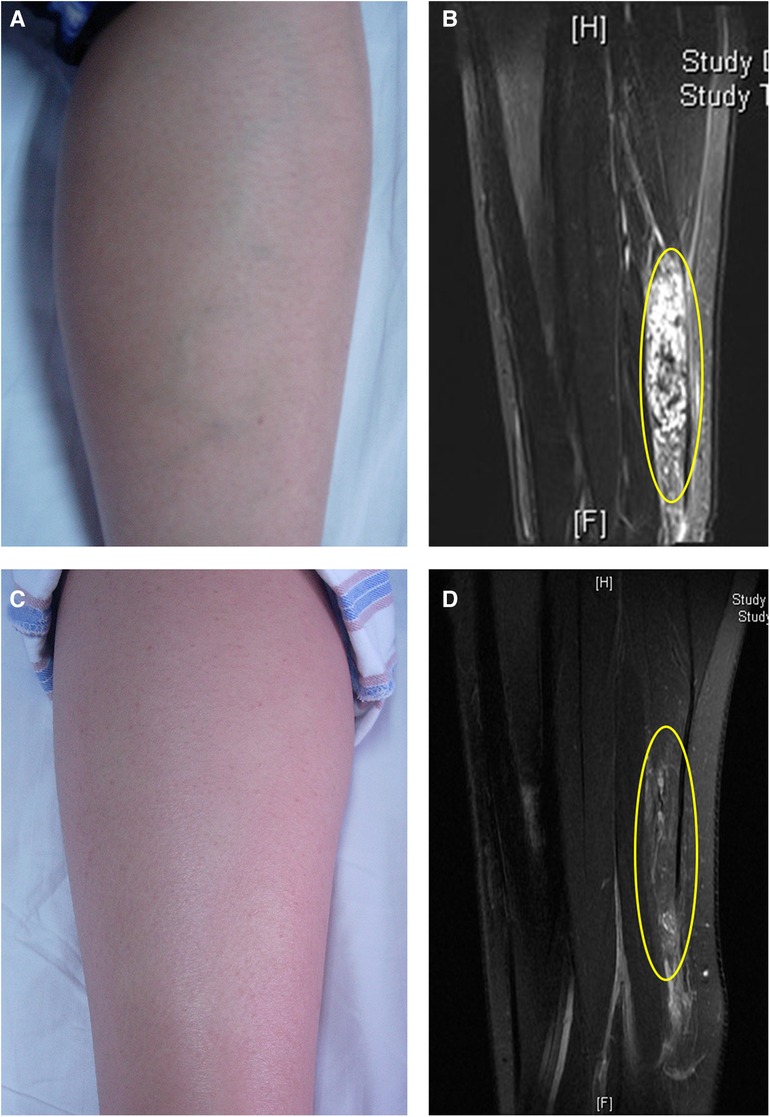
Figure 3. Focal mass type IMVM in the left calf. (A) The appearance before treatment. (B) The MRI before treatment. The yellow ellipse indicated that the lesion was located in the gastrocnemius muscle. (C) The appearance after three times of treatment. (D) The MRI after treatment. The yellow ellipse indicated the lesion. The copyrights of the figures were held by corresponding author.
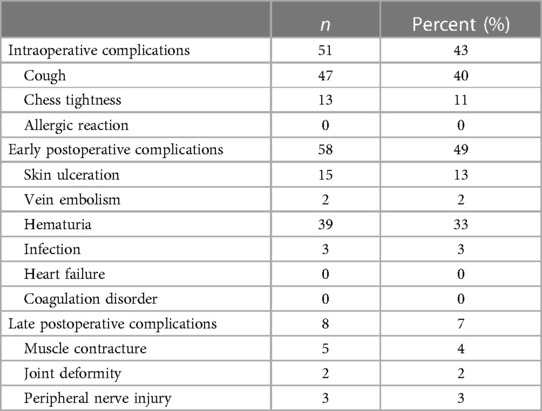
Complication analysis
The incidence of complications related to sclerotherapy is shown in Table 3, including the following: (1) intraoperative complications: cough (47/118) and chest tightness (13/118); (2) early postoperative complications: skin ulceration (15/118), superficial vein embolization (2/118), hematuria (39/118), and infection (3/118); and (3) late postoperative complications: muscle contracture (5/118), joint deformity (2/118), and peripheral nerve injury (3/118). The above complications were relieved after symptomatic treatment. Life-threatening complications such as hemolysis, heart failure, pulmonary embolism, and allergic reactions were not observed.
Discussion
IMVM is a congenital chronic refractory disease, and the lesions are mostly located in the muscles of limbs, showing progressive growth (1). Most patients experienced varying degrees of pain, swelling, or motion limitation. More critically, the presence of limb contracture deformity can significantly decline the patients’ quality of life. Although VM is a benign lesion, it has the characteristics of destructibility and invasiveness, leading to the lack of muscle coherence, reduced muscle contractility, and potential bone deformities.
Currently, the treatment of IMVM is controversial. Some scholars believe that surgical resection should be the primary therapy for focal mass type, by which the deformed venous lesions can be completely removed (2). However, due to IMVMs invasive nature and deep location within the muscles, it is challenging to entirely eliminate the lesions with surgical intervention. In addition, it may lead to serious postoperative complications such as bleeding and muscle and nerve injury. Sclerotherapy is the most commonly used treatment for IMVM. This treatment involves injecting sclerosing agents or chemicals into the malformed veins, contacting with the vascular endothelium, which will result in aseptic inflammation, thrombosis, and fibrosis (3). Compared with surgical resection, sclerotherapy alleviates the burden and shortens hospital stay. Therefore, sclerotherapy should be preferred for IMVM patients with focal or diffuse lesions.
A wide variety of sclerosants are available, such as absolute ethanol, monoethanolamine oleate, bleomycin, sodium tetradecyl sulfate (STS), and polidocanol (4). According to the form, they can be also classified into liquid sclerosants and foam sclerosants. Ethanol is considered to be the most effective and destructive liquid sclerosant for treating lesions (5). In contrast, foam sclerosants such as STS and polidocanol are less destructive for tissues and thus needs more treatment sessions. In this study, all the subjects were treated using ethanol. Out of all the patients studied, 109 patients experienced pain, of which 63 (58%) patients demonstrated improvement; 62 patients experienced swelling, of which 34 (55%) patients had improved; and 39 patients had combined limitation of motion, of which 17 (44%) patients had improved.
With regard to complications following ethanol sclerotherapy, some researchers have confirmed that 0.25 mL/kg of ethanol is considered to be the critical threshold that may cause adverse reactions (6). In addition, the locations of IMVM lesions are relatively deep, hence reducing the likelihood of skin necrosis following ethanol sclerotherapy (7). The injection dose was controlled to less than 0.2 mL/kg. Patients were required for follow-up visits every 3 months, and the subsequent treatments were mainly based on symptom improvement or imaging results. The appropriate dose of ethanol for each injection and the multiple injections at an interval of 3 months can effectively reduce the occurrence of complications and achieve optimal efficacy step by step. The common complications of ethanol sclerotherapy include intraoperative complaints of chest tightness and dyspnea. However, administering glucocorticoids prior to treatment can effectively relieve these symptoms (8). The complications were categorized based on the timing of their occurrence into three groups: intraoperative complications, early postoperative complications, and late postoperative complications. In our study, intraoperative complications occurred in 51 patients, including 47 cases of cough and 13 cases of chest tightness, of which nine patients experienced both cough and chest tightness. No allergic reactions were observed. The above patients probably developed microthrombi in the blood vessels during ethanol sclerotherapy, which refluxed into the pulmonary capillaries and triggered choking. However, it was relieved by preoperative administration of hydrogenated prednisone and a brief period of intraoperative rest.
Petechiae and local skin necrosis observed in 15 patients were among the early postoperative complications in this study, of which 13 patients recovered completely after symptomatic treatment manifesting as improved microcirculation and enhanced venous return after regular dressing changes. Only two patients required a second operation, specifically skin grafting, to repair the secondary wound. The occurrence of localized skin petechiae and necrosis were caused by the destructive effects of ethanol on both the lesion and the return veins of the skin and subcutaneous tissue when destroying the deformity, which is a special phenomenon of sclerotherapy of IMVM. Among the two patients with venous embolism, one case was superficial vein embolism, which showed local skin petechiae and necrosis and was cured after regular dressing changes, as shown in Figure 4. The other case was a deep femoral vein embolism, characterized by swelling in the affected lower limb, the course of this condition lasted for more than 1 month, and the symptom gradually improved after anticoagulation treatment and wearing elastic stockings. Meanwhile, we observed that 39 patients had transient hematuria, all of which were hemoglobinuria. Some scholars believe that transient hematuria occurs after ethanol sclerotherapy due to the physiological reaction of the chemical nature of ethanol in the organism (9). We have not observed severe hemolytic gross hematuria requiring intravenous application of binding bead protein. As far as coagulation is concerned, our previous studies have found elevated fibrinogen degradation product and D–D in patients with ethanol sclerotherapy, and this elevation was often associated with a good therapeutic outcome; however, no serious disorders of coagulation were found (10).
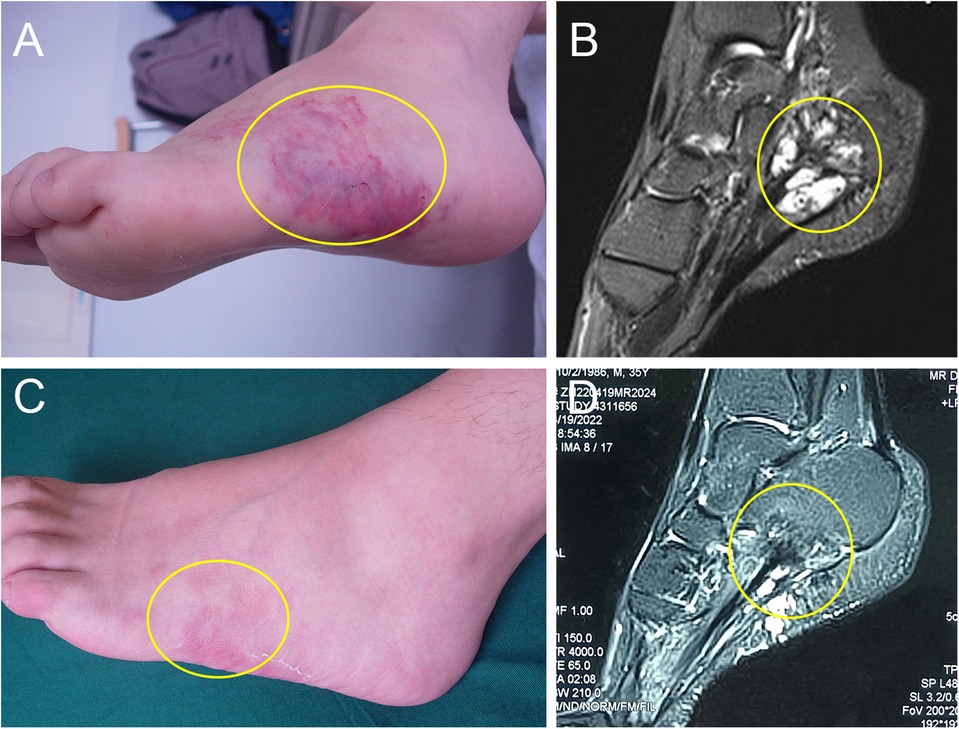
Figure 4. Diffuse infiltrative type IMVM in the left foot. (A) The immediate postoperative appearance. The local skin showed extensively damaged. (B) The MRI before treatment, which indicated that the lesions were located in the plantaris muscle. (C) The appearance after 4 weeks of treatment. The local skin was intact with no scarring. (D) The MRI after three times of treatment. The yellow ellipse indicated the lesion. The copyrights of the figures were held by corresponding author.
Among the late postoperative complications, a total of eight patients were observed, and five of them experienced muscle contracture, which was relieved in three patients after regular stretching of the contracted muscles and the corresponding rehabilitation treatment. However, two patients refused to receive further treatment, resulting in a deformity of the corresponding joint. Muscle contracture occurs due to muscle fibrosis during ethanol sclerotherapy in IMVM, so patients should be treated at the early stage of contracture to prevent further fibrosis and joint deformity. If the muscle contracture is severe and the conservative treatment fails, surgical intervention may be considered as a viable option, including excision of the diseased muscle or a Z-lengthening of the Achilles tendon, the Hoke technique, and the Taylor Spatial Frame external fixation (11). Furthermore, three patients with peripheral nerve injury showed numbness in the innervated area. They were treated with neurotrophic therapy and completely recovered after 4–6 months.
To minimize the incidence rate of complications caused by ethanol sclerotherapy, surgeons should be extremely careful during the operation. Prior to the procedure, fully understanding the anatomy of the puncture site is necessary to avoid unwanted damage to the arteries and important nerves. During the procedure, confirming the puncture site could avoid leakage of sclerosant. If the lesion is too small to confirm the puncture in place, fluoroscopy or ultrasound could assist. After the procedures, it is essential to closely monitor the vital signs of the patient and conduct regular follow-ups for early detection and early intervention of postoperative complications. Meanwhile, in order to avoid damaging normal veins and ensure the accurate injection of anhydrous ethanol, it is necessary to perform fluoroscopy or ultrasound procedures due to the highly destructive nature of anhydrous ethanol. Particularly for VMs in the facial or cervical part and deep tissue, operation under the premise of visualization has been found to improve the accuracy of sclerotherapy and perhaps reduce the occurrence of complications to a certain extent, which could improve the efficacy of sclerotherapy.
To improve the effectiveness of ethanol sclerotherapy and reduce complications, researchers have developed ethanol gels. Because ethanol gel has a higher viscosity than liquid ethanol, it remains in the blood vessels for a longer period after injection into the vessels, resulting in a longer contact time with the lesion and a stronger effect on the local vessel wall. Thus, the ethanol dose and the occurrence of complications could be reduced, and the quality of life of the patients may be improved (12, 13). However, there are few clinical studies related to the use of ethanol gel, and additional research is required to confirm its effectiveness for clinical application in treating IMVM. Furthermore, some scholars reported simultaneous application of physical and chemical treatment could effectively destroy the endothelium of malformed veins (14, 15). In some huge and extensive infiltrative types of IMVMs, safe doses of sclerosants are often not enough for a good curative effect. Scholars tried to employ intravascular laser therapy for IMVM patients, in which the laser beams destroyed the lesion and the residual lesion was then treated with sclerotherapy. This kind of combined treatment also reduces the dose of sclerosants, thus decreasing the risks of complications or side effects.
Conclusion
Within safe doses, ethanol sclerotherapy effectively shrinks lesions, reduces pain, relieves motion limitation, and improves appearance, with minimal occurrence of severe complications. Overall, ethanol sclerotherapy for IMVM is safe and effective and could be the preferred treatment for IMVMs. However, it is crucial for surgeons to perform operations prudently and provide timely treatment for postoperative complications due to the potential occurrence of multiple short- or long-term complications.
Data availability statement
The raw data supporting the conclusions of this article will be made available by the authors, without undue reservation.
Ethics statement
The studies involving humans were approved by the Medical Ethics Committee of Jinling Hospital. The studies were conducted in accordance with the local legislation and institutional requirements. Written informed consent for participation in this study was provided by the participants’ legal guardians/next of kin. Written informed consent was obtained from the individual(s) for the publication of any potentially identifiable images or data included in this article.
Author contributions
C-JJ: Conceptualization, Investigation, and Writing – original draft. QW: Conceptualization, Data curation, and Writing – review and editing. MW: Formal analysis, Project administration, and Writing – review and editing. YC: Formal analysis, Project administration, and Writing – review and editing. S-MY: Conceptualization, Data curation, Methodology, Supervision, Writing – review and editing.
Funding
The authors declare financial support was received for the research, authorship, and/or publication of this article.
This study was supported by the National Natural Science Foundation of China (No. 81272989, awarded to S-MY) and the “333 Project” of Jiangsu Province, China (No. BRA2020416, awarded to S-MY).
Acknowledgments
The authors thank the participating patients and their families.
Conflict of interest
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
Publisher's note
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
References
1. Wieck MM, Nowicki D, Schall KA, Zeinati C, Howell LK, Anselmo DM. Management of pediatric intramuscular venous malformations. J Pediatr Surg. (2017) 52(4):598–601. doi: 10.1016/j.jpedsurg.2016.08.019
2. Kim YH, Ryu JY, Lee JS, Lee SJ, Lee JM, Lee SY, et al. The effects of surgical treatment and sclerotherapy for intramuscular venous malformations: a comparative clinical study. Arch Plast Surg. (2021) 48(6):622–9. doi: 10.5999/aps.2021.00913
3. Dasgupta R, Patel M. Venous malformations. Semin Pediatr Surg. (2014) 23(4):198–202. doi: 10.1053/j.sempedsurg.2014.06.019
4. Sun LM, Ni XD, Yuan SM. The efficacy of absolute ethanol and polidocanol in the treatment of venous malformations. J Craniofac Surg. (2020) 31(3):e272–5. doi: 10.1097/SCS.0000000000006268
5. Steiner F, FitzJohn T, Tan ST. Ethanol sclerotherapy for venous malformation. ANZ J Surg. (2016) 86(10):790–5. doi: 10.1111/ans.12833
6. Bisdorff A, Mazighi M, Saint-Maurice JP, Chapot R, Lukaszewicz AC, Houdart E. Ethanol threshold doses for systemic complications during sclerotherapy of superficial venous malformations: a retrospective study. Neuroradiology. (2011) 53(11):891–4. doi: 10.1007/s00234-010-0803-5
7. Ali S, Mitchell SE. Outcomes of venous malformation sclerotherapy: a review of study methodology and long-term results. Semin Intervent Radiol. (2017) 34(3):288–93. doi: 10.1055/s-0037-1604300
8. Burrows PE, Mason KP. Percutaneous treatment of low flow vascular malformations. J Vasc Interv Radiol. (2004) 15(5):431–45. doi: 10.1097/01.RVI.0000124949.24134.CF
9. Kaji N, Kurita M, Ozaki M, Takushima A, Harii K, Narushima M, et al. Experience of sclerotherapy and embolosclerotherapy using ethanolamine oleate for vascular malformations of the head and neck. Scand J Plast Reconstr Surg Hand Surg. (2009) 43(3):126–36. doi: 10.1080/02844310902840296
10. Yu MW, Han YY, Wang Q, Wang M, Chen Y, Yuan SM. Treatment outcomes and effects of ethanol sclerotherapy on systemic coagulation profile of patients with venous malformation. Ann Vasc Surg. (2022) 85:268–75. doi: 10.1016/j.avsg.2022.03.022
11. Hu L, Chen H, Yang X, Sun Y, Liu H, Gu H, et al. Operative management of equinus associated with lower limb venous malformations. Phlebology. (2022) 37(2):125–33. doi: 10.1177/02683555211047286
12. Teusch VI, Wohlgemuth WA, Hammer S, Piehler AP, Müller-Wille R, Goessmann H, et al. Ethanol-gel sclerotherapy of venous malformations: effectiveness and safety. AJR Am J Roentgenol. (2017) 209(6):1390–5. doi: 10.2214/AJR.16.17603
13. Ierardi AM, Colletti G, Biondetti P, Dessy M, Carrafiello G. Percutaneous sclerotherapy with gelified ethanol of low-flow vascular malformations of the head and neck region: preliminary results. Diagn Interv Radiol. (2019) 25(6):459–64. doi: 10.5152/dir.2019.18542
14. Kang M, Connor DE, Parsi K. Treatment of venous malformations with tumescent-assisted sclero-embolic and ablative lasers (SEALs): safe and effective long-term outcomes. Phlebology. (2022) 37(5):367–80. doi: 10.1177/02683555221080045
Keywords: intramuscular venous malformations, ethanol, sclerotherapy, safety, efficacy
Citation: Jin C-J, Wang Q, Wang M, Chen Y and Yuan S-M (2023) Therapeutic evaluation and analysis of complications of ethanol sclerotherapy for intramuscular vascular malformations: a single-center retrospective study. Front. Surg. 10:1274313. doi: 10.3389/fsurg.2023.1274313
Received: 8 August 2023; Accepted: 19 September 2023;
Published: 24 October 2023.
Edited by:
Hirotaka Suga, Teikyo University Mizonokuchi Hospital, JapanReviewed by:
Mine Ozaki, Kyorin University Hospital, JapanWeimin Shen, Nanjing Children’s Hospital, China
© 2023 Jin, Wang, Wang, Chen and Yuan. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Si-Ming Yuan eXVhbnNtQDE2My5jb20=
†These authors have contributed equally to this work
 Cai-Jun Jin
Cai-Jun Jin Qian Wang
Qian Wang Min Wang
Min Wang Yong Chen
Yong Chen Si-Ming Yuan
Si-Ming Yuan