- 1School of Social Work, Virginia Commonwealth University, Richmond, VA, United States
- 2Faculty of Social Work, University of Calgary, Calgary, AB, Canada
- 3Department of Human Development, Washington State University, Pullman, WA, United States
- 4Department of Psychology, University of Windsor, Windsor, ON, Canada
- 5Addictive Disorders and Recovery Studies, Texas Tech University, Lubbock, TX, United States
- 6Department of Psychiatry, Robert Wood Johnson Medical School, Rutgers, The State University of New Jersey, Piscataway, NJ, United States
Introduction: Experiencing trauma is well-known to negatively impact AOSUD recovery and recovery capital. However, having a stronger recovery identity positively impacts recovery capital, and can be strengthened through recovery-supportive relationships. Identity change and reconstruction is also central to trauma healing, making it likely that recovery identity buffers the effect of trauma on recovery capital. This study examines this relationship and identifies types of recovery supports that facilitate development of stronger recovery identity within participants in collegiate recovery programs (CRPs).
Methods: The sample consisted of participants in the National Longitudinal Collegiate Recovery Study who completed all measures at their baseline assessment (N = 168). Total scores of the PCL-5 short form (trauma) and Recovery Identity scale (RI) were regressed on the Brief Assessment of Recovery Capital (BARC) total score. Measures of recovery support, including a measure of support from CRP staff and individual yes/no questions about experiencing various recovery supports, were regressed on RI scores.
Results: Lower PCL-5 scores and higher RI scores both significantly predicted higher recovery capital scores [adjR2 = .51; F(3, 168) = 59.61, p < .001], and interacted such that having higher RI scores buffered the impact of having higher trauma scores on recovery capital [ΔR2 = .01, F(4, 168) = 46.66, p < .001]. Perceiving CRP staff (β = .04, p = .007) and peers in recovery (β = .32, p < .001) as being supportive of one's recovery significantly predicted higher recovery identity scores [adjR2 = .16; F(5, 173) = 107.01, p < .001].
Conclusion: Having a stronger recovery identity buffers the impact of trauma symptoms on recovery capital for CRP participants. CRP participants who perceive their CRP staff as being strong role models and providing a safe, welcoming recovery space and who have support from peers in recovery had stronger recovery identities. CRPs can help participants with higher trauma levels to build recovery-supportive relationships with their peers, and can create supportive, trauma-responsive spaces for all participants.
1 Introduction
Estimates suggest that approximately 600,000 college students are in recovery from substance use disorders (SUDs) (1). Recovery is more than remission from SUDs, and can be understood as a holistic process through the framework of recovery capital (2). Recovery capital (RC) is a multidimensional strength-based framework that encompasses the internal and external resources an individual accumulates to sustain long-term recovery from SUDs (3). While various models of recovery capital exist, common domains include personal (motivation, coping skills), social (friends/family supportive of recovery), and community (norms, policies) (4, 5). RC and time in remission are positively and reciprocally related, with greater recovery capital predicting longer time in remission, and longer time in remission predicting accrual of greater recovery capital (6). Greater recovery capital is also associated with several other positive outcomes for individuals in recovery, including greater quality of life and mental and physical wellbeing (2). RC is an important metric in itself and also serves as a mechanism by which many positive recovery-related outcomes are obtained. In sum, RC significantly enhances resilience and promotes sustained recovery.
Gaps remain in understanding how different factors interact to influence the development, trajectory, and function of RC during recovery, particularly among adolescents and young adults (5). College students are developmentally in a transitional stage where they are forming new identities as independent adults (7). The development of recovery identity–often defined as a change in identity from someone who uses substances to someone in recovery (8)–is part of this process for students in recovery, and thus is particularly useful for understanding RC in young adults in college settings. However, additional research on the interplay between recovery identity and RC is needed.
1.1 Collegiate recovery programs and RC
Collegiate Recovery Programs (CRPs) are community-based and primarily peer-driven organizations that aim to increase RC by offering supportive environments tailored for young adults in recovery (5, 9, 10). CRPs began in the 1970s and have expanded rapidly; currently, there are at least 138 in the United States (11), with several new programs introduced in Canada and the United Kingdom since 2019 (12–14). These programs provide critical resources, foster peer relationships, and facilitate connections to recovery-oriented activities essential to recovery processes. CRPs systematically target personal, social, and community-level barriers, and enhance the accumulation of recovery capital through diverse programmatic offerings (5, 11). Considering most CRPs are peer-driven, social recovery capital is central to their success in promoting recovery. Social capital encompasses the resources individuals can access through relationships and is often categorized as bonding capital—the strength of connections within peer groups—and bridging capital, which refers to the ability to establish new networks and access broader social resources (15). Within CRPs, both forms of social capital are essential, as students rely on peer and professional relationships to develop the therapeutic alliances that foster resilience and recovery identity (16).
1.2 Recovery identity and RC
College often represents a critical developmental period for young adults in recovery for many reasons. In addition to being a key period for identity development (7), individuals in recovery from SUDs are also focused on establishing a strong recovery identity and accruing RC. Although recovery identity has been conceptualized in various ways, there is general agreement that developing a recovery identity involves a fundamental shift in self-perception (17) that also incorporates a social dimension based on groups that people belong to (18). Thus, adopting a recovery identity is underpinned by moving away from social groups centered on substance use toward identifying with groups whose values support recovery goals (8). Recent research has increasingly examined recovery identity through the lens of social identity theory (19), utilizing a variety of both qualitative and quantitative methods. For example, foundational work by Best and colleagues has used social identification scales that measure the extent of adults' identification with therapeutic communities to examine associations between recovery identity and RC (20, 21). Other research, including with samples of adolescents and young adults, has used a novel visual technique called Social Identity Mapping (SIM) to assess changes in social identity and social networks (22–24). Despite these advances, some scientists have noted that other important aspects of recovery-related identities, including both the process and content of identities, are needed and that measurement of user (and we would argue, recovery) identity development is lacking (25).
Further, recovery identity is a strong predictor of positive recovery outcomes, including lower relapse rates, increased treatment retention, and higher recovery self-efficacy (22, 26, 27). There is also evidence that a stronger recovery identity is associated with greater personal and social RC. Dingle et al. (28) found that among 132 adults in a therapeutic community, those who transitioned from a substance-using identity to a recovery identity experienced lower substance use and greater life satisfaction at follow-up. Similarly, Best et al. (20) and Mawson et al. (29) demonstrated that identifying with recovery-focused groups is linked to increased recovery capital, reduced substance use, and greater social support. However, not all individuals adopt a recovery-oriented identity, as some struggle to relate to recovery culture or prefer alternative ways of conceptualizing their healing (5, 30). Research also suggests that the intensity of relationships within non-using groups strengthens recovery identity, reinforcing the importance of structured support systems such as CRPs in fostering identity change and long-term recovery (30).
1.3 Trauma exposure and RC
The association between recovery capital and one's ability to recover from SUDs is grounded in the transactional model of stress and coping (31, 32), whereby individuals with greater recovery capital appraise situations as less stressful and are more likely to cope with them effectively (6). Examples of recovery capital and predictors of sustained recovery over time include self-efficacy, social support, quality of life, health, spirituality, and abstinence or controlled substance use (33–37). In contrast, less recovery capital (e.g., low self-efficacy, low social support, poor quality of life, negative affect) can lead to greater distress and the use of coping strategies that threaten one's recovery (38). Roughly 25% to 50% of people who have SUDs have co-occurring posttraumatic stress disorder (PTSD) symptoms (39, 40), and constitute a significant stressor for many people in recovery. SUDs and PTSD are highly comorbid (41); young adults with SUDs are 3.6 times more likely to have co-occurring PTSD (42), and those who develop PTSD are 1.6 times more likely to also be diagnosed with AUD (43). Experiencing trauma is associated with a range of negative consequences, including higher rates of developing a SUD or psychiatric disorder (44–48) and interruption of key developmental tasks (49), like identity development. Further, trauma exposure and PTSD symptoms are linked to diminished personal, social, and community resources that facilitate recovery, limiting individuals' ability to engage in recovery-supportive networks, build RC, and sustain long-term recovery (46, 50, 51).
According to the stress-buffering hypothesis (52–54), social support can buffer against the negative effects of stressful events, like trauma exposure (55). Social support includes instrumental, material, informational, or emotional resources one can provide in order to reduce the burden of stress or increase the ability of another to cope with stress (56). Positive social relationships can help reduce the effects of stressful events and improve psychosocial and physical health outcomes (54, 55, 57). Specifically, positive social relationships can promote healthy habit development (54, 58) and facilitate a sense of security, connectedness, purpose, and autonomy (59), all of which are forms of personal RC. Among college students in recovery, one potential source of positive social relationships (and RC) includes relationships through CRPs. However, additional research is needed to investigate the protective association between supportive relationships and RC within a CRP setting and in the context of other influential factors, like trauma exposure and PTSD symptoms.
1.4 Trauma exposure and recovery identity
Theoretical models of recovery identity construction (8, 19) posit that experiencing higher trauma symptom severity potentially impacts identity formation, and it stands to reason that having a stronger recovery identity might buffer the impact of trauma on recovery capital. A strong recovery identity enhances engagement in recovery-support behaviors and increases RC by reinforcing identification with non-using peer groups, fostering a sense of belonging, and reducing internalized stigma (29, 60). Given the high prevalence of trauma among college students and its impact on recovery, it is essential to examine whether a strong recovery identity can buffer the negative effects of trauma on RC. Prior research has established that trauma exposure is associated with lower RC (50). However, little is known about the role of recovery identity in mitigating this effect. CRPs provide a critical setting to explore this dynamic, offering structured peer and mentor support that reinforces recovery identity, fosters social connection, and enhances overall well-being.
1.5 Current study
This study aims to explore how trauma and recovery identity interact to predict level of recovery capital. Based on the reviewed literature, we hypothesize that:
A. Students with higher levels of trauma will have lower levels of recovery capital;
B. Having a stronger recovery identity will predict having higher recovery capital;
C. There will be a moderating effect between recovery identity and trauma such that higher recovery identity lessens the negative impact of trauma on recovery capital.
D. Having greater recovery support will predict stronger recovery identity.
By understanding the protective role of recovery identity, we can better inform the development of CRP interventions that maximize social support and resilience, ultimately improving recovery outcomes for young adults navigating both trauma and SUD recovery.
2 Methods
2.1 Sample
This analysis used data from the ongoing National Longitudinal Collegiate Recovery Study (CoRe Study; 16). The CoRe Study, described in depth elsewhere, was designed to understand the impact of CRPs on participating students' recovery, academic, and socioemotional outcomes (16) and included students affiliated with CRPs across the US, Canada, and the UK. Individuals who were at least 18 years of age, currently enrolled in higher education, and active participants in a CRP were eligible to complete the baseline survey. Participating CRP directors provided information about the study and a link to complete the survey to their students for the baseline survey, and those who participated at baseline were sent invitations to complete follow-up surveys by the study team. As this study did not gather administrative data about the CRPs (e.g., program size), the baseline response rate could not be calculated. Informed consent and study data were collected and managed using Research Electronic Data Capture (REDCap; 61, 62). This study was approved by the Virginia Commonwealth University institutional review board.
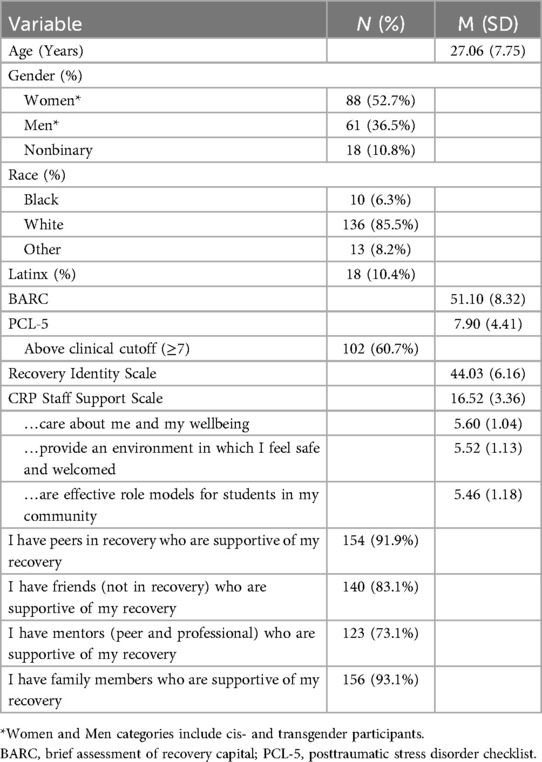
The analytic sample consisted of individuals who completed all relevant measures at baseline during the two waves of data collection conducted between Spring and Fall, 2023 (N = 168). The complete demographic and clinical characteristics of the sample are presented in Table 1. Multiple imputation for pattern analysis indicated that any cases missing demographic or clinical data were missing at random.
2.2 Measures
The Brief Assessment of Recovery Capital (BARC) is a 10-item scale derived from the Assessment of Recovery Capital and measures 10 sub-domains of RC: Substance use and sobriety, global psychological health, global physical health, citizenship and community involvement, social support, meaningful activities, housing and safety, risk-taking, coping and life functioning, and recovery experience (63, 64). The items are scored on a scale of 1 (Strongly disagree) to 6 (Strongly agree) and include items such as, “I get lots of support from friends”, and “There are more important things to me in life than using substances”. The BARC showed good internal consistency reliability (α = .90) and good validity with other measures of recovery (64).
The Recovery Identity Scale (RIS) is a novel measure adapted from the Utrecht-Management of Identity Commitments Scale (65), which measures strength and processes of identity formation such as commitment, exploration, and reconsideration of commitment. The RIS has 10 items coded on a scale of 1 (Strongly disagree) to 5 (Strongly agree). Sample items include, “Being in recovery gives me security for the future”, “I often reflect on what being in recovery means to me”, and “I often think it would be better if I was not in recovery anymore” (reverse-coded). Recent psychometric evaluation of the RIS in this sample showed good internal consistency reliability for the overall scale (α = .86) and for the three identified subscales (Commitment to a recovery identity, α = .95; in-depth exploration, α = .84; and reconsideration of commitment to a recovery identity, α = .90), and good convergent and discriminant validity with measures of quality of life and loneliness, similar to the parent scale (65).1
Trauma symptomatology was measured with the short form of the posttraumatic stress disorder checklist (PCL-5; see text footnote 1). The CoRe Study selected the short form of the PCL-5 rather than a more comprehensive measure in order to reduce participant fatigue while still validly capturing trauma symptomatology. The PCL-5 has 4 items with one item assessing each DSM-5 Criteria, including re-experiencing symptoms (suddenly feeling or acting as if the stressful experience were actually happening again; B3), avoidance symptoms (avoiding external reminders of the stressful experience; C2), mood and cognitive alterations (feeling distant or cut off from other people; D6), and hyperarousal symptoms (irritable, angry outbursts, or acting aggressively). Individual items are scored 0 (not at all) to 4 (extremely), with a total score range of 0–16. Clinical cutoff scores for the PCL-5 are based on the type of clinically-engaged population (military vs. civilian) and the desired level of sensitivity and specificity as provided in the Supplementary Table S10 of the article (66). For this civilian population with moderate levels of sensitivity and specificity, we chose a cutoff of ≥7. This cutoff was used to dichotomize the trauma variable into scores ≥7 (1, indicating potential for clinically significant trauma symptomatology) and scores <7 (0, indicating sub-clinical trauma symptomatology). The PCL-5 demonstrates good convergent and discriminant validity and showed good internal consistency reliability in this sample (α = .83).
Level of recovery support was measured with internally developed items that included three items asking about support from staff at their CRP rated on a scale of 1 (strongly disagree) to 6 (strongly agree) (e.g., “Staff at my collegiate recovery program are effective role models for students in my community”), one item asking “Who in your family is supportive of your recovery?” (0 = none, 1 = some, 2 = most or all of the family members are supportive), and three response categories for the question “Who in your life is supportive of your recovery?” (checked = 1, unchecked = 0): Peers in recovery, friends (not in recovery), and mentors (peer and professional). These categories of support were selected based on previous analyses that identified key recovery support categories for this population (67).
Demographic variables of age, race/ethnicity, and gender identity (see Table 1) were considered for inclusion in the model based on correlations of continuous variables with the outcomes at p < .20 (68). Of these, only age was significantly associated with the outcome and was included in the model.
2.3 Analysis plan
All analyses were completed using SPSS Version 28 (69). Examination of the univariate descriptive statistics determined all variables were acceptable for analysis (70). There were statistically significant differences in BARC or RIS scores as a function of age but not racial categories and gender identity, so age was the only covariate included in the main models (68).
The analysis consisted of two linear regression models. First, hierarchical linear regression with two blocks regressed a base model of RIS scores and dichotomized PCL-5 scores with age as a control variable on BARC scores in the first block, and added the interaction term of mean-centered RIS and PCL-5 scores in the second block to test moderation using significance of the interaction term in the model and R2 change and significance. Second, sources of recovery support with age as a control variable were regressed on RIS scores using simple linear regression.
Overall model fit for all models was assessed using adjusted R2 (71). No variables correlated with each other above.396, and VIF values were all <10 and tolerance values were all >.10, indicating no multicollinearity (68, 72). Examination of outliers identified no multivariate outliers, identified as those cases with residuals falling more than 3 standard deviations above or below the mean (73), or influential outliers, identified using values of Cook's Distance >1.0, dfBeta values >1, and leverage values > .50 (72).
3 Results
Our analysis examined the extent to which recovery identity (RIS) scores and trauma symptomatology (PCL-5) scores predicted recovery capital (BARC-10) scores using hierarchical linear regression. Descriptive statistics for all model variables are presented in Table 1, and full model results are provided in Table 2. The final model with all variables explained 43.5% of BARC total scores for participants in CRPs [R2 = 0.435, F(4,160) = 30.807, p < .001]. Adding the interaction term of mean-centered RIS and PCL-5 scores in the second block to test moderation provided 1.7% additional variance in the model (ΔR2 = 0.017), a statistically significant increase at p = 0.028.
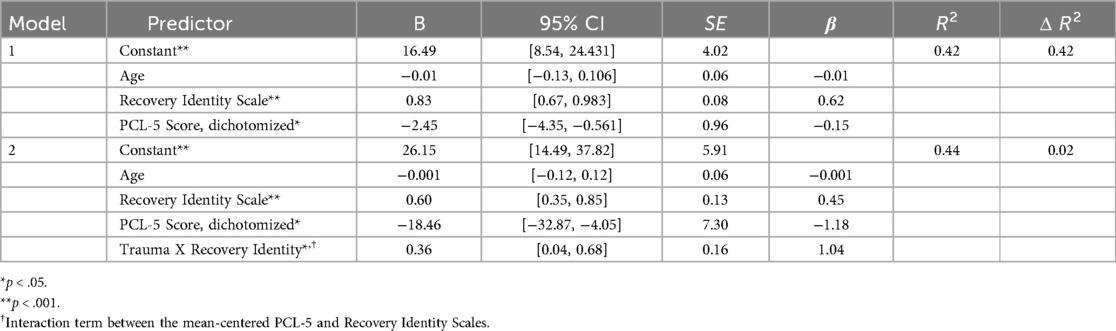
Table 2. Hierarchical linear regression of recovery identity scale scores and dichotomized PCL-5 trauma scores on BARC total scores (N = 168).
Age was not a statistically significant predictor in the model. The interaction between PCL-5 trauma scores and RIS scores was significant, indicating a moderating effect on BARC scores (β = 1.037, p = .028). In general, higher recovery identity scores were associated with higher BARC scores (β = .452, p < .001), and higher PCL-5 trauma scores were associated with lower BARC scores (β = −1.176, p = .012). However, inspection of the significant interaction between trauma and recovery identity indicated that RIS scores were more strongly associated with RC among participants with PCL-5 scores above the clinical cutoff (see Figure 1). Thus, when RIS values were high, these participants were likely to report similar levels of RC as participants below the clinical cutoff, while participants above the cutoff with low levels of RIS were likely to report less RC.
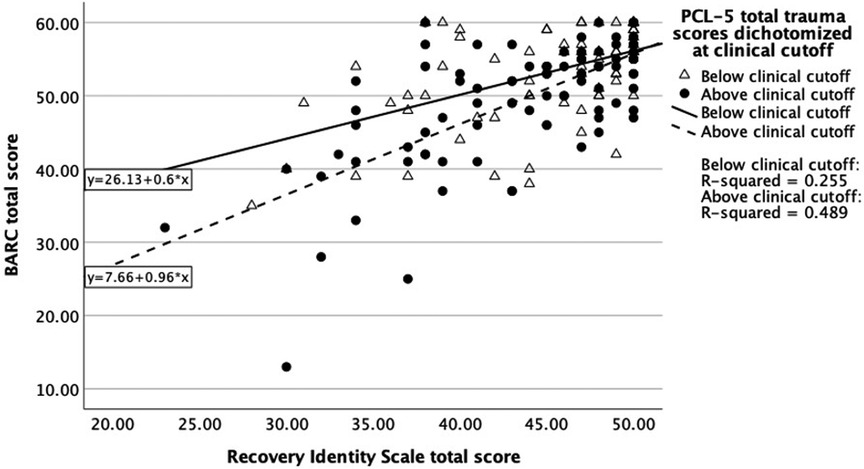
Figure 1. Baseline brief assessment of recovery capital scores by recovery identity scale scores dichotomized at clinical trauma cutoff (N = 168).
Measures of recovery support were used to predict RIS scores using linear regression in the second model. Descriptive statistics for all model variables are provided in Table 1, and full model results are presented in Table 3. The model with all of the variables explained 19.5% of recovery identity scale scores in CRP participants [R2 = .195, F(8,151) = 4.566, p < .001]. Staff care, safe environment, non-recovery peer support, family support, and age were not statistically significant predictors of RIS scores in the model. Perceiving CRP staff as effective role models for students in recovery (β = .364, p = .043), having recovery support from peers who are in recovery (β = .191, p = .015), and having recovery support from mentors were all associated with higher recovery identity scores (β = .031, p = .006).
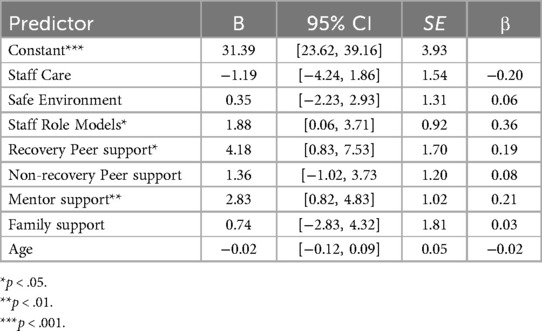
Table 3. Linear regression of types of recovery support on recovery identity scale scores (N = 168).
4 Discussion and implications
4.1 Summary of key findings
This study examined how trauma and recovery identity interact to influence levels of recovery capital among CRP students. Consistent with our hypotheses, having a stronger recovery identity predicted greater RC, while having higher trauma symptom severity was associated with lower recovery capital. However, the negative relationship between trauma and RC was significantly moderated by recovery identity, such that stronger recovery identity buffered against the adverse effects of trauma on students' RC. Further, consistent with hypotheses, our findings also suggest that recovery supports—both with CRP staff and peer recovery support—predict stronger recovery identity. This aligns with existing literature and suggests a potential mechanism by which supportive relationships in collegiate recovery facilitate accrual of RC. Findings underscore the importance of intentionally bolstering structured recovery supports within CRPs. By leveraging the therapeutic relationship as well as personal lived experiences, staff can help students cope with past traumas, facilitate healing, and foster identity growth as a person in recovery from both addiction and trauma. Ultimately, promoting stronger recovery identities through therapeutic relationships may be a key strategy in bolstering recovery capital and sustaining long-term stability in collegiate recovery environments.
4.2 Theoretical implications: a call for expansion of the recovery capital model for young adults in recovery
4.2.1 The trauma-informed RC framework
These findings broaden existing RC models by emphasizing the impact of trauma on recovery pathways. While traditional RC frameworks primarily focus on individual, social, and community assets (2), integrating a trauma-informed lens reveals how trauma experiences can fundamentally shape how individuals perceive, develop, and utilize these resources. A trauma-informed Recovery Capital model could redefine elements of RC to incorporate principles of psychological safety, trustworthiness, empowerment, and relational healing and post-traumatic growth. Learning from existing trauma-informed approaches in treatment centers suggests the need for CRPs to adopt explicit practices such as staff training, trauma-sensitive environmental design, clearly articulated policies, and trauma-informed peer support systems (74, 75).
By linking Recovery Capital and recovery identity to post-traumatic growth (PTG) theories (76, 77), this model highlights the role of stress-buffering processes and self-determination theory as essential components of sustainable recovery. Recovery from both SUDs and trauma involves a process of narrative revision or “restorying” and “acceptance of a changed world” through self-reflection and social relationships, resulting in identity development (77).
4.2.2 Recovery identity as a protective factor
CRPs provide a unique opportunity to support students in addressing the impact of substance-related trauma while fostering personal growth and connection through peer and mentor relationships that strengthen recovery identity and promote resilience. The concept of recovery identity, rooted in social identity theory (8), is a key factor in young adults' recovery trajectories. Environments, like CRPs that foster autonomy, competence, and relatedness can help individuals reclaim agency over their recovery narratives, reinforcing resilience and positive identity transformation. Learning from trauma-informed approaches in treatment centers, CRPs can integrate explicit practices such as staff training, trauma-sensitive environmental design, clearly articulated policies, and trauma-informed peer support systems to create a more effective, recovery-supportive context.
4.2.3 Building recovery capital through socio-ecological systems: the role of CRPs
Building on the work of Witkiewitz and Tucker (78), which argues for a broader behavioral ecological perspective in understanding recovery, CRPs emerge as critical place-based interventions that provide the built-in social and structural support necessary for sustaining long-term recovery. Their work challenges the narrow focus on individual-level abstinence and instead highlights the importance of dynamically varying environmental factors—such as community, neighborhood influences, and social determinants of health—in shaping recovery trajectories. CRPs exemplify this approach by embedding students in an ecological system that fosters recovery through stable peer networks, structured support, and institutional backing, thereby reinforcing both recovery identity and recovery capital in ways that go beyond the individual as the sole change agent. Situational and environmental factors, further underscore that both trauma recovery and substance use disorder (SUD) recovery are deeply social and place-based processes (79, 80). Recovery occurs both from the inside out—through shifts in cognition, self-perception, and identity—and from the outside in, as individuals engage with external systems of support. Social support has been consistently identified in the literature as a buffer against PTSD, highlighting the protective role of recovery-supportive environments in mitigating trauma's long-term effects.
Together, these insights call for a theoretical expansion of Recovery Capital frameworks that actively acknowledge trauma, social environments, and cognitive transformation as central and interconnected components in shaping sustainable recovery trajectories.
4.3 Implications for practice and policy
4.3.1 Peer support and mentorship as “Just in Time” interventions
The findings from this study align with Laudet et al. (81), who emphasized that peer relationships—such as mentors, peer support networks, and structured sober social activities—represent core components of recovery capital within CRPs. Their research demonstrated that students primarily joined CRPs seeking same-age peer support to navigate recovery within a challenging collegiate environment, underscoring the critical role of supportive peer relationships in maintaining sobriety and academic engagement. Students with trauma may particularly benefit from CRPs' peer networks, as these environments normalize recovery experiences, promote positive identity transformation, and reinforce long-term well-being.
Peer support and mentoring services in CRPs may potentially operate as immediate, small-dose interventions outside of what we traditionally consider formal treatment, where students experiencing trauma triggers can receive support in the moment, preventing escalation, preventing the need to numb emotions, and reinforcing their recovery identity. Thus, these interactions may help students navigate the often intertwined nature of both SUD and trauma recovery and act as a buffer against long-term trauma effects by fostering a supportive community that promotes recovery identity and engagement.
4.3.2 For CRP staff and peers
For collegiate recovery professionals and potentially for other peer recovery specialists, this study highlights a potentially unique and powerful benefit to peer support. CRP staff might consider prioritizing interventions and programming that strengthen recovery identity as an indirect trauma intervention that supports long term recovery. This might include providing recovery speakers at on campus events, having a visible recovery presence on campus, providing tangible supports like scholarships that show that universities value students in recovery, and providing service opportunities that allow students to see how their recovery can impact others. On its own, the presence of the CRP staff member in recovery may be an intervention in and of itself. While peer support in CRPs do not directly address trauma, it provides a critical social support network that facilitates a deeper recovery identity and more posttraumatic growth.
Additionally, the long-term nature of CRP support offers an important model for other SUD interventions, and this study may highlight a way that longer term interventions facilitate healing from trauma. CRP staff, who are usually not working in clinical roles, also will benefit from knowing that though many of their students are functioning as well as other students with less serious trauma histories, these past traumas may still require further clinical attention, and staff should be prepared to recognize trauma responses and facilitate next steps for support as need arises.
For those working with individuals seeking recovery from substance use disorders, the impact of helping people adopt a recovery identity without positive examples of people in recovery or a community of recovery may be limited. For people without lived experience, this highlights potential for the additional impact of partnering with people in recovery to deliver recovery support services or introducing individuals to recovery communities. Additionally, for those in recovery working in clinical roles rather than peer support roles, this study may support why it may be helpful to disclose personal recovery status as a part of care.
4.3.3 Building a strong, trauma-responsive peer recovery workforce
The findings of this work highlight the role of peer mentors, social support and recovery networks in buffering the impact of trauma on RC, and indicate that a trained, competent, and well-supported peer workforce is critical to ensure long term positive outcomes. Paid peer support specialists are critical components of the staff structures of many recovery community organizations—including CRPs—but experience high turnover rates related to low compensation, little training opportunities, and feeling undervalued by clinical staff (82). This high rate of turnover has significant implications based in the findings of this study, which emphasize the need for stable, supportive therapeutic relationships with peers in recovery. The lack of standardization in certification for peer recovery support specialists across the U.S. (83) and the need for training opportunities specifically designed for peer recovery support specialists that can support professional certification through continuing education credits are two additional and related issues highlighted by these findings. In particular, there is a need for standardized training around the role of peer support workers in recovery identity development, the impacts of a variety of trauma experiences and symptoms on recovery, and on specific trauma-related skillsets such as adverse childhood experiences (both individual- and community-level) and trauma-informed systems of care (84–86), all of which can be integrated into professional certification. The recovery field in general and CRPs specifically can benefit from investing in training, professional certification, and support for peer recovery support specialists. This investment is vital for maximizing impact on recovery outcomes and trauma healing within CRPs and in other recovery settings.
4.4 Future research
For scientists, these findings should drive more research into recovery identity, including studies that examine the environments in which recovery identity is formed, such as impacts of density and frequency of contact with people in recovery. Studies might also assess differences in outcomes in treatment environments with and without staff that are open about their recovery. It should also encourage further investigation into how trauma history and current presentation drive longer term recovery outcomes and how recovery identity shifts over time. Scientists should also examine whether this mechanism continues to function in areas outside of collegiate recovery or if the particular context of education and recovery identity is a driver of this outcome.
For policymakers, this research points to a potential unique mechanism through which peer services benefit individuals. Further, for administrators hiring collegiate recovery professionals and for hiring in other health related professions lived experience in recovery should be considered a significant asset. This also points to the need for standardization of professional peer service providers, which varies substantially across states. This professionalization and standardization can help mitigate and perceived risks of peer-based services, while continued research in this area can help further legitimize this work. The study highlights that individuals with severe SUDs have very high rates of trauma and that trauma related training is a necessity for anyone working with this population. These implications point to the overarching need for increased compensation and advancement opportunities for collegiate recovery professionals and other peer recovery specialists, as these potentially unique contributions added to continued training and development in other areas may lead to exceptional outcomes. Unfortunately, current compensation and advancement opportunities often lead to individuals leaving collegiate recovery for other professions. This also highlights the negative impact of turnover on students in CRPs which typically have 1–2 staff members, as a significant amount of the impact of these programs may be driven by the staff relationship.
4.5 Limitations and future directions
While our findings provide important insights into recovery identities, trauma and recovery capital, and its implications, several limitations must be acknowledged.
Selection bias is a key consideration, as individuals with a strong recovery identity may be more likely to participate in study. Future research should assess potential self-selection effects and consider strategies to capture a more diverse sample. Related to this, it is important to note that many people who have resolved a SUD do not identify as being “in recovery” (30, 78), which may impact the development of a recovery identity, and may also impact likelihood of belonging to a CRP to begin with. According to Kelly et al. (30), only 46% of individuals who have resolved an SUD self-identify as being “in recovery”, suggesting that the concept of recovery identity may not fully encompass all individuals with lived experience. Future research should address potential self-selection effects and implement strategies to capture a more diverse sample of people who may have resolved a SUD but do not identify as being “in recovery”.
Another limitation of this study is the use of the short form of the Posttraumatic Stress Disorder Checklist (PCL-5; see text footnote 1) to measure trauma symptomatology. While the short-form PCL-5 provides an efficient screening tool for PTSD symptoms, it may not capture the full complexity and severity of post-traumatic stress responses. The abbreviated nature of the measure may limit its sensitivity to certain symptom clusters, such as avoidance, hyperarousal, and negative alterations in mood and cognition, which are critical components of PTSD as outlined in the DSM-5. Additionally, this measure focuses on PTSD symptoms rather than broader trauma exposure, meaning it does not account for cumulative or complex trauma experiences that may contribute to psychological distress. Finally, occurrence of traumatic experiences earlier in childhood and earlier onset of trauma symptoms can have profound impacts on identity formation in general (87, 88), and may impact the formation of recovery identity. A more comprehensive assessment, such as the full PCL-5, or broader trauma measures that capture early lifetime exposures, like the original and expanded Adverse Childhood Experiences (ACEs) scales (84, 85), could provide a more nuanced understanding of trauma's impact. Future research should consider utilizing more extensive trauma assessments to ensure a deeper and more accurate evaluation of trauma symptomatology.
Additionally, our study does not disaggregate the Recovery Identity Scale into distinct subcategories that potentially describe different aspects of forming a recovery identity. A refined, multidimensional approach that examines how these three aspects (commitment to recovery identity, in-depth exploration of recovery identity, and reconsideration of recovery commitment) may facilitate accumulation of recovery capital and buffer the impact of trauma on recovery outcomes is needed. In particular, this multidimensional conceptualization of recovery identity emphasizes the adaptive process of exploring current commitments to maintain and validate existing identities (65). Thus, a person may attempt to change current commitments (i.e., identities), which are not satisfactory and no longer meet their needs. This process of reconsidering one's identity commitments strongly aligns with the fundamental shift from social groups defined by substance use toward recovery-supportive groups described in the Social Identity Model of Recovery (8). Understanding the factors that facilitate and support in-depth exploration and reconsideration of identity commitments can offer further opportunities for interventions aimed at increasing social capital, especially in the early stages of recovery. Our research team is currently engaged in a more in-depth examination of the RIS scale development and future plans include exploring how various dimensions of recovery identity and recovery capital interact over time.
While the sample for this study is quite diverse in terms of gender and age, it is less racially diverse than hoped for. This is a common, known problem in studies of this population (5, 11, 81), with study samples skewing towards a majority of white participants compared to other racial and ethnic groups. It would be useful to replicate this analysis in a more racially-diverse sample, and to explore the potential interplay of recovery identity and racial identity in the context of trauma.
Finally, post-traumatic growth is an important yet underexplored area within recovery research. Future studies could examine how individuals experience post-traumatic growth at different stages of recovery and whether these trajectories vary across different populations. Currently, we lack the necessary data to make such comparisons, highlighting the need for more longitudinal and mixed-methods research in this domain.
4.6 Conclusion
This study identified that recovery identity buffers the impact of trauma symptomatology and recovery capital for students involved in CRPs such that students with high levels of trauma and with strong recovery identities experienced similar levels of recovery capital as students with sub-clinical trauma levels. In addition, this study highlighted supportive relationships with CRP staff and peers in recovery as important predictors of strong recovery identity for this population. These findings underscore the need for CRPs to build a strong, trauma-informed peer recovery workforce that can leverage the therapeutic relationship to better support students in managing trauma, building strong recovery identities, and developing recovery capital within the collegiate recovery environment.
Data availability statement
The raw data supporting the conclusions of this article will be made available by the authors, without undue reservation.
Ethics statement
The studies involving humans were approved by Virginia Commonwealth University Institutional Review Board. The studies were conducted in accordance with the local legislation and institutional requirements. The participants provided their written informed consent to participate in this study.
Author contributions
MF: Conceptualization, Investigation, Supervision, Project administration, Methodology, Funding acquisition, Formal analysis, Writing – review & editing, Visualization, Writing – original draft, Validation. RS: Data curation, Methodology, Project administration, Conceptualization, Writing – original draft, Funding acquisition, Formal analysis, Writing – review & editing, Investigation. RM: Writing – original draft, Data curation, Conceptualization, Writing – review & editing, Formal analysis. Y-LY: Writing – review & editing, Conceptualization, Investigation, Methodology, Writing – original draft, Data curation, Formal analysis, Project administration. TB: Project administration, Writing – original draft, Supervision, Validation, Investigation, Conceptualization, Writing – review & editing, Funding acquisition. VB: Writing – review & editing, Writing – original draft, Conceptualization. MC: Writing – review & editing, Validation, Resources, Writing – original draft. KK: Resources, Writing – original draft, Validation, Writing – review & editing. OL: Writing – original draft, Writing – review & editing. DM: Writing – original draft, Writing – review & editing. MP: Conceptualization, Writing – review & editing, Writing – original draft.
Funding
The author(s) declare that financial support was received for the research and/or publication of this article. The project described was supported by a grant from the Office of Research at the School of Social Work at Virginia Commonwealth University.
Conflict of interest
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
Generative AI statement
The author(s) declare that no Generative AI was used in the creation of this manuscript.
Publisher's note
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
Footnote
1. ^Cleveland M, Burns V, Bom, Francis MW, LaBelle O, Bannard T, et al. Adapting the Utrecht-management of identity commitments scale to assess recovery identity: results from a national study of collegiate recovery students. Psychol Addict Behav.
References
1. American College Health Association. American College Health Association-National College Health Assessment III: Undergraduate Student Reference Group Executive Summary Spring 2024. Silver Spring, MD: American College Health Association (2024). Available online at: https://www.acha.org/wp-content/uploads/NCHA-IIIb_SPRING_2024_UNDERGRADUATE_REFERENCE_GROUP_EXECUTIVE_SUMMARY.pdf
2. Hennessy EA. Recovery capital: a systematic review of the literature. Addict Res Theory. (2017) 25(5):349–60. doi: 10.1080/16066359.2017.1297990
3. Cloud W, Granfield R. Conceptualizing recovery capital: expansion of a theoretical construct. Subst Use Misuse. (2008) 43(12–13):1971–86. doi: 10.1080/10826080802289762
5. Hennessy EA, Nichols LM, Brown TB, Tanner-Smith EE. Advancing the science of evaluating collegiate recovery program processes and outcomes: a recovery capital perspective. Eval Program Plann. (2022) 91:102057. doi: 10.1016/j.evalprogplan.2022.102057
6. Kelly JF, Hoeppner B. A biaxial formulation of the recovery construct. Addict Res Theory. (2015) 23(1):5–9. doi: 10.3109/16066359.2014.930132
7. Arnett JJ. Emerging adulthood: a theory of development from the late teens through the twenties. Am Psychol. (2000) 55(5):469–80. doi: 10.1037/0003-066X.55.5.469
8. Best D, Beckwith M, Haslam C, Alexander Haslam S, Jetten J, Mawson E, et al. Overcoming alcohol and other drug addiction as a process of social identity transition: the social identity model of recovery (SIMOR). Addict Res Theory. (2016) 24(2):111–23. doi: 10.3109/16066359.2015.1075980
9. Hennessy EA, George S, Klein M, O’Connor J, Eddie D, Kelly JF. A systematic review of recovery high schools and collegiate recovery programs for building recovery capital among adolescents and emerging adults. Front Adolesc Med. (2025) 3:1522678. doi: 10.3389/fradm.2025.1522678
10. Workman CL. “Knowing where we’ve been, and what we’ve overcome is key”: the role of campus environment on development of recovery identity in members of a collegiate recovery program (Doctoral dissertation). University of Wisconsin, Madison, WI (2020).
11. Vest N, Reinstra M, Timko C, Kelly J, Humphreys K. College programming for students in addiction recovery: a PRISMA-guided scoping review. Addict Behav. (2021) 121:106992. doi: 10.1016/j.addbeh.2021.106992
12. Burns VF, Tye S, Ingrid S, Hadad N. Recovery is complicated”: a qualitative exploration of Canadian university Students’ diverse recovery experiences. Alcohol Treat Q. (2024) 42(3):359–76. doi: 10.1080/07347324.2024.2347241
13. Park M, Fudjack S, Soucie K, LaBelle O. Participant experiences in student recovery programs in Canada: an interpretative phenomenological analysis. Alcohol Treat Q. (2023) 41(3):338–61. doi: 10.1080/07347324.2023.2204819
14. Day E, Trainor L. Recovery from addiction on a university campus—a UK perspective. Alcohol Treat Q. (2024) 42(4):495–508. doi: 10.1080/07347324.2024.2364694
15. Putnam R. Bowling alone: america’s declining social capital. In: Crothers L, Lockhart C, editors. Culture and Politics. New York: Palgrave Macmillan (2000):223–34. doi: 10.1007/978-1-349-62965-7_12
16. Smith RL, Bannard T, McDaniel J, Aliev F, Brown A, Holliday E, et al. Characteristics of students participating in collegiate recovery programs and the impact of COVID-19: an updated national longitudinal study. Addict Res Theory. (2024) 32(1):58–67. doi: 10.1080/16066359.2023.2216459
17. Stall R, Biernacki P. Spontaneous remission from the problematic use of substances: an inductive model derived from a comparative analysis of the alcohol, opiate, tobacco, and food/obesity literatures. Int J Addict. (1986) 21(1):1–23. doi: 10.3109/10826088609063434
18. Koski-Jännes A. Social and personal identity projects in the recovery from addictive behaviors. Addict Res Theory. (2002) 10(2):183–202. doi: 10.1080/16066350290017266
19. Chen G. Identity construction in recovery from substance use disorders. J Psychoactive Drugs. (2024) 56(1):109–16. doi: 10.1080/02791072.2022.2159592
20. Best D, Lubman DI, Savic M, Wilson A, Dingle G, Haslam SA, et al. Social and transitional identity: exploring social networks and their significance in a therapeutic community setting. Ther Communities Int J Ther Communities. (2014) 35(1):10–20. doi: 10.1108/TC-04-2013-0007
21. Haslam C, David B, Dingle A, Staiger G, Petra K, Michael S, et al. Social group membership before treatment for substance dependence predicts early identification and engagement with treatment communities. Addict Res Theory. (2019) 27(5):363–72. doi: 10.1080/16066359.2018.1537393
22. Beckwith M, Best D, Savic M, Haslam C, Bathish R, Dingle G, et al. Social identity mapping in addiction recovery (SIM-AR): extension and application of a visual method. Addict Res Theory. (2019) 27(6):462–71. doi: 10.1080/16066359.2018.1544623
23. Blyth SH, Cowie K, Jurinsky J, Hennessy EA. A qualitative examination of social identity and stigma among adolescents recovering from alcohol or drug use. Addict Behav Rep. (2023) 18:100505. doi: 10.1016/j.abrep.2023.100505
24. Hennessy EA, Jurinsky J, Cowie K, Pietrzak A, Blyth S, Krasnoff P. Visualizing the influence of social networks on recovery: a mixed-methods social identity mapping study with recovering adolescents. Subst Use Misuse. (2024) 59(9):1405–15. doi: 10.1080/10826084.2024.2352618
25. Ingram PF, Finn PR. The nomological network of drinker identity: a scoping review. Addict Behav. (2023) 141:107654. doi: 10.1016/j.addbeh.2023.107654
26. Buckingham SA, Frings D, Albery IP. Group membership and social identity in addiction recovery. Psychol Addict Behav. (2013) 27(4):1132–40. doi: 10.1037/a0032480
27. Frings D, Albery IP. The social identity model of cessation maintenance: formulation and initial evidence. Addict Behav. (2015) 44:35–42. doi: 10.1016/j.addbeh.2014.10.023
28. Dingle GA, Stark C, Cruwys T, Best D. Breaking good: breaking ties with social groups may be good for recovery from substance misuse. Br J Soc Psychol. (2015) 54(2):236–54. doi: 10.1111/bjso.12081
29. Mawson E, Best D, Beckwith M, Dingle GA, Lubman DI. Social identity, social networks and recovery capital in emerging adulthood: a pilot study. Subst Abuse Treat Prev Policy. (2015) 10(1):45. doi: 10.1186/s13011-015-0041-2
30. Kelly JF, Abry AW, Milligan CM, Bergman BG, Hoeppner BB. On being “in recovery”: a national study of prevalence and correlates of adopting or not adopting a recovery identity among individuals resolving drug and alcohol problems. Psychol Addict Behav J Soc Psychol Addict Behav. (2018) 32(6):595–604. doi: 10.1037/adb0000386
31. Folkman S. Personal control and stress and coping processes: a theoretical analysis. J Pers Soc Psychol. (1984) 46(4):839–52. doi: 10.1037/0022-3514.46.4.839
33. White WL, Cloud W. Recovery capital: a primer for addictions professionals. Counselor. (2008) 9(5):22–7.
34. Kaskutas LA, Borkman TJ, Laudet A, Ritter LA, Witbrodt J, Subbaraman MS, et al. Elements that define recovery: the experiential perspective. J Stud Alcohol Drugs. (2014) 75(6):999–1010. doi: 10.15288/jsad.2014.75.999
35. Laudet A, Morgen K, White WL. The role of social supports, spirituality, religiousness, life meaning and affiliation with 12-step fellowships in quality of life satisfaction among individuals in recovery from alcohol and drug problems. Alcohol Treat Q. (2006) 24(1–2):33–73. doi: 10.1300/J020v24n01_04
36. Granfield R, Cloud W. Social context and “natural recovery”: the role of social capital in the resolution of drug-associated problems. Subst Use Misuse. (2001) 36(11):1543–70. doi: 10.1081/JA-100106963
37. Neale J, Panebianco D, Finch E, Marsden J, Mitcheson L, Rose D, et al. Emerging consensus on measuring addiction recovery: findings from a multi-stakeholder consultation exercise. Drugs Educ Prev Policy. (2016) 23(1):31–40. doi: 10.3109/09687637.2015.1100587
38. Hendershot CS, Witkiewitz K, George WH, Marlatt GA. Relapse prevention for addictive behaviors. Subst Abuse Treat Prev Policy. (2011) 6(1):17. doi: 10.1186/1747-597X-6-17
39. Brady KT, Back SE, Coffey SF. Substance abuse and posttraumatic stress disorder. Curr Dir Psychol Sci. (2004) 13(5):206–9. doi: 10.1111/j.0963-7214.2004.00309.x
40. Substance Abuse and Mental Health Services Administration. Substance use Disorder Treatment for People with co-occurring disorders, Updated 2020 Treatment Improvement Protocol Tip 42. Bethesda, MD: SAMHSA (2020). (Treatment Improvement Protocol (TIP) Series). Available online at: https://library.samhsa.gov/sites/default/files/pep20-02-01-004.pdf
41. Ouimette P, Read JP. Trauma and Substance Abuse: Causes, Consequences, and Treatment of Comorbid Disorders. Second. Washington, D.C: American Psychological Association (2014).
42. Welsh JW, Knight JR, Hou SSY, Malowney M, Schram P, Sherritt L, et al. Association between substance use diagnoses and psychiatric disorders in an adolescent and young adult clinic-based population. J Adolesc Health. (2017) 60(6):648–52. doi: 10.1016/j.jadohealth.2016.12.018
43. Stewart SH. Alcohol abuse in individuals exposed to trauma: a critical review. Psychol Bull. (1996) 120(1):83–112. doi: 10.1037/0033-2909.120.1.83
44. Broekhof R, Nordahl HM, Tanum L, Selvik SG. Adverse childhood experiences and their association with substance use disorders in adulthood: a general population study (young-HUNT). Addict Behav Rep. (2023) 17:100488. doi: 10.1016/j.abrep.2023.100488
45. Degenhardt L, Bharat C, Bruno R, Glantz MD, Sampson NA, Lago L, et al. Concordance between the diagnostic guidelines for alcohol and cannabis use disorders in the draft ICD-11 and other classification systems: analysis of data from the WHO’s world mental health surveys. Addiction. (2019) 114(3):534–52. doi: 10.1111/add.14482
46. Merrick MT. Vital signs: estimated proportion of adult health problems attributable to adverse childhood experiences and implications for prevention — 25 states, 2015–2017. MMWR Morb Mortal Wkly Rep. (2019) 68:999–1005. doi: 10.15585/mmwr.mm6844e1
47. Kessler RC, Chiu WT, Demler O, Walters EE. Prevalence, severity, and comorbidity of 12-month DSM-IV disorders in the national comorbidity survey replication. Arch Gen Psychiatry. (2005) 62(6):617–27. doi: 10.1001/archpsyc.62.6.617
48. Keyes KM, Eaton NR, Krueger RF, McLaughlin K, Wall MM, Grant BF, et al. Childhood adversities and the structure of common psychiatric disorders. Compr Psychiatry. (2011) 52(6):e8. doi: 10.1016/j.comppsych.2011.04.028
49. Cicchetti D, Handley ED. Child maltreatment and the development of substance use and disorder. Neurobiol Stress. (2019) 10:100144. doi: 10.1016/j.ynstr.2018.100144
50. Francis MW, McCutcheon VV, Farkas KJ. Social processes during recovery: an expansion of Kelly and Hoeppner’s biaxial formulation of recovery. Addict Res Theory. (2023) 31(6):416–23. doi: 10.1080/16066359.2023.2195641
51. Wang Y, Chung MC, Wang N, Yu X, Kenardy J. Social support and posttraumatic stress disorder: a meta-analysis of longitudinal studies. Clin Psychol Rev. (2021) 85:101998. doi: 10.1016/j.cpr.2021.101998
52. Cohen S, Wills TA. Stress, social support, and the buffering hypothesis. Psychol Bull. (1985) 98(2):310–57. doi: 10.1037/0033-2909.98.2.310
53. Kiecolt-Glaser JK, Wilson SJ. Lovesick: how Couples’ relationships influence health. Annu Rev Clin Psychol. (2017) 13(2017):421–43. doi: 10.1146/annurev-clinpsy-032816-045111
54. Umberson D, Crosnoe R, Reczek C. Social relationships and health behavior across the life course. Annu Rev Sociol. (2010) 36(2010):139–57. doi: 10.1146/annurev-soc-070308-120011
55. Smith RL, Dick DM, Amstadter A, Thomas N, Group the S for SW, Salvatore JE. A longitudinal study of the moderating effects of romantic relationships on the associations between alcohol use and trauma in college students. Addiction. (2021) 116(11):3008–18. doi: 10.1111/add.15490
56. Cohen S. Social relationships and health. Am Psychol. (2004) 59(8):676–84. doi: 10.1037/0003-066X.59.8.676
57. Ditzen B, Heinrichs M. Psychobiology of social support: the social dimension of stress buffering. Restor Neurol Neurosci. (2014) 32(1):149–62. doi: 10.3233/RNN-139008
58. Umberson D, Karas Montez J. Social relationships and health: a flashpoint for health policy. J Health Soc Behav. (2010) 51(1):S54–66. doi: 10.1177/0022146510383501
59. Robles TF, Slatcher RB, Trombello JM, McGinn MM. Marital quality and health: a meta-analytic review. Psychol Bull. (2014) 140(1):140–87. doi: 10.1037/a0031859
60. Bliuc AM, Best D, Iqbal M, Upton K. Building addiction recovery capital through online participation in a recovery community. Soc Sci Med. (2017) 193:110–7. doi: 10.1016/j.socscimed.2017.09.050
61. Harris PA, Taylor R, Thielke R, Payne J, Gonzalez N, Conde JG. Research electronic data capture (REDCap)—a metadata-driven methodology and workflow process for providing translational research informatics support. J Biomed Inform. (2009) 42(2):377–81. doi: 10.1016/j.jbi.2008.08.010
62. Harris PA, Taylor R, Minor BL, Elliott V, Fernandez M, O’Neal L, et al. The REDCap consortium: building an international community of software platform partners. J Biomed Inform. (2019) 95:103208. doi: 10.1016/j.jbi.2019.103208
63. Groshkova T, Best D, White W. The assessment of recovery capital: properties and psychometrics of a measure of addiction recovery strengths. Drug Alcohol Rev. (2013) 32(2):187–94. doi: 10.1111/j.1465-3362.2012.00489.x
64. Vilsaint CL, Kelly JF, Bergman BG, Groshkova T, Best D, White W. Development and validation of a brief assessment of recovery capital (BARC-10) for alcohol and drug use disorder. Drug Alcohol Depend. (2017) 177:71–6. doi: 10.1016/j.drugalcdep.2017.03.022
65. Crocetti E, Schwartz SJ, Fermani A, Meeus W. The Utrecht-management of identity commitments scale (U-MICS). Eur J Psychol Assess. (2010) 26(3):172–86. doi: 10.1027/1015-5759/a000024
66. Zuromski KL, Ustun B, Hwang I, Keane TM, Marx BP, Stein MB, et al. Developing an optimal short-form of the PTSD checklist for DSM-5 (PCL-5). Depress Anxiety. (2019) 36(9):790–800. doi: 10.1002/da.22942
67. Francis MW, Smith R, Yang YL, Miola R. The national longitudinal collegiate recovery study. College students in AOSUD recovery: characteristics and trajectories [symposium abstract]. Alcohol Clin Exp Res. (2024) 48(S1):11–141. doi: 10.1111/acer.15316
68. Mickey RM, Greenland S. The impact of confounder selection criteria on effect estimation. Am J Epidemiol. (1989) 129(1):125–37. doi: 10.1093/oxfordjournals.aje.a115101
70. Curran PJ, West SG, Finch JF. The robustness of test statistics to nonnormality and specification error in confirmatory factor analysis. Psychol Methods. (1996) 1(1):16–29. doi: 10.1037/1082-989X.1.1.16
71. Cohen J. Applied Multiple Regression/Correlation Analysis for the Behavioral Sciences. 3rd ed Mahwah, N.J: L. Erlbaum Associates (2003).
72. Lomax RG, Hahs-Vaughn DL. An introduction to Statistical Concepts. 3rd ed. New York: Routledge (2012).
73. King J. Binary logistic regression. In: Osborne J, editor. Best Practices in Quantitative Methods. Thousand Oaks, CA: Sage (2008). p. 358–84.
74. Bartholow LAM, Huffman RT. The necessity of a trauma-informed paradigm in substance use disorder services. J Am Psychiatr Nurses Assoc. (2021) 29(6):470–47. doi: 10.1177/10783903211036496
75. López-Castro T, Hu MC, Papini S, Ruglass LM, Hien DA. Pathways to change: use trajectories following trauma-informed treatment of women with co-occurring post-traumatic stress disorder and substance use disorders. Drug Alcohol Rev. (2015) 34(3):242–51. doi: 10.1111/dar.12230
76. Tedeschi RG, Calhoun LG. The posttraumatic growth inventory: measuring the positive legacy of trauma. J Trauma Stress. (1996) 9(3):455–71. doi: 10.1002/jts.2490090305
77. Tedeschi RG, Shakespeare-Finch J, Taku K. Posttraumatic Growth: Theory, Research and Applications. 1st ed. New York: Routledge (2018).
78. Witkiewitz K, Tucker JA. Abstinence not required: expanding the definition of recovery from alcohol use disorder. Alcohol Clin Exp Res. (2020) 44(1):36–40. doi: 10.1111/acer.14235
79. Best D, Irving J, Collinson B, Andersson C, Edwards M. Recovery networks and community connections: identifying connection needs and community linkage opportunities in early recovery populations. Alcohol Treat Q. (2017) 35(1):2–15. doi: 10.1080/07347324.2016.1256718
80. Witkiewitz K, Tucker JA. Whole person recovery from substance use disorder: a call for research examining a dynamic behavioral ecological model of contexts supportive of recovery. Addict Res Theory. (2025) 33(1):1–12. doi: 10.1080/16066359.2024.2329580
81. Laudet AB, Harris K, Kimball T, Winters KC, Moberg DP. In college and in recovery: reasons for joining a collegiate recovery program. J Am Coll Health. (2016) 64(3):238–46. doi: 10.1080/07448481.2015.1117464
82. Castedo de Martell S, Wilkerson JM, Ranjit N, Holleran Steiker L, McCurdy SA, Shelton Brown H III. What we know about the peer workforce and economic evaluation for peer recovery support services: a systematic review. Subst Use Addict J. (2025) 46(1):90–102. doi: 10.1177/29767342241281009
83. Substance Abuse and Mental Health Services Administration. National Model Standards for Peer Support Certification. Rockville, MD: Office of Recovery, Substance Abuse and Mental Health Services Administration (2023). Report No.: PEP23-10-01–001.
84. Cronholm PF, Forke CM, Wade R, Bair-Merritt MH, Davis M, Harkins-Schwarz M, et al. Adverse childhood experiences: expanding the concept of adversity. Am J Prev Med. (2015) 49(3):354–61. doi: 10.1016/j.amepre.2015.02.001
85. Felitti VJ, Anda RF, Nordenberg D, Williamson DF, Spitz AM, Edwards V, et al. Relationship of childhood abuse and household dysfunction to many of the leading causes of death in adults. The adverse childhood experiences (ACE) study. Am J Prev Med. (1998) 14(4):245–58. doi: 10.1016/S0749-3797(98)00017-8
86. Substance Abuse and Mental Health Services Administration. Trauma-Informed Care in Behavioral Health Services. Rockville, MD: Substance Abuse and Mental Health Services Administration (2014). (Treatment Improvement Protocol (TIP) Series 57). Report No.: HHS Publication No. (SMA) 13-4801.
87. Patrick J, Noor A. Impact of adverse childhood experiences on adolescent identity development and mental health outcomes. J Asian Dev Stud. (2024) 13(2):1657–62. doi: 10.62345/jads.2024.13.2.130
Keywords: recovery capital, recovery identity, trauma, collegiate recovery program, social support
Citation: Francis M, Smith R, Miola R, Yang Y-L, Bannard T, Burns V, Cleveland M, Karimova K, LaBelle O, Murphy D and Piccirillo M (2025) Recovery identity as a buffer: mitigating trauma's impact on recovery capital in collegiate recovery programs. Front. Adolesc. Med. 3:1602130. doi: 10.3389/fradm.2025.1602130
Received: 28 March 2025; Accepted: 30 June 2025;
Published: 22 July 2025.
Edited by:
Jo-Hanna H. Ivers, Trinity Biomedical Sciences Institute, Trinity College Dublin, IrelandReviewed by:
Derling Jose Mendoza Velazco, National University of Education, EcuadorDeirdre Osullivan, The Pennsylvania State University (PSU), United States
Copyright: © 2025 Francis, Smith, Miola, Yang, Bannard, Burns, Cleveland, Karimova, LaBelle, Murphy and Piccirillo. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Meredith Francis, ZnJhbmNpc213M0B2Y3UuZWR1
 Meredith Francis
Meredith Francis Rebecca Smith
Rebecca Smith Rose Miola
Rose Miola Ya-Li Yang
Ya-Li Yang Thomas Bannard
Thomas Bannard Victoria Burns2
Victoria Burns2 Michael Cleveland
Michael Cleveland Konul Karimova
Konul Karimova Onawa LaBelle
Onawa LaBelle Marilyn Piccirillo
Marilyn Piccirillo