- 1Eliot-Pearson Department of Child Study and Human Development, Tufts University, Boston, MA, United States
- 2Recovery Research Institute, Center for Addiction Medicine, Massachusetts General Hospital and Harvard Medical School, Boston, MA, United States
- 3Department of Human and Organizational Development, Vanderbilt University, Nashville, TN, United States
Introduction: Adolescent development and substance use disorder recovery unfold within diverse contexts, where recovery capital is key to planning. This study examined the relationship between social and personal recovery capital, community recovery capital, and cannabis and alcohol use among adolescents.
Methods: In this cross–sectional study, 416 students from 20 U.S. recovery high schools reported their past 90–day alcohol and cannabis use and completed the Assessment of Recovery Capital (adapted for youth readability). Student data were merged with data from the Recovery Ecosystem Index, which measures county–level recovery ecosystem, using each high school's county as a proxy for residence. Zero–inflated Poisson regression models estimated the odds of abstinence and substance use days, with recovery capital and recovery ecosystem index as predictors, while accounting for age, race, gender, and duration of enrollment (≥90 days).
Results: There were 378 (91%) and 360 (87%) students who provided alcohol and cannabis use data and were subsequently included in each model, respectively. Students, 47% female and 60% White person/persons/people, reported alcohol (M = 2.0; SD = 8.1) and cannabis (M = 6.0; SD = 18.0) use days, with most reporting zero days of use (284 and 266). The results indicated that the recovery capital score was positively associated with alcohol abstinence [adjusted odds ratio (aOR) = 1.03; 95% confidence interval (CI) = 1.01–1.06; P = 0.02] and cannabis abstinence (aOR = 1.03; 95% 1.01–1.06; P = 0.01). As recovery capital increased, adolescents reported fewer alcohol use days [incidence rate ratio (IRR) = 0.93, 95% CI = 0.93–0.94; P < 0.001] and fewer cannabis use days (IRR = 0.95; 95% CI = 0.95–0.96, P < 0.001). The recovery ecosystem index was not associated with alcohol or cannabis abstinence, but days of alcohol use (IRR = 1.12; 95% CI = 1.04–1.22, P = 0.01) and cannabis use (IRR = 1.10; 95% CI = 1.05–1.15; P < 0.001) increased as the index increased.
Discussion: Findings suggest that greater recovery capital is linked to greater alcohol and cannabis abstinence among recovery high school students. Unexpected was that a higher recovery ecosystem index score was associated with more substance use days. Youth–focused recovery supports could benefit from examining how changes in individual recovery capital influence service usage and how service usage, in turn, impacts recovery capital. There is also the need for a youth–tailored recovery ecosystem measure which focuses on factors unique to their developmental phase.
1 Introduction
Adolescence is a developmental period characterized by several unique milestones, including the onset of puberty, transitions in educational settings, increasing influence from peers, initial engagement in the workforce, and the process of individuation from the family. These milestones collectively contribute to the formation of a young person's identity and their growing autonomy (1–3). Yet, the transition and milestones do not happen in isolation nor are they uniform across individuals or contexts. Adolescent development is greatly impacted by their social relationships (i.e., peers and caregivers), community, and cultural norms (4, 5). Many health decisions and behaviors during these years influence health and health behaviors well into adulthood (5).
Amid the significant developmental changes of adolescence, the opportunity and interest in alcohol and other drug (AOD) use often emerge (6). For many adolescents, AOD use is perceived to serve positive functions (2, 7). It may be employed as a coping mechanism to manage stress, as a means of distancing oneself from parental influence while fostering connections with peers, or as a way to experiment, seek novel sensations, and explore emerging self-concepts (2, 7).
Alcohol is the most commonly used substance among adolescents globally (8, 9), and its use can differ across age or grades, race/ethnicity, and gender. In 2023, 52% of US adolescents had consumed alcohol by the end of high school and 15% had done so by 8th grade (9). Cannabis is the second most used substance among adolescents, with 18% of US adolescents in 2023 reporting cannabis use in the last year (10). AOD use can pose a significant risk for healthy adolescent biological, emotional, and social development (3, 7, 11, 12). Moreover, most adolescents who use substances use two or more substances (i.e., polysubstance use), with significant health consequences (13). AOD use can quickly escalate from experimentation to patterns of use with significant long-term consequences, driven by disparities in population level social resources by individual, family, and community contexts (14). These consequences may include disrupted life transitions, academic difficulties, impaired judgment, future AOD disorders, and even injury or death (15). Additionally, the trajectories of adolescent AOD use, as well as the associated consequences, vary across different populations, locations, and cultures (14).
Despite the harm and consequences of youth AOD use, many people do recover. An estimated 9% of adults in the US have resolved an AOD problem, with half of them identifying as being in recovery (16). Youth with AOD problems also pursue recovery (1, 17). Although there are many pathways and definitions of recovery, the two consistent characteristics are a reduction or discontinuation of substance use and improvements in health and well-being (18, 19). An individual's recovery journey can be impacted by the resources they have access to, both within themselves and within their community. Conceptualizing and operationalizing an individual's available resources can aid in recovery care planning as well as recognize the larger ecosystem individuals are recovering in.
Recovery capital is one conceptualization of the available resources that can support recovery (20, 21). Recovery capital is an ecological model that addresses individual-level factors (i.e., personal or human recovery capital), inter-individual factors (i.e., social recovery capital), and the larger context (i.e., community or cultural recovery capital) (20). The concept has been operationalized in at least ten unique scales with over forty unique domains, all of which rely on self-report (22). Although recovery capital has been theorized to differ for adolescents in the Recovery Capital for Adolescent Model (23), there is not yet a validated adolescent-specific measure of recovery capital (1, 20, 22). Furthermore, there is a dearth of quantitative recovery research with adolescents, which limits our ability to know whether recovery capital is related to key outcomes such as substance use among this high-risk population.
Although recovery capital is an ecological conceptualization of recovery-related resources, recovery capital measurement is almost exclusively at the individual level and self-reported. The exclusion of objective measurement at the community and policy levels may limit the understanding of community recovery capital (24, 25). These community recovery capital factors may include recovery support services such as recovery housing, recovery community-organizations, mutual-aid societies (e.g., Alcoholics Anonymous, SMART Recovery), and specialty substance use treatment and policies like required insurance coverage of medications for opioid use disorder, Good Samaritan laws, and laws that support syringe service programs. One unique community-level support for adolescents is the recovery high school (RHS). RHSs are secondary schools designed to support students in recovery and meet state requirements for awarding a secondary school diploma (26). There are currently 43 schools in operation across the United States, with the Office of National Drug Control Policy recommending more be founded (27, 28). RHSs range in size from 2 to 115 students, vary in funding structure (e.g., public, private, charter), and exist as both independent schools and programs embedded within another school (29). In addition to traditional classes and coursework, which meets state standards, RHSs offer recovery-oriented services like group check-ins, one-on-one counseling or referrals to mental health resources, chances to participate in community volunteer work, and consistent communication with parents or guardians (29). Students attending a RHS following substance use treatment have reported reduced substance use and improved attendance compared to adolescents that returned to a traditional high school following treatment (17). Cost benefit analyses have also indicated these schools are beneficial to society in the short and long term (30).
One operationalization of community recovery capital that is not self-reported is the Recovery Ecosystem Index, through which a numeric score is assigned to a county and represents their recovery ecosystem strength. The Recovery Ecosystem Index Map is a publicly available tool that includes data collected through the Center for Disease Control, the US Census, and the Prescription Drug Abuse Policy System for each county in the United States (31). US counties with higher overdose mortality generally also have higher recovery ecosystems (32). One unique feature of the Index is that it is an objective measure of community recovery resources providing both an overall score as well as information about treatment and recovery supports (e.g., average distance to nearest medication treatment provider, number of self-help recovery meetings per 100,000 residents). While the Index is not adolescent-specific, as it includes items like adult drug courts and lacks a focus on adolescent treatment, it may offer a valuable snapshot of the general community recovery capital within a given area. However, adolescent and adult community recovery capital may need to be considered as distinct constructs.
There is a critical gap in research that comprehensively examines how individual and community resources are associated with substance use among adolescents in recovery. Without this knowledge, practitioners and policy makers lack the evidence to tailor recovery care planning, potentially missing opportunities to enhance well-being and recovery maintenance.
The present study examines the relationships among recovery capital, the recovery ecosystem, and cannabis and alcohol use among adolescents attending a RHS in the United States. We hypothesized that adolescents with higher recovery capital and higher recovery ecosystem scores would be less likely to engage in cannabis and alcohol use, and if engaging in it, do so less frequently.
2 Materials and methods
2.1 Study design and participants
This is a secondary data analysis of cross-sectional data collected through two sources: the Systematic Evaluation of the Association of Recovery Schools (SEARS) project and the Recovery Ecosystem Index Map (31). SEARS collects data on students' recovery experiences to support programming and enhance student success. The Association of Recovery Schools—the national association for RHSs in the United States—invites all member RHSs to participate in SEARS, which features a comprehensive tool measuring recovery capital and substance use. RHSs enroll students throughout the year and survey participation dates vary by school. Our analytic sample included all students and schools that had completed SEARS at the time of this study: 416 students attending 20 RHSs across the US were included. Data were collected between February 2022 and June 2023. Students must have been enrolled at a RHS at the time of the survey to participate. The county of each RHS is used as a proxy for each student's county of residence. Thus, each student is linked with a Recovery Ecosystem Index score.
2.2 Measures
Recovery capital is measured using the Assessment of Recovery Capital, which is one of the most commonly used scales of recovery capital (22, 33). The assessment is a 50-item measure providing a total summed score where higher values represent greater RC. Six items were modified for readability (Supplementary Table S1).
Participants reported their past 90-day alcohol and cannabis use as well as their gender (male, female, self-identify/other), age, race (American Indian or Alaska Native, Asian, Black or African American, Native Hawaiian or Other Pacific Islander, White, Other person/persons/people), ethnicity (Hispanic, non-Hispanic) and RHS enrollment date. Days of RHS enrollment was calculated by subtracting the number of days between enrollment date and day of survey completion (M = 191; SD = 390; Mdn = 133). The student's enrollment status for 90 days or more (Yes/No) was calculated as a proxy for the dose-effect of attending a RHS. Days of enrollment were converted into this binary variable to address non-normal variability while preserving all available data.
Respondents also completed the Global Appraisal of Individual Needs—Short Screener (GAIN-SS) (34), which is a brief screener for possible internalizing (e.g., depression, anxiety, bi-polar, schizophrenia), externalizing (e.g., attention deficits, hyperactivity, impulsivity, conduct problems), and substance use disorders. The GAIN-SS scores for each screener are summed and then categorized as low, moderate, or high-severity of problems and need for services. A result of moderate to high severity on any single screener is strongly associated with a disorder diagnosis via the DSM-IV and DSM-5 (34).
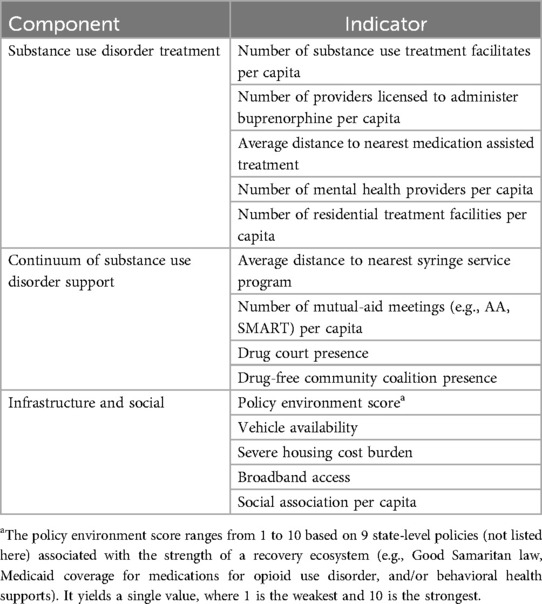
The Recovery Ecosystem Index (REI) is a numerical score reflecting the strength of a county's recovery ecosystem using the county of each RHS as a proxy for each student's county of residence. The REI was developed through a multistep process that entailed extensive literature reviews, and expert opinion (25, 35). A final set of 14 publicly available indicators at the county level were selected using a ranking system among a panel of experts. Each indicator was assigned to a class: substance use disorder treatment, continuum of substance use disorder support, or infrastructure and social (Table 1). The treatment and continuum of support classes included substance-specific indicators (e.g., number of substance use treatment facilities per capital, number of Narcotics Anonymous or SMART meetings per capita). The infrastructure and social class focused on related yet substance non-specific indicators (e.g., severe housing cost burden, social connections per capita). The overall REI score ranges from 1 (strongest) to 5 (weakest) and were calculated for each county. More information on the REI and its calculation are publicly available through the mapping tool, including the data sources for the included indicators (31).
2.3 Analysis
2.3.1 Data preparation
Due to the small sample, race was recategorized as Hispanic, Black non-Hispanic, White non-Hispanic, and Other non-Hispanic person/persons/people. The REI was reverse coded for analysis, so a higher REI score equated to a more robust community recovery capital score. The reverse coding of REI also aligned with the direction of the Assessment of Recovery Capital where higher scores indicate better participant outcomes. The intraclass correlations for alcohol and cannabis use across schools were non-trivial (ICC = 0.03, 95% CI [0.01, 0.09] for alcohol use and ICC = 0.14, 95% CI [<0.01, 0.36] for cannabis use). However, school-level differences in alcohol and cannabis use were not statistically significant in one-way ANOVAs and can be attributed to chance, F(1, 376) = 0.093, P = .76 for alcohol use and F(1, 358) = 0.919, P = .338 for cannabis use (36). Thus, although the data is collected across 20 schools, the analyses were conducted at a single level.
2.3.2 Models
Two zero-inflated Poisson regression models using the pscl package in R version 4.4.0 (37, 38) estimated the odds of abstinence from alcohol/cannabis (Models 1a and 2a) and the number of days of use (Models 1b and 2b) with the primary independent variable being Assessment of Recovery Capital and Recovery Ecosystem Index, while controlling for age, race, gender, and whether they had been at the RHS for 90 days. Missingness for predictor variables ranged from 0% to 11%. Responses on these variables were assumed missing at random and imputed via conditional multiple imputations by chained equations (39, 40). Statistical significance was assessed using an alpha level of 0.05, with p-values less than this threshold considered statistically significant.
3 Results
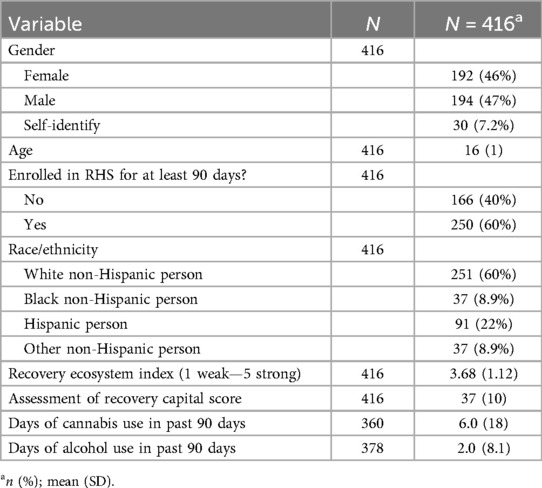
Table 2 shows the counts and percentages for all study variables. There were 378 (91%) and 360 (87%) participants that provided alcohol and cannabis use data, respectively. Respondents missing alcohol or cannabis use data were excluded from that analysis. The average number of alcohol use days in the last 90 days was 2 but was highly variable (SD = 8.1), and the average number of cannabis use days in the last 90 was 6—again with high variability in the estimate of central tendency (SD = 18). A minority of participants self-identified as a gender other than female or male (7%), with a nearly even split between those identifying as female (n = 192, 46%) or male (n = 194, 47%). The average age of participants was 16 (SD = 1) and most (n = 250, 60%) had been enrolled in a RHS for at least 90 days. The majority of participants identified as White non-Hispanic person/persons/people (n = 251, 60%). Nearly all students (97%) had a high probability of a mental health disorder or problem in the past year in addition to substance use per the GAIN-SS. Poisson regression models were estimated for both alcohol and cannabis use days to investigate the presence of multicollinearity. All variance inflation factors for predictor variables were found to be less than 1.09, which indicates little to no multicollinearity. Correlations for all numeric variables can be found in Supplementary Table S2.
3.1 Past 90-day alcohol use
Our multivariable findings (Table 3, Model 1a) for odds of alcohol use in the last 90 days indicate that the odds of reporting zero alcohol use days (i.e., abstinence) is higher among Hispanic identifying students, compared to White identifying students [adjusted odds ratio (aOR) = 2.19, 95% confidence interval (CI) = 1.10–4.37, P = 0.03]. Those enrolled in a RHS for at least 90 days were also more likely to report alcohol abstinence (aOR = 1.68, 95% CI = 1.01–2.79, P = 0.05. The odds of alcohol abstinence increased as Assessment of Recovery Capital score increased (aOR = 1.03, 95% CI = 1.01–1.06, P = 0.02).
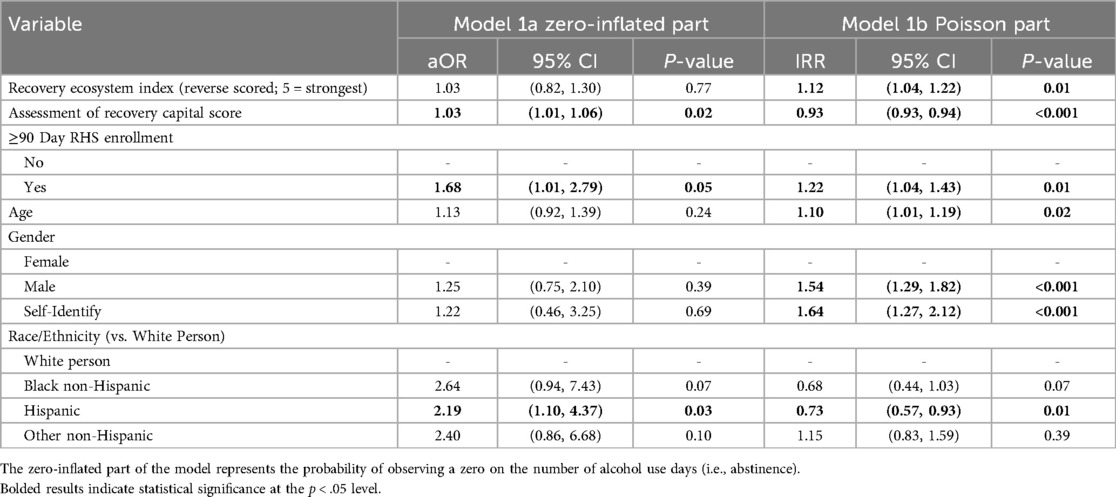
Table 3. Zero-inflated Poisson regression estimating adjusted odds ratios (aOR) of alcohol abstinence and incidence rate ratio (IRR) of alcohol use days in past 90.
In contrast, our multivariable findings estimating the number of alcohol use days (Table 3, Model 1b) suggest that as age increased, the rate of drinking days also increased [incidence rate ratio (IRR) = 1.10, 95% CI = 1.01–1.19, P = 0.02]. Males (IRR = 1.54, 95% CI = 1.29–1.82, P < 0.001) and participants self-identifying their gender (IRR = 1.64, 95% CI = 1.27–2.12, P < 0.001) also reported higher rates of drinking days compared to females. As the Recovery Ecosystem Index increased, so did the rate of the drinking days (IRR = 1.12, 95% CI = 1.04–1.22, P = 0.01). Students enrolled for at least 90 days also had higher rates of drinking days (IRR = 1.22, 95% CI = 1.04–1.43). Hispanic identifying students reported lower rates of drinking days compared to white persons (IRR = 0.73, 95% CI = 0.57–0.93, P = 0.01), and the rate of drinking days decreased as Assessment of Recovery Capital Score increased (IRR = 0.93, 95% CI = 0.93–0.94, P < 0.001).
3.2 Past 90-day cannabis use
For cannabis use, our multivariable findings estimating the odds of cannabis use days in last 90 days (Table 4, Model 2a) show that Black non-Hispanic identifying students were more likely to report cannabis abstinence compared their students identifying as White (aOR = 2.86, 95% CI = 1.02–8.03, P = 0.05). Students who had been enrolled for at least 90 days at a RHS also had higher odds of reporting cannabis abstinence compared to those that had been enrolled for less than 90 days (aOR = 2.01, 95% CI = 1.21–3.33, P = 0.01). Additionally, as Assessment of Recovery Capital score increased so too did the odds of cannabis abstinence (aOR = 1.03, 95% CI = 1.01–1.06, P = 0.01).
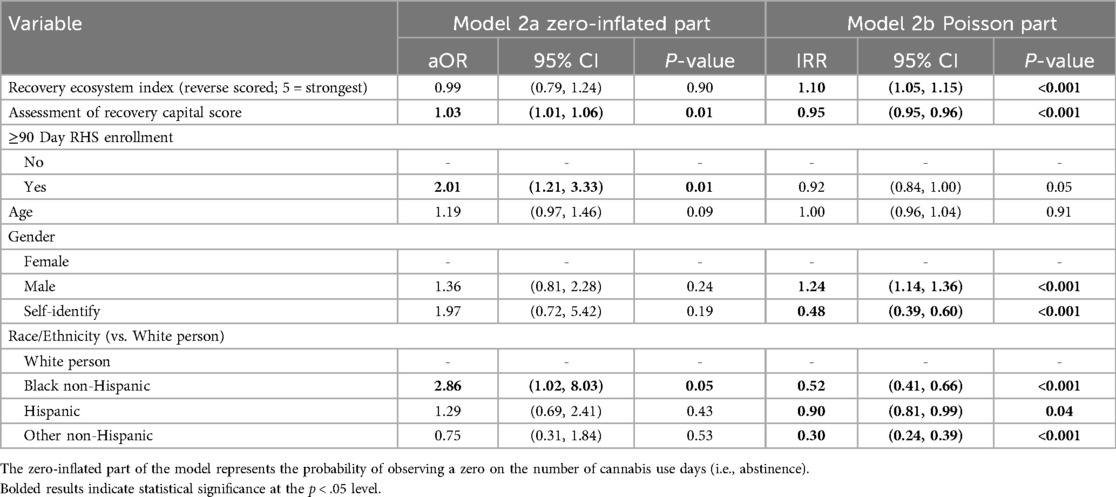
Table 4. Zero-inflated Poisson regression estimating adjusted odds ratios (aOR) of cannabis abstinence and incidence rate ratio (IRR) of cannabis use days in past 90.
Our multivariable findings estimating the number of cannabis use days (Table 4, Model 2b) found that students who were enrolled in an RHS for at least 90 days trended towards fewer cannabis use days compared to those who were not enrolled for 90 days (IRR = 0.92, 95% CI = 0.84–1.00, P = 0.05), though this difference was not statistically significant. Black non-Hispanic (IRR = 0.52, 95% CI = 0.41–0.66, P < 0.001), Hispanic (IRR = 0.73, 95% CI = 0.57–0.99, P = 0.04), and Other non-Hispanic (IRR = 0.30, 95% CI = 0.24–0.39, P < 0.001) students had lower rates of cannabis use days compared to White identifying students. Students who self-identified their gender as non-binary also had a lower rate of cannabis use days compared to female identifying students (IRR = 0.48, 95% CI = 0.39–0.60, P < 0.001). Male students had a higher rate of cannabis use days compared to female students (IRR = 1.24, 95% CI = 1.14–1.36, P < 0.001). As Assessment of Recovery Capital scores increased, the rate of cannabis use days decreased (IRR = 0.95, 95% CI = 0.95–0.96, P < 0.001). Yet, the rate of cannabis use days increased as the Recovery Ecosystem Index score increased (IRR = 1.10, 95% CI = 1.05–1.15, P < 0.001).
4 Discussion
In this study, we examined the associations between recovery capital at the individual level, community recovery capital (i.e., the recovery ecosystem index), and days of cannabis and alcohol use among adolescents enrolled in a RHS. This study contributes to the recovery literature in three key ways: (1) by focusing on a unique and resilient adolescent sample engaged in recovery programming, (2) by utilizing a novel, objective measure of community recovery capital—the recovery ecosystem index, (3) by examining the two most commonly used substances among adolescents—alcohol and cannabis. Adolescence has been called a time of “storm and stress”, and the unique challenges of adolescence are often referenced when adolescent substance use is examined (6, 41). However, adolescents also exhibit unique strengths, potential, and resilience (42, 43). Adolescents in recovery from substance use problems are one such group of young people. RHSs are one place where this can be seen—adolescents with substance use problems maintain their recovery while completing secondary school. In this study, students who had been enrolled in a RHS for at least 90 days had higher odds of abstinence from both alcohol and cannabis. Being enrolled for at least 90 days was associated with 68% higher odds of alcohol abstinence and 101% higher odds of cannabis abstinence. However, students who were in a RHS for at least 90 days reported a higher rate of alcohol use days compared to those that had not been enrolled as long. These findings may suggest that, in general, attending a RHS supports discontinuation of use, which aligns with previous work that has found attending a RHS instead of a traditional school after substance use treatment to be linked with reduced substance use (17). However, the higher reported rate of alcohol use days among students enrolled for at least 90 days may reflect differences in the population of students who persist in these schools. For instance, students with more severe substance use histories may stay enrolled longer to receive continued support, which could explain their higher rates of alcohol use days despite the observed benefits in abstinence odds. Future research would benefit from incorporating more detailed clinical assessments or longitudinal data to better understand these patterns and address the apparent contradiction.
Although our findings suggest that RHS attendance for at least 90 days is linked with higher odds of abstinence, there are less than 50 RHSs across the US. Questions remain about how RHSs may shape public attitudes towards substance use and recovery. Although some worry that designating a separate school for youth in recovery could reinforce stigma–akin to “not in my backyard” (NIMBY) reactions–there is reason to believe the opposite is true. RHSs often highlight students' resilience through personal stories via media outlets and graduation ceremonies (44). The schools offer visible examples of successful recovery that could help challenge stigmatizing narratives of substance use and recovery. However, to our knowledge, no empirical research has investigated how RHSs impact stigma, either within the broader school ecosystem or in their surrounding communities. Future work is needed to explore whether and how RHSs might influence public perceptions of youth substance use and recovery.
On the theoretical premise that context matters to recovery (45, 46), experts in the field of recovery developed the Recovery Ecosystem Index as a novel measure to quantify how recovery supportive a county is, which could be considered community recovery capital. Findings in this study indicated that as a students' community recovery capital increased, so too did their rate of both alcohol and cannabis use. Although unexpected, this study was cross-sectional and cannot determine the causal direction of effects between substance use, recovery capital at the individual level, and community recovery capital. Some areas may generally have higher rates of substance use which have led to a more robust recovery ecosystem. In this case, it would be beneficial for community recovery capital to be higher in places where students' use is also higher. Conversely, it may be that the Recovery Ecosystem Index is not appropriately measuring community recovery capital for adolescents. The Index was created with adults in mind and includes recovery programming frequented by adults (e.g., adult drug treatment courts, SMART recovery programs). Thus, it does not capture youth-focused policies, services, or supports. Future investigation would likely benefit from a tailored community recovery capital measure for young people. Such research could help illuminate the distinctions between adult and adolescent recovery ecosystems, providing more targeted insights for youth-focused recovery efforts.
Measurement of recovery capital has expanded exponentially in the last decade, despite the lack of a measure of recovery capital for adolescents (1, 22). Recovery capital aims to encompass recovery-supportive resources at multiple ecological levels (e.g., personal, social, community). The Assessment of Recovery Capital is one of the most commonly used measures of recovery capital, but the psychometrics of the scale have been mixed (47, 48). Findings in this study, however, align with the expected outcomes for recovery capital. Specifically, each one-unit increase in the recovery capital score (on a scale of 0–50) corresponded to a 3% increase in the odds of being abstinent from both alcohol and cannabis. Similarly, every one-unit increase in the recovery capital score was linked to 7% fewer days of alcohol use and 5% fewer days of cannabis use. While these effects were modest, they may reflect potential ceiling effects within the sample, limiting the ability to detect stronger associations. Although the Assessment of Recovery Capital lacks a developmental focus, it may still provide useful information for recovery care planning. For example, focusing on increasing aspects of recovery capital, such as building social connections, may improve substance use outcomes among adolescents (49, 50). Future scholarship would benefit from longitudinal data collection to establish the causal effect of improving recovery capital. Furthermore, creating a youth-focused measure of recovery capital would likely improve the reliability, validity, and clinical utility of recovery capital.
The current study has several limitations. First, the RHSs and students who participated in the study are likely not representative of the entire RHS population. The convenience sampling limits generalizing these findings to all students attending a RHS or that are in recovery. Only 44% of currently operating RHSs are included in this study, and the exact response rate within each school is unknown. However, feedback from participating schools indicated that at least 80% of their students took the survey (personal communications, February 2022 to June 2023). Second, the Assessment of Recovery Capital and the Recovery Ecosystem Index were not constructed for adolescents. The unique developmental period of adolescence likely warrants tailored measures. For example, the recovery ecosystem index was inversely related to substance use, which is not aligned with existing theory (22, 25). This may have resulted from the exclusion of adolescent-specific treatment and recovery services in the metric as well as findings from previous studies showing that adolescents rarely engage in some services (e.g., mutual aid) (51–53). Yet, the findings for recovery capital aligned with recovery capital theory (20, 21, 46). Third, students may not live in the county that the RHS is in, which was the proxy for student county-of-residence. Fourth, the study did not control for other important variables that influence rates of alcohol and cannabis use such as recovery goals, motivation for abstinence, and self-efficacy. Fifth, the study did not assess participants' definitions of recovery, and individuals likely identified with a range of recovery pathways. Recovery-informed theory suggests that recovery encompasses multiple mechanisms of behavior change and a broad set of outcomes related to health and well-being. Future research should examine how changes in substance use relate to diverse recovery definitions and pathways. For instance, even if substance use remains unchanged in the short term, individuals may develop stronger coping skills or other protective factors that support longer-term recovery trajectories.
In conclusion, the study's findings suggest that higher recovery capital is associated with increased odds of complete abstinence and reduced days of alcohol and cannabis use among adolescents attending a RHS. These findings underscore the value of assessing and supporting recovery capital in youth-focused recovery settings like RHSs (29). Although the recovery ecosystem index was unexpectedly associated with more days of alcohol and cannabis use, this highlights the need for further refinement of youth-specific measures. Overall, the results support continued investment in recovery-supportive environments, such as RHSs, and call for future research to develop and validate tools that can inform individualized and education-based recovery support planning.
Data availability statement
The data analyzed in this study is subject to the following licenses/restrictions: data for this study was made available by the Association of Recovery Schools. All data requests must be made through the Association of Recovery Schools and their Data Subcommittee. The R code for this study is available upon request. Requests to access these datasets should be directed to info@recoveryschools.org.
Author contributions
JJ: Conceptualization, Data curation, Formal analysis, Investigation, Methodology, Writing – original draft, Writing – review & editing. SG: Data curation, Writing – review & editing. AR: Investigation, Project administration, Writing – review & editing. AF: Investigation, Writing – review & editing. JK: Writing – review & editing. EH: Methodology, Writing – review & editing.
Funding
The author(s) declare that financial support was received for the research and/or publication of this article. Research reported in this publication was supported by the National Institute on Alcohol Abuse and Alcoholism of the National Institutes of Health under Award Number K01AA028536 to EH and K24AA022136-10 to JK. The content is solely the responsibility of the authors and does not necessarily represent the official views of the National Institutes of Health.
Acknowledgments
We would like to acknowledge that data for this study was collected from the Systematic Evaluation of the Association of Recovery Schools (SEARS) in partnership with the Association of Recovery Schools. We would also like to thank the recovery high school staff and students, for whom this project would not have been possible.
Conflict of interest
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
The author(s) declared that they were an editorial board member of Frontiers, at the time of submission. This had no impact on the peer review process and the final decision.
Generative AI statement
The author(s) declare that no Generative AI was used in the creation of this manuscript.
Publisher's note
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
Supplementary material
The Supplementary Material for this article can be found online at: https://www.frontiersin.org/articles/10.3389/fradm.2025.1567567/full#supplementary-material
References
1. Finch AJ, Jurinsky J, Anderson BM. Recovery and youth: an integrative review. Alcohol Res. (2020) 40(3):6. doi: 10.35946/arcr.v40.3.06
2. Schulenberg JE, Maslowsky J, Patrick ME, Martz M. Substance use in the context of adolescent development. In: Zucker RA, Brown SA, editors. The Oxford Handbook of Adolescent Substance Abuse. New York, NY: Oxford University Press (2015). p. 18–36.
3. Brown SA, McGue M, Maggs J, Schulenberg J, Hingson R, Swartzwelder S, et al. A developmental perspective on alcohol and youths 16 to 20 years of age. Pediatrics. (2008) 121(Supplement 4):S290–310. doi: 10.1542/peds.2007-2243D
4. Bronfenbrenner U. The Ecology of Human Development: Experiments by Nature and Design. Cambridge, Mass: Harvard University Press (1979). p. 330.
5. Sawyer S, Afifi RA, Bearinger LH, Blakemore SJ, Dick B, Ezeh AC, et al. Adolescence: a foundation for future health. Lancet. (2012) 379(9826):1630–40. doi: 10.1016/S0140-6736(12)60072-5
6. Jackson KM. A developmental perspective on substance involvement from adolescence to emerging adulthood. In: Zucker RA, Brown SA, editors. The Oxford Handbook of Adolescent Substance Abuse. New York, NY: Oxford University Press (2015). p. 36–74.
7. Schulenberg JE, Maggs JL. A developmental perspective on alcohol use and heavy drinking during adolescence and the transition to young adulthood. J Stud Alcohol Suppl. (2002) (s14):54–70. doi: 10.15288/jsas.2002.s14.54
8. Charrier L, van Dorsselaer S, Canale N, Baska T, Kilibarda B, Comoretto RI, et al. A focus on adolescent substance use in Europe, Central Asia and Canada. Health behaviour in school-aged children international report from the 2021/2022 survey. Volume 3. Copenhagen: WHO Regional Office for Europe (2024). Available at: https://www.who.int/europe/publications/i/item/9789289060936 (Accessed April 25, 2024).
9. Miech RA, Johnston LD, Patrick ME, O’Malley PM, Bachman JG, Schulenberg JE. Monitoring the future national survey results on drug use, 1975–2022: secondary school students. Ann Arbor, MI: Institute for Social Research, The University of Michigan (2023). (Monitoring the Future Monograph Series). Available at: https://monitoringthefuture.org/results/publications/ (Accessed March 12, 2024).
10. Miech RA, Johnston LD, Patrick ME, O’Malley PM, Bachman JG. Monitoring the future national survey results on drug use, 1975–2023: overview and detailed results for secondary school students. Ann Arbor, MI: Institute for Social Research, University of Michigan (2024). (Monitoring the Future Monograph Series). Available at: https://monitoringthefuture.org/results/annual-reports/ (Accessed March 22, 2024).
11. Crosnoe R, Benner AD, Schneider B. Drinking, socioemotional functioning, and academic progress in secondary school. J Health Soc Behav. (2012) 53(2):150–64. doi: 10.1177/0022146511433507
12. Daw J, Margolis R, Wright L. Emerging adulthood, emergent health lifestyles: sociodemographic determinants of trajectories of smoking, binge drinking, obesity, and sedentary behavior. J Health Soc Behav. (2017) 58(2):181–97. doi: 10.1177/0022146517702421
13. Zuckermann AME, Williams GC, Battista K, Jiang Y, de Groh M, Leatherdale ST. Prevalence and correlates of youth poly-substance use in the COMPASS study. Addict Behav. (2020) 107:106400. doi: 10.1016/j.addbeh.2020.106400
14. Schwartz SJ, Des Rosiers SE, Unger J, Szapocznik J. Adolescent cultural contexts for substance use: intergroup dynamics, family processes, and neighborhood risks. In: Zucker RA, Brown SA, editors. The Oxford Handbook of Adolescent Substance Abuse. New York, NY: Oxford University Press (2015). p. 716–42.
15. Chassin L, Colder CR, Hussong A, Sher KJ. Substance use and substance use disorders. In: Cicchetti D, editor. Developmental Psychopathology. Hoboken, NJ: John Wiley & Sons, Inc. (2016). p. 833–97.
16. Kelly JF, Bergman B, Hoeppner BB, Vilsaint C, White WL. Prevalence and pathways of recovery from drug and alcohol problems in the United States population: implications for practice, research, and policy. Drug Alcohol Depend. (2017) 181(181):162–9. doi: 10.1016/j.drugalcdep.2017.09.028
17. Finch AJ, Tanner-Smith E, Hennessy EA, Moberg DP. Recovery high schools: effect of schools supporting recovery from substance use disorders. Am J Drug Alcohol Abuse. (2018) 44(2):175–84. doi: 10.1080/00952990.2017.1354378
18. Ashford RD, Brown A, Brown T, Callis J, Cleveland HH, Eisenhart E, et al. Defining and operationalizing the phenomena of recovery: a working definition from the recovery science research collaborative. Addict Res Theory. (2019) 27(3):179–88. doi: 10.1080/16066359.2018.1515352
19. Hagman BT, Falk D, Litten R, Koob GF. Defining recovery from alcohol use disorder: development of an NIAAA research definition. Am J Psychiatry. (2022) 179:807–13. doi: 10.1176/appi.ajp.21090963
20. Best D, Hennessy EA. The science of recovery capital: where do we go from here? Addiction. (2022) 117(4):1139–45. doi: 10.1111/add.15732
21. Hennessy EA. Recovery capital: a systematic review of the literature. Addict Res Theory. (2017) 25(5):349–60. doi: 10.1080/16066359.2017.1297990
22. Bunaciu A, Bliuc AM, Best D, Hennessy EA, Belanger MJ, Benwell CSY. Measuring recovery capital for people recovering from alcohol and drug addiction: a systematic review. Addict Res Theory. (2023) 32(3):1–12. doi: 10.1080/16066359.2023.2245323
23. Hennessy EA, Cristello JV, Kelly JF. RCAM: a proposed model of recovery capital for adolescents. Addict Res Theory. (2019) 27(5):429–36. doi: 10.1080/16066359.2018.1540694
24. Mumba MN, Mugoya GT. Recovery ecosystems: a whole health approach to substance use prevention and treatment. J Psychosoc Nurs Ment Health Serv. (2022) 60(9):10–4. doi: 10.3928/02793695-20220809-05
25. Ashford RD, Brown AM, Ryding R, Curtis B. Building recovery ready communities: the recovery ready ecosystem model and community framework. Addict Res Theory. (2019) 28(1):1–11. doi: 10.1080/16066359.2019.1571191
26. Finch AJ, Moberg DP, Krupp AL. Continuing care in high schools: a descriptive study of recovery high school programs. J Child Adolesc Subst Abuse. (2014) 23(2):116–29. doi: 10.1080/1067828X.2012.751269
27. Finch AJ. Recovery high schools growth chart: 1979-2021. Association of Recovery Schools (2021). >Available at: https://recoveryschools.org/rhs-growth-chart/ (Accessed January 25, 2022).
28. Office of National Drug Control Policy. National drug control strategy. The white house, executive office of the president (2022). Available at: https://www.whitehouse.gov/wp-content/uploads/2022/04/National-Drug-Control-2022Strategy.pdf (Accessed March 14, 2023).
29. Hennessy EA, George SS, Klein MR, O’Connor JB, Eddie D, Kelly JF. A systematic review of recovery high schools and collegiate recovery programs for building recovery capital among adolescents and emerging adults. Front Adolesc Med. (2025) 3:1522678. doi: 10.3389/fradm.2025.1522678
30. Weimer DL, Moberg DP, French F, Tanner-Smith EE, Finch AJ. Net benefits of recovery high schools: higher cost but increased sobriety and increased probability of high school graduation. J Ment Health Policy Econ. (2019) 22(3):109–20.31811754
31. NORC at the University of Chicago. East Tennessee state university, the fletcher group, ETSU/NORC rural health equity research center. Recovery ecosystem index map. Available at: https://rei.norc.org/ (Accessed September 25, 2024).
32. Wahlquist AE, Mathis SM, Trull LH, Toitole KK, Howard A, Fletcher E, et al. Associations between drug overdose mortality and recovery ecosystems in the United States: a county-level analysis using a novel index. Subst Use Addict J. (2024) 46(2):1–9. doi: 10.1177/29767342241262125
33. Groshkova T, Best D, White WL. The assessment of recovery capital: properties and psychometrics of a measure of addiction recovery strengths. Drug Alcohol Rev. (2013) 32(2):187–94. doi: 10.1111/j.1465-3362.2012.00489.x
34. Dennis ML, Feeney T, Titus JC. Global appraisal of individual needs—short screener (GAIN-SS): administration and scoring manual, version 3. Bloomington, IL: Chestnut Health Systems (2013).
35. Behringer B. Responding to Appalachian voices: steps in developing substance-use recovery ecosystems. (2020). Available at: https://uknowledge.uky.edu/jah/vol2/iss3/10/ (Accessed March 4, 2024).
36. Snijders TAB, Bosker RJ. Multilevel Analysis an Introduction to Basic and Advanced Multilevel Modeling. 1st ed. Thousand Oaks, CA: SAGE (1999).
37. Zeileis A, Kleiber C, Jackman S. Regression models for count data in R. J Stat Software. (2008) 27(8):1. doi: 10.18637/jss.v027.i08
38. R Core Team. R: a langauge and environment for statistical computing. Vienna, Austria: R Foundation for Statistical Computing (2020). Available at: https://www.R-project.org/ (Accessed April 30, 2024).
39. van Buuren S, Groothuis-Oudshoorn K. Mice: multivariate imputation by chained equations in R. J Stat Software. (2011) 45:1–67. doi: 10.18637/jss.v045.i03
40. Azur MJ, Stuart EA, Frangakis C, Leaf PJ. Multiple imputation by chained equations: what is it and how does it work? Int J Methods Psychiatr Res. (2011) 20(1):40–9. doi: 10.1002/mpr.329
41. Buchanan CM, Romer D, Wray-Lake L, Butler-Barnes ST. Adolescent storm and stress: a 21st century evaluation. Front Psychol. (2023) 14:1257641. doi: 10.3389/fpsyg.2023.1257641
42. Lerner RM. The Good Teen: Rescuing Adolescence From the Myths of the Storm and Stress Years. 1st ed. New York: Three Rivers Press (2007). p. 257; (A Stonesong Press Book).
43. Hurd N, Zimmerman M. Adolescent resilience: promoting more positive outcomes among youth at risk of using and abusing substances. In: Zucker RA, Brown SA, editors. The Oxford Handbook of Adolescent Substance Abuse. New York, NY: Oxford University Press (2015). p. 504–28.
44. Mulkerrins J. The straight AA students; welcome to Boston’s pioneering William J Ostiguy High School for teenage alcoholics and addicts, where 12-step recovery is on the timetable and the students learn to live clean and sober. Sunday Telegraph (2014).
45. Cloud W, Granfield R. Natural recovery from substance dependency: lessons for treatment providers. J Soc Work Pract Addict. (2001) 1(1):83–104. doi: 10.1300/J160v01n01_07
46. Cloud W, Granfield R. Conceptualizing recovery capital: expansion of a theoretical construct. Subst Use Misuse. (2008) 43(12–13):1971–86. doi: 10.1080/10826080802289762
47. Bowen EA, Scott CF, Irish A, Nochajski TH. Psychometric properties of the assessment of recovery capital (ARC) instrument in a diverse low-income sample. Subst Use Misuse. (2020) 55(1):108–18. doi: 10.1080/10826084.2019.1657148
48. Vilsaint CL, Kelly JF, Bergman BG, Groshkova T, Best D, White WL. Development and validation of a brief assessment of recovery capital (BARC-10) for alcohol and drug use disorder. Drug Alcohol Depend. (2017) 177:71–6. doi: 10.1016/j.drugalcdep.2017.03.022
49. Nash AJ, Hennessy EA, Collier C. Exploring recovery capital among adolescents in an alternative peer group. Drug Alcohol Depend. (2019) 199:136–43. doi: 10.1016/j.drugalcdep.2019.02.025
50. Jurinsky J, Cowie K, Blyth S, Hennessy EA. “A lot better than it used to be”: a qualitative study of adolescents’ dynamic social recovery capital. Addict Res Theory. (2022) 31(2):77–83. doi: 10.1080/16066359.2022.2114076
51. Nash AJ, Hennessy EA, Collier C, Kelly JF. Young people’s perceptions of the 12-steps’ role in supporting their recovery (or not). J Child Adolesc Subst Abuse. (2020) 28(5):1–15. doi: 10.1080/1067828X.2020.1766619
52. Kelly JF, Dow SJ, Yeterian JD, Kahler CW. Can 12-step group participation strengthen and extend the benefits of adolescent addiction treatment? A prospective analysis. Drug Alcohol Depend. (2010) 110(1–2):117–25. doi: 10.1016/j.drugalcdep.2010.02.019
Keywords: recovery high school, addiction, adolescent, substance use, recovery ecosystem, recovery capital, alcohol, cannabis
Citation: Jurinsky J, George SS, Riccio AA, Finch AJ, Kelly JF and Hennessy EA (2025) Recovery capital, the recovery ecosystem, and substance use among recovery high school students. Front. Adolesc. Med. 3:1567567. doi: 10.3389/fradm.2025.1567567
Received: 27 January 2025; Accepted: 30 May 2025;
Published: 13 June 2025.
Edited by:
Ottar Ness, Norwegian University of Science and Technology, NorwayReviewed by:
Wouter Vanderplasschen, Ghent University, BelgiumLucy Webb, Manchester Metropolitan University, United Kingdom
Copyright: © 2025 Jurinsky, George, Riccio, Finch, Kelly and Hennessy. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Jordan Jurinsky, Sm9yZGFuLmp1cmluc2t5QHR1ZnRzLmVkdQ==
 Jordan Jurinsky
Jordan Jurinsky Shane S. George
Shane S. George Arianna A. Riccio3
Arianna A. Riccio3 Andrew J. Finch
Andrew J. Finch John F. Kelly
John F. Kelly Emily A. Hennessy
Emily A. Hennessy